Abstract
The evaluation and management of thrombocytopenia is a daily challenge for clinicians in the intensive care unit (ICU). Thrombocytopenia is incredibly common, present in upwards of 60% of ICU patients. Additionally, thrombocytopenia in the critically ill is rarely caused by a single etiology. Several causes of thrombocytopenia in the ICU including heparin-induced thrombocytopenia (HIT) and thrombotic thrombocytopenic purpura demand urgent recognition and intervention. This chapter provides a general overview of thrombocytopenia in the ICU and highlights important diagnostic and management considerations for some of the most common etiologies.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
Case Presentation
A 68-year-old male is admitted to the medical ICU with acute hypoxemic respiratory failure from community acquired pneumonia. He was recently hospitalized for acute cholecystitis during which he received prophylactic subcutaneous heparin. He is placed on invasive mechanical ventilation and given ceftriaxone and azithromycin. A lower extremity duplex ultrasound is performed for unilateral leg swelling which demonstrates an acute right femoral deep vein thrombosis. He is subsequently started on an infusion of unfractionated heparin. The following morning, his platelet count is noted to have dropped from 250 × 109 cells/L to 110 × 109 cells/L.
Question
What diagnostic test should be performed?
Answer
An enzyme-linked immune assay (ELISA) for anti-platelet factor 4 (PF4)/heparin antibodies.
This patient has a high pre-test probability for HIT based on his 4Ts score. While HIT typically causes thrombocytopenia 5–10 days after initiation of heparin, patients who have recently received heparin may develop a much more rapid fall in platelet count with heparin re-exposure. If this patient’s HIT ELISA is positive, the diagnosis should be confirmed with a serotonin release assay. Heparin should be switched to a direct thrombin inhibitor or factor Xa inhibitor while the diagnosis of HIT is pursued.
Principles of Management
Platelet Structure and Function
Platelets are small (2–4 μm) oval-shaped anucleated cells derived from bone marrow megakaryocytes. They are short-lived, circulating in the blood for 7–10 days before they are cleared by the liver or spleen [1]. Platelets are versatile cells and important mediators of hemostasis and the immune response [2].
Platelets play a central role in primary hemostasis. In the setting of vascular injury, circulating platelets are exposed to components of the sub-endothelial matrix including collagen and von Willebrand factor (VWF) . These interactions mediate platelet adhesion and subsequent activation. Activated platelets release a number of mediators which promote recruitment of additional platelets to the site of injury, ultimately leading to the formation of a fibrin plug [1].
Platelets also perform a host of immune functions. Toll-like receptors on platelets can directly bind bacteria [2]. Additionally, platelets can activate neutrophils through both cell-cell interactions and the release of inflammatory cytokines. Through activation of antigen presenting cells including dendritic cells and monocytes, platelets can enhance the adaptive immune response [3].
Epidemiology
There is no single platelet threshold that is universally used to define thrombocytopenia. In general, thrombocytopenia is diagnosed when platelet counts fall below 100–150 × 109 cells/L. [4, 5]
Thrombocytopenia in critical illness is common. Depending on the definition used and patient population studied, between 8–67% of patients will have thrombocytopenia on admission to the ICU [6,7,8,9]. Additionally, upwards of 46% of patients will develop thrombocytopenia at some point during their ICU stay [7, 8, 10, 11]. In general, ICU patients who develop thrombocytopenia are sicker than patients with normal platelet counts, with higher illness severity scores, more need for vasoactive infusions, and more organ dysfunction [8, 9].
Implications
The presence of thrombocytopenia in the critically ill has consistently been associated with poor outcomes. In a m ulticenter review of over 3000 critically ill patients, patients with severe thrombocytopenia (defined as a platelet count <50 × 109 cells/L) had an adjusted hazard ratio for hospital mortality of 2.78 (95% CI, 2.20–3.53) compared to patients with normal platelet counts [8]. The association between thrombocytopenia and mortality has been identified in multiple studies [6, 9, 10, 12]. Regardless of the absolute value, a fall in platelet count by >30% from a patient’s admission level identifies patients who may be up to 4 times more likely to die during their hospital stay [11, 13]. Patients whose platelet count fails to recover during their ICU course represent a particularly high risk group [6, 14]. The presence and severity of thrombocytopenia is included in several validated severity scores including the Multiple Organ Dysfunction Score and the Sepsis-related Organ Failure Assessment [15, 16].
Differential Diagnosis and Evaluation
The evaluation of thr ombocytopenia in the ICU is challenging as thrombocytopenia is both a common problem and rarely due to a single etiology. In a study of over 300 ICU patients with either absolute (platelet count <100 × 109 cells/L) or relative (decrease in platelet count >30%) thrombocytopenia who underwent extensive evaluation including bone marrow aspiration, 37% had 3 or more identifiable etiologies for their thrombocytopenia [17]. As such, a structured approach to the evaluation and management of thrombocytopenia is essential.
