Abstract
The Paralympic boccia is a sport played by athletes with spasticity and severe impairment in the four limbs. Three (BC1, BC2, and BC3) of the four classes in boccia allow People with Cerebral Palsy (CP) to participate. The ranking is performed manually through the American Spasticity Scale. Like all qualitative scales, however, this evokes controversy among the evaluation board members who apply it, altering the classification of the athletes. A helpful option would be the use of mechanomyography (MMG), a method of acquiring muscle vibrations quantitatively based on accelerometers. Thus, the objective of this article was to conduct a pilot study analyzing the differences in the MMG signals of flexors and extensors muscles between two groups: 6 boccia athletes with spasticity and 6 non-impaired. Volunteers remained seated on the wheelchair, with their elbow bent close to 90°. They were verbally stimulated to perform the manual grip by pressing the evaluator’s hand while the MMG signals were recorded and stored. The mean MMGRMS descriptor was calculated for each signal. The experimental tests indicated differences between the two groups. For the spasticity group: 0.4058 and 0.4258 mV for the left flexor and extensor wrist muscles, respectively; 0.4215 and 0.4529 mV for the right flexor and extensor wrist muscles, respectively. For the non-impaired group, the MMGRMS was 0.3694 and 0.3945 mV for the left flexor and extensor wrist muscles, respectively; 0.35033 and 0.3728 mV for the right flexor and extensor wrist muscles, respectively. Thus, these results indicate greater spasticity for the spastic group and so, volunteers classification in lower levels.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Paralympic boccia is a sport played by athletes with severe impairment in all four limbs and spasticity. Three of the four classes in boccia allow People with Cerebral Palsy to participate. Athletes of classes BC1 and BC2 hold the ball to the throw. In class BC3, assistive devices, such as a ramp, are allowed – in this case, the athlete may have strength, but not enough coordination to throw a ball manually [1]. These classifications are based on functional evaluations carried out by skilled physiotherapists using the ASAS scale (Australian Spasticity Assessment Scale), but still in a qualitative manner, which sometimes leads to disagreement among physiotherapists as to which class an athlete can belong to. This may have an impact on winning a Paralympic medal. Faced with the subjectivity of the evaluation process, quantitative data are performed and recommended. Quantitative measures of spasticity can be taken by biomechanical and neurophysiological approaches [2,3,4]. The biomechanical approaches use high-cost devices (such as isokinetics), a restriction that frequently makes their use infeasible in places of classification before the competition. The neurophysiological approaches take into account the neural aspects, so that further clarification of the correlation between this approach and clinical findings is still required. Thus, there are few quantitative studies on the analysis of spasticity of boccia athletes, which could abate or moderate the divergence during classification.
One option for quantitative analysis, which is currently being studied, is mechanomyography (MMG). MMG is a non-invasive technique that, by means of accelerometric sensors, registers muscle vibrations, and has been used in several studies to provide information on muscle strength production, mechanical properties of the muscular system, motor control, muscular atrophy, spasticity, muscular fatigue and other applications [5]. Authors such as Beck et al. [6] and Alves et al. [7] have already demonstrated the effectiveness of MMG for the analysis of muscle contraction.
Therefore, the goal of this study was to investigate the feasibility of using MMG as a quantitative method to evaluate the spasticity in wrist flexors and extensors muscle of boccia athletes during manual gripping.
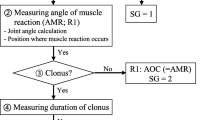
2 Methods
This study is part of a larger project approved by the Human Research Ethics Committee of Pontifícia Universidade Católica do Paraná (CEP-PUCPR) under register 2.745.072/2018. For all procedures, instruction and familiarization were offered when necessary. Data collection was carried at Association of Physically Disabled People of Paraná (ADFP).
Twelve volunteers were selected, divided into two groups: (i) Cerebral Palsy Group (CP), (n = 6, 3 male, 3 female), including Paralympic athletes BC2 and BC3, of both genders, with spasticity; (ii) non-impaired group (NI), (n = 6, 4 male, 2 female), including healthy individuals, ages between 18 and 70 years, of both genders.
2.1 Mechanomyography Acquisition System
For data collection, an MMG equipment, developed by Nogueira-Neto [8] was used, composed by a Freescale MMA7260Q triaxial accelerometers (13 × 18 mm, 0.94 g) with the sensitivity of 800 mV/G (in 1.5 G mode and G = 9.8 m.s−2). The custom hardware provided 2x amplification and a 3rd order 5–50 Hz Butterworth filter. A LabVIEW® virtual instrument acquired the MMG signals through a National Instruments™ NI USB-6221 acquisition board at a sampling frequency of 1 kHz.
