Abstract
Less than 20 years ago, infectious syphilis was on the verge of eradication in the United States. Since that time, however, syphilis rates have increased dramatically in the United States particularly among adolescents and young adults. While young, Black MSM have the highest risk of acquiring syphilis, it is important to keep in mind that rates have increased in adolescents and young adults of every age, gender, and sexual orientation. This chapter examines the changing epidemiology of syphilis as well as the microbiology and pathophysiology and clinical manifestations at different stages of the syphilitic infection. It then goes on to consider current approaches to diagnostic testing, including diagnostic testing algorithms, and treatment of the different stages of syphilis. Prevention and other public health considerations such as syphilis screening are also discussed. The chapter ends with other considerations that affect syphilis and its treatment such as HIV coinfection, pregnancy, and syphilis in MSM.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Case StudyA 17-year-old male presented to the emergency room in a large public hospital, with a chief complaint of sore throat. He was in his usual state of health until 2 weeks prior to presentation, when he noticed the development of bilateral enlarged “bumps” in his groin. A few days later, he developed a sore throat and more swollen glands in his neck, particularly on the right. He initially presented to an urgent care clinic near his home, where a rapid streptococcal antigen test was negative, and he was presumed to have a viral upper respiratory illness. However, his symptoms progressed – leading to the current presentation in the emergency department. Physical examination was notable for temperature of 102 degrees F, right-sided unilateral tonsillitis, 3–4 cm ipsilateral anterior and posterior cervical lymph nodes, and an erythematous macular rash over his trunk and upper extremities, with involvement of the palms and soles. A careful history elicited mention of a painless ulcer near the patient’s anus that persisted for several days approximately 2 months prior to presentation. He also reported occasional episodes of unprotected sexual encounters with male partners (Figs. 11.1 and 11.2).
Questions for Consideration
-
What diagnostic tests should be performed?
-
What risk factors for syphilis does this patient have?
-
What preventative screening should the patient receive in the future?
Epidemiology
Less than 20 years ago, infectious syphilis was on the verge of eradication in the United States. The Centers for Disease Control and Prevention (CDC) published a “National Plan to Eliminate Syphilis from the United States” in 1999, and less than 10,000 cases of primary and secondary syphilis were reported the following year [1]. Since that time, however, syphilis rates have increased dramatically in the United States [2]. In 2015, 23,872 new syphilis cases (including all stages) were reported in the United States – more than doubling in the 15 years since the CDC’s elimination plan was proposed [3].
Rates of syphilis are higher among men, especially men who have sex with men (MSM). Men accounted for 90.3% of all primary and secondary syphilis cases in 2015 [3]. New cases are diagnosed with increasing frequency among young adults; the highest rates of primary and secondary syphilis are now found among young men ages 20–29. This represents a marked epidemiologic shift over the past 10 years; previously, syphilis was much more common among middle-aged men (ages 35–59). Racial disparities are also seen in syphilis – primary and secondary syphilis rates are disproportionately high among Black men: 27.9 in 100,000 compared to 5.4 in 100,000 for White men, although increases among White and Hispanic men have also been noted over the past several years [4]. Additionally, geographic disparities in syphilis prevalence have been documented. The Southeastern United States has the largest proportion of syphilis cases with 41% of cases reported there, although the West has the highest case rate (7.9 cases per 100,000) [10].
Among adolescents and young adults, the incidence of syphilis continues to increase. Between 2014 and 2015, primary and secondary syphilis among young people aged 15–19 increased 10.2%, and among those aged 20–24, rates increased 14.9%. Incidence rates were relatively lower among young women compared to young men (2.8 cases per 100,000 for 15–19-year-old women and 5.1 cases per 100,000 for 20–24-year-old women compared to 8 per 100,000 for 15–19-year-old men and 35.7 per 100,000 for 20–24-year-old men), but the incidence has increased in every sex and age category since 2013 [11]. Thus, while young, Black MSM have the highest risk of acquiring syphilis, it is important to keep in mind that rates have increased in adolescents and young adults of every age, gender, and sexual orientation.
