Abstract
Aging is a natural process defined by the gradual, time-dependent decline of biological and behavioural functions, for which individuals of the same chronological age show variability. The capacity of biological systems to continuously adjust for optimal functioning despite ever changing environments is essential for healthy aging, and variability in these adaptive homeostatic mechanisms may reflect such heterogeneity in the aging process. With an ever-increasing aging population, interest in biomarkers of aging is growing. Although no universally accepted definition of biomarkers of healthy aging exists, mediators of homeostasis are consistently used as measures of the aging process. As important sex differences are known to underlie many of these systems, it is imperative to consider that this may reflect, to some extent, the sex differences observed in aging and age-related disease states. This chapter aims to outline sex differences in key homeostatic domains thought to be associated with the pathophysiology of aging, often proposed as biomarkers of aging and age-related disease states. This includes considering sex-based differences and hormonal status with regards to the gonadal and adrenal endocrine systems and immune function.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
1 Introduction
Aging is a natural process defined by the gradual, time-dependent decline of physiological and behavioural function, and individuals of the same chronological age can show great variability in these parameters [1]. The capacity of biological systems to continuously adjust for optimal functioning despite ever changing environments is essential for healthy aging, and variability in these adaptive homeostatic mechanisms may reflect the heterogeneity observed [2].
Adaptive homeostasis refers to “The transient expansion or contraction of the homeostatic range in response to exposure to sub-toxic, non-damaging, signalling molecules or events, or the removal or cessation of such molecules or events” [3], and represents the framework in which the body dynamically maintains biological and behavioural processes required for life. The endocrine, metabolic and immune systems are well established in the literature as homeostatic mechanisms [3]. These systems are complex and integrated, involving feedback-dependent mechanisms and cross-talk across networks, thereby contributing to overall system regulation [4]. These integrated systems are ultimately governed by the complex interaction between genetic and environmental factors, including lifestyle factors, which may affect homeostatic mechanisms and ultimately change the progression of aging. Growing evidence suggests that the adaptability of these homeostatic systems decline with age, with many linked to age-related morbidities suggesting a shared pathophysiology of disrupted cellular homeostasis [2]. This change or decline in key homeostatic systems may therefore reflect the inability to activate or modulate several adaptive responses.
With an ever-increasing aging population, interest in biomarkers of healthy or accelerated aging is growing. Although there is no universally accepted definition of ‘aging’ biomarkers, attempts to identify objective biomarkers often point to mediators of homeostatic systems including physiological functions, cognitive processes, and endocrine and immune functions [5]. Importantly, sex differences are often reported in many of these adaptive systems, and this may reflect, to some extent, sex differences observed in aging and age-related disease states. Therefore, it is imperative to consider sex and gender differences in aging and age-related diseases.
Known sex differences in key homeostatic mediators may influence the differential susceptibility and resilience to aging outcomes between males and females. Therefore, within the context of biomarkers in aging, it is important to consider biological sex differences and the role of gender, which includes a person’s psychosocial and cultural self-identification [6], and how these may influence analytical measurement. From a physiological standpoint, biological sex may play an important factor in the variability of biomarkers due to the capacity of sex chromosomes and sex hormones (i.e., estrogen, testosterone), to alter biomarkers present in blood, saliva, cerebral spinal fluid, or tissue samples [4]. From a behavioural standpoint, biological sex hormones, sex chromosomes, and gender may impart differential adaptive processes seen in the cognitive domain [7].
This chapter aims to outline sex differences in key homeostatic domains thought to be associated with the pathophysiology of aging, and which are often proposed as biomarkers of aging and age-related disease states. This includes summarising the available literature of sex-based differences and hormonal status with regards to the gonadal and adrenal endocrine systems and immune function.
2 Sex Differences in Age-Related Diseases
Sex differences in longevity , mortality and age-related diseases are well established in the literature. In developed nations, females tend to live longer than males and have notably lower death rates than men at all ages. However, it is also known that females suffer from higher levels of morbidity than men [8]. Salient gender-related differences have been associated with risk, clinical expression, treatment response and course of several age-related neurodegenerative disorders, such as Alzheimer’s disease and Parkinson’s disease [9].
Alzheimer’s disease , the most common cause of dementia, disproportionately affects females, with a higher incidence compared to males [10]. Females have a faster rate of cognitive and functional decline following diagnosis and appear to suffer significantly greater cognitive impairments after accounting for sex differences in age, education and dementia severity [11]. Sexual dimorphisms in Alzheimer’s disease pathologies have been reported in several mouse models, with females expressing greater pathology [12]. Sex has also been demonstrated to modify genetic risk factors for Alzheimer’s disease. For example, the apolipoprotein E gene ε4 allele confers a greater Alzheimer’s disease risk in females, as compared to males [13]. In contrast, males have at least a two-fold greater risk and prevalence of Parkinson’s disease [14]. In comparison to females, males have a later onset of Parkinson’s disease. Clinical and cognitive profiles also differ between males and females with Parkinson’s disease. Males are more likely to present with rigidity, rapid eye movement behaviour disorder and sleep disturbances. The cognitive profile in males is more likely to include verbal fluency deficits and a lack of facial emotions. Females are more likely to present with a tremor dominant form of Parkinson’s disease. A reduction in visuospatial cognition is more frequent in females [9, 15, 16]. Possible reasons for these sex differences in age-related, neurodegenerative disorders and longevity are thought to be due to intrinsic differences based on genes, sex hormones, and reproductive physiology. These can confer differential risks of morbidity. In addition, extrinsic factors such as lifestyle, health habits, exercise, nutrition, and others may also have a connection with sex difference in biological vigor as potential moderators.
3 Endocrine Markers of Aging
The endocrine system represents a key facilitator of homeostatic function, maintaining critical functions including development, growth, metabolism, stress responses, reproduction, and sleep patterns. As such, it is one of the most important regulators of physiology over the lifespan. The hypothalamus can be considered as the link between the nervous system and endocrine system, continually adjusting according to internal and external environments using feedback mechanisms, and subsequently regulating all hormone-related physiology and behaviour. With advancing age, alterations in hormonal networks, with concomitant excesses or deficits in steroidal hormones occur [17]. This is further exacerbated by poor sensitivity of tissues to their action, and a decreased sensitivity toward feedback control [18]. These alterations are thought to be translated clinically to losses of function seen in aging of the reproduction system including menopause, developmental and maintenance growth axes, and the adrenal endocrine axis [18].
4 Aging of the Female and Male Reproductive System and the Aging Gonadotropic Axis
Sex steroid hormones, including estrogens and androgens (testosterones) are regulated by the hypothalamus pituitary gonadal (HPG) axis. While the endocrine feedback mechanisms are complex, a simplified account of the HPG axis suggests that the hypothalamus releases gonadotropin-releasing hormone (GnRH), stimulating the anterior pituitary to produce and secrete gonadotropins, luteinizing hormone (LH) and follicle-stimulating hormone (FSH). The ovary, comprised of two cellular components, is synergistically stimulated by FSH and LH, leading to the release of sex steroids [19]. FSH and LH then complete the endocrine feedback loop by posing both positive and negative feedback effects on the axes, depending on timing and context [20].
A clear change observed throughout aging is the decline in sex hormone production. As women age, the natural transition from reproductive years to menopause is associated with fluctuating and eventual decreasing levels of ovarian sex steroids. Suggested to be a predictor of reduced ovarian reserve, gonadotropin FSH increases pre-menopausally [21]. Subsequent to the menopausal transition, eventual decreases in FSH and LH occur [18]. Again, alteration at the level of the hypothalamus-pituitary-gonadal axis is thought to principally contribute to this progressive decline. This appears to be moderated by increased levels of GnRH which increase with age with hypothalamic adaptations during aging, favouring its release [22, 23]. Moreover, the feedback effect of estrogen on FSH responsiveness is greater than on LH and is attenuated with aging [24].
