Abstract
Poor ovarian response has been a challenging problem during controlled ovarian stimulation for in vitro fertilization. Microdose flare gonadotropin agonist protocol used to be the mainstay for these patients until gonadotropin releasing hormone antagonists became available, and there was debate as to which protocol was better. In the past decade, many new and fascinatingly innovative ideas have been proposed and tried on these patients with no protocol emerging as the most effective. In this chapter, we will review the evidence for the efficacy of the conventional IVF protocols and examine the role of gonadotropin dose, adjuvants, double trigger, follicular flushing, and freezing all embryos in adding to the success rate.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Poor responders
- Gonadotropin dose
- Adjuvants
- Growth hormone
- DHEA
- Testosterone
- Double trigger
- Follicular flushing
- Freezing all embryos
1 Introduction
A substantial number of women (10–24%) undergoing controlled ovarian stimulation (COS) for in vitro fertilization (IVF) do not respond well and may have very few oocytes retrieved or have the cycle cancelled [1]. These women have been collectively called “poor responders,” and considerable energy has been devoted to finding a suitable way to stimulate their ovaries to achieve the ultimate goal of live birth.
At least 75 randomized controlled trials have been published on poor responders to COS leading up to IVF cycles. Despite this, no clear consensus has materialized on the appropriate stimulation protocol to achieve success in these women [2]. Numerous problems have been identified with these trials including lack of uniform definition of poor responders and lack of blinding of patients and/or staff. ESHRE came up with the Bologna criteria to define poor ovarian response (POR) to alleviate this problem as discussed in Chaps. 1 and 4 of this book. These criteria have been shown to predict poor ovarian response in women aged <40. Regardless of the prediction, women over the age of 40 had poor response uniformly [3].
Historically, there were three protocols for COS leading to IVF: long agonist protocol, microdose agonist flare protocol, and the antagonist protocol. In the last decade, numerous other innovative protocols have been introduced in the hope of obtaining a better response in women with POR. As a result, the original three protocols have been called “conventional stimulation protocols.” Conventional IVF is defined by the American Society for Reproductive Medicine as “COS with exogenous gonadotropins to induce multiple oocyte development for retrieval” [4]. The purpose of this chapter is to review the various strategies that have been examined to optimize the conventional protocols to elicit the best ovarian response in women with expected poor ovarian response or known poor responders.
2 Conventional Stimulation Protocols
As physicians taking care of women desiring to achieve a pregnancy, we are eternal optimists. We refuse to give up hope that our patients cannot have biological children of their own – the very existence of IVF today is testament to that hope and tireless struggle! It is therefore not surprising that faced with poor response to COS, we are constantly engaged in finding a better protocol which would achieve a live birth for our patients [5,6,7]. Despite our best intentions, we have come to realize that quality evidence is still lacking for robust recommendations of any of the described protocols to date [1, 8]. Lack of perfect evidence notwithstanding, it is clear that a good number of these POR women will ultimately achieve a successful pregnancy using one or many of the described protocols [9,10,11,12,13,14,15,16].
In a study of 1152 women, the live birth rate was 23.8% in women meeting the Bologna criteria for POR [9]. In the same study, the cumulative birth rate was 18.6% in women with <3 eggs retrieved compared with 44% if they had >3 eggs retrieved. Other studies have confirmed that although the success rate is as expected, low, it is not nonexistent and the live birth rates range from 9.9% to 20.5% [10, 11].