Microbiology and Pathophysiology
Syphilis is a systemic infection with the spirochete Treponema pallidum , subspecies pallidum. Venereal syphilis infection occurs after the spirochete directly penetrates the mucous membranes or enters through the breaches in the skin that result from sexual contact. The first step of infection involves the spirochete attaching to the host cells and extracellular matrix, as it is primarily an extracellular pathogen. The spirochete then multiplies locally and disseminates via the lymphatic system and the bloodstream within minutes of infection. Because the spirochete is long and flat, it can easily penetrate human tissue and vascular structures via an undulating, corkscrew movement. This early and widespread hematogenous dissemination explains the eventual widespread involvement of the disease. The outer membrane of the spirochete lacks both lipopolysaccharide and toll-like receptor 2 (the latter of which can be found beneath the pathogen’s outer membrane); this helps the spirochete to evade detection by the innate immune system and help to explain the lack of systemic inflammation in primary syphilis [12]. Once opsonization occurs, spirochetes are more easily located and destroyed, causing a systemic inflammatory response and tissue damage that leads to the wide variety of clinical manifestations of secondary syphilis. T. pallidum does not appear to secrete any commonly recognized virulence factors. Despite the development of opsonic antibodies, the infection is not usually cleared, and the infection (if untreated) proceeds to the latent stages of the disease. Several mechanisms have been proposed to explain how T. pallidum evades the immune system, but the process is incompletely understood. It is clear, however, that T. pallidum is able to penetrate the central nervous system, the eye, and the placenta, all of which are considered “immune-privileged” areas where the infection can occur. Additionally, the spirochete’s slow metabolism might work to its advantage, allowing it to slowly replicate even in non-“privileged” sites and still remain under the radar of the host’s immune defenses. The factors that induce T. pallidum to begin dividing rapidly once again in some hosts (causing the manifestations of late syphilis) remain uncharacterized [13].
Clinical Manifestations
Syphilis is a chronic infection characterized by three stages of active disease, primary, secondary, and latent. However, syphilis can be asymptomatic, and unobtrusive lesions may go unnoticed; thus, not all patients are aware of having experienced each stage of the disease. The disease can be sexually transmitted only during the primary, secondary, and early latent stages, although vertical transmission can occur during any stage, including latency [14].
Primary syphilis is heralded by a chancre – a painless, indurated, clean-based ulcer – after 2–6 weeks of incubation following direct contact with another person’s infectious lesion. Chancres are most often seen in men at the head of the penis, but can erupt anywhere that direct contact occurred. Chancres have been reported in the vagina, cervix, in and around the rectum, in the mouth, and even on the fingers and neck. The chancre usually heals spontaneously without scarring within 4–6 weeks, although with treatment it will likely regress more quickly (within 2–3 days). Regional lymphadenopathy may or may not be present and may or may not be tender [14].
Around 6–8 weeks after the healing of the chancre, secondary syphilis usually develops. The findings in secondary syphilis include generalized lymphadenopathy, a non-pruritic, maculopapular rash that often involves the palms and soles. However, the rash of secondary syphilis can be highly variable. The rash can be localized or widespread and can manifest as pustular or scaly in appearance (as opposed to the classic maculopapular description). In intertriginous areas (particularly the anogenital region), these lesions can coalesce to from condylomata lata, plaques resembling flat warts. Gray mucus patches may also be found on the oral or genital mucosa. All of these lesions are highly infectious through contact. Flu-like symptoms, such as sore throat, fever, and myalgias, are common. Other end-organ manifestations, including hepatosplenomegaly, hepatitis, nephrotic syndrome, aseptic meningitis, uveitis, and generalized lymphadenopathy, have also been described [12].
If untreated, syphilis can progress to a latent stage. There are no clinical manifestations during this stage, and the disease can only be detected via serologic testing. The latent stage is then subdivided into early, late, and unknown latency. Early latent syphilis occurs within a year of infection – if the date of infection is over a year ago or unknown, the patient is treated as having late latent syphilis. About one-quarter of those in early latency will have a recurrence of secondary syphilis symptoms, usually within the first year [14].
After a variable period of latency, the disease may progress in about one-third of those infected to late manifestations of syphilis such as cardiovascular syphilis, gummas, or tabes dorsalis. Cardiovascular syphilis classically involves the ascending aorta and can cause aneurysms with or without aortic valve insufficiency and coronary artery stenosis. Gummas are granulomatous lesions that can occur anywhere on the body and may include cerebral locations with mass effect or local inflammation. Both cardiac manifestations and gummas have become very rare with the advent of effective antibiotic therapy, and given the long period of latency that usually precedes them, they would be particularly unlikely in adolescent patient population [14].
