Abstract
In at least half the patients diagnosed with noncompaction cardiomyopathy (NCCM) genetics plays an important role. In familial NCCM, like in other inherited cardiomyopathies, timely identification and treatment of relatives at risk is important. This chapter focusses on the process of identifying a genetic cause, predicting risk for relatives, informing index cases and relatives on subsequent recommendations for family screening.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Left ventricular non-compaction
- LVNC
- Familial noncompaction cardiomyopathy
- NCCM
- Genetic noncompaction
- Sarcomere gene mutation
- Familial risk
- Family screening for cardiomyopathy
- Genetic counseling for cardiomyopathy
Introduction
Noncompaction cardiomyopathy (NCCM) is characterized by endocardial hypertrabeculation of the myocardium of the left ventricle. In 1997 the first genetic cause for NCCM, a mutation in the X-linked TAZ gene, was identified in a family were six boys had Barth syndrome with hypertrabeculation of the left ventricle [1]. The link of familial NCCM to defects in the sarcomere genes that had previously been linked to the more frequent hereditary hypertrophic (HCM) and dilated cardiomyopathies (DCM) , came in 2007 by the report of MYH7 mutations in NCCM and was followed by reports of other sarcomere gene mutations in familial NCCM [2, 3].
In NCCM the sarcomere genes are the most prevalent genetic causes. More recently the introduction of next generation sequencing (NGS) , allowing simultaneous analysis of panels of 50 or more cardiomyopathy genes, showed that around 35% of NCCM patients have a mutation, and that mutations occur more frequently in children diagnosed with NCCM than in patients diagnosed as adults [4, 5].
Overall, approximately 50% of NCCM patients are considered to have a genetic cause [4]. Some because they have inherited a mutation in a cardiomyopathy gene, other patients have family members with a cardiomyopathy without having a mutation in a known cardiomyopathy gene. In 45% of familial NCCM no mutation can be identified [4], indicating that many genetic causes for NCCM are still unknown. Overall around 50% of cases diagnosed today with NCCM have no mutation in a cardiomyopathy gene or familial disease. In these -mostly adult patients- NCCM may be attributed to non-genetic, secondary causes for hypertrabeculation. Alternatively, these cases may have yet unknown (complex) genetic cause(s) carrying small risk for relatives [4]. For NCCM, like for HCM and DCM, it is important for relatives of patients to be informed about the increased risk of having a cardiomyopathy.
For that reason referral of patients diagnosed with NCCM for genetic counseling , has become common practice [6]. This allows, by taking family histories and performing DNA testing of the index case, to estimate the risk for relatives to have NCCM. When there is a mutation, DNA testing for the familial mutation of first degree relatives is advised, with subsequent cardiologic screening of mutation carriers. In NCCM genetic defects may predict risk of having severe cardiac events (MACE ). Some genes, like MYH7, carry lower risk for MACE than other genes. In this perspective DNA testing may help stratify risk for MACE of patient and relatives and help guide clinical management of genetic NCCM accordingly [4]. For families of patients without a mutation, cardiologic screening of first degree relatives is recommended, also in absence of a family history of cardiomyopathy, because we cannot exclude that these patients may have an unknown genetic predisposition with low penetrance that conveys a small risk to relatives.
The aim of this chapter is to give an overview of the genetic causes for NCCM, and describe the routine of genetic diagnostics i.e. genetic counseling, DNA testing and initiating family screening. Illustrating in this way the importance of integrating genetic diagnostics to clinical management of NCCM patients by conveying appropriate information to patients and their families, in order to make early diagnosis and timely treatment accessible for the families of all NCCM patients.
The Genetics of NCCM
Genetics plays a more important role in some patients with hypertrabeculation of the left ventricle than in others. Currently three main categories of genetic burden for noncompaction are recognized (Fig. 8.1). (1) Patients with a genetic noncompaction cardiomyopathy . These are the patients with a mutation in a cardiomyopathy gene and/or relatives with a cardiomyopathy (familial cardiomyopathy ). In genetic NCCM relatives have an increased risk of having a cardiomyopathy. In 45% of familial NCCM no mutation is found, indicating that not all NCCM genes have been identified yet [4]. The majority of the genes associated with NCCM also play an important role in genetic hypertrophic (HCM) and dilated cardiomyopathy (DCM) [7, 8]. For now, there is no explanation how overlapping genetic defects in these sarcomere genes cause the spectrum of phenotypes ranging from hypertrophic, dilated and noncompaction cardiomyopathy. (2) Cardiomyopathy patients with noncompaction without a genetic cause; in these ‘sporadic’ NCCM cases no evidence for a genetic cause is found by DNA analysis, and the family history and/ or family screening are uninformative. These patients have similar cardiac outcomes as genetic NCCM patients. In sporadic patients NCCM may be the result of pathologic cardiac remodeling, activated by other (now unknown genetic or non-genetic) causes leading to hypertrabeculation. In these patients high incidences of left bundle branch blocks were identified [4]. Also cardiac comorbidities like hypertension may play a role in these patients [4]. We cannot exclude that apparently sporadic patient may have defect in a yet unknown cardiomyopathy gene, since not all cardiomyopathy genes have been identified yet. We know that at least one third of the NCCM patients with a mutation in a cardiomyopathy gene, did not report familial disease, indicating that negative family history does not exclude a genetic cause [4]. Another possibility is that a group of apparently sporadic NCCM patients may have variants in known or unknown cardiomyopathy genes that have insufficient genetic effects and need additional interaction with other genetic or non-genetic factors to cause NCCM. (3) Healthy individuals with a benign LV hypertrabeculation ; large population based studies have reported that LV hypertrabeculation may occur as frequently as in 43% of the healthy adult population [9]. A higher susceptibility for having more prominent trabeculations, without features of a cardiomyopathy was reported in blacks and athletes [10, 11]. The cause might be a genetic or epigenetic regulation of gene expression or translation, activating similar pathways as mutations in sarcomere genes, causing hypertrabeculation without cardiomyopathy. The high incidence of hypertrabeculation supports that the currently used echo and MRI diagnostic criteria, relying on the ratio between noncompacted and compacted layer of myocardium, cannot distinguish pathologic noncompaction cardiomyopathy from benign, sometimes reversible, left ventricle hypertrabeculation without cardiomyopathy and therefore more sensitive diagnostic criteria are needed.
NCCM Genes
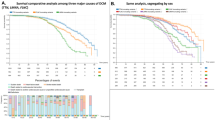
In familial NCCM around 55% of NCCM patients have a mutation, indicating that the genetic cause has not been found for a large proportion of familial NCCM [4]. In children and in adult patients the majority of the mutations occur in genes encoding for proteins of the cardiac sarcomere structure and function (Fig. 8.2) [4]. Less frequent genetic causes for NCCM are defects in genes encoding for intracellular signaling, homeostasis and cytoskeletal integrity associated with NCCM [12]. Genetic causes are identified more frequently in patients diagnosed in childhood than in adults with NCCM [4]. These observations show how little we understand about the development of the hypertrabeculation, because they suggest that the genetic effects might involve cardiac development as well as cardiac remodeling at older age.
