Abstract
This chapter describes the role ureolytic biofilms (communities of microbes attached to surfaces) play in struvite stone formation in the urinary tract. The formation of struvite stones (MgNH4PO4·6H2O), commonly known as infection stones, is associated with urinary tract infections, particularly, with ureolytic microorganisms. Establishment of ureolytic biofilms in the urinary tract can result in increased microbial resistance to medical treatment and development of the necessary urine conditions to promote struvite (or other mineral) precipitation possibly leading to stone formation. Ureolytic microorganisms produce urease, an enzyme that breaks down urea (CO(NH2)2) generating ammonium (NH4 +) and alkalizing urine, which changes urine chemistry to potentially promote struvite and other mineral precipitation. This chapter describes the series of steps involved in biofilm development and struvite precipitation leading to stone formation. Furthermore, this chapter presents an overview of controlled laboratory experiments and computer simulations currently used in different disciplines to study microbe-fluid-mineral interactions. We conclude that an interdisciplinary approach including the disciplines of engineering, mathematics, chemistry, microbiology and medicine will provide a more comprehensive understanding of the process of stone formation in the urinary tract and will ultimately allow for the development of improved management and prevention strategies for infection stones.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Formation of Struvite Stones by Ureolytic Microorganisms
Infection stones account for almost 10–15% of urinary tract stones in the general population. Infection stone formation is one of the most complicated stone diseases due to the association of stone growth with bacterial infections, fast stone growth, high recurrence and tendency to form large aggregates (e.g. staghorn calculi) [1]. Infection stones are comprised of struvite (MgNH4PO4 ·6H2O), which is frequently accompanied by calcium phosphate, mostly in the form of carbonate apatite (carbapatite, Ca10(PO4)6CO3). Indeed, the composition of -so called- struvite stones is quite heterogeneous; Flannigan et al. [2] reported that among 121 struvite stones collected, 13.2% were homogeneous struvite, whereas 86.8% were heterogenous stones admixed with calcium phosphate (42.1%), calcium oxalate (33.9%), calcium carbonate (27.3%), and uric acid (5.8%).
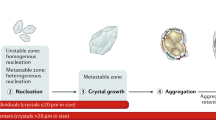
Formation of stones is an intricate process that starts with urine supersaturation (presence of a solute in solution at a higher concentration than that of its own solubility), leading to crystal nucleation and proceeds via crystal growth along with the aggregation of crystals [3]. Supersaturation in urine is a prerequisite for stone formation, however supersaturated urine is also observed in non-stone formers. Supersaturation implies that mineral precipitation is possible, but the presence of inhibitors (e.g. proteins, polysaccharides, etc.) [4] and slow kinetics of precipitation can keep urine supersaturated without significant mineral precipitation or stone growth. In the urinary tract, nucleation of crystals most likely occurs on pre-existing surfaces (heterogeneous nucleation); crystals usually become associated with surfaces ranging from suspended particles in urine (e.g. bacteria, organic substances, cellular debris), to the urothelium, to medical devices (e.g. ureter, catheter) [5]. Formation of microcrystals (roughly those ≤20 μm) is also observed in non-stone formers, but the crystals are small enough to be excreted through the urinary tract. Thus, for a stone to form, crystals do not only need to be formed but also need to grow and aggregate to be retained within the urinary tract.
The formation of infection stones depends on urine chemistry, which is driven by two key processes [1]: (i) urine pH; a pH >7.2 is commonly considered the threshold for struvite precipitation, and (ii) supersaturation of urine with respect to the solubility product of magnesium (Mg2+), ammonium (NH4 +) and phosphate (PO4 3−). Urine normally contains Ca2+, Mg2+ and PO4 3−, but the concentration of NH4 + in urine is usually not high enough to promote struvite precipitation. Formation of infection stones seems to be associated with urinary tract infections (UTIs) [1], particularly with the presence of ureolytic (urea-hydrolyzing) microorganisms. Ureolytic microorganisms produce the enzyme urease [6], which catalyzes the hydrolysis of urea (CO(NH2)2) (also known as ureolysis ) that leads to the production of ammonia (NH3) and carbon dioxide (CO2) (Fig. 6.1, Eq. 1). NH3 functions as a Bronsted-Lowry base, generating hydroxide (OH−) ions, resulting in urine alkalization and production of NH4 + (Fig. 6.1, Eq. 2), and ultimately triggering struvite precipitation (Fig. 6.1, Eq. 7). CO2 generation during ureolysis leads to the production of carbonate (CO3 2−) and bicarbonate (HCO3 −) ions (Fig. 6.1, Eqs. 3–5). Formation of CO3 2− can promote the precipitation of carbapatite and calcium carbonate (Fig. 6.1, Eqs. 6 and 8), which have been described to occur at pH˜6.8 and lower. Carbapatite crystals appear to aggregate as the pH increases during ureolysis [7].