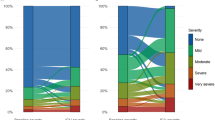
A comprehensive review of the myriad causes of thrombocytopenia is beyond the scope of this review. What follows is a simplified approach to the critically ill patient with new-onset thrombocytopenia (Fig. 83.1).
Simplified approach to the critically ill patient with new-onset thrombocytopenia. Abbreviations: CNS central nervous system, EDTA ethylenediaminetetraacetic acid, IABP intra-aortic balloon pump, ICU intensive care unit, TMA thrombotic microangiopathy, VV-ECMO veno-venous extracorporeal membrane oxygenation
Step 1: Confirm True Thrombocytopenia
Pseudothrombocytopenia
Occasionally, a low reported platelet count d oes not represent true thrombocytope nia. Exposure to ethylenediaminetetraacetic acid (EDTA) in blood collection tubes induces a conformational change in the platelet surface protein glycoprotein IIb/IIIa [18]. Patients may develop IgM autoantibodies to these newly exposed GIIb/IIIa epitopes which causes in vitro platelet clumping. Large platelet aggregates are not recognized by automated counters, leading to a falsely low reported platelet count. The identification of platelet clumps on a peripheral blood smear and re-drawing blood using heparin or citrate containing collection tubes can help confirm the diagnosis.
Step 2: Is the Patient Bleeding?
There is a consensus that patients with clinically significant bleeding should be transfused to a platelet count of >50 × 109 cells/L. [4, 19, 20] The transfusion threshold should be increased to 100 × 109 cells/L in patients with intracranial bleeding [21].
Step 3: Consider a Thrombotic Microangiopathy
Thrombotic microangiopathy (TMA) is a pathologic term used t o describe microvascular thrombosis in the arterioles and capillaries [22]. The key clinical manifestations of TMAs are microangiopathic hemolytic anemia (MAHA) and thrombocytopenia. TMAs are a diverse group of disorders that can be classified broadly as primary (thrombotic thrombocytopenic purpura, hemolytic uremic syndrome, drug-mediated, etc.) or secondary t o a systemic disorder (disseminated intravascular coagulation, severe hypertension, hemolysis with elevated liver enzymes and low platelets during pregnancy, etc.) [23]. While diseases like thrombotic thrombocytopenic purpura (TTP) are uncommon, their prompt recognition is critical as delayed or missed diagnosis can lead to significant patient harm. TTP and disseminated intravascular coagulation (DIC) will be reviewed here as examples of primary and secondary TMAs respectively.
TTP
TTP is characterized by a functiona l deficiency in a VW F clea ving protein termed, “an acronym for a disintegrin and metalloprotease with thrombospondin-1-like-domains” (ADAMTS 13) [24]. With a functional deficiency of ADAMTS 13, large VWF multimers accumulate, triggering platelet adhesion, activation, and the formation of platelet rich microthrombi [25]. TTP is a rare disease with an incidence of 10 cases per million in the United States [26].
Roughly 75% of cases of TTP are acquired, caused by the production of IgG autoantibodies against ADAMTS 13 [25]. Antibody production can be idiopathic (≅50% of cases) or driven by a variety of conditions including malignancy, human immunodeficiency virus infection, pregnancy, autoimmune disease, medications, and following organ transplantation [27].
TTP has historically been associated with a clinical pentad of MAHA, thrombocytopenia, neurologic symptoms, renal impairment, and fever. In the modern era, this constellation of symptoms is rarely seen [27]. While MAHA and thrombocytopenia are universally present, upwards of 90% of patients will be afebrile and 50% will have either normal mental status or renal function [28]. Presenting symptoms are often non-specific and include nausea and abdominal pain [24].
Initial laboratory testing in patients with suspected TTP should confirm the presence of hemolysis (e.g., an elevated lactate dehydrogenase level, low haptoglobin, elevated indirect bilirubin, and elevated reticulocyte index). In contrast to DIC, coagulation parameters are typically normal. A peripheral blood smear should be reviewed to identify fragmented red blood cells called schistocytes – one of the histologic hallmarks of TMA (Fig. 83.2). Renal and cardiac biomarkers should be obtained to screen for organ dysfunction. The role of ADAMTS 13 assays is debated [24, 25]. A severely low level (<5%) confirms the diagnosis of TTP. However, it is imperative that the decision to initiate therapy is made urgently on the basis of an initial clinical and laboratory evaluation without waiting for ADAMTS 13 activity levels to result [29].
TTP was previously viewed as an almost universally fatal diagnosis. However, with the rapid initiation of plasma exchange, survival rates now approach 90% [24, 30]. Plasma exchange should be continued until platelet counts are >150 × 109 cells/L for 2 days [29]. Steroids and rituximab may have a role in the treatment of refractory and recurrent disease [25].
