Abstract
Thyroid storm is a life-threatening presentation of hyperthyroidism. Its presentation includes nonspecific signs and symptoms, and its diagnosis is clinical. Providers need to address any precipitating conditions while simultaneously treating thyroid storm. Thyroid storm management requires understanding of underlying pathophysiology. New thyroid hormone synthesis must be inhibited by thionamides before iodine is administered, which may serve as additional substrate for thyroid hormone synthesis. These patients require admission for a critical care unit for further management.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Thyroid storm
- Hyperthyroidism
- Endocrinology
- Endocrinological emergencies
- T4, TSH
- Thyroid Storm—It’s Raining Thyroxine
Case
Palpitations and Diaphoresis
Pertinent History
Patient is a 53-year-old female who presents to the Emergency Department accompanied by her husband. She states she has felt like her heart was racing all day today, and she feels hot and sweaty. She denies any upper respiratory symptoms, chest pain, shortness of breath, abdominal pain, vomiting, or diarrhea. She feels slightly nauseated. Her husband also adds that she has been mildly confused over the past few days and seems to get lost in familiar areas or intermittently forgets what she is doing, but she seems more agitated today. They deny any hallucinations or substance abuse. She does not have a history of dysrhythmias or coronary artery disease. She has never had a stress test or undergone cardiac catheterization. Her husband brought the patient’s medication bottles with him. He denies that she has started any new medications, vitamins, or supplements recently.
Past Medical History
Gastroesophageal reflux disease (GERD), hyperthyroidism, arthritis.
Family History
Mother – hypertension, diabetes; Father – hypertension, Coronary Artery Disease, hyperlipidemia.
Surgical History
Cesarean section.
Social History
Nonsmoker, Consumes Alcohol Socially, Denies Intravenous Drug Use (IVDU)
Pertinent Physical Exam
-
Vitals: Heart Rate 160, Blood Pressure 130/74, Oxygen saturation (O2 sat) 98% on room air, Respiratory rate 24, Temperature 102.2 °F/39 °C.
Except as noted below, the findings of the complete physical exam are within normal limits.
-
Head, Ears, Eyes, Nose, and Throat: Normocephalic, atraumatic. Exophthalmos present bilaterally. Ears and nose unremarkable. Neck supple. Enlarged thyroid palpated with nodules.

Exophthalmos. (Image courtesy of Colin Kaide, MD)
-
Cardiovascular: Tachycardic, irregular rhythm. No murmurs . Intact symmetric distal pulses.
-
Pulmonary: Lungs clear to auscultation bilaterally (CTAB), appropriate chest wall excursion. Speaking in slightly shortened sentences secondary to tachypnea at rest.
-
Abdomen: Soft, Nontender/Nondistended, Positive bowel sounds.
-
Extremities: No clubbing, cyanosis, or edema.
-
Neuro: Hyperreflexia noted throughout all extremities. Generally tremulous at rest. No clonus or rigidity. No focal weakness or deficits. Appears anxious and delirious, occasionally staring off during questioning.
-
Skin: Diaphoretic. Thin hair.
Pertinent Diagnostic testing
Lab results | |||
|---|---|---|---|
Test | Results | Units | Normal range |
WBC | 13.3 | K/uL | 3.8–11.0 103 / mm3 |
Hgb | 11 | g/dL | (male) 14–18 g/dL (female) 11–16 g/dL |
Platelets | 212 | K/uL | 140–450 K /uL |
Creatinine | 0.8 | Mg/dL | 0.6–1.5 mg/dL |
Potassium | 4.3 | mEq/L | 3.5–5.5 mEq/L |
Glucose | 146 | Mg/dL | 65–99 mg/dL |
Lactate | 1.0 | Mmol/L | < 2.0 |
Uric acid | 11.6 | Mg/dL | (3.5–7.7 mg/dL) |
Troponin | <0.01 | Ng/ml | < 0.04 |
BNP | 170 | Pg/ml | <100 |
TSH | 0.0003 | μU/mL | Less than 9 μU/mL |
Free T4 | 6 | μU/mL | 5–13 μg/dL |
Chest X-Ray
No acute cardiopulmonary findings.
