Abstract
Traditional pharmacologic approaches to the management of patients with heart failure with reduced systolic function (HFrEF) have been based on neurohormonal inhibition on a background of hemodynamic effects. The agents that have been shown to be associated with improved outcomes in this patient population are inhibitors of the renin-angiotensin-aldosterone (RAAS) system, mineralocorticoids, and beta-blockers. More recently, two agents were FDA-approved for improved outcomes in HFrEF, sacubitril/valsartan, and ivabradine. Sacubitril/valsartan combines RAAS inhibition (valsartan) with inhibition of natriuretic peptide breakdown, while ivabradine is a novel means of heart rate control. While the evidence for clinical benefit of sacubitril/valsartan is substantial, evidence for the use of ivabradine is emerging.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction and Background
Over the past 5 years, two novel FDA-approved agents for the treatment of heart failure have been introduced, the angiotensin receptor-neprilysin inhibitor (ARNi), sacubitril/valsartan (Entresto) , and the funny current (I f) inhibitor ivabradine (Corlanor) . Prior to the approval of these agents, hemodynamic optimization – using vasodilators including hydralazine and isosorbide [1, 4, 5] – and neuro-humoral inhibition, combining angiotensin-converting enzyme inhibition, ß-blockade, and mineralocorticoid-receptor antagonism [2, 3, 6,7,8,9,10,11], have been the evidence-based pharmaceutical approaches to improve outcome in chronic systolic heart failure. The majority of the agents tested in the referenced trials rested on a background of proven hemodynamic benefit. There is a relative paucity of published hemodynamic data for sacubitril/valsartan and ivabradine, as randomized trials for these agents in systolic heart failure have been endpoint-driven. This chapter summarizes the outcome data, quality of life results, and available hemodynamic data for these two drugs. Other modalities which have been shown to improve survival in systolic heart failure include the implantable cardioverter defibrillator, cardiac resynchronization therapy, and left ventricular assist device implantation, but these are not discussed here.
Rationale and Research Leading to Sacubitril/Valsartan
Heart failure activates the sympathetic nervous system (SNS) and the renin-angiotensin-aldosterone system (RAAS) , leading to vasoconstriction and increased sympathetic tone, in turn resulting in downregulation of the ß-receptors. Activation of RAAS leads to increased secretion of angiotensin II and aldosterone, which also results in increased ADH secretion. These neurohormonal maladaptations result in fluid retention, perpetuating the cycle of heart failure. ACE inhibition, or angiotensin receptor blockade, ß-blockade, and mineralocorticoid antagonism modulate the effects of the SNS and RAAS.
Since the early 1980s, the natriuretic peptide system (NPS) began to receive attention as a potential target in heart failure treatment. Within the NPS are three hormones, atrial natriuretic peptide (ANP), B-type natriuretic peptide (BNP), and C-type atrial natriuretic peptide (CNP). While CNP is secreted from endothelial cells and cardiac fibroblasts and has vasodilatory and anti-remodeling effects, ANP and BNP are secreted, respectively, from the atria and the ventricles, are released in response to fiber stretch and volume overload and promote diuresis, natriuresis, and vasodilation, counteracting the maladaptive effects of SNS and RAAS activation [12]. With the development of angiotensin receptor blockers, which exert their effects primarily at the Type 1 angiotensin II receptor, there was hope that a more specific RAAS antagonist would result in further survival improvement in heart failure outcomes. However, while the Valsartan Heart Failure Trial (Val HeFT) [13] (2001) demonstrated reduced heart failure hospitalizations, leading to an FDA-approved indication in heart failure, overall mortality in the valsartan and placebo groups was similar. The demonstration of the beneficial effects of the natriuretic peptides led to the development of human recombinant BNP, namely nesiritide, which was FDA-approved for use in 2001 on the basis of improvement in dyspnea in decompensated heart failure. However, a larger randomized trial released in 2011, the Acute Study of Clinical Effectiveness of Nesiritide in Decompensated Heart Failure (ASCEND-HF) [14], demonstrated no improvement in dyspnea, 30-day mortality, or readmission rates in the nesiritide group. Hypotension was significant in the nesiritide group. As a result, nesiritide is used rarely in practice today, but natriuretic peptide levels remain well established as biomarkers.
