Abstract
Behçet’s syndrome (BS), a distinct disease with orogenital ulceration and uveitis known as the triple-symptom complex, is an idiopathic chronic relapsing multisystem vascular-inflammatory disease of unknown origin. The neurological involvement of BS is termed as neuro-Behçet’s syndrome (NBS). Direct neurological involvement of BS may be classified into two forms: (1) parenchymal (p-NBS) and (2) vascular involvement. p-NBS with the rate of 75% among neurological involvements of BS usually presents with an acute-subacute brain stem syndrome. Headache, cranial neuropathy, dysarthria, ataxia, and hemiparesis are the most prominent symptoms. The most common areas affected in p-NBS are the mesodiencephalic junction (MDJ), pons, and medulla oblongata. MDJ lesions tend to extend upward to involve the diencephalic structures and downward to involve the pontobulbar region which is the most common radiological finding observed in p-NBS. The only drug that has been shown to be effective based on the Class IV evidence is infliximab for the treatment of p-NBS.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Behçet’s syndrome
- Parenchymal neuro-Behçet’s syndrome
- Cerebral venous sinus thrombosis
- Bagel Sign
- Infliximab
Introduction
Behçet’s syndrome (BS) was originally described in 1937 by the Turkish dermatologist Hulusi Behçet as a distinct disease with orogenital ulceration and uveitis known as the triple-symptom complex. BS is an idiopathic chronic relapsing multisystem vascular-inflammatory disease of unknown origin [1]. Due to the lack of specific laboratory, radiologic, or histologic findings of BS, accurate diagnosis of BS depends on clinical features. According to International Study Group (ISG)’s classification for a diagnosis, recurrent oral ulcerations plus two of the following are required: (a) recurrent genital ulcerations, (b) skin lesions, (c) eye lesions, and (d) positive pathergy test [2]. Given that the BS affects many organs and systems implying a “syndrome” rather than “disease,” we will use the term Behçet’s syndrome (BS) in this chapter [3].
Epidemiology
While BS is more prevalent in the regions along the “Silk Road,” prevalence tends to increase in Western countries over the past few years due to the increased migration from some of these countries to Western countries. The estimated prevalence of BS is variable across Europe, being low in the northern part of Europe compared to the south [4]. The prevalence of BS in Turkey is between 20 and 421 in 100,000 with the highest rate across the Silk Road, giving a high rate in the Anatolia. These findings support the environmental hypothesis on BS pathogenesis [5]. Another finding supporting the environmental hypothesis is that no patient was diagnosed as BS in Hawaii where the population of Japanese (genetically susceptible) is high [6]. On the other hand, the higher prevalence of BS among Turkish immigrants living in Germany compared to native Germans, and the lower rates of this syndrome in Germany compared to Turkey, suggests that genetic influences are stronger than environmental factors in the disease etiology [7]. Furthermore, the positive family history up to 12% and a sibling risk ratio ranging from 11.4 to 52.5 support the genetic hypothesis of BS similar to complex gene disorders [8].
Around 50–80% of BS patients along the “Silk Road” carry HLA-B51, whereas the frequency of this allele is ~25% in the general population. However, in the regions where the BS is uncommon, the HLA-B51 positivity ratio is similar to the general population, and this distribution of HLA-B5 and its HLA-B∗51 subtype positivity differing among the countries may give a clue of disease origin [9]. The positivity of HLA-B51 was significantly higher in the hospital-based studies, so it can be argued that the HLA-B51 is probably related not with the disease itself but with its severity [10].
The usual onset of BS is in the third or fourth decade of life. However, onset in children has also been reported, although this is rare [11]. While BS shows equal frequency between each sex, males have a more severe disease course. Interestingly, there is no relationship between age at immigration and the risk of BS [12].
Clinical Manifestations of BS
Clinical manifestations of BS are highly variable among the patients.
Mucocutaneous Symptoms
Mucocutaneous manifestations in BS are common and include oral and genital ulcerations, papulopustular skin lesions, erythema nodosum (EN)-like skin lesions, pathergy reaction, and other rare skin lesions. Recurrent aphthous stomatitis is the hallmark of the syndrome. Aphtous lesions are usually small, round, or oval painful [13]. External genital ulcers usually occur on the scrotum in men and on the labia in women. They are deep and very painful and leave scars, producing an objective sign even in the absence of active lesions [14]. The pathergy phenomenon is a non-specific hypersensitivity reaction of the hyperirritable skin seen in BS and is produced by inserting a 20-gauge needle into the dermis of the forearm (skin pathergy test). The reaction is considered positive if a papule or pustule is formed at the site of the puncture within 48 hours [2].
Ocular Involvement
Ocular involvement is one of the most disabling complications of BS causing progressive vision loss in half of the patients if not treated properly [15]. Anterior uveitis, posterior uveitis, cells in the vitreous on a slit-lamp examination, and/or retinal vasculitis are the primary clinical features, but optic neuritis may also be present in extremely rare instances [16].