Computed Tomography Angiogram Chest
No pulmonary embolism identified. No focal consolidation or effusion bilaterally.
Urinalysis and Urine Drug Screen
Negative.
Electrocardiogram
Irregularly irregular rhythm rate of 160 bpm, narrow QRS, unable to identify P waves, nonspecific ST or T wave changes. Consistent with atrial fibrillation with rapid ventricular response.
Emergency Department (ED) Course
Patient’s home medications were brought to the ED by husband and include chondroitin, aspirin, omeprazole, and methimazole. On further discussion with the patient’s husband, he states they were recently traveling out of the country and she forgot to pack her medications, so she had not taken her methimazole for the past 5 days. Due to recent travel and new onset atrial fibrillation (a-fib), computer tomography angiography (CTA) of the chest was obtained to evaluate for pulmonary embolism, which was negative. Vitals were significant for tachycardia and hyperthermia. Labs were relatively unremarkable other than a mild leukocytosis, but she did not have overt signs of infection evident on her physical exam, chest X-ray, or urinalysis. Urine drug screen negative for tested substances. Electrocardiogram (EKG) showed atrial fibrillation with rapid ventricular response (RVR), which was new-onset atrial fibrillation as patient had no history of previous dysrhythmia. Given her history of hyperthyroidism and recent medication noncompliance, a clinical diagnosis of thyroid storm was suspected.
Update 1
Patient was given 1 mg IV propranolol every 15 minutes for heart rate control and 600 mg of oral propylthiouracil (PTU). 1 hour after PTU, 8 drops of Lugol’s solution iodine was administered. She was also given hydrocortisone 300 mg IV and acetaminophen for hyperpyrexia. Blood and urine cultures were drawn. As her medication noncompliance was a reasonable cause of thyroid storm without identified infectious etiologies, broad-spectrum antibiotics were held. On reassessment, patient’s heart rate improved to 138 from 160, her temperature was 98.6 °F/37 °C, she was more alert, oriented times 3, and answering questions appropriately. An admission to ICU was requested.
Learning Points: Thyroid Storm
Priming Questions
-
1.
How do you differentiate between hyperthyroidism and thyroid storm? What is used to make the diagnosis of thyroid storm?
-
2.
If so many people have thyroid dysfunction and hyperthyroidism, which subset of these people develop thyroid storm and who is predisposed?
3. When treating thyroid storm, does the order in which you give the medications make a difference?
Introduction/Background
-
1.
Hyperthyroidism progresses to thyroid storm in approximately 12% of patients [1].
-
2.
Thyroid storm is a life-threatening condition that can lead to end-organ damage and cardiovascular collapse if not treated emergently [2].
-
3.
The cause of progression from hyperthyroidism to thyroid storm is not well defined but is thought to be due to altered peripheral response to thyroid hormone and resulting adrenergic hyperactivity [3].
-
4.
The most common precipitating event of thyroid storm is infection, however, there are other physiologic triggers including burns, diabetic ketoacidosis (DKA), pulmonary embolism (PE), stroke, surgery, trauma, and parturition [4].
-
5.
Thyroid storm has a nonspecific presentation that mimics many other more common ED presentations, thus the physician must maintain a high index of suspicion for the diagnosis.
-
6.
The most common clinical features of thyroid storm are hyperpyrexia, tachycardia, central nervous system (CNS) dysfunction, and gastrointestinal (GI) manifestations [4,5,6].
-
7.
Mortality of thyroid storm is currently reported at 10% [7].
Physiology/Pathophysiology
-
1.
Hyperthyroidism is classically defined as low TSH and elevated free T3 and T4 hormone.
-
The hypothalamus secretes thyroid releasing hormone (TRH), which stimulates release of thyroid stimulating hormone (TSH) from the pituitary. TSH binds receptors on the thyroid cells to stimulate release of thyroid hormone [7].
-
The T4 form of the hormone, thyroxine, is the most prevalent type in circulation; however, triiodothyronine (T3) is the active form that binds nuclear receptors [8].
-
The ratio of T4 to T3 circulating in the blood stream is 20:1 [3].
-
The majority of circulating thyroid hormone is bound to proteins including thyroid binding globulin (TBG), albumin, and transthyretin [7]. The percentage of free hormone determines thyroid activity.