Research efforts have been directed at toward identifying agents that could inhibit the enzyme that breaks down endogenous natriuretic peptides, namely, neprilysin. Neprilysin (NEP) is a neutral endopeptidase, and its inhibition increases bioavailability of natriuretic peptides, bradykinin, and substance P, resulting in natriuretic, vasodilatatory, and anti-proliferative effects. The natural hypothesis was that combined inhibition of the RAAS and NEP would result in a better heart failure treatment (Fig. 8.1). This led to the development of omapatrilat, a combined ACEi/NEPi. Several trials of the agent were conducted in heart failure, culminating in the Omapatrilat Versus Enalapril Randomized Trial of Utility in Reducing Events (OVERTURE) Trial [15] in patients with NYHA Functional Class II–IV heart failure. While post hoc analyses appeared to demonstrate potential benefit, there was an increased incidence of life-threatening angioedema, which was substantiated in a subsequent study of the agent in hypertension. These results effectively thwarted ACEi-NPi as a treatment in heart failure.
Angiotensin receptor-neprilysin inhibitors have the potential to modulate two counter-regulatory neurohormonal systems in HF: the renin-angiotensin-aldosterone system and natriuretic peptide system. ANG angiotensin, AT1 angiotensin type 1, HF heart failure, NP natriuretic peptide, RAAS renin-angiotensin-aldosterone system. (Indian Heart Journal Volume 70, Supplement 1, July 2018, Pages S102–S110)
An important advantage of ARBs over ACE is is that ARBs do not block the degradation of bradykinin, the principal instigator of cough, a side effect noted in at least 10% of patients on an ACE, and do not cause angioedema which can occur in about 0.1% of patients on an ACE [16]. Omapatrilat was subsequently demonstrated to inhibit an enzyme responsible for bradykinin metabolism . A logical solution to the adverse effects of omapatrilat was to combine an ARB with an NEPi, termed ARNI or angiotensin receptor-neprilysin inhibitor – LCZ696, Sacubitril/Valsartan. Sacubitril is a prodrug which is converted in the body to sacubitrilat, which inhibits neprilysin and thereby the degradation of NPs. A Phase III trial [17] published in 2010 comparing sacubitril/valsartan to valsartan showed greater reduction in systolic, diastolic, and pulse pressures with sacubitril/valsartan. The Prospective Comparison of ARNI with ARB on Management of Heart Failure with Preserved Ejection Fraction (PARAMOUNT) Trial [18], published in 2012 was a Phase II randomized trial that assessed NT-proBNP after 12 weeks of sacubitril/valsartan compared to valsartan in patients with heart failure with preserved left ventricular ejection fraction (HFpEF). At 12 weeks, NT-proBNP was significantly lower in the sacubitril/valsartan group, and an echocardiographic reduction in left atrial volume and size was also demonstrated. The NT-proBNP lowering effect appeared to be independent of a blood pressure lowering effect of the drug.
Published in 2014, the Prospective Comparison of ARNI with ACEI to Determine Impact on Global Mortality and Morbidity in Heart Failure (PARADIGM-HF) trial randomized 8399 patients with HFrEF (LVEF ≤40%) and NYHA Class II–IV symptoms to sacubitril/valsartan 200 mg PO BID or enalapril 10 mg PO BID (the goal dose from CONSENSUS and SOLVD), in addition to standard therapy for chronic systolic heart failure. The majority of the study population was receiving ß-blockers and mineralocorticoid antagonists. The primary end point of the trial was the combination of death from cardiovascular causes and heart failure hospitalization. There being insufficient Phase II safety data for sacubitril/valsartan, the PARADIGM protocol stipulated safety and tolerability run-ins for all participants in the trial. If participants tolerated both sacubitril/valsartan and enalapril, they were randomly assigned to the two study arms. This approach allowed assessment not only of the end point of the trial but also provided safety and tolerability data. The study was stopped early, after median follow-up of 27 months, when the study met the prespecified cutoff for significant benefit. The ARNI combination resulted in a 20% decrease in the primary end point, HR = 0.80, P < 0.001, giving a Number Needed to Treat of 21. The study drug also reduced the individual components of the combined end point, death from cardiovascular cause by 20% and heart failure hospitalizations by 21%, both p < 0.001. All-cause mortality in the sacubitril/valsartan arm was reduced by 16%, HR = 0.84, p < 0.001. While sacubitril/valsartanb resulted in 14% experiencing hypotension as compared to 9% in the enalapril arm, the discontinuation rate was not significantly different (sacubitril/valsartan 0.9%, enalapril 0.7%). No significant difference was noted in the occurrence of non-serious angioedema between the two groups.
