Abstract
Following the basic principles and basic and advanced protocols, we will provide an overview, with tables, of the role of magnetic resonance spectroscopy (MRS) and the clinical features in which MRS will be used in the clinical management of brain tumors.
For example, MRS could be used before brainstem biopsies for brainstem lesions with mass effect or to differentiate necrotic masses. MRS is also used to predict survival, tumor activity, and early progression. It is used to monitor treatments: chemotherapy (e.g., Temozolomide), new sources of radiation (stereotactic, proton, and Hadron therapy), antiangiogenic and immune therapies, tumoral interventional therapies, and symptomatic treatments.
Important metabolites and ratios that affect clinical management will be explained or presented, such as Choline/Creatine (Cho/Cr) and Choline/N-acetyl aspartate (Cho/NAA), Lactate (Lac), and Lac/Cr, Glucose (Glc), Glutamine (Gln), CH2 Lipids (CH2-Lip), Taurine (Tau), Citrate (Cit), and Alanine (Ala). The importance of analysis of the whole spectral profile is emphasized with the help of multidimensional analysis and artificial intelligence.
Finally, a brief overview and table of practical clinical cases of brain tumor MRS, such as in glioblastomas (GBM), gliomas, metastases, lymphomas, meningiomas, and necrotic tumors, will be presented.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
1.1 Basic Principles
Magnetic resonance spectroscopy (MRS) analyzes the frequency of different atomic groups of molecules. Each atomic group corresponds to a free induction decay signal (FID) in the time domain.
In a molecule as well as in cerebral tissue, several different atomic groups correspond to different FIDs resonating at different frequencies after Fourier transform. Each atomic group, and thus FID, appears as a peak at a particular frequency allowing biochemical characterization. MRS has therefore become a useful analytical and diagnostic tool in biomedicine.
In the past two decades, human localized MRS (single voxel or multivoxel-spectroscopy or spectroscopic imaging) has emerged as an in vivo MR-based spectroscopic approach to translational and clinical research of parenchymal human tissues of interest.
One of the greatest advantages of cerebral MRS techniques is their ability to detect multiple tissue-specific physicochemical metabolites in a single experiment compared to Positron-emission tomography (PET) tracers (with membrane receptor affinity assumptions or hypotheses). The quantitative nature and translational component of in vivo MRS biomarkers come from the spectral and metabolic biomarkers discovered in in vitro/ex vivo and preclinical research studies. For these reasons, these in vivo MRS biomarkers can be easily translated and integrated into noninvasive spectroscopic and cerebral imaging protocols.
Disadvantages of in vivo MRS include low sensitivity, poor spectral resolution due to the inherently wider lines of “in vivo” metabolites, and B0 and B1 inhomogeneities. This will lead to overlapping resonances that are difficult to model and measure very accurately. It also suffers from poor time resolution, therefore offering fewer metabolic biomarkers to be measured and followed in vivo. Other disadvantages of the technique could be the difficulty in integrating all MRS measurements into a clinical protocol because it sometimes is perceived as taking too long.
In this chapter, we will reiterate several known MRS techniques and situations and provide considerations for establishing reliable indications and protocols, metabolite detection, measurement and quantification of in vivo brain tumor MR spectra. We will also explain how these techniques can contribute to diagnosis, follow-up, prediction, and monitoring of brain tumors. In this chapter, we will also present an overview of the role of cerebral MRS and when MRS could be used, and we will provide practical tables and examples of clinical cases of brain tumor spectroscopy.
1.2 Basic Protocol
For 3 T and 1.5 T, perform 1 min of calibration that encompasses the rough setup of the center frequency, then the optimization of the transmit and receiver gains, then the fine setup of center frequency, then the optimization of water suppression, and finally the single voxel MRS acquisition with 2 or 3 Echo Times (TEs):
-
35 ms (with 64 acquisitions for 2min12)
-
144 ms (with 96 acquisitions for 3min00)
-
288 ms (with 128 acquisitions for 3min48) = total 6–10 min
For new 3 T (with more head coil elements and better signal-to-noise ratios):
-
35 ms (with 16 or 32 acquisitions for 32 s or 1min34)
-
144 ms (with 64 acquisitions for 2min10)
-
288 ms (with 96 acquisitions for 3min00) = total 5–7 min
Monovoxel acquisition and processing are fast and relatively easy. However, there is not enough information about the extension and the heterogeneity of the tumor. On the other hand, we can easily quantitate, using monovoxel MRS, the most aggressive part of the tumor, which is most often used along with anatomo-pathology, to predict the prognosis the treatment response and make therapeutic decisions during the neuro-oncologic multidisciplinary staff meeting.