Disseminated Intravascular Coagulation
DIC is defined by the International Society on Thrombosis and Haemostasis (ISTH) as “an acquired syndrome characterized by the intravascular activation of coagulation with a loss of localization arising from different causes. It can originate from and cause damage to the microvasculature , which if sufficiently severe, can produce organ dysfunction.” [31]
The pathobiology of DIC is complex and is driven by dysregulated coagulation and fibrinolysis pathways. A central component of DIC is excessive tissue factor (TF) expression and thrombin generation. Depending on the clinical scenario, this can be caused by the release of inflammatory cytokines including IL-1 and Il-6, increased TF expression on mononuclear cells, injury to vascular endothelial cells, and exposure to pro-coagulant molecules (e.g. amniotic fluid) [32]. Activated platelets contribute to excessive thrombin generation and the formation of microvascular clots. Concurrently, the 3 major anticoagulant systems (antithrombin, the protein C system, and TF pathway inhibitor) are dampened due to impaired synthesis and increased degradation of the relevant factors [32]. Finally, intrinsic fibrinolysis is impaired in part due to elevated levels of plasminogen activator inhibitor 1. The propagation of microvascular thrombi leads to organ ischemia and dysfunction—one of the clinical hallmarks of DIC. [33]
By far, the most common underlying cause of DIC is sepsis. Depending on the patient population and definition used, 25–60% of patients with sepsis develop DIC [32, 34, 35]. In cases series, sepsis is identified as a risk factor for DIC in over 50% of patients [36]. Other important causes of DIC include trauma, obstetric emergencies, malignancies, and liver failure among many others [32]. DIC is consistently identified as a risk factor for increased mortality both in patients with sepsis and in critically ill patients more broadly [34, 36, 37].
The diagnosis of DIC should be suspected in any critically ill patient with thrombocytopenia, abnormal coagulation parameters (e.g., a prolonged prothrombin and partial thromboplastin times), MAHA, and laboratory evidence of fibrinolysis (e.g., an elevated d-dimer and reduced fibrinogen) [38]. While catastrophic hemorrhage is uncommon, most patients have evidence of bleeding, often at sites of intravenous access [33]. Diagnostic criteria developed by the ISTH are available to aid diagnosis (Table 83.1) [37]. In a prospective validation study, a score > 5 had a sensitivity of 91% and specificity of 97% for the diagnosis of DIC [39]. A score should be calculated daily both to accurately confirm the diagnosis and to aid prognostication [40].
The foundation of DIC management is treatment of the underlying disorder. There is limited data to guide the administration of blood products in DIC. In general, guidelines agree that platelets, fresh-frozen plasma, and a source of fibrinogen should be given to patients who are actively bleeding or those undergoing invasive procedures [41]. A platelet count >50 × 109 cells/L, prothrombin (PT) and partial thromboplastin time (aPTT) < 1.5 times normal, and a fibrinogen level > 1.5 g/L are typical targets [19]. Recommendations for the use of heparin vary across guidelines [41]. In general, heparin is reserved for patients with clinical evidence of thrombosis.
A host of targeted interventions aimed at augmenting the major anticoagulant pathways have failed to show benefit in large randomized trials including recombinant TF pathway inhibitors and anti-thrombin III [42, 43]. Early studies of activated protein C (APC) in patients with sepsis showed promise, especially in the subset of patients with DIC [44, 45]. However, the recent PROWESS-SHOCK trial, which included over 1500 patients with septic shock, did not identify any benefit to the use of APC [46].
Step 4: Careful Medication Review
A careful review of a patient’s medication list is an essential step in the evaluation of thrombocytopenia in the ICU. Indeed, medications may contribute to over 10% of new onset thrombocytopenia in the critically ill [17]. Well over 300 drugs have been linked to the development of thrombocytopenia [47]. A list of notable drugs known to cause thrombocytopenia is provided in Table 83.2.
Drug-induced thrombocytopenia can be grouped into two major categories: drug-induced non-immune thrombocytopenia and drug-induced immune thrombocytopenia [48]. Drug-induced non-immune thrombocytopenia is far more common and is characterized by dose-dependent suppression of bone marrow platelet production. Representative medications include linezolid, chemotherapeutics, and immunosuppressive agents like azathioprine [49].
Drug-induced immune thrombocytopenia occurs through a variety of mechanisms. Rarely, medications may induce autoantibodies that destroy host platelets in the absence of the drug. Examples include gold salts and procainamide [50]. More commonly, a drug will induce the production of antibodies that bind to an epitope on a platelet glycoprotein in the presence of the medication. Many antibiotics including aztreonam, piperacillin, sulfonamides, and vancomycin likely act through this mechanism [51]. Heparin-induced thrombocytopenia (HIT) is a particularly important example and is reviewed in detail below. Finally, antiplatelet agents such as eptifibatide used in the treatment of acute coronary syndrome facilitate antibody-mediated destruction of platelets through their binding of glycoprotein IIb/IIIa [4].