The three stimulation protocols that fall under the definition of “conventional IVF protocols” are well described and will be briefly reviewed here for the sake of completion. All three protocols may be preceded by a few weeks of oral contraceptive pills intake. This is usually for ease of starting the gonadotropin releasing hormone agonist (GnRHa, usually leuprolide) at a convenient time prior to commencing the stimulation cycle. The long agonist (LA) protocol consists of 10 to 14 days of pituitary downregulation using GnRHa followed by about 10 days of stimulation using gonadotropin with a combination of pelvic ultrasound and serum hormone monitoring ultimately culminating in release of oocytes using human chorionic gonadotropin (Fig. 8.1). The microdose flare (MDF) protocol consists of using microdose quantities of GnRHa to stimulate and at the same time downregulate the pituitary while exogenously stimulating the ovary with gonadotropins. The idea is to augment the stimulation of ovary using exogenous and endogenous follicle stimulating hormone (FSH) (Fig. 8.2). The antagonist (ANT) protocol differs in that the ovary is stimulated using exogenous gonadotropins without any downregulation of the pituitary. Approximately 5 days into the stimulation, the antagonist is started to prevent the LH surge while the ovary continues to be stimulated. The idea is to stimulate the ovary using endogenous and exogenous gonadotropins in the first half of the cycle before downregulating the pituitary in the latter half of the cycle (Fig. 8.3).
In the following text, the various factors within an individual protocol that can affect cycle response in patients with POR will be reviewed such as FSH dose, use of augmentation agents growth hormone (GH), dehydroepiandrosterone (DHEA) and testosterone, dual trigger, follicular flushing, freezing all the embryos for later transfer, progesterone supplementation, conversion to IUI as a strategy, comparison of the conventional protocols against each other, followed finally by comparison of the conventional protocols with newer protocols.
2.1 Dose of Gonadotropins
A randomized controlled trial (RCT) of 308 patients used AMH levels to individualize the FSH dosing for patients using the LA protocol. In fact, the study showed that cycles using AMH to dose were more likely to yield <5 oocytes compared to the other arm (25.7% vs 11%) [17].
A systematic review including seven RCTs concluded that more trials are needed to prove or disprove a benefit for individualized dosing of FSH in women with POR [18].
A recent Cochrane Review included 20 trials and concluded that lack of blinding, severe heterogeneity of the trials, and poor-to-moderate quality of the studies hampered firm conclusions, but dosing differences were unlikely to be of clinical benefit in increasing the live birth in women with POR [19].
On the contrary, a retrospective review of 1394 treatment cycles concluded that increasing the daily dose of FSH to >450 units is unlikely to be of benefit and is more likely to do harm [20]. A similar conclusion was arrived at by two other sets of investigators using MDF protocol and comparing 450 units with 600 units of FSH daily [21, 22].
2.2 Augmentation Agents
2.2.1 Growth Hormone
Many studies have been published regarding the use of GH to improve pregnancy rate in POR as also discussed extensively in Chap. 5. Almost all of them have study design problems including insufficient numbers and inconsistent definition of POR. A few studies are worth reviewing; however, and not surprisingly, they provide conflicting results. An open randomized trial using LA protocol included 240 women who fit the Bologna criteria. There was no difference in the live birth rate between the two groups [23]. In contrast, a meta-analysis of 16 eligible studies, including 663 patients, showed a significant difference in live birth rate (RR 1.73) with use of GH [24]. In direct contrast, a meta-analysis of 6 RCTs and 5 controlled clinical trials including 3788 patients concluded that there was no difference in pregnancy rates [25].
Another open-label, randomized trial included 287 patients and randomized them to 3 arms comparing the 3 conventional stimulation protocols with augmentation using GH. There was no statistically significant difference in pregnancy rates between the three groups [26].
2.2.2 Testosterone
Studies using testosterone as an adjuvant in POR patients are beset with the same problems as other studies in POR also echoed in Chap. 5. There are many studies proving a lack of efficacy as there are showing benefit [27,28,29]. A meta-analysis of 3 RCTs with 221 subjects showed a twofold increase in LBR (RR 2.01). The duration of treatment with testosterone may hold the key to success according to one study that compared different duration of exposure to testosterone ranging from 2 weeks to 4 weeks. The maximum benefit was seen in women who had used testosterone for at least 4 weeks [28].