Genes for Autosomal Dominant Inherited NCCM
Defects in sarcomere genes are the most common genetic cause for NCCM (Fig. 8.2) [4]. These forms of NCCM have an autosomal dominant inheritance pattern . Patients (usually) inherited the mutation from one of the parents. Siblings and offspring of these patients have a 50% risk of having inherited the familial mutation. Reduced penetrance is a well-known feature of sarcomere mutations in genetic cardiomyopathies [13], meaning that for unknown reasons, around 30% (the percentage may vary by gene and variant) of the carriers (i.e. relatives with the familial mutation) do not have a cardiomyopathy. In a small proportion (4%) of the patients the mutation has occurred de novo [4, 14]. In that case the mutation is not inherited from the parents and there is no increased risk for siblings, although risk for offspring of having the mutations remains 50%. Compound heterozygosity for sarcomere mutations, occurs when a patient inherited a (different) mutation from each parent. This is not very rare, since sarcomere mutations occur relatively frequently in the population [15]. Patients with two sarcomere gene mutations may have more severe clinical features than their relatives with single mutations [16]. In NCCM the most frequent genetic causes (71%) are defects in sarcomere genes: MYH7, TTN and MYBPC3. Less frequently (11%) affected are the other sarcomere genes: ACTC1, LDB3, TNNC1, TNNI3 and TNNT2. Rare genetic causes are the other autosomal dominantly inherited cardiomyopathy genes CASQ2, HCN4, KCNH2, KCNQ1, RYR2 and SCN5A, involved in ion transport and genes affecting other cardiomyocyte functions or structure like, CSRP3, DSP, LMNA, MIB1, MIB2 and PLN [4, 5], occurring altogether in approximately 6% of the patients.
Genes for X-linked Inherited NCCM
Defects of genes on the X chromosome affect only males and are inherited in an X linked pattern. With this type of inheritance sons of unaffected female carriers have 50% risk of being affected. Daughters of patients or of female carriers have 50% risk of being an (unaffected) carrier and transmitting the trait to their sons. Barth syndrome is caused by defects in the TAZ gene on the X chromosome. Among the other X-linked causes for NCCM are some genes causing neuromuscular disorders, DMD, EMD, FHL1, GLA, LAMP2,and rare neurodevelopmental disorders caused by mutations in the NONO, and RPS6KA3 genes [17].
Genes for Autosomal Recessive Inherited NCCM
Recessive inherited NCCM is rare and was reported in single childhood cases with inborn errors of metabolism, related to a FKTN or SDHD mutation [18, 19].
Mitochondrial Defects and NCCM
Mitochondrial disorders are caused by defects in the mitochondrial (Mt) DNA or by a defect in nuclear DNA genes encoding for structures of the mitochondria. Defects in Mt genes are passed on cytoplasmatically in germ cells from mother to child. Defects in nuclear genes have dominant, recessive or X-linked inheritance pattern. Mutations in genes affecting the mitochondrial functioning lead to insufficient energy production required in various organs, particularly those with high energy demands, like the central nervous system, skeletal and cardiac muscles. These disorders present with a wide spectrum of clinical features including cardiomyopathy, visual impairment, deafness, stroke, epilepsy and diabetes. Mt. genes linked to NCCM are MT-ATP6, MT-ATP8, MT-CO1, MT-CO3, MT-CYB, MT-ND1, MT-ND2 and MT-ND6 [20, 21]. Nuclear genes coding for the mitochondria linked to NCCM are DNAJC19, GARS, HADHB, MIPEP, MTFMT and NNT [22]. To find Mt gene defects a specific analysis of the Mt DNA and nuclear DNA is needed, since these genes are not routinely sequenced in NGS cardiomyopathy gene panels.
Chromosomal Defects
A number of chromosomal deletions and duplications have been associated with NCCM. These chromosomal defects are usually identified in children. Because they affect multiple genes they lead to complex congenital malformation syndromes. The 1p36 deletion syndrome is frequently reported presenting with NCCM, intellectual disability, delayed growth, hypotonia, seizures, limited speech ability, hearing and vision impairment and distinct facial features [23]. Other chromosome anomalies linked to NCCM are deletions of 1q, 5q35, 7p21, 8p23.1, 22q11 and Xq28 [24]. In addition NCCM has been observed in monosomy X (Turner syndrome) and trisomy 13, trisomy 18, trisomy 21 and trisomy 22 patients [25]. To detect a small chromosome anomaly, an array analysis has to be performed, since these defects are not recognized by NGS sequencing of cardiomyopathy genes.
Genetic Counseling and Genetic Diagnosis of NCCM
Genetic counseling is recommended for all patients fulfilling diagnostic criteria for NCCM to perform DNA analysis and detect familial disease. This information is needed to estimate risk for relatives, convey information on the risks to index cases and their families and subsequently initiate family screening. Like in HCM and DCM family screening for NCCM is recommended because it allows accurate and timely diagnosis of NCCM improving prognosis of patients in the family. To initiate genetic diagnostics for NCCM, index patients are counseled about the consequences of the results of DNA testing, and an informed consent for DNA testing is requested.
Genetic counseling involves communicating the goal of genetic testing and the explaining the importance of informing family members. Genetic counselors are trained to explain the clinical features of the disease and the inheritance pattern, to the index case and organize informing and screening family members. Genetic counseling has grown out of the need to personalize scientific information and to translate it into a user-friendly language that is accessible intellectually and emotionally for the patient and its family. Helping index cases and their relatives—if necessary-to handle the information on heredity, and discuss the subsequent risks and consequences, is an important part of the process of genetic counseling. The routine for genetic diagnosis and family screening for NCCM is summarized in Fig. 8.3. It is hereby the role of the genetic counselor to identify and help, during pre- and post-test counseling, coping with adverse feelings that some patients or relatives may experience like distress, anxiety or guilt, evoked by the possibility of a genetic cause for NCCM [26]. It is important, in particular for asymptomatic relatives, to discuss that having a genetic risk and having a choice of predictive testing, whether by DNA analysis or cardiologic exam, may have medical implications, as well as psychological and socio -economic consequences. The genetic counselor may offer access to specialized psychologic support when needed by families.