Drug-induced immune-mediated thrombocytopenia typically occurs 5–7 days after exposure to the causative medication. T hrombocytopenia is often severe with platelet counts falling to <20 x 109 cells/L. Mucocutaneous bleeding and systemic symptoms may be present [48]. The diagnosis requires a high index of suspicion given the lag between when a drug is started and the subsequent fall in platelet count. Identifying drug-dependent platelet reactive antibodies helps confirm the diagnosis; however, testing is time consuming and available at a limited number of centers. Treatment is focused on the identification and removal of the causative medication. When the offending drug is removed, platelets typically begin to improve in 1–2 days. The role of steroids and intravenous immunoglobulin in the treatment of refractory drug-induced immune thrombocytopenia is controversial [50].
A helpful website, https://ouhsc.edu/platelets/ditp.html, includes a curated list of all drugs associated with drug-dependent platelet-reactive antibodies identified by the BloodCenter of Wisconsin dating back to 1995.
Heparin-Induced Thrombocytopenia
HIT is caused by the production of host IgG antibodies against platelet factor 4 (PF4)-heparin complexes. The Fc domain of these immune complexes binds to the platelet FCγ RIIa receptor causing platelet aggregation, platelet activation, and eventual thrombin formation [52]. Thrombocytopenia is caused by intravascular platelet consumption.
While a diagnosis of HIT is frequently considered for thrombocytopenic patients in the ICU, it is relatively uncommon. For patients in the medical ICU, the incidence may be as low as 0.02% [53]. The biggest risk factors for HIT include the use of unfractionated heparin and cardiac surgery. In these settings, the incidence increases up to 3% [53].
HIT is unique among the common causes of thrombocytopenia in the critically ill in that it is characterized by thrombosis rather than bleeding. Over 50% of patients with HIT develop thrombosis, most commonly in the deep veins of the extremities and pulmonary arteries [53, 54]. HIT can also cause arterial thrombosis, thrombosis in unusual venous structures (e.g. mesenteric vessels), and myocardial infarction [54].
HIT should be suspected when platelet counts fall by at least 50% 5–10 days after the initiation of heparin therapy [55]. An important caveat to this pattern is patients who have been previously exposed to heparin. Host IgG against PF4-heparin complexes can remain active for up to 85 days. During this window, heparin re-exposure can produce a rapid drop in platelet count within 24 hours [52]. Up to 30% of cases of HIT may present in this manner [55]. Thrombocytopenia in HIT is generally less severe than other causes of thrombocytopenia in the ICU with levels rarely falling below 20 × 109 cells/L. [54]
Up to 20% of patients exposed to heparin produce IgG antibodies against PF4-heparin complexes while only a small minority develop HIT [56]. Given the costs associated with laboratory testing for HIT and the potential risk of transitioning to a non-heparin anticoagulant agent, the diagnosis of HIT should only be pursued in patients with an intermediate to high pre-test probability of having the disease [57]. The most widely used pre-test probability assessment tool for HIT is the 4Ts score (Table 83.3) [58]. A score < 4 is ass ociated with a negative predictive value for HIT of >99% and obviates the need for further testing [59]. Patients with a score ≥ 4 should undergo step-wise serologic testing.
The initial serologic test for patients with an intermediate to high pre-test probability of HIT is an enzyme-linked immunoassay (ELISA) to detect HIT antibodies. These assa ys are widely available and result in a matter of hours. IgG-specific ELISAs have a sensitivity of 96% and specificity of 89% for the diagnosis of HIT [60]. Results are typically reported quantitatively as an optical density (OD). The higher the OD threshold used to identify a positive test, the more likely a positive ELISA will predict a positive functional assay. The commonly used OD cutoff of 0.4 has a sensitivity of >99% for HIT [53].
Patients with a positive ELISA should undergo confirmatory testing with a functional assay – typically a serotonin release assay (SRA). A SRA evaluates for in vitro activation of platelets in the presence of patient serum and heparin. A positive SRA has a specificity of nearly 100% for the diagnosis of HIT [60].
The cornerstone of management for patients with either an intermediate to high pre-test probability of HIT or a confirmed diagnosis is transition to a non-heparin anticoagulant. Options include direct thrombin inhibitors (e.g., lepirudin, argatroban, and bivalrudin) and factor Xa inhibitors (e.g., danaparoid and fondaparinux) [54]. There is currently insufficient evidence to support the use of direct oral anticoagulant agents in this setting [53]. Warfarin is contraindicated in patients with HIT until the platelet counts rises above 150 x 109 cells/L as warfarin reduces protein C levels and may exacerbate thrombus formation [54]. Platelet transfusions should be avoided if possible and are only recommended for patients who are actively bleeding or those undergoing an invasive procedure associated with a high risk of bleeding [54].
