Abstract
Genetic testing has become an important tool in diagnosing monogenic disorders, particularly after the widespread availability of next-generation sequencing technologies in commercial laboratories. In rheumatology, hereditary diseases often present early in childhood, but adult-onset genetic disorders are also seen. The monogenic autoinflammatory syndromes (MAIS) and heritable disorders of connective tissue (HDCT) are two heterogeneous groups of conditions that are seen in rheumatology practice and largely depend on genetic testing for an accurate diagnosis. MAIS are a group of diseases characterized by recurrent and spontaneous episodes of inflammation, including fever, arthritis, and serositis, with long-term serious complications such as AA amyloidosis if untreated. HDCT are a heterogeneous group of diseases characterized by defects in several extracellular matrix elements, producing clinically obvious changes in the skeleton, skin, ligaments, tendons, and other soft tissues. This chapter presents an overview of terminology in clinical genetics, the regulations and advantages of genetic testing in rheumatology, and a review of the most common MAIS and HDCT.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Autoinflammatory syndrome
- Genetic testing
- Connective tissue
- Ehlers-Danlos syndrome
- Marfan syndrome
- Osteogenesis imperfecta
Introduction
The dramatic advances in human genome research and the number of available genetic tests call for improved genetic knowledge among healthcare providers, including rheumatologists. Genetic testing is most clinically applicable in monogenic conditions, where a mutation in a single gene is directly responsible of the disease. In this setting, genetic testing may confirm or refute the diagnosis and can guide therapeutic interventions. Nonetheless, genetics is a fundamental component of complex multifactorial disorders, where multiple susceptibility genes, along with environmental influences, play a role in the etiopathogenesis of several rheumatologic conditions such as rheumatoid arthritis, systemic lupus erythematosus, and osteoarthritis, among others [1,2,3,4].
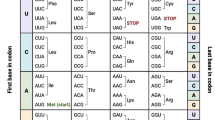
Overview of General Concepts in Clinical Genetics
A mutation is any change in the primary nucleotide sequence of DNA. Mutations can have a variety of functional consequences ranging from silent (without phenotypical significance) to loss- or gain-of-function mutations. Usually, mutations need to affect the exons (i.e., the encoding regions of the genome) in order to cause a disease. Germline mutations lead to potential transmissibility of genetic diseases. The patterns of transmission in monogenic or single-gene disorders is typically autosomal (affecting one of the 22 nonsex chromosomes) dominant (AD) or autosomal recessive (AR). A disease is said to be transmitted on an AD pattern if one mutated copy of the gene in each cell is enough for a person to be affected by such disorder, while for AR diseases to manifest, there needs to be two copies of an abnormal gene (one paternal and one maternal). Other conditions are transmitted in the sex chromosomes (X or Y chromosomes) and therefore affect males or females differently. For instance, X-linked disorders will be expressed fully in men as they only possess one X chromosome, while the same disease may be less severe or not expressed at all in females. Notably, X-linked conditions are only transmitted from the maternal side, which is important to consider while evaluating a patient’s family history [4,5,6].
AD conditions can have variable penetrance, which refers to the proportion of people with a genetic change who will exhibit signs and symptoms of the particular genetic disorder. In this sense, a typical Mendelian inheritance pattern may not be seen if there is incomplete penetrance of an AD disorder. Another possibility for unaffected parents in the cases of AD diseases is a new germline mutation, such as it has been reported in Marfan syndrome. However, in most cases, AD disorders are present in one of the parents, and the probability of transmission to the offspring is 50% for each child, with the same risks for males and females. Variable expressivity is another relevant concept in clinical genetics, which refers to the degree to which a specific genotype is expressed in the phenotype, and can affect the severity, type of organ involvement, or age of onset of the disease. A phenomenon called heterogeneity also increases the complexity of identifying genetic disorders, as mutations in different genes can sometimes translate into a very similar clinical phenotype, which is sometimes seen in conditions affecting the inflammasome pathways or the extracellular matrix, causing autoinflammatory syndromes or heritable connective tissue disorders, respectively [4,5,6].
Mosaicism and mitochondrial disorders are also exceptions to simple Mendelian inheritance patterns. In mosaicism, there are two or more genetically distinct cell lines in the tissues due to mutations occurring during or after embryonic development. Inherited mitochondrial disorders occur due to mutations in genes encoded by DNA in the mitochondria and are transmitted in a matrilineal fashion (i.e., all children from an affected mother will inherit the mutations, but there will be sparing of all the progeny from affected males) [4,5,6].
