Abstract
Laparoscopic right hemicolectomy for malignant disease is a safe and effective approach to achieve an adequate oncologic outcome and decrease perioperative complications. Data from studies comparing open and laparoscopic surgery are presented and compared. Appropriate patient selection and preparation are important in attaining these goals. Experience in open oncologic technique and advanced laparoscopy are mandatory to master difficulties which may occur especially in right hemicolectomy with its multiple anatomic vascular variations. Modifications to the operative technique can facilitate challenging dissections, but the oncologic principles must be followed which comprise complete mesocolic excision and high vascular tie and removal of the specimen with preserved surfaces and no tears or defects. A medial-to-lateral approach is recommended but a primarily lateral mobilization is also feasible. A standardized stepwise approach is presented and illustrated which should facilitate the procedure, improve outcomes and avoid complications. The most frequently reported complication is bleeding which may be harzardous if central vessels like the superior mesenteric vein or artery are affected. By choosing appropriate dissection instruments and carefully handling dissection planes and mesenteric tissue in general, complications will be minimized and the advantages of a laparoscopic approach will be fully accomplished.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction and Rationale
Laparoscopic right hemicolectomy is oncologically effective for malignant disease and associated with improved patient outcomes when compared to open operations [1, 2]. This approach has therefore become an important tool in the arsenal of surgeons who perform right colon resections. Compared with an open approach, minimally invasive surgery has been associated with reduced length of hospital stay, faster return to work, earlier normalization of diet, decreased perioperative pain, improved cosmesis, lower incidence of incisional hernia, lower narcotic utilization, decreased transfusion requirement, and improved quality of life.
Laparoscopic right hemicolectomy was first described in the early 1990s following the success of laparoscopic cholecystectomy [3, 4]. The initial reports of the procedure utilized between four and six laparoscopic trocars to perform a lateral-to-medial mobilization and intracorporeal mesenteric ligation; however, the anastomosis was performed extracorporeally. The variation of a hand-assisted laparoscopic surgery (HALS) approach showed equivalent short- and long-term recovery and oncological outcomes when compared with traditional laparoscopic surgery, but longer operative times were reported for hand-assisted laparoscopic surgery [5]. Even for those surgeons who prefer straight laparoscopy for a right colectomy, the hand-assisted approach can be an excellent adjunct to prevent conversion to laparotomy.
Over time, the laparoscopic dissection technique has evolved. The medial-to-lateral dissection gained acceptance and was increasingly favored based on shorter operative times, improved exposure, and equivalent oncologic outcomes when compared with a lateral-to-medial dissection [6, 7].
Adhering to the basic principles of oncologic resection, single-incision laparoscopic approaches have been employed. Single-incision right colectomy claimed improved cosmetic results, while it was shown to have equivalent operative times and blood loss when compared to traditional laparoscopic resection [8]. A large randomized controlled trial comparing single-incision and multi-port laparoscopy for colon resection suggested that the cosmetic result was only improved for those undergoing a truly single-incision resection [9]. The single-incision approach therefore remains a viable option for patients who desire the best possible cosmetic result.
The most recent evolution to minimally invasive right colectomy is robotic surgery. A randomized controlled trial comparing the robotic to traditional laparoscopic approach found similar oncologic results and short- and long-term outcomes. However, longer operative times and increased cost lead some to question its role for right-sided colon cancer [10]. The robot, however, offers opportunities for advanced minimally invasive techniques even for right colectomy, e.g., facilitating performance of an intracorporeal anastomosis (ICA) . Data suggest that robotic right hemicolectomy with ICA may result in a shorter time to return of bowel function and decreased overall incision length, at the cost of higher expense and longer operative times [11]. For more details on techniques and results, please refer to the chapters on robotic right-sided colon resection (Chap. 15) and options for ileocolonic reconstruction (Chap. 14).
In the current chapter, the oncologic principles of a right hemicolectomy performed for malignancy will be reviewed, with emphasis on complete mesocolic excision (CME) and laparoscopic techniques .