Family History
At the departments of clinical genetics information on the occurrence of cardiomyopathies in the family of NCCM patients is obtained, and medical records of affected relatives are retrieved for verification of the diagnosis, when possible. Family history taking helps to determine if cardiomyopathy is familial and to identify the mode of inheritance [27]. It is importance to acknowledge that an uninformative family history cannot completely exclude a genetic cause for NCCM. Because around 20% of NCCM patients without affected relatives had a mutation [4]. The reasons for underreporting of familial cardiomyopathy might be that affected relatives might not have been diagnosed with NCCM. It is known that approximately 30% of the NCCM patients have a cardiomyopathy without the typical symptoms of cardiomyopathy at time of diagnosis [28]. Also, like in HCM, non-penetrance occurs in around 30% of the carriers of a familial (sarcomere) mutations and these carriers do not have a cardiomyopathy [28]. Another explanation for underreporting familial disease may be that family histories are not informative when families are small or patients have little information on relatives. Important questions when taking a family history for the purpose of establishing whether there is a familial cardiomyopathy is asking if relatives have had heart failure, arrhythmias, accidental or unexpected deaths, thromboses (including stroke), any kind of cardiac surgery, or if they had a congenital heart defect or neuromuscular disease. When family screening is performed the family histories are adjusted according to the results of the DNA and cardiac screening of relatives.
DNA Testing for NCCM
The purpose of DNA testing— irrespective of the age of the patient—is to identify the genetic cause for NCCM [4, 5]. An important aspect of DNA testing is that finding a mutation allows asymptomatic relatives to have a predictive DNA test that identifies accurately which relatives have a mutation and have an increased risk of developing a cardiomyopathy. In this way identifying the causative mutation facilitates genetic cascade screening. In families with a mutation, relatives who do not carry the familial mutation can be excluded from regular cardiac follow-up and can be reassured that there is no increased risk for their offspring. DNA testing may help to confirm the diagnosis for patient with borderline features of NCCM. In addition as we have shown recently, the genotype (specific genetic defect) may help to predict risk for ventricular systolic dysfunction and major cardiac adverse events for patients and guide clinical management accordingly [4], as discussed in more detail in the paragraph on genotype-phenotype correlations .
NGS Cardiomyopathy Gene Panels
Since a large number of genes are involved in NCCM, the application of novel methods of DNA analysis like NGS and exome based testing has been proven to improve the yield of genetic testing with the simultaneous analysis of panels with large numbers of cardiomyopathy genes [3]. Current cardiomyopathy gene panels used in diagnostic and commercial laboratories may include the following genes: ABCC9, ACTC1 , ACTN2 , ANKRD1, BAG3, CALR3, CRYAB, CSRP3, DES, DMD , DSC2, DSG2, DSP , EMD , GLA , JPH2, JUP, LAMA4, LAMP2 , LDB3, LMNA , MYBPC3 , MYH6, MYH7 , MYL2, MYL3, MYPN , MYOZ1, MYOZ2, PKP2 , PLN , PRKAG2, RBM20 , RYR2 , SCN5A , SGCD, TAZ , TCAP, TMEM43, TNNC1 , TNNI3 , TNNT2 , TPM1 , TTN and VCL (in bold the genes that were associated so far with NCCM). These genes encode proteins constituting structure and function of the sarcomere, cytoskeleton, desmosome, ion channels or nuclear lamina, and proteins participating in Ca2+ handling during contraction phase of action potential of the cardiomyocyte or affecting cardiac energy metabolism and are related to a large spectrum of cardiomyopathies. In case a cardiomyopathy gene panel is not available, DNA testing for NCCM of a smaller number of genes including MYH7, MYBPC3 and TTN, which have a large proportion of the genetic defects in NCCM, is advised.
Gene Variant Classification System
For a correct interpretation of the results of DNA analysis stringent novel guidelines for classification of genetic variants are applied since 2015 [29]. The outcome of DNA analysis for clinical purpose are currently classified into pathogenic variants (PV), likely pathogenic variants (LPV), variants of unknown clinical significance (VUS), likely benign or benign variants. This classification system for variants is based on in silico prediction of pathogenicity, population frequencies and previous reports providing (functional) evidence of the pathogenic nature of the specific variants [30]. Variants classified as PV or LPV in sarcomere genes are usually nonsynonymous substitutions or deletions of a nucleotide classified as missense, nonsense, or frameshift mutations and have a deleterious effect on the protein. Older results of DNA testing should be re-evaluated, because some of the variants previously reported as (pathogenic) mutations may now be reclassified as not pathogenic. Application of novel classification system to a large number of variants in sarcomere genes in NCCM patients showed recently that 50% of variants previously reported to be pathogenic, were reclassified as VUS or benign variants [31]. Similarly a large proportion of variants reported previously as mutations in sarcomere genes in HCM patients, were reclassified recently as VUS or benign variants [32]. This endorses that the continuous surveillance of variant classification is needed, because new evidence on DNA variants like population frequencies, results of novel functional tests or in silico predictor tools comes out [33]. DNA testing of pre-symptomatic family members is only indicated when there is a PV or LPV in the family. Since the effect of VUS is not known, these variants cannot reliably predict risk for NCCM in relatives and therefor these variants are not of used for family screening.
DNA Testing of NCCM Patients with CHD, Neuromuscular Disease or NCCM with Multiple Congenital Anomalies Syndrome
Around 10% of NCCM patients have a concomitant congenital heart defect [34]. Some families with NCCM and Ebstein anomaly , have a mutation in MYH7 [35]. There is little evidence that the combination of NCCM with other forms of CHD segregate in families or are caused by specific genetic defects. Thus it remains unknown if there are common (epi)genetic causes affecting embryologic cardiac development explaining the co-occurrence of NCCM and CHD, or that they co-occur by coincidence. NCCM in some patients represent cardiac manifestations of inherited neuromuscular disorders, for which specific diagnostic gene panels need to be requested since these genes are usually not included in the regular cardiomyopathy gene panels [36]. Also NCCM patients with multiple congenital malformations, usually children, need additional DNA testing and/ or chromosome analysis (array). According to clinical features, that may include screening for mitochondrial defects or metabolic disorders occurring predominantly in childhood NCCM.