-
T4 undergoes conversion to T3 by 5′ deiodinase. T3 then enters the cells and binds to receptors, which affect gene regulation and transcription [7].
-
-
2.
Excess thyroid hormone has effects including elevated metabolic rate, increased temperature and heart rate, increased cardiac contractility, as well as muscle and CNS excitability.
-
3.
There is no clinical feature or single lab test that distinguishes hyperthyroidism from its more severe form, thyroid storm.
-
Thyroid storm occurs most commonly in patients with underlying Graves’ disease, but may also be seen in patients with toxic multinodular goiter and other causes of elevated thyroid levels [9].
-
-
4.
Thyroid storm is not well understood. It is currently believed that thyroid storm develops when there is upregulation of peripheral thyroid hormone receptors and increased sensitivity to catecholamines.
-
There is no evidence of increased production of T3/T4 in thyroid storm.
-
Typically some preceding stressor occurs which causes increased catecholamines and increased responsiveness peripherally, thus leading to excessive adrenergic response [9].
-
Increased levels of free hormone in circulation (unbound to proteins) contributes to increased adrenergic activity.
-
Multiple factors can interfere with hormone binding and may increase levels of free hormone including burns, trauma, surgery, ketoacidosis, infections, etc. [4]
-
Excess free T3 leads to enhanced beta-adrenergic receptor activity [8].
-
Multiple organ systems are sensitive to the adrenergic response, explaining the most common cause of death from thyroid storm: cardiovascular collapse and multiorgan failure [6, 7].
-
-
5.
Complications of excessive thyroid stimulation most often include cardiovascular pathology such as heart failure or atrial fibrillation.
-
EKG findings typically show sinus tachycardia in 40% of patients and atrial fibrillation in 10% to 35% of patients [9].
-
Clinicians must be aware of an abnormal presentation of thyroid storm in the elderly known as apathetic thyrotoxicosis. Elderly patients may not develop the agitation or CNS excitability, but rather display depressed mental status, anorexia, or lethargy. Their presentation may only be new onset atrial fibrillation or heart failure, thus complicating the diagnosis of thyroid storm even further [10].
-
Thyrotoxic periodic paralysis is a serious and feared complication, but its incidence is only 0.2% in North America. The paralysis is caused by a shift of potassium into the cells, which inhibits muscle function. Treatment with potassium can restore muscle function [8, 11].
-
-
6.
One of the predictors of mortality is total bilirubin level. It has been shown that level >3 mg/dL was associated with significantly higher mortality compared to people with bilirubin <3 mg/dL [2]. This is more specific than just the presence or absence of jaundice.
Making the Diagnosis
Understanding the pathophysiology of thyroid function and excess hormone effects in thyroid storm is the most important factor for making the diagnosis. There is no defining lab test or classic presentation of thyroid storm, so the key is to keep it on the differential in any patient that has a significant past medical history and presents with symptoms of increased sympathetic tone.
The diagnosis of thyroid storm may be challenging and is frequently overlooked. Clinical presentation of these patients is nonspecific and can mimic many other more common ED presentations. The diagnosis is clinical, and there are no routinely reliable lab tests to make the diagnosis [1].
-
1.
The most common signs and symptoms are fever, tachycardia, CNS dysfunction, and GI manifestations [4]. These are not specific for any one condition! We see these presenting symptoms every day in the Emergency Department, and the cause is rarely thyroid storm.
-
2.
The differential for these nonspecific symptoms is broad, including sepsis, heat stroke, meningitis, encephalitis, serotonin syndrome, neuroleptic malignant syndrome, stimulant toxidrome, adrenal insufficiency, pheochromocytoma, and many more.
-
3.
The most important part of making the diagnosis is keeping thyroid storm on the differential and remaining mindful of a patient’s past medical history and current medication list.
-
If the patient has a history of thyroid disorder and presents with the aforementioned symptoms, thyroid storm should always be considered. If suspected, it should be treated in an expeditious fashion, as delay or failure to treat may lead to poor outcomes and death.
-
Be aware that some people may take exogenous thyroid hormone for weight loss purposes; therefore, it is important to consider this during evaluation of patients with hyperthyroid presentations.
-
-
4.