Step 5: Evaluation for Sepsis
Sepsis is one of the most comm on causes of thrombocytopenia in the ICU and may contribute to a low platelet count in up to 75% of casas [17]. The incidence of thrombocytopenia in patients with sepsis varies by illness severity. In a multicenter prospective evaluation of 1238 patients with severe sepsis, thrombocytopenia was present in 14.5% of patients [61]. In patients with septic shock, the incidence of thrombocytopenia approaches 50% [62, 63]. Thrombocytopenia has consistently been associated with increased mortality in septic patients [10, 61, 62].
Multiple mechanisms cause thrombocytopenia during sepsis. Decreased bone marrow production, hemophagocytosis, platelet consumption in microvascular beds, sequestration, and hemodilution may all contribute to varying degrees [64]. Septic patients are at high risk for DIC which can further lower platelet counts. Additionally, many medications routinely administered to septic patients including antibiotics are associated with thrombocytopenia.
Based on very low-quality evidence, the Surviving Sepsis Campaign recommends prophylactic platelet transfusions in septic patients with a platelet count <10 × 109 cells/L and 20 × 109 cells/L for patients at high risk of bleeding. A platelet count >50 × 109 cells/L is recommended for patients who are actively bleeding or undergoing invasive procedures [65].
Step 6: Consider Hemodilution
Dilutional thrombocyt openia is a well-recognized complication of massive transfusion. The incidence of severe thrombocytopenia (defined as a platelet count <50 × 109 cells/L) may be as high as 75% when patients require more than 20 red blood cell containing products [66]. Prompt damage control and transfusion of blood products in a balanced ratio (1:1:1 of red blood cells:plasma:platelets) are important preventative strategies [67].
Step 7: Evaluate Support Devices
Support devices used in critically ill patients may lower platelet counts through mechanical shearing. Veno-venous extracorporeal membrane oxygenation (VV-ECMO) is increasingly utilized in the management of severe acute respiratory distress syndrome (ARDS). In a retrospective study of 100 patients placed on VV-ECMO for respiratory failure, 22% developed thrombocytopenia [68]. Severity of illness and the platelet count at the time of cannulation were the strongest predictors of developing thrombocytopenia. In a large randomized trial of ECMO for severe ARDS, 27% of patients randomized to ECMO developed severe thrombocytopenia (defined as a platelet count <20 × 109 cells/L) vs 16% in the control arm [69].
For patients placed on an intra-aortic balloon pump, roughly 50% will develop thrombocytopenia [70, 71].
Evidence Contour
Indications for Prophylactic Platelet Transfusion
Despite the high incidenc e of thrombocytopenia in critically ill patients, there is a paucity of data to guide when prophylactic platelet transfusion is indicated. Indeed, a recent systematic review did not identify a single high-quality study that investigated the impact of prophylactic platelet transfusions on bleeding rates in critically ill patients [72].
Recommendations on prophylactic platelet transfusions in critically ill patients are largely extrapolated from studies in patients with hematologic malignancies. In a landmark trial of platelet transfusion thresholds in 255 patients with acute myeloid leukemia undergoing induction chemotherapy, a transfusion threshold of 10 × 109 cells/L did not increase the risk of major bleeding and reduced the need for platelet transfusions by 21.5% compared to a threshold of 20 × 109 cells/L. [73] A recent Cochrane review supports the conclusion that a restrictive platelet transfusion threshold is safe in patients with hematologic malignancies [74]. Guidelines by the American Society of Clinical Oncology recommend a prophylactic platelet transfusion threshold of 10 × 109 cells/L in patients with malignancy [75]. It is unclear, however, if data from patients with malignancies can be reliably generalized to the heterogeneous group of patients cared for in the ICU [76]. Some have advocated for an approach which reserves platelet transfusions for critically ill patients with clinical evidence of bleeding (regardless of the actual platelet count) [48]. However, there is insufficient data to support the safety or efficacy of this practice.
Platelet Thresholds for Invasive Procedures
There is equally limited evidence to guide the platelet count needed to limit bleeding complications during bedsi de procedures commonly performed in the ICU. The American Association of Blood Banks recommends a platelet threshold of 20 × 109 cells/L for patients undergoing central line insertion and 50 × 109 cells/L for patients undergoing lumbar puncture although both are weak recommendations supported by low-quality evidence [77]. A recent Cochrane review of platelet thresholds for patients undergoing central line insertion was unable to draw any conclusions given the complete lack of data on the subject [78]. There is mounting evidence that thoracentesis can be safely performed by an experienced operator in thrombocytopenic patients without prophylactic platelet transfusions [79].
References
van der Meijden PEJ, Heemskerk JWM. Platelet biology and functions: new concepts and clinical perspectives. Nat Rev Cardiol. 2019;16(3):166–79.
Katz JN, Kolappa KP, Becker RC. Beyond thrombosis: the versatile platelet in critical illness. Chest. 2011;139(3):658–68.
Semple JW, Italiano JE Jr, Freedman J. Platelets and the immune continuum. Nat Rev Immunol. 2011;11(4):264–74.
