Abstract
We apply process modeling and simulation to improve surgery planning, through the coordination of operation rooms and intensive care unit (ICU). A case study was carried out in a Brazilian hospital. With the proposed changes, we obtained a 39% reduction in surgery cancelations and a 61% decrease in preoperative length of stay.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
The surgical center (SC) is often the highest cost and revenue department in a hospital and therefore exerts a major impact on the performance of the hospital as a whole [3]. The flow followed by a patient scheduled for an operation involves a number of stages. Each stage requires specific resources, as personnel (such as surgeons, anesthetists and nurses), and specialized equipment and facilities (preoperative facilities, operation rooms, post-anesthesia care units, etc.), which must be synchronized [5]. Blake and Carter [2] note that in addition to resources directly related to the SC, external resources (e.g., the intensive care unit (ICU) and ward beds) must also be scheduled.
Knowing that surgery planning is affected by various factors and involves coordination of resources and activities in uncertain environments, we sought to investigate a planning problem at the operational level involving coordination of the SC with external resources (the ICU) in a Brazilian public hospital. Of note, a surgical center (SC) is composed by a set of operation rooms (OR, also referred in the literature as operating theater); in this article, we use SC and OR as interchangeable terms.
In the literature on OR planning and scheduling, discrete event simulation (DES) is used for many different purposes. At an operational level, it is frequently used to evaluate different ways of allocating and sequencing surgical procedures in ORs [4, 7, 9, 10, 15, 16]. There are also studies on rescheduling, in which the schedule is adjusted on the day of surgery when the schedule is subjected to disruptions. An example is the paper of Allen et al. [1]. Many papers evaluating the utilization of the SC and associated resources can also be found in the literature [6, 17].
Monte Carlo simulation (MCS) is used in, for example, by Lebowitz [8], in which various combinations of short and long surgical procedures are scheduled, and by Paoletti and Marty [13], in which the objective is to calculate the likelihood of an anesthetist being needed simultaneously in two ORs.
While computer simulation has been widely used to analyze various metrics in SC performance, there are few articles that integrate the surgery booking and scheduling process with resources outside the SC. However, the number of papers that integrate booking and scheduling decisions with factors related to ICU resources is very small.
In Brazilian hospitals, most decisions related to bed and SC management are based on tacit knowledge and limited empirical observation, leading to long waiting lists and low service levels. In this article, we use Monte Carlo simulation and discrete event simulation (DES) to identify opportunities for improving the surgery planning process. The aim of the study was to analyze the activities involved in surgical procedures in the hospital, where the main problem is the high surgery cancelation rate.
To this end, we utilize Monte Carlo simulation to identify how better use could be made of beds in the ICU so that bookings would be more in line with the available ICU capacity. Then, we evaluate the proposed changes to the booking process for surgical procedures requiring postoperative admission to the ICU and investigate the impact of the suggested changes on length of stay (LOS) and surgery cancelation rate using DES.
This article is divided into five sections including this one. Section 14.2 describes the problem. Section 14.3 presents the solution framework. Section 14.4 presents the results and discussion, and the conclusions are given in Sect. 14.5.
2 Problem Statement
The case studied is a Brazilian public hospital that was set up to carry out medium- and high-complexity neurologic, vascular and orthopedic surgery. It has a mean capacity of 350 admissions per month. The hospital has wards for each specialty with a total of 145 beds as well as an ICU with 18 beds. There are five ORs. All have different characteristics and are assigned to each specialty according to these.
The main problems mentioned by senior management at the hospital were the high surgery cancelation rate and excessive LOS. Many visits were made to the hospital in order to identify the root cause of the problem mentioned. In these visits, we interview the SC nursing coordinator, the nursing manager and the ICU coordinator; we observe the activities related to the surgery planning process in the hospital; we perform the modeling using BPMN 2.0 (Business Process Model and Notation)—(Object Management Group [11]); and we collect data about patient admissions, operations and internal transfers over one year, data on surgery scheduling, including details of bookings and information about each patient scheduled between April and December 2014, as well as data on the reasons for surgery cancelations between July and December 2014. The data were taken from the hospital electronic medical records (EMRs). The interviews and visits were carried out in the same year of data collection. The situation continues to reflect the reality lived in the hospital because, according to recent contact with senior management, the hospital processes have not yet been changed and the case mix of patients also remains the same.