TSH and free T3/T4 levels are not always helpful in the diagnosis of acute phase thyroid storm.
-
T3 and T4 levels may be elevated in thyroid storm, but not always. Therefore, these labs cannot be used to make the diagnosis. Most important out of the thyroid tests is the free concentration of thyroid hormone [4].
-
It has also been proposed that maybe the rapidity of the rise in thyroid hormone, rather than a one-time level, may be a determinant for development of thyroid storm [7, 12].
-
-
5.
Burch and Wartofsky developed a scoring system in 1993 to aid in the diagnosis of thyroid storm. It has been said that the scoring system leads to many false-positive diagnoses due to low specificity [2]. Patients with severe nonthyroidal illness will test positive on this scoring system.
Burch – Wartofsky’s diagnostic criteria | |
|---|---|
Thermoregulatory dysfunction | Scoring points |
37.2–37.7 | 5 |
37.8–38.2 | 10 |
38.3–38.8 | 15 |
38.9–39.4 | 20 |
39.4–39.9 | 25 |
>40.0 | 30 |
Effects on CNS | |
Mild (agitation) | 10 |
Moderate (delirium, psychosis) | 20 |
Severe (seizures, coma) | 30 |
Gastrointestinal and liver dysfunction | |
Moderate (diarrhea, N/V, abdominal pain) | 10 |
Severe (unexplained jaundice) | 20 |
Cardiovascular dysfunction (heart rate) | |
99–109 | 5 |
110–119 | 10 |
120–129 | 15 |
130–139 | 20 |
≥140 | 25 |
Atrial fibrillation | 10 |
Heart failure | |
Mild (peripheral edema) | 5 |
Moderate (bibasilar rales) | 10 |
Severe (pulmonary edema) | 15 |
History of triggering factor | |
Negative | 0 |
Positive | 10 |
-
6.
If thyroid storm is suspected based on history and clinical findings, the provider should begin empiric treatment immediately. This diagnosis is clinical and one should not rely on lab results [14].
-
7.
These patients will always require admission and likely be admitted to the ICU due to the high mortality of the disease process and the propensity for hemodynamic instability and cardiovascular collapse [14].
-
8.
Remember to investigate for any underlying triggers of thyroid storm and begin treatment for these as well. Currently, the most common precipitant is infection [7].
Treating the Patient
Once thyroid storm is recognized, treatment consists of several steps aimed at multiple points of the pathway. The keys to successful treatment include blocking additional thyroid hormone synthesis, inhibiting release of thyroid hormone, antagonizing peripheral effects of catecholamines, inhibiting peripheral conversion of T4 to active T3, and other supportive care directed at hemodynamic status and the inciting event that precipitated the storm. The American Thyroid Association recommends this multimodal approach to all patients in thyroid storm [1, 14, 15].
-
1.
Decrease synthesis of new thyroid hormone.
-
Thionamides , most commonly propylthiouracil (PTU) or methimazole, are used.
-
Typically for hyperthyroidism, methimazole is used because it has less serious side effects compared to PTU, however in the case of thyroid storm, the American Thyroid Association recommends PTU as the first line thionamide [5, 15]. This is because PTU has an added benefit of also inhibiting peripheral conversion of T4 to T3. Dosing includes a 600 mg oral loading dose followed by 250 mg q4 h [7].
-
These medications are given orally; no intravenous form currently exists. If the patient is unable to take the medication orally, they can both be given via nasogastric (NG) tube or rectally via enema.
-
It is appropriate to give thionamides to pregnant patients in thyroid storm. PTU is typically the drug of choice in the first trimester, with methimazole preferred in the second and third trimesters [8, 11, 15]. Methimazole has been associated with teratogenic effects early on in pregnancy, but it is the preferred agent after the first trimester due to the risk of hepatotoxicity from PTU [8, 11].
-
-
2.
Block release of preformed hormone from the thyroid gland .
-
Iodine prevents additional release.
-
It is important to wait 1 hour after administration of a thionamide before giving iodine, as iodine is a substrate for thyroid hormone production. Without blockade of the synthesis of new hormone, iodine administration would contribute to further synthesis of new hormone [9, 12].