AR disorders are less common than AD diseases and usually relate to consanguinity or when mutations are very common due to selective evolutionary advantage (such as protection against deadly infections). The mutated genes cause a partial or complete loss of function, leading to alterations in receptors, enzymes, or adaptor proteins in intracellular signaling or metabolic pathways. X-linked and Y-linked (sex chromosomes) transmitted disorders are less commonly seen in rheumatology [1, 2, 4,5,6].
Genetic Testing in Rheumatology
Hereditary diseases often present early in childhood, but adult-onset genetic disorders are also seen in rheumatology practice. The first challenge is to identify based on history when a clinical scenario may be due to a genetic disease. As with any ancillary testing, before initiating genetic evaluation, it is crucial to obtain a thorough history, including detailed family history, which may help with recognition of clinical patterns associated with specific genetic diseases. Physical exam findings, as well as laboratory (such as inflammatory markers), biochemical, and imaging tests are often useful in establishing a differential diagnosis. In rheumatology, genetic testing for autoinflammatory disorders and hereditable connective tissue disorders has become an essential tool in the last decade, as an accurate diagnosis can lead to appropriate and timely therapeutic interventions and/or monitoring for specific organ affectation [1, 2, 7,8,9].
Before performing genetic testing, it is imperative to discuss with patients the benefits and expectations and to obtain an informed consent. It is also important to consider the sensitivity and specificity of the test, as some mutations are not identified in standard testing, particularly in cases of mosaicism or new undiscovered variants [1,2,3,4, 10,11,12]. For instance, cases of somatic mosaicism of the nucleotide-binding domain, leucine-rich repeat, and pyrin domain-containing protein 3 (NLRP3) have been reported in patients with chronic infantile neurological cutaneous and articular (CINCA) syndrome or neonatal-onset multisystem inflammatory disease (NOMID) [13].
The involvement of a genetic counselor is strongly recommended in all cases to address the emotional burden of genetic testing, and to help communicating the results, as well as the nature, and recurrence risk of the disease [3, 11].
Genetic testing for diagnostic purposes is not to be confused with direct-to-consumer testing, where the test is offered as a service from a private company directly to the consumer, without a clinician or expert geneticist to interpret the results. These types of genetic tests are not typically comprehensive enough to identify specific single-gene disorders [14].
Clinically Available Methodologic Approaches to Genetic Testing
In general, genetic testing involves the use of specific assays to study the genes in an individual’s genome, who is suspected to be at an increased risk for a specific inherited condition based on clinical findings and family history. All types of genetic testing involve the analysis of specimens (commonly leukocytes, buccal cells, fibroblasts, o other tissues). There are different methods for genetic testing with variable sensitivity, specificity, expensiveness, and requirement for expertise and time. Gene panels assess alterations in multiple genes that have been implicated in specific genetic conditions. For instance, many commercial laboratories have panels to evaluate for heritable connective tissue disorders and autoinflammatory or periodic fever syndromes that include a few to dozens of probable genes, depending on the laboratory. This is particularly relevant as multiple rheumatologic conditions have very similar clinical presentations but may be caused by mutations in different genes (a phenomenon called heterogeneity, as previously mentioned). Single-gene testing is also commercially available for most heritable connective tissue disorders and autoinflammatory monogenic diseases [4, 15, 16].
Since the use of next-generation sequencing (NGS) technologies has dramatically expanded, it is now widely used in commercial laboratories. The use of targeted deletion/duplication analysis has now also become a standard test when no pathogenic aberrations are detected by NGS. With this test, it is possible to identify partial or whole gene deletions and duplications in the associated genes. The required specimens for single-gene testing or gene panels are usually whole blood in an EDTA tube (purple or lavender top tube) and/or buccal swabs/saliva, and the turnaround time is generally 10–21 days for most commercial laboratories [4, 15].
Prior to NGS, the traditional Sanger sequencing test was widely used for DNA sequencing. Sanger sequencing is based on the selective incorporation of chain-terminating nucleotides in vitro, which were radioactively or fluorescently tagged for detection in automated equipment. This method has good accuracy, but it only allows to identify mutations in a specific gene and cannot be used to provide information about larger portions of the genome. Sanger sequencing is currently mainly used in commercial laboratories as a confirmation step once the pathogenic variants have been identified [4, 15, 17].
In individuals with unexplained syndromes that are suspected to be inherited or genetic disorders, whole-genome sequencing (WGS) is available. Genome sequencing can include only coding regions (whole-exome sequencing) or the entire genome (regulatory and noncoding regions included). Besides increased cost and being more time-consuming, WGS also increases the likelihood of identifying unexpected genetic alterations that may be completely unrelated to the test indication or of unclear clinical relevance [4].