Gastrointestinal Involvement
The most common symptoms indicating gastrointestinal involvement are right upper quadrant abdominal pain, diarrhea, and gastrointestinal bleeding, respectively. Any part of the gastrointestinal tract, especially the distal ileum and cecum, may have ulcers, and at times it may be difficult to distinguish inflammatory bowel disease from BS [17].
Arthritis
Nonerosive , nonmigrating, oligoarticular involvement of large joints, especially the knees, ankles, and wrists, is reported in 35–50% of patients and resolves spontaneously within a few weeks [18].
Neurological Involvement in BS
The neurological involvement of BS is termed as neuro-Behçet’s syndrome (NBS). While there is no biomarker for NBS, the diagnosis is mainly based on the clinical and neuroimaging features. NBS is not included in the current criteria of International Study Group. Considering the rate of 5–10% neurological involvement among BS patients and taking into account the increased atypical presentation of neurological involvement especially over the last years, the importance of NBS is increasing [19, 20]. Therefore, ISG criteria need to be reevaluated in terms of neurological involvement. The criteria of NBS can be summarized as: “The occurrence of neurological symptoms and signs in a patient who meets the International Study Group Criteria for BS, when those symptoms/signs are not otherwise referable to any other known systemic or neurological disease, or treatment thereof, and in whom objective abnormalities consistent with NBS are evident either on neurological examination or MRI, or upon cerebrospinal fluid (CSF) analysis [19].”
The neurological involvement may be observed either directly or indirectly which is due to the complications of systemic involvement of BS or related with the drugs used in BS [21]. Neurological involvement developing indirectly includes increased intracranial pressure secondary to superior vena cava syndrome and cerebral emboli secondary to cardiac involvement. Central nervous system (CNS) neurotoxicity caused by cyclosporine and peripheral neuropathy secondary to thalidomide or colchicine use are neurological complications associated with BS treatment [21].
Direct neurological involvement of BS may be classified into two forms: (1) parenchymal (p-NBS) and (2) vascular involvement.
p-NBS
p-NBS with the rate of 75% among neurological involvements of BS usually presents with an acute-subacute brain stem syndrome characterized by headache, cranial neuropathy, dysarthria, ataxia, and hemiparesis as the most prominent symptoms [19]. While the headache is also the cardinal symptom of vascular involvement, differentiation of the neurologic type should be done cautiously together with the MRI features as the long-term treatment differs between these two types of neurological involvement [22]. Regarding the clinical phenotype p-NBS, it may be classified as four subtypes similar to multiple sclerosis (MS): (1) single attack, (2) relapsing form, (3) secondary progressive, and (4) primary progressive [23]. One of the main clinical differences between p-NBS and MS is that patients with the relapsing form of MS usually recover well, while those with the relapsing form of p-NBS do not [24]. The other difference between MS and NBS relies on laboratory findings: while CSF cell counts are typically within normal limits and oligoclonal bands are present in MS, pleocytosis is frequently observed, and oligoclonal bands are rarely detected in p-NBS [25].
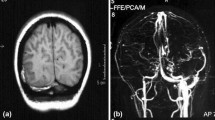
Besides clinical features of p-NBS, MRI patterns are of utmost importance of distinguishing the p-NBS from the other disorders mimicking p-NBS (Fig. 1). The most common areas affected in p-NBS are the mesodiencephalic junction (MDJ), pons, and medulla oblongata. MDJ lesions tend to extend upward to involve the diencephalic structures and downward to involve the pontobulbar region which is the most common radiological finding observed in p-NBS (Fig. 1) [26]. Brainstem lesions extending into the diencephalic and basal ganglia during acute disease may exert mass effects caused by vasogenic edema and thus resemble tumors. Some tumefactive lesions have been confused with primary or metastatic tumors, but only a few were located in structures other than the brainstem and deep hemispheric structures such as the frontoparietal or temporal lobe or the cerebellum [27].