-
Once the synthesis pathway is blocked, increases in iodine prevent release of hormone from the gland by the Wolff-Chaikoff effect. The principle states that increasing levels of iodine leads to decreased organification and hormone synthesis [3, 7].
-
Iodine is given in the form of Lugol’s solution or SSKI. Dose is 8 drops of Lugol’s every 6 hours or 5 drops of supersaturated potassium iodide (SSKI) every 6 hours [4, 7]. If the patient has a severe allergy to iodine, lithium can be used instead and has the same effect of decreasing release of hormone [4].
-
Lithium is a second-line agent. The mechanism of action is not clear; however lithium is also known to inhibit the coupling of iodotyrosine during thyroid hormone synthesis. Dosing is 300 mg every 6–8 hours with very close monitoring. The narrow therapeutic index of lithium makes it a less desirable option [4, 7].
-
-
3.
Address the excess thyroid hormone already in circulation.
-
Thyroid hormone in circulation has a half-life of approximately 3–6 days in a thyrotoxic patient [4].
-
Beta-blockade is used to treat the symptoms of increased sympathetic tone. Propranolol is the most commonly used beta-blocker for thyroid storm because it has the additional benefit of inhibiting peripheral conversion of T4 to T3. Dose is either 1–2 mg IV q15 minutes or 60–120 mg PO q6 hours [4, 7].
-
The downside of propranolol is that it has a relatively long half-life and suppresses cardiac contractility, which can worsen heart failure.
-
Alternatives include esmolol, which has the benefit of a shorter half-life and more selective beta blockade, thus less bronchospasm. It can be used as a constant infusion and titrated easily making it an attractive option for the ED setting [7].
-
Beta-blockers are the mainstay of treatment, but patients must be closely monitored for worsening heart failure. Some patients are already in high output heart failure due to their increased cardiac activity and decreased peripheral vascular resistance from thyroid storm. When beta-blockers are added and cardiac contractility is decreased, heart failure can worsen and fluid overload or pulmonary edema can develop rapidly. Echocardiography is recommended when using rate control in patients with thyroid storm [16].
-
Cholestyramine is not a mainstay of treatment, but can be used to bind thyroid hormone and interrupt enterohepatic circulation thus facilitating elimination via the GI tract [4, 7].
-
In severe situations where the patient is not responding to usual treatment within 24–48 hours of initiation, thyroid hormone can be removed from circulation via plasma exchange or dialysis [4, 7, 14, 18]. Plasma exchange removes thyroid binding globulin (TBG) with bound thyroid hormone and replaces it with free albumin, which contains unsaturated binding sites for remaining free thyroid hormone in circulation [7].
-
-
4.
Block peripheral conversion of T4 to T3.
-
Propranolol and PTU both may block peripheral T4 to T3 conversion, however, the most potent blockade of peripheral conversion is from glucocorticoids [7].
-
Stress dose steroids are given; 300 mg hydrocortisone IV loading dose, followed by 100 mg q8 hours [7].
-
Steroids are often part of the treatment algorithm for this reason, as well as helping to counteract adrenal insufficiency in the shock state [4, 6].
-
-
5.
Treat the underlying precipitant of the thyroid storm if one can be identified.
-
The most common precipitant is infection, so obtaining cultures, urinalysis, and chest X-ray are important diagnostics [4].
-
Often these patients will be started on broad spectrum antibiotics until underlying infection is either identified or excluded.
-
Other precipitating causes such as myocardial infarction (MI), pulmonary edema (PE), and diabetic ketoacidosis (DKA) should concurrently be treated using their respective typical standard of care measures.
-
-
6.
Supportive Care
-
Volume resuscitation from fluid losses due to sweating, diarrhea, or vomiting.
-
Normal saline containing dextrose may help combat glycogen depletion from increased metabolic rate [3, 4].
-
Sometimes vasopressors may be needed to maintain an appropriate mean arterial pressure (MAP) in the acute phase.
-
Hyperpyrexia is treated with acetaminophen. Avoid aspirin as it can disrupt binding of thyroid hormone to TBG, leading to increased free hormone levels and worsening of disease! [5, 12]
-
External cooling measures: cool mist, cooling blanket, ice packs, etc.
-
-
7.
Clinicians should keep in mind the pathophysiology of this condition when considering other medication use.