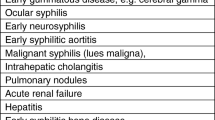
Neurosyphilis can occur at any time during the course of the infection. T. pallidum can be detected in the cerebrospinal fluid (CSF) early in the course of the disease even without symptoms [15]. Other manifestations of neurological involvement can include uveitis and cranial nerve palsies. Syphilis can also cause an aseptic meningitis or meningovascular syphilis, a type of inflammatory arteritis that can cause headaches, movement disorders, and behavioral changes, and even strokes and seizures later on. During late syphilis, general paresis or tabes dorsalis can occur. General paresis can cause progressive dementia, seizures, psychosis and other psychiatric manifestations. Tabes dorsalis, which involves damage to the posterior column of the spinal cord, presents as ataxia from loss of proprioception and sharp, radicular pain. The signs of tabes dorsalis include the Argyll Robertson pupil (pupil accommodates but does not react to light), loss of vibratory sensation, and loss of reflexes [14].
Ocular syphilis is another serious manifestation of syphilis that can occur either in the presence or absence of other nervous system involvement [15]. Symptoms may include eye redness and blurry vision that can progress to vision loss. Retinitis, optic neuritis, and retinal detachment can also be seen.
Diagnostic Testing
T. pallidum cannot be cultured. Diagnostic testing therefore relies on either direct detection using dark-field microscopy or tests to detect T pallidum from lesion exudate. Dark-field microscopy is a technically difficult test and therefore is rarely performed. A presumptive diagnosis of syphilis is made with a combination of serologic tests used for screening and confirmatory testing.
Serologic tests can be divided into treponemal and non-treponemal tests. The non-treponemal tests, such as the rapid plasma reagin (RPR) and Venereal Disease Research Laboratory (VDRL) tests, are usually used for screening purposes. The non-treponemal tests detect the presence of an immune system product that is produced in response to an infection with T. pallidum (a non-specific cardiolipin-cholesterol-lecithin reagin antigen). False positives are a concern and are more likely in the setting of autoimmune disease, viral infections, pregnancy, intravenous drug use, advanced malignancy, tuberculosis, malaria, and rickettsial diseases. Persons with a reactive non-treponemal test should receive a treponemal test for confirmation [16].
The treponemal tests detect antibodies to T. pallidum. There are several treponemal IgG tests commercially available, and some of these tests can also detect false-positive treponemal tests that can occur but a false-positive reaction to both treponemal and non-treponemal tests is uncommon. The serologic diagnosis of syphilis relies on the combination of a reactive non-treponemal test and treponemal test [17].
In the usual sequence of syphilis serologic testing, a non-treponemal test (RPR or VDRL) is performed followed by a treponemal test. However, some clinical laboratories use a reverse sequence algorithm, or screening with a treponemal test followed by a non-treponemal test. If the treponemal test is positive, but the non-treponemal test is negative, a second treponemal test is then recommended. If the second treponemal test is positive but the patient has a past history of treated syphilis, then no treatment is required, unless there is a concern for re-exposure. If a patient was previously unaware of any history of syphilis, then the patient should be treated for late latent syphilis. The use of this reverse sequence algorithm may be more likely to diagnose early primary, previously treated, or long-standing untreated syphilis, all of which can be associated with a negative RPR (Fig. 11.3) [18].
Treatment
Syphilis is treated with parenteral penicillin G, regardless of the stage of the infection. Despite the fact that penicillin has been used to treat syphilis for more than 60 years, there has never been a documented case of penicillin resistance [5]. In very typical cases, treatment should be initiated based on clinical suspicion alone before laboratory results are available, because early treatment of syphilis helps to prevent further transmission [19].
For primary, secondary, or early latent syphilis, a single dose of 2.4 million units IM is given. Alternatives to penicillin include doxycycline (100 mg PO twice daily for 2 weeks) and ceftriaxone (1–2 g parenterally daily for 10–15 days), although data are limited on the optimal dose and duration of ceftriaxone. Azithromycin has documented efficacy against early syphilis; however, due to concerns about underlying resistance, it is not a recommended treatment option [5].
Late latent syphilis or syphilis of unknown duration is treated with 2.4 million units of benzathine penicillin G IM once a week for 3 weeks [18]. Again, doxycycline and ceftriaxone may be used as alternatives, although the optimal dose and duration of ceftriaxone are not known [5]. There is pharmacologic evidence to guide clinicians if a patient misses a dose, but clinical experience suggests that an interval of 10–14 days between doses may be acceptable [20].
