Abstract
Being devoid of direct blood, lymph, and nerve supply, articular cartilage defects pose a major challenge to regenerate. Cartilage once damaged usually heals by formation of fibrocartilage rather than a mechanically more compliant hyaline tissue. Numerous surgical techniques currently available have failed to address the issue. The cartilage tissue engineering incorporating stem cells, relevant growth factors, and scaffolds is considered to carry the potential to overcome the limitations associated with the currently available surgical methods. Mesenchymal stem cells (MSCs), being readily available with no associated ethical issues and a potential to differentiate into chondrocytes enhanced by the application of different growth factors and scaffolds, are considered for effective repair of articular cartilage. However, cartilage tissue engineering is in its infancy due to the lack of sufficient evidences of effective cartilage rehabilitation. The discrepancies in the cell culture methods, concentrations, type of growth factors, and their doses and type of the scaffolds demand further studies in the area. In addition, the clinical studies comparing established surgical techniques and tissue engineering techniques need attention. This review focuses on the role of MSCs, growth factors, and scaffolds in light of the in vitro as well as in vivo studies (preclinical as well as clinical studies) of the articular cartilage repair.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
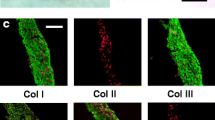
The articular cartilage, a connective tissue with characteristic structural, biochemical, and metabolic features, furnishes an exceptional resiliency and almost frictionless movement to the diarthrodial joints [1]. The average articular cartilage thickness is at the most a few millimeters with knee thickness being 0.3 mm in rabbits, 0.4–0.5 mm in sheep, 0.6–1.3 mm in dog, 0.7–1.5 mm in goats, and 1.5–2.0 mm and 2.2–2.5 mm in humans. Among the commonly used animals for preclinical studies, horse knee cartilage thickness has closest approximation to human knee cartilage followed by goats [2]. Its composition as well as thickness even vary from joint to joint and with age among species [3]. In general, articular cartilage constitutes three layers/zones with the deep zone separated from subchondral bone by a wavy calcified zone known as tidemark (Fig. 18.1). The three zones bear unique arrangement of matrix and cells. In the superficial zone, the cells are flattened disc-like, while in deeper zones the cells appear more rounded. Collagen arrangement appears parallel to the surface in superficial zone, while it becomes random in middle zone and perpendicular in deep zone. The main proteoglycan, aggrecan, content in superficial zone is limited, while in deeper zone it constitutes a major portion. The tissue ingredients in decreasing order of their concentration include water (approximately 75%), collagen especially type II (15%), proteoglycans (10%), and chondrocytes (<2%) [4]. The collagen provides the tissue strength while the proteoglycans provide functional resistance against compression [5]. The resident cells, chondrocytes that reside in lacunae singly or in groups (cell nests), occupy less than 10% of the tissue. The cells maintain tissue homeostasis through mechanical links generated from extracellular matrix (ECM) via cell surface receptors known as integrins [6]. In addition, the growth factors/cytokines act upon chondrocytes and/synovial cells to secrete proteinases such as aspartic/cysteine/serine and metalloproteinases for tissue homeostasis (Fig. 18.2). Among various proteinases, currently, matrix metalloproteinases that degrade all elements of ECM are considered to carry arthritic degeneration potential [7].
Cartilage is a highly differentiated tissue devoid of any direct blood, lymph, or nerve supply and with a scarce number of less proliferative chondrocytes [8, 9]. Articular cartilage upon damage carries limited regeneration potential. The injury in the form of defects is generally divided into partial- and full-thickness defects with the former confined to the tissue itself and the latter penetrating subchondral bone [10]. Partial-thickness defects do not heal spontaneously as the lesion remains devoid of fibrin clot and thus reparative stem cells. The defects are analogous to fissures or clefts seen in early stages of osteoarthritis [11]. Full-thickness defects though heal spontaneously but with a fibrous tissue that is weaker in structural and mechanical competence [11,12,13,14,15]. Osteoarthritis is a progressive erosion of articular cartilage with about 21.4% of the humans [16] and 20% of dogs [17] affected. The exact pathophysiological basis of osteoarthritis is still disputed but the cardinal signs include inflammation and pain, and the pathognomonic radiological features include articular cartilage thinning characterized by decreased joint space, sclerosis, and osteophyte formation [18, 19]. The pain and subsequent loss of functional activity that arise from an insult to the cartilage and its advancement into osteoarthritis demand advanced techniques for better cartilage rehabilitation [11, 12, 14, 20, 21].
To date no repair procedure has been able to heal the cartilage defects to a satisfactory level. Immediately post-injury the local death of cells hampers matrix production that may integrate with the native tissue. The main aim remains to repair the defects by true hyaline cartilage that has seamless local integration. Numerous invasive procedures such as microfracture [22], subchondral bone drilling [23], lavage, debridement and perichondral arthroplasty [24], periosteal arthroplasty [25], autologous osteochondral transplantation [26], autologous chondrocyte implantation [12, 27, 28], and application of autogenic cancellous bone graft [29, 30] have been attempted for cartilage rehabilitation. The techniques, however, lack true hyaline cartilage repair potential besides being limited to small/medium focal sized osteochondral defects [31]. Autologous chondrocyte implantation (ACI) , currently better among the lot, has drawbacks in the form of limited chondrocyte source availability, proneness of the cells to dedifferentiate to fibroblasts, and degeneration in pre-damaged cartilage [32, 33]. In addition, the ageing chondrocytes show declining mitotic and synthetic activity, and synthesize smaller and less uniform aggrecan molecules bearing less functional link proteins [34].
Currently, tissue engineering is being employed to achieve better cartilage rehabilitation. For successful cartilage tissue engineering, various components are required such as cells, growth factors, and three-dimensional matrices. Appropriate cells like autologous chondrocytes or autologous or allogenic stem cells may be implanted. Most of the cell-based therapies currently utilize chondrocytes (approx. 80%), while stem cells constitute only 15% [35]. The limitations associated with ACI mentioned above demand other cell types like stem cells, which are considered to be immunosuppressive. Growth factors incorporated by either viral/nonviral vectors, nucleofection, or direct delivery may regulate directed differentiation. However, the growth factors such as bone morphogenetic proteins (BMPs) direct both bone and cartilage formation and thus need to be regulated at particular step towards chondrogenic lineage [36]. The cells should be implanted on three-dimensional matrices that support the growth and prevent hazardous effect of local environment [10]. Scaffolds, either natural or synthetic, however, bear limitations like early degradation, lack of sufficient porosity, and non-supportive cell growth, and thus the scaffolds that mimic the desired properties of both and exclude the limitations are in demand.