This natural consequence of aging of the reproductive axis and sex-steroid privation leads to the loss of reproductive capability, in addition to a sequelae of clinical symptomatologies including loss of muscle and bone mass, visceral tissue accumulation, insulin resistance, and negative impacts on mood, cognition, and importantly, quality of life [25]. A recent meta-analysis of 310,329 women demonstrated that younger age at menopause (occurring prior to 45 years old) was associated with a higher risk of coronary heart disease, stroke, cardiovascular mortality, and of all-cause mortality [26]. In addition, the occurrence of age-related morbidities including Alzheimer’s disease and Parkinson’s disease has led to the suggestion that the loss of sex steroid hormones, in both female and males, is a contributor to the aetiology [27, 28].
Although not as dramatic as seen during the female menopausal transition, a modest, progressive decline in anabolic androgen is observed in males throughout the aging process [29]. No specific age can be defined as to when this process begins, although several cross-sectional and longitudinal studies have confirmed that testosterone (free and bound) decline in aging, while LH increases with age [30,31,32,33,34]. Recently, weight and lifestyle factors have been shown to moderate these hormonal changes [30]. In addition, the levels of sex hormone binding globulin (SHBG) increase during aging which binds testosterone, resulting in relatively less free biologically-available testosterone [35]. Clinically, low testosterone levels have been associated with increased mortality in men, showing an approximate doubling in mortality risk compared to men with normal levels [36]. Associations between low testosterone and adverse outcomes have also been reported, including diabetes mellitus, osteoporosis, decreased libido, and cardiovascular disease [37,38,39]. In a recent biomarker analysis that included sex hormones in an aging ‘panel’, it was reported that low levels of testosterone are correlated with high-sensitivity cardiovascular risk factors, consistent with a potential increased risk of cardiovascular disease [40].
Fluctuating hormone levels throughout the menstrual cycle of reproductive aged women and in perimenopausal women should be also be considered, as female hormonal status has been shown to modulate many age-related biomarkers. As an example, stress-induced cortisol levels are associated with impaired emotional retrieval [41] and affect serum biomarkers in clinical tests only in some menstrual phases [42]. In addition, hormonal contraceptives used by many women of reproductive age have shown to vary clinical measurement of serum biomarkers [42], and this is rarely considered within the context of system dynamics and levels of molecular outputs. Although the contributions and mechanisms are yet to be fully elucidated, sex steroid hormones exhibit clear functional activity on age-related processes and may govern, in large part, the sexual dimorphisms observed in many age-related morbidities.
5 Dehydroepiandrosterone in Aging
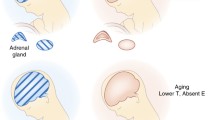
Adrenal secretion of dehydroepiandrosterone (DHEA) also profoundly fluctuates across the lifespan and represents one of the largest endocrine changes observed in human aging. Although the physiological role of DHEA is not yet completely understood, its apparent influence in age and age-related disease states has yielded much interest.
DHEA is predominately synthesised within the adrenal zona reticularis of the adrenal cortex in response to adrenocorticotropic hormone (ACTH) and subsequently released into the bloodstream [43]. The majority of circulating DHEA is converted to its sulphated derivative DHEA-S via the enzyme steroid sulphotransferase, which is mostly bound to the carrier protein, albumin. As the precursor to the sex steroid hormones, it is also synthesised to a smaller extent in human gonads [44]. DHEA-S serves as a precursor to approximately 50% of androgens in adult men, 75% of active estrogens in premenopausal and nearly 100% in postmenopausal women [45]. More recently, reports pertaining to its de novo synthesis in human brain highlights the important neurosteroidal properties that DHEA may have, posited to have direct activity at estradiol receptors [46] and NMDA receptors [47], possess neuroprotective properties, and participate in neurogenesis, catecholamine synthesis and secretion, in addition to anti-inflammatory effects [44]. Indeed, it has been reported that concentrations of DHEA/DHEA-S are considerably higher in the brain than in any other organ.
At birth, DHEA-S levels are markedly high until involution of the adrenal fetal zone, which leads to a cessation in DHEA production and it remains dormant until the childhood period, when production once again commences. Peak levels for both females and males are observed when they are in their thirties, after which point DHEA levels fall by approximately 2–3% each year [48], declining to levels that are approximately 20% of peak values in men and 30% of those in women [43, 49].
Several studies have reported the association between low levels of DHEA-S and DHEA and frailty in older populations [50,51,52]. In addition, several cross-sectional studies, including investigations of serum and cerebrospinal fluid (CSF), have implicated DHEA levels in a number of age-related pathologies including type 2 diabetes mellitus, psychiatric disease states, and neurocognitive disorders, including Alzheimer’s disease [29, 43]. Although many studies have provided support for a positive correlation between higher levels of DHEA and improved health outcomes, including muscle strength, higher bone density and increased longevity in males, other studies have demonstrated that DHEA is associated with negative health outcomes. For example, lower DHEA-S levels have been associated with greater risk of ischemic stroke, having been adjusted for appropriate potential confounders [53].
Due to such accumulating literature, DHEA has drawn much attention as a putative ‘anti-aging’ supplement, although little is known about the underlying mechanism with regards to its progressive decline and associated pathologies. Hypotheses pertaining to plausible biological mechanisms include the ability of DHEA/DHEA-S to modulate energy metabolism, systemic inflammation, and that it may counteract or modulate the stress endocrine hormone, cortisol [54,55,56]. Given the critical role of sex steroids and age-related associations, the function of DHEA as an alternative source of androgens and estrogens to local tissues may be a plausible way in which DHEA/ DHEA-S protects against aging and age-related pathologies [57]. Although there is some evidence to suggest that DHEA supplementation may improve skin status and bone turnover in older females, there are few clinical studies powered enough to conclude the effects of DHEA on aging and age-related diseases. In addition, data on the safety profile of long-term DHEA supplementation are still lacking [58].
5.1 Sex Differences in DHEA
Differential trajectories of DHEA levels between the sexes begin following the onset of adrenarche, and differences in levels can again be observed during the perimenopausal period in women, and in older people [59]. Peak levels have also been reported to occur earlier for females [60]. The biological reason for this difference has yet to be elucidated but it has been suggested that higher levels observed in males may reflect chromosomal differences [61]. The gene for steroid sulfatase, which degrades androgens, is located on the X chromosome. Therefore, as males only have one copy of the gene, they consequently have less degradation and higher DHEA concentrations [57]. Although the literature reports somewhat inconsistent results, a recent review concluded that enough evidence supports the association between DHEA and aging in males, but in females this may not exist, or displays a non-linear, U-shaped association. Larger studies, with a prior stratification of sex, are required to confirm these findings [62].
6 Analyses of Steroidal Hormones
The complexity of sex steroid measurement should not be underestimated, and there is current debate over the best technologies to use (see [63] for overview). These steroids exhibit only modest differences in structure, but which amount to profound functional differences. Owing to such subtle differences in structure and small size, steroids are not easy to measure.
Although immunoassays have remained the mainstay of steroid analysis, the reliability of the specificity and sensitivity of these assays have come into questions, particularly commonly used commercially derived assays [64]. Unless preanalytical extraction methods or chromatographic steps are introduced to purify samples prior to the immune-assay, these assays are prone to inaccuracy due to their non-specificity [63]. Mass spectrometry has introduced far greater specificity of steroidal hormones and allows for specific analysis of different steroids (i.e., estrogen, and testosterone). Currently this technique provides the highest specificity due to mass spectrometry providing the exact structural information of the analyte, allowing for specificity between steroid analytes and their precursors. However, it is noted that costs and expertise required for such analyses may prevent many researchers from conducting such analyses. As technology advances and becomes cheaper, this gold standard technology will grow in use.