The basic protocol in multivoxel MRS could be Chemical Shift Imaging (CSI) of one slice with 12 × 12 or 16 × 16 phase encoding at TE 144 ms in 3 min with a 1min30 calibration.
Basic and frequent applications are brain tumors, metabolic brain diseases, inflammation and demyelination diseases, intensive care unit and epilepsy patients (cf. Chap. 3).
2 Important Metabolites Affecting Clinical Management
2.1 Metabolites
The main metabolites detected in proton MRS, in brain tumors, are, as you can see in Fig. 5.1, from 0 to 6 ppm: CH3-Lipids (CH3-Lip → 0.9 ppm), CH2-Lipids + Lactate (CH2-Lip + Lac → 1.3 ppm), N-Acetylaspartic Acid (NAA → 2.02 ppm), Glutamate + Glutamine (Glu + Gln → from 2.05 to 2.55 ppm), PolyUnsaturated Fatty Acid (PUFA → 2.8 ppm), CH3-Total Creatine (CH3-tCr → 3.03 ppm), Total Choline (tCho → 3.22 ppm), Taurine (Tau → 3.4 ppm), Myoinositol + Glycine (mI + Gly → 3.56 ppm), Glutamate + Glutamine (Glu + Gln → from 3.6 to 3.9 ppm), CH2-Total Creatine (CH2-tCr → 3.93 ppm), Water (H2O → from 4.5 to 4.9 ppm), Glucose + Lipids (Glc + Lip → 5.24 ppm).
All metabolites are often measured as ratios over Creatine because this is the most stable metabolite in the brain in the most common brain diseases.
2.1.1 Cho/Cr and Cho/NAA
The first ratio to measure is the Choline/Creatine ratio (Cho/Cr), which is estimated at TE = 144 ms [1] (cf. Fig. 5.2). This ratio corresponds to tumor proliferation: the higher the ratio (above 2.5), the more proliferation and the mitotic index (Ki-67) reflecting proliferative activity is elevated [2]. We determine the grade of glioma based primarily on this ratio [3]. The ratio of Cho/NAA also allows us to confirm the tumor grade [1].
Spectrum of a glioblastoma at TE/TR = 35/1500 ms (a) and TE/TR = 144/1500 ms (b) The ratio of Cho/Cr is measured by the neuroradiologist on the TE/TR = 144/1500 ms and correspond to the ratios of areas under the resonances of Choline (3.22 ppm) and Creatine (3.03 ppm). Here, the Cho/Cr ratio is a little above 2
2.1.2 Lactate and Lac/Cr
The presence of lactate in a tumor lesion gives us information about the aggressiveness of the tumor. Its presence in large quantities can sometimes differentiate a lymphoma from a GBM and a transition to a higher grade of a glioma [4].
The detection of lactate is particular because its resonance frequency is located at the same frequency position as a part of necrotic CH2 phospholipids (1.3 ppm). For this, several TEs are needed as shown in Fig. 5.3: a TE at 35 ms to detect the presence of lactate and lipids, both at 1.3 ppm, at TE = 144 ms: if the 1.3 ppm signal goes negative, then there is more lactate than necrotic CH2 phospholipids. The concentration can be estimated at TE = 288 ms [5]. We should be cautious on 3 T MRS because the lactate detection is decreased at TE = 144 ms [5, 6]. Its concentration is therefore underestimated because of the chemical shift error and the PRESS sequence. We should thus use a third TE at 288 ms.
A multi-TE study (TE = 35, 144, 288 and 432 ms) can, in some cases, help with the quantification of lactate and the differentiation between Lipids and lactate. If at TE = 144 ms the lactate doublet appears (a), it means that the lactate is predominant in the Volume of Interest (VOI). If it does not appear, it is that the resonances are of the same intensity (b). If, on the contrary, the resonance remains positive, it is that the lipids are still predominant (c)
It is important, especially in low-grade gliomas, to associate Cho/Cr and Lac/Cr. When the glycolytic metabolism (Lac/Cr) is increased (>12 Mmol as in Fig. 5.3), it is a sign that a glioma transformation has resulted in a high-grade glioma, even though there is limited proliferation and almost no contrast enhancement.