2 Mesenchymal Stem Cells
Stem cells (SCs), characterized by the properties of self-renewal, multiplication, immunomodulation, and multi-lineage differentiation potential, are present in almost all the adult tissues of an individual to maintain normal cells, and thus tissue matrix turnover [10, 37]. The stem cells are of various types such as pluripotent (embryonic SCs, and induced pluripotent SCs) or multipotent (mesenchymal stem cells) based upon their potential to differentiate (Fig. 18.3). Pluripotent stem cells carry extended potential to act multipurpose research and clinical tools to understand and model diseases, develop and screen candidate drugs, and deliver cell replacement in regenerative medicine including cartilage [38]. However, limitations in the form of uncontrolled forced expression (iPSCs), and teratogenic effects and ethical issues (iPSCS/ESCs), have restricted their clinical applications [39, 40]. Currently, mesenchymal stem cells (MSCs) carry maximum share among all stem cells both in preclinical and clinical settings in human and veterinary medicine. The cells are easily available, are capable to differentiate, and secrete certain factors that modulate inflammation and promote healing, and in comparison to pluripotent stem cells they have minimal teratogenic and ethical issues associated [39, 41]. The cells are differentiated as per the available local niche/microenvironment and thus contribute to tissue repair or regeneration. Mesenchymal stem cells implanted into osteochondral defects differentiate into chondrocytes [42,43,44], while MSC-derived cartilage pellets if implanted subcutaneously either disappear [45] or calcify upon vascular invasion [32]. This indicates the role of microenvironment plausibly through cell-surface receptor stimulation by growth factors, extracellular matrix, or direct interaction with surface receptors of other resident cells (chondrocytes) [46,47,48]. Currently, MSCs are believed to largely act therapeutically by releasing a diverse array of cytokines, growth factors, chemokines, and immunomodulatory proteins, though they may also achieve terminal differentiation [49]. Despite the studies that show immunomodulatory potential of MSCs, two recent studies in equines demonstrated development of allo-MSC antibody [50, 51]. One of the studies even showed that the MHC-mismatched MSCs underwent targeted death due to the activation of complement-dependent cytotoxicity. Thus, cautioning about some potential adverse effects that may ensue in addition to the reduced therapeutic efficacy on application of allogenic MSCs [50]. Lack of in-depth understanding in the area demands further steps that need to be deliberated to understand the mechanism(s) behind such differentiation and thereby controlled cell applications.
MSCs that carry maximum share in therapeutics may be derived from almost all the adult tissues (Fig. 18.3) including bone marrow, adipose tissue, embryonic tissue, synovial fluid and membrane, umbilical and peripheral blood, umbilical cord vein, Wharton’s jelly, periosteum, muscle, heart, dental pulp, gingiva, periodontal ligament, and mammary tissue [52], each of which carries the potential to differentiate into chondrogenic lineage [36]. Among all the above mentioned sources the most commonly utilized stem cell sources for therapeutics so far have been bone marrow and adipose tissue [53].
Chondrogenic potential of MSCs was first evaluated under in vitro conditions in 1998 employing transforming growth factor-β (TGF-β) and dexamethasone [54]. Further investigations employing various other growth factors such as bone morphogenetic proteins (BMPs), insulin-like growth factor-1 (IGF-1) , and parathyroid hormone-related peptide (pTHRP) showed enhanced MSC chondrogenesis [54,55,56,57]. However, the in vitro micromass culture method used in such studies may not produce tissue comparable to the native one as the process does not mimic the developmental sequences that actually occur during fetal development. A thorough understanding of embryonic development of the concerned tissue and biological features of the implanted cells is a must-learn criterion for successful cartilage tissue engineering [10]. Recently, under in vitro conditions cartilage tissue was generated approaching hyaline cartilage in physiologic stratification and biomechanical features. This could only be done after recapitulating various developmental processes of mesenchymal condensation via TGF-β1 [58, 59]. The various processes involved include MSC condensation into cellular bodies and condensed mesenchymal cell bodies (CMBs) followed by chondrogenic differentiation that leads to cartilaginous tissue formation. The CMBs under in vitro conditions have been able to generate tissue comparable to native cartilage on osseous tissue surface and also developed mechanically strong cartilage-to-cartilage tissue interface with complete integration [60].
Variations in MSCs’ chondrogenic potential have been observed with respect to their source, culture periods, and age of the donors [53]. Among MSCs from various sources, synovial derived MSCs had better chondrogenic potential and led to formation of a large and heavy cartilage pellet compared to BM-MSCs, AD-MSC, Periosteal-MSC and M-MSCs [61]. In another study that compared BM-MSCs and AD-MSCs, the frequency of colony-forming units reportedly had been three times in the latter compared to the former [62]. In elderly patients, the differentiation potential and proliferation capacity of MSCs are reduced and may affect the healing outcome. The immunomodulation property of MSCs may allow allogenic cells to be used [63, 64]. MSCs are able to maintain their differentiation potential for limited periods with long ex vivo-cultured MSCs manifesting reduced chondrogenic matrix formation, undesired mineralization, and rapid cell death after implantation [32, 65]. The reduced cell population may be compensated by implantation of higher cell density for better cartilage healing as reported in some studies [66, 67]. But it may be noted that higher cell density has chances of more cell apoptosis and thus more inflammation at the site.
3 Growth Factors
In healthy cartilage environment various growth factors work either individually or in combination to complement each other for maintenance of cartilage homeostasis [68]. The main roles played by the growth factors are to promote MSC differentiation towards chondrogenic lineage, stimulate chondrocytic matrix synthesis, and decrease catabolic effect of MMPs and cytokines such as interleukin-1 [10, 69,70,71]. The factors act either at earliest phases to promote chondrocyte proliferation and differentiation like TGF-β [72] or at later stages to promote chondrocyte differentiation rather than initiation of maturation like BMP-2, BMP-4, BMP-6, and TGFβ-3 [73, 74]. To promote MSC differentiation towards chondrogenic lineage, BMP-2 appears superior but has the tendency to promote differentiation towards hypertrophy and osteogenesis characterized by type X collagen and Runx2 expression [72]. Similarly, high intraarticular doses of TGF-β1 have been reported to induce chemotaxis and activation of inflammatory cells tending towards fibrosis and osteophyte formation [72]. To address this issue, combinations of the growth factors have been used either to reduce the activity of each other at certain stage or to complement each other’s physiological function. One of the proposals is to co-treat cells with BMP-2 and TGF-β as the latter may potentially prevent differentiation of MSCs into osteogenic lineage [75]. BMP-7 has been reported to inhibit MSC proliferation but does allow proliferation in the presence of TGF-β [76, 77]. Further, growth factors may complement each other and work in synergism. BMP-7 and IGF-1 lead to an enhanced cartilage matrix synthesis [78]. Similarly, IGF-1, IGF-2, and TGF-β regulate each other’s gene expression and thus protein production [79]. Further, combination of IGF-1 and TGF- β has better healing potential compared to individual effect as the former is involved in protection of synovium and reduces the synovial thickening depicting lack of chronic inflammation [80]. Limitations in the form of osteogenic synthesis [72], synovial thickening [81, 82], and osteophyte formation [71, 83] as mentioned above may be managed by using growth factors in right combinations and dosages [72, 80, 84].
4 Scaffolds
Another criterion for successful cartilage tissue engineering is availability of three-dimensional matrices, as evidences have shown that two-dimensional culture system hardly supports MSCs’ chondrogenic differentiation. The micromass culture system as mentioned earlier has failed to recapitulate the cartilage developmental stages, besides express hypertrophic marker, collagen type X [85]. For cartilage rehabilitation most of the investigators prefer MSC application along with scaffold. This allows cellular growth and prevents them against deleterious effects of local environment. In addition, the cells are retained in situ at the desired locations avoiding the common problem of cell leakage [10]. Selected scaffold is supposed to bear features of biocompatibility, support cellular growth and expansion, and facilitate diffusion and movement, yet maintain adequate mechanical strength and properties till tissue is regenerated and integrated [10, 86,87,88]. In osteochondral lesions, survival time of scaffold is critical as the neocartilage that replaces it should have preformed subchondral bone to survive in addition to its integration with surrounding native cartilage [89]. Usually the cartilage islands that form during healing fail to survive unless not integrated with the adjacent native cartilage [11].