Relevant to this chapter, difficulty in the measurement of steroids has been proposed for the reason for the inconsistent findings seen in the DHEA aging literature. The low specificity and precision of immunoassays may have yielded incorrect measurements in subjects low in DHEA/ DHEA-S [62].
7 Aging of the Adrenal Endocrine System: The Hypothalamus-Pituitary-Adrenal Axis
Activation of the hypothalamus-pituitary- adrenal (HPA) endocrine axis and the subsequent stress response is a fundamental homeostatic mechanism that enables a wide array of physiological and behavioural responses to actual or perceived threat. Initiated at the level of the hypothalamus via corticotrophin releasing hormone (CRF), a signalling cascade then ensues with adrenocorticotropin hormone (ACTH) released from the anterior pituitary, followed by glucocorticoids being synthesised from cholesterol in the adrenal cortex, and released directly into the bloodstream. Glucocorticoids are lipophilic and largely transported bound to cortisol binding globulin (CBG) leaving only a small fraction (10%) biologically active [65]. As glucocorticoids can readily cross the blood-brain-barrier, the steroids consequently can exert action at both local central nervous system level and systemic peripheral levels, where it induces or represses the transcription of a plethora of target genes [66, 67]. In this way, glucocorticoids orchestrate a vast repertoire of adjustments to adapt to external or internal changes to the environment, ensuring optimal regulation of several interlinked regulatory systems including reproduction, growth, and immunity, and cognitive signalling processes [68]. In addition, fast acting, non-genomic action of glucocorticoids occur, engaging glutamatergic system alterations [69].
Glucocorticoids mediate its own activity and termination via two receptors; the high affinity type 1 mineralocorticoid receptor (MR) and lower affinity type 11 glucocorticoid receptors (GR) [70]. The high affinity of MR to glucocorticoids is thought to be responsible for regulating tonic activity and dictates the basal circadian and ultradian rhythms observed across the day [71]. GR are found widely distributed throughout the brain, with high density found in most neurons and glia. With lower affinity to physiological GC, these receptors only become functionally activated as the stress endocrine hormone cortisol rise following a stressor and play an important role in mediating GC effects on mobilising energy stores, inflammation and neural function [72]. Importantly, it is thought to be primarily responsible for blunting further activity of the HPA stress response. Both receptors act in synergy to mediate HPA dynamics important for several of these systems of homeostasis, eloquently fine tuning the HPA dynamics depending on the necessary action. An example of this is found within cognitive processes, such as learning and memory. GR and MR are both abundantly expressed in neurons of the hippocampus, prefrontal cortex, and amygdala [73] where they are thought to have opposing functions which regulate hippocampal synaptic neuroplasticity during the stress response, important in long term potentiation mechanism of learning and memory. Preclinical rat models have demonstrated that activation of the MRs may be a prerequisite for hippocampal plasticity, while GRs may exert an inhibitory effect of plasticity [74]. Although initial sensitivity to feedback of glucocorticoids due to the high expression of GRs and MRs, after repeated responses seen in acute and chronic stress, the hippocampus down-regulates receptor expression [75]. In line with this, although acute, moderated activation of the HPA axis is a necessary and beneficial response, such chronic activation may lead to tissue damage or receptor desensitisation, resulting in attenuated negative feedback, and ultimately adverse outcomes [76]. Individual differences in vulnerability and resistance to stress, governed by HPA dynamics [77] may thereby contribute to the heterogeneity of the aging, and age-related diseases.
There is evidence that HPA axis dynamics [78] and GR expression levels in areas of the dentate gyrus [79] change over the natural process of aging and are postulated to be a major driver in accelerated aging, with lower diurnal cortisol levels having been associated with longevity [80]. In healthy humans, the HPA axis, and glucocorticoid output typically follows a diurnal pattern. The typical pattern displays a sharp increase upon awakening, known as the cortisol awakening response (CAR) , followed by reduced levels throughout the day, until the sleep nadir [81]. Increased basal cortisol output [82], diurnal amplitude flattening [83], and an altered CAR response both in magnitude and in day to day variability [84] have all been associated in aging models [61]. In addition, attenuated negative feedback by glucocorticoid receptors at the level of the paraventricular nucleus, hypothalamus, hippocampus, and prefrontal cortex have been reported [61, 70]. Furthermore, the 11-β hydroxysteroid dehydrogenase enzymatic activity responsible for the interconversion of inactive cortisone to active cortisol has been reported to decrease with age, resulting in the inefficient inactivation of active cortisol to inactive cortisone [85]. The two isoforms of this enzyme have also been suggested as a potential key mechanism in the acceleration of aging [86]. In addition, the systemic 11-β hydroxysteroid dehydrogenase isoform 1 is predictive of progressive brain atrophy and cognitive decline [87].
Such age-related changes in HPA dynamics are often related with declined cognitive processes, cardiovascular alterations, and psychiatric disease states. For example, a higher 24 h urine output has been associated with Alzheimer’s disease [88]. Mechanistically speaking, this may be a result of cortisol induced apoptosis and death of hippocampal neurons [89], as observed by decreased adult hippocampal neurogenesis in an Alzheimer’s disease model [90].
7.1 Sex Differences in HPA Axis Regulation
Research suggests there are substantial sex differences in HPA-axis dynamics and cortisol levels during regular diurnal maintenance and in response to stress, which may contribute to differential aging dynamics between the sexes [91]. In vitro models have shown that female rodents exhibit greater basal corticosterone production by the adrenal glands [92] and have a more robust HPA axis response to both physical and psychological stressors, thought to be a result of circulating estradiol levels [93]. Clinical investigations have also provided support for the sexual dimorphism of the HPA axis stress response [94]. The HPA axis stress response in females is characterised by a larger, more sustained secretion of ACTH and cortisol, suggesting enhanced activity and reduced negative feedback [95], while the pulsatile cortisol feedback on ACTH mediated by GC receptors appears to be influenced by sex [96]. In addition, there is evidence indicating that both GRs and MRs are less sensitive to cortisol modulation in females than males, suggesting reduced feedback by autoregulation of these receptors [70].
Although the exact mechanism of action remains to be elucidated, estradiol has been shown to enhance HPA activity, while testosterone appears to have an inhibitory effect by acting upon the hypothalamus [97]. In contrast, there is also evidence to indicate that estradiol, but not testosterone, heightens the cortisol-mediated negative feedback on pulsatile ACTH secretion in both aged men and women [96]. Further research must be conducted to understand this complex interplay between the HPA and HPG axis, across the life-course and considering sexual dimorphisms.
In line with these findings, a clear association between menstrual cycle phase and cortisol basal measurement has been shown. Women in the luteal phase of the menstrual cycle have a similar cortisol response to men, whereas in the follicular phase, attenuation of cortisol production has been shown [98]. Notably, increased CBG is known to occur in cases of estrogen excess (e.g., pregnancy and use of estrogen-containing oral contraceptives, resulting in higher concentrations of total cortisol [99], although free cortisol levels are usually unaltered in states of increased CBG [100].
It is also now appreciated that prenatal exposure to early life stressors and increased levels of glucocorticoids can influence later life behaviour, biological processes, and susceptibility for disease states. Support for sex differences in such early-life programming of the HPA in humans has been demonstrated in rodent models, with evidence for the female HPA axis being more vulnerable to stress and glucocorticoid programming, and female offspring demonstrating an increased HPA reactivity [101]. This may be one mechanism underlying sex differences in later life diseases and sex dimorphisms shown in aging.