The particular combination of elevated NH4 + concentration and alkaline urine pH promoting struvite precipitation is almost exclusively associated with the infection of the urinary tract with ureolytic microorganisms, most commonly Proteus spp., Klebsiella spp., Pseudomonas spp., Staphylococcus spp. and some species of E. coli [1, 8, 9]. P. mirabilis, a frequent microorganism involved in UTIs [10], has been the most commonly detected microorganism to be associated with struvite formation.
Biofilm Development and Struvite Precipitation
The presence of pathogens in the urinary tract can lead to biofilm formation, i.e. surface-attached microbial communities embedded in self-produced extracellular polymeric substances (EPS) [11, 12]. Biofilms are generally more resistant to physical and chemical stresses compared to their planktonic counterparts [11, 13, 14]. Biofilm resistance is attributed to the protective effect of the EPS matrix that can hinder the transport of antimicrobials into the biofilm, to the formation of chemical and metabolic gradients within biofilms, and due to other possible resistance mechanisms [13, 15].
Ureolytic biofilm formation in the urinary tract may play a key role in struvite stone formation, as ureolytic microorganisms can provide the appropriate conditions for struvite precipitation, and the EPS matrix can act as additional nucleation site for crystal development. Biofilm development and mineral precipitation in the urinary tract seem to follow a series of steps [16]. (i) attachment of ureolytic microorganisms in the urinary tract: a thin layer is formed comprised of planktonic cells and urinary metabolites, and ureolysis possibly commences; (ii) formation of microcolonies : this is often the first phase of biofilm development accompanied by production of EPS; ureolysis increases the pH, NH4 + and CO3 2− concentrations in the urine; (iii) formation of crystals : primary crystals start forming due to alkaline conditions and increase of NH4 + and CO3 2− in urine (supersaturation leads to carbapatite, struvite and possibly calcium carbonate precipitation, Eqs. 6–8); crystals can become entrapped in the EPS matrix; detachment of microbes from the biofilm may occur; (iv) crystal growth/aggregation and secondary nucleation : crystals form and start growing around the attached bacteria and possibly outside the EPS matrix; planktonic bacteria adhere to pre-existing crystals resulting in the formation of more microcolonies that also precipitate minerals; this results in the formation of layers of bacteria encased in minerals; crystal aggregation is influenced by organic macromolecules in urine (e.g. proteins, lipids, glycosaminoglycans), which can inhibit or promote crystal aggregation [17]; (v) stone formation is the result of repeated cycles of the previous steps (bacterial attachment, formation of microcolonies/biofilms and growth/aggregation of crystals) to integrate minerals within the bacterial biofilm, and vice versa.
The inherent heterogeneous structural, chemical and biological nature of biofilms [13] influences the biomineralization process taking place in the urinary tract (Fig. 6.2). Urine flow and chemistry vary spatially in the urinary tract; ureolytic microorganisms hydrolyze urea, generating NH4 +, changing the local urine saturation; the natural heterogeneity of biofilms [13] creates gradients of NH4 + concentration, and induces mineral precipitation within the biofilm (Fig. 6.2). Urea concentration heterogeneities arise in biofilms due to reaction-diffusion interactions; urea concentration decreases with depth into the biofilm as ureolysis occurs. Oversaturation with respect to minerals such as struvite occurs within and around biofilms owing to the production of NH4 +, carbonates, hydroxyl ions, etc. to increase the saturation index to greater than 0. As the biofilm grows thicker more highly saturated zones develop, which increase the likelihood of mineral precipitation in and around biofilms. Mineral precipitation can potentially occur rapidly at the biofilm-urine i nterface, as the external flow of urine efficiently transports ions to the biofilm [18].