Family Screening
Risk for Cardiomyopathy in Relatives
Overall affected relatives of NCCM patients have less severe cardiac features than the index cases, and relatives of index cases with a mutation have more risk of having a cardiomyopathy than the relatives of cases without a mutation. Because, at diagnosis affected relatives have usually less attenuated cardiac symptoms than the index case, independent of age at diagnosis, since most relatives are asymptomatic [28]. And some of the index cases without a mutation may have a non-genetic, secondary cause for NCCM, with lower risk for relatives. The risk for relatives of having a cardiomyopathy is furthermore related to the genetic defect in the index case, the mode of inheritance, the gene specific penetrance and—chance of having asymptomatic disease. These factors and also the age at diagnosis of the index case may help to determine the genetic risk for relatives. Also family history of cardiomyopathy or sudden cardiac death in the family may add information about the genetic risk for relatives. It is important for relatives to know that carriers of a familial mutation may have no signs of cardiomyopathy at cardiologic examination. Non-penetrance was observed in 17% of carriers of familial MHY7 mutations, 33% of carriers of MYBPC3 and 28% of carriers of TTN mutations [28]. Intra-familial variability of cardiac features is a well-known feature of familial cardiomyopathies. The left ventricle (LV) dimension of the NCCM index case may be a predictor for disease severity in relatives. The dimension of the LV in NCCM relatives corresponded significantly with the LV phenotype of the index case. In addition, since the LV dimension in NCCM patients was related to the course of the disease, the LV function may predict severity for relatives. Patients with NCCM and normal LV-dimensions had a mild course of the disease, with less frequent LV-systolic dysfunction or cardiac events. Patients with NCCM with a dilated LV-dimensions (like in DCM), had a more severe disease course with frequent LV-systolic dysfunction and adverse events. In the families of NCCM patients, 20% of the affected relatives have HCM or DCM without signs of hypertrabeculation [28]. In addition relatives of NCCM patients may have an increased risk for CHD, compared to population risk [28].
Screening Adult Relatives of NCCM Patients
In families with a causative mutation, adult relatives can be offered predictive DNA testing. Predictive DNA testing of relatives can reliably identify which relatives carry a mutation and have an increased risk of developing a cardiomyopathy and thus need clinical surveillance. Relatives who do not carry the mutation can be excluded from regular cardiac follow-up and also can be reassured that there is no increased risk for cardiomyopathy for their offspring.
In families without a mutation, cardiologic family screening of first-degree relatives is recommended. Family screening can be initiated by asking the index patients to distribute a letter to their first and second-degree relatives with information on counseling for genetic risk for NCCM and recommendations for predictive DNA and/or cardiologic family screening. The legal framework for informing relatives varies, in most countries it is the index patient and not the clinician, who must inform relatives and invite them for screening on behalf of the healthcare system [37]. It is important that relatives consent and are correctly informed, before they are tested, about the risk of having a cardiomyopathy and about the eventual consequences when they are carriers of a familial mutation and/or signs of cardiomyopathy are detected at cardiologic exam. Diagnosis of a mutation or a cardiomyopathy, even when a relative is asymptomatic may have medical, psychologically as well as socio- economically consequences. For instance regarding life insurance, pension, life style (sporting activities), and eligibility for fostering and adoption [38]. Most relatives have no symptoms of cardiomyopathy and have not been diagnosed when they have a predictive DNA test or have the first cardiologic examination. One of the reasons relatives may choose to have a predictive test is that they want to be in control of their life and gain clarity. Others, doubt wanting to have disclosure, because they believe they may be better of not knowing about the risk giving the chance of being asymptomatic for years. A genetic counselor can help to guide in their decisions to have a pre-symptomatic test.
Screening Young Relatives for NCCM
Like in other age dependent hereditary cardiomyopathies, the recommendations for pre-symptomatic screening are not the same for adults and children. Cardiologic screening is usually recommended from the age that first symptoms may appear. For instance for HCM, cardiologic screening starts around 10–12 years for asymptomatic children with unknown genetic status [38]. In practice these guidelines are followed for NCCM as well. In families with a mutation, predictive DNA testing in children is usually postponed until the age that they can make an informed decision. Because the medical benefit of pre-symptomatic DNA diagnosis of having a familial mutation has not been established for children. The main advantage of pre-symptomatic DNA testing of children is that when a familial mutation can be excluded the child can be discharged from life-long follow-up. In contrast, for the asymptomatic children who are found to be carriers of a familial mutation, recommendations include regular cardiologic follow-up and address life style, like refraining from competitive sports [38]. The burden for children of regular hospital visits, may have adverse psychological like anxiety or depression and may harm a child’s self-esteem [39, 40]. Another adverse effect of pre-symptomatic testing in children and adults alike are possible economic disadvantages like higher life insurance or mortgages later in life. For that reason predictive DNA testing for a familial mutation is usually performed in relatives above the age of 18 years. Clinical and/or genetic screening should be considered from younger age if the child has symptoms which can point to a cardiomyopathy or in families with a history of early-onset cardiomyopathy.
Pregnancy and Prenatal Testing
An important aspect of the counseling and cardiologic care of young women with NCCM is to inform patients that a pregnancy may carry a risk for themselves as well as for their offspring. For women with NCCM, the maternal risk in pregnancy for developing heart failure and/or arrhythmias requires extensive follow-up during pregnancies. Women with a cardiomyopathy who have symptoms before pregnancy have an increased risk and need specialized obstetric care [41]. Women with asymptomatic cardiomyopathies usually tolerate pregnancy well and these women may have a spontaneous labor and vaginal delivery [42]. NCCM patients have an increased risk of having a child with a cardiomyopathy. Depending on whether the patient has a mutation and the estimated risk for the child, prenatal diagnosis of NCCM (prenatal DNA testing and/or prenatal cardiac ultrasound of the fetus) can be discussed. Prenatal diagnostics for NCCM, however, are rarely requested, because the risk that a child has severe congenital NCCM is small, given that onset of symptoms of NCCM are age related, and patients/ carriers of mutations may not have symptoms. Unless there is an affected child in the family, in which case prenatal diagnostics for NCCM will be recommended.
The individual options and limitations of prenatal diagnosis of NCCM are discussed with NCCM patients with reproductive wishes. Pre- and post-test counseling is necessary because risks and prenatal testing in these pregnancies may evoke anxiety in parents and they may need help to make far reaching decisions during the pregnancy. It is important to acknowledge, that the likelihood that testing may cause distress, meaning that steps should be taken to minimize distress and provide support, not that testing should be denied.
For prenatal testing for NCCM the familial mutation is important. In families with a mutation, prenatal DNA testing can be performed. We have the choice of a DNA testing in chorionic villus sampling (conducted at 10–12 weeks of gestation) or amniocentesis (conducted at 14–20 weeks of gestation). The DNA test results are known within 2–3 weeks, well within the legal framework in most countries for terminating a pregnancy affected with a severe disorder. The parents need to be informed that these interventions carry a risk for the mother and fetus including miscarriage [43]. If the child is shown to have the familial mutation that may causes (severe) childhood cardiomyopathy, parents may choose to terminate the pregnancy or have additional prenatal echocardiography for structural defects and assessment of cardiac function to detect a congenital cardiomyopathy [44]. Prenatal cardiac sonography is performed in specialized tertiary prenatal centers, and allows to detect fetal cardiac malformations, cardiomyopathies, systolic and diastolic function and arrhythmia in the second –and third trimester of pregnancy. Prenatal cardiac sonography is also the method of choice for prenatal screening of NCCM when there is no mutation in the family. A major limitation of prenatal sonography for NCCM is that little is known about the onset and prenatal development of NCCM, and we do not know in which NCCM patients we may and in which we cannot find prenatally signs of noncompaction and in which trimester the first cardiac signs of noncompaction be may observed. There are few reports, showing early prenatal onset of NCCM in cases with a MYH7 mutation [45]. Since prenatal diagnosed NCCM may remain asymptomatic after birth, prediction of disease severity from the results of prenatal testing remains difficult [46]. However, prenatal testing does have a role in assessment which pregnancy may need perinatal cardiac monitoring.