Cranial magnetic resonance imaging patterns in Behçet’s syndrome. (a) Axial T2W, axial Gd+T1W images during the episode #1. Axial T2W reveals pontine lesion and weakly gadolinium enhancement in axial Gd+T1W. (b) Axial T2W, axial Gd+T1W images 6 months after the episode #1. The lesion was resolved with a sequela on T2W and hypo-intensity is observed in axial Gd+T1W. (c) Axial T2W, axial Gd+T1W images during the episode #2, 1 year after the episode #1. Axial T2W reveals lesion in the medulla oblongata and gadolinium enhancement in the corresponding area. (d) Axial T2W, axial Gd+T1W images during the episode #3, 1 month after episode #2 while the patient was on oral steroid after the administration of intravenous methylprednisolone daily for 7 days. Axial T2W reveals lesion in the medulla oblongata and prominent gadolinium enhancement in the corresponding area
Out of the brainstem, spinal cord involvement is also observed in p-NBS. A long segment myelopathy occurs in most cases, which mimics neuromyelitis optica spectrum disorder (NMOSD) and myelin oligodendrocyte glycoprotein (MOG) antibody-associated disorders (MOGSD) [28,29,30]. However, the recently described “Bagel Sign” pattern of spinal cord involvement in BS may be helpful for differentiating NMOSD and MOG antibody-associated disorders from p-NBS as this pattern has not been observed in these disorders so far [28]. “Bagel Sign” pattern is characterized by a central lesion with a hypo-intense core and a hyper-intense rim, with or without contrast enhancement.
Neuro-psycho-Behçet syndrome may be expressed with a number of symptoms such as euphoria, loss of insight, disinhibition, indifference to the disease, psychomotor agitation, or retardation with paranoid attitudes, and obsessive concerns may be seen in BS with or without cognitive impairment [31, 32].
Given that the subacute progressive presentation of the clinical findings, the distribution of the lesions prominently in the area where the venous anastomosis is few, the significant resolution of the perilesional edema with some small residue, and the pathological findings regarding p-NBS support that the venous pathogenesis plays a major role in the development of p-NBS.
Peripheral nervous system involvement is extremely rare in BS. Mononeuritis multiplex, polyradiculoneuritis, sensorimotor axonal neuropathy, or recurrent episodes of myositis had been reported in BS. However, peripheral neuropathy is much more observed in BS as a result of thalidomide or colchicine treatment rather than the direct involvement of BS [40].
Vascular Involvement
The main type of vascular involvement is cerebral venous sinus thrombosis (CVST) associated with a better prognosis than p-NBS. The clinical manifestations vary by the site and extension of venous thrombosis [33]. Major vascular involvement other than CVST includes aneurysm and/or dissection. The sites of involvement include the common carotid, internal carotid, middle cerebral, superior cerebellar, anterior cerebral, anterior communicating, and vertebral arteries [34].
CVST occurs in up to 20% of BS patients with neurological involvement. In such patients, the principal clinical features (severe headache, papilledema, and sixth-nerve palsy on neurological examination) are compatible with intracranial hypertension [19]. Most studies show that BS-associated CVST has a good prognosis in contrast to other etiologies causing CVST. The systemic features of BS in CVST patients, especially those living in endemic regions, should be looked for. CVST is usually subacute or chronic; only about 25% of cases exhibit clinical features for more than 1 month [35]. Hemiparesis, impaired consciousness, and epileptic seizures are uncommon in CVST patients with NBS. This may be explained by the extremely low probability of seeing hemorrhagic venous infarcts associated with NBS-CVST. Cranial MRI and magnetic resonance venography (MRV) will show that the most commonly involved dural venous sinuses are the superior and transverse sinuses, followed by the sigmoid and straight sinuses [33, 36]. Single-sinus occlusion is more frequent than multiple occlusions [36]. However, if treatment is delayed because of misdiagnosis, multiple sites may be affected in the later stages of BS-CVST and, in a few, may compromise the optic nerves, resulting in blindness. Additionally, clinicians should be aware that cranial MRI and MRV scans may not show sinus thrombosis, even if the clinical findings strongly suggest its presence. In such situations, MRV of the thoracic and cervical venous structures should be evaluated. Irrespective of whether the neuroimaging data are abnormal or normal, we generally perform a spinal tap to study CSF pressure and contents in the suspected cases. Two case series found that CVST was more common in younger patients, supporting the idea that age is important in terms of NBS presentation [37, 38]. Interestingly, despite the observation of an elevated opening pressure, the CSF is free of inflammatory changes in BS-CVST patients.
Vascular involvement other than CNS includes deep venous thrombosis, thrombophlebitis, and pulmonary artery aneurysm, and pulmonary artery aneurysm is a serious cause of morbidity and mortality in BS [39].
The differential diagnosis for NBS is summarized in Table 1 [40].
Pathogenesis
Both innate and adaptive immune systems are thought to play roles in the pathogenesis of BS [3]. Increased Th1, CD4+ and CD8+ T cell, γδ+ T cell, and neutrophil activities have been found both in the serum and in inflamed tissues of BS patients, suggesting the involvement of innate and adaptive immunity in the pathogenesis of BS [41, 42]. However, the exact pathogenesis of the disease remains unknown, but an autoimmune vasculitis predisposed by genetic determinants triggered by exogenous factors is suspected [43].