The scaffold design in cartilage tissue engineering is aimed at maintaining the physical (scaffold architecture, mechanical function, and degradation) and biochemical (relevant to cellular behavior and activity) properties [89]. The matrices evaluated include natural fibrin [43, 90,91,92,93], agarose and alginate [86], collagen [94,95,96,97], hyaluronan [47, 98,99,100] as well as synthetic polylactic acid [101,102,103], polyglycolic acid [104], and polylactic and polyglycolic acid [105, 106]. Natural scaffolds that bear desired biocompatibility, better cell attachment, and differentiation have limitations in the form of availability, ease of fabrication, mesh properties, and controllable biodegradability, in addition to immunological reactions and disease transmission [10]. Synthetic scaffolds in comparison though are modified chemically for desired fabrication, and have better versatility, suitable mesh properties, and controllable degradability, but again fall short with respect to cyto-compatibility and may elicit host response upon release of toxic by-products [86, 87]. To overcome such impediments, hybrid scaffolds have been developed incorporating solid polymer scaffold and hydrogel [10]. The former provides mechanical strength and the latter supports cell delivery resembling the biphasic (solid and liquid phases) nature of cartilage. The cells in hydrogel are maintained in three-dimensional stages and are homogenously distributed in solid polymer scaffold pores [107].
In order to utilize such scaffolds in clinical practice, both in vitro and in vivo studies need to be conducted especially in relation to their biocompatibility and mechanical strength. Apart from the above mentioned scaffold designs, two other types including biomimetic zonal and nonfibrous/nanoporous scaffolds have been developed based on the concept to provide microenvironment comparable to that of native cartilage for the cells [10]. Biomimetic zonal scaffold comprises different zones like that of cartilage in order to mimic the physical properties. The implanted cells thus secrete matrix based on the available environment [108]. Nonfibrous/nanoporous scaffolds constitute nano-size matrix that mimics physicochemical and biological properties of cartilage matrix, and thus tends to develop relevant signals for cellular differentiation (MSCs) and matrix synthesis (from MSCs and chondrocytes) [109]. For creating such scaffolds, numerous fabrication techniques (electro-spinning, chemical etching, particulate clumping, 3D printing, and phase separation) may be employed [10]. Preclinical studies that encapsulated cells in nanofibrous scaffolds by electro-spinning have failed to maintain cell homogeneity and have resulted in cell clumping [110]. 3D printing is currently seen to carry the potential to replicate the cartilage structure. The cells are delivered in a suspension or with a gel as an ink in layer-by-layer process creating an appropriate pericellular environment for the cells located in each cartilage zone [111, 112]. One of the impediments in utilizing the technology in tissue engineering is the need to integrate vascular network for proper nutrient and gas supply. Cartilage, however, being devoid of direct blood, lymph, and nerve supply may act as a good candidate for 3D bioprinting [113]. Direct bioprinting into an ex vivo cartilage defect has resulted in some level of integration into native cartilage and mechanical competence [114]. This demands a detailed analysis of the fabrication process and its evaluation in preclinical as well as clinical studies.
5 Clinical Trials
The successful outcome in clinical settings is the ultimate aim of cartilage tissue engineering. So far the aim is unmet both in veterinary practice and in human medicine though the reports appear promising. The application in animals may provide the basis for human stem cell therapy. In veterinary practice, canines and equines comprise majority of the clinical application studies.
Stem cell therapy in canines has been instituted both in preclinical [115,116,117] and in clinical settings [118,119,120,121,122,123]. A single-time, local implantation of the cells in all the studies has been made barring a single study wherein cells were implanted at acupoints [122]. The cells were either applied directly without employing the vehicle [122, 123] or implanted with platelet-rich plasma [120] or hyaluronic acid [124]. All these studies have reported improved healing (pain, visual analog scale, and range of motion) on MSC application with follow-up varying from 1 month [122, 124] and 6 months [120, 121] to 5 years [119,120,121,122, 124]. Two comparative studies were conducted involving AD-MSCs versus platelet-rich growth factors (PRGF) [121] and AD-MSC versus stromal vascular fraction (SVF) [122]. In both the studies improved results have been reported with MSCs; however, in the former study MSCs showed better results at 6 months compared to PRGF, while in the latter SVF had better results than MSCs. In another comparative study, vascular endothelial growth factor transgenic BM-MSCs were shown to improve early healing in comparison to simple MSCs [117].
In equines, most of the studies so far have been unable to fetch positive results for better cartilage repair in osteoarthritis patients [71, 125, 126]. Some of the studies, clinical as well as experimental, though have shown beneficial effects in cartilage repair but are mainly on the basis of reduction in pain perception [127,128,129]. In a clinical study of 40 horses having joint affections treated with BM-MSCs, 77% of the patients returned to work; among them 38% were able to work to the previous condition or exceeded [125]. Currently, the stem cell being implanted is at 2 × 107 concentration in hyaluronan scaffold (22 mg of Hyvisc) (hyaluronate sodium, 3 × 106 Da, Anika Therapeutics, Woburn, MA) [130], prior to which NSAIDs were recommended to reduce joint flare [131].
In human medicine numerous cartilage-related clinical trials implanting stem cells have been registered at http://www.clinicaltrial.gov/. Among them some are completed, while some are in progress. The cells have been injected either locally (intra-articularly) or implanted surgically. All the registered studies located were uncontrolled. The stem cell reported studies are either case series [66, 132,133,134,135,136,137], case reports [138,139,140,141,142,143,144], or comparative [66, 141,142,143,144,145,146,147,148] type. The cell types employed in such studies have been AD-MSCs, bone marrow concentrate, and BM-MSCs with or without the scaffolds. The patient number in case series studies ranged from 4 to 48. The follow-up period of at least 3 months and a maximum of 5 years has been made. An overall improvement in the clinical parameters (Visual Analog Score, Improved Knee and Osteoarthritis Outcome Score, and International Knee Documentation Score), MRI, and histological score in the patients has been reported with no major adverse effect observed on cell application. With respect to the formation of the healing tissue, the variability in outcome was reported. Some of the patients had hyaline-like tissue [135, 140, 145, 149], while others had combination of the hyaline/fibrocartilage [135] or mainly fibrocartilaginous tissue [141]. In a study that compared MSCs versus ACI with equal patient number of 36 in each group, the clinical results were comparable except for improvement in physical functioning of patients in BM-MSC groups [146]. In a study that evaluated dose-dependent healing potential of MSCs, the group of patients that received higher dose (1.0 × 108) had better clinical scores and reduced pain compared to those patients that received lower dose of AD-MSCs (1.0 × 107 and 5.0 × 107) [67].
In clinical settings, variability in lesion type, site, duration of existence, age of the patient, cell culture techniques, and cell application methods and their number, besides addition of growth factors and scaffolds, have bearing on the outcome, and thus demand controlled studies [10].