Indications and Contraindications
Laparoscopic right hemicolectomy is an appropriate operation for the majority of right-sided colon malignancies [12]. Several well-designed, large, multinational, randomized controlled trials have shown mostly equivalent oncologic outcomes for laparoscopic and open approaches to right-sided colon cancers [13,14,15,16]. The non-inferiority of oncologic outcomes, coupled with decreased length of hospital stay, wound complication rates, blood loss, and time to return of work, have led most surgeons to view this as a safe and effective technique for managing right-sided colon cancers.
Care must be taken to assure that the laparoscopic operation accomplishes the same dissection as a laparotomy. Regardless of the pathology or the technical experience of the surgeon, an appropriate oncologic resection must be achieved in the end.
Careful patient selection is important to identify those who are appropriate for a laparoscopic resection. In particular, tumors invading the abdominal wall or other organs can pose significant technical challenges to a laparoscopic resection and may be better suited to a laparotomy. Likewise, perforated tumors with extensive adjacent inflammatory changes present a unique challenge in pursuit of an R0 resection. These patients carry a high risk for peritoneal recurrence and therefore warrant meticulous attention to assure a complete resection [17]. Perforated tumors may also result in sepsis, and the hemodynamic instability may be exacerbated with the creation of CO2 pneumoperitoneum, possibly as a result of decreased venous return from gas compression of the inferior vena cava. Active communication with the anesthesiology team is essential in such cases.
Patients presenting with obstructing right-sided colon cancers may not be amenable to a laparoscopic resection due to poor visualization from dilated bowel if their ileocecal valve is incompetent. These patients are also at high risk for dehydration and benefit from fluid resuscitation prior to operation.
Principles and Quality Benchmarks
The key benchmarks are the oncologic outcomes of patients and the quality of the resection. The tumor must be resected to include at least 5 cm negative margins and the entire lymphovascular drainage system [18]. The arterial supply to the portion of colon containing the tumor should be excised at the takeoff of its feeding vessel.
The importance of total mesorectal excision has been well described for rectal cancer. Extrapolating from this, the concepts of complete mesocolic excision (CME) and central vascular ligation (CVL) have evolved in the treatment of right-sided colon malignancies. For tumors in the cecum and ascending colon, the ileocolic artery (and if present the right colic artery) should be divided at the takeoff from the superior mesenteric artery. While for these tumors the trunk of the middle colic artery does not need to be divided, the right branch of the middle colic artery should be ligated. The colon should be divided at the level of the middle colic artery [19, 20]. This will assure a complete lymphovascular en bloc excision which must achieve a minimum of 12 lymph nodes in the specimen, as the patient’s survival may otherwise be negatively impacted [21]. For more details on this topic, please refer to Chap. 11 on principles of complete mesocolic excision (CME) for colon cancer.
Conversion to an open operation should never be viewed as a complication and should be undertaken whenever the safety or effectiveness of a laparoscopic resection is in doubt. As was noted above, the addition of a hand port may allow for preservation of the minimally invasive advantages while avoiding a conversion to full laparotomy. In a recent meta-analysis, a conversion rate of 2–13% was reported from comparable studies of laparoscopic right hemicolectomy [22]. Individual surgeons should be encouraged to follow their conversion rates and to be cognizant if higher than expected.
Preoperative Planning, Patient Work-Up, and Optimization
Preoperative planning for a laparoscopic right hemicolectomy for malignancy should begin with appropriate staging. This should include a CT scan of the chest, abdomen, and pelvis to ensure that no metastatic disease is present. Complete blood count (CBC), serum chemistry, and carcinoembryonic antigen (CEA) level are also recommended by the National Comprehensive Cancer Network (NCCN) as part of the initial cancer staging [23]. A complete colonoscopy is also recommended, as synchronous lesions are not infrequent and may change the operative plan.