Microbial infections were thought to trigger BS either directly (streptococci and viruses) or indirectly (via heat shock proteins or molecular mimicry), since the first description of BS [44]. Although laboratory results, including the proliferation of T cells induced by heat shock proteins (HSP) associated with Streptococcus sanguinis, Mycobacterium tuberculosis, and a variety of autoantibodies support autoimmune processes as the cause of BS, it is currently thought that these antibodies are the result of tissue injury rather than the cause of BS [3].
The HLA-B51 allele located in the major histocompatibility (MHC) locus on chromosome 6p21 is strongly associated with BS and is positive in 50–80% of BS patients. However, the HLA-B51 positivity rates differ substantially among regions, and the specificity of HLA-B51 decreases in the population living along the Silk Road [45]. A recent meta-analysis revealed that HLA-B51/B5 is associated with significantly increased disability [46]. The MICA (an MHC class I related gene) and TNF genes were also found to be associated with disease susceptibility when they are present in a MHC locus other than HLA-B51. Nevertheless, it is unclear whether these genes are primarily related to the disease or the result of linkage disequilibrium with HLA-B51 [47]. Moreover, genome-wide association studies did not find an independent association between MICA and BS [48]. In addition to HLA, other candidate BS genes have also been studied. Although polymorphisms in coagulation factor V, endothelial nitric oxide synthase, and intercellular adhesion molecule-1 were found to be associated with BS, the contribution of these genetic variants to disease susceptibility remains unclear due to the limited number of cases in these studies [48]. Recently, a robust genetic association of PSORS1C1 with B and an independent genetic association of HLA-Cw∗1602 with BS, with genome-wide significance, were identified in two independent cohorts [49].
Given the presence of prolonged inflammation (i.e., pathergy), both the innate and adaptive immune systems are thought to be involved in the pathogenesis of BS [50]. Nonetheless, whether this hyperactivity results from autoimmune or autoinflammatory processes remains controversial [51]. Several autoantigens are part of the inflammatory response in BS, including anti-endothelial antigen, retinal S antigen, heat shock proteins (HSP), killer immunoglobulin-like receptors, co-stimulatory molecules, tropomyosin, and oxidized low-density lipoprotein. However, it is unclear whether these are truly pathogenic or the result of the intense inflammation of BS during disease activation [3]. Recently, Lule et al. identified antibodies to human and mouse neurofibrils that cross-react with bacterial HSP-65, which supports the autoimmune disease theory [52].
Several cytokines are known to be elevated isn BS, including IL-1β, tissue necrosis factor α (TNFα), IL-6, IL-10, and IL-23. IL-1β is the principal pro-inflammatory cytokine, and it leads to the expression of many chemokines and secondary mediators of inflammation and upregulates innate immunity in response to infectious agents. Gül et al. strongly implicated IL-1β in BS and observed significant improvements in patients with uveitis treated with IL-1β-regulating antibody [53]. TNFα is another pro-inflammatory cytokine that has been widely investigated in BS. The elevated TNFα levels in BS and significant association between TNFα polymorphisms and BS susceptibility suggest that the treatment of BS with TNFα blockers is reasonable [54]. IL-6 was also found to be elevated in active BS patients compared with inactive BS and healthy controls. Although tocilizumab, an agent that blocks IL-6 signaling, has shown promising results in treating the neurological involvement of BS, the effectiveness of the drug in other forms of BS is controversial [55, 56].
In contrast to other autoimmune disorders, common autoantibodies (e.g., antinuclear antibody), female predominance, and comorbid autoimmune diseases are not observed in BS [50]. Most of the clinical features of BS satisfy some of the clinical criteria of autoinflammatory diseases, such as the self-limited nature of the disease, variable recurrence rate, and spontaneous healing of its lesions without scarring. Other factors argue against it being an autoinflammatory disease, such as the involvement of the retina, vascular structures, and central nervous system during episodes causing permanent damage, the later age of onset, the presence of vasculitis, and the ineffectiveness of IL-1β treatments in BS [3]. Nevertheless, autoinflammatory diseases should be included in the differential diagnosis of BS. Recently, McGonagle et al. proposed a new term called “MHC-I-opathy A” in a group of disease sharing immunopathogenetic basis [57]. This group of disorder mainly consists of BS and clinically distinct spondyloarthropathies whereas they are all associated with MHC Class I alleles, such as HLA-B∗51, HLA-B∗27, and HLA-C∗0602, and epistatic endoplasmic reticulum aminopeptidase 1 (ERAP-1) interactions.
As BS involves both venous and arterial vessels of all sizes, it has been classified as a “variable vessel vasculitis” in the 2012 International Chapel Hill Consensus Conference on the Nomenclature of Vasculitides [58]. The infiltrates in BS are predominantly constituted of neutrophils and lymphocytes. Elevated concentrations of pro-inflammatory cytokines, including IL-8, INF-γ, and TNFα, may be the reason for the neutrophil infiltrates [59]. Unlike the histology of other systemic vasculitides, in BS, these cells are localized around the vessels rather than inside the vessel wall. This histological “perivascular” pattern of BS, which is more similar to neutrophilic dermatosis than to classical systemic vasculitides, has been demonstrated in tissues, especially in mucosal and ocular inflammatory lesions and in pulmonary aneurysms. Similarly, skin pathergy testing reveals perivascular infiltrates of neutrophils and lymphocytes at different time points, however, without the typical features of a “true” vasculitis [60].