Genetic testing regulations are similar to other specialized laboratory tests. The Clinical Laboratory Improvement Amendments (CLIA), a Centers for Medicare and Medicaid Services (CMS) program, are the federal regulatory standards that ensure quality laboratory testing in the United States, including in the field of genetics [18]. As of April 2018, the Food and Drug Administration (FDA) issued new guidelines to ensure the analytical and clinical validity of NGS-based testing results [19].
Genetic Testing in Monogenic Autoinflammatory Syndromes
Autoinflammatory syndromes are a group of diseases characterized by recurrent and spontaneous episodes of fever, arthritis, serositis, elevated inflammatory markers, skin rashes, and long-term serious complications such as AA amyloidosis as the result of chronic inflammation. In contrast to autoimmune diseases where there are autoantibodies or reactive T cells, autoinflammatory diseases are mediated by the innate immune system. Specifically, they are caused by anomalous activation of the inflammasome, a multiprotein scaffold complex that leads to generation of interleukin-1 (IL-1) and consequent uncontrolled inflammation. Many of the monogenic autoinflammatory syndromes (MAIS) present during early childhood, but adult-onset forms are also often seen, particularly familial Mediterranean fever (FMF) and tumor necrosis factor receptor-associated periodic syndrome (TRAPS) [1, 7, 8].
Genetic testing has become essential to accurately diagnose MAIS. Most commercial genetic laboratories in the United States use NGS technology followed by targeted deletion/duplication analysis if no pathogenic aberrations are detected by NGS (see “Clinically Available Methodologic Approaches to Genetic Testing” for more details). A summary of the clinical presentation, pattern of inheritance, and affected gene/protein for most common MAIS is shown in Table 19.1.
Familial Mediterranean fever (FMF) is the most common monogenic periodic fever syndrome. FMF is an AR disorder caused by mutations at the MEFV gene which codes for the protein pyrin. Although FMF typically presents during childhood, adult-onset forms can be occasionally seen. The clinical diagnosis is made based on the Tel Hashomer criteria (two major criteria or one major and two minor criteria are needed to make the diagnosis): major criteria, (1) recurrent febrile episodes with serositis (peritonitis, synovitis, or pleuritis), (2) AA amyloidosis without a predisposing disease, and (3) favorable response to regular colchicine treatment; and minor criteria – (1) recurrent febrile episodes, (2) erysipelas-like erythema, and (3) FMF in first-degree relative [1, 8, 20, 21].
TRAPS is a monogenic periodic syndrome with an AD pattern of inheritance, caused by mutations in the TNF receptor superfamily member 1A (TNFRSF1A) gene. TRAPS is characterized by recurrent inflammatory attacks lasting 1–3 weeks, with fever, arthralgia or arthritis, rash, serositis, cramps, myalgia, lymphadenopathy, headache, and fatigue. Secondary AA amyloidosis is common in untreated patients [8, 20, 21].
Mevalonate kinase deficiency (MKD) , formerly known as hyper-immunoglobulin D syndrome, is an AR disorder caused by a mutation in the mevalonate kinase (MVK) gene. Clinically, the inflammatory attacks are characterized by fever, gastrointestinal compromise, skin rash, lymphadenopathy, arthralgia or arthritis, and fatigue. The attacks usually last for 3–7 days and they resolve spontaneously [8, 20, 21].
The cryopyrin-associated periodic syndromes (CAPS) comprise a group of AD disorders that include the familial cold autoinflammatory syndrome (FCAS), Muckle-Wells syndrome (MWS), and chronic infantile neurological cutaneous and articular (CINCA) syndrome, caused by mutations in the NLRP3/CIAS1 gene that codes for cryopyrin. Nucleotide-binding domain, leucine-rich repeat, and pyrin domain-containing protein 12 (NLRP12)-associated autoinflammatory disorder (NLRP12AD) is caused by NLRP12 mutation (monarch-1). The CAPS most commonly present in the first 6 months of life, but there have been rare cases reported in adulthood. CAPS commonly present with fever, urticaria-like rash, conjunctivitis, and arthritis, but more specific clinical features depend on the time of onset, with the perinatal form being the most severe presentation (uveitis, optic nerve atrophy, chronic aseptic meningitis, sensorineural hearing loss) [8, 20, 21].