6 Conclusions and Future Perspectives
Articular cartilage upon damage carries limited regeneration potential. Currently, tissue engineering, employing cells, growth factors, and scaffolds are considered to have the potential to support regeneration and integration of neo-cartilage with the surrounding native tissue. MSCs especially BM-MSCs and AD-MSCs carry maximum share among all stem cells in cartilage tissue engineering. There is a need to investigate cell source to find out whether only autogenous cells or both autogenic and allogenic/xenogenic cells can be utilized. The cell survival posttransplantation and integration of regenerated tissue matrix with the host native tissue remain the major causes of concern. One of the promising technologies to develop mechanically strong cartilage-to-cartilage interface includes the mesenchymal condensation into cellular bodies under the influence of growth factors. However, more research especially under in vivo conditions is desired in the area to evaluate its actual clinical application. Growth factors form an indispensable part of the tissue engineering and demand further evaluation on the basis of their individual properties as well as combinations including dosages. Scaffold that affects the desired chondrogenesis remains to be elucidated. Newer fabrication technologies that appear promising need to be evaluated and compared against the conventional technologies especially in relation to the maintenance of scaffold mechanical and biological properties. Tissue engineering that appears promising needs to be evaluated with respect to the cell sources; culture methods; concentration; implantation methods; growth factors, their combinations, doses, and frequency; and scaffolds, their sources, design, and type, before it becomes a clinical reality.
References
Mankin HJ. Synovium and cartilage in health and disease. In: Newton CD, Nunamaker DM, editors. Textbook of small animal orthopaedics. Philadelphia: JB. Lippincott Company; 1984. p. 90.
Frisbie DD, Cross MW, McIlwraith CW. A comparative study of articular cartilage thickness in the stifle of animal species used in human pre-clinical studies compared to articular cartilage thickness in the human. Vet Comp Orthop Traumatol. 2006;19(3):142–6.
Athanasiou AK, Agarwal A, Muffoletto A. Biomechanical properties of hip cartilage in experimental animal models. Clin Orthop. 1995;316:254–66.
Poole AR. Cartilage in health and disease. In: Koopman WJ, editor. Arthritis and allied conditions. Philadelphia: Lippincott Williams and Wilkins; 2001. p. 226–84.
Maroudas A. Physicochemical properties of articular cartilage. In: Freeman M, editor. Adult articular cartilage. London: Pitman Medical; 1979. p. 215–90.
Jeffrey AK, Blunn GW, Archer CW. Three-dimensional collagen architecture in bovine articular cartilage. J Bone Joint Surg. 1991;73:795–801.
Woessner JF, Nagase H. Matrix Metalloproteinases and TIMPs. Oxford, UK: Oxford University Press; 2002.
Kinner B, Capito RM, Spector M. Regeneration of articular cartilage. Adv Biochem Eng Biotechnol. 2005;94:91–123.
Duarte Campos DF, Drescher W, Rath B, Tingart M, Fischer H. Supporting biomaterials for articular cartilage repair. Cartilage. 2012;3:205–21.
Gugjoo MB, Amarpal, Sharma GT, Kinjavdekar P, Aithal HP, Pawde AM. Cartilage tissue engineering: role of mesenchymal stem cells along with growth factors and scaffolds. Indian J Med Res. 2016;144:339–47.
Hunziker EB. Biologic repair of articular cartilage. Defect models in experimental animals and matrix requirements. Clin Orthop Relat Res. 1999;367:S135–46.
Breinan HA, Minas T, Hsu HP, Nehrer S, Sledge CB, Spector M. Effect of cultured autologous chondrocytes on repair of chondral defects in a canine model. J Bone Joint Surg Am. 1997;79:1439–51.
Arican M, Koylu O, Uyaroglu A, Erol M, Calim KN. The effect of (Hylan G-F 20) on bone metabolism in dogs with experimental osteochondral defects. J Turk Vet Surg. 2006;12:20–3.
Günes T, Sen C, Erdem M, Köseoglu RD, Filiz NO. Combination of microfracture and periosteal transplantation techniques for the treatment of full-thickness cartilage defects. Acta Orthop Traumatol Turc. 2006;40:315–23.
Tiwary R, Amarpal, Aithal HP, Kinjavdekar P, Pawde AM, Singh R. Effect of IGF-1 and uncultured autologous bone-marrow-derived mononuclear cells on repair of osteochondral defect in rabbits. Cartilage. 2014;5:43–54.
Barbour KE, Helmick CG, Boring M. Prevalence of doctor diagnosed arthritis at state and county levels-United States, 2014. MMWR—Morbid Mortal Week Report. 2016;65(19):489–94.
Johnston SA. Osteoarthritis. Joint anatomy, physiology, and pathobiology. Vet Clin North Am Small Anim Pract. 1997;27:699–723.
Brandt KD, Dieppe P, Radin E. Etiopathogenesis of osteoarthritis. Med Clin North Am. 2009;93(1):1e24.
Hugle T, Geurts J. What drives osteoarthritis?—synovial versus subchondral bone pathology. Rheumatology (Oxford). 2016;56(9):1461–71.
Bilgili H, Yildiz C, Kurum B, Soysal Y, Bahce M. Repair of osteochondral defects with autologous chondrocyte implantation: clinical study on the stifle joint of 9 dogs. Ankara Univ J Vet Fac. 2006;53:103–9.
Juneau C, Paine R, Chicas E, Gardner E, Bailey L, McDermott J. Current concepts in treatment of patellofemoral osteochondritis dissecans. Int J Sports Phys Ther. 2016;11(6):903–25.
Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG. Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year follow-up. Art Ther. 2003;19:477–84.
Sgaglione NA, Miniaci A, Gillogly SD, Carter TR. Update on advanced surgical techniques in the treatment of traumatic focal articular cartilage lesions in the knee. Art Ther. 2002;18:9–32.
O’Driscoll SW. The healing and regeneration of articular cartilage. J Bone Joint Surg Am. 1998;80:1795–812.
Tsai CL, Liu TK, Fu SL, Perng JH, Lin AC. Preliminary study of cartilage repair with autologous periosteum and fibrin adhesive system. J Formos Med Assoc. 1992;91:S239–45.
Outerbridge HK, Outerbridge AR, Outerbridge RE. The use of a lateral patellar autologous graft for the repair of a large osteochondral defect in the knee. J Bone Joint Surg Am. 1995;77:65–72.
Grande DA, Halberstadt C, Naughton G, Schwartz R, Manji R. Evaluation of matrix scaffolds for tissue engineering of articular cartilage grafts. J Biomed Mater Res. 1997;34:211–20.
Tins BJ, McCall IW, Takahashi T, Cassar-Pullicino V, Roberts S, Ashton B, Richardson J. Autologous chondrocyte implantation in knee joint: MR imaging and histologic features at 1-year follow-up. Radiology. 2005;234:501–8.
van Dyk GE, Dejardin LM, Flo G, Johnson LL. Cancellous bone grafting of large osteochondral defects: an experimental study in dogs. Art Ther. 1998;14:311–20.
Gunay C, Sagliyan A, Unsaldi E, Yaman M. Repair of experimentally induced osteochondral defects of dog knee joint with cancellous autograft. Firat Univ J Health Sci. 2005;19:107–13.
Reddy S, Pedowitz DI, Parekh SG, Sennett BJ, Okereke E. The morbidity associated with osteochondral harvest from asymptomatic knees for the treatment of osteochondral lesions of the talus. Am J Sports Med. 2007;35:80–5.