CSF Findings
During the acute phase of p-NBS, the CSF shows inflammatory changes in most cases of p-NBS with an increased number of cells, up to a hundred and sometimes more per ml, neutrophils being mostly the predominating cells and modestly elevated protein levels. However, an early lymphocytic pleocytosis is not an exception. When the neutrophilic pleocytosis is the case, it is later replaced by lymphocytes. The oligoclonal band positivity rate is low at a rate of 20% or less [25].
An elevated concentration of IL-6 in the CSF of patients correlating with disease activity has also been reported in p-NBS [61,62,63]. More recently, an increase of CSF IL-10 and CSF/serum matrix metallopeptidase-9 ratio (increased in serum and decreased in CSF compared to multiple sclerosis) was reported and suggested to be a discriminative marker between NBS and multiple sclerosis [64, 65].
Diagnosis
The diagnostic flowchart of NBS is illustrated in Table 2.
Prognosis
Brain stem or spinal cord involvement, frequent relapses, early disease progression, and high CSF pleocytosis are the poor prognostic features for NBS, which was pointed out by International Consensus Recommendation (ICR) [66]. Initiation with severe disability, primary or secondary progressive course, fever at onset, relapse during steroid tapering, meningeal signs, and bladder involvement are possible association with poor outcome. Gender, accompanying systemic features, and age onset do not change the prognosis of NBS [67].
Treatment
Due to multisystemic involvement of BS, long-term treatments should be decided by multidisciplinary team. The first goal of the treatment in NBS is to suppress the acute episode in order to shorten the recovery time with minimal disability, and the second goal is to prevent from further attacks. However, as there are no controlled trials for the management of neurological involvement, long-term treatments depend on the clinical experience rather than trials. In this regard, prognostic factors should be taken into account for choosing the appropriate treatment together with the patients’ age, gender, and patient preferences.
High-dose intravenous methylprednisolone (IVMP) pulse therapy for 5–10 days, followed by a slow oral tapering, is the first choice for treating acute episodes. The dose and duration of steroid treatment vary among centers. Colchicine, azathioprine, cyclosporine, cyclophosphamide, methotrexate, chlorambucil, thalidomide, interferon alpha, anti-TNF agents, and IL-6 blockers are among the drugs used for the preventive treatment of the systemic features of BS, which were tried for CNS involvement as well [40].
Currently, the only drug that has been shown to be effective based on the Class IV evidence is infliximab for the treatment of p-NBS [68, 69]. Although that the efficacy of azathioprine is not clear in NBS, there are a few reports suggesting that it may be effective. Due to the risk of activating latent tuberculosis among patients using infliximab, tuberculosis screening should be conducted prior to the administration of infliximab, and isoniazid prophylaxis (300 mg/day) should be prescribed for 6 or 9 months in patients with latent tuberculosis. In many centers, azathioprine is the first-line drug to be initiated once patients develop p-NBS as also suggested by the 2018 updated European League Against Rheumatism (EULAR) recommendations [69]. We tend to start infliximab in patients in whom azathioprine fails and sometimes as a first-line therapy in patients who present with a severe acute attack of p-NBS and who have poor prognostic factors [68]. Given that the cyclosporine-A is associated with the increased risk of neurological involvement, it should be avoided in patients having NBS and immediately stopped in patients developing NBS under cyclosporine-A [40].
Since the recurrence of CVST is very rare, the duration of azathioprine treatment in CVST is contradictive. In our practice, we usually use azathioprine at least 5 years, and before cessation of azathioprine, we consult the patient with rheumatologists and neuro- ophthalmologist whether AZA is required for systemic features of BS other than CVST.
Mycophenolate mofetil might be reasonable in NBS if gastrointestinal intolerance occur under AZA treatment. The addition of anticoagulant medication to steroids is controversial, as BS patients with CVST are more likely to have systemic large vessel disease, including pulmonary and peripheral aneurysms that carry a high risk of bleeding [69]. The complication rate with warfarin should be considered. Results of anticoagulation treatment in BS are controversial in CVST. Recurrence rate of deep vein thrombosis is more likely to decrease with an immunosuppressant; therefore, the use of immunosuppressants in the treatment of CVST should be the priority.
References
Behçet H. [Uber residivierende, aphtöse, durch ein virus verursachte Geschwüre am Mund, am Auge und an den Genitalien.] Dermatol Woschenscr. 1937;105:1152–7 (In German).