7.2 Measurement of the HPA Axis
Glucocorticoids have traditionally been assayed using a range of substrates including blood, saliva and urine that provide a sampling procedure that is simple and relatively non-invasive [102]. More recently, cortisol has been measured using hair sampling, which gives a chronic reading of cortisol levels [103]. Salivary cortisol represents the bioavailable, active form of the molecule that escapes the CBGs in the salivary glands and saliva [65]. In addition, unbound cortisol is excreted in the urine and 24 h measurements correlate well with those in serum in cases of cortisol excess [65]. Hair analysis provides the opportunity to determine past cortisol exposure and represents a retrospective index of cumulative cortisol output which is not influenced by the circadian rhythm of the HPA-axis, or by acute stress. As hair grows at an average rate of 1 cm/month, the 1 cm segment closest to the scalp represents total cortisol levels during the most recent month, with the outer segments representing previous months [103,104,105]. However, several limitations should be noted, as different hair care routines (e.g., use of hair dye), seasonal variations, and storage length have all been documented to influence readings [106]. The time of sample collection is also a critical consideration as cortisol follows a circadian rhythm of secretion. The cortisol awakening response (CAR) is measured using a minimum of three separate sampling times using blood or saliva (upon awakening, 30 min after waking, and 45 min after waking) [107]. However, the majority of studies employ a ‘minimal protocol’ by analysing one time point only, which has potential implications for the reliability of measurement. For cross-sectional studies it is recommended that up to six consecutive days of samples should be collected to accurately assess single time-points, and that four measures at two consecutive weeks days are required to reliably measure the CAR as a trait measure [108]. HPA axis dynamics and feedback sensitivity can also be measured using a synthetic glucocorticoid, dexamethasone. In clinical testing of suspected hypercortisolemia, the dexamethasone suppression test (DST) can detect abnormal HPA axis activity by a failure to reduce total cortisol production via stimulating the negative feedback mechanism and ACTH production. Interestingly, this has been found to be moderated by genetic variation [109] and use of hormonal contraceptives. The false positive effect found in fertile women using hormonal contraceptives, due to the resultant increased levels of CBG and consequent increase in total cortisol concentrations, was found to be eliminated after one-week cessation of contraceptive use [110]. Various stressful stimuli that can reliably induce the cortisol response in human research participants can also be used to evaluate HPA dynamics. These include standardised psychosocial protocols, such as the Trier Social Stress Test (TSST), and physical stressors (electrical stimulation).
8 Aging of the Immune System
A functional immune system is critical for protecting the host against infections and malignancies, regulation of wound healing, and ultimately for separation of the ‘self’ from surrounding organisms that compete for space and resources [111]. The immune system is coordinated into two sub-classifications that govern the immune response. The innate immune system mounts a fast, non-discriminatory response, initiated by macrophages and dendritic cells that produce inflammatory mediators, including histamine, bradykinin, serotonin, leukotrienes, prostaglandins, cytokines and several growth factors and enzymes. This promotes either tissue repair/regeneration with subsequent resolution of inflammation, or tissue remodelling/fibrosis [112]. The adaptive response is initiated if the innate immune response fails to respond sufficiently, creating an immunological memory after the initial response to a specific pathogen. This more sophisticated arm of the immune system requires recruitment of B and T cells, followed by antibody and cell-mediated responses, respectively, and consequently has a targeted, albeit slower action [113].
Like all successful adaptive homeostatic responses, subsequent to the activation of the immune response, an ensuing cessation or resolution of inflammation must occur, returning the tissue environment to the basal state allowing for tissue repair/regeneration. Recruitment of macrophages to an anti-inflammatory phenotype is critical to this process and involves the release of anti-inflammatory cytokines including interleukin (IL)-10 and TGF-β, as well as lipid mediators [114]. An overactivated immune response leads to tissue remodelling (tissue fibrosis), autoimmune and neurodegenerative diseases, rather than tissue regeneration [114, 115]. Changes in inflammatory mediators have been identified in age-related syndromes including type 2 diabetes, Alzheimer’s disease and cardiovascular disease [116].
During aging, the immune system loses the ability to protect against pathogens effectively, and fails to support appropriate wound healing [111]. Such a decline in effective immunological functioning results in these subjects not responding efficiently to novel or previously encountered antigens [117]. The adaptive immunological arm undergoes complex changes in the aging process that includes epigenetic and metabolic changes affecting naïve, memory and effector T cells, and B cells [118]. A decrease in the number of naïve T lymphocytes and increase in memory and effector T cells occurs with age, in addition to the reduced diversity in T-cell receptors with consequential diminished functionality of naïve and memory T-cells [116]. Clinically, this results in most vaccines being less immunogenic and efficient in the elderly [119].
Additionally, aging is also associated with progression toward a chronic, sub-clinical inflammatory state, characterised by elevation of peripheral pro-inflammatory chemical mediators in the absence of overt infection, a term coined ‘inflamm-aging ’ [120]. Several human studies have demonstrated an association between elevated levels of cytokines, especially IL-6, and a decline in innate immune function in older individuals [121]. Such a peripheral inflammatory state has been associated with the susceptibility and progression of many age-related disease states including cancer, diabetes [122], and cognitive and structural brain changes [123]. Moreover, it has been demonstrated as a key risk factor of mortality [124]. In addition, the innate arm of the immune system initiates cross talk with the adaptive arm through antigen presentation, co-stimulatory molecule expression and cytokine production, and consequently can contribute to adaptive immune responses [125]. More recently, it has been discovered that at sites of infection, adaptive immune memory cells can also regulate the innate inflammatory response, by the epigenetic reprogramming of innate immune cells by previous experiences [126]. Interestingly, it has been hypothesised that centenarians exert a counter action to this pro-inflammatory state, by producing increased amounts of anti-inflammatory cytokine mediators including IL-10 and TGF-β [127].
8.1 Sex Differences the Immunological Response
There is a growing body of evidence demonstrating inherent sex differences in the immune response, which includes both the innate and adaptive arms of the immune system. On average, females exhibit a stronger innate and adaptive immune response than males, resulting in improved pathogen clearance, vaccine efficiency, but greater predisposition to autoimmunity and chronic inflammatory disorders [128]. Sex chromosomes contribute to genetic differences due to the fact that many immune-related genes (e.g., FoxP3 and toll like receptors 7 and 8) are present on the X chromosome. As the possibility of incomplete X-chromosome inactivation occurring in females exists, this can lead to over-expression in females of such immune related genes [129, 130]. Sex hormones can also interact with genetic and environmental factors that determine immunity and appear to influence multiple aspects of the immune system, including the contribution to cell differentiation, cytokine profiles, and epigenetic alterations [130, 131]. Estrogen receptors have been shown to regulate cells and pathways in both arms of the immune system in a predominately stimulatory fashion, in addition to immune cell development [132]. On the other hand, androgens have been shown to be primarily immunosuppressive, suppressing immune reactivity and inflammation [133]. Evidence for sex disparity does exists in the immunological response throughout aging, although the majority of studies do not stratify for sex. Females who are in the menopausal period of their reproductive lives show increased peripheral pro-inflammatory markers, higher numbers of natural killer immune cells with reduced cytotoxicity, and reduced numbers of B and T cells, relative to premenopausal females [134]. Research investigating differential sex influence in the innate immune system is still in its infancy, although data exist suggesting an elevated production of inflammatory cytokines and proteins in females compared to males persists among aged individuals [135, 136]. With regards to adaptive immunity, proliferation of T cells, central to the adaptive immune response, shows a decrease with aging, although this rate of decline was significantly lower in females, than in males [137]. Sex differences have also been noted to occur in response to vaccines protecting against influenza, tetanus, pertussis, shingles and pneumococcal infections, and the efficacy of vaccines in older individuals is consistently higher in females than in males [136].