After treatment, patients should receive follow-up non-treponemal testing and clinical evaluation at 6 and 12 months after treatment of early syphilis, as these tests reflect disease activity. Based on serologic testing, a fourfold decrease in the titer at 6–12 months after treatment is considered an appropriate decline. Those patients whose titers do not decrease fourfold may have treatment failure or a titer that is serofast. Further clinical evaluation and a CSF evaluation may be required [20].
In some cases, titers of non-treponemal antibodies decline, but the test never reverts to nonreactive. The serofast state may be explained by variability of host antibody response to infection, persistent low-level infection, and a false-positive non-treponemal test. After treatment of early syphilis, approximately 15–41% can remain in a serofast state after treatment. Re-treatment does not appear to benefit these individuals if there is no evidence of reinfection [5].
In patients with tertiary syphilis, a CSF analysis is warranted to evaluate for neurological involvement. If the CSF testing is negative for syphilis, then treatment for late latent syphilis – 2.4 million units of penicillin G IM once a week for 3 weeks – is recommended [17]. These patients should also be tested for HIV infection [20].
In the case of neurological, ophthalmologic, or audiologic symptoms during any stage of syphilis, lumbar puncture is required to evaluate for central nervous system involvement. Involvement of the central nervous system which includes ocular and auditory symptoms warrants intravenous penicillin because benzathine penicillin cannot reach sufficient concentration in the CSF. Intravenous aqueous crystalline penicillin G is used, 18 million to 24 million units per day in continuous infusion or divided into 6 daily doses for 10 to 14 days.
The Jarisch-Herxheimer reaction is an acute reaction that sometimes occurs following treatment of syphilis. It can occur with any antimicrobial but is most common after penicillin. It can occur in 10 to 35% of patients treated for syphilis [5]. Its symptoms, which usually occur within the first 24 hours of treatment, include fever, myalgias, and headache. Because the spirochete burden is highest in early syphilis, and the reaction is caused by the release of inflammatory factors from the killed organisms, the reaction most commonly occurs at that stage. Symptomatic treatment may be needed to support the patient through this brief but uncomfortable reaction [18].
Sexual partners of patients diagnosed with primary, secondary, and early latent syphilis should be treated for syphilis as well, regardless of their test results, if they had intercourse with the patient in the 90 days prior to diagnosis. If the intercourse occurred more than 90 days prior to diagnosis, treatment should be based on the results on serologic testing. The sexual partners of those patients with late latent and tertiary syphilis only require serologic testing if they are long-term partners of the patient, because the infection is not usually transmitted sexually during those stages. Those sexual partners should then be treated based on their test results. If the titers are high and the patient and sexual partner belong to a high-risk population, the sexual partner should be treated presumptively for early syphilis [18].
Prevention
Prevention of syphilis follows similar guidelines as those established for other sexually transmitted infections. Strategies include as screening of high-risk individuals and immediate treatment of the individuals and their partners. Additionally, the role of the health department in controlling syphilis outbreaks via mandatory notification programs should be emphasized. Barrier contraception (e.g., condoms) is also a useful prevention strategy.
Screening and treating are effective forms of prevention in high-risk populations. The United States Preventive Services Task Force (USPFTF) updated their screening recommendations for syphilis in asymptomatic, nonpregnant adults in 2016. Syphilis screening is recommended in high-risk populations, such as MSM and persons living with HIV, and should be screened periodically (Grade A recommendation). Additional risk factors to consider include a history of incarceration, commercial sex work, geography (metropolitan centers in the Southeastern and Western United States), race/ethnicity, and being a male younger than 29 years. However, the optimal interval for screening has not been well established. Initial studies do suggest that detection increases when the interval is increased to 3 months from once a year in high-risk individuals [10]. Similarly, the CDC recommends at least annual screening in sexually active MSM and persons living with HIV, with more frequent screening depending on ongoing risk behavior. Screening for syphilis should also be considered in correctional facilities based on local epidemiology and institutional prevalence [20].