In secondary analyses, sacubitril/valsartan demonstrated clinical benefits in other indices of heart failure progression, including improved NYHA class, reduced need for intensification of medical treatment, and reduction in the need for emergency department visits, intensive care, and inotropic support. Other findings from PARADIGM-HF include significantly lower NT-proBNP and troponin levels in the sacubitril/valsartan group, significant reduction in the incidence of sudden cardiac death and death from worsening heart failure independent of cardioverter defibrillation implantation, and a non-significant reduction in the need for left ventricular assist device implantation and cardiac transplantation. The PARADIGM-HF investigators also carried out a comparison of the sacubitril/valsartan arm with the treatment arms of the SOLVD Trial (enalapril) and the CHARM-Alternative Trial [19] (candesartan) and found substantial relative risk reductions for both the composite end point and for cardiovascular death. Using the Kansas City Cardiomyopathy Questionnaire, the PARADIGM-HF investigators [20] demonstrated remarkable improvement in physical and social activity limitations with sacubitril/valsartan compared to enalapril. The largest improvements were reported in household chores (p < 0.001) and sexual relationships (p = 0.002); these benefits persisted through 36 months of assessment. In another secondary analysis [21], the PARADIGM-HF investigators found the frequency of episodes of hyperkalemia to be significantly greater in the enalapril arm compared to ARNI, (3.1 versus 2.2 incidents per 100 patient-years, HR = 1.37, CI 1.06–1.76, p = 0.02) for patients already taking a mineralocorticoid antagonist.
Criticisms of the PARADIGM-HF Trial include that the study was predominantly white (66%), male (78%), and enrolled predominantly NYHA Functional Class II (70%) patients. Only 5% of the study population was black, perhaps limiting the ability of the study to accurately detect the incidence of angioedema. It has also been suggested that the enalapril dose in PARADIGM-HF was too low [22]. Narrowly defined, only patients with systolic heart failure and an ejection fraction of ≤35% would be candidates for the drug, based on PARADIGM-HF entry criteria. An additional criticism is that neprilysin has been shown to have a role in maintaining homeostasis of amyloid-ß peptide, raising the issue that a neprilysin inhibitor might lead to increased deposits of this protein in brain [11]. However, in a randomized, double-blind trial measuring sacubitril/valsartan levels in cerebrospinal fluid in healthy human subjects [23], sacubitril/valsartan did not cause changes in aggregable amyloid β isoforms compared with placebo, despite achieving CSF concentrations of a metabolite of sacubitril/valsartan sufficient to inhibit neprilysin.
The Prospective Comparison of ARNI with ARB Global Outcomes in HF With Preserved Ejection Fraction (PARAGON-HF Trial) [24], a prospective randomized trial of the impact of sacubitril/valsartan in HFpEF, has completed enrollment and has an estimated study completion date of March 15, 2019 (clinicaltrials.gov). Serial cognitive testing is being carried out in PARAGON-HF in an effort to assess the impact of sacubitril/valsartan on cognition.
In summary, in prespecified measures of nonfatal clinical deterioration of heart failure, the PARADIGM-HF investigators demonstrated that the combination of sacubitril/valsartan prevented the clinical progression of surviving heart failure patients more effectively than did enalapril alone [25]. On the basis of the PARADIGM-HF Trial, sacubitril/valsartan was FDA-approved in July 2015 to reduce the risk of death and hospitalization for heart failure in patients with chronic heart failure (NYHA Class II–IV) and reduced ejection fraction.
The comParIson Of sacubitril/valsartaN versus Enalapril on Effect on nt-pRo-bnp in patients stabilized from an acute Heart Failure (PIONEER-HF) trial (PMID:30415601) enrolled 881 patients with heart failure with reduced ejection fraction who were hospitalized for acute decompensated heart failure at 129 sites in the United States. After hemodynamic stabilization, patients were randomly assigned to receive either sacubitril–valsartan (target dose, 97 mg of sacubitril with 103 mg of valsartan twice daily) or enalapril (target dose, 10 mg twice daily). The primary efficacy outcome was the time-averaged proportional change in the N-terminal pro–B-type natriuretic peptide (NT-proBNP) concentration from baseline through weeks 4 and 8. Key safety outcomes were the rates of worsening renal function, hyperkalemia, symptomatic hypotension, and angioedema.
The investigators noted that time-averaged reduction in the NT-proBNP concentration was significantly greater in the sacubitril–valsartan group than in the enalapril group. In addition, the two drugs appeared to be equally safe; the rates of worsening renal function, hyperkalemia, symptomatic hypotension, and angioedema did not differ significantly. In an analysis of exploratory clinical outcomes, the in-hospital initiation of sacubitril–valsartan therapy was associated with a lower rate of rehospitalization for heart failure at 8 weeks than enalapril therapy.