By the process modeling and data analysis, the main reason for cancelations is a shortage of beds in the ICU, about 57% of the cancelations. Under the hospital’s current policy, surgical procedures requiring postoperative admission to the ICU are scheduled without information about expected patient discharges from the ICU. Consequently, there is a tendency for more bookings for procedures requiring postoperative admission to the ICU to be made than there is capacity for, resulting in a high cancelation rate. To address this issue, we proposed a framework based on MCS and DES that is detailed in the following sections.
3 Solution Framework
Since the major cause of surgery cancelations is the shortage of beds in the ICU, the senior management at the hospital want to know: How many surgical procedures requiring postoperative admission to the ICU should be scheduled per day in order to reduce the number of cancelations?
For this, we used MCS to establish the ideal number of bookings/day requiring postoperative admission to the ICU and we used DES to test the proposed changes to the booking process at the hospital and to evaluate whether it would provide the expected benefits in terms of a reduction in the number of cancelations and a shorter LOS. Figure 14.1 shows how the techniques are used to solve the problem.
It should be stressed that only regular elective cases were considered, as emergency and outpatient cases are rare and have little influence on hospital planning.
3.1 Monte Carlo Simulation
An average of 12 surgical procedures is carried out every day in the hospital studied, but an average of 14 is scheduled. Approximately 50% of the surgical procedures require postoperative admission to the ICU. However, the number of beds available each day at the ICU is not sufficient to meet this demand. This is the main reason why procedures are canceled.
In practice, not all patients for whom the ICU has been recommended will actually need to be admitted to the unit due to other reasons for cancelation, as shown in Table 14.1. There are also some patients for whom the ICU was recommended who do not actually use a bed there because their clinical condition was reassessed during surgery. The data for the ICU are given in Table 14.1.
As said previously, surgical procedures requiring postoperative admission to the ICU are scheduled without information about expected patient discharges from the ICU. Therefore, we carried out an MCS to identify a better surgery booking policy for the hospital and support decision-making regarding the number of bookings requiring postoperative admission to the ICU that should be made each day.
A trade-off was sought between the number of surgery cancelations and the number of empty beds in the ICU, as a large number of surgical procedures requiring postoperative admission to the ICU each day imply a large number of surgery cancelations. However, if there are fewer bookings, there may be empty beds in the ICU and a longer LOS.
Using the historical data, the distributions of the three data series in Table 14.1 were determined. The series correspond to the percentage of patients scheduled for surgery with postoperative admission to the ICU who did not performed the surgery (NR), the percentage of patients who underwent surgery but did not use an ICU bed (RS_ICU) and the number of discharges from the ICU each day (AICU). The chi-square test was used to identify the best-fit distribution for each series, as it can be used for continuous and discrete data [12]. The results indicate that NR has an exponential distribution (0.1), RS_ICU a triangular distribution (0; 0; 0.7) and AICU a binomial distribution (9; 0.4).
Ten experiments were run, each of which corresponded to analysis of a number/day of scheduled surgical procedures requiring postoperative admission to the ICU. For each experiment, 10,000 iterations were performed to guarantee convergence to the expected values. Figure 14.2 shows the logic of the experiments.
3.2 Discrete Event Simulation
The DES model was developed (in Arena Simulation [14]) to identify whether the limit on surgery bookings defined with MCS could reduce the preoperative LOS, measured from the time the patient was admitted to hospital to the time when the operation had been performed. The length of the postoperative stay depends exclusively on clinical aspects and thus is out of scope of our study.