2.2.3 DHEA
DHEA has probably been studied the most as an adjuvant agent for patients with POR and almost all studies are small with heterogeneity in the study population. As is the case with other adjuvants, many studies seem to show a benefit, and a similar number of studies don’t show any benefit. Nevertheless, a 2015 Cochrane Review included 17 RCT with 1496 subjects and concluded that pretreatment with DHEA or testosterone may improve the live birth rates in poor responder patients [30].
2.2.4 Double Trigger
The idea behind the double trigger is to ensure ovulation by giving the injection at staggered times before the retrieval (GnRHa at 40 hours and hCG at 34 hours prior to retrieval) [31]. In a small pilot study, double trigger was compared with GnRHa alone or hCG alone. A higher number of top-quality embryos were noticed in the double-trigger arm compared with the other two arms. More studies are needed to confirm if this translated into more live births [32].
2.3 Follicular Flushing with Conventional Stimulation
Follicular flushing has been advocated as a strategy in normal responders and proven to be ineffective [33]. Each follicle is flushed three times with 2 mL of culture medium using a double lumen needle [34]. In the first RCT in POR patients, 50 women were randomized to have direct aspiration or follicular flushing. The average number of oocytes retrieved was four in the direct aspiration group and three in the follicular flushing group. Significantly, a lower pregnancy rate of 4 vs 36% was observed [33]. In another RCT, 80 patients were randomized, and similar live birth rates (25 vs 22.5%) were observed [34]. Similarly, another RCT recruited 80 patients and did not show any difference between the 2 groups for birth rate. Both the above trials showed a significant doubling of procedure time, however [35].
2.4 Freezing All Embryos After Conventional Stimulation
The optimal embryo transfer (ET) strategy was studied retrospectively in 2263 women undergoing IVF; 879 women fit the criteria for POR, and 645 had day 2 or cleavage stage transfer while remaining 234 had blastocyst transfer. Of the latter group, 59 had fresh transfer, and 87 had frozen embryo transfer. The cycle cancellation was lowest in the women who had day 2 or cleavage stage transfers, but the live birth rate per ET (LBR/ET) was also the lowest. Whereas the former group had an LBR/ET of 21.5%, the blastocyst transfer group had an LBR/ET of 41.1%. Among those, the LBR/ET was 30.5% and 40.2% for fresh transfer and frozen transfers (FET), respectively [36].
Another retrospective study reviewed 433 women with POR. Two hundred and seventy-seven women underwent fresh transfer, and 156 had FET. The clinical pregnancy rate was not different between the two groups (14.1 vs 13.7%) [37]. Another retrospective study included 559 patients with POR and failed to show a significant difference between the fresh transfer and FET groups [38].
2.5 Conversion to Intrauterine Insemination
A multicenter retrospective study looked into the strategy of cycle cancellation vs intrauterine insemination (IUI vs IVF) when two or less follicles were recruited during COS. Of the 461 cycles that met the criteria, 136 were cancelled, 141 were converted to IUI, and 184 completed IVF. LBR was significantly higher (11.6 vs 1.6%) in the IVF group regardless of the age of the patient and was even more significant in women aged <40 (13.1 vs 2%) [39]. More studies are needed to confirm that even in women with only one or two follicles, it is worthwhile to continue with IVF rather than cycle cancellation or converting to IUI.
3 Comparison of the Three Conventional Stimulation Protocols
The three conventional stimulation protocols were compared in an RCT involving 111 women with POR. The duration of stimulation and the total dose of gonadotropins used were significantly greater with the LA protocol compared to the other two protocols. The ongoing pregnancy rate was highest (16.2%) with the ANT protocol, and the other two protocols had an ongoing pregnancy rate of 8.1% [40].
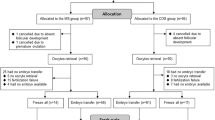
In contrast, another RCT showed an entirely different outcome. The researchers allocated 330 women between ANT protocol (168 women) and LA protocol (162 women). The cycle cancellation rate was higher in the ANT group compared to the LA group but was not statistically significant (22.15 vs 15.2%). The clinical pregnancy rate per transfer was also not significant (42.3 vs 33.1%). However, when the cycle cancellation rates were considered, the clinical pregnancy rate per cycle initiated was significantly lower in the ANT group compared to the LA group (25.6 vs 35.8%) [41].