Pharmacokinetics of Sacubitril/Valsartan
Absorption of sacubitril/valsartan is rapid, with maximum levels of sacubitril, sacubitrilat, and valsartan all achieved by 2–3 h [26]. With twice-daily dosing, steady-state concentrations are reached within 3 days. Sacubitril is eliminated as predominantly sacubitrilat by the kidney, while valsartan is eliminated by the biliary route. In heart failure patients, area under the concentration-time curves for sacubitril, sacubitrilat, and valsartan was higher. Renal impairment had no impact on sacubitril or valsartan, but increased the area under the concentration-time curve for sacubitrilat. Moderate hepatic impairment increased the area under the concentration-time curve of valsartan and sacubitrilat approximately two-fold. Regarding drug-drug interactions, sacubitril/valsartan increased plasma concentrations of atorvastatin. Pharmacokinetics of the drug were not affected by age, sex, or ethnicity.
Hemodynamic Impact of Sacubitril/Valsartan
Surprisingly little specific functional and hemodynamic data are available regarding sacubitril/valsartan. A post hoc analysis of the PARAGIGM-HF demonstrated that the drug was effective at reducing cardiovascular death and heart failure hospitalization across the spectrum of left ventricular ejection fraction (LVEF), when assessed in stepwise 5-point reductions in LVEF [27]. Addition of sacubitril/valsartan in patients with advanced systolic heart failure may be a useful strategy to improve hemodynamics and to potentially facilitate the transitioning from intravenous HF therapies.
Ivabradine
Background and Pharmacology
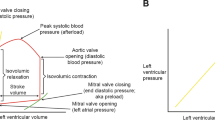
The search for a direct sinoatrial node inhibitor began four decades ago. Ivabradine was the first drug specifically developed as a heart rate lowering agent, and in Europe was initially considered for the treatment of angina pectoris. Sinoatrial myocytes have the capacity to develop slow diastolic depolarizations, driving membrane voltage toward the threshold for initiating an action potential (Fig. 8.2). Sinoatrial node activity involves several ionic currents flowing through channels, including the funny or hyperpolarization-activated cyclic nucleotide-gated channel that regulates the I f current, so-called for its unusual properties compared with other channels at the time of its discovery. The I f current is carried across the sarcolemma by both sodium and potassium ions, is directly activated by cyclic adenosine monophosphate (cAMP), and is related to I h neuronal channels. Ivabradine has substantial selectivity for inhibiting the I f channel at doses that allow heart rate slowing [28]. Studies in experimental models have demonstrated that ivabradine has a pure heart rate lowering effect, does not affect LV contractile state [29], and does not have negative lusitropic properties. In healthy volunteers, equipotent doses of ivabradine (30 mg) and propranolol (40 mg) had similar effects on heart rate and heart rate variability, whereas propranolol was associated with significant systolic and mean blood pressure lowering, and a greater decrease in cardiac output measured noninvasively, compared to ivabradine, placebo, or both [30]. Under fasting conditions, peak plasma ivabradine concentrations are reached in approximately 1 hour. Food delays absorption by approximately 1 hour but appears to increase plasma levels of the drug. Ivabradine is extensively metabolized in the liver. The excretion of ivabradine and its metabolites is both renal and hepatic. The half-life of ivabradine and its metabolites requires twice-daily dosing. There is no direct effect of ivabradine on the QT interval. Phosphenes, the off-target effect of ivabradine, are bright sensations not mediated by retinal stimuli, due to effects on hyperpolarization-activated channels in the retina.
Ivabradine’s primary mechanism of action on cardiac tissue is on the sinoatrial (SA) node, which occupies a predominantly subepicardial position at the junction of the superior vena cava (SVC) and the right atrium (RA). (a) Heart with position of the Sinoatrial (SA) node. (b) In the sinoatrial node, ivabradine blocks the intracellular aspect of the hyperpolarization-activated cyclic nucleotide-gated (HCN) transmembrane channel, which is responsible for the transport of sodium (Na+) and potassium (K+) ions across the cell membrane, in the open state. This results in the inhibition of the inward funny current (I f), which is specifically activated at hyperpolarized membrane potentials. (c) By selectively inhibiting I f, there is a reduction in the slope of diastolic depolarization of the pacemaker action potential (shaded region) and an increase in the duration of diastole, without altering other phases of the action potential. This results in heart rate reduction. Ao aorta, IVC inferior vena cava, PA pulmonary artery, RV right ventricle. (PMID:28958335)
While ivabradine was initially targeted as a drug for heart rate control, randomized data failed to demonstrate a significant advantage in patents with stable coronary artery disease without clinical heart failure [31]. Similarly, ivabradine compared to placebo did not significantly improve the change in physical limitation score at 1 year in patients with anginas pectoris [32], although ivabradine patients had better angina scores compared to placebo on the Seattle Angina Questionnaire on every visit to 36 months. Ivabradine did not result in significant exercise tolerance testing benefit, compared to low-dose atenolol, and no advantage was noted when added to full-dose amlodipine [33, 34].