Collectively, the major changes of the innate and adaptive immune system with aging result in vulnerability to certain infections, and decreased efficacy of many vaccines. Although sex differences in the aging immune system have not been studied extensively, addressing such sex differences may aid in greater effectiveness of vaccines and immunotherapies [130]. As several diseases associated with age are also sensitive to alterations of the immune system, it is important to evaluate potentially- associated sex differences in the underlying pathophysiological processes.
9 Conclusions
The capacity of homeostatic biological systems to continuously adjust for optimal functioning during healthy aging may reflect heterogeneity observed in the aging process. Importantly, such systems including endocrine, immune and cognitive systems appear to be moderated by sex, which may be a defining factor in determining sex-based differences in age-related processes, and diseases. Aging appears to be multi-factorial and characterised by the dysregulation of complex system dynamics, namely the interplay of these homeostatic mechanisms driving the aging process. It can be hypothesised that dysregulation in any of these systems may impose feed-forward alterations on other systems, and dysregulation early in the accelerated aging process may be different for different people. This makes it particularly challenging to research this field, especially early in the aging process. Composite biomarker panels are required at multiple time points in order to target multiple systems and to better understand the chronicity of biomarkers during aging. Moreover, it is critical that future studies specifically address sex-effects when studying the aging process and age-related diseases, to enable sex differences, which are non-modifiable risk factors, to be differentiated from potentially modifiable lifestyle and environmental risk factors. This is crucial to advance therapeutic options that may include sex-based and hormone-based interventions. Policies put forward by the National Institute of Health regarding the requirement of sex and gender inclusion plans in both preclinical and clinical research, underscores this point. Biomarkers of aging cannot escape this necessity.
References
Lowsky DJ, Olshansky SJ, Bhattacharya J, Goldman DP (2013) Heterogeneity in healthy aging. J Gerontol A Biol Sci Med Sci 69(6):640–649
Pomatto LCD, Davies KJA (2017) The role of declining adaptive homeostasis in aging. J Physiol 595(24):7275–7309
Davies KJ (2016) Adaptive homeostasis. Mol Asp Med 49:1–7
Rios FJ, Moustaid-Moussa N, Martins JO (2018) Interplay between hormones, the immune system, and metabolic disorders. Mediat Inflamm 2018:8654212. https://doi.org/10.1155/2018/8654212
Lara J, Cooper R, Nissan J, Ginty AT, Khaw K-T, Deary IJ et al (2015) A proposed panel of biomarkers of healthy aging. BMC Med 13:222. https://doi.org/10.1186/s12916-015-0470-9
Podcasy JL, Epperson CN (2016) Considering sex and gender in Alzheimer disease and other dementias. Dialogues Clin Neurosci 18(4):437–446
Gobinath A, Choleris E, Galea L (2017) Sex, hormones, and genotype interact to influence psychiatric disease, treatment, and behavioral research. J Neurosci Res 95(1–2):50–64
Austad SN, Fischer KE (2016) Sex differences in lifespan. Cell Metab 23(6):1022–1033
Ullah MF, Ahmad A, Bhat SH, Abu-Duhier FM, Barreto GE, Ashraf GM (2019) Impact of sex differences and gender specificity on behavioral characteristics and pathophysiology of neurodegenerative disorders. Neurosci Biobehav Rev 102:95–105
Laws KR, Irvine K, Gale TM (2018) Sex differences in Alzheimer’s disease. Curr Opin Psychiatry 31(2):133–139
Mielke MM, Vemuri P, Rocca WA (2014) Clinical epidemiology of Alzheimer’s disease: assessing sex and gender differences. Clin Epidemiol 6:37–48
Jiao SS, Bu XL, Liu YH, Zhu C, Wang QH, Shen LL et al (2016) Sex dimorphism profile of Alzheimer’s disease-type pathologies in an APP/PS1 Mouse Model. Neurotox Res 29(2):256–266
Altmann A, Tian L, Henderson VW, Greicius MD, Alzheimer’s Disease Neuroimaging Initiative Investigators (2014) Sex modifies the APOE-related risk of developing Alzheimer disease. Ann Neurol 75(4):563–573
Jurado-Coronel JC, Cabezas R, Avila Rodriguez MF, Echeverria V, Garcia-Segura LM, Barreto GE (2018) Sex differences in Parkinson’s disease: features on clinical symptoms, treatment outcome, sexual hormones and genetics. Front Neuroendocrinol 50:18–30
Georgiev D, Hamberg K, Hariz M, Forsgren L, Hariz GM (2017) Gender differences in Parkinson’s disease: a clinical perspective. Acta Neurol Scand 136(6):570–584
Liu R, Umbach DM, Peddada SD, Xu Z, Tröster AI, Huang X et al (2015) Potential sex differences in nonmotor symptoms in early drug-naive Parkinson disease. Neurology 84(21):2107–2115
Nugent BM, Tobet SA, Lara HE, Lucion AB, Wilson ME, Recabarren SE et al (2012) Hormonal programming across the lifespan. Horm Metab Res 44(8):577–586
Diamanti-Kandarakis E, Dattilo M, Macut D, Duntas L, Gonos ES, Goulis DG et al (2017) MECHANISMS IN ENDOCRINOLOGY: aging and anti-aging: a combo-endocrinology overview. Eur J Endocrinol 176(6):R283–R308
Raju GAR, Chavan R, Deenadayal M, Gunasheela D, Gutgutia R, Haripriya G et al (2013) Luteinizing hormone and follicle stimulating hormone synergy: a review of role in controlled ovarian hyper-stimulation. J Hum Reprod Sci 6(4):227–234
Del Río JP, Alliende MI, Molina N, Serrano FG, Molina S, Vigil P (2018) Steroid hormones and their action in women’s brains: the importance of hormonal balance. Front Public Health 6:141. https://doi.org/10.3389/fpubh.2018.00141
Podfigurna A, Lukaszuk K, Czyzyk A, Kunicki M, Maciejewska-Jeske M, Jakiel G et al (2018) Testing ovarian reserve in pre-menopausal women: why, whom and how? Maturitas 109:112–117
Gill S, Sharpless JL, Rado K, Hall JE (2002) Evidence that GnRH decreases with gonadal steroid feedback but increases with age in postmenopausal women. J Clin Endocrinol Metab 87(5):2290–2296
Veldhuis JD (2013) Changes in pituitary function with ageing and implications for patient care. Nat Rev Endocrinol 9(4):205–215
Shaw ND, Histed SN, Srouji SS, Yang J, Lee H, Hall JE (2010) Estrogen negative feedback on gonadotropin secretion: evidence for a direct pituitary effect in women. J Clin Endocrinol Metab 95(4):1955–1961
Bhatta S, Blair JA, Casadesus G (2018) Luteinizing hormone involvement in aging female cognition: not all is estrogen loss. Front Endocrinol (Lausanne) 9:544. https://doi.org/10.3389/fendo.2018.00544
Muka T, Oliver-Williams C, Kunutsor S, Laven JSE, Fauser BCJM, Chowdhury R et al (2016) Association of age at onset of menopause and time since onset of menopause with cardiovascular outcomes, intermediate vascular traits, and all-cause mortality: a systematic review and meta-analysis. JAMA Cardiol 1(7):767–776