Blau syndrome (BS) and early-onset sarcoidosis (EOS) are autoinflammatory granulomatous disorders caused by mutations in the nucleotide-binding oligomerization domain-containing protein 2/caspase recruitment domain-containing protein 15 (NOD2/CARD15). BS and EOS present during childhood and have the characteristic histologic findings of noncaseating granulomatous inflammation in affected tissues. BS is transmitted on an AD pattern and presents with a triad of granulomatous arthritis, dermatitis, and uveitis, while EOS is the sporadic form and patients present with polyarthritis with lymphadenopathy and skin and ocular involvement [8, 20, 21].
Pyogenic arthritis, pyoderma gangrenosum and cystic acne (PAPA) syndrome , Majeed syndrome (MS) , and deficiency of the interleukin-1 receptor antagonist (DIRA) are autoinflammatory pyogenic disorders that typically present in early childhood. PAPA syndrome is an AD disorder caused by mutations in the proline-serine-threonine phosphatase-interacting protein 1/cluster of differentiation 2 binding protein 1 (PSTPIP1/CD2BP1) gene. MS is predominantly an AR disorder (although sporadic forms have been described), caused by mutations in the LPIN2 gene coding for lipin-2. DIRA is an AR disorder due to mutations in the IL1RN gene that codes for the interleukin-1 receptor antagonist protein [8, 20, 21].
Genetic Testing in Heritable Disorders of Connective Tissue
The heritable disorders of connective tissue (HDCT) are a heterogeneous group of diseases characterized by defects in several extracellular matrix elements including elastin, collagen, mucopolysaccharides, and many others, producing clinically obvious changes in the skeleton, skin, ligaments, tendons, and other soft tissues [22, 23].
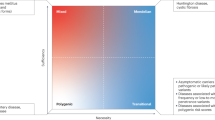
As with the MAIS, genetic testing has allowed a reliable pathway to confirm the diagnosis of many HDCT. Among the clinical features that should lead to a high index of suspicion for HDCT and subsequent genetic testing include joint hypermobility or frequent dislocations, abnormal skin findings (cutis laxa, abnormal scarring, spontaneous bruising, velvety, highly elastic or translucent skin), tissue fragility (multiple hernias or rectal prolapse in early childhood), early-onset hearing loss, ocular findings (ectopia lentis, retinal detachment, scleral fragility, vitreous abnormalities), spontaneous or recurrent pneumo- or hemothoraces, classic cardiovascular abnormalities (early-onset aneurysms, dissections, arterial tortuosity, or family history of any of these disorders), musculoskeletal findings such as pectus excavatum or carinatum, arachnodactyly, brachydactyly, osteoarthritis before age 40, congenital clubfoot or Marfanoid appearance, and craniofacial abnormalities (including cleft palate and hypertelorism), among others [9, 22, 23]. For a summary of clinical findings, affected genes, and the pattern of inheritance of most common HDCT, see Table 19.2.
While some of the HDCT have a known genetic background with specific mutations that serve for diagnostic purposes, others are still not well understood. For instance, the joint hypermobility syndrome/Ehlers-Danlos syndrome hypermobility type (JHS/EDS-HT) is the most common HDCT described so far. JHS/EDS-HT is an AD disorder considered a clinical diagnosis but without a defined molecular basis in most cases (although mutations in the TNXB gene causing heterozygous tenascin X defects has been described in some of these patients), in contrast to the other Ehlers-Danlos syndrome (EDS) variants where mutations in different types of collagen are typically found. EDS is characterized by joint hypermobility and hyperextensible skin. There are several types of EDS (some of them categorized as EDS I to EDS VIII), based on the tissues involved and the molecular and biochemical abnormalities involved. EDS I and II are the classic forms, with predominant joint hypermobility, skin fragility, and hyperextensibility, related to mutations in COL5A1/COL5A2 causing defects in collagen V. EDS IV is the vascular form, which predisposes to spontaneous intestinal and vascular ruptures, with life-threatening consequences. EDS IV is an AD disorder due to mutations in COL3A1 (collagen III gene) [9, 20,21,22,23].
Many other forms of EDS have been described, with variable joint, skin, dental, and ocular manifestations, secondary to enzymatic or protein defects involving extracellular matrix-related genes such as ADAMTS2 (procollagen I N-terminal proteinase), PLOD1 (procollagen-lysine 5 dioxygenase), B4GALT7 (galactosyltransferase 7), and COL1A1/COL1A2 (procollagen). In contrast, mutations in the elastin gene (ELN) can be associated with similar clinical features in non-EDS conditions, including the AD form of cutis laxa , manifested by loose and redundant folds of skin due to lack of elasticity. Other forms of cutis laxa include X-linked form or occipital horn syndrome, caused by mutations in the ATP7A gene (which codes for a transmembrane copper-transporting protein) [20,21,22,23].