The USPSTF and the CDC have several further recommendations for syphilis prevention. First, high-intensity behavioral counseling for all sexually active adolescents to prevent sexually transmitted infections is recommended [19]. The USPSTF also notes that, in the case of syphilis prevention, the role of local health departments and public health agencies is critical. Investigating incident cases and finding and treating partners are imperative in controlling the spread of syphilis. Primary care providers should also be aware of local laws regarding reporting to public health officials [10].
Condoms are only effective at preventing transmission of syphilis if the condom covers the chancre. Promotion of condom use is still helpful to decrease syphilis rates, however, as currently only 56.9% of teenagers report that they used a condom during their last episode of sexual intercourse [21]. Like other ulcerative sexually transmitted infections, syphilis can be transmitted via oral and digital sex. In fact, one observational study in MSM found that 13.7% of syphilis cases were contracted via oral sex [21]. Thus, condoms, dental dams, female condoms, and other barrier forms of STI prevention should be encouraged.
Unfortunately, there is no vaccine for syphilis. A vaccine using irradiated T. pallidum has been shown to provide protection from infection in animal models. Recent articles have suggested that syphilis would be a prime candidate for further vaccine research, but no vaccine has made it to human trials [22].
Other Considerations
HIV Coinfection
Syphilis and HIV are closely interrelated and have been so since the beginning of the AIDS epidemic. Worldwide, 9.5% of people living with HIV are reported to have syphilis [23]. Ever since the early 1990s, syphilis has been considered a risk factor for HIV infection both because of facilitated transmission [24] and overlapping risk factors and behaviors [25]. For these reasons, persons living with HIV should be screened for syphilis at least annually as part of their routine care, although more frequent screening can be performed based on the assessment of risk behaviors [20].
Syphilis is often associated with high-risk sexual behavior and HIV coinfection. HIV coinfection has been reported as high as 50–70% among MSM diagnosed with primary or secondary syphilis [5]. In individuals living with HIV, the presentation of syphilis is highly variable. Primary and secondary stages of syphilis may overlap, and the cutaneous manifestations may range from impressive to relatively asymptomatic [26].
Data from before the 1980s and 1990s (prior to the advent of highly active combination HIV therapies) suggests that HIV coinfection presents an increased risk for progression to neurosyphilis with a shorter latency period. However, effective treatment of HIV appears to reduce this risk. Subsequent serologic testing should occur more frequently in people with HIV (e.g., at 3, 6, 9, 12, and 24 months) [5].
Finally, if the individual with HIV is severely immunocompromised, initiation of treatment of the HIV with antiretrovirals can result in immune reconstitution syndrome in those persons with undiagnosed syphilis; however, this is uncommon [26].
Pregnancy
Recent reports indicate an increase in syphilis in women in the United States and globally [27]. In utero transmission of syphilis can have effects in the developing fetus that range from silent to severe consequences. Fetal loss and stillbirth occur more frequently in infected mothers. However, two-thirds of infants with maternally acquired syphilis are asymptomatic at birth. Symptoms most commonly appear during the first 3 months of life, including rash, hepatosplenomegaly, neurosyphilis, pneumonitis, failure to thrive, blood-tinged nasal discharge, meningitis, and pseudoparalysis due to long bone damage. Late congenital syphilis, in which symptoms appear after the age of two, involves gummas on the nasal septum, hard palate, as well as the skull and tibias, resulting in saber shins. Teeth and jaw bone deformities lead to Hutchinson incisors, mulberry molars, rhagades, and bulldog facies. Tabes dorsalis and other manifestations of neurosyphilis may occur even into adolescence. Blindness due to interstitial keratitis and sensorineural deafness may also occur [27]. Because of these significant ramifications, it is of vital importance to treat syphilis immediately during pregnancy.
Primary and secondary syphilis carry the highest risk for vertical transmission, but even with late latent syphilis and low titers, the risk of transmission is still significant. The only recommended treatment during pregnancy is penicillin G, so women with penicillin allergy should undergo desensitization. Some evidence suggests that additional therapy can be beneficial in the case of pregnancy, so in early syphilis, a second dose can be given 1 week after the first. Missed doses are unacceptable given the severe consequences of vertical transmission, and so treatment should be reinitiated from the beginning of the series following any missed dose. Follow-up testing should occur at 28–32 weeks, as well as at delivery [19]. Despite the risk of the Jarisch-Herxheimer reaction provoking early labor or fetal distress, treatment should not be delayed or withheld because of the potential for this reaction causing harm to the developing fetus [5].