Endoscopic tattooing of the lesion is useful in patients planned for laparoscopic right hemicolectomy. Misidentification of the segment of colon in which a lesion sits occurs around 20% of the time after colonoscopy [24]. As such, it is imperative to assure accurate localization of the involved colon segment prior to resection. Laparoscopic colectomy does not provide much tactile feedback about the colon, and visualization is limited to the serosa. Therefore, a colonoscope should be available in the operating room to permit on-table localization if needed.
A preoperative mechanical bowel preparation with antibiotics has been shown to reduce the incidence of anastomotic leak, surgical site infection, and ileus [25, 26]. Many combinations of antibiotics and mechanical preparation agents exist, though none have yet been reported superior to another. It does seem clear, however, that bowel preparation alone without antibiotics is not sufficient to achieve these improved outcomes [27]. For more details on this topic, please refer to Chaps. 7 and 8 on enhanced recovery protocols in colorectal surgery.
Operative Setup
The patient is placed under general anesthesia, ideally in an OR that is specially equipped for minimally invasive procedures. At least two monitors should be available, one on each side of the patient. A 10-mm laparoscopic camera with a 30-degree optical system is ideal. The patient may be positioned modified-lithotomy or split-leg to facilitate hepatic flexure mobilization from between the legs if needed. The anus needs to remain easily accessible in the event intraoperative endoscopy is required. The patient’s abdomen is disinfected and draped.
Operative Technique: Surgical Steps, Medial-to-Lateral Approach
For an open access, a vertical 1.5-cm midline incision is made near the umbilicus, and the abdominal cavity is opened stepwise using retractors and Kocher clamps. A 12-mm Hasson trocar is inserted. Pneumoperitoneum is created with a pressure of 12-mm Hg. Two 5-mm trocars are placed on the left in the upper and lower quadrants. An additional port on the right may be added to facilitate dissection. A diagnostic laparoscopy is performed for staging purposes to localize the tumor and inspect the entire abdominal cavity for distant metastases.
The patient’s right side is now tilted up and in Trendelenburg position. This way the right colon is exposed. A medial-to-lateral dissection is often easier and strongly recommended. Dissection starts by incising the peritoneum anterior to the right iliac artery and inferior to the terminal ileum to enter both planes of Gerota’s fascia and start dissecting them from each other. This guarantees preservation of the mesocolic plane. The incision should be enlarged medially toward the mesenteric root (Fig. 13.1) and lateral toward the cecum (Fig. 13.2). Careful mobilization is now continued cephalad, laterally and medially to separate both planes of Gerota’s fascia toward the right transverse colon, the hepatic flexure, and the ascending colon and mobilize the duodenum and the pancreatic head posteriorly (Fig. 13.3). This dissection effectively creates a blind-ending retroperitoneal tunnel below the right mesocolon.
Lateral mobilization is now facilitated. This portion of the dissection starts around the cecum and the appendix (Fig. 13.4), and then gradually the lateral suspension of the ascending colon is taken down. Hepatic flexure mobilization is completed by taking down its suspension toward the fatty tissue around the right kidney and the retroperitoneum below the liver. The omentum is gradually taken down until the central transverse colon is reached.
The ileocolic vascular bundle (Fig. 13.5) is exposed by lifting it up laterally close to the cecum. An incision is made medially below it, and a connection is created toward the previously created blind ending located posteriorly. The peritoneum is further incised below the ileocolic vessels toward their origin. The superior mesenteric vein (SMV) is identified and dissected for further central lymph node harvest (Fig. 13.6). The origin of the ileocolic vessels is identified, skeletonized, and divided with the laparoscopic energy device, a laparoscopic stapler or clips. The dissection continues cephalad along the SMV. In a minority of cases, a true right colic artery (Fig. 13.7), originating from the superior mesenteric artery (SMA), is identified and similarly divided. Further central dissection will lead toward the gastrocolic trunk of Henle (Fig. 13.8) where anatomic variations are frequent. In most cases, the right colic vein, superior right colic vein, and right gastroepiploic vein form this trunk, but they may also have separate origins from the SMV. The trunk or the individual veins are sealed and transected centrally. Next, the middle colic vein and artery (Fig. 13.9) are identified. The SMA normally runs posteriorly toward the anatomical left side of the SMV in this region. Central dissection continues along the middle colic vein and artery toward the right branches of both vessels (Fig. 13.10). They are also sealed and transected centrally. The transverse mesocolon may be further transected distally to facilitate mobilization if needed. At this point the central dissection is complete (Fig. 13.11). The bowel is grasped close to the cecum using a laparoscopic bowel grasper. The right ureter stays behind the anterior peritoneal envelope which is never injured or dissected and may be visualized in skinny patients easily.