Marfan syndrome (MFS) is another common HDCT that primarily affects the musculoskeletal (long and thin extremities, tall stature, scoliosis, chest deformities), cardiovascular (predominantly aortic aneurysms and dilated aortic root, mitral valve prolapse), and ocular (ectopia lentis with upward displacement, retinal detachments) systems, as well as increased frequency of spontaneous pneumothorax and hernias. MFS is typically associated with mutations in the FB1 gene which codes for fibrillin 1. Similarly, congenital contractural arachnodactyly (an MFS-like disorder) has been linked to mutations in the FB2 gene. In contrast, some patients with an MFS phenotype have mutations in TGFBR2 (transforming growth factor-β or TGF-β receptor 2). Loeys-Dietz syndrome (LDS) , an MFS-related disorder, is also associated with mutations affecting TGF-β signaling, specifically the TGFBR1 and TGFBR2 genes, likely illustrating the important role of this molecule in the pathogenesis of these disorders. LDS is usually manifested by craniofacial abnormalities (mainly hypertelorism and cleft palate) [20,21,22,23].
Osteogenesis imperfecta (OI) is an AD disorder caused mainly by mutations affecting type I collagen, the most abundant protein in skin, bones, and tendons. Specifically, more than 90% of mutations in OI involve the genes coding for the pro-α1 or pro-α2 chain of type I procollagen (COL1A1 or COL1A2, respectively). Main clinical features include blue sclerae, multiple fractures, abnormal dentinogenesis, progressive early-onset hearing loss, and a positive family history (although sporadic new mutations and germline mosaicism have also been described). However, less classic clinical manifestations are also seen, including joint laxity, kyphoscoliosis, excessive cutaneous scarring, cardiac valvular disease, and fragility of large blood vessels [20,21,22,23].
Summary
-
Genetics is a fundamental component of complex multifactorial disorders, but genetic testing is most clinically applicable nowadays in the diagnosis of monogenic disorders in rheumatology.
-
Most genetic conditions are transmitted in an autosomal dominant, autosomal recessive, or X-linked pattern.
-
A typical Mendelian inheritance pattern may not be seen in cases of incomplete penetrance, variable expressivity, and mosaicism.
-
A thorough history, physical exam, and laboratory testing are usually necessary to establish a differential diagnosis focused on genetic conditions.
-
Obtaining an informed consent and discussing the potential benefits and risks are essential prior to performing genetic testing.
-
Most commercial laboratories have genetic panels available to evaluate for monogenic autoinflammatory syndromes and heritable disorders of connective tissue based on next-generation sequencing technologies.
-
Genetic panels evaluate multiple probable genes, in contrast to single-gene testing where each gene is tested individually.
-
Autoinflammatory syndromes are a group of diseases characterized by recurrent and spontaneous episodes of systemic inflammation and long-term development of secondary AA amyloidosis, as a result of anomalous activation of the inflammasome and generation of interleukin-1.
-
The heritable disorders of connective tissue are a heterogeneous group of diseases characterized by defects in several extracellular matrix elements, producing clinically obvious changes in the skeleton, skin, ligaments, tendons, and other soft tissues.
-
Genetic testing has allowed a reliable pathway to confirm the diagnosis in monogenic autoinflammatory syndromes and many heritable disorders of connective tissue.
Questions and Answers
-
1.
A 29-year-old man presents for evaluation of severe scoliosis, tall stature, history of retinal detachments, and recurrent spontaneous pneumothoraces. A diagnosis of Marfan syndrome is suspected. On further evaluation, patient reveals his father also has tall stature and ectopia lentis, but no history of cardiopulmonary disease. The patient’s paternal grandfather died at the age of 28 due to a ruptured aneurysm. The different clinical presentations in this patient’s family members are most likely due to:
-
A.
The mutated genes are different in each family member.
-
B.
Incomplete penetrance.
-
C.
Mosaicism.
-
D.
Variable expression.
-
E.
The patient does not have a genetic disorder.