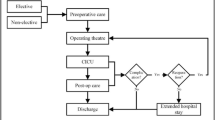
Figure 14.3 shows the flowchart of the simulated surgery planning and scheduling process at the hospital studied in BPMN 2.0. The model has three main parts: (A) arrival of patients for admission and subsequent surgery in the SC, (B) booking surgery and clearing patients for surgery and (C) release of beds in the ICU.
We carried out the initial tests to ensure that the model accurately reflected the situation in the hospital. Based on a number of experiments, it was determined that a 30-day warm-up period and 10 replications would be used to ensure that ward occupancy corresponded to the real starting conditions. Each replication simulated 270 days of operations, similar to the period the real observations were made. The model was validated by comparing the real hospital data with the values of the output variables that had the greatest influence in the study. The simulated data accurately reflect the real data, as the percentage variation is less than 10%. To confirm that the simulated and real data can be considered equivalent, a t-test was used to compare them at a significance level of 95% (α = 0.05). For all the control variables tested, the hypothesis of equivalent means could not be rejected.
4 Numerical Results and Discussion
The results of the MCS experiments are shown in Fig. 14.4. As mentioned previously, there is a trade-off between canceled procedures and empty ICU beds.
Each point on the graph represents the mean number of cancelations/empty beds in the experiments for a given number of simulated bookings per day. For example, for four bookings per day requiring postoperative admission to the ICU, there are 0.7 empty beds and 0.5 cancelations.
If it is more important for the hospital to avoid cancelations, five operations requiring postoperative admission to the ICU should be scheduled, but if avoiding empty beds in the ICU and reducing LOS have greater priority, then six bookings should be made.
Once the DES model had been verified and validated (as discussed in Sect. 14.3.2), the idea of imposing a daily limit on the number of surgical procedures requiring postoperative admission to the ICU could be evaluated. The limit of six surgery bookings per day determined in the Monte Carlo simulation was used in the tests with the DES model and yielded a 61% reduction in the LOS. The results are shown in Table 14.2.
Significant reductions in surgery cancelations were achieved. The most significant reduction (53%) was in cancelations due to a shortage of ICU beds. There was a 14% reduction in cancelations for other reasons and an overall improvement of 39% in surgery cancelations.
As there was a substantial reduction in the number of cancelations and the LOS, more patients can be treated in the hospital. A simulation was therefore run using the proposed policy (a fixed number of six bookings requiring postoperative admission to the ICU) and a higher patient arrival rate. With this policy, the number of scheduled neurologic and orthopedic procedures can be increased by 30% and the number of vascular procedures by 10% while keeping mean surgery waiting time below the actual waiting time observed in the hospital. This corresponds to a potential increase of 19% in the overall number of procedures.
In practice, the solutions identified help solve an important, real problem and can improve quality of service by reducing the LOS and increasing the number of patients treated in the hospital. The results of this study hold promise for healthcare provision in Brazil as users of the public healthcare system face long queues and low service levels because of insufficient use of advanced techniques for decision-making in bed and SC management. The results can therefore be expected to contribute to a general improvement in the Brazilian public health system, as the proposals described here allow hospitals to treat more patients because of the reduced LOS and greater turnover of beds.
5 Conclusions
The study showed that OR planning and scheduling are affected by various factors and involve coordinating a range of resources and performing different activities in an uncertain environment. When coordination of OR planning and scheduling takes into account resources outside the SC, better overall hospital performance can be achieved. Using the solution framework proposed in this study, which is based in Monte Carlo Simulation and Discrete Event Simulation, to establish the number of surgeries requiring postoperative admission to the ICU should be scheduled per day, the hospital expect to achieve 39% of reduction in number of surgery cancellations and 61% of reduction in overall LOS. The use of MSC is important to establish the number of surgeries requiring postoperative admission to the ICU should be scheduled per day DES as it is important to evaluate the impact of this on hospital operation.
Further studies could include an analysis of bed occupancy in the wards, as once the number of patients treated in the hospital increases, beds tend to become a critical resource. Thus, it is possible to evaluate the redistribution of beds in each specialty or identify opportunities to improve the number of wards or ICU beds. In addition, an optimization study to define which patients should be scheduled each day and for each room could also be undertaken to increase OR utilization.