Biofilm induced struvite precipitation. (a) Ureolytic biofilm cross-section in the urinary tract with continuous urine external flow. Ureolytic microorganisms hydrolyze urea, which results in an increase of pH values as well as ammonium (NH4 +) and carbonate (CO3 2−) concentrations in the biofilm and the urine. Minerals form and become entrapped inside and around the microbial biofilm. (b) Shear stress from the urine flow can stretch and deform the biofilm. (c) Transport of urea within the biofilm occurs via diffusion; ureolysis within the biofilm decreases urea concentration inside the biofilms and induces heterogeneity. (d) Certain areas within and around the biofilm become oversaturated with respect to struvite due to the production of NH4 + (saturation index, S > 0); as the biofilm grows thicker areas of supersaturated environment increase. (e) As a result of oversaturation within the biofilm, it is more likely for minerals to precipitate. Mineral precipitation can occur rapidly at the biofilm-urine interface, as the external flow of urine efficiently transports ions to the biofilm surface. This figure was modified based on the results from a mathematical model of biofilm-induced calcite precipitation developed by Zhang and Klapper [18]. (Figured modified and reproduced from Zhang and Klapper [18], with permission from the copyright holders, IWA Publishing)
Investigation of Struvite Stone Formation Using In Vitro and In Silico Techniques
As outlined, infection stone formation is an intricate multi-step process influenced by physicochemical, biochemical and physiological factors. Due to the complexity of biofilm development combined with mineral precipitation in the urinary tract, in vivo observations of stone formation have been hitherto very challenging. The use of controlled laboratory experiments (in vitro) along with computer simulations (in silico) is an attractive alternative to investigating and ultimately developing strategies to control stone formation. In vitro and in silico experiments indeed allow for the study of microbe-mineral interactions at the required spatial and temporal resolution relevant to stone formation. Understanding key microbe-mineral interactions is anticipated to be a key in the development of new treatments and management strategies for struvite stones.
Controlled laboratory experiments such as batch and continuous flow systems have been used to investigate struvite stone formation and the effect of different urine conditions on stone development. Batch experiments have been performed to evaluate (i) the effect of inhibitor or promoter substances on struvite crystallization [7, 19, 20], (ii) the effect of urease inhibitors [21], (iii) the influence of substances potentially inhibiting microbial colonization and biofilm development by uropathogens [23,24,24], and (iv) the resistance of materials to encrustation [25]. However, batch experiments generally do not simulate the flow conditions present in the urinary tract, and generally do not allow for long-term experimentation and assessments. Continuous flow systems allow to simulate the hydraulic conditions in the urinary tract and -if designed properly- for real-time observations over extended periods of time. Flow systems have been mostly used to test ureteral stents, antimicrobials and precipitation-inhibitors (both compounds and devices/materials) [26, 27]. Due to demonstrated reproducibility of results, the Center for Disease Control (CDC) biofilm reactor [28] has been suggested to be used for the evaluation of urological device materials [26]. The CDC reactor allows for the observation of biofilm growth and mineral precipitation over time under tightly controlled conditions using removable coupons (Fig. 6.3a). Flow systems have also been developed to test the resistance of different biomaterials used in urinary tract devices against colonization and encrustation (e.g. silicone, polyurethane, Percuflex) [27]; flow systems allow for the exposure of stent devices to flows similar to those in the urinary tract (Fig. 6.3b). Hobbs et al. [29] developed an in vitro laboratory model to investigate infection stone formation. The model simulates the urinary tract system using a series of analog components: CDC reactors as kidney and bladder analogues, tubing and glass capillaries simulating the ureter, and sponge coupons representing the porous structure of the kidneys. This system indeed allows for the real-time observation of biofilm formation and mineral precipitation (Fig. 6.3c). The CDC reactor used as kidney analog allows for sampling of the coupons over time; biofilm-mineral composites accumulate on the coupons as a result of ureolysis induced by ureolytic microorganisms in the reactor; glass capillaries integrated in the “ureter” line allow for microscopic observations over time to assess bacterial migration or mineral precipitation.