2.1.3 Glucose
The amount of glucose [7] in a tumor is usually related to lactate [8].
2.1.4 Glutamine
The glutaminergic complex also confirms the aggressiveness of a tumor [9]. Its detection and measurement without processing software is more complex for distinguishing difference between glutamate and glutamine in particular [10] because of the overlapping resonances. They are added most of the time, but it is possible to differentiate them. The most useful energetic proton tumor biomarker for detection is glutamine, which is closer to CH2 creatine (while glutamate is closer to the higher mI resonance at 3.56 ppm). Glutamine shows the metabolic activity of the tumors and is predictive of future proliferation [11].
2.1.5 CH2-Lipids
CH2 phospholipids are not present in substantial quantity in the normal human brain. The presence of lipids and the amount of CH2-Phospholipids (1.3 ppm) tells us about several elements. Before treatment initiation, they allow us to estimate the grade of the tumor. The higher they are, the higher the grade is. After treatment has been started, if the ratios detected are significantly different, they can indicate the effectiveness of the treatment [12] in producing necrosis [13].
2.1.6 Taurine
The Glucose/Taurine peaks (3.40 ppm), positioned to the left of Choline (3.22 ppm), can also indicate tumor grade [14].
2.1.7 Citrate
Citrate can be found in aggressive pediatric glial tumors [15] and active glioblastomas as in Fig. 5.4 below, and can be correlated to citrate synthase activity.
2.1.8 Alanine
When alanine is detected at 1.47 ppm in cerebral tumors, we should suspect meningioma [16].
2.1.9 Miscellaneous
Polyamines (between creatine and choline at 35 ms) could help to follow embolization and therapies of some GBM.
Myoinositol (at 35 ms) and glycine (at 35 and 144 ms) at around 3.56 ppm are elevated in glial tumors.
Polyunsaturated fatty acids (PUFA) at 2.8 ppm could be detected [17].
2.2 Etiologies
Table 5.1 below is giving a brief overview of main metabolites and ratios in main etiologies of brain tumors. It is sometimes important to consider spectral frequency resonances of metastases that could be detected in tumors, necrosis, and edema. This may suggest etiologic types of metastasis, or when the scale of the intensity changes, could give us information on the distribution. In the future, pharmacokinetics of some concentrated therapies such as Solumedrol, Diprivan, or antiepileptics could be followed.
2.3 Importance of Analysis of the Whole Spectral Profile
All of these ratios can be analyzed together (by multidimensional analysis with main compound analysis (MCA), correspondence factorial analysis (CFA) with discriminant analysis, or hierarchical classification), increasing the discriminative power of MRS. Performing multiple TEs at different sites of the tumor and brain allows for better differentiation of coupled spins from noise. It also allows the collection of as much relevant information as possible from tumoral processes, differential diagnoses, and treatment responses (included in contralateral normal appearing brain). Artificial intelligence and neuronal networks as well as deep learning could, of course, be helpful after evaluation and validation of a sufficient number of relevant and well-labeled data.
3 Role of MRS in Clinical Management of Brain Tumors
MRS provides additional quantitative information about the aggressive part of the tumor and the different pathological processes, acquired within a regular MR examination in 3–5 min.
MRS facilitates additional metabolic analysis far more inexpensively and quickly than PET, with physicochemical measurements, independent of the affinity of the receptor, and in real time (and with membrane changes). MRS is sometimes diagnostic, particularly for necrotic masses and for distinguishing tumoral from infectious processes, notably bacterial infection. For other tumoral conditions, and after registration, association with morphologic MRI 3D sequences, perfusion, and different PET tracers are always informative.
Once the tumoral process is confirmed (Cho/Cr >3), MRS used along with MRI increases the likelihood of detecting malignant tumors in some cases. It could help to measure the spectral and metabolic treatment response in vivo and monitor some highly concentrated treatments. In the future, monitoring biomarkers for responses to treatment could be possible. These biomarkers and their combinations could allow us to predict early survival (if the patient is still alive at 6, 8, or 10 months after relapse) and to predict the response to costly therapies such as antiangiogenics. It is particularly useful when contrast enhancement and hyperperfusion disappear while proliferation continues [18] or with anti-hypoxia or antimetabolite therapies. It could be possible to follow therapies in real time and monitor metabolic pharmacology [19].