Psychological Impact of Genetic Testing for Index and for Relatives
Having a genetic cardiomyopathy implies that your children and other family members may have an increased risk of having a cardiomyopathy. For patients, this knowledge may add to the burden of having a cardiomyopathy. For insight in the psychological effects of genetic testing, we depend on studies focusing on familial cardiomyopathies or other genetic disorders. The studies looking at the impact of having a genetic cardiomyopathy showed that overall the burden of cardiac symptoms had greater psychosocial impact than the burden of the condition being genetic [26, 47]. Index cases might be pressured by their relatives to have genetic testing. But this did not negatively affect satisfaction with the genetic counseling process or getting the results of DNA testing [48]. Overall clinical symptoms are the principal source of concern: index cases showed more distress when having a diagnostic DNA test than relatives having a predictive DNA test, probably because the index cases had a cardiomyopathy, while the relatives usually are asymptomatic [49]. Predictive testing can evoke anxiety about risk of being affected and transmitting the predisposition for disease to offspring, but it may also bring clarity about a subject that has been on the mind for a significant time. Overall relatives at risk for hereditary cardiac diseases did not have more emotional distress the normal population [50]. Understandably, relatives with a positive genetic test showed more distress than relatives where a familial mutation could be excluded [49]. Despite the result of the genetic test, the vast majority (80%) of the patients was satisfied with the decision of undergoing a genetic test [49]. Patients who had less understanding of carriership of the mutation or had stronger belief in serious consequences had more symptoms of depression [47]. High levels of anxiety were linked to a younger age, females, less formal education and fewer social contacts [47, 51]. From these studies we have learned the importance of focusing during pre- and post-test counseling on the individual perception of risk and disease and helping the patients to cope with the consequences of the test result. The way of giving the test result, by telephone or by a face to face appointment, did not have an impact on contentment of the patient [48].
Cardiologic Screening
In case a mutation is identified in a patient, the patient is referred for cardiologic screening. Cardiologic screening is also recommended for relatives from a family with a mutation, who chooses not to have a predictive DNA test. Likewise, in families were no mutation is found, relatives are advised to have a cardiologic examination from age of 10 years onwards. Cardiologic screening may be initiated before the age of 10 years if the child is planning to engage in competitive sports, or there is a family history of sudden cardiac death. Cardiologic screening in family members contains a physical examination, 12-lead electrocardiography and echocardiography. When abnormalities are found the cardiac work up should be expanded. For example when signs of a cardiomyopathy on echocardiography are identified, additionally cardiac magnetic resonance imaging (CMR) can be performed. A48-h ambulatory electrocardiography should be performed when patients have palpitations or there are other indications for an arrhythmia.
In familial NCCM, relatives have less severe cardiac features than the index cases. Early detection in relatives is important and allows treatment and prevention of severe complications. Index cases with a mutation had a higher prevalence of familial disease. Cardiologic family screening is recommended for the families of all cases, because family screening may identify asymptomatic relatives with a cardiomyopathy in families without evidence for genetic disease. In this way cardiologic family screening may help to identify familial NCCM and stratify risk for relatives into a high genetic risk. In the sporadic cases without a mutation and negative results of cardiac family screening, as expected in approximately 50% of all cases diagnosed with NCCM, secondary causes (non-genetic) for NCCM are expected with low recurrence risks for relatives.
Cardiologic Follow-Up
In general, the diagnosis NCCM requires lifelong follow-up to detect changes in symptoms, risk for adverse events, LV function and cardiac rhythm. Prevalence of LV systolic dysfunction and atrial arrhythmias increases with age [52, 53]. The frequency of monitoring is determined by the severity of disease, age and symptoms. A clinical examination, including 12-lead ECG and TTE, should be performed every 1–2 years or sooner if patients have new cardiac symptoms [38]. In 50–70% of the mutation carriers a cardiomyopathy is identified by first screening, 30% of these patients are asymptomatic [28, 54]. These asymptomatic carriers with a phenotype should also have follow-up every 1–2 years. The clinical significance of mild morphological and functional abnormalities is uncertain but probably minor in most [54, 55]. In 30% of the adult relatives with a mutation no cardiomyopathy at first cardiologic screening is identified, these are mutation carriers without a phenotype [28]. Studies suggest a benign clinical course for mutation carriers without a phenotype in HCM families [56, 57]. However, a proportion of mutation carriers without a phenotype will develop a cardiomyopathy later in life, because of age-related increase in penetrance [13]. This is why mutation carriers without a phenotype should have cardiac examination at least every 5 years [38]. Also first degree family members without a phenotype from families without a mutation cannot be discharged from medical follow-up and should also be screened at least every 5 years [38]. This is because not all genetic causes for NCCM are identified yet, and these relatives might have a yet unknown genetic cause for NCCM.
Genotype-Phenotype Correlation
Knowledge of the genetic cause for familial NCCM may help to predict the outcome. Specific genetic defects were associated with the phenotype, and associated clinical features, including risk for major adverse cardiac events for the index case and affected relatives. In other words, complementing cardiologic diagnosis with genetic status may allow tailoring clinical management and follow-up of familial NCCM according to genetic burden. In the future the associations between specific mutations and clinical features or risks may become clearer, by more extended methods of DNA testing and the analysis of the features large numbers of patients. Although specific genotype based cardiomyopathy treatments are not available, the established genotype-phenotype correlations for NCCM can help to guide clinical management of the patients.
Genetic Versus Sporadic NCCM
There are distinct differences between the genetic (the NCCM patients with a mutation and/or patients with a family history of cardiomyopathy) and the patients without a mutation or family history, the sporadic cases. Mutations occur more frequently in young patients and in patients with familial cardiomyopathies [4]. In children with genetic NCCM severe outcome of NCCM is more than in children with sporadic NCCM [4]. Children diagnosed before the age of 1 year, had frequently a mutation, cardiac symptoms, LV systolic dysfunction, and a high risk for major adverse cardiac events (MACE) . In contrast to sporadic children, who had a good prognosis, with a mild clinical course and low risk for complications. In severe forms of NCCM occurring in childhood the possibility exists that it may involve a complex genotype. For that reason if a child is diagnosed with a cardiomyopathy in the family of an adult NCCM case, we recommend to perform a full panel of genes testing instead of only testing for the familial mutation.