In laparoscopic right colectomy with extracorporeal anastomosis (ECA) , the camera trocar is removed, and a periumbilical incision is made around the left side of the umbilicus to create a mini-laparotomy. A 4- or 5-cm incision is typically adequate. A wound protector is placed, and the mobilized right colon is exteriorized. Alternative extraction sites would be the right lower abdominal trocar site (transverse incision) or a Pfannenstiel incision which may bear a lower risk of hernias, but both alternatives would demand a more comprehensive mobilization of the transverse colon for optimal reach to create a tension-free anastomosis.
Alternatively, laparoscopic right colectomy can be combined with intracorporeal anastomosis (ICA), which facilitates specimen extraction through a Pfannenstiel incision, since extensive mobilization of the transverse colon and terminal ileum is not needed. For detailed techniques of ECA and ICA during laparoscopic and robotic right colectomy, please refer to the chapters on options for ileocolonic reconstruction (Chap. 14) and robotic right-sided colon resection (Chap. 15), respectively.
The position of the tumor is verified by careful palpation. Mesenteric transection is completed toward the ileum and transverse colon at the sites of planned transection. The bowel is divided using a linear stapler. Photo documentation of the specimen may be performed with a ruler next to it. The central transection areas of the major vessels may be marked using sutures of different colors based on institutional availability. The ileocolic anastomosis is performed with proper orientation of the ileum and colon. The oncologic principles of conventional surgery do not change as the omentum is taken off the right transverse colon in cancers proximally to the hepatic flexure and taken along en bloc with the specimen in tumors of the hepatic flexure and right transverse colon.
Operative Technique: Comparison with Lateral-to-Medial Approach
The technique of creating a retroperitoneal tunnel in the medial-to-lateral approach offers several advantages such as a minimized risk of injury to the retroperitoneal envelope which covers the right ureter and the gonadal vessels. Furthermore, the named arteries are clearly visible posteriorly at their origins, and they may be ligated early, proximally, and safely to minimize the risk of bleeding and keeping the small intestine out of the operative field; an early proximal ligation of the mesenteric vessels (observation of no-touch isolation technique) is achieved. By leaving the lateral attachments of the colon intact until the mesenteric division has been carried out, important natural anatomic countertraction is applied to the bowel as the mesentery and bowel are mobilized. Colectomy is facilitated by leaving the lateral attachments intact, and the described anatomic landmarks are highlighted clearly. Only minimal manipulation of the tumor-bearing colon is needed, as most of the colon mobilization and dissection of the mesentery are accomplished before the cecum and ascending colon are freed from their lateral attachments (no-touch isolation technique).
In a lateral-to-medial approach, the tumor-bearing colon is mobilized first. The lateral dissection is started by elevating the colon on its vascular pedicle, and then both planes of Gerota’s fascia must be entered laterally and dissected apart from each other. The mesenteric and vascular division is the same as in a medial-to-lateral approach with respect to the principles of CME. The vessels are ligated intra- or extracorporeally in a second step; however, it must be ensured that the superior mesenteric vessels and the origins of the mesenteric vessels are clearly identified and divided at their origins. An assistant has to pull on the tumor-bearing bowel to create traction and countertraction for central exposure of the mesentery and avoid the risk of tearing the colon and mesentery. It is important to note that the mobilized colon and small bowel become more difficult to manage laparoscopic surgery relative to open surgery.