Hasanpour M, Nourazarian A, Geranmayeh MH, Nikanfar M, Khaki-Khatibi F, Rahbarghazi R (2018) The dynamics of neurosteroids and sex-related hormones in the pathogenesis of Alzheimer’s disease. NeuroMolecular Med 20(2):215–224
Gurvich C, Hoy K, Thomas N, Kulkarni J (2018) Sex differences and the influence of sex hormones on cognition through adulthood and the aging process. Brain Sci 8(9). pii: E163. https://doi.org/10.3390/brainsci8090163
Jones CM, Boelaert K (2015) The endocrinology of aging: a mini-review. Gerontology 61(4):291–300
Camacho EM, Huhtaniemi IT, O’Neill TW, Finn JD, Pye SR, Lee DM et al (2013) Age-associated changes in hypothalamic-pituitary-testicular function in middle-aged and older men are modified by weight change and lifestyle factors: longitudinal results from the European Male Aging Study. Eur J Endocrinol 168(3):445–455
Lapauw B, Goemaere S, Zmierczak H, Van Pottelbergh I, Mahmoud A, Taes Y et al (2008) The decline of serum testosterone levels in community-dwelling men over 70 years of age: descriptive data and predictors of longitudinal changes. Eur J Endocrinol 159(4):459–468
Travison T, Araujo A, Kupelian V, O’Donnell A, McKinlay J, Travison T et al (2007) The relative contributions of aging, health, and lifestyle factors to serum testosterone decline in men. J Clin Endocrinol Metab 92(2):549–555
Derby C, Zilber S, Brambilla D, Morales K, McKinlay J, Derby C et al (2006) Body mass index, waist circumference and waist to hip ratio and change in sex steroid hormones: the Massachusetts Male Aging Study. Clin Endocrinol 65(1):125–131
Feldman H, Longcope C, Derby C, Johannes C, Araujo A, Coviello A et al (2002) Age trends in the level of serum testosterone and other hormones in middle-aged men: longitudinal results from the Massachusetts Male Aging Study. J Clin Endocrinol Metab 87(2):589–598
Wu FC, Tajar A, Beynon JM, Pye SR, Silman AJ, Finn JD et al (2010) Identification of late-onset hypogonadism in middle-aged and elderly men. New Eng J Med 363(2):123–315
Shores MM, Matsumoto AM, Sloan KL, Kivlahan DR (2006) Low serum testosterone and mortality in male veterans. Arch Intern Med 166(15):1660–1665
O’Donnell AB, Araujo AB, McKinlay JB, Kupelian V, Travison TG (2007) The relative contributions of aging, health, and lifestyle factors to serum testosterone decline in men. J Clin Endocrinol Metab 92(2):549–555
Matsumoto AM (2002) Andropause: clinical implications of the decline in serum testosterone levels with aging in men. J Gerontol A Biol Sci Med Sci 57(2):M76–M99
Forsberg CW, Smith NL, Shores MM, Matsumoto AM, Anawalt BD (2012) Testosterone treatment and mortality in men with low testosterone levels. J Clin Endocrinol Metab 97(6):2050–2058
Pastuszak AW, Kohn TP, Estis J, Lipshultz LI (2017) Low plasma testosterone is associated with elevated cardiovascular disease biomarkers. J Sex Med 14(9):1095–1103
Maki PM, Mordecai KL, Rubin LH, Sundermann E, Savarese A, Eatough E et al (2015) Menstrual cycle effects on cortisol responsivity and emotional retrieval following a psychosocial stressor. Horm Behav 74:201–208
Ramsey JM, Cooper JD, Penninx BW, Bahn S (2016) Variation in serum biomarkers with sex and female hormonal status: implications for clinical tests. Sci Rep 6:26947. https://doi.org/10.1038/srep26947
Yiallouris A, Tsioutis C, Agapidaki E, Zafeiri M, Agouridis AP, Ntourakis D et al (2019) Adrenal aging and its implications on stress responsiveness in humans. Front Endocrinol (Lausanne) 10:54. https://doi.org/10.3389/fendo.2019.00054
Powrie YSL, Smith C (2018) Central intracrine DHEA synthesis in ageing-related neuroinflammation and neurodegeneration: therapeutic potential? J Neuroinflammation 15(1):289. https://doi.org/10.1186/s12974-018-1324-0
Kroboth PD, Salek FS, Pittenger AL, Fabian TJ, Frye RF (1999) DHEA and DHEA-S: a review. J Clin Pharmacol 39(4):327–348
Miller KK, Al-Rayyan N, Ivanova MM, Mattingly KA, Ripp SL, Klinge CM et al (2013) DHEA metabolites activate estrogen receptors alpha and beta. Steroids 78(1):15–25
Webb SJ, Geoghegan TE, Prough RA, Michael Miller KK (2006) The biological actions of dehydroepiandrosterone involves multiple receptors. Drug Metab Rev 38(1–2):89–116
Ferrari E, Cravello L, Muzzoni B, Casarotti D, Paltro M, Solerte SB et al (2001) Age-related changes of the hypothalamic-pituitary-adrenal axis: pathophysiological correlates. Eur J Endocrinol 144(4):319–329
van den Beld AW, Kaufman JM, Zillikens MC, Lamberts SWJ, Egan JM, van der Lely AJ (2018) The physiology of endocrine systems with ageing. Lancet Diabetes Endocrinol 6(8):647–658
Voznesensky M, Walsh S, Dauser D, Brindisi J, Kenny AM (2009) The association between dehydroepiandosterone and frailty in older men and women. Age Ageing 38(4):401–406
Rendina DN, Ryff CD, Coe CL (2017) Precipitous dehydroepiandrosterone declines reflect decreased physical vitality and function. J Gerontol A Biol Sci Med Sci 72(6):747–753
Morrison MF, Katz IR, Parmelee P, Boyce AA, TenHave T (1998) Dehydroepiandrosterone sulfate (DHEA-S) and psychiatric and laboratory measures of frailty in a residential care population. Am J Geriatr Psychiatry 6(4):277–284
Jiménez MC, Sun Q, Schürks M, Chiuve S, Hu FB, Manson JE et al (2013) Low dehydroepiandrosterone sulfate is associated with increased risk of ischemic stroke among women. Stroke 44(7):1784–1789
Vieira-Marques C, Arbo BD, Cozer AG, Hoefel AL, Cecconello AL, Zanini P et al (2017) Sex-specific effects of dehydroepiandrosterone (DHEA) on glucose metabolism in the CNS. J Steroid Biochem Mol Biol 171:1–10
Prall SP, Muehlenbein MP (2018) DHEA modulates immune function: a review of evidence. Vitam Horm 108:125–144
Kamin HS, Kertes DA (2017) Cortisol and DHEA in development and psychopathology. Horm Behav 89:69–85
Labrie F (2010) DHEA, important source of sex steroids in men and even more in women. Prog Brain Res 182:97–148
Samaras N, Samaras D, Frangos E, Forster A, Philippe J (2013) A review of age-related dehydroepiandrosterone decline and its association with well-known geriatric syndromes: is treatment beneficial? Rejuvenation Res 16(4):285–294
Sulcová J, Hill M, Hampl R, Stárka L (1997) Age and sex related differences in serum levels of unconjugated dehydroepiandrosterone and its sulphate in normal subjects. J Endocrinol 154(1):57–62
Orentreich N, Brind JL, Rizer RL, Vogelman JH (1984) Age changes and sex differences in serum Dehydroepiandrosterone sulfate concentrations throughout adulthood. J Clin Endocrinol Metab 59(3):551–555
Quinn TA, Robinson SR, Walker D (2018) Dehydroepiandrosterone (DHEA) and DHEA sulfate: roles in brain function and disease. In: Drevensek G (ed) Sex hormones in neurodegenerative processes and diseases. IntechOpen. ISBN-10: 1789230144