MRS, which detects tumoral processes (Cho/Cr >3), allows early detection of brain tumors, the extension of their progression, and their boundaries, in CSI or multivoxel for glial tumors and their relapses under treatment, MRS can detect early response to specific treatments and their combinations (e.g., costly antiangiogenics, signaling pathway inhibitors, and new sources of radiation). Therefore, this technique is able to change the monitoring and treatment combinations used in brain tumor patients. MRS techniques and sequences should be adapted to the clinical question: Is there a malignant or benign tumor process? What is the extension assessment and stage? How is the tumor lesion progressing under therapy (degree of proliferation, necrosis, glycolytic, and glutamatergic metabolism)?
In metastasis, MRS will help to first differentiate multiple lesions, MS lesions, or vascular lesions from metastasis, then with more difficulty from some infectious diseases. In cases of unique necrotic masses, as we will see below, MRS helps to differentiate metastasis from abscess and GBM. In addition, in some cases it could help to evaluate or monitor treatment effectiveness, e.g., Solumedrol effectiveness.
Moreover, MRS is useful for better understanding and following the physiopathology of brain tumors and the different pathological processes that occur over time, particularly in treatment responses. Indeed, the volumetric response criteria (RECIST, RANO) are often not sufficient although they are used in clinical research protocols because they are more reproducible and quantifiable than clinical criteria. More sensitive, discriminant, and informative (regarding the pathological processes) measurements, such as multidimensional analysis of the different spectroscopic ratios and spectral profiles and their combinations over time, are needed. Artificial intelligence, neuronal networks, and deep learning could naturally be helpful after evaluation and validation of enough relevant and well-labeled data.
4 Clinical Features in Which MRS Will Be Used for Clinical Management
4.1 MRS Before Brainstem Biopsies of Brainstem Lesions with Mass Effect
Spectroscopy with perfusion and diffusion first helps to rule out differential diagnoses of brain tumor processes such as infectious, inflammatory, granulomatous, or autoimmune diseases [20].
Among brainstem tumors, we can justify differentiating between lymphomas, metastases, and necrotic or non-necrotic lesions, with increased CH2 phospholipids. Spectroscopy could subsequently predict the grade and the progression as well as short-term survival of the patients, followed by the differentiation between low-grade and high-grade gliomas.
4.2 Differentiation of Necrotic Masses
Diffusion and spectroscopy (with acetate, valine, leucine, isoleucine, and succinate) will confirm the diagnosis of abscesses with an accuracy rate of more than 99% [21, 22].
In non-treated necrotic masses, spectroscopy results with a CH2 phospholipids to creatine ratio >15 and a Cho/Cr ratio <3, in metastasis can help to differentiate them from glioblastomas.
Spectroscopy showing the amount of lactate, CH2 phospholipids and the value of Cho/Cr and mI/Cr, could help to differentiate GBM from lymphomas, especially when there is involvement of the corpus callosum in both cases.
4.3 Prediction of Survival, Tumor Activity, Early Progression, and Treatment Response
Usually, in cancer, four kinds of responses are used to evaluate treatment efficacy: complete and partial response, stability, and progression. To be classified into one of these responses, size comparisons using previous exams are done.
Two imaging exams are often used: the initial exam (baseline, before treatment) and the NADIR (the imaging exam in which the patient achieved the best treatment response). If the size increases by more than 20% compared to the NADIR, we classify it into “tumor progression,” which often leads to a treatment change. In the same way, spectroscopy criteria could be set up and optimized to define best tumoral progression. For example, comparisons between two exams, or between the last exam and the initial or first one after treatment or the NADIR. Thus, these criteria are easier for proliferation and glycolytic metabolites, but more difficult for glutamine and other metabolites. To find MRS differences between necrosis and apoptosis in a clinical setting is still very challenging.
The complete response in spectroscopy is not seen often because the different tumoral pathological processes do not disappear quickly and easily. In contrast, we can see various combinations of changes, therefore the tumoral stability is difficult to define and the partial response needs further MRS/MRI studies and evaluations.