Adults with a mutation had high risk for LV and RV systolic dysfunction [4]. Prognosis in adult NCCM patients with a mutation was correlated with left ventricular function. Adult NCCM patients with a mutation and a persevered LV ejection fraction had a good prognosis. In contrast to adults with a mutation and LV systolic dysfunction, who had worse outcome. In sporadic adult patients prognosis was not related to LV systolic function. The sporadic NCCM patients had frequently hypertension, suggesting an acquired form of NCCM, and this may have consequences for recommendations of family screening.
Sarcomere Genes
MYH7 gene mutations are the most prevalent genetic cause for NCCM are associated with a relatively milder course of disease with low risk for complications, compared to other genetic causes [4]. The prognosis for patients with mutations in the head of the MYH7 gene was better than for patients with mutations in the tail of the gene [28]. Mutations in the head of MYH7 were associated with NCCM with normal dimensions of the LV and a milder course of the disease. Mutations in the tail had high incidence of LV dilatation and LV systolic dysfunction. An explanation for the association between mutations in the tail and the dilated subtype could be that tail mutations may infer with the binding site for TTN, and thus may have a similar effect as the effect of TTN mutations , which are important causes of DCM. Also frequent relatives with DCM without hypertrabeculation were identified. Another feature of the MYH7 was that this is one of the rare sarcomere genes that was observed in families where Ebstein anomaly occurred in NCCM patients [35]. The TTN gene, which is a major cause of DCM, is also a frequent cause of NCCM, predominantly in adult NCCM patients [4]. This could indicate that younger TTN carriers are not symptomatic, which may be important for relatives (children) who are carriers of a TTN mutation. The adult NCCM patients with TTN mutations had high prevalence of LV systolic dysfunction and LV dilatation, similar to DCM patients with TTN mutations. In families of NCCM patients with a TTN mutation relatives may have DCM without hypertrabeculation [28]. MYBPC3 (compound) homozygous mutations were observed in NCCM cases with a severe phenotype and major cardiac events at young age [16]. NCCM patients with a single MYBPC3 mutation had high prevalence of RV systolic dysfunction [4]. In the families of NCCM patients with a MYBPC3 mutation, HCM without signs of hypertrabeculation may occur in relatives. Also an increased risk for LV hypertrophy (HCM) was observed [28]. Relatives with HCM without sigs of hypertrabeculation occur in the families of NCCM patients with a MYBPC3 mutation.
Other Cardiomyopathy Genes
Mutations in HCN4 were associated with NCCM and also bradycardia [58]. Mutations in RYR2 lead to catecholaminergic polymorphic ventricular tachycardia (CPVT) and may also cause NCCM, especially variants in exon 3 [59]. LMNA and RBM20 are rare causes for NCCM and may be associated with worse outcome, like in DCM [5]. SCN5A was reported to be a genetic modifier, increasing the risk for arrhythmias in NCCM [60].
Future Directions of Genetic Diagnosis and Family Screening for NCCM
The application of whole exome or genome sequencing of NCCM patients in the near future will reveal novel genetic causes or genetic interactions with modifiers, some of which may explain remodeling into different cardiomyopathy phenotypes within families. A disease model may be developed to obtain functional evidence of the deleterious effect of genetic variants for better understanding and a more accurate classification of the DNA variants in cardiomyopathy genes, especially for the variants that are now regarded as variants of unknown significance. The expected broad application in the general population of predictive DNA testing for genetic susceptibilities for a large range of disease, may achieve a change in attitude towards and the perception of having a genetic susceptibility. Because it is clear that all of us are carrying genetic defects for one disease or another. This awareness hopefully leads to ban the discriminatory socio economic sanctions experienced currently whenrevealing personal genetic burden.
Prospective large follow up studies are needed to confirm the genotype-phenotype correlations in NCCM, and adjust guidelines for clinical follow up of patients and at risk relatives accordingly. Leading eventually to family- and gene tailored follow-up and management of NCCM patients and their families. The risk for cardiomyopathy for relatives of sporadic NCCM patients seems low, also risk for mutation carriers without a phenotype seems low. Follow-up studies of these relatives at low risk are needed to evaluate the value of interval screening in these groups and to confirm the low risk. When al NCCM genes are known, excluding a genetic predisposition in a proportion of patients may be achieved, thus allowing making the important distinction between genetic and non-genetic NCCM. And follow-up strategies can be designed according to genetic burden. In the distant future genetic classification may lead to the development of genotype specific treatment and eventually gene therapy for NCCM.
References
Bleyl SB, Mumford BR, Thompson V, Carey JC, Pysher TJ, Chin TK, et al. Neonatal, lethal noncompaction of the left ventricular myocardium is allelic with Barth Syndrome. Am J Hum Genet. 1997;61(4):868–72.
Hoedemaekers YM, Caliskan K, Majoor-Krakauer D, van de Laar I, Michels M, Witsenburg M, et al. Cardiac beta-myosin heavy chain defects in two families with non-compaction cardiomyopathy: linking non-compaction to hypertrophic, restrictive, and dilated cardiomyopathies. Eur Heart J. 2007;28(22):2732–7.
Klaassen S, Probst S, Oechslin E, Gerull B, Krings G, Schuler P, et al. Mutations in sarcomere protein genes in left ventricular noncompaction. Circulation. 2008;117(22):2893–901.
van Waning JI, Caliskan K, Hoedemaekers YM, van Spaendonck-Zwarts KY, Baas AF, Boekholdt SM, et al. Genetics, clinical features, and long-term outcome of noncompaction cardiomyopathy. J Am Coll Cardiol. 2018;71(7):711–22.
Sedaghat-Hamedani F, Haas J, Zhu F, Geier C, Kayvanpour E, Liss M, et al. Clinical genetics and outcome of left ventricular non-compaction cardiomyopathy. Eur Heart J. 2017;38(46):3449–60.
Charron P, Arad M, Arbustini E, Basso C, Bilinska Z, Elliott P, et al. Genetic counselling and testing in cardiomyopathies: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2010;31(22):2715–26.
Gati S, Rajani R, Carr-White GS, Chambers JB. Adult left ventricular noncompaction: reappraisal of current diagnostic imaging modalities. JACC Cardiovasc Imaging. 2014;7(12):1266–75.
Hoedemaekers YM, Caliskan K, Michels M, Frohn-Mulder I, van der Smagt JJ, Phefferkorn JE, et al. The importance of genetic counseling, DNA diagnostics, and cardiologic family screening in left ventricular noncompaction cardiomyopathy. Circ Cardiovasc Genet. 2010;3(3):232–9.
Kawel-Boehm N, McClelland RL, Zemrak F, Captur G, Hundley WG, Liu CY, et al. Hypertrabeculated left ventricular myocardium in relationship to myocardial function and fibrosis: the multi-ethnic study of atherosclerosis. Radiology. 2017;284:667.