Pitfalls and Troubleshooting
For carcinomas of the hepatic flexure and right transverse colon, an extended right hemicolectomy is indicated. The omentum is not dissected off the colon, but the dissection is continued along the lower edge of the duodenum toward the right aspect of the greater curvature of the stomach. The gastrocolic ligament is transected at the left transverse colon. The middle colic vein and artery are dissected and transected centrally at the level of the SMV and SMA to assure a complete lymphovascular resection. The right branches of the middle colic vessels are also divided. In patients where a tension-free anastomosis may be challenging, such as those who are obese, splenic flexure mobilization in combination with further takedown of the omentum may be beneficial as well as a total laparoscopic approach with intraabdominal bowel transection and creation of an intracorporeal ileocolonic anastomosis (ICA) to avoid tension from an extracorporeal approach (ECA).
In obese patients, the landmarks of dissection are more difficult to find, especially the SMV. In such cases, a laparoscopic lateral-to-medial approach may provide improved exposure. In particularly challenging cases, the laparoscopic colon mobilization may be followed by central mesocolic and lymph node dissection in an open technique through a relatively short midline incision.
If the tumor has not been tattooed and cannot be identified at exploration, intraoperative colonoscopy may be necessary. CO2 insufflation should be used to minimize dilatation of the colon that will hinder further laparoscopic dissection. If the tumor cannot be localized laparoscopically or endoscopically, conversion to laparotomy and careful palpation of the colon may be necessary. As pointed out previously, a conversion to a hand-assisted approach can facilitate medial-to-lateral mobilization, especially in reoperative and obese cases.
The most frequently described intraoperative complication is bleeding. In order to avoid any vascular injury which may be hazardous especially with SMV, SMA, and middle colic vessels, a very slow and meticulous dissection technique is imperative. The laparoscopic energy devices and instruments used for dissection should be carefully observed to avoid contact with vessels. Especially in obese patients, the visualization may be difficult, and the threshold for conversion should be kept very low. As explained above, in a medial-to-lateral approach, the risk of injury to adjacent organs is low: duodenal adhesions by small ligaments toward the posterior mesocolon should be taken down cautiously. The same applies to adhesions between the pancreatic head and the mesocolon. In cases of previous pancreatitis with firm adhesions, conversion is recommended. The ureter normally stays safely below the surface of the retroperitoneal envelope; whenever possible it should be visualized.
If against expectations from preoperative staging by CT scans a T4 tumor is found at exploration, conversion to open approach for planned en bloc resection is recommended.
There are no data of the learning curve in oncologic laparoscopic right hemicolectomy. However, when possible, the technique of CME should be mastered first in the context of open surgery to better understand variations in the relevant anatomy. Also, the laparoscopic expertise required to perform these cases should be advanced, and it may be helpful to practice the procedure first in benign cases, especially adenomas. The retroperitoneal tunnel approach has advantages also when applied in Crohn’s disease and may be practiced in such cases first to gain confidence and become familiar with the technique.
Outcomes
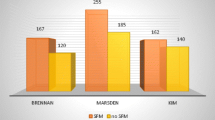
Numerous retrospective studies have shown that a laparoscopic oncologic approach for right colon cancer has results comparable to that of open procedures [28] (Table 13.1). The laparoscopic approach to right hemicolectomy , specifically, has been shown equivalent to the open approach with regard to key oncologic outcome measures. These include the ability to obtain R0 resection with negative resection margins, disease-free and overall survival, lymph node harvest, and incidence of local and systemic recurrence. With experience, some would argue the laparoscopic view provides an advantage over open resection regarding lymph node harvest. With the magnified view provided by the laparoscopic camera, surgical planes can be visualized and dissected with more accuracy and less trauma to surrounding structures.
Conclusions
Laparoscopic right hemicolectomy for malignant disease is a procedure with standardized setup, equipment, and surgical steps leading to short- and long-term results equivalent to open surgery. The principles of high vascular ligation and preservation of the mesocolic planes need to be respected. A low threshold for conversion in challenging cases will keep complication rates low.