Interestingly, 2 years before the publication of the above trials, a meta-analysis of 14 studies involving 566 patients in ANT protocol and 561 patients in LA protocol was performed. This showed a shorter duration of stimulation in the ANT group as the only significant difference between the two groups. There was no difference in cycle cancellation rate or the clinical pregnancy rates [42]. Taken together, it is likely that there is no significant difference in pregnancy rates between the three protocols.
4 Comparison of the Conventional Protocols with Newer Protocols
4.1 Mild Stimulation
Multiple studies have been published on using mild stimulation of ovaries for IVF in POR patients compared to conventional protocols that traditionally use high or very high doses of gonadotropins. The common features of many of the protocols described under this category are use of clomiphene citrate, aromatase inhibitors, and low-dose gonadotropins, as discussed in the chapter in Part II. ASRM Practice Committee recently reviewed the available studies and recommended that mild-stimulation IVF protocols be considered as primary stimulation protocols in POR patients as the pregnancy rates are similar and the cost of stimulation is lower [4].
4.2 Luteal Phase Estrogen Priming with Flexible Antagonist Start
This protocol was first described by Dragisic in 2005 using luteal phase estrogen followed by GnRH antagonist and gonadotropin started at the same time. The underlying principle is suppression of luteal follicle recruitment and decreasing follicular heterogeneity. In a retrospective study, 117 patients underwent estrogen priming protocol, and 69 underwent MDF protocol. Although similar number of oocytes were retrieved in both groups, the ongoing pregnancy rate was 37% in the estrogen priming group vs 25% in the MDF group which was not statistically significant [43].
In another retrospective study, 86 patients had luteal estrogen with antagonist start midway through stimulation compared with 69 patients who had ANT protocol for COS. The ongoing pregnancy rates were 27.1 vs 20% which did not reach statistical significance [44].
4.3 Delayed Start
Delayed start with GnRH antagonist protocol for young POR patients was first described in 2014 [45]. The modification in delayed-start protocol compared to estrogen priming with flexible antagonist start protocol is that estrogen priming is followed by 7 days of GnRH antagonist treatment before starting ovarian stimulation with gonadotropins.
One hundred women were randomly assigned to receive the delayed-start protocol or the MDF protocol. There was no significant difference between clinical or ongoing pregnancy rate between the two groups [46]. Similarly, another smaller RCT with 54 patients did not show any difference in any of the measured outcomes including pregnancy rate [47].
5 Conclusion
Conventional IVF stimulation protocols are likely equally effective and better than IUI for patients with POR. There is no consensus on one specific conventional IVF stimulation protocol for patients with POR. However, mild-stimulation IVF may be more cost-effective and may at least result in similar outcome as using conventional IVF protocols with fresh embryo transfers. More detailed discussions on mild approaches for COS are extensively discussed in the upcoming chapters.
References
Patrizio P, Vaiarelli A, Levi Setti PE, Tobler KJ, Shoham G, Leong M, et al. How to define, diagnose and treat poor responders? Responses from a worldwide survey of IVF clinics. Reprod Biomed Online. 2015;30(6):581–92.
Papathanasiou A, Searle BJ, King NM, Bhattacharya S. Trends in ‘poor responder’ research: lessons learned from RCTs in assisted conception. Hum Reprod Update. 2016;22(3):306–19.
Yakin K, Oktem O, Balaban B, Urman B. Bologna criteria are predictive for ovarian response and live birth in subsequent ovarian stimulation cycles. Arch Gynecol Obstet. 2019;299(2):571–7.