Criteria for diagnosis of Behçet’s disease. International Study Group for Behçet’s disease. Lancet. 1990;335:1078–80.
Yazici H, Seyahi E, Hatemi G, Yazici Y. Behçet syndrome: a contemporary view. Nat Rev Rheumatol. 2018;14(2):107–19.
Salvarani C, Pipitone N, Catanoso MG, et al. Epidemiology and clinical course of Behçet’s disease in the Reggio Emilia area of Northern Italy: a seventeen-year population-based study. Arthritis Rheum. 2007;57(1):171–8.
Yurdakul S, Günaydin TY, Tankurt N, Pazarli H, Ozyazgan Y, Yazici H. The prevalence of Behçet’s syndrome in a rural area in northern Turkey. J Rheumatol. 1988;15(5):820–2.
Hirohata T, Kuratsune M, Nomura A, Jimi S. Prevalence of Behçet’s syndrome in Hawaii. With particular reference to the comparison of the Japanese in Hawaii and Japan. Hawaii Med J. 1975;34(7):244–6.
Papoutsis NG, Abdel-Naser MB, Altenburg A, et al. Prevalence of Adamantiades-Behçet’s disease in Germany and the municipality of Berlin: results of a nationwide survey. Clin Exp Rheumatol. 2006;24(5 Suppl 42):S125.
Gül A, Inanç M, Ocal L, Aral O, Koniçe M. Familial aggregation of Behçet’s disease in Turkey. Ann Rheum Dis. 2000;59(8):622–5.
Moore SB, O’Duffy JD. Lack of association between Behçet’s disease and major histocompatibility complex class II antigens in an ethnically diverse North American Caucasoid patient group. J Rheumatol. 1986;13(4):771–3.
Yazici H, Akokan G, Yalçin B, Müftüoğlu A. The high prevalence of HLA-B5 in Behçet’s disease. Clin Exp Immunol. 1977;30(2):259–61.
Yazici Y, Yurdakul S, Yazici H. Behçet’s syndrome. Curr Rheumatol Rep. 2010;12:429–35.
Yurdakul S, Yazici H. Behcet’s syndrome. Best Pract Res Clin Rheumatol. 2008;22(5):793–809.
Esatoglu SN, Kutlubay Z, Ucar D, Hatemi I, Uygunoglu U, Siva A, et al. Behçet’s syndrome: providing integrated care. J Multidiscip Healthc. 2017;10:309–19.
Mat MC, Goksugur N, Engin B, Yurdakul S, Yazici H. The frequency of scarring after genital ulcers in Behcet’s syndrome: a prospective study. Int J Dermatol. 2006;45(5):554–6.
Cunningham ET Jr, Tugal-Tutkun I, Khairallah M, Okada AA, Bodaghi B, Zierhut M. Behçet Uveitis. Ocul Immunol Inflamm. 2017;25(1):2–6.
Akdal G, Toydemir HE, Saatci AO, et al. Characteristics of optic neuropathy in Behçet disease. Neurol Neuroimmunol Neuroinflamm. 2018;5(5):e490.
Hatemi I, Hatemi G, Çelik AF. Gastrointestinal involvement in Behçet disease. Rheum Dis Clin N Am. 2018;44(1):45–64.
Bicer A. Musculoskeletal findings in Behcet’s disease. Pathol Res Int. 2012;2012:653806.
Siva A, Kantarci OH, Saip S, et al. Behçet’s disease: diagnostic & prognostic aspects of neurological involvement. J Neurol. 2001;248:95–103.
Siva A, Esatoglu SN, Uygunoglu U, et al. Could neurological involvement in Behçet’s disease occur atypically? (P5.410). Neurology. 2018;90(15 Supplement).
Siva A, Saip S. The spectrum of nervous system involvement in Behcet’s syndrome and its differential diagnosis. J Neurol. 2009;256:513–29.
Saip S, Akman-Demir G, Siva A. Neuro-Behçet syndrome. Handb Clin Neurol. 2014;121:1703–23.
Uygunoğlu U, Siva A. Behçet’s syndrome and nervous system involvement. Curr Neurol Neurosci Rep. 2018;18:35.
Siva A. Common clinical and imaging conditions misdiagnosed as multiple sclerosis: A Current Approach to the Differential Diagnosis of Multiple Sclerosis. Neurol Clin. 2018;36(1):69–117.
Saruhan-Direskeneli G, Yentür SP, Mutlu M, Shugaiv E, Yesilot N, Kürtüncü M, et al. Intrathecal oligoclonal IgG bands are infrequently found in neuro-Behçet’s disease. Clin Exp Rheumatol. 2013;31(3 Suppl 77):25–7.
Kocer N, Islak C, Siva A, et al. CNS involvement in neuro-Behcet’s syndrome: an MR study. Am J Neuroradiol. 1999;20:1015–24.