Rice TW, Wheeler AP. Coagulopathy in critically ill patients: part 1: platelet disorders. Chest. 2009;136(6):1622–30.
Drews RE, Weinberger SE. Thrombocytopenic disorders in critically ill patients. Am J Respir Crit Care Med. 2000;162(2 Pt 1):347–51.
Akca S, Haji-Michael P, de Mendonca A, Suter P, Levi M, Vincent JL. Time course of platelet counts in critically ill patients. Crit Care Med. 2002;30(4):753–6.
Crowther MA, Cook DJ, Meade MO, et al. Thrombocytopenia in medical-surgical critically ill patients: prevalence, incidence, and risk factors. J Crit Care. 2005;20(4):348–53.
Williamson DR, Albert M, Heels-Ansdell D, et al. Thrombocytopenia in critically ill patients receiving thromboprophylaxis: frequency, risk factors, and outcomes. Chest. 2013;144(4):1207–15.
Hui P, Cook DJ, Lim W, Fraser GA, Arnold DM. The frequency and clinical significance of thrombocytopenia complicating critical illness: a systematic review. Chest. 2011;139(2):271–8.
Baughman RP, Lower EE, Flessa HC, Tollerud DJ. Thrombocytopenia in the intensive care unit. Chest. 1993;104(4):1243–7.
Strauss R, Wehler M, Mehler K, Kreutzer D, Koebnick C, Hahn EG. Thrombocytopenia in patients in the medical intensive care unit: bleeding prevalence, transfusion requirements, and outcome. Crit Care Med. 2002;30(8):1765–71.
Vanderschueren S, De Weerdt A, Malbrain M, et al. Thrombocytopenia and prognosis in intensive care. Crit Care Med. 2000;28(6):1871–6.
Moreau D, Timsit JF, Vesin A, et al. Platelet count decline: an early prognostic marker in critically ill patients with prolonged ICU stays. Chest. 2007;131(6):1735–41.
Nijsten MW, ten Duis HJ, Zijlstra JG, et al. Blunted rise in platelet count in critically ill patients is associated with worse outcome. Crit Care Med. 2000;28(12):3843–6.
Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related organ failure assessment) score to describe organ dysfunction/failure. On behalf of the working group on Sepsis-related problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–10.
Marshall JC, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ. Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med. 1995;23(10):1638–52.
Thiolliere F, Serre-Sapin AF, Reignier J, et al. Epidemiology and outcome of thrombocytopenic patients in the intensive care unit: results of a prospective multicenter study. Intensive Care Med. 2013;39(8):1460–8.
Tan GC, Stalling M, Dennis G, Nunez M, Kahwash SB. Pseudothrombocytopenia due to platelet clumping: a case report and brief review of the literature. Case Rep Hematol. 2016;2016:3036476.
Hunt BJ. Bleeding and coagulopathies in critical care. N Engl J Med. 2014;370(9):847–59.
Estcourt LJ, Birchall J, Allard S, et al. Guidelines for the use of platelet transfusions. Br J Haematol. 2017;176(3):365–94.
Slichter SJ. Evidence-based platelet transfusion guidelines. Hematology Am Soc Hematol Educ Program. 2007:172–8.
Scully M, Cataland S, Coppo P, et al. Consensus on the standardization of terminology in thrombotic thrombocytopenic purpura and related thrombotic microangiopathies. J Thromb Haemost. 2017;15(2):312–22.
George JN, Nester CM. Syndromes of thrombotic microangiopathy. N Engl J Med. 2014;371(7):654–66.
George JN. Clinical practice. Thrombotic thrombocytopenic purpura. N Engl J Med. 2006;354(18):1927–35.
Joly BS, Coppo P, Veyradier A. Thrombotic thrombocytopenic purpura. Blood. 2017;129(21):2836–46.
Terrell DR, Williams LA, Vesely SK, Lammle B, Hovinga JA, George JN. The incidence of thrombotic thrombocytopenic purpura-hemolytic uremic syndrome: all patients, idiopathic patients, and patients with severe ADAMTS-13 deficiency. J Thromb Haemost. 2005;3(7):1432–6.
Mariotte E, Azoulay E, Galicier L, et al. Epidemiology and pathophysiology of adulthood-onset thrombotic microangiopathy with severe ADAMTS13 deficiency (thrombotic thrombocytopenic purpura): a cross-sectional analysis of the French national registry for thrombotic microangiopathy. Lancet Haematol. 2016;3(5):e237–45.
Page EE, Kremer Hovinga JA, Terrell DR, Vesely SK, George JN. Thrombotic thrombocytopenic purpura: diagnostic criteria, clinical features, and long-term outcomes from 1995 through 2015. Blood Adv. 2017;1(10):590–600.
Scully M, Hunt BJ, Benjamin S, et al. Guidelines on the diagnosis and management of thrombotic thrombocytopenic purpura and other thrombotic microangiopathies. Br J Haematol. 2012;158(3):323–35.