Practice Committee of the American Society for Reproductive Medicine. Comparison of pregnancy rates for poor responders using IVF with mild ovarian stimulation versus conventional IVF: a guideline. Fertil Steril. 2018;109(6):993–9.
Check JH, Slovis B. Choosing the right stimulation protocol for in vitro fertilization-embryo transfer in poor, normal, and hyper-responders. Clin Exp Obstet Gynecol. 2011;38(4):313–7.
Busnelli A, Papaleo E, Del Prato D, La Vecchia I, Iachini E, Paffoni A, et al. A retrospective evaluation of prognosis and cost-effectiveness of IVF in poor responders according to the Bologna criteria. Hum Reprod. 2015;30(2):315–22.
Giovanale V, Pulcinelli FM, Ralli E, Primiero FM, Caserta D. Poor responders in IVF: an update in therapy. Gynecol Endocrinol. 2015;31(4):253–7.
Polat M, Bozdag G, Yarali H. Best protocol for controlled ovarian hyperstimulation in assisted reproductive technologies: fact or opinion? Semin Reprod Med. 2014;32(4):262–71.
Chai J, Lee VC, Yeung TW, Li HW, Ho PC, Ng EH. Live birth and cumulative live birth rates in expected poor ovarian responders defined by the Bologna criteria following IVF/ICSI treatment. PLoS One. 2015;10(3):e0119149.
Polyzos NP, Nwoye M, Corona R, Blockeel C, Stoop D, Haentjens P, et al. Live birth rates in Bologna poor responders treated with ovarian stimulation for IVF/ICSI. Reprod Biomed Online. 2014;28(4):469–74.
Ke H, Chen X, Liu YD, Ye DS, He YX, Chen SL. Cumulative live birth rate after three ovarian stimulation IVF cycles for poor ovarian responders according to the bologna criteria. J Huazhong Univ Sci Technolog Med Sci. 2013;33(3):418–22.
Sefrioui O, Madkour A, Aboulmaouahib S, Kaarouch I, Louanjli N. Women with extreme low AMH values could have in vitro fertilization success. Gynecol Endocrinol. 2019;35(2):170–3.
Xu B, Chen Y, Geerts D, Yue J, Li Z, Zhu G, et al. Cumulative live birth rates in more than 3,000 patients with poor ovarian response: a 15-year survey of final in vitro fertilization outcome. Fertil Steril. 2018;109(6):1051–9.
Gonda KJ, Domar AD, Gleicher N, Marrs RP. Insights from clinical experience in treating IVF poor responders. Reprod Biomed Online. 2018;36(1):12–9.
Busnelli A, Somigliana E. Prognosis and cost-effectiveness of IVF in poor responders according to the Bologna criteria. Minerva Ginecol. 2018;70(1):89–98.
Bozdag G, Polat M, Yarali I, Yarali H. Live birth rates in various subgroups of poor ovarian responders fulfilling the Bologna criteria. Reprod Biomed Online. 2017;34(6):639–44.
Magnusson Å, Nilsson L, Oleröd G, Thurin-Kjellberg A, Bergh C. The addition of anti-Müllerian hormone in an algorithm for individualized hormone dosage did not improve the prediction of ovarian response-a randomized, controlled trial. Hum Reprod. 2017;32(4):811–9.
van Tilborg TC, Broekmans FJ, Dólleman M, Eijkemans MJ, Mol BW, Laven JS, et al. Individualized follicle-stimulating hormone dosing and in vitro fertilization outcome in agonist downregulated cycles: a systematic review. Acta Obstet Gynecol Scand. 2016;95(12):1333–44.
Lensen SF, Wilkinson J, Leijdekkers JA, La Marca A, Mol BWJ, Marjoribanks J, et al. Individualised gonadotropin dose selection using markers of ovarian reserve for women undergoing in vitro fertilisation plus intracytoplasmic sperm injection (IVF/ICSI). Cochrane Database Syst Rev. 2018;2:CD012693.