Correct answer: D
The question illustrates a case with multiple features of Marfan syndrome (MFS), including tall stature, scoliosis, classic ocular manifestations, and recurrent pneumothoraces in a young man. Moreover, his father and paternal grandfather also show features of MFS. Variable expression (or expressivity) refers to the degree to which a specific genotype is expressed in the phenotype and can affect the severity, type of organ involvement, or age of onset of the disease. MFS commonly shows variable expression. Incomplete penetrance refers to a proportion of people with a genetic change who will not exhibit signs and symptoms of the particular genetic disorder but are able to transmit the mutations to their offspring. As all the generations have some degree of organ involvement from MFS, option B is incorrect. Mosaicism occurs when there are two or more genetically distinct cell lines in the tissues due to mutations occurring during or after embryonic development. Mosaicism would not explain the different clinical presentations in this patient’s family members (option C). It would be very unlikely that every family member had a different mutation that would explain their similar pattern of symptoms suggestive of MFS or that the patient did not have a genetic disease (options A and E).
-
A.
-
2.
An 18-year-old woman presents to rheumatology clinic for evaluation of recurrent episodes of fever, skin rash, and joint and abdominal pain. The episodes started approximately 18 months ago, and she has had multiple admission to the emergency department due to this. During her last ED visit 4 weeks ago, she was diagnosed with appendicitis, but she decided to leave against medical advice as she has noticed her symptoms resolve after a few days with rest and ibuprofen. She is otherwise healthy and does not take any prescription medications. The patient is adopted and is unable to provide a family history. Today she feels well and denies any of her typical symptoms. Regarding this patient’s clinical presentation:
-
A.
The patient has features of a monogenic autoinflammatory syndrome, but no additional intervention is necessary as her symptoms resolve spontaneously.
-
B.
The age of onset in this case rules out a monogenic autoinflammatory syndrome.
-
C.
The patient has appendicitis and requires antibiotics and a referral to surgery.
-
D.
The patient likely has monogenic autoinflammatory syndrome, but due to lack of family history, she should be sent for whole-exome sequencing.
-
E.
The patient’s clinical presentation is suggestive of an autoinflammatory syndrome, and the risks and benefits of genetic testing should be thoroughly discussed with the patient.
Correct answer: E
A young woman with recurrent episodes of inflammation with fever, arthralgias, skin involvement, and likely peritonitis (abdominal pain and previous misdiagnosed appendicitis) is strongly suggestive of an autoinflammatory syndrome. The lack of family history in this case can make the diagnosis more challenging, but sending the patient directly for whole-genome sequencing would be premature (option D). Option E is the most appropriate option as this patient would benefit from genetic testing, preceded by obtaining an informed consent and a thorough discussion, including rationale and implications, risks versus benefits of genetic testing, and alternatives. Many of the monogenic autoinflammatory syndromes (MAIS) are associated with secondary AA amyloidosis if left untreated; therefore, option A is incorrect. Even though some of the MAIS present during early childhood, adult-onset forms are common and must be considered (option B). Serositis, particularly peritonitis, is frequently associated with the recurrent inflammatory episodes in MAIS which are sometimes misdiagnosed with acute abdomen in the emergency department. Her previous history of recurrent symptoms with spontaneous resolution without antibiotics makes a diagnosis of acute appendicitis much less likely (option D).
-
A.
-
3.
An 18-year-old woman presents for follow-up. During early childhood, she developed recurrent episodes of fever, conjunctivitis, polyarthritis, and generalized hives lasting for 24–48 h. After clinical evaluation and genetic testing, she was diagnosed with familial cold autoinflammatory syndrome and has been appropriately treated since then. She feels well and has not noticed any significant flares. This patient’s autoinflammatory syndrome is due to abnormalities in which of the following proteins:
-
A.
Mevalonate kinase (MVK gene)
-
B.
Pyrin (MEFV gene)
-
C.
Cryopyrin (NLRP3 gene)
-
D.
IL-1 receptor antagonist (IL1RN gene)
-
E.
TNF receptor 1 (TNFRSF1A)
Correct answer: C
This patient has been diagnosed with familial cold autoinflammatory syndrome (FCAS), which is a cryopyrin-associated periodic syndrome (CAPS). CAPS are caused by mutations in the NLRP3/CIAS1 or NLRP12 genes, which code for the proteins cryopyrin or monarch-1, respectively. Mevalonate kinase is the affected protein in mevalonate kinase deficiency, formerly known as hyper-IgD syndrome (option A). Familial Mediterranean fever is caused by mutations in the MEFV gene, which codes for pyrin (option B). Deficiency of the IL-1 receptor antagonist and mutations affecting the TNF receptor 1 are also causes of monogenic inflammatory syndromes but are not specifically associated with the familial cold autoinflammatory syndrome (options D and E).
-
A.
-
4.
Which of the following is a true statement about genetic testing?
-
A.
Genetic testing is strictly regulated and under similar federal regulatory standards as other specialized laboratory tests.
-
B.