2.2 Data Collection
Two MMG sensors were positioned on the volunteer. Sensor 1 was fixed on the skin surface, on the motor point of the wrist flexors and sensor 2, on the motor point of the wrist extensors (Fig. 1-A).
The volunteer remained seated in the wheelchair, with their elbow bent close to 90°, forearm in neutral position and stabilized by the wheelchair’s backrest (Fig. 1-B). The volunteer was instructed to maintain the muscles as maximally relaxed as possible for 3 s and, after this period, he/she was verbally stimulated to perform the manual grip by pressing the evaluator’s hand. Simultaneously, the MMG signals were recorded and stored. The test was performed in two replicates and considered the mean of both MMGRMS signals.
2.3 Data Processing
Signals were selected and processed using MATLAB® software (MathWorks®, Inc. v. R2017b). The analysis window was in the range 1–4 s, with 4000 samples. The triaxial MMG sensor registered vibrations in three orthogonal directions: perpendicular (Z), transverse (X) and longitudinal (Z) to muscle fibers. The MMGRMS was determined for each axis. Then, the MMGRMS 3D module was determined for both CP and NI groups.
3 Results
Figures 1 and 2 show the acquisition of the MMG signals, without processing, for the three axes of muscle vibration of a volunteer. Figure 2 shows the MMG signal for the flexor and extensor muscles of a NI group’s volunteer. Figure 3 shows the MMG signal of the flexor muscle and extensor muscle of a CP group’s volunteer. These figures were generated to illustrate the differences of the signals between the investigated volunteers and also between the muscular groups.
Table 1 shows the magnitude of the MMGRMS for each volunteer, followed by the MMGRMS 3D module for each volunteer of both CP and NI groups.
4 Discussion
The goal of the research described in this article was to investigate possible differences in the MMG signal of wrist flexors and extensors muscles between boccia athletes who present spasticity and non-committed athletes, in order to assist, in the future, in the classification of the athlete for the Paralympic Games, since the traditional manual testing cause divergences due to its subjectivity. It is possible to observe in Table 1 that the resultant mean MMGRMS equivalent voltage for CP group was 0.4058 mV to the left wrist flexor muscles and 0.4258 mV to left wrist extensor muscles, 0.4215 mV to the right wrist flexor muscles and 0.4529 mV to right wrist extensor muscles. Still in Table 1, the mean MMGRMS modulus of NI group was 0.3694 mV to left wrist flexor muscles, 0.3945 mV to left wrist extensor muscles, 0.3503 mV to right wrist flexor muscles, and 0.3728 mV to right wrist extensor muscles.
Mean MMGRMS 3D module of the CP group was greater than the NI group. These results show that MMG can identify the difference between the vibration of muscles of healthy people and people with spasticity. This can also be observed in Fig. 1 so that the amplitude of the signals without processing of the NI group is larger than the CP group. This difference may be related to the changes in muscle mechanical properties and which may influence muscle vibration. Thus, the results corroborate previous studies that investigated the correlation between the assessment of spasticity by the manual test and the mechanomyography signals [9,10,11].
The data were not analyzed statistically because the small sample, but with the sensitivity of the sensor, variations are observed in relation to the mean of the signals, showing the differences between the muscular contractions of volunteers with and without spasticity.
Table 1 also shows that there are differences between the volunteers of the CP group, in which volunteer CP_1 presents a MMGRMS value greater than the others, for both arms, indicating greater spasticity. On the other hand, volunteers CP_3 and CP_5 have greater spasticity in the left wrist than in the right one. The opposite occurred with volunteers CP_4 and CP_6 since both had greater spasticity in the right wrist. In the para sport classification, these volunteers are classified as B2 or B3, volunteer CP_1 to CP_3 are classified as B3, whereas volunteers CP_4 to CP_6 are classified as B2. For this classification other functional movements are also taken into account. Therefore, a larger study, with more muscles analyzed, is necessary to correlate MMG with this classification.
According with Krueger et al. [9], the amplitude of MMG signals increased significantly in subjects with some degree of spasticity (MAS “2”, for instance) compared to subjects without spasticity (MAS “0”). Santos et al. [10] investigated the correlation between MAS groups and MMG signals in both time and frequency domains and showed correlation between MAS levels and MMG amplitude in the time domain. Wang et al. [11] used MMG and EMG to evaluate the spasticity of the elbow of post-stroke patients in association with a vector support machine (SVM) and showed correlation between MAS and level of spasticity. However, authors mentioned above didn’t investigate wrist flexor and extensor muscles regarding the spasticity, neither in relation to boccia athletes.
Based on this pilot study, it is possible to observe that MMG is sensitive to identify differences between muscle contractions of NI and CP subjects, and some differences between the CP classes for spasticity in each limb. Finally, the use of MMG as an extra resource for clinical evaluation of spasticity is intended to help prevent divergences between evaluators, and contribute to higher safety from rehabilitation to the classification of functionality in sports.