Pelttari K, Winter A, Steck E, Goetzke K, Hennig T, Ochs BG, Aigner T, Richter W. Premature induction of hypertrophy during in vitro chondrogenesis of human mesenchymal stem cells correlates with calcification and vascular invasion after ectopic transplantation in SCID mice. Arthritis Rheum. 2006;54:3254–66.
Punwar S, Khan WS. Mesenchymal stem cells and articular cartilage repair: clinical studies and future direction. Open Orthop J. 2011;5:296–301.
Adkisson HD, Gillis MP, Davis EC, Maloney W, Hruska KA. In vitro generation of scaffold independent neocartilage. Clin Orthop Relat Res. 2001;391(Suppl):280–94.
Fraser JK, Wulur I, Alfonso Z, Hedrick MH. Fat tissue: an underappreciated source of stem cells for biotechnology. Trends Biotechnol. 2006;24(4):150–4.
Kessler MW, Grande DA. Tissue engineering and Cartilage. Organogenesis. 2008;4(1):28–32.
Gade NE, Pratheesh MD, Nath A, Dubey PK, Amarpal, Sharma B, Saikkumar G, Taru Sharma G. Molecular and cellular characterization of buffalo bone marrow-derived mesenchyme stem cells. Reprod Domest Anim. 2013;48(3):358–67.
Guzzo RM, Scanlon V, Sanjay A, Xu RH, Drissi H. Establishment of human cell type-specific iPS cells with enhanced chondrogenic potential. Stem Cell Rev Rep. 2014;10(6):820–9.
Zuk P, Zhu M, Mizuno H, Huang J, Futrell J, Katz A, Behhaim P, Lorenz HP, Hedrick MH. Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng. 2001;7:211–28.
Wang M, Yuan Z, Ma N, Hao C, Guo W, Zou G, Zhang Y, Chen M, Gao S, Peng J, Wang A, Wang Y, Sui X, Xu W, Lu S, Liu S, Guo Q. Advances and prospects in stem cells for cartilage regeneration. Stem Cells Int. 2017;2017:Article ID 4130607.
Singh A, Singh A, Sen D. Mesenchymal stem cells in cardiac regeneration: a detailed progress report of the last 6 years (2010–2015). Stem Cell Res Ther. 2016;7(1):82.
Wakitani S, Goto T, Pineda SJ, Young RG, Mansour JM, Caplan AI, Goldberg VM. Mesenchymal cell-based repair of large, full-thickness defects of articular cartilage. J Bone Joint Surg Am. 1994;76:579–92.
Wang F, Li Z, Tamama K, Sen CK, Guan J. Fabrication and characterization of prosurvival growth factor releasing, anisotropic scaffolds for enhanced mesenchymal stem cell survival/growth and orientation. Biomacromolecules. 2009;10:2609–18.
Kazemi D, Asenjan SK, Dehdilani N, Para H. Canine articular cartilage regeneration using mesenchymal stem cells seeded on platelet rich fibrin. Bone Joint Res. 2017;6(2):98–107.
De Bari C, Dell ‘Accio F, Luyten FP. Failure of in vitro differentiated mesenchymal stem cells from the synovial membrane to form ectopic stable cartilage in vivo. Arthritis Rheum. 2004;50:142–50.
Csaki C, Schneider PR, Shakibaei M. Mesenchymal stem cells as a potential pool for cartilage tissue engineering. Ann Anat. 2008;190:395–412.
Solchaga LA, Penick KJ, Welter JF. Chondrogenic differentiation of bone marrow-derived mesenchymal stem cells: tips and tricks. Methods Mol Biol. 2011;698:253–78.
Gugjoo MB, Amarpal, Ahmed AA, Kinjavdekar P, Aithal HP, Pawde AM, Kumar GS, Sharma GT. Mesenchymal stem cells with IGF-1 and TGF-β1 in laminin gel for osteochondral defects in rabbits. Biomed Pharmacother. 2017;93:1165–74.
Stewart MC, Stewart AA. Mesenchymal stem cells: characteristics, sources, mechanisms of action. Vet Clin North Am Equine Pract. 2011;27:243–61.
Berglund AK, Schnabel LV. Allogeneic major histocompatibility complex-mismatched equine bone marrow-derived mesenchymal stem cells are targeted for death by cytotoxic anti-major histocompatibility complex antibodies. Equine Vet J. 2017;49(4):539–44.
Owens SD, Kol A, Walker NJ, Borjesson DL. Allogeneic mesenchymal stem cell treatment induces specific allo-antibodies in horses. Stem Cells Int. 2016;2016:Article ID 5830103.
Mafi R, Hindocha S, Mafi P, Griffin M, Khan WS. Sources of adult mesenchymal stem cells applicable for musculoskeletal applications - a systematic review of the literature. Open Orthop J. 2011;5:242–8.
Lee WYW, Wang BW. Cartilage repair by mesenchymal stem cells: clinical trial update and perspectives. J Orthop Translation. 2017;9:76–88.
Johnstone B, Hering TM, Caplan AI, Goldberg VM, Yoo JU. In vitro chondrogenesis of bone marrow-derived mesenchymal progenitor cells. Exp Cell Res. 1998;238:265–72.
Sekiya I, Colter DC, Prockop DJ. BMP-6 enhances chondrogenesis in a subpopulation of human marrow stromal cells. Biochem Biophys Res Commun. 2001;284:411–8.
Kim YJ, Kim HJ, Im GI. PTHrP promotes chondrogenesis and suppresses hypertrophy from both bone marrow-derived and adipose tissue-derived MSCs. Biochem Biophys Res Commun. 2008;373:104–8.
Pei M, He F, Vunjak-Novakovic G. Synovium-derived stem cell-based chondrogenesis. Differentiation for cartilage repair: monitoring its success by magnetic resonance imaging and histology. Arthritis Res Ther. 2008;5:R60–3.
DeLise AM, Fischer L, Tuan RS. Cellular interactions and signalling in cartilage development. Osteoarthr Cartil. 2000;8:309–34.
Hall BK, Miyake T. All for one and one for all: condensations and the initiation of skeletal development. Bioessays. 2000;22:138–47.
Bhumiratana S, Eton RE, Oungoulian SR, Wan LQ, Ateshian GA, Vunjak-Novakovic G. Large, stratified, and mechanically functional human cartilage grown in vitro by mesenchymal condensation. Proc Natl Acad Sci U S A. 2014;111:6940–5.
Shirasawa S, Sekiya I, Sakaguchi Y, Yagishita K, Ichinose S, Muneta T. In vitro chondrogenesis of human synovium derived mesenchymal stem cells: optimal condition and comparison with bone marrow-derived cells. J Cell Biochem. 2006;97(1):84–97.
Mitchell JB, Mcintosh K, Zvonic S, Garrett S, Floyd ZE, Kloster A, Di Halvorsen Y, Storms RW, Goh B, Kilroy G, Wu X, Gimble JM. Immunophenotype of human adipose-derived cells: temporal changes in stromal-associated and stem cell–associated markers. Stem Cells. 2006;24(2):376–85.
Steinert AF, Ghivizzani SC, Rethwilm A, Tuan RS, Evans CH, Noth U. Major biological obstacles for persistent cell-based regeneration of articular cartilage. Arthritis Res Ther. 2007;9(3):213.