Rock GA, Shumak KH, Buskard NA, et al. Comparison of plasma exchange with plasma infusion in the treatment of thrombotic thrombocytopenic purpura. Canadian Apheresis Study Group. N Engl J Med. 1991;325(6):393–7.
Taylor FB Jr, Toh CH, Hoots WK, et al. Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost. 2001;86(5):1327–30.
Gando S, Levi M, Toh CH. Disseminated intravascular coagulation. Nat Rev Dis Primers. 2016;2:16037.
Levi M. Disseminated intravascular coagulation. Crit Care Med. 2007;35(9):2191–5.
Saito S, Uchino S, Hayakawa M, et al. Epidemiology of disseminated intravascular coagulation in sepsis and validation of scoring systems. J Crit Care. 2019;50:23–30.
Zeerleder S, Hack CE, Wuillemin WA. Disseminated intravascular coagulation in sepsis. Chest. 2005;128(4):2864–75.
Singh B, Hanson AC, Alhurani R, et al. Trends in the incidence and outcomes of disseminated intravascular coagulation in critically ill patients (2004–2010): a population-based study. Chest. 2013;143(5):1235–42.
Toh CH, Hoots WK, SSCoDICot ISTH. The scoring system of the scientific and standardisation committee on disseminated intravascular coagulation of the International Society on Thrombosis and Haemostasis: a 5-year overview. J Thromb Haemost. 2007;5(3):604–6.
Vincent JL, Castro P, Hunt BJ, et al. Thrombocytopenia in the ICU: disseminated intravascular coagulation and thrombotic microangiopathies-what intensivists need to know. Crit Care. 2018;22(1):158.
Bakhtiari K, Meijers JC, de Jonge E, Levi M. Prospective validation of the International Society of Thrombosis and Haemostasis scoring system for disseminated intravascular coagulation. Crit Care Med. 2004;32(12):2416–21.
Gando S, Meziani F, Levi M. What's new in the diagnostic criteria of disseminated intravascular coagulation? Intensive Care Med. 2016;42(6):1062–4.
Wada H, Matsumoto T, Yamashita Y. Diagnosis and treatment of disseminated intravascular coagulation (DIC) according to four DIC guidelines. J Intensive Care. 2014;2(1):15.
Abraham E, Reinhart K, Opal S, et al. Efficacy and safety of tifacogin (recombinant tissue factor pathway inhibitor) in severe sepsis: a randomized controlled trial. JAMA. 2003;290(2):238–47.
Warren BL, Eid A, Singer P, et al. Caring for the critically ill patient. High-dose antithrombin III in severe sepsis: a randomized controlled trial. JAMA. 2001;286(15):1869–78.
Bernard GR, Vincent JL, Laterre PF, et al. Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med. 2001;344(10):699–709.
Dhainaut JF, Yan SB, Joyce DE, et al. Treatment effects of drotrecogin alfa (activated) in patients with severe sepsis with or without overt disseminated intravascular coagulation. J Thromb Haemost. 2004;2(11):1924–33.
Ranieri VM, Thompson BT, Barie PS, et al. Drotrecogin alfa (activated) in adults with septic shock. N Engl J Med. 2012;366(22):2055–64.
Reese JA, Li X, Hauben M, et al. Identifying drugs that cause acute thrombocytopenia: an analysis using 3 distinct methods. Blood. 2010;116(12):2127–33.
Greinacher A, Selleng S. How I evaluate and treat thrombocytopenia in the intensive care unit patient. Blood. 2016;128(26):3032–42.
Priziola JL, Smythe MA, Dager WE. Drug-induced thrombocytopenia in critically ill patients. Crit Care Med. 2010;38(6 Suppl):S145–54.
Aster RH, Bougie DW. Drug-induced immune thrombocytopenia. N Engl J Med. 2007;357(6):580–7.
Mitta A, Curtis BR, Reese JA, George JN. Drug-induced thrombocytopenia: 2019 update of clinical and laboratory data. Am J Hematol. 2019;94(3):E76–8.
Greinacher A. CLINICAL PRACTICE. Heparin-Induced Thrombocytopenia. N Engl J Med. 2015;373(3):252–61.
East JM, Cserti-Gazdewich CM, Granton JT. Heparin-induced thrombocytopenia in the critically ill patient. Chest. 2018;154(3):678–90.
Linkins LA, Dans AL, Moores LK, et al. Treatment and prevention of heparin-induced thrombocytopenia: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e495S–530S.
Warkentin TE, Kelton JG. Temporal aspects of heparin-induced thrombocytopenia. N Engl J Med. 2001;344(17):1286–92.
Warkentin TE, Sheppard JA, Horsewood P, Simpson PJ, Moore JC, Kelton JG. Impact of the patient population on the risk for heparin-induced thrombocytopenia. Blood. 2000;96(5):1703–8.
Tardy-Poncet B, Nguyen P, Thiranos JC, et al. Argatroban in the management of heparin-induced thrombocytopenia: a multicenter clinical trial. Crit Care. 2015;19:396.