Because of the documented beneficial effect of heart rate lowering in heart failure with reduced ejection fraction, ivabradine was tested in this setting, beginning with the Morbidity-Mortality Evaluation of the I f Inhibitor Ivabradine in Patients With Coronary Artery Disease and Left Ventricular Dysfunction (BEAUTIFUL) Trial [35], a randomized double-blind, placebo-controlled trial of 10,917 patients. Enrollment characteristics included LVEF <40%, 85% NYHA Class II and III, 83% male, and 87% were taking ß-blockers. At a median of 19 months of follow-up, no difference was found between the ivabradine and placebo groups for the composite end point of cardiovascular death, hospitalization for myocardial infarction (MI), or hospitalization for worsening heart failure. A subgroup analysis of 14% of patients with activity-limiting angina had reduction in hospitalization for MI and borderline reduction in the composite end point (p = 0.05); the difference was statistically significant for patients in this subgroup with baseline heart rate ≥ 70 [36].
To investigate the potential benefits on ischemia seen in this subgroup, the SIGNIFY [37] Trial was undertaken, enrolling 19,102 patients with stable coronary artery disease who did not have clinical heart failure. This study again enrolled predominantly male patients; 75% had angina pectoris, and the mean LV ejection fraction was 56%. While heart rate was significantly reduced by ivabradine, there was no significant benefit of ivabradine on the primary composite end point of cardiovascular death or nonfatal MI after median follow-up of 28 months. When the prespecified subgroup with activity-limiting angina was analyzed for the composite outcome, there was in fact evidence of harm with ivabradine therapy; an absolute increase in the composite end point of 1.1% (p = 0.02). The reason or reasons for this adverse outcome remain unclear, but the conclusion to be drawn from trials of ivabradine in angina pectoris without LV systolic dysfunction is that no benefit occurs, and even though there may be symptomatic improvement, those patients appear to be at greater risk of an adverse effect of the drug.
The Systolic Heart Failure Treatment with the I f-inhibitor Ivabradine (SHIFT) Trial [38] randomized 6505 patients with ischemic and nonischemic heart failure, NYHA Class II–IV but predominantly Class II–III, LVEF ≤35%, to ivabradine or placebo. The trial randomized no patients from the United States; most patients were male, 89% taking ß-blockers, 91% ACEi or ARB, 60% aldosterone antagonists, 22% a digitalis preparation. More than two-thirds achieved the target dose of 7.5 mg ivabradine twice daily. Compared to placebo, the composite end point of cardiovascular death or first hospitalization for heart failure was significantly reduced (hazard ratio 0.82, p < 0.0001, driven primarily by reduction in HF hospitalization) (Fig. 8.3) Trends were detected for less benefit in patients also receiving ß-blockers and greater benefit for nonischemic patients. There were significant improvements in the NYHA Class and Kansas City Cardiomyopathy Questionnaire summary scores [39]. When patients with baseline heart rate ≥70 from BEAUTIFUL and SHIFT were pooled, no significant impact on mortality could be demonstrated. An echo substudy [40] from SHIFT of 275 patients demonstrated a small but significant increase on LVEF after 8 months of ivabradine therapy (4 ± 10%, p = 0.004).