Roobrouck VD, Ulloa-Montoya F, Verfaillie CM. Self-renewal and differentiation capacity of young and aged stem cells. Exp Cell Res. 2008;314(9):1937–44.
van der Bogt KE, Schrepfer S, Yu J, Sheikh AY, Hoyt G, Govaert JA, Velotta JB, Contag CH, Robbins RC, Wu JC. Comparison of transplantation of adipose tissue- and bone marrow-derived mesenchymal stem cells in the infarcted heart. Transplantation. 2009;87(5):642–52.
Koga H, Muneta T, Ju YJ, Nagase T, Nimura A, Mochizuki T, Ichinose S, von der Mark K, Sekiya I. Synovial stem cells are regionally specified according to local microenvironments after implantation for cartilage regeneration. Stem Cells. 2007;25:689–96.
Jo CH, Lee YG, Shin WH, Kim H, Chai JW, Jeong EC, Kim JE, Shim H, Shin JS, Shin IS, Ra JC, Oh S, Yoon KS. Intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritis of the knee: a proof-of-concept clinical trial. Stem Cells. 2014;32:1254–66.
Goldring MB, Tsuchimochi K, Ijiri K. The control of chondrogenesis. J Cell Biochem. 2006;97:33–4.
Middleton J, Manthey A, Tyler J. Insulin-like growth factor (IGF) receptor, IGF-I, interleukin-1 beta (IL-1 beta), and IL-6 mRNA expression in osteoarthritic and normal human cartilage. J Histochem Cytochem. 1996;44:133–41.
Gouttenoire J, Valcourt U, Ronzière MC, Aubert-Foucher E, Mallein-Gerin F, Herbage D. Modulation of collagen synthesis in normal and osteoarthritic cartilage. Biorheology. 2004;41:535–42.
Wilke MM, Nydam DV, Nixon AJ. Enhanced early chondrogenesis in articular defects following arthroscopic mesenchymal stem cell implantation in an equine model. J Orthop Res. 2007;25:913–25.
Baugé C, Girard N, Lhuissier E, Bazille C, Boumediene K. Regulation and role of TGF𝛽 signaling pathway in aging and osteoarthritis joints. Aging Dis. 2014;5(6):394–405.
Kameda T, Koike C, Saitoh K, Kuroiwa A, Iba H. Analysis of cartilage maturation using micromass cultures of primary chondrocytes. Dev Growth Differ. 2000;42(3):229–36.
Spagnoli A. Mesenchymal stem cells and fracture healing. Orthopedics. 2008;31(9):855–6.
Mehlhorn AT, Schmal H, Kaiser S, Lepski G, Finkenzeller G, Stark GB, Südkamp NP. Mesenchymal stem cells maintain TGF-𝛽-mediated chondrogenic phenotype in alginate bead culture. Tissue Eng. 2006;12(6):1393–403.
Goodrich LR, Hidaka C, Robbins PD, Evans CH, Nixon AJ. Genetic modification of chondrocytes with insulin-like growth factor-1 enhances cartilage healing in an equine model. J Bone Joint Surg Br. 2007;89:672–85.
Elshaier AM, Hakimiyan AA, Rappoport L, Rueger DC, Chubinskaya S. Effect of interleukin-1beta on osteogenic protein 1-induced signaling in adult human articular chondrocytes. Arthritis Rheum. 2009;60:143–54.
Loeser RF, Pacione CA, Chubinskaya S. The combination of insulin-like growth factor 1 and osteogenic protein 1 promotes increased survival of and matrix synthesis by normal and osteoarthritic human articular chondrocytes. Arthritis Rheum. 2003;48:2188–96.
Shi S, Mercer S, Eckert GJ, Trippel SB. Growth factor regulation of growth factors in articular chondrocytes. J Biol Chem. 2009;284:6697–704.
Davies LC, Blain EJ, Gilbert SJ, Caterson B, Duance VC. The potential of IGF-1 and TGFbeta1 for promoting “adult” articular cartilage repair: an in vitro study. Tissue Eng Part A. 2008;14:1251–61.
Bakker AC, van de Loo FA, van Beuningen HM, Sime P, van Lent PL, van der Kraan PM, Richards CD, van den Berg WB. Overexpression of active TGF-beta-1 in the murine knee joint: evidence for synovial layer-dependent chondro-osteophyte formation. Osteoarthr Cartil. 2001;9:128–36.
Boehm AK, Seth M, Mayr KG, Fortier LA. Hsp90 mediates insulin-like growth factor 1 and interleukin-1beta signaling in an age-dependent manner in equine articular chondrocytes. Arthritis Rheum. 2007;56:2335–43.
Miyakoshi N, Kobayashi M, Nozaka K, Okada K, Shimada Y, Itoi E. Effects of intraarticular administration of basic fibroblast growth factor with hyaluronic acid on osteochondral defects of the knee in rabbits. Arch Orthop Trauma Surg. 2005;125:683–92.
Mierisch CM, Cohen SB, Jordan LC, Robertson PG, Balian G, Diduch DR. Transforming growth factor-beta in calcium alginate beads for the treatment of articular cartilage defects in the rabbit. Art Ther. 2002;18:892–900.
Johnstone B, Alini M, Cucchiarini M, Dodge GR, Eglin D, Guilak F. Tissue engineering for articular cartilage repair—the state of the art. Eur Cell Mater. 2013;25:248–67.
Lu L, Zhu X, Valenzuela RG, Currier BL, Yaszemski MJ. Biodegradable polymer scaffolds for cartilage tissue engineering. Clin Orthop Relat Res. 2001;391(Suppl):251–70.
Risbud MV, Sittinger M. Tissue engineering: advances in in vitro cartilage generation. Trends Biotechnol. 2002;20:351–6.
Frenkel SR, Di Cesare PE. Scaffolds for articular cartilage repair. Ann Biomed Eng. 2004;32:26–34.
Hutmacher DW. Scaffold design and fabrication technologies for engineering tissues—state of the art and future perspectives. J Biomater Sci Polym Ed. 2001;12:107–24.
Hendrickson DA, Nixon AJ, Grande DA, Todhunter RJ, Minor RM, Erb H, Lust G. Chondrocyte-fibrin matrix transplants for resurfacing extensive articular cartilage defects. J Orthop Res. 1994;12:485–97.
Brittberg M, Sjögren-Jansson E, Lindahl A, Peterson L. Influence of fibrin sealant (Tisseel) on osteochondral defect repair in the rabbit knee. Biomaterials. 1997;18:235–42.
Fortier LA, Mohammed HO, Lust G, Nixon AJ. Insulin like growth factor-I enhances cell-based repair of articular cartilage. J Bone Joint Surg Br. 2002;84:276–88.
Fortier LA, Nixon AJ, Lust G. Phenotypic expression of equine articular chondrocytes grown in three-dimensional cultures supplemented with supraphysiologic concentrations of insulin-like growth factor-1. Am J Vet Res. 2002;63:301–5.
Grande DA, Pitman MI, Peterson L, Menche D, Klein M. The repair of experimentally produced defects in rabbit articular cartilage by autologous chondrocyte transplantation. J Orthop Res. 1989;7:208–18.
Nehrer S, Breinan HA, Ramappa A, Shortkroff S, Young G, Minas T, Sledge CB, Yannas IV, Spector M. Canine chondrocytes seeded in type I and type II collagen implants investigated in vitro. J Biomed Mater Res. 1997;38:95–104.
Wakitani S, Imoto K, Yamamoto T, Saito M, Murata N, Yoneda M. Human autologous culture expanded bone marrow mesenchymal cell transplantation for repair of cartilage defects in osteoarthritic knees. Osteoarthr Cartil. 2002;10:199–206.