-
Avoid medications that increase sympathetic tone such as ketamine, albuterol, or pseudoephedrine during acute thyroid storm for fear of worsening the adrenergic response [9].
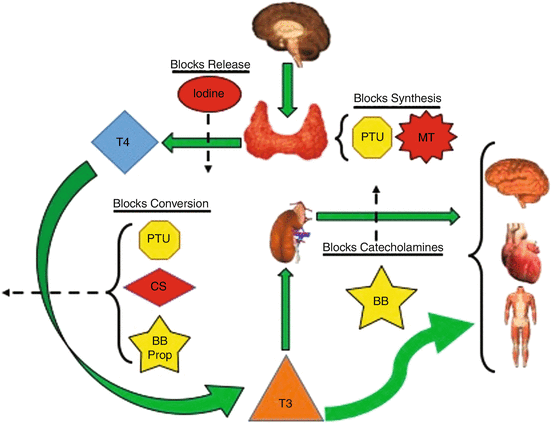 Thyroid Storm Treatment. (Graphic Courtesy of Colin Kaide, MD)
Thyroid Storm Treatment. (Graphic Courtesy of Colin Kaide, MD)
-
Treating thyroid storm | ||
|---|---|---|
Drug | Initial dose | Ongoing dosing |
Propothiouracil | 600 mg PO | 250 mg q4 h |
Methimazole | 20–25 mg PO | 20–25 mg PO q4 h |
Propranolol | 1–2 mg IV q15 min | 60–120 mg PO q6 h |
Iodine Lugol’s solution Or SSKI (potassium iodide) | 8 drops 6 drops | 8 drops q 6 h 6 drops q 6 h |
Hydrocortisone | 300 mg IV | 100 mg q 8 h |
Common Pitfalls
-
1.
Failure to recognize and treat the underlying cause, which leads to persistent thyrotoxicosis [17].
-
2.
Failure to recognize thyroid storm in a patient with history of hyperthyroidism [17].
-
3.
Failure to treat in an expedited fashion [17].
-
4.
Inducing cardiogenic shock from overaggressive beta-blockade treatment to lower heart rate too quickly [17].
Case Conclusion
The patient was treated with PTU, iodine, propranolol, and steroids in the ED and was subsequently admitted to the ICU. Once in the ICU, her blood and urine cultures were monitored and were negative for growth. She remained in the ICU for 3 days and her PTU, steroid, and propranolol were weaned. She was restarted on her methimazole and transferred to the floor.
Discussion
Maintain a high clinical suspicion for this can’t miss diagnosis! For the patient who presents to the ED with hyperthermia, tachycardia, tachypnea, and altered mental status, the differential will be broad. More common causes such as sepsis and heat stroke should always be considered, but beware of anchoring and premature closure.
Review the patient’s past medical history and medication list for diagnostic clues. Strongly consider the diagnosis in patients with hyperthyroidism on baseline PTU or methimazole, but also in patients with hypothyroidism who take thyroid hormone replacement. They can overdose on exogenous thyroid hormone and induce a hyperthyroid state or thyroid storm.
If you suspect thyroid storm, start treating it! This is a clinical diagnosis. If your treatment for sepsis is not working and you find yourself thinking ‘something is not right’, this should be a red flag prompting reconsideration of the diagnosis. Thyroid storm can be rapidly fatal so early and empiric treatment is important. Once it is suspected, begin treatment with thionamides, iodine, beta-blockers, and steroids right away.
Remember the correct order of treatment in order to prevent additional thyroid hormone synthesis. Remember supportive care such as intravenous fluids and antipyretics to maintain blood pressure and normothermia.
Pattern Recognition
•
-
History of Hyperthyroidism or newly diagnosed hyperthyroidism
-
Tachycardia
-
Tachypnea
-
Hyperthermia
-
Altered mental status
References
Ross DS, Burch HB, Cooper DS, et al. 2016 American Thyroid Association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid. 2016;26:1343–421.
Akamizu T, Satoh T, Isozaki O, et al. Diagnostic criteria, clinical features, and incidence of thyroid storm based on nationwide surveys. Thyroid. 2012;22:661–79.