Friedler S, Meltzer S, Saar-Ryss B, Rabinson J, Lazer T, Liberty G. An upper limit of gonadotropin dose in patients undergoing ART should be advocated. Gynecol Endocrinol. 2016;32(12):965–9.
Lefebvre J, Antaki R, Kadoch IJ, Dean NL, Sylvestre C, Bissonnette F, et al. 450 IU versus 600 IU gonadotropin for controlled ovarian stimulation in poor responders: a randomized controlled trial. Fertil Steril. 2015;104(6):1419–25.
Haas J, Zilberberg E, Machtinger R, Kedem A, Hourvitz A, Orvieto R. Do poor-responder patients benefit from increasing the daily gonadotropin dose during controlled ovarian hyperstimulation for IVF? Gynecol Endocrinol. 2015;31(1):79–82.
Dakhly DMR, Bassiouny YA, Bayoumi YA, Hassan MA, Gouda HM, Hassan AA. The addition of growth hormone adjuvant therapy to the long down regulation protocol in poor responders undergoing in vitro fertilization: randomized control trial. Eur J Obstet Gynecol Reprod Biol. 2018;228:161–5.
Li XL, Wang L, Lv F, Huang XM, Wang LP, Pan Y, et al. The influence of different growth hormone addition protocols to poor ovarian responders on clinical outcomes in controlled ovary stimulation cycles: a systematic review and meta-analysis. Medicine (Baltimore). 2017;96(12):e6443.
Yu X, Ruan J, He LP, Hu W, Xu Q, Tang J, et al. Efficacy of growth hormone supplementation with gonadotrophins in vitro fertilization for poor ovarian responders: an updated meta-analysis. Int J Clin Exp Med. 2015;8(4):4954–67.
Dakhly DM, Bayoumi YA, Gad Allah SH. Which is the best IVF/ICSI protocol to be used in poor responders receiving growth hormone as an adjuvant treatment? A prospective randomized trial. Gynecol Endocrinol. 2016;32(2):116–9.
Doan HT, Quan LH, Nguyen TT. The effectiveness of transdermal testosterone gel 1% (androgel) for poor responders undergoing in vitro fertilization. Gynecol Endocrinol. 2017;33(12):977–9.
Bosdou JK, Venetis CA, Dafopoulos K, Zepiridis L, Chatzimeletiou K, Anifandis G, et al. Transdermal testosterone pretreatment in poor responders undergoing ICSI: a randomized clinical trial. Hum Reprod. 2016;31(5):977–85.
Kim CH, Ahn JW, Moon JW, Kim SH, Chae HD, Kang BM. Ovarian features after 2 weeks, 3 weeks and 4 weeks transdermal testosterone gel treatment and their associated effect on IVF outcomes in poor responders. Dev Reprod. 2014;18(3):145–52.
Nagels HE, Rishworth JR, Siristatidis CS, Kroon B. Androgens (dehydroepiandrosterone or testosterone) for women undergoing assisted reproduction. Cochrane Database Syst Rev. 2015;(11):CD009749.
Kasum M, Kurdija K, Orešković S, Čehić E, Pavičić-Baldani D, Škrgatić L. Combined ovulation triggering with GnRH agonist and hCG in IVF patients. Gynecol Endocrinol. 2016;32(11):861–5.
Haas J, Zilberberg E, Nahum R, Mor Sason A, Hourvitz A, Gat I, et al. Does double trigger (GnRH-agonist + hCG) improve outcome in poor responders undergoing IVF-ET cycle? A pilot study. Gynecol Endocrinol. 2019;35(7):628–30.
Mok-Lin E, Brauer AA, Schattman G, Zaninovic N, Rosenwaks Z, Spandorfer S. Follicular flushing and in vitro fertilization outcomes in the poorest responders: a randomized controlled trial. Hum Reprod. 2013;28(11):2990–5.