Lee CR, Grodzinsky AJ, Hsu HP, Spector M. Effects of a cultured autologous chondrocyte-seeded type II collagen scaffold on the healing of a chondral defect in a canine model. J Orthop Res. 2003;21:272–81.
Knudson W, Casey B, Nishida Y, Eger W, Kuettner KE, Knudson CB. Hyaluronan oligosaccharides perturb cartilage matrix homeostasis and induce chondrocytic chondrolysis. Arthritis Rheum. 2000;43:1165–74.
Gao J, Dennis JE, Solchaga LA, Goldberg VM, Caplan AI. Repair of osteochondral defect with tissue-engineered two-phase composite material of injectable calcium phosphate and hyaluronan sponge. Tissue Eng. 2002;8:827–37.
Solchaga LA, Gao J, Dennis JE, Awadallah A, Lundberg M, Caplan AI, Goldberg VM. Treatment of osteochondral defects with autologous bone marrow in a hyaluronan-based delivery vehicle. Tissue Eng. 2002;8:333–47.
Chu CR, Dounchis JS, Yoshioka M, Sah RL, Coutts RD, Amiel D. Osteochondral repair using perichondrial cells. A 1-year study in rabbits. Clin Orthop Relat Res. 1997;340:220–9.
Dounchis JS, Bae WC, Chen AC, Sah RL, Coutts RD, Amiel D. Cartilage repair with autogenic perichondrium cell and polylactic acid grafts. Clin Orthop Relat Res. 2000;377:248–64.
Frenkel SR, Chang J, Maurer S, Baitner A, Wright K. Bone protein in a grafton flex carrier for articular cartilage repair. Trans Am Acad Orthop Surg. 2001;26:356.
Liu Y, Chen F, Liu W, Cui L, Shang Q, Xia W, Wang J, Cui Y, Yang G, Liu D, Wu J, Xu R, Buonocore RD, Cao Y. Repairing large porcine full-thickness defects of articular cartilage using autologous chondrocyte-engineered cartilage. Tissue Eng. 2002;8:709–21.
Niederauer GG, Slivka MA, Leatherbury NC, Korvick DL, Harroff HH, Ehler WC, Dunn CJ, Kieswetter K. Evaluation of multiphase implants for repair of focal osteochondral defects in goats. Biomaterials. 2000;21:2561–74.
Cohen SB, Meirisch CM, Wilson HA, Diduch DR. The use of absorbable co-polymer pads with alginate and cells for articular cartilage repair in rabbits. Biomaterials. 2003;24:2653–60.
Caterson EJ, Nesti LJ, Li WJ, Danielson KG, Albert TJ, Vaccaro AR, Tuan RS. Three-dimensional cartilage formation by bone marrow-derived cells seeded in polylactide/alginate amalgam. J Biomed Mater Res. 2001;57:394–03.
Klein TJ, Schumacher BL, Schmidt TA, Li KW, Voegtline MS, Masuda K, Thonar EJ, Sah RL. Tissue engineering of stratified articular cartilage from chondrocyte subpopulations. Osteoarthritis Cartilage. 2003;11:595–602.
Zhang L, Webster TJ. Nanotechnology and nanomaterials: promises for improved tissue regeneration. Nano Today. 2009;4:66–80.
Li WJ, Jiang YJ, Tuan RS. Cell-nanofiber-based cartilage tissue engineering using improved cell seeding, growth factor, and bioreactor technologies. Tissue Eng Part A. 2008;14:639–48.
Cohen DL, Lipton JI, Bonassar LJ, Lipson H. Additive manufacturing for in situ repair of osteochondral defects. Biofabrication. 2010;2(3):12.
Fedorovich NE, Schuurman W, Wijnberg HM, Prins HJ, van Weeren PR, Malda J, Alblas J, Dhert WJ. Biofabrication of osteochondral tissue equivalents by printing topologically defined, cell-laden hydrogel scaffolds. Tissue Eng Part C Methods. 2012;18(1):33–44.
Ozbolat IT, Yu Y. Bioprinting toward organ fabrication: challenges and future trends. IEEE Transactions Biomed Eng. 2013;60(3):691–9.
Cui XF, Breitenkamp K, Finn MG, Lotz M, D’Lima DD. Direct human cartilage repair using three-dimensional bioprinting technology. Tissue Eng Part A. 2012;18(11–12):1304–12.
Mokbel A, El-Tookhy O, Shamaa AA, Sabry D, Rashed L, Mostafa A. Homing and efficacy of intraarticular injection of autologous mesenchymal stem cells in experimental chondral defects in dogs. Clin Exp Rheumatol. 2011;29:275–84.
Yang Q, Peng J, Lu SB, Guo QY, Zhao B, Zhang L, Wang AY, Xu WJ, Xia Q, Ma XL, Hu YC, Xu BS. Evaluation of an extracellular matrix-derived acellular biphasic scaffold/cell construct in the repair of a large articular high-load-bearing osteochondral defect in a canine model. Chin Med J. (Engl). 2011;124:3930–8.
Hang D, Wang Q, Guo C, Chen Z, Yan Z. Treatment of osteonecrosis of the femoral head with VEGF165 transgenic bone marrow mesenchymal stem cells in mongrel dogs. Cells Tissues Organs. 2012;195:495–506.
Black LL, Gaynor J, Adams C, Dhupa S, Sams AE, Taylor R, Harman S, Gingerich DA, Harman R. Effect of intraarticular injection of autologous adipose-derived mesenchymal stem and regenerative cells on clinical signs of chronic osteoarthritis of the elbow joint in dogs. Vet Ther. 2008;9:192–200.
Yoon HY, Lee JH, Jeong SW. Long-term follow-up after implantation of autologous adipose tissue derived mesenchymal stem cells to treat a dog with stifle joint osteoarthrosis. J Vet Clin. 2012;29:82–6.
Vilar JM, Morales M, Santana A, Spinella G, Rubio M, Cuervo B, Cugat R, Carrillo JM. Controlled, blinded force platform analysis of the effect of intraarticular injection of autologous adipose-derived mesenchymal stem cells associated to PRGF-Endoret in osteoarthritic dogs. BMC Vet Res. 2013;9:131.
Cuervo B, Rubio M, Sopena J, Dominguez JM, Vilar J, Morales M, Cugat R, Carrillo JM. Hip osteoarthritis in dogs: a randomized study using mesenchymal stem cells from adipose tissue and plasma rich in growth factors. Int J Mol Sci. 2014;15:13437–60.
Marx C, Silveira MD, Selbach I, Da Silva AS, De Macedo Braga LMG, Camassola M, Nardi NB. Acupoint injection of autologous stromal vascular fraction and allogeneic adipose-derived stem cells to treat hip dysplasia in dogs. Stem Cells Int. 2014;2014:391274.
Vilar JM, Batista M, Morales M, Santana A, Cuervo B, Rubio M, Cugat R, Sopena J, Carrillo JM. Assessment of the effect of intraarticular injection of autologous adipose-derived mesenchymal stem cells in osteoarthritic dogs using a double blinded force platform analysis. BMC Vet Res. 2014;10:143.
Guercio A, Di Marco P, Casella S, Cannella V, Russotto L, Purpari G, Di Bella S, Piccione G. Production of canine mesenchymal stem cells from adipose tissue and their application in dogs with chronic osteoarthritis of the humeroradial joints. Cell Biol Int. 2012;36:189–94.