MSM
The increase in syphilis among MSM has been attributed to several different factors, including a decrease in safer sex practices, changing harm reduction/HIV prevention strategies, the increased use of online social networks to find sexual partners, decreasing mortality due to HIV, and decreased funding for STI prevention [6]. The decline in safer sex practices particularly among MSM has been ascribed to HIV prevention fatigue, optimism regarding HIV treatment, and an increase in recreational drug use among MSM, particularly methamphetamines. Harm reduction strategies like serosorting (choosing sex partners based on HIV status in order to have unprotected sex) and pre-exposure prophylaxis (PrEP) are somewhat effective against preventing HIV but do not decrease transmission of other STIs like syphilis [7]. Online social networks and dating apps have increased the pool of sex partners and may facilitate anonymous sex [8], which in turn makes it more difficult to treat sexual partners once syphilis is diagnosed. Additionally, because of overlapping risk factors, the decrease in mortality due to HIV has increased the size of the population at risk for syphilis [9]. Finally, funding for STI prevention has not kept pace with the increasing incidence. States have experienced budget cuts for STI prevention services, and HIV, while an important cause, has decreased spending in other STI prevention efforts [6]. All of these factors combined have contributed to the resurgence of syphilis in the United States [2].
Although general screening for syphilis in asymptomatic individuals is not recommended, the CDC does recommend that young MSM be screened for syphilis at least annually. Increased syphilis screening practices have demonstrated a doubling of the detection of early syphilis, although the majority of syphilis diagnoses are in patients who sought care for symptoms. Screening is especially important because primary syphilis, like all ulcerative sexually transmitted infections, facilitates HIV infection [20].
WSW
Men who have sex with men are certainly at the highest risk for syphilis infection, but other transmission between women who have sex with women (WSW) has been reported, likely through oral sex [20]. As noted above, rates are relatively low but still increasing among young women [11], so providers should emphasize that risk still exists for WSW (as well as heterosexual women).
Case Conclusion
The patient’s RPR was reactive at 1:32 and a treponemal IgG was positive. These serologic tests in combination with his clinical presentation is consistent with secondary syphilis. Intramuscular benzathine penicillin (2.4 million units) was administered per national guideline recommendations. His symptoms began to resolve after the penicillin injection, and after 2 days, he was afebrile with resolving odynophagia and rash. When he returned to clinic 8 days later, his lymphadenopathy and tonsillitis had completely resolved.
Despite having well-described, classic symptoms, syphilis was coined “the great imitator” by Sir William Osler for its ability to manifest in unexpected ways. A handful of case reports of syphilis presenting as tonsillitis have been reported in the literature. Cases of syphilitic tonsillitis have been associated with both secondary and late syphilis. Both bilateral and unilateral tonsillitis have been described. In particular, syphilitic tonsillitis appears to be unusually common in the HIV+ MSM population.
Syphilis is highly contagious but it is also easily treated. Avoidance of late complications of syphilis is dependent on its early detection. Syphilis screening should be performed regularly in all high-risk populations, including sexually active adolescents and young adults, and particularly young MSM.
References
Centers for Disease Control and Prevention. The national plan to eliminate syphilis from the United States. Atlanta: U.S. Department of Health and Human Services; 1999.
Cohen SE, Klausner JD, Engelman J, Philip S. Syphilis in the modern era. Infect Dis Clin N Am. 2013;27(4):705–22.
Centers for Disease Control and Prevention. 2015 Sexually transmitted diseases surveillance. http://www.cdc.gov.proxy.library.emory.edu/std/stats15/syphilis.
Morbidity and Mortality Weekly Report (MMWR). Primary and Secondary Syphilis — United States, 2005–2013. 2014;63(18):402–6.
Clement ME, Okeke NL, Hicks CB. Treatment of syphilis: a systematic review. JAMA. 2014;312(18):1905–17. https://doi.org/10.1001/jama.2014.13259.
Clement ME, Hicks CB. Syphilis on the rise: what went wrong? JAMA. 2016;315(21):2281–3. https://doi.org/10.1001/jama.2016.7073.
Truong HM, Kellogg T, Klausner JD, Katz MH, Dilley J, Knapper K, Chen S, Prabhu R, Grant RM, Louie B, McFarland W. Increases in sexually transmitted infections and sexual risk behaviour without a concurrent increase in HIV incidence among men who have sex with men in San Francisco: a suggestion of HIV serosorting? Sex Transm Infect. 2006;82(6):461–6.