Approval timeline of ivabradine across Europe and the United States. The indications for the use of ivabradine have evolved over time and differ based on region. Since it was first approved for use in angina by the European Medicines Agency (EMA) in 2005, the findings of several randomized controlled trials have resulted in expanded indications to include select heart failure patients and only recent approval by the US Food and Drug Administration (FDA) for this indication. BEAUTIFUL Morbidity-Mortality Evaluation of the I f-Inhibitor Ivabradine in Patients With Coronary Disease and Left Ventricular Dysfunction, CAD coronary artery disease, CV cardiovascular, HFrEF heart failure with reduced ejection fraction, LVEF left ventricular ejection fraction, MI myocardial infarction, NYHA New York Heart Association, NSR normal sinus rhythm, SHIFT Systolic Heart Failure Treatment with the I f-Inhibitor Ivabradine Trial, SIGNIFY Study Assessing the Morbidity-Mortality Benefits of the I f-Inhibitor Ivabradine in Patients With Coronary Artery Disease. (PMID:28958335)
Shortcomings of the SHIFT Trial include that 25% of trial participants were not taking a ß-blocker for HRrEF and that ivabradine did not significantly reduce any end point in patients with baseline HR ≤ 75 bpm. Whereas trials of carvedilol, metoprolol succinate, and bisoprolol demonstrated consistent survival benefit, a similar heart rate reduction by ivabradine resulted in no all-cause survival benefit. Another SHIFT subgroup analysis demonstrated that a statistically significant improvement for the primary end point occurred only for patients <50% of target ß-blocker doses [41]. Thus, ivabradine appeared to exert a beneficial effect only in patients who were also being treated with ß-blockers in whom a heart rate goal of ≤75 bpm had not been achieved. Regarding adverse effects, ivabradine increased the frequency of bradycardia , both asymptomatic and symptomatic, was associated with an increased incidence of atrial fibrillation, and resulted in some ivabradine withdrawals due to phosphenes, which resolved upon discontinuation of drug. The 1.7% increase in the risk of atrial fibrillation noted in pooled BEAUTIFUL and SHIFT data underscore the importance of observing patients on ivabradine for this rhythm disturbance, especially in view of the negative prognostic impact of atrial fibrillation on systolic heart failure. The FDA approved ivabradine in April 2015 for patients with HFrEF with LVEF ≤35% on a ß-blocker at the maximum tolerated dose, with HR ≥ 70 bpm (Fig. 8.4). The drug is contraindicated in patients with sinus node dysfunction or atrioventricular block. The FDA approval underscores the prerequisite for guideline-based treatment with maximally tolerated ß-blockers proven effective in HFrEF. In such patients in whom HR remains >70–75 beats per minute, the addition of ivabradine is reasonable. For patients with HFrEF who are proven intolerant of ß-blockers, treatment with ivabradine appears reasonable, keeping in mind that while ivabradine results in decreased heart rate, the exact mechanism of benefit remains uncertain.
Kaplan-Meier cumulative event curves for different end points in SHIFT. Primary composite outcome (Panel A); cardiovascular mortality or heart failure hospitalization and its two components cardiovascular mortality (Panel B); heart failure hospitalizations (Panel C) and heart failure deaths (Panel D) in the ivabradine and the placebo arms. CV cardiovascular, HF heart failure, SHIFT Systolic Heart Failure Treatment with the I f-Inhibitor Ivabradine Trial. (Swedberg et al.; SHIFT Investigators. Lancet. 2010;376:875–885)
Questions remain regarding the efficacy of ivabradine. From a recent meta-analysis of the ivabradine trials [42], the authors concluded that while use of ivabradine in patients with HFrEF in sinus rhythm with HR ≥ 70 to reduce HF hospitalization was supported by the literature, the strength of the evidence was such that more widespread adoption of ivabradine in HF would require additional randomized trials. Recent guideline updates [43] emphasize adherence to the ivabradine FDA package indication.
On the other hand, the guidelines advise that for any patient in NYHA Class II–IV HFrEF not on an ARNI, the threshold to consider discontinuing an ACEi or ARB in favor of sacubitril/valsartan should be low [44]. The number of women and ethnicities different from white in many of the foregoing trials is low enough that one might question scientific efficacy of these agents in these populations. For further guidance on the use of sacubitril/valsartan and ivabradine, the reader is referred to the 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure [43] and the 2017 ACC Expert Consensus Decision Pathway for Optimization of Heart Failure Treatment [44].
References
Cohn JN, Archibald DG, Ziesche S, et al. Effect of vasodilator therapy on mortality in chronic congestive heart failure. N Engl J Med. 1986;314:1547–52.
CONSENSUS Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure. N Engl Med. 1987;316:1429–35.
SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 1991;325:293–302.
Cohn JN, Johnson G, Ziesche S, et al. A comparison of enalapril with hydralazine-isosorbide dinitrate in the treatment of chronic congestive heart failure. N Engl J Med. 1991;325:303–10.
Taylor AL, Ziesche S, Yancy C, et al. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N Engl J Med. 2004;351:2049–57.
Packer M, Coats AJ, Fowler MB, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med. 2001;344:1651–8.