Frisbie DD, Kisiday JD, Kawcak CE, Werpy NM, McIlwraith CW. Evaluation of adipose-derived stromal vascular fraction or bone marrow-derived mesenchymal stem cells for treatment of osteoarthritis. J Orthop Res. 2009;27:1675–80.
McIlwraith CW, Frisbie DD, Rodkey WG, Kisiday JD, Werpy NM, Kawcak CE, Steadman JR. Evaluation of intraarticular mesenchymal stem cells to augment healing of microfractured chondral defects. Art Ther. 2011;27:1552–61.
Ferris D, Frisbie DD, Kisiday J, McIlwraith CW, Hague B, Major MD, Schneider RK, Zubrod CJ, Watkins JJ, Kawcak CE, Goodrich LR. Clinical evaluation of bone marrow-derived mesenchymal stem cells in naturally occurring joint disease. Regen Med. 2009;4(Suppl 2):16.
Raheja LF, Galuppo LD, Bowers-Lepore J, Dowd JP, Tablin F, Yelowley CE. Treatment of bilateral medial femoral condyle articular cartilage fissures in a horse using bone marrow-derived multipotent mesenchymal stromal cells. J Equine Vet Sci. 2011;31:147–54.
Yamada ALM, Carvalho AD, Moroz A, Deffune E, Watanabe MJ, Hussni CA, Rodrigues CA, Alves ALG. Mesenchymal stem cell enhances chondral defects healing in horses. Stem Cell Disc. 2013;3(4):218–25.
Schnabel LV, Fortier LA, McIlwraith CW, Nobert KM. Therapeutic use of stem cells in horses: which type, how, and when? Vet J. 2013;197:570–7.
Ferris DJ, Frisbie DD, Kisiday JD, McIlwraith CW, Hague BA, Major MD, Schneider RK, Zubrod CJ, Kawcak CE, Goodrich LR. Clinical follow up of thirty-three horses treated for stifle injury with bone marrow derived mesenchymal stem cells intra-articularly. Vet Surg. 2014;43(3):255–65.
Haleem AM, Singergy AA, Sabry D, Atta HM, Rashed LA, Chu CR, El Shewy MT, Azzam A, Abdel Aziz MT. The clinical use of human culture-expanded autologous bone marrow mesenchymal stem cells transplanted on platelet-rich fibrin glue in the treatment of articular cartilage defects: a pilot study and preliminary results. Cartilage. 2010;1(4):253–61.
Buda R, Vannini F, Cavallo M, Grigolo B, Cenacchi A, Giannini S. Osteochondral lesions of the knee: a new one-step repair technique with bone-marrow-derived cells. J Bone Joint Surg Am. 2010;92(2):2–11.
Davatchi F, Abdollahi BS, Mohyeddin M, Shahram F, Nikbin B. Mesenchymal stem cell therapy for knee osteoarthritis. Preliminary report of four patients. Int J Rheum Dis. 2011;14(2):211–5.
Gigante A, Calcagno S, Cecconi S, Ramazzotti D, Manzotti S, Enea D. Use of collagen scaffold and autologous bone marrow concentrate as a one-step cartilage repair in the knee: histological results of second-look biopsies at 1 year follow-up. Int J Immunopathol Pharmacol. 2011;24(2):69–72.
Emadedin M, Aghdami N, Taghiyar L, Fazeli R, Moghadasali R, Jahangir S, Farjad R, Baghaban EM. Intraarticular injection of autologous mesenchymal stem cells in six patients with knee osteoarthritis. Arch Iran Med. 2012;15(7):422–8.
Mardones R, Jofre CM, Tobar L, Minguell JJ. Mesenchymal stem cell therapy in the treatment of hip osteoarthritis. J Hip Preservation Surg. 2017;4(2):159–63.
Wakitani S, Mitsuoka T, Nakamura N, Toritsuka Y, Nakamura Y, Horibe S. Autologous bone marrow stromal cell transplantation for repair of full-thickness articular cartilage defects in human patellae: two case reports. Cell Transplant. 2004;13(5):595–600.
Adachi N, Ochi M, Deie M, Ito Y. Transplant of mesenchymal stem cells and hydroxyapatite ceramics to treat severe osteochondral damage after septic arthritis of the knee. J Rheumatol. 2005;32(8):1615–8.
Kuroda R, Ishida K, Matsumoto T, Akisue T, Fujioka H, Mizuno K, Ohgushi H, Wakitani S, Kurosaka M. Treatment of a full-thickness articular cartilage defect in the femoral condyle of an athlete with autologous bone-marrow stromal cells. Osteoarthr Cartil. 2007;15(2):226–31.
Wakitani S, Nawata M, Tensho K, Okabe T, Machida H, Ohgushi H. Repair of articular cartilage defects in the patellofemoral joint with autologous bone marrow mesenchymal cell transplantation: three case reports involving nine defects in five knees. J Tissue Eng Regen Med. 2007;1(1):74–9.
Centeno CJ, Busse D, Kisiday J, Keohan C, Freeman M, Karli D. Increased knee cartilage volume in degenerative joint disease using percutaneously implanted, autologous mesenchymal stem cells. Pain Physician. 2008;11(3):343–53.
Kasemkijwattana C, Hongeng S, Kesprayura S, Rungsinaporn V, Chaipinyo K, Chansiri K. Autologous bone marrow mesenchymal stem cells implantation for cartilage defects: two cases report. J Med Assoc Thai. 2011;94(3):395–400.
Pak J. Regeneration of human bones in hip osteonecrosis and human cartilage in knee osteoarthritis with autologous adipose-tissue-derived stem cells: a case series. J Med Case Reports. 2011;5:296.
Giannini S, Buda R, Vannini F, Cavallo M, Grigolo B. One-step bone marrow-derived cell transplantation in talar osteochondral lesions. Clin Orthop Relat Res. 2009;467(12):3307–20.
Nejadnik H, Hui JH, Feng Choong EP, Tai BC, Lee EH. Autologous bone marrow-derived mesenchymal stem cells versus autologous chondrocyte implantation: an observational cohort study. Am J Sports Med. 2010;38(6):1110–6.
Varma HS, Dadarya B, Vidyarthi A. The new avenues in the management of osteoarthritis of knee-stem cells. J Indian Med Assoc. 2010;108:583–5.
Koh YG, Choi YJ. Infrapatellar fat pad-derived mesenchymal stem cell therapy for knee osteoarthritis. Knee. 2012;19(6):902–7.
Giannini S, Buda R, Cavallo M, Ruffilli A, Cenacchi A, Cavallo C, Vannini F. Cartilage repair evolution in post-traumatic osteochondral lesions of the talus: from open field autologous chondrocyte to bone-marrow-derived cells transplantation. Injury. 2010;41(11):1196–203.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Gugjoo, M.B., Aithal, H.P., Kinjavdekar, P., Amarpal (2019). Cartilage Tissue Engineering: Role of Mesenchymal Stem Cells, Growth Factors, and Scaffolds. In: Duscher, D., Shiffman, M.A. (eds) Regenerative Medicine and Plastic Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-19962-3_18
Download citation
DOI: https://doi.org/10.1007/978-3-030-19962-3_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-19961-6
Online ISBN: 978-3-030-19962-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)