5 Conclusion
There are few studies that related the mechanomyographic signals between Cerebral Palsy and those with no impairment, and no study attempting to use this technology with athletes. Considering the results of this study, it is possible to observe that the MMG signal presented differences between the two groups, during the movement of adhesion, being greater in the CP group, besides differences among CP volunteers. More studies will be necessary to determine the spasticity difference between CP persons and CPs and non-impaired groups, and to use MMG as a means for defining category levels in the Paralympic Games.
References
BISFED – Boccia International Sports Federation. Classification Rules. http://www.bisfed.com/wp-content/uploads/2014/02/Boccia-Classification-Rules-3rd-Edition-2017.pdf. Accessed 11 May 2019
Gordon, L.M., Keller, J.L., Stashinko, E.E., Hoon, A.H., Bastian, A.J.: Can spasticity and dystonia be independently measured in cerebral palsy? Pediatr. Neurol. 35(6), 375–381 (2006)
Pandyan, A.D., Price, C.I., Rodgers, H., Barnes, M.P., Johnson, G.R.: Biomechanical examination of a commonly used measure of spasticity. Clin. Biomech. 16(10), 859–865 (2001)
Lee, H.M., Chen, J.J.J., Ju, M.S., Lin, C.C.K., Poon, P.P.W.: Validation of portable muscle tone measurement device for quantifying velocity-dependent properties in elbow spasticity. J. Electromyogr. Kinesiol. 14(5), 577–589 (2004)
Krueger, E., Scheeren, E.M., Nogueira-Neto, G.N., Button, V.L.S.N., Nohama, P.: Advances and perspectives of mechanomyography. Braz. J. Biomed. Eng. 30(4), 384–401 (2014)
Beck, T.W., Housh, T.J., Cramer, J.T., Weir, J.P., Johnson, G.O., Coburn, J.W., Malek, M.H., Mielke, M.: Mechanomyographic amplitude and frequency responses during dynamic muscle actions: a comprehensive review. BioMed. Eng. OnLine 4(67), 1–23 (2005)
Alves, N., Sejdić, E., Sahota, B., Chau, T.: The effect of accelerometer location on the classification of single-site forearm mechanomyograms. BioMed. Eng. OnLine 9(23), 1–14 (2010)
Nogueira-Neto, G.N.: Viabilidade do emprego de mecanomiografia no controle motor artificial em lesados medulares empregando estimulação elétrica neuromuscular. Tese de Doutorado - Programa de Pós-Graduação em Engenharia Elétrica - Universidade Estadual de Campinas, Campinas/SP, Brazil (2013)
Krueger, E., Scheeren, E.M., Nogueira-Neto, G.N., Button, V.S.N., Nohama, P.: A new approach to assess the spasticity in hamstrings muscles using mechanomyography antagonist muscular group. In: 34th Annual International Conference of the Institute of Electrical and Electronics Engineers Inc. (IEEE): Engineering in Medicine and Biology Society (EMBC), pp. 2060–2063. IEEE, San Diego (2012)
Santos, E.L., Santos, M.C., Krueger, E., Nogueira-Neto, G.N., Nohama, P.: Mechanomyography signals in spastic muscle and the correlation with the modified Ashworth scale. In: 38th Annual International Conference of the Institute of Electrical and Electronics Engineers Inc. (IEEE): Engineering in Medicine and Biology Society (EMBC), pp. 3789–3792. IEEE, Orlando (2016)
Wang, H., Wang, L., Xiang, Y., Zhao, N., Li, X., Chen, S., Lin, C., Li, G.: Assessment of elbow spasticity with surface electromyography and mechanomyography based on support vector machine. In: 39th Annual International Conference of the Institute of Electrical and Electronics Engineers Inc. (IEEE): Engineering in Medicine and Biology Society (EMBC), pp. 3860–3863. IEEE, Seogwipo (2017)
Acknowledgment
The authors would like to thank the National Council for Scientific and Technological Development (CNPq) and Araucária Foundation (FA) for the scholarships and financial resources. This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this paper
Cite this paper
da Luz dos Santos, E. et al. (2020). Mechanomyography Spasticity Assessment of Flexor and Extensor Wrist Muscles for the Classification of Boccia Athletes in Para Sports: A Pilot Study. In: González Díaz, C., et al. VIII Latin American Conference on Biomedical Engineering and XLII National Conference on Biomedical Engineering. CLAIB 2019. IFMBE Proceedings, vol 75. Springer, Cham. https://doi.org/10.1007/978-3-030-30648-9_154
Download citation
DOI: https://doi.org/10.1007/978-3-030-30648-9_154
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-30647-2
Online ISBN: 978-3-030-30648-9
eBook Packages: EngineeringEngineering (R0)