Cohen-Aubart F, Psimaras D, Galanaud D, et al. Cerebral pseudo-tumoral neuro-Behcet: histological demonstration of an inflammatory and vascular disease. Clin Neurol Neurosurg. 2017;161:48–50.
Uygunoglu U, Zeydan B, Ozguler Y, et al. Myelopathy in Behçet’s disease: the Bagel sign. Ann Neurol. 2017;82:288–98.
Lee HS, Kim do Y, Shin HY, Choi YC, Kim SM. Spinal cord involvement in Behcet’s disease. Mult Scler. 2016;22:960–3.
Uygunoglu U, Pasha M, Saip S, Siva A. Recurrent longitudinal extensive transverse myelitis in a neuro-Behcet syndrome treated with infliximab. J Spinal Cord Med. 2015;38:111–4.
Siva A, Özdoğan H, Yazıcı H, Yurdakul S, Yardım M, Akyatan N, et al. Headache, neuro-psychiatric and computerized tomography findings in Behçet’s syndrome. In: Lehner T, Barnes CG, editors. Recent advances in Behçet’s disease. London: Royal Society of Medicine Service; 1986. p. 247–54.
Gündüz T, Emir Ö, Kürtüncü M, Mutlu M, Tumaç A, Akca S, et al. Cognitive impairment in neuro-Behcet’s disease and multiple sclerosis: a comparative study. Int J Neurosci. 2012;122(11):650–6.
Aguiar de Sousa D, Mestre T, Ferro JM. Cerebral venous thrombosis in Behçet’s disease: a systematic review. J Neurol. 2011;258(5):719–27.
Kizilkilic O, Albayram S, Adaletli I, et al. Endovascular treatment of Behçet’s disease-associated intracranial aneurysms: report of two cases and review of the literature. Neuroradiology. 2003;45:328–34.
Yesilot N, Bahar S, Yilmazer S, Mutlu M, Kurtuncu M, Tuncay R, et al. Cerebral venous thrombosis in Behçet’s disease compared to those associated with other etiologies. J Neurol. 2009;256(7):1134–42.
Uluduz D, Midi I, Duman T, et al. Behçet’s disease as a causative factor of cerebral venous sinus thrombosis: subgroup analysis of data from the VENOST study. Rheumatology (Oxford). 2019;58(4):600–8. https://doi.org/10.1093/rheumatology/key153.
Uluduz D, Kürtüncü M, Yapıcı Z, et al. Clinical characteristics of pediatric-onset neuro-Behçet disease. Neurology. 2011;77(21):1900–5.
Shi J, Huang X, Li G, Wang L, Liu J, Xu Y, Zeng X, Zheng W. Cerebral venous sinus thrombosis in Behçet’s disease: a retrospective case-control study. Clin Rheumatol. 2018;37(1):51–7.
Hamuryudan V, Yurdakul S, Moral F, et al. Pulmonary arterial aneurysms in Behçet’s syndrome: a report of 24 cases. Br J Rheumatol. 1994;33(1):48–51.
Uygunoglu U, Saip S, Siva A. Chapter 28: Behcet’s syndrome and nervous system involvement. In: Lisak RP, Truong DD, Carroll WM, et al., editors. International neurology, vol. 2016. 2nd ed. Chichester: John Wiley & Sons, Ltd. p. 88–93.
Alpsoy E. Behçet’s disease: a comprehensive review with a focus on epidemiology, etiology and clinical features, and management of mucocutaneous lesions. J Dermatol. 2016;43(6):620–32.
Direskeneli H, Fujita H, Akdis CA. Regulation of TH17 and regulatory T cells in patients with Behçet disease. J Allergy Clin Immunol. 2011;128(3):665–6.
Davatchi F, Shahram F, Akbarian M, et al. Behçet disease: analysis of 3443 cases. APLAR J Rheumatol. 1997;1:2–5.
Zierhut M, Mizuki N, Ohno S, et al. Immunology and functional genomics of Behçet’s disease. Cell Mol Life Sci. 2003;60(9):1903–22.
Yazıcı H, Fresko I, Yurdakul S. Behçet’s syndrome: disease manifestations, management, and advances in treatment. Nat Clin Pract Rheumatol. 2007;3:151–5.
Maldini C, Lavalley MP, Cheminant M, de Menthon M, Mahr A. Relationships of HLA-B51 or B5 genotype with Behcet’s disease clinical characteristics: systematic review and meta-analyses of observational studies. Rheumatology (Oxford). 2012;51(5):887–900.
Marshall SE. Behçet’s disease. Best Pract Res Clin Rheumatol. 2004;18(3):291–311.
Mizuki N, Meguro A, Ota M, Ohno S, Shiota T, Kawagoe T, et al. Genome-wide association studies identify IL23R-IL12RB2 and IL10 as Behçet’s disease susceptibility loci. Nat Genet. 2010;42:703–6.