Within heterogeneous glial tumors, we can try to define target(s) such as the most aggressive parts of the tumor that could be good target(s) for localizing therapies such as stereotaxic radiation, boost radiation, or intra-tumoral therapy delivery. MRS in GBM and in metastasis could be predictive of volumetric changes.
Segmentation in the VOI to obtain a percentage of gray/white matter and the different tumoral compartments is useful in multivoxel and in monovoxel as well, allowing the correction of certain effects of the partial volume effect.
Any sign of spectral, or metabolic, progression needs to be thoroughly evaluated when there is no proliferation and when there is a combination of spectral changes. As mentioned before, it could be useful to study the relationship between the volume of necrosis in post-gadolinium T1-weighted imaging and the CH2 necrotic phospholipids to creatine ratio.
4.3.1 Chemotherapy (Temozolomide)
It is possible to detect Temozolomide (TMZ) in vitro and, in some cases, in vivo during glioma and GBM chemotherapy [23].
4.3.2 New Sources of Radiation
MRS could help to monitor stereotaxic, proton and Hadron therapy and to detect proliferation and relapse from radio-necrosis or pseudo-progression, or tissular antioxidant level [24].
4.3.3 Antiangiogenic Therapy
Some tumors, such as GBM, after genomic analysis with functional assays for identifying patients specific targetable alterations [25], can respond well to antiangiogenic therapy, with disappearance of hyper-perfusion and contrast enhancement. However, the glycolytic metabolism and proliferation persist [18]. Some other GBM have nevertheless shown decreased neo-angiogenesis (with disappearance of contrast enhancement and hyper-perfusion). They have, however, increased in size, mostly due to necrosis (in T1-weighted imaging post-gadolinium), and are confirmed by a markedly increased quantity of CH2 necrotic phospholipids without proliferation or glycolytic metabolism.
4.3.4 Immunotherapy: Detection of Inflammation and Immune Response
MRS, in some cases, can detect inflammation and immuno-response secondary to immunotherapy.
4.4 Interventional Therapeutic Monitoring of Tumors
Biopsies could be studied with HR-MAS. Tumoral ablation could be studied by thermo or cryoablation, focus ultrasound, or lasers, and could be monitor by spectroscopy.
Embolization in tumors such as meningiomas [16] could be monitored by MRS to follow experimental ischemia, embolization agents, metabolism changes, and glial tumor follow-up with glucose and polyamine. MRS could help to follow venous perfusion of medication, intra-arterial or intra-tumoral chemotherapy, or therapy delivery such as microbubbles and nanoparticles under ultrasound, laser, or radiation.
4.5 Symptomatic Treatment
MRS could detect and measure in vitro and in vivo symptomatic treatments such as antiepileptics, antibiotics, mannitol, steroids (Solumedrol), and Diprivan.
4.6 Summary of Clinical Features of Brain Tumors Pathologies for Which MRS Is Useful
Table 5.2 below is giving a summary of the main clinical features of brain tumors pathologies with metabolic changes for which MRS is useful.
5 Brief Overview of Practical Clinical Cases: Examples of Brain Tumor MRS
For each pathology, a brief summary of the usefulness of MRS with examples are reviewed. Then, necrotic tumors and differential diagnosis of brain tumors will be discussed.
5.1 Glioblastoma
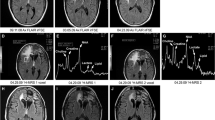
The usefulness of conventional, advanced MR imaging and MRS become clear when the biopsies are negative as in these two cases (Figs. 5.5 and 5.6).
MRI and MRS of a glioblastoma secondary to a glial tumor, with a negative biopsy and no proliferation T2 FLAIR (a) with infiltration, no proliferation (TE/TR = 144/2500 ms (c)), Glutamine and glycolytic metabolism (MRS TE/TR = 35/1500 ms (b)) Glucose - Taurine resonances can be seen around 3.4 ppm. If the glucose peak appears at 5.24 ppm, glucose is predominant
The study of the agreement with anatomo-pathology features is also essential (Fig. 5.7).
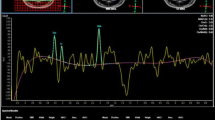
It would be useful to do a longitudinal spectral variation follow-up to predict survival, progression, and proliferation (Fig. 5.8), glycolytic (Fig. 5.9) metabolism, and treatment monitoring.