Luijkx T, Cramer MJ, Zaidi A, Rienks R, Senden PJ, Sharma S, et al. Ethnic differences in ventricular hypertrabeculation on cardiac MRI in elite football players. Neth Heart J. 2012;20(10):389–95.
Gati S, Chandra N, Bennett RL, Reed M, Kervio G, Panoulas VF, et al. Increased left ventricular trabeculation in highly trained athletes: do we need more stringent criteria for the diagnosis of left ventricular non-compaction in athletes? Heart. 2013;99(6):401–8.
Vatta M, Mohapatra B, Jimenez S, Sanchez X, Faulkner G, Perles Z, et al. Mutations in Cypher/ZASP in patients with dilated cardiomyopathy and left ventricular non-compaction. J Am Coll Cardiol. 2003;42(11):2014–27.
Michels M, Soliman OI, Phefferkorn J, Hoedemaekers YM, Kofflard MJ, Dooijes D, et al. Disease penetrance and risk stratification for sudden cardiac death in asymptomatic hypertrophic cardiomyopathy mutation carriers. Eur Heart J. 2009;30(21):2593–8.
Budde BS, Binner P, Waldmuller S, Hohne W, Blankenfeldt W, Hassfeld S, et al. Noncompaction of the ventricular myocardium is associated with a de novo mutation in the beta-myosin heavy chain gene. PLoS One. 2007;2(12):e1362.
Maron BJ, Gardin JM, Flack JM, Gidding SS, Kurosaki TT, Bild DE. Prevalence of hypertrophic cardiomyopathy in a general population of young adults. Echocardiographic analysis of 4111 subjects in the CARDIA Study. Coronary Artery Risk Development in (Young) Adults. Circulation. 1995;92(4):785–9.
Wessels MW, Herkert JC, Frohn-Mulder IM, Dalinghaus M, van den Wijngaard A, de Krijger RR, et al. Compound heterozygous or homozygous truncating MYBPC3 mutations cause lethal cardiomyopathy with features of noncompaction and septal defects. Eur J Hum Genet. 2015;23(7):922–8.
Finsterer J, Stollberger C. Spontaneous left ventricular hypertrabeculation in dystrophin duplication based Becker’s muscular dystrophy. Herz. 2001;26(7):477–81.
Amiya E, Morita H, Hatano M, Nitta D, Hosoya Y, Maki H, et al. Fukutin gene mutations that cause left ventricular noncompaction. Int J Cardiol. 2016;222:727–9.
Alston CL, Ceccatelli Berti C, Blakely EL, Olahova M, He L, McMahon CJ, et al. A recessive homozygous p.Asp92Gly SDHD mutation causes prenatal cardiomyopathy and a severe mitochondrial complex II deficiency. Hum Genet. 2015;134(8):869–79.
Finsterer J, Bittner R, Bodingbauer M, Eichberger H, Stollberger C, Blazek G. Complex mitochondriopathy associated with 4 mtDNA transitions. Eur Neurol. 2000;44(1):37–41.
Tang S, Batra A, Zhang Y, Ebenroth ES, Huang TS. Left ventricular noncompaction is associated with mutations in the mitochondrial genome. Mitochondrion. 2010;10(4):350–7.
Ojala T, Polinati P, Manninen T, Hiippala A, Rajantie J, Karikoski R, et al. New mutation of mitochondrial DNAJC19 causing dilated and noncompaction cardiomyopathy, anemia, ataxia, and male genital anomalies. Pediatr Res. 2012;72(4):432–7.
Cremer K, Ludecke HJ, Ruhr F, Wieczorek D. Left-ventricular non-compaction (LVNC): a clinical feature more often observed in terminal deletion 1p36 than previously expected. Eur J Med Genet. 2008;51(6):685–8.
Pauli RM, Scheib-Wixted S, Cripe L, Izumo S, Sekhon GS. Ventricular noncompaction and distal chromosome 5q deletion. Am J Med Genet. 1999;85(4):419–23.
McMahon CJ, Chang AC, Pignatelli RH, Miller-Hance WC, Eble BK, Towbin JA, et al. Left ventricular noncompaction cardiomyopathy in association with trisomy 13. Pediatr Cardiol. 2005;26(4):477–9.
Brouwers C, Caliskan K, Bos S, Van Lennep JE, Sijbrands EJ, Kop WJ, et al. Health status and psychological distress in patients with non-compaction cardiomyopathy: the role of burden related to symptoms and genetic vulnerability. Int J Behav Med. 2015;22(6):717–25.
Morales A, Cowan J, Dagua J, Hershberger RE. Family history: an essential tool for cardiovascular genetic medicine. Congest Heart Fail. 2008;14(1):37–45.
van Waning JI, Caliskan K, Michels M, Schinkel AFL, Hirsch A, Dalinghaus M, Hoedemaekers YM, Wessels MW, IJpma AS, Hofstra RMW, van Slegtenhorst MA, Majoor-Krakauer D. Cardiac phenotypes, genetics, and risks in familial noncompaction cardiomyopathy. J Am Coll Cardiol. 2019;73(13):1601–11. https://doi.org/10.1016/j.jacc.2018.12.085.
Plon SE, Eccles DM, Easton D, Foulkes WD, Genuardi M, Greenblatt MS, et al. Sequence variant classification and reporting: recommendations for improving the interpretation of cancer susceptibility genetic test results. Hum Mutat. 2008;29(11):1282–91.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17(5):405–24.
Abbasi Y, Jabbari J, Jabbari R, Yang RQ, Risgaard B, Kober L, et al. The pathogenicity of genetic variants previously associated with left ventricular non-compaction. Mol Genet Genomic Med. 2016;4(2):135–42.
Walsh R, Buchan R, Wilk A, John S, Felkin LE, Thomson KL, et al. Defining the genetic architecture of hypertrophic cardiomyopathy: re-evaluating the role of non-sarcomeric genes. Eur Heart J. 2017;38(46):3461–8.
Walsh R, Thomson KL, Ware JS, Funke BH, Woodley J, McGuire KJ, et al. Reassessment of Mendelian gene pathogenicity using 7,855 cardiomyopathy cases and 60,706 reference samples. Genet Med. 2017;19(2):192–203.
Stahli BE, Gebhard C, Biaggi P, Klaassen S, Valsangiacomo Buechel E, Attenhofer Jost CH, et al. Left ventricular non-compaction: prevalence in congenital heart disease. Int J Cardiol. 2013;167(6):2477–81.
Vermeer AM, van Engelen K, Postma AV, Baars MJ, Christiaans I, De Haij S, et al. Ebstein anomaly associated with left ventricular noncompaction: an autosomal dominant condition that can be caused by mutations in MYH7. Am J Med Genet C Semin Med Genet. 2013;163C(3):178–84.