Ohlsson C, Vandenput L, Tivesten A (2015) DHEA and mortality: what is the nature of the association? J Steroid Biochem Mol Biol 145:248–253
Wudy SA, Schuler G, Sanchez-Guijo A, Hartmann MF (2018) The art of measuring steroids: principles and practice of current hormonal steroid analysis. J Steroid Biochem Mol Biol 179:88–103
Stanczyk FZ, Cho MM, Endres DB, Morrison JL, Patel S, Paulson RJ (2003) Limitations of direct estradiol and testosterone immunoassay kits. Steroids 68(14):1173–1178
El-Farhan N, Rees DA, Evans C (2017) Measuring cortisol in serum, urine and saliva - are our assays good enough? Ann Clin Biochem 54(3):308–322
Galon J, Franchimont D, Hiroi N, Frey G, Boettner A, Ehrhart-Bornstein M et al (2002) Gene profiling reveals unknown enhancing and suppressive actions of glucocorticoids on immune cells. FASEB J 16(1):61–71
Oakley RH, Cidlowski JA (2013) The biology of the glucocorticoid receptor: new signaling mechanisms in health and disease. J Allergy Clin Immunol 132(5):1033–1044
Sapolsky RM, Romero LM, Munck AU (2000) How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocr Rev 21(1):55–89
Finsterwald C, Alberini CM (2014) Stress and glucocorticoid receptor-dependent mechanisms in long-term memory: from adaptive responses to psychopathologies. Neurobiol Learn Mem 112:17–29
Herman JP, McKlveen JM, Ghosal S, Kopp B, Wulsin A, Makinson R et al (2016) Regulation of the hypothalamic-pituitary-adrenocortical stress response. Compr Physiol 6(2):603–621
den Boon FS, Sarabdjitsingh RA (2017) Circadian and ultradian patterns of HPA-axis activity in rodents: significance for brain functionality. Best Pract Res Clin Endocrinol Metab 31(5):445–457
McEwen BS, De Kloet ER, Rostene W (1986) Adrenal steroid receptors and actions in the nervous system. Physiol Rev 66(4):1121–1188
Lupien SJ, Maheu F, Tu M, Fiocco A, Schramek TE (2007) The effects of stress and stress hormones on human cognition: implications for the field of brain and cognition. Brain Cogn 65(3):209–237
Avital A, Segal M, Richter-Levin G (2006) Contrasting roles of corticosteroid receptors in hippocampal plasticity. J Neurosci 26(36):9130–9134
Vyas S, Rodrigues AJ, Silva JM, Tronche F, Almeida OFX, Sousa N et al (2016) Chronic stress and glucocorticoids: from neuronal plasticity to neurodegeneration. Neural Plast 2016:6391686. https://doi.org/10.1155/2016/6391686
Herman JP (2013) Neural control of chronic stress adaptation. Front Behav Neurosci 7:61. https://doi.org/10.3389/fnbeh.2013.00061
Ancelin M-L, Scali J, Norton J, Ritchie K, Dupuy A-M, Chaudieu I et al (2017) Heterogeneity in HPA axis dysregulation and serotonergic vulnerability to depression. Psychoneuroendocrinology 77:90–94
Gupta D, Morley JE (2014) Hypothalamic-pituitary-adrenal (HPA) axis and aging. Compr Physiol 4(4):1495–1510
Wang Q, Van Heerikhuize J, Aronica E, Kawata M, Seress L, Joels M et al (2013) Glucocorticoid receptor protein expression in human hippocampus; stability with age. Neurobiol Aging 34(6):1662–1673
Noordam R, Jansen SWM, Akintola AA, Oei NYL, Maier AB, Pijl H et al (2012) Familial longevity is marked by lower diurnal salivary cortisol levels: the Leiden Longevity Study. PLoS One 7(2):e31166. https://doi.org/10.1371/journal.pone.0031166
Weitzman ED, Fukushima D, Nogeire C, Roffwarg H, Gallagher TF, Hellman L (1971) Twenty-four hour pattern of the episodic secretion of cortisol in normal subjects. J Clin Endocrinol Metab 33(1):14–22
Lupien S, Lecours AR, Lussier I, Schwartz G, Nair NP, Meaney MJ (1994) Basal cortisol levels and cognitive deficits in human aging. J Neurosci 14(5 Pt 1):2893–2903
Deuschle M, Gotthardt U, Schweiger U, Weber B, Korner A, Schmider J et al (1997) With aging in humans the activity of the hypothalamus-pituitary-adrenal system increases and its diurnal amplitude flattens. Life Sci 61(22):2239–2246
Almeida DM, Piazza JR, Stawski RS (2009) Interindividual differences and intraindividual variability in the cortisol awakening response: an examination of age and gender. Psychol Aging 24(4):819–827
Fardella CE, Campino C, Carvajal CA, Baudrand R, Kalergis AM, Martinez-Aguayo A et al (2013) Age-related changes in 11β-hydroxysteroid dehydrogenase type 2 activity in normotensive subjects. Am J Hypertens 26(4):481–487
Chapman K, Holmes M, Seckl J (2013) 11β-hydroxysteroid dehydrogenases: intracellular gate-keepers of tissue glucocorticoid action. Physiol Rev 93(3):1139–3206
MacLullich AM, Ferguson KJ, Reid LM, Deary IJ, Starr JM, Wardlaw JM et al (2012) 11beta-hydroxysteroid dehydrogenase type 1, brain atrophy and cognitive decline. Neurobiol Aging 33(1):207.e1-8
Ennis GE, An Y, Resnick SM, Ferrucci L, O’Brien RJ, Moffat SD (2017) Long-term cortisol measures predict Alzheimer disease risk. Neurology 88(4):371–378
Zhao H, Xu H, Xu X, Young D (2007) Predatory stress induces hippocampal cell death by apoptosis in rats. Neurosci Lett 421(2):115–120
Donovan MH, Yazdani U, Norris RD, Games D, German DC, Eisch AJ (2006) Decreased adult hippocampal neurogenesis in the PDAPP mouse model of Alzheimer’s disease. J Comp Neurol 495(1):70–83
Rincón-Cortés M, Herman JP, Lupien S, Maguire J, Shansky RM (2019) Stress: influence of sex, reproductive status and gender. Neurobiol Stress 10:100155. https://doi.org/10.1016/j.ynstr.2019.100155
Kitay JI (1961) Enhancement of steroidogenesis by rat adrenal slices in vitro with estradiol-17-beta. Nature 192:358–359
Oyola MG, Handa RJ (2017) Hypothalamic-pituitary-adrenal and hypothalamic-pituitary-gonadal axes: sex differences in regulation of stress responsivity. Stress 20(5):476–494
Toufexis D, Rivarola MA, Lara H, Viau V (2014) Stress and the reproductive axis. J Neuroendocrinol 26(9):573–586
Handa RJ, McGivern RF (2009) Stress response: sex differences. In: Squire LR (ed) Encyclopedia of neuroscience. Academic, Oxford, pp 511–517. ISBN: 9780080446172
Roelfsema F, Aoun P, Veldhuis JD (2016) Pulsatile cortisol feedback on ACTH secretion is mediated by the glucocorticoid receptor and modulated by gender. J Clin Endocrinol Metab 101(11):4094–4102
Viau V (2002) Functional cross-talk between the hypothalamic-pituitary-gonadal and -adrenal axes. J Neuroendocrinol 14(6):506–513
Kirschbaum C, Kudielka BM, Gaab J, Schommer NC, Hellhammer DH (1999) Impact of gender, menstrual cycle phase, and oral contraceptives on the activity of the hypothalamus-pituitary-adrenal axis. Psychosom Med 61(2):154–162
Simunkova K, Stárka L, Hill M, Kríz L, Hampl R, Vondra K (2008) Comparison of total and salivary cortisol in a low-dose ACTH (Synacthen) test: influence of three-month oral contraceptives administration to healthy women. Physiol Res 57(Suppl 1):S193–S199
Roche DJO, King AC, Cohoon AJ, Lovallo WR (2013) Hormonal contraceptive use diminishes salivary cortisol response to psychosocial stress and naltrexone in healthy women. Pharmacol Biochem Behav 109:84–90