Usefulness of separation of short responders from long responders (Fig. 5.10).
MRS of short responder patient with glioblastoma with high metabolic activity (higher proliferation, higher lactate and glutamine) at TE/TR = 35/1500 ms (a); TE/TR = 144/1500 ms (b); TE/TR = 288/1500 ms (c) Compared to GBM long responder patient TE/TR = 35/1500 ms (d) and TE/TR = 144/1500 ms (e) without proliferation or high lactate
5.2 Low- and High-Grade Gliomas
Usefulness of perfusion and spectral profiles in predicting progression or improvement, particularly in low-grade and diffuse infiltrative gliomas (Fig. 5.11).
5.3 Metastasis
MRI and MRS are useful for differential diagnosis of multiple lesions (number and size), edema assessment (Fig. 5.12), for treatment, prognosis prediction, and sometimes type of the metastasis.
5.4 Lymphoma
Lymphoma (Fig. 5.13) is a differential diagnosis from gliomas [26]. Lymphoma can also be differentiated from toxoplasmosis (Fig. 5.14).
5.5 Meningioma
MRS is helpful in the diagnosis of meningioma by showing the presence of alanine and sometimes very low Cr (Fig. 5.15). There are at least five meningioma spectra profile types showing different metabolic activity [16]. MRS could also be useful in following treatment (embolization, surgery, and/or radiation).
5.6 Necrotic Tumors
In front of necrotic tumors MRS could be very useful to distinguish abscesses from metastasis and GBM.
5.6.1 Abscess
Together with diffusion imaging, MRS with branched amino acid, acetate, and succinate (Fig. 5.16) helps to recognize bacterial abscess.
ADC (a) and diffusion imaging (b), MRS from a necrotic bacterial abscess (TE/TR = 35/1500 ms (c); TE/TR = 144/1500 ms (d); TE/TR = 288/1500 ms (e)) and normal spectra from a healthy control subject (f). The abscess spectra are not normal. Very high resonances of acetate, lactate, and branched amino acids (leucine, isoleucine, and valine) that are coupled (positive at TE = 35 ms (c), negative at TE = 144 ms (d) and again positive at TE = 288 ms (e) are seen. Acetate and branched amino acids specific for bacterial abscesses are seen. In addition, the elevated succinate resonance seen here are indicative of anaerobic bacteria
5.6.2 Metastasis
MRS shows usually a very high quantity of necrotic CH2-Phospholipids (Fig. 5.17).
5.6.3 Glioblastoma
MRS from GBM shows usually high proliferation and relatively low CH2-Phospholipids before treatment (Fig. 5.18).
5.7 Summary of Main Metabolite Ratios Variations
Table 5.3 shows the summary of the main metabolite ratios variations found for the most frequently encountered brain tumors.
References
Weybright P, et al. Differentiation between brain tumor recurrence and radiation injury using MR spectroscopy. AJR Am J Roentgenol. 2005;185(6):1471–6.
Herminghaus S, et al. Increased choline levels coincide with enhanced proliferative activity of human neuroepithelial brain tumors. NMR Biomed. 2002;15(6):385–92.
Ott D, et al. Human brain tumors: assessment with in vivo proton MR spectroscopy. Radiology. 1993;186(3):745–52.
Bruhn H, et al. Noninvasive differentiation of tumors with use of localized H-1MR spectroscopy in vivo: initial experience in patients with cerebral tumors. Radiology. 1989;172(2):541–8.
Yablonskiy DA, et al. Homonuclear J coupling effects in volume localized NMR spectroscopy: pitfalls and solutions. Magn Reson Med. 1998;39(2):169–78.
Lange T, et al. Pitfalls in lactate measurements at 3T. AJNR Am J Neuroradiol. 2006;27(4):895–901.
Griffin JL, et al. Metabolic profiles of cancer cells. Nat Rev Cancer. 2004;4(7):551–61.
Pfeuffer J, et al. Extracellular-intracellular distribution of glucose and lactate in the rat brain assessed non-invasively by diffusion-weighted 1H nuclearmagnetic resonance spectroscopy in vivo. J Cereb Blood Flow Metab. 2000;20(4):736–46.
Fan G, et al. In vivo single-voxel proton MR spectroscopy in the differentiation of high-grade gliomas and solitary metastases. Clin Radiol. 2004;59(1):77–85.