Direct-to-consumer testing is an adequate initial approach for patients with a suspected genetic disease.
-
C.
Single-gene testing is most helpful when the clinical presentation is vague and there are multiple candidate genes as potential causes for the disease.
-
D.
Next-generation sequencing has become obsolete since the Sanger sequencing technique became commercially available.
-
E.
Genetic testing is safe; therefore, obtaining an informed consent is not recommended.
Correct answer: A
Genetic testing regulations are similar to other specialized laboratory tests to ensure the analytical and clinical validity, under the Clinical Laboratory Improvement Amendments (CLIA), a Centers for Medicare and Medicaid Services (CMS) program. Direct-to-consumer genetic testing is not currently recommended as a diagnostic tool for genetic diseases (option B). In contrast to genetic panels where multiple genes are evaluated, single-gene testing is a much narrower strategy and would only be useful if there is only one or very few candidate genes (option C). Next-generation sequencing (NGS) technologies are widely used in commercial laboratories, while the Sanger technique is mostly used for confirmatory purposes (option D). Even though genetic testing is considered safe, the emotional impact and the possibility of identifying unexpected and unrelated genetic alterations, among other implications of genetic testing, need to be discussed with patients, and an informed consent should be obtained (option E).
-
A.
-
5.
A 22-year-old woman presents to rheumatology clinic for evaluation of effort-related arthralgias. She reports that since childhood she has been more flexible than her peers. She can bend her thumbs backward to her wrists but cannot touch the floor with her palms when bending forward with her knees extended. She also states that her skin bruises very easily and is thin. Her mother died in her 20s while pregnant due to uterine rupture, and her father died in his 30s due to a spontaneous bowel perforation. A diagnosis of vascular Ehlers-Danlos syndrome (EDS) is considered. What is the most likely affected gene in this type of EDS?
-
A.
FBN1
-
B.
ADAMTS2
-
C.
COL3A1
-
D.
PLOD1
-
E.
TNXB
Correct answer: C
Vascular or type IV EDS is an AD disorder caused by a mutated COL3A1 gene, which codes for a collagen III pro-α1 chain. Vascular EDS is a life-threatening disease due to spontaneous rupture of blood vessels and internal organs (intestines or uterus). FBN1 codes for fibrillin 1, the protein affected in Marfan syndrome (option A). ADAMTS2 is a procollagen peptidase associated with EDS VIIC or dermatosparaxis type, an AR characterized by prominent redundant and extremely fragile skin, hernias, and short stature (option B). PLOD1 codes for a lysyl hydroxylase and is associated with EDS type VI or kyphoscoliotic EDS type 1 (option D). TNXB mutations (option E) are associated with classic-like EDS (AR disorder) and in less than 10% of patients with hypermobile EDS (AD inheritance).
-
A.
References
Turanlı ET, Everest E, Balamir A, Aydın AK, Kasapçopur Ö. Role of genetics in pediatric rheumatology. Turk Pediatri Ars. 2017;52(3):113–21.
Cornélis F. Genetics and clinical practice in rheumatology. Joint Bone Spine. 2003;70(6):458–64.
Kirmani S. Molecular genetic testing in endocrinology – a practical guide. Endocr Pract. 2012;18(1):85–9.
Domchek SM, Jameson J, Miesfeldt S. The practice of genetics in clinical medicine. In: Kasper D, Fauci A, Hauser S, Longo D, Jameson J, Loscalzo J, editors. Harrison’s principles of internal medicine. 19th ed. New York, NY: McGraw-Hill; 2014. http://accessmedicine.mhmedical.com.ezproxy.med.nyu.edu/content.aspx?bookid=1130§ionid=79728285. Accessed 28 Jan 2019.
Jameson J, Kopp P. Genes, the environment, and disease. In: Kasper D, Fauci A, Hauser S, Longo D, Jameson J, Loscalzo J, editors. Harrison’s principles of internal medicine. 19th ed. New York, NY: McGraw-Hill; 2014. http://accessmedicine.mhmedical.com.ezproxy.med.nyu.edu/content.aspx?bookid=1130§ionid=79728075. Accessed 06 Feb 2019.
Griffiths AJF, Miller JH, Suzuki DT, et al. An introduction to genetic analysis. In: Penetrance and expressivity. 7th ed. New York: W. H. Freeman; 2000. Available from: https://www.ncbi.nlm.nih.gov/books/NBK22090/.
Federici L, Rittore-Domingo C, Koné-Paut I, Jorgensen C, Rodière M, Le Quellec A, Touitou I. A decision tree for genetic diagnosis of hereditary periodic fever in unselected patients. Ann Rheum Dis. 2006;65(11):1427–32.