Tintinalli JE, Stapczynski JS, Ma OJ, Cline D, Meckler GD, Yealy DM. Tintinallis emergency medicine: a comprehensive study guide. New York: McGraw-Hill Education; 2016.
Stathatos N, Wartofsky L. Thyrotoxic storm. J Intensive Care Med. 2002;17:1–7.
Bacuzzi A, Dionigi G, Guzzetti L, Martino AID, Severgnini P, Cuffari S. Predictive features associated with thyrotoxic storm and management. Gland Surg. 2017;6:546–51.
Wang H-I, Yiang G-T, Hsu C-W, Wang J-C, Lee C-H, Chen Y-L. Thyroid storm in a patient with trauma – a challenging diagnosis for the emergency physician: case report and literature review. J Emerg Med. 2017;52:292–8.
Chiha M, Samarasinghe S, Kabaker AS. Thyroid storm. J Intensive Care. 2013;30(3):131–40.
Franklyn JA, Boelaert K. Thyrotoxicosis. Lancet. 2012;379:1155–66.
Marx JA, Hockberger RS, Walls RM. Rosens emergency medicine: concepts and clinical practice. Vol 1 & 2. St Louis: Mosby; 2010.
Bhattacharyya A, Wiles PG. Thyrotoxic crisis presenting as acute abdomen. J R Soc Med. 1997;90:681–2.
Leo SD, Lee SY, Braverman LE. Hyperthyroidism. Lancet. 2016;388:906–18.
Yoshida D. Thyroid storm precipitated by trauma. J Emerg Med. 1996;14:697–701.
Sabir AA, Sada K, Yusuf BO, Aliyu I. Normothermic thyroid storm: an unusual presentation. Ther Adv Endocrinol Metab. 2016;7:200–1.
Satoh T, Isozaki O, Suzuki A, et al. 2016 guidelines for the management of thyroid storm from the Japan Thyroid Association and Japan Endocrine Society (first edition). Endocr J. 2016;63:1025–64.
Bahn RS, Burch HB, Cooper DS, et al. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Thyroid. 2011;21:593–646.
Ngo SYA, Chew HC. When the storm passes unnoticed—a case series of thyroid storm. Resuscitation. 2007;73:485–90.
Wolfson AB, Cloutier RL, Hendey GW, Ling L, Rosen CL, Schaider J. Harwood- Nuss clinical practice of emergency medicine. Philadelphia: Wolters Kluwer; 2015.
Deng Y, Zheng W, Zhu J. Successful treatment of thyroid crisis accompanied by hypoglycemia, lactic acidosis, and multiple organ failure. Am J Emerg Med. 2012; https://doi.org/10.1016/j.ajem.2012.01.003.
Disclosure Statement
The authors of this chapter report no significant disclosures.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ferretti, N., Yee, J. (2020). Thyroid Storm: Glands Gone Wild! . In: Kaide, C., San Miguel, C. (eds) Case Studies in Emergency Medicine. Springer, Cham. https://doi.org/10.1007/978-3-030-22445-5_57
Download citation
DOI: https://doi.org/10.1007/978-3-030-22445-5_57
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-22444-8
Online ISBN: 978-3-030-22445-5
eBook Packages: MedicineMedicine (R0)





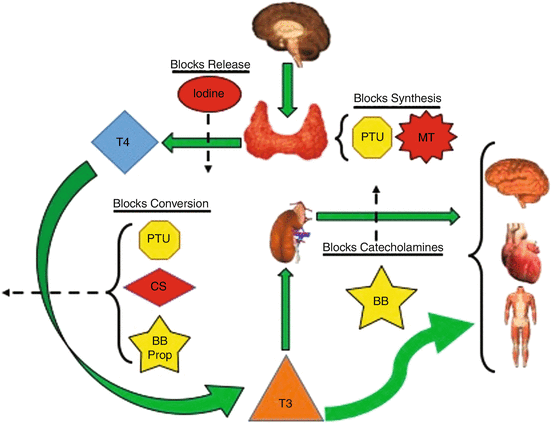 Thyroid Storm Treatment. (Graphic Courtesy of Colin Kaide, MD)
Thyroid Storm Treatment. (Graphic Courtesy of Colin Kaide, MD)