Michaelis T, et al. On the identification of cerebral metabolites in localized 1H NMR spectra of human brain in vivo. NMR Biomed. 1991;4(2):90–8.
Constans JM, et al. Importance of early spectral variations during 61 months of longitudinal follow MRI and MRS in 100 patients treated glioblastomes. In: ISMRM. 2018.
Hakumäki JM, et al. 1H-MRS detects poly unsaturated fatty acid accumulation during gene therapy of glioma: implications for the in vivo detection of apoptosis. Nat Med. 1999;5(11):1323–7.
Lehtimäki KK, et al. Metabolite changes in BT4C rat gliomas undergoing ganciclovir-thymidine kinase gene therapy-induced programmed cell death as studied by 1H NMR spectroscopy in vivo, ex vivo, and in vitro. J Biol Chem. 2003;278(46):45915–23. Epub 2003 Sept 3.
Kovanlikaya A, et al. Untreated pediatric primitive neuroectodermal tumor in vivo: quantitation of taurine with MR spectroscopy. Radiology. 2005;236(3):1020–5.
Blüml S, et al. Elevated citrate in pediatric astrocytomas with malignant progression. Neuro-Oncology. 2011;13(10):1107–17. Epub 2011 Jul 19. https://doi.org/10.1093/neuonc/nor087.
Constans JM, et al. 1H MRS of meningiomas before and after embolization. J Neuroradiol. 2002;29(HS 1):157–8.
Arias-Ramos N, et al. Metabolomics of therapy response in preclinical glioblastoma: a multi-slice MRSI-based volumetric analysis for noninvasive assessment of temozolomide treatment. Metabolites. 2017;7(2):E20. https://doi.org/10.3390/metabo7020020.
Constans JM, et al. Five-year longitudinal MRI follow-up and 1H single voxel MRS in 14 patients with gliomatosis treated with temodal, radiotherapy and antiangiogenic therapy. Neuroradiol J. 2011;24(3):401–14.
Tafreshi NK, et al. Carbonic anhydrase IX as an imaging and therapeutic target for tumors and metastases. Subcell Biochem. 2014;75:221–54.
Duran A, et al. P07.02 Diagnostic pitfalls in brainstem lesions mimicking gliomas in adults. Neuro-Oncology. 2016;18(Suppl 4):iv33–4.
Mishra AM, et al. Role of diffusion-weighted imaging and in vivo proton magnetic resonance spectroscopy in the differential diagnosis of ring-enhancing intracranial cystic mass lesions. J Comput Assist Tomogr. 2004;28(4):540–7.
Hanafi R, et al. Variations spectrales et IRM aident à différencier métastases et abcès dans les processus expansifs cérébraux nécrotiques. In: SFNR 2017 congres.
Delgado-Goñi T, et al. Molecular imaging coupled to pattern recognition distinguishes response to temozolomide in preclinical glioblastoma. NMR Biomed. 2014;27(11):1333–45. Epub 2014 Sept 10. https://doi.org/10.1002/nbm.3194.
Constans JM, et al. Effects of reactive oxygen species on metabolism monitored by longitudinal 1H single voxel MRS follow-up in patients with mitochondrial disease or cerebral tumors. J Phys Conf Ser. 2011;261:012011.
Loriguet L, et al. Combining genomic analyses with tumour-derived slice cultures for the characterization of an EGFR-activating kinase mutation in a case of glioblastoma. BMC Cancer. 2018;18(1):964. https://doi.org/10.1186/s12885-018-4873-9.
Hakumäki JM, et al. 1H MRS detects polyunsaturated fatty acid accumulation during gene therapy of glioma: implications for the in vivo detection of apoptosis. Nat Med. 1999;5(11):1323–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Heintz, A., Constans, JM. (2020). Role of Magnetic Resonance Spectroscopy in Clinical Management of Brain Tumors. In: Özsunar, Y., Şenol, U. (eds) Atlas of Clinical Cases on Brain Tumor Imaging. Springer, Cham. https://doi.org/10.1007/978-3-030-23273-3_5
Download citation
DOI: https://doi.org/10.1007/978-3-030-23273-3_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-23272-6
Online ISBN: 978-3-030-23273-3
eBook Packages: MedicineMedicine (R0)