Haydardedeoglu B, Gjemalaj F, Aytac PC, Kilicdag EB. Direct aspiration versus follicular flushing in poor responders undergoing intracytoplasmic sperm injection: a randomised controlled trial. BJOG. 2017;124(8):1190–6.
von Horn K, Depenbusch M, Schultze-Mosgau A, Griesinger G. Randomized, open trial comparing a modified double-lumen needle follicular flushing system with a single-lumen aspiration needle in IVF patients with poor ovarian response. Hum Reprod. 2017;32(4):832–5.
Berkkanoglu M, Coetzee K, Bulut H, Ozgur K. Optimal embryo transfer strategy in poor response may include freeze-all. J Assist Reprod Genet. 2017;34(1):79–87.
Roque M, Valle M, Sampaio M, Geber S. Does freeze-all policy affect IVF outcome in poor ovarian responders? Ultrasound Obstet Gynecol. 2018;52(4):530–4.
Xue Y, Tong X, Zhu H, Li K, Zhang S. Freeze-all embryo strategy in poor ovarian responders undergoing ovarian stimulation for in vitro fertilization. Gynecol Endocrinol. 2018;34(8):680–3.
Quinquin M, Mialon O, Isnard V, Massin N, Parinaud J, Delotte J, et al. In vitro fertilization versus conversion to intrauterine insemination in Bologna-criteria poor responders: how to decide which option? Fertil Steril. 2014;102(6):1596–601.
Sunkara SK, Coomarasamy A, Faris R, Braude P, Khalaf Y. Long gonadotropin-releasing hormone agonist versus short agonist versus antagonist regimens in poor responders undergoing in vitro fertilization: a randomized controlled trial. Fertil Steril. 2014;101(1):147–53.
Prapas Y, Petousis S, Dagklis T, Panagiotidis Y, Papatheodorou A, Assunta I, et al. GnRH antagonist versus long GnRH agonist protocol in poor IVF responders: a randomized clinical trial. Eur J Obstet Gynecol Reprod Biol. 2013;166(1):43–6.
Pu D, Wu J, Liu J. Comparisons of GnRH antagonist versus GnRH agonist protocol in poor ovarian responders undergoing IVF. Hum Reprod. 2011;26(10):2742–9.
Shastri SM, Barbieri E, Kligman I, Schoyer KD, Davis OK, Rosenwaks Z. Stimulation of the young poor responder: comparison of the luteal estradiol/gonadotropin-releasing hormone antagonist priming protocol versus oral contraceptive microdose leuprolide. Fertil Steril. 2011;95(2):592–5.
Chang EM, Han JE, Won HJ, Kim YS, Yoon TK, Lee WS. Effect of estrogen priming through luteal phase and stimulation phase in poor responders in in-vitro fertilization. J Assist Reprod Genet. 2012;29(3):225–30.
Cakmak H, Tran ND, Zamah AM, Cedars MI, Rosen MP. A novel “delayed start” protocol with gonadotropin-releasing hormone antagonist improves outcomes in poor responders. Fertil Steril. 2014;101(5):1308–14.
Davar R, Neghab N, Naghshineh E. Pregnancy outcome in delayed start antagonist versus microdose flare GnRH agonist protocol in poor responders undergoing IVF/ICSI: an RCT. Int J Reprod Biomed (Yazd). 2018;16(4):255–60.
DiLuigi AJ, Engmann L, Schmidt DW, Benadiva CA, Nulsen JC. A randomized trial of microdose leuprolide acetate protocol versus luteal phase ganirelix protocol in predicted poor responders. Fertil Steril. 2011;95(8):2531–3.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Bhagavath, B. (2020). Conventional Controlled Ovarian Stimulation Protocols for Diminished Ovarian Reserve Patients and Poor Responders. In: Bukulmez, O. (eds) Diminished Ovarian Reserve and Assisted Reproductive Technologies. Springer, Cham. https://doi.org/10.1007/978-3-030-23235-1_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-23235-1_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-23234-4
Online ISBN: 978-3-030-23235-1
eBook Packages: MedicineMedicine (R0)