MERIT-HF Study Group. Effect of metoprolol CR/XL in chronic heart failure: metoprolol CR/XL randomised intervention trial in congestive heart failure (MERIT-HF). Lancet. 1999;353:2001–7.
Pitt B, Zannad F, Remme WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized aldactone evaluation study investigators. N Engl J Med. 1999;341:709–17.
Kagawa CM, Sturtevant FM, Van Arman CG. Pharmacology of a new steroid that blocks salt activity of aldosterone and desoxycorticosterone. J Pharm Exp Ther. 1959;126:123–30.
Zannad F, McMurray JJ, Frum H, et al. Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med. 2011;364:11–21.
Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med. 1997;336:525–33.
Srikanth Y, Aronow WS, Mondal P, Chabbott DR. The evolution of natriuretic peptide augmentation in management of heart failure and the role of sacubitril/valsartan. Arch Med Sci. 2017;13:1207–16.
Cohn JN, Tognoni G, for the Valsartan Trial Investigators. A randomized trial of the angiotensin receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001;345:1667–1675.
O’Connor CM, Starling RC, Hernandez AF, et al. Effect of nesiritide in patients with acute decompensated heart failure. N Engl J Med. 2011;365:32–43.
Packer M, Califf RM, Konstam MA, et al. Comparison of omapatrilat and enalapril in patients with chronic heart failure: the Omapatrilat Versus Enalapril Randomized Trial of Utility in Reducing Events (OVERTURE). Circulation. 2002;106:920–6.
Braunwald E. The path to an angiotensin receptor neprilysin inhibitor in the treatment of heart failure. J Am Coll Cardiol. 2015;65:1029–41.
Ruilope LM, Dukat A, Bohm M, et al. Blood-pressure reduction with LCZ696, a novel dual-acting inhibitor of the angiotensin II receptor and neprilysin: a randomised, double-blind, placebo-controlled, active comparator study. Lancet. 2010;375:1255–66.
Solomon SD, Zile M, Pieske B, et al. The angiotensin receptor neprilysin inhibitor LCZ696 in heart failure with preserved ejection fraction: a phase 2 double-blind randomised controlled trial. Lancet. 2012;380:1387–95.
Young JB, Dunlap ME, Pfeffer MA, et al. Mortality and morbidity reduction with candesartan in patients with chronic heart failure and left ventricular systolic dysfunction: results of the CHARM low-left ventricular ejection fraction trials. Circulation. 2004;110:2618–26.
Chandra A, Lewis EF, Claggett BL, et al. Effects of sacubitril/valsartan on physical and social activity limitations in patients with heart failure: a secondary analysis of the PARADIGM-HF trial. JAMA Cardiol. 2018;3:498–505. https://doi.org/10.1001/jamacardio.2018.0398 . Published online April 4.
Desai AS, Vardeny O, Claggett B, et al. Reduced risk of hyperkalemia during treatment of heart failure with mineralocorticoid receptor antagonists by use of sacubitril/valsartan compared with enalapril: a secondary analysis of the PARADIGM-HF trial. JAMA Cardiol. 2017;2:79–85.
Bernardez-Pereira S, Ramires FJA, de Melo RFT, Pereira-Barretto AC. Was the enalapril dose too low in the PARADIGM-HF trial? Cardiol Rev. 2018; https://doi.org/10.1097/CRD.0000000000000193. [Epub ahead of print]
Langenickel TH, Tsubouchi C, Ayalasomayajula S, et al. The effect of LCZ696 (sacubitril/valsartan) on amyloid-ß concentrations in cerebrospinal fluid in healthy subjects. Br J Clin Pharmacol. 2016;81:878–90.
Solomon SD, Rizkala AR, Gong J, et al. Angiotensin receptor neprilysin inhibition in heart failure with preserved ejection fraction: rationale and design of the PARAGON-HF Trial. JACC Heart Fail. 2017;5:471–82.
Packer M, McMurray JJ, Desai AS, et al. Angiotensin receptor neprilysin inhibition compared to enalapril on the risk of clinical progression in surviving patients with heart failure. Circulation. 2015;131:54–61.
Ayalasomayajula S, Langenickel T, Pal P, et al. Clinical pharmacokinetics of sacubitril/valsartan (LCZ696): a novel angiotensin receptor neprilysin inhibitor. Clin Pharmacokinet. 2017;56:1461–78.