Investigation of biofilm formation and mineral precipitation in the urinary tract should consider the effect of physicochemical factors including reaction (e.g. ureolysis and precipitation), transport (e.g. advection and diffusion), and hydrodynamics (e.g. fluid flow and shear stress). Furthermore, the viscoelasticity and mechanical properties of the biofilm-mineral composites should be considered when investigating mineral precipitation in infected urinary tract systems. As stated above, biofilms are non-uniform systems with structural, biological and chemical heterogeneity; moreover, biofilms in the urinary tract are subjected to fluctuating conditions, such as variations in urine flow and urine chemistry [18]. Quantitative descriptions of urine flow and urine chemistry can be obtained using mathematical modeling along with the simulation of biofilm development and mineral precipitation similarly to work done in the development of engineered biomineralization technologies [31,32,33,34,35,35].
Reactive transport modeling is a tool commonly used in engineering that allows for the analysis of coupled physical, chemical and biological processes [36]. An example of a user-friendly modeling program that can be used to model reactive transport is COMSOL Multiphysics® software (a finite element framework, COMSOL Inc., Burlington, MA, USA). Connolly et al. [33] used this software to estimate biofilm-specific kinetics of ureolytic biofilms (E. coli MJK2) in flow systems. Estimating ureolysis biofilm-kinetics along with other tools to characterize biofilms (e.g. confocal microscopy) can aid in understanding local chemical gradients in ureolytic biofilms. Hence, determining biofilm-specific kinetics can provide a more accurate representation of biofilms in flow systems, for example, development of ureolytic biofilms on urethral catheters [37].
Geochemical modeling software can simulate the saturation conditions of aqueous solutions (e.g. urine) under a variety of conditions and can predict the likelihood of precipitation. Geochemical modeling estimates the saturation state of a system by considering the chemical species in solution and the influence of solid phases. Common geochemical modeling packages are Visual MINTEQ [38] and PHREEQC [39]. These computer-based models can be used to simulate saturation conditions, pH and ionic strength in urine, and thus predict the potential for mineral (e.g. struvite) precipitation [40], which could lead to stone formation. Combinations of different modeling tools (e.g. COMSOL-PHREEQC) [41] can provide an insight into systems as complex as the urinary tract, in which formation of ureolytic biofilms under flow conditions along with mineral precipitation is occurring, taking into account urine chemistry and changes in hydrodynamics.
Summary
The formation of struvite stones (MgNH4PO4·6H2O), also known as infection stones, is typically associated with urinary tract infections, particularly, with ureolytic microorganisms. These microorganisms hydrolyze urea, produce ammonium (NH4 +) and potentially increase the urine pH. This process, in turn, can affect urine chemistry and can promote struvite and other mineral precipitation. Ureolytic biofilm development in the urinary tract (e.g. on implanted devices) can provide the conditions necessary for struvite precipitation and stone formation. Factors that influence stone formation and that need to be considered when investigating infection stone formation include: (i) the structural, chemical and biological heterogeneity of biofilms, (ii) urine chemistry and its effect on mineral precipitation and biofilm formation; (iii) presence of modulators in urine (inhibitors or promoters of crystal growth and aggregation, e.g. organics), and (iv) the hydrodynamic conditions (flow) in the urinary tract. Controlled experiments and computer simulations can aid in better understanding the microbe-fluid-mineral interactions occurring within ureolytic biofilms in the urinary tract system. A more comprehensive understanding of stone formation is predicted to ultimately lead to the development of improved management and prevention strategies for infection stones.
References
Bichler KH, et al. Urinary infection stones. Int J Antimicrob Agents. 2002;19(6):488–98.
Flannigan RK, et al. Evaluating factors that dictate struvite stone composition: a multi-institutional clinical experience from the EDGE Research Consortium. Can Urol Assoc J. 2018;12(4):131–6.
Finlayson B. Physicochemical aspects of urolithiasis. Kidney Int. 1978;13(5):344–60.
Fleisch H. Inhibitors and promoters of stone formation. Kidney Int. 1978;13(5):361–71.
Finlayson B, Reid F. The expectation of free and fixed particles in urinary stone disease. Investig Urol. 1978;15(6):442–8.
Mobley HL, Hausinger RP. Microbial ureases: significance, regulation, and molecular characterization. Microbiol Rev. 1989;53(1):85–108.
Prywer J, Mielniczek-Brzóska E, Olszynski M. Struvite crystal growth inhibition by trisodium citrate and the formation of chemical complexes in growth solution. J Cryst Growth. 2015;418:92–101.