References
Lacy AM, García-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM, et al. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359(9325):2224–9.
McCombie AM, Frizelle F, Bagshaw PF, Frampton CM, Hewett PJ, McMurrick PJ, et al. The ALCCaS trial: a randomized controlled trial comparing quality of life following laparoscopic versus open colectomy for colon cancer. Dis Colon Rectum. 2018;61(10):1156–62.
Schlinkert RT. Laparoscopic-assisted right hemicolectomy. Dis Colon Rectum. 1991 Nov;34(11):1030–1.
Jacobs M, Verdeja JC, Goldstein HS. Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc. 1991;1(3):144–50.
Chung CC, Ng DCK, Tsang WWC, Tang WL, Yau KKK, Cheung HYS, et al. Hand-assisted laparoscopic versus open right colectomy: a randomized controlled trial. Ann Surg. 2007;246(5):728–33.
Liang JT, Lai HS, Lee PH. Laparoscopic medial-to-lateral approach for the curative resection of right-sided colon cancer. Ann Surg Oncol. 2007;14(6):1878–9.
Rotholtz NA, Bun ME, Tessio M, Lencinas SM, Laporte M, Aued ML, et al. Laparoscopic colectomy: medial versus lateral approach. Surg Laparosc Endosc. 2009;19(1):43–7.
Remzi FH, Kirat HT, Kaouk JH, Geisler DP. Single-port laparoscopy in colorectal surgery. Color Dis. 2008;10(8):823–6.
Maggiori L, Tuech JJ, Cotte E, Lelong B, Denost Q, Karoui M, et al. Single-incision laparoscopy versus multiport laparoscopy for colonic surgery: a multicenter, double-blinded, randomized controlled trial. Ann Surg. 2018;268(5):740–6.
Park JS, Choi GS, Park SY, Kim HJ, Ryuk JP. Randomized clinical trial of robot-assisted versus standard laparoscopic right colectomy. Br J Surg. 2012;99(9):1219–26.
Akram WM, Al-Natour RH, Albright J, Wu J, Ferraro J, Shanker B-A, et al. A propensity score-matched comparison of intracorporeal and extracorporeal techniques for robotic-assisted right colectomy in an enhanced recovery pathway. The American Journal of Surgery 2018. 2018 Dec;216(6):1095–100.
Vogel JD, Eskicioglu C, Weiser MR, Feingold DL, Steele SR. The American society of colon and rectal surgeons clinical practice guidelines for the treatment of colon cancer. Dis Colon Rectum. 2017;60(10):999–1017.
COST. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350(20):2050–9.
Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW, et al. Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg. 2007;246(4):655–62.
Green BL, Marshall HC, Collinson F, Quirke P, Guillou P, Jayne DG, et al. Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg. 2013;100(1):75–82.
Kuhry E, Schwenk WF, Gaupset R, Romild U, Bonjer HJ. Long-term results of laparoscopic colorectal cancer resection. Cochrane Database Syst Rev. 2008;(2):CD003432.
Asano H, Kojima K, Ogino N, Fukano H, Ohara Y, Shinozuka N. Postoperative recurrence and risk factors of colorectal cancer perforation. Int J Color Dis. 2017;32(3):419–24.
Paquette IM, Varma M, Ternent C, Melton-Meaux G, Rafferty JF, Feingold D, et al. The American Society of Colon and Rectal Surgeons’ clinical practice guideline for the evaluation and management of constipation. Dis Colon Rectum. 2016;59(6):479–92.
Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S. Standardized surgery for colonic cancer: complete mesocolic excision and central ligation – technical notes and outcome. Color Dis. 2009;11(4):354–64.
Kim NK, Kim YW, Han YD, Cho MS, Hur H, Min BS, et al. Complete mesocolic excision and central vascular ligation for colon cancer: principle, anatomy, surgical technique, and outcomes. Surg Oncol. 2016;25(3):252–62.