Ichida F, Tsubata S, Bowles KR, Haneda N, Uese K, Miyawaki T, et al. Novel gene mutations in patients with left ventricular noncompaction or Barth syndrome. Circulation. 2001;103(9):1256–63.
van der Roest WP, Pennings JM, Bakker M, van den Berg MP, van Tintelen JP. Family letters are an effective way to inform relatives about inherited cardiac disease. Am J Med Genet A. 2009;149A(3):357–63.
Authors/Task Force Members, Elliott PM, Anastasakis A, Borger MA, Borggrefe M, Cecchi F, et al. 2014 ESC guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J. 2014;35(39):2733–79.
Fanos JH. Developmental tasks of childhood and adolescence: implications for genetic testing. Am J Med Genet. 1997;71(1):22–8.
Bratt EL, Ostman-Smith I, Axelsson A, Berntsson L. Quality of life in asymptomatic children and adolescents before and after diagnosis of hypertrophic cardiomyopathy through family screening. J Clin Nurs. 2013;22(1–2):211–21.
Pieper PG, Walker F. Pregnancy in women with hypertrophic cardiomyopathy. Neth Heart J. 2013;21(1):14–8.
European Society of Gynecology, Association for European Paediatric Cardiology, German Society for Gender Medicine, Regitz-Zagrosek V, Blomstrom Lundqvist C, Borghi C, et al. ESC guidelines on the management of cardiovascular diseases during pregnancy: the Task Force on the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology (ESC). Eur Heart J. 2011;32(24):3147–97.
Tabor A, Philip J, Madsen M, Bang J, Obel EB, Norgaard-Pedersen B. Randomised controlled trial of genetic amniocentesis in 4606 low-risk women. Lancet. 1986;1(8493):1287–93.
Pedra SR, Smallhorn JF, Ryan G, Chitayat D, Taylor GP, Khan R, et al. Fetal cardiomyopathies: pathogenic mechanisms, hemodynamic findings, and clinical outcome. Circulation. 2002;106(5):585–91.
Hoedemaekers YM, Cohen-Overbeek TE, Frohn-Mulder IM, Dooijes D, Majoor-Krakauer DF. Prenatal ultrasound diagnosis of MYH7 non-compaction cardiomyopathy. Ultrasound Obstet Gynecol. 2013;41(3):336–9.
Stollberger C, Wegner C, Benatar A, Chin TK, Dangel J, Majoor-Krakauer D, et al. Postnatal outcome of fetal left ventricular hypertrabeculation/noncompaction. Pediatr Cardiol. 2016;37(5):919–24.
Christiaans I, van Langen IM, Birnie E, Bonsel GJ, Wilde AA, Smets EM. Quality of life and psychological distress in hypertrophic cardiomyopathy mutation carriers: a cross-sectional cohort study. Am J Med Genet A. 2009;149A(4):602–12.
Christiaans I, van Langen IM, Birnie E, Bonsel GJ, Wilde AA, Smets EM. Genetic counseling and cardiac care in predictively tested hypertrophic cardiomyopathy mutation carriers: the patients’ perspective. Am J Med Genet A. 2009;149A(7):1444–51.
Wynn J, Holland DT, Duong J, Ahimaz P, Chung WK. Examining the psychosocial impact of genetic testing for cardiomyopathies. J Genet Couns. 2018;27:927.
Hoedemaekers E, Jaspers JP, Van Tintelen JP. The influence of coping styles and perceived control on emotional distress in persons at risk for a hereditary heart disease. Am J Med Genet A. 2007;143A(17):1997–2005.
Vernon SW, Gritz ER, Peterson SK, Amos CI, Baile WF, Perz CA, et al. Design and methodology of a study of psychosocial aspects of genetic testing for hereditary colorectal cancer. Ann N Y Acad Sci. 1997;833:190–4.
Olivotto I, Cecchi F, Casey SA, Dolara A, Traverse JH, Maron BJ. Impact of atrial fibrillation on the clinical course of hypertrophic cardiomyopathy. Circulation. 2001;104(21):2517–24.
Thaman R, Gimeno JR, Murphy RT, Kubo T, Sachdev B, Mogensen J, et al. Prevalence and clinical significance of systolic impairment in hypertrophic cardiomyopathy. Heart. 2005;91(7):920–5.
Charron P, Dubourg O, Desnos M, Bouhour JB, Isnard R, Hagege A, et al. Diagnostic value of electrocardiography and echocardiography for familial hypertrophic cardiomyopathy in genotyped children. Eur Heart J. 1998;19(9):1377–82.
Gandjbakhch E, Gackowski A, Tezenas du Montcel S, Isnard R, Hamroun A, Richard P, et al. Early identification of mutation carriers in familial hypertrophic cardiomyopathy by combined echocardiography and tissue Doppler imaging. Eur Heart J. 2010;31(13):1599–607.
Jensen MK, Havndrup O, Christiansen M, Andersen PS, Diness B, Axelsson A, et al. Penetrance of hypertrophic cardiomyopathy in children and adolescents: a 12-year follow-up study of clinical screening and predictive genetic testing. Circulation. 2013;127(1):48–54.
Gray B, Ingles J, Semsarian C. Natural history of genotype positive-phenotype negative patients with hypertrophic cardiomyopathy. Int J Cardiol. 2011;152(2):258–9.
Milano A, Vermeer AM, Lodder EM, Barc J, Verkerk AO, Postma AV, et al. HCN4 mutations in multiple families with bradycardia and left ventricular noncompaction cardiomyopathy. J Am Coll Cardiol. 2014;64(8):745–56.
Campbell MJ, Czosek RJ, Hinton RB, Miller EM. Exon 3 deletion of ryanodine receptor causes left ventricular noncompaction, worsening catecholaminergic polymorphic ventricular tachycardia, and sudden cardiac arrest. Am J Med Genet A. 2015;167A(9):2197–200.
Shan L, Makita N, Xing Y, Watanabe S, Futatani T, Ye F, et al. SCN5A variants in Japanese patients with left ventricular noncompaction and arrhythmia. Mol Genet Metab. 2008;93(4):468–74.
Acknowledgement
J.I. van Waning is supported by a grant from the Jaap Schouten Foundation.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
van Waning, J.I., Majoor-Krakauer, D. (2019). Genetics and Family Screening for Noncompaction Cardiomyopathy. In: Caliskan, K., Soliman, O., ten Cate, F. (eds) Noncompaction Cardiomyopathy. Springer, Cham. https://doi.org/10.1007/978-3-030-17720-1_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-17720-1_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-17719-5
Online ISBN: 978-3-030-17720-1
eBook Packages: MedicineMedicine (R0)