Abstract
The Brazilian experience shows that the intragastric balloon device leads to satisfactory weight loss with a low rate of adverse events. A consensus meeting was held, bringing together 39 Brazilian endoscopists with extensive experience from all regions of the country. Topics on patient selection, indications, contraindications, multidisciplinary follow-up, technique, and adverse events were discussed in the form of questions. Also, data regarding the group’s experience was gathered.
The experts discussed and reached consensus on several points, concerning technical recommendations, indications and contraindications, complications management, among others. The overall Brazilian expert data encompassed 41,186 IGBs, with a mean percentage total body weight (%TBW) loss of 18.4 ± 2.9%. The adverse event rate after the adaptation period was 2.5%, the most common being hyperinflation (0.9%) and spontaneous deflation (0.8%) of the device. The early removal rate due to intolerance was 2.2%.
This chapter demonstrates the main points of consensus among Brazilian experts, reflecting the country’s experience with the intragastric balloon device.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
A consensus meeting was organized in Brazil, gathering expert endoscopists, with the aim of filling the gap of intragastric balloons (IGB) technique and follow-up standardization. The goal of the meeting was to reach a consensus on best practice based on scientific literature and practice of experts [1].
Prior to the meeting, a questionnaire was sent to all participants to compile data of IGB procedures performed by the group. These data comprised a total of 41,866 IGB cases. In addition to providing a source of information for the meeting, they reflect the panel’s extensive experience in this procedure.
Brazilian Experience Data
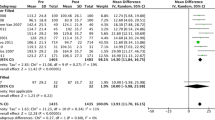
The total number of IGBs in the group’s experience were 41,866 implants and 38,120 explants. Mean patient age was 37.7 years, with 75.9% being female, on average. The mean pre-procedure BMI was 34.4 kg/m2. The minimum reported pre-procedure BMI was 25 kg/m2 and the maximum was 102 kg/m2 (patient with dwarfism) (Table 4.1).
The most used balloon was the non-adjustable, fluid-filled Orbera® (Apollo Endosurgery Inc., Austin, TX, USA), totaling 32,735 implants (78.2%) (Table 4.2). The mean percentage of total body weight (TBW) loss was 18.4 ± 2.9%. The minimum %TBW loss reported was 0.0% and the maximum was 52%. Patients lost a mean of 18.3 ± 4.4 kg, with a minimum reported TBW loss (kg) of 0 kg and maximum of 87.5 kg. The failure rate (defined as %TBW loss <10%) was 8.3 ± 6.7% (Table 4.3).
The most common adverse events were hyperinflation (0.9%) and spontaneous deflation (0.8%). Migrations needing surgical treatment happened in 24 cases, most common with air-filled balloons (1%). Gastric ulcers occurred in 141 cases, more common with the adjustable balloon (5.7%). There were no esophageal or gastric perforations during the implant procedure and a total of six perforations during the explant, mostly with the Silimed® balloon, a device with a more rigid structure and difficult removal (Table 4.4).
Intolerance leading to early removal happened in 2.2% (n = 928). The air-filled device had the lowest early removal rate (0.8%), probably because of its lightweight leading to less symptoms. Fungal infection of the device occurred in 5.8% of the cases, more frequent in the air-filled balloon (14.9%), probably because of its double-layer characteristic.
There were 12 deaths (0.03%) reported during the presence of the balloon, with a variety of causes, with balloon-related deaths in only three cases. The balloon-related causes were gastric rupture due to overfeeding in a superobese patient (n = 1), pulmonary aspiration with uncoercive vomiting 4 days after implant (n = 1), and one case of pulmonary embolism (n = 1), which may not have been caused directly by the balloon.
Consensus Results
Indications and Contraindications
Placement
According to the experts, minimum age for balloon implant is 12 years, after established puberty, with multidisciplinary evaluation and parental consent. There is no maximum age limit for implant, each case should be considered individually. The minimum BMI for balloon implant is 25 kg/m2, after failure of clinical treatment, with no influence of BMI on choice of balloon type.
Absolute Contraindications
Esophageal, gastric, and duodenal ulcers were considered absolute contraindications for balloon implant, owing to the increased risk of perforation. Previous gastric surgery was considered a contraindication by 93.8% of the participants.
Relative Contraindications
Gastric angioectasias without signs of bleeding (75%), eosinophilic esophagitis (81.3%), immunocompetent HIV positive patient (96.9%), and uncontrolled/untreated psychiatric disorders (75.8%).
Pre-procedure Evaluation and Multidisciplinary Follow-Up
Prior Endoscopy and Exams
Regarding pre-procedure evaluation, prior endoscopy was not considered essential (84.4%), since it is possible to evaluate the stomach during the implant procedure. No imaging exams were considered mandatory before the procedure (84.4%), unless there is clinical indication for such, and/or the request of the anesthesiologist. Regarding laboratory exams, no consensus was reached, 41.9% agree that these should always be requested.