Hughes T, Coit P, Adler A, et al. Identification of multiple independent susceptibility loci in the HLA region in Behçet’s disease. Nat Genet. 2013;45(3):319–24.
Direskeneli H. Autoimmunity vs autoinflammation in Behcet’s disease: do we oversimplify a complex disorder? Rheumatology (Oxford). 2006;45(12):1461–5.
Gul A. Behcet’s disease as an autoinflammatory disorder. Curr Drug Targets Inflamm Allergy. 2005;4:81–3.
Lule S, Colpak AI, Balci-Peynircioglu B, et al. Behçet disease serum is immunoreactive to neurofilament medium which share common epitopes to bacterial HSP-65, a putative trigger. J Autoimmun. 2017;84:87–96.
Gül A, Tugal-Tutkun I, Dinarello CA, et al. Interleukin-1β-regulating antibody XOMA 052 (gevokizumab) in the treatment of acute exacerbations of resistant uveitis of Behcet’s disease: an open-label pilot study. Ann Rheum Dis. 2012;71:563–6.
Arida A, Fragiadaki K, Giavri E, Sfikakis PP. Anti-TNF agents for Behçet’s disease: analysis of published data on 369 patients. Semin Arthritis Rheum. 2011;41:61–70.
Addimanda O, Pipitone N, Pazzola G, Salvarani C. Tocilizumab for severe refractory neuro-Behçet: three cases IL-6 blockade in neuro-Behçet. Semin Arthritis Rheum. 2015;44:472–5.
Deroux A, Chiquet C, Bouillet L. Tocilizumab in severe and refractory Behcet’s disease: four cases and literature review. Semin Arthritis Rheum. 2016;45:733–7.
McGonagle D, Aydin SZ, Gül A, Mahr A, Direskeneli H. ‘MHC-I-opathy’-unified concept for spondyloarthritis and Behçet disease. Nat Rev Rheumatol. 2015;11:731–40.
Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013;65(1):1–11.
Neves FS, Spiller F. Possible mechanisms of neutrophil activation in Behçet’s disease. Int Immunopharmacol. 2013;17(4):1206–10.
Ergun T, Gurbuz O, Harvell J, Jorizzo J, White W. The histopathology of pathergy: a chronologic study of skin hyperreactivity in Behcet’s disease. Int J Dermatol. 1998;37:929–33.
Hirohata S, Isshi K, Oguchi H, et al. Cerebrospinal fluid interleukin-6 in progressive neuro-Behçet s syndrome. Clin Immunol Immunopathol. 1997;82(1):12–7.
Akman-Demir G, Tuzun E, Icoz S, et al. Interleukin-6 in neuro-Behçet s disease: association with disease subsets and long-term outcome. Cytokine. 2008b;44(3):373–6.
Hirohata S, Kikuchi H. Changes in biomarkers focused on differences in disease course or treatment in patients with neuro-Behçet’s disease. Intern Med. 2012a;51(24):3359–65.
Aldinucci A, Bonechi E, Biagioli T, et al. CSF/serum matrix metallopeptidase-9 ratio discriminates neuro Behçet from multiple sclerosis. Ann Clin Transl Neurol. 2018;5(4):493–8.
Belghith M, Bahrini K, Kchaou M, Maghrebi O, Belal S, Barbouche MR. Cerebrospinal fluid IL-10 as an early stage discriminative marker between multiple sclerosis and neuro-Behçet disease. Cytokine. 2018;108:160–7.
Kalra S, Silman A, Akman-Demir G, et al. Diagnosis and management of neuro-Behcet’s disease: international consensus recommendations. J Neurol. 2014;261:1662–76.
Al-Araji A, Kidd DP. Neuro-Behçet’s disease: epidemiology, clinical characteristics, and management. Lancet Neurol. 2009;8:192–204.
Zeydan B, Uygunoglu U, Saip S, et al. Infliximab is a plausible alternative for neurologic complications of Behçet disease. Neurol Neuroimmunol Neuroinflamm. 2016;3(5):e258.
Ozguler Y, Leccese P, Christensen R, et al. Management of major organ involvement of Behçet’s syndrome: a systematic review for update of the EULAR recommendations. Rheumatology (Oxford). 2018;57(12):2200–12.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Uygunoglu, U., Siva, A. (2019). Behçet’s Syndrome and the Nervous System Involvement. In: Mitoma, H., Manto, M. (eds) Neuroimmune Diseases. Contemporary Clinical Neuroscience. Springer, Cham. https://doi.org/10.1007/978-3-030-19515-1_22
Download citation
DOI: https://doi.org/10.1007/978-3-030-19515-1_22
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-19514-4
Online ISBN: 978-3-030-19515-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)