Lo GK, Juhl D, Warkentin TE, Sigouin CS, Eichler P, Greinacher A. Evaluation of pretest clinical score (4 T's) for the diagnosis of heparin-induced thrombocytopenia in two clinical settings. J Thromb Haemost. 2006;4(4):759–65.
Cuker A, Gimotty PA, Crowther MA, Warkentin TE. Predictive value of the 4Ts scoring system for heparin-induced thrombocytopenia: a systematic review and meta-analysis. Blood. 2012;120(20):4160–7.
Shen YM, Wolfe H, Barman S. Evaluating thrombocytopenia during heparin therapy. JAMA. 2018;319(5):497–8.
Martin CM, Priestap F, Fisher H, et al. A prospective, observational registry of patients with severe sepsis: the Canadian Sepsis Treatment and Response Registry. Crit Care Med. 2009;37(1):81–8.
Claushuis TA, van Vught LA, Scicluna BP, et al. Thrombocytopenia is associated with a dysregulated host response in critically ill sepsis patients. Blood. 2016;127(24):3062–72.
Thiery-Antier N, Binquet C, Vinault S, et al. Is thrombocytopenia an early prognostic marker in septic shock? Crit Care Med. 2016;44(4):764–72.
Larkin CM, Santos-Martinez MJ, Ryan T, Radomski MW. Sepsis-associated thrombocytopenia. Thromb Res. 2016;141:11–6.
Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis campaign: international guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43(3):304–77.
Sihler KC, Napolitano LM. Complications of massive transfusion. Chest. 2010;137(1):209–20.
Bogert JN, Harvin JA, Cotton BA. Damage control resuscitation. J Intensive Care Med. 2016;31(3):177–86.
Abrams D, Baldwin MR, Champion M, et al. Thrombocytopenia and extracorporeal membrane oxygenation in adults with acute respiratory failure: a cohort study. Intensive Care Med. 2016;42(5):844–52.
Combes A, Hajage D, Capellier G, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;378(21):1965–75.
Bream-Rouwenhorst HR, Hobbs RA, Horwitz PA. Thrombocytopenia in patients treated with heparin, combination antiplatelet therapy, and intra-aortic balloon pump counterpulsation. J Interv Cardiol. 2008;21(4):350–6.
Roy SK, Howard EW, Panza JA, Cooper HA. Clinical implications of thrombocytopenia among patients undergoing intra-aortic balloon pump counterpulsation in the coronary care unit. Clin Cardiol. 2010;33(1):30–5.
Lieberman L, Bercovitz RS, Sholapur NS, Heddle NM, Stanworth SJ, Arnold DM. Platelet transfusions for critically ill patients with thrombocytopenia. Blood. 2014;123(8):1146–51. quiz 1280
Rebulla P, Finazzi G, Marangoni F, et al. The threshold for prophylactic platelet transfusions in adults with acute myeloid leukemia. Gruppo Italiano Malattie Ematologiche Maligne dell'Adulto. N Engl J Med. 1997;337(26):1870–5.
Estcourt LJ, Stanworth SJ, Doree C, Hopewell S, Trivella M, Murphy MF. Comparison of different platelet count thresholds to guide administration of prophylactic platelet transfusion for preventing bleeding in people with haematological disorders after myelosuppressive chemotherapy or stem cell transplantation. Cochrane Database Syst Rev. 2015;11:CD010983.
Schiffer CA, Bohlke K, Delaney M, et al. Platelet transfusion for patients with Cancer: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol. 2018;36(3):283–99.
Gajic O, Dzik WH, Toy P. Fresh frozen plasma and platelet transfusion for nonbleeding patients in the intensive care unit: benefit or harm? Crit Care Med. 2006;34(5 Suppl):S170–3.
Kaufman RM, Djulbegovic B, Gernsheimer T, et al. Platelet transfusion: a clinical practice guideline from the AABB. Ann Intern Med. 2015;162(3):205–13.
Estcourt LJ, Desborough M, Hopewell S, Doree C, Stanworth SJ. Comparison of different platelet transfusion thresholds prior to insertion of central lines in patients with thrombocytopenia. Cochrane Database Syst Rev. 2015;12:CD011771.
Cantey EP, Walter JM, Corbridge T, Barsuk JH. Complications of thoracentesis: incidence, risk factors, and strategies for prevention. Curr Opin Pulm Med. 2016;22(4):378–85.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Walter, J.M. (2020). Thrombocytopenia in the Intensive Care Unit. In: Hyzy, R.C., McSparron, J. (eds) Evidence-Based Critical Care. Springer, Cham. https://doi.org/10.1007/978-3-030-26710-0_83
Download citation
DOI: https://doi.org/10.1007/978-3-030-26710-0_83
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-26709-4
Online ISBN: 978-3-030-26710-0
eBook Packages: MedicineMedicine (R0)