References
Allen, R.W., Taaffe, K.M., Ritchie, G.: Surgery rescheduling using discrete event simulation: a case study. In: Proceedings of the 2014 Winter Simulation Conference. IEEE Computer Society, Savannah, GA, USA (2014)
Blake, J.T., Carter, M.W.: Surgical process scheduling: a structured review. J. Health Syst. 5(3), 17–30 (1997)
Cardoen, B., Demeulemeester, E., Beliën, J.: Operating room planning and scheduling: a literature review. Eur. J. Oper. Res. 201(3), 921–932 (2010)
Fei, H., Meskens, N., El-Darzi, E.: Evaluating alternative surgery plans with discrete event simulation model. In: Workshop on Health Care Management. https://doi.org/10.1109/whcm.2010.5441241 (2012)
Guinet, A., Chaabane, S.: Operating theatre planning. Int. J. Prod. Econ. 85(1), 69–81 (2003)
Harper, P.R.: A framework for operational modelling of hospital resources. Health Care Manag. Sci. 5, 165–173 (2002)
Harper, P.R., Gamlin, H.M.: Reduced outpatient waiting times with improved appointment scheduling: a simulation modelling approach. OR Spectrum 25, 207–222 (2003)
Lebowitz, P.: Schedule the short procedure first to improve or efficiency. AORN J. 78(4), 651–659 (2003)
Marcon, E., Dexter, F.: Impact of surgical sequencing on post anesthesia care unit staffing. Health Care Manag. Sci. 9, 87–98 (2006)
Marcon, E., Dexter, F.: An observational study of surgeons’ sequencing of cases and its impact on postanesthesia care unit and holding area staffing requirements at hospitals. Anesth. Analg. 105, 119–126 (2007)
Object Management Group: Documents associated with Business Process Model and Notation™ (BPMN™): version 2.0. Available at http://www.omg.org/spec/BPMN/2.0/ (2011). Accessed 15 Mar 2015
Palisade: Risk Analysis and Simulation Add-In for Microsoft® Excel. Available at https://www.palisade.com/downloads/manuals/6/EN/RISK6_EN.pdf (2012). Accessed 1 Mar 2016
Paoletti, X., Marty, J.: Consequences of running more operating theatres than anaesthetists to staff them: a stochastic simulation study. Brit. J. Anaesth. 98(4), 462–469 (2007)
Rockwell Automation: Arena® simulation software. Available at https://www.arenasimulation.com/ (2016). Accessed 30 Apr 2016
Sciomachen, A., Tanfani, E., Testi, A.: Simulation models for optimal schedules of operating theatres. Int. J. Simul. 6, 26–34 (2005)
Shultz, J., Claudio, D.: Variability based surgical scheduling: a simulation approach. In: Proceedings of the 2014 Winter Simulation Conference. IEEE Computer Society, Savannah, GA, USA (2014)
Steins, K., Persson, F., Holmer, M.: Increasing utilization in a hospital operating department using simulation modeling. Simulation 86(8–9), 463–480 (2010)
Acknowledgements
This work was supported by the CNPq, CAPES, FAPERJ and PUC-Rio.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this paper
Cite this paper
Marchesi, J.F., Hamacher, S., Cyrino Oliveira, F.L. (2020). Improving Operation Rooms and Planning to Reduce Surgery Cancelations and Inpatient Length of Stay. In: Leiras, A., González-Calderón, C., de Brito Junior, I., Villa, S., Yoshizaki, H. (eds) Operations Management for Social Good. POMS 2018. Springer Proceedings in Business and Economics. Springer, Cham. https://doi.org/10.1007/978-3-030-23816-2_14
Download citation
DOI: https://doi.org/10.1007/978-3-030-23816-2_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-23815-5
Online ISBN: 978-3-030-23816-2
eBook Packages: Economics and FinanceEconomics and Finance (R0)