Solomon SD, Claggett B, Desai AS, et al. Influence of ejection fraction on outcomes and efficacy of sacubitril/valsartan (LCZ696) in heart failure with reduced ejection fraction. The prospective comparison of ARNI with ACEI to determine impact on global mortality and morbidity in heart failure (PARADIGM-HF) trial. Circ Heart Fail. 2016;9:e002744.
Sulfi S, Timmis AD. Ivabradine – the first selective sinus node I f channel inhibitor in the treatment of stable angina pectoris. Int J Clin Pract. 2006;60:222–8.
Vilaine JP, Bidouard JP, Lesage L, et al. Anti-ischemic effects of ivabradine, a selective heart rate-reducing agent, in exercise-induced myocardial ischemia in pigs. J Cardiovasc Pharmacol. 2003;42:688–96.
Joannides R, Moore N, Iacob M, et al. Comparative effects of ivabradine, a selective heart rate lowering agent, and propranolol on systemic and cardiac haemodynamics at rest and during exercise. Br J Clin Pharmacol. 2006;61:127–37.
Borer JS, Fox K, Jaillon P, et al. Antianginal and antiischemic effects of ivabradine, and I f inhibitor, in stable angina: a randomized, double-blind, multicentered, placebo-controlled trial. Circulation. 2003;107:817–23.
Tendera M, Chassany O, Ferrari R, et al. Quality of life with ivabradine in patients with angina pectoris. The study assessing the morbidity and mortality benefits of the I f inhibitor ivabradine in patients with stable coronary artery disease quality of life substudy. Circ Cardiovasc Qual Outcomes. 2016;9:31–8.
Tardif JC, Ponikowski P, Kahan T, et al. Efficacy of the I f current inhibitor ivabradine in patients with chronic stable angina receiving beta blocker therapy: a 4-month, randomize, placebo-controlled trial. Eur Heart J. 2009;30:540–8.
European Medicines Agency. Ivabradine: European public assessment report – scientific discussion. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Scientific_Discussion/human/000597/WC500043587.pdf
Fox K, Ford I, Steg PG, et al. Ivabradine for patients with stable coronary artery disease and left-ventricular systolic dysfunction (BEAUTIFUL): a randomised, double-blind, placebo-controlled trial. Lancet. 2008;372:807–16.
Fox K, Ford I, Steg PG, et al. Relationship between ivabradine treatment and cardiovascular outcomes in patients with stable coronary artery disease and left ventricular systolic dysfunction with limiting angina: a subgroup analysis of the randomized, controlled BEAUTIFUL trial. Eur Heart J. 2009;30:2337–45.
Fox K, Ford I, Steg PG, et al. Ivabradine in stable coronary artery disease without clinical heart failure. N Engl J Med. 2014;371:1091–9.
Swedberg K, Komaida M, Bohm M, Borer JS, et al. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled trial. Lancet. 2010;376:875–85.
Ekman I, Chassany O, Komajda M, et al. Heart rate reduction with ivabradine and health related quality of life in patients with chronic heart failure: results from the SHIFT study. Eur Heart J. 2011;32:2395–404.
Tardif JC, O’Meara E, Komajda M, SHIFT Investigators, et al. Effects of selective heart rate reduction with ivabradine on left ventricular remodelling and function: results from the SHIFT echocardiography substudy. Eur Heart J. 2011;32:2507–15.
Böhm M, Borer J, Ford I, et al. Heart rate at baseline influences the effect of ivabradine on cardiovascular outcomes in chronic heart failure: analysis from the SHIFT study. Clin Res Cardiol. 2013;102:11–22.
Narayanan MA, Reddy YNV, Baskaran J, et al. Ivabradine in the treatment of systolic heart failure – a systematic review and meta-analysis. World J Cardiol. 2017;9:182–90.
Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2017;70:776–803.
Yancy CW, Januzzi JL, Allen LA, et al. 2017 ACC expert consensus decision pathway for optimization of heart failure treatment: answers to 10 pivotal issues about heart failure with reduced ejection fraction: a report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. J Am Coll Cardiol. 2018;71:201–30.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Booth, D.C., Rajagopalan, N. (2019). Recently Approved Pharmacologic Agents to Improve Outcomes in Heart Failure. In: Askari, A., Messerli, A. (eds) Cardiovascular Hemodynamics. Contemporary Cardiology. Humana, Cham. https://doi.org/10.1007/978-3-030-19131-3_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-19131-3_8
Published:
Publisher Name: Humana, Cham
Print ISBN: 978-3-030-19130-6
Online ISBN: 978-3-030-19131-3
eBook Packages: MedicineMedicine (R0)