Chang GJ, Rodriguez-Bigas MA, Skibber JM, Moyer VA. Lymph node evaluation and survival after curative resection of colon cancer: systematic review. J Natl Cancer Inst. 2007;99(6):433–41.
Wang G, Zhou J, Sheng W, Dong M. Hand-assisted laparoscopic surgery versus laparoscopic right colectomy: a meta-analysis. World J Surg Oncol. 2017;15(1):215.
NCCN. NCCN Guidelines Version 3.2018. Colon cancer. Retrieved 1 Oct 2018. From https://www.nccn.org/professionals/physician_gls/pdf/colon.pdf.
Offermans T, Vogelaar FJ, Aquarius M, Janssen-Heijnen MLG, Simons PCG. Preoperative segmental localization of colorectal carcinoma: CT colonography vs. optical colonoscopy. Eur J Surg Oncol. 2017;43(11):2105–11.
Klinger AL, Green H, Monlezun DJ, Beck D, Kann B, Vargas HD. The role of bowel preparation in colorectal surgery. Ann Surg. 2019 Apr;269(4):671–7.
Kiran RP, Murray ACA, Chiuzan C, Estrada D, Forde K. Combined preoperative mechanical bowel preparation with oral antibiotics significantly reduces surgical site infection, anastomotic leak, and ileus after colorectal surgery. Ann Surg. 2015;262(3):416–23.
Koller SE, Bauer KW, Egleston BL, Smith R, Philp MM, Ross HM, et al. Comparative effectiveness and risks of bowel preparation before elective colorectal surgery. Ann Surg. 2018;267(4):734–42.
Ozben V, Aytac E, Atasoy D, Erenler Bayraktar I, Bayraktar O, Sapci I, et al. Totally robotic complete mesocolic excision for right-sided colon cancer. J Robot Surg. 2019 Feb;13(1):107–14.
Siani LM, Lucchi A, Berti P, Garulli G. Laparoscopic complete mesocolic excision with central vascular ligation in 600 right total mesocolectomies: Safety, prognostic factors and oncologic outcome. Am J Surg. 2017;214(2):222–7.
Wu QB, Deng XB, Yang XY, Chen BC, He WB, Hu T, et al. Hand-assisted laparoscopic right hemicolectomy with complete mesocolic excision and central vascular ligation: a novel technique for right colon cancer. Surg Endosc Other Interv Tech. 2017;31(8):3383–90.
Wang Y, Zhang C, Zhang D, Fu Z, Sun Y. Clinical outcome of laparoscopic complete mesocolic excision in the treatment of right colon cancer. World J Surg Oncol. 2017;15(1):1–6.
Huang JL, Wei HB, Fang J, Zheng ZH, Chen TF, Wei B, et al. Comparison of laparoscopic versus open complete mesocolic excision for right colon cancer. Int J Surg. 2015;23:12–7.
Bae SU, Saklani AP, Lim DR, Kim DW, Hur H, Min BS, et al. Laparoscopic-assisted versus open complete mesocolic excision and central vascular ligation for right-sided colon cancer. Ann Surg Oncol. 2014;21(7):2288–94.
Kang J, Kim IK, Kang SI, Sohn SK, Lee KY. Laparoscopic right hemicolectomy with complete mesocolic excision. Surg Endosc Other Interv Tech. 2014;28(9):2747–51.
Adamina M, Manwaring ML, Park K-J, Delaney CP. Laparoscopic complete mesocolic excision for right colon cancer. Surg Endosc. 2012;26(10):2976–80.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Society of American Gastrointestinal and Endoscopic Surgeons (SAGES)
About this chapter
Cite this chapter
Kessler, H., Lipman, J.M. (2020). Laparoscopic Right Colectomy for Malignant Disease. In: Sylla, P., Kaiser, A., Popowich, D. (eds) The SAGES Manual of Colorectal Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-24812-3_13
Download citation
DOI: https://doi.org/10.1007/978-3-030-24812-3_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-24811-6
Online ISBN: 978-3-030-24812-3
eBook Packages: MedicineMedicine (R0)