Caso F, Rigante D, Vitale A, Lucherini OM, Costa L, Atteno M, Compagnone A, Caso P, Frediani B, Galeazzi M, Punzi L, Cantarini L. Monogenic autoinflammatory syndromes: state of the art on genetic, clinical, and therapeutic issues. Int J Rheumatol. 2013;2013:513782.
Colombi M, Dordoni C, Chiarelli N, Ritelli M. Differential diagnosis and diagnostic flow chart of joint hypermobility syndrome/ehlers-danlos syndrome hypermobility type compared to other heritable connective tissue disorders. Am J Med Genet C Semin Med Genet. 2015;169C(1):6–22.
Knob AL. Principles of genetic testing and genetic counseling for renal clinicians. Semin Nephrol. 2010;30(4):431–7.
Marsick R, Limwongse C, Kodish E. Genetic testing for renal diseases: medical and ethical considerations. Am J Kidney Dis. 1998;32(6):934–45.
Institute of Medicine (US) Committee on Assessing Genetic Risks. In: Andrews LB, Fullarton JE, Holtzman NA, et al., editors. Assessing genetic risks: implications for health and social policy. Washington, DC: National Academies Press (US); 1994. 2, Genetic testing and assessment. Available from: https://www.ncbi.nlm.nih.gov/books/NBK236037/.
Finetti M, Omenetti A, Federici S, Caorsi R, Gattorno M. Chronic infantile neurological cutaneous and articular (CINCA) syndrome: a review. Orphanet J Rare Dis. 2016;11:167.
Middleton A, Mendes Á, Benjamin CM, Howard HC. Direct-to-consumer genetic testing: where and how does genetic counseling fit? Per Med. 2017;14(3):249–57.
Zhang W, Cui H, Wong LJ. Application of next generation sequencing to molecular diagnosis of inherited diseases. Top Curr Chem. 2014;336:19–45.
Nakayama M, Oda H, Nakagawa K, Yasumi T, Kawai T, Izawa K, Nishikomori R, Heike T, Ohara O. Accurate clinical genetic testing for autoinflammatory diseases using the next-generation sequencing platform MiSeq. Biochem Biophys Rep. 2016;9:146–52.
Mu W, Lu HM, Chen J, Li S, Elliott AM. Sanger confirmation is required to achieve optimal sensitivity and specificity in next-generation sequencing panel testing. J Mol Diagn. 2016;18(6):923–32.
Clinical Laboratory Improvement Amendments (CLIA). Baltimore, MD: Centers for Medicare & Medicaid. Accessed 23 Feb 2019. World Wide Web URL: https://www.cms.gov/Regulations-and-Guidance/Legislation/CLIA/index.html
FDA finalizes guidances to accelerate the development of reliable, beneficial next generation sequencing-based tests. Silver Spring, MD: U.S. Food and Drug Administration. Accessed 23 Feb 2019. World Wide Web URL: https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm604462.htm
Online Mendelian Inheritance in Man, OMIM®. McKusick-Nathans Institute of Genetic Medicine. Baltimore, MD: Johns Hopkins University. Accessed 23 Feb 2019. World Wide Web URL: https://omim.org/
Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle, WA: University of Washington, Seattle; 1993–2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1116/
Bascom R, Schubart JR, Mills S, Smith T, Zukley LM, Francomano CA, McDonnell N. Heritable disorders of connective tissue: description of a data repository and initial cohort characterization. Am J Med Genet A. 2019; https://doi.org/10.1002/ajmg.a.61054. [Epub ahead of print]
Prockop DJ, Bateman JF. Heritable disorders of connective tissue. In: Jameson J, Fauci AS, Kasper DL, Hauser SL, Longo DL, Loscalzo J, editors. Harrison’s principles of internal medicine. 20th ed. New York, NY: McGraw-Hill. http://accessmedicine.mhmedical.com.ezproxy.med.nyu.edu/content.aspx?bookid=2129§ionid=192530885. Accessed 23 Feb 2019.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Fernandez-Ruiz, R., Efthimiou, P. (2020). Clinical Genetics in Rheumatology. In: Efthimiou, P. (eds) Absolute Rheumatology Review. Springer, Cham. https://doi.org/10.1007/978-3-030-23022-7_19
Download citation
DOI: https://doi.org/10.1007/978-3-030-23022-7_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-23021-0
Online ISBN: 978-3-030-23022-7
eBook Packages: MedicineMedicine (R0)