Rosser BR, Oakes JM, Horvath KJ, Konstan JA, Danilenko GP, Peterson JL. HIV sexual risk behavior by men who use the Internet to seek sex with men: results of the Men’s INTernet Sex Study-II (MINTS-II). AIDS Behav. 2009;13(3):488–98. https://doi.org/10.1007/s10461-009-9524-3.
Chesson HW, Dee TS, Aral SO. AIDS mortality may have contributed to the decline in syphilis rates in the United States in the 1990s. Sex Transm Dis. 2003;30(5):419–24.
US Preventive Services Task Force (USPSTF). Screening for syphilis infection in nonpregnant adults and adolescents: US Preventive Services Task Force Recommendation Statement. JAMA. 2016;315(21):2321–2327. https://doi.org/10.1001/jama.2016.5824.
Centers for Disease Control. Sexually transmitted diseases in adolescents and young adults 2015. http://www.cdc.gov/std/stats14/adolescents.htm
Radolf JD, Deka RK, Anand A, Šmajs D, Norgard MV, Yang XF. Treponema pallidum, the syphilis spirochete: making a living as a stealth pathogen. Nat Rev Microbiol. 2016;14(12):744–59.
LaFond RE, Lukehart SA. Biological basis for syphilis. Clin Microbiol Rev. 2006;19(1):29–49.
Hook EW. Syphilis. The Lancet. Published Online December 16, 2016. https://doi.org/10.1016/S0140-6736(16)32411-4.
Lukehart SA, Hook EW, Baker-Zander SA, Collier AC, Critchlow CW, Handsfield HH. Invasion of the central nervous system by Treponema pallidum: implications for diagnosis and treatment. Ann Intern Med. 1988;109:855–62.
Oliver SE, Aubin M, Atwell L, Matthias J, Cope A, et al. Ocular syphilis – eight jurisdictions, United States 2014-2015. MMWR. 2016;65(43):1185–8.
Clement ME, Hicks CB. RPR and the serologic diagnosis of syphilis. JAMA. 2014;312(18):1922–3. https://doi.org/10.1001/jama.2014.2087.
Eickhoff CA, Decker CF. Syphilis. Sex Transm Dis. 2016;62(8):280–6. https://www.ncbi.nlm.nih.gov/pubmed/27091635/.
Morsheda MG, Singhb AE. Recent trends in the serologic diagnosis of syphilis. Clin Vaccine Immunol. 2015;22(2):137–47.
Workowski KA, Bolan GA, Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64:RR–03):1-137.
Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Hawkins J, Queen B, Lowry R, O’Malley Olsen E, Chyen D, Whittle L, Thornton J, Lim C, Yamakawa Y, Brener N, Zaza S. Youth risk behavior surveillance — United States, 2015. Surveillance Summaries. 2016;65(6):1–174.
Cameron CE, Lukehart SA. Current status of syphilis vaccine development: need, challenges, prospects. Vaccine. 2014;32(14):1602–9. https://doi.org/10.1016/j.vaccine.2013.09.053.
Kalichman SC, Pellowski J, Turner C. Prevalence of sexually transmitted co-infections in people living with HIV/AIDS: systematic review with implications for using HIV treatments for prevention. Sex Transm Infect. 2011;87:183–90. https://doi.org/10.1136/sti.2010.047514.
Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Inf. 1999;75:3–17.
Otten MW Jr, Zaidi AA, Peterman TA, et al. High rate of HIV seroconversion among patients attending urban sexually transmitted disease clinics. AIDS. 1994;8:549–53. https://doi.org/10.1097/00002030-199404000-00020.
Mayer K. HIV and syphilis. Int J Infect Dis. 2016;45:67.
Braccio S, Sharland M, Ladhani SN. Prevention and treatment of mother-to-child transmission of syphilis. Curr Opin Infect Dis. 2016;29(3):268–74.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Goodstein, E., Workowski, K. (2020). Syphilis in Adolescents and Young Adults. In: Hussen, S. (eds) Sexually Transmitted Infections in Adolescence and Young Adulthood. Springer, Cham. https://doi.org/10.1007/978-3-030-20491-4_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-20491-4_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-20490-7
Online ISBN: 978-3-030-20491-4
eBook Packages: MedicineMedicine (R0)