Gifford RM, Reynolds RM (2017) Sex differences in early-life programming of the hypothalamic-pituitary-adrenal axis in humans. Early Hum Dev 114:7–10
Levine A, Zagoory-Sharon O, Feldman R, Lewis JG, Weller A (2007) Measuring cortisol in human psychobiological studies. Physiol Behav 90(1):43–53
Staufenbiel S, Penninx BW, Spijker A, Elzinga BM, van Rossum E (2012) Hair cortisol, stress exposure, and mental health in humans: a systematic review. Psychoneuroendocrinology 38(8):1220–1235
Novak MA, Meyer JS (2012) Minireview: hair cortisol: a novel biomarker of hypothalamic-pituitary-adrenocortical activity. Endocrinology 153(9):4120–4127
Noppe G, de Rijke YB, Dorst K, van den Akker ELT, van Rossum EFC (2015) LC-MS/MS-based method for long-term steroid profiling in human scalp hair. Clin Endocrinol 83(2):162–166
Abell JG, Stalder T, Ferrie JE, Shipley MJ, Kirschbaum C, Kivimäki M et al (2016) Assessing cortisol from hair samples in a large observational cohort: the Whitehall II study. Psychoneuroendocrinology 73:148–156
Steptoe A, Serwinski B (2016) Cortisol awakening response. In: Fink G (ed) Stress: concepts, cognition, emotion, and behavior, 1st edn. Academic, pp 277–283. ISBN-10: 0128009519
Hellhammer J, Fries E, Schweisthal OW, Schlotz W, Stone A, Hagemann D (2007) Several daily measurements are necessary to reliably assess the cortisol rise after awakening: state- and trait components. Psychoneuroendocrinology 32(1):80–86
Fujii T, Hori H, Ota M, Hattori K, Teraishi T, Sasayama D et al (2014) Effect of the common functional FKBP5 variant (rs1360780) on the hypothalamic-pituitary-adrenal axis and peripheral blood gene expression. Psychoneuroendocrinology 42:89–97
Vastbinder M, Kuindersma M, Mulder AH, Schuijt MP, Mudde AH (2016) The influence of oral contraceptives on overnight 1 mg dexamethasone suppression test. Neth J Med 74(4):158–161
Weyand CM, Goronzy JJ (2016) Aging of the immune system. Mechanisms and therapeutic targets. Ann Am Thorac Soc 13(Suppl 5):S422–S428
Eming SA, Wynn T, Martin P (2017) Inflammation and metabolism in tissue repair and regeneration. Science 356(6342):1026–1030
Bonilla FA, Oettgen HC (2010) Adaptive immunity. J Allergy Clin Immunol 125(2 Suppl 2):S33–S40
Kulkarni OP, Lichtnekert J, Anders HJ, Mulay SR (2016) The immune system in tissue environments regaining homeostasis after injury: is “inflammation” always inflammation? Mediat Inflamm 2016:2856213. https://doi.org/10.1155/2016/2856213
Blach-Olszewska Z, Leszek J (2007) Mechanisms of over-activated innate immune system regulation in autoimmune and neurodegenerative disorders. Neuropsychiatr Dis Treat 3(3):365–372
Fulop T, Larbi A, Dupuis G, Le Page A, Frost EH, Cohen AA et al (2018) Immunosenescence and inflamm-aging as two sides of the same coin: friends or foes? Front Immunol 8:1960. https://doi.org/10.3389/fimmu.2017.01960
Ciabattini A, Nardini C, Santoro F, Garagnani P, Franceschi C, Medaglini D (2018) Vaccination in the elderly: the challenge of immune changes with aging. Semin Immunol 40:83–94
Kondilis-Mangum HD, Wade PA (2013) Epigenetics and the adaptive immune response. Mol Asp Med 34(4):813–825
Weinberger B, Grubeck-Loebenstein B (2012) Vaccines for the elderly. Clin Microbiol Infect 18(Suppl 5):100–108
Franceschi C, Bonafe M, Valensin S, Olivieri F, De Luca M, Ottaviani E et al (2000) Inflamm-aging. An evolutionary perspective on immunosenescence. Ann N Y Acad Sci 908:244–254
Shaw AC, Goldstein DR, Montgomery RR (2013) Age-dependent dysregulation of innate immunity. Nat Rev Immunol 13(12):875–887
Rea IM, Gibson DS, McGilligan V, McNerlan SE, Alexander HD, Ross OA (2018) Age and age-related diseases: role of inflammation triggers and cytokines. Front Immunol 9:586. https://doi.org/10.3389/fimmu.2018.00586
Jiang J, Wen W, Sachdev PS (2016) Macrophage inhibitory cytokine-1/growth differentiation factor 15 as a marker of cognitive aging and dementia. Curr Opin Psychiatry 29(2):181–186
Sullivan DH, Roberson PK, Johnson LE, Mendiratta P, Bopp MM, Bishara O (2007) Association between inflammation-associated cytokines, serum albumins, and mortality in the elderly. J Am Med Dir Assoc 8(7):458–463
Leliefeld PHC, Koenderman L, Pillay J (2015) How neutrophils shape adaptive immune responses. Front Immunol 6:471. https://doi.org/10.3389/fimmu.2015.00471
Cronkite DA, Strutt TM (2016) The regulation of inflammation by innate and adaptive lymphocytes. J Immunol Res 2018:1467538. https://doi.org/10.1155/2018/1467538
Minciullo PL, Catalano A, Mandraffino G, Casciaro M, Crucitti A, Maltese G et al (2016) Inflammaging and anti-inflammaging: the role of cytokines in extreme longevity. Arch Immunol Ther Exp (Warsz) 64(2):111–126
Klein SL, Flanagan K (2016) Sex differences in immune responses. Nat Rev Immunol 16(10):626–638
Gubbels Bupp MR (2015) Sex, the aging immune system, and chronic disease. Cell Immunol 294(2):102–110
Edwards M, Dai R, Ahmed SA (2018) Our environment shapes us: the importance of environment and sex differences in regulation of autoantibody production. Front Immunol 9:478. https://doi.org/10.3389/fimmu.2018.00478
Jorgensen TN (2015) Sex disparities in the immune response. Cell Immunol 294(2):61–62
Kovats S (2015) Estrogen receptors regulate innate immune cells and signaling pathways. Cell Immunol 294(2):63–69
Gubbels Bupp MR, Jorgensen TN (2018) Androgen-induced immunosuppression. Front Immunol 9:794. https://doi.org/10.3389/fimmu.2018.00794
Flanagan KL, Fink AL, Plebanski M, Klein SL (2017) Sex and gender differences in the outcomes of vaccination over the life course. Annu Rev Cell Dev Biol 33:577–599
Furman D, Hejblum BP, Simon N, Jojic V, Dekker CL, Thiebaut R et al (2014) Systems analysis of sex differences reveals an immunosuppressive role for testosterone in the response to influenza vaccination. Proc Natl Acad Sci U S A 111(2):869–874
Fink AL, Klein SL (2015) Sex and gender impact immune responses to vaccines among the elderly. Physiology (Bethesda) 30(6):408–416
Hirokawa K, Utsuyama M, Hayashi Y, Kitagawa M, Makinodan T, Fulop T (2013) Slower immune system aging in women versus men in the Japanese population. Immun Ageing 10(1):19. https://doi.org/10.1186/1742-4933-10-19
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Thomas, N., Gurvich, C., Kulkarni, J. (2019). Sex Differences in Aging and Associated Biomarkers. In: Guest, P. (eds) Reviews on Biomarker Studies in Aging and Anti-Aging Research. Advances in Experimental Medicine and Biology(), vol 1178. Springer, Cham. https://doi.org/10.1007/978-3-030-25650-0_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-25650-0_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-25649-4
Online ISBN: 978-3-030-25650-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)