Technique
Balloon Implant
It is recommended that the minimum required structure is an outpatient clinic with advanced life support and patient transfer service available if needed (83.9%).
Anesthesia
No consensus was reached regarding sedation: 14.7% prefer conscious sedation; 41.2% prefer deep/general sedation, without orotracheal intubation or the presence of an anesthesiologist; 17.7% prefer a deep/general sedation without orotracheal intubation, performed by anesthesiologist and 26.5% prefer to have an anesthesiologist choose and perform the sedation.
Balloon Volume
No consensus was reached for recommended maximum balloon filling volume. For the adjustable liquid balloon, 54.8% agree that minimum initial filling volume is between 500 and 600 ml; 38.7% believe minimum volume should be between 400 and 500 ml. At the readjustment session, there was no consensus on the additional filling volume: 42.9% recommend a maximum additional volume of 200–300 ml, 25% recommend 100–200 ml, 14.3% recommend 300–400 ml.
For downward adjustments, owing to intolerance (nausea and vomiting), 59.3% believe the minimum filling volume to remain in the adjustable balloon is between 300 and 400 ml, leading to symptom improvement and subsequent upward adjustment.
Balloon Explant
At least 2 days of liquid diet is recommended prior to balloon removal (90.9%), followed by 12-hour fasting (80.7%). Ingestion of cola carbonated drinks (without sugar) is useful as preparation for balloon removal, since this helps to clean any food residues from the stomach (78.1%).
Anesthesia
Regarding explant sedation, once again no consensus was reached.
Technique
A hybrid jaw grasper (alligator + rat tooth) is the preferred accessory for balloon removal (75%). In selected cases, an esophageal overtube may be used to facilitate removal (74.1%); whilst 56.7% also agree that a small amount of vegetable cooking oil can be selectively used to lubricate the esophagus and 30% believe it should always be used [2].
Post-implant Follow-Up
Medications recommended to be administered during the adaptation period to attenuate symptoms are ondansetron, hyoscine, corticosteroid, proton pump inhibitor (PPI), analgesic and dimenhydrinate, usually for up to 3–5 days after implant. The use of PPIs should be maintained throughout treatment (87.5%). Metoclopramide is not recommended in the adaptation period (70.4%) because it increases gastrointestinal motility and may worsen symptoms. Anti-inflammatory drugs are not recommended (96.3%), due to the risk of gastric injury.
Adverse Events
IGB removal is recommended in cases of moderate or severe pancreatitis (90.6%), gastrointestinal bleeding successfully treated only by endoscopic methods (76.5%), gastric ulcer with nonadjustable balloon (90%), recurrent antral impaction (86.7%), symptomatic hyperinflation (96.9%), and recurrent hydro electrolytic disorder (76.7%). In the case of antral impaction, the balloon can be repositioned. In the event of pregnancy, the balloon should be removed (81.3%), preferably in the second trimester.
In the case of adjustable balloon, 53.9% believe the presence of an ulcer demands balloon removal, even if the patient does not agree. In cases where removal is not performed, repositioning the balloon-filling catheter together with clinical treatment is recommended, except in cases of deep ulcers, with increased risks of perforation, in which case the removal is necessary.
In the presence of mild pancreatitis, removal is not mandatory (76.7%). In the cases of gastrointestinal bleeding that is spontaneously stopped, the balloon can also remain in place (84.4%). In the presence of severe erosive esophagitis, 87.1% recommend that the balloon not be removed before appropriate treatment, due to the increased risk of esophageal lesion during removal. The Mallory–Weiss Syndrome cases should also be treated with the balloon in place.
Conclusions
The full version of the Brazilian Intragastric Balloon Consensus has been published as a scientific paper [1]. This consensus and data collection represents the extensive experience of Brazilian experts, a country that pioneered IGB therapy.
References
Neto MG, Silva LB, Grecco E, de Quadros LG, Teixeira A, Souza T, et al. Brazilian Intragastric Balloon Consensus Statement (BIBC): practical guidelines based on experience of over 40,000 cases. Surg Obes Relat Dis. 2018;14(2):151–9.
Neto G, Campos J, Ferraz A, Dib R, Ferreira F, Moon R, et al. An alternative approach to intragastric balloon retrieval. Endoscopy. 2016;48(Suppl 1 UCTN):E73.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Galvao Neto, M., Silva, L.B., Usuy, E.N., Campos, J.M. (2020). Brazilian Experience on the Use of Intragastric Balloons. In: Galvao Neto, M., Silva, L., Usuy Jr., E., Campos, J. (eds) Intragastric Balloon for Weight Management. Springer, Cham. https://doi.org/10.1007/978-3-030-27897-7_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-27897-7_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-27896-0
Online ISBN: 978-3-030-27897-7
eBook Packages: MedicineMedicine (R0)