Golechha S, Solanki A. Bacteriology and chemical composition of renal calculi accompanying urinary tract infection. Indian J Urol. 2001;17(2):111–7.
Thompson R, Stamey T. Bacteriology of infected stones. Urology. 1973;2(6):627–33.
Schaffer JN, Pearson MM. Proteus mirabilis and urinary tract infections. Microbiol Spectr. 2015;3(5) https://doi.org/10.1128/microbiolspec.UTI-0017-2013.
Flemming H-C, Wingender J. The biofilm matrix. Nat Rev Microbiol. 2010;8:623–33.
Jacobsen SM, Shirtliff ME. Proteus mirabilis biofilms and catheter-associated urinary tract infections. Virulence. 2011;2(5):460–5.
Stewart S, Franklin MJ. Physiological heterogeneity in biofilms. Nat Rev Microbiol. 2008;6(3):199–210.
Nickel JC, et al. Bacterial biofilms: influence on the pathogenesis, diagnosis and treatment of urinary tract infections. J Antimicrob Chemother. 1994;33(Suppl A):31–41.
Mah T-FC, O’Toole GA. Mechanisms of biofilm resistance to antimicrobial agents. Trends Microbiol. 2001;9(1):34–9.
Espinosa-Ortiz EJ, Eisner BH, Lange D, Gerlach R. Current insights into the mechanisms and management of infection stones. Nature Reviews Urology. 2019;(1):35–53. https://doi.org/10.1038/s41585-018-0120-z.
Aggarwal KP, et al. Nephrolithiasis: molecular mechanism of renal stone formation and the critical role played by modulators. Biomed Res Int. 2013;2013:292953.
Zhang T, Klapper I. Mathematical model of biofilm induced calcite precipitation. Water Sci Technol. 2010;61(11):2957–64.
Chauhan CK, Joshi MJ. In vitro crystallization, characterization and growth-inhibition study of urinary type struvite crystals. J Cryst Growth. 2013;362:330–7.
Olszynski M, Prywer J, Mielniczek- Brzóska E. Inhibition of struvite crystallization by tetrasodium pyrophosphate in artificial urine: chemical and physical aspects of nucleation and growth. Cryst Growth Des. 2016;16(6):3519–29.
Jones DS, Djokic J, Gorman SP. Characterization and optimization of experimental variables within a reproducible bladder encrustation model and in vitro evaluation of the efficacy of urease inhibitors for the prevention of medical device-related encrustation. J Biomed Mater Res B Appl Biomater. 2006;76B(1):1–7.
O’May C, et al. Cranberry derivatives enhance biofilm formation and transiently impair swarming motility of the uropathogen Proteus mirabilis HI4320. Can J Microbiol. 2016;62(6):464–74.
Rajasekharan SK, et al. Burdock root extracts limit quorum-sensing-controlled phenotypes and biofilm architecture in major urinary tract pathogens. Urolithiasis. 2015;43(1):29–40.
Salini R, et al. Inhibition of quorum sensing mediated biofilm development and virulence in uropathogens by Hyptis suaveolens. Anton Van Leeuw. 2015;107(4):1095–106.
Venkatesan N, et al. Effect of uropathogens on in vitro encrustation of polyurethane double J ureteral stents. Urol Res. 2011;39(1):29–37.
Gilmore BF, et al. Validation of the CDC biofilm reactor as a dynamic model for assessment of encrustation formation on urological device materials. J Biomed Mater Res B Appl Biomater. 2010;93B(1):128–40.
Gorman SP, et al. Design and validation of a dynamic flow model simulating encrustation of biomaterials in the urinary tract. J Pharm Pharmacol. 2003;55(4):461–8.
Goeres DM, et al. Statistical assessment of a laboratory method for growing biofilms. Microbiology. 2005;151(3):757–62.
Hobbs T, et al. Evaluation of biofilm induced urinary infection stone formation in a novel laboratory model system. J Urol. 2018;199(1):178–85.
Hommel J, et al. Finding a balance between accuracy and effort for modeling biomineralization. Energy Procedia. 2016;97:379–86.
Phillips AJ, et al. Fracture sealing with microbially-induced calcium carbonate precipitation: a field study. Environ Sci Technol. 2016;50(7):4111–7.
Hommel J, et al. A revised model for microbially induced calcite precipitation: improvements and new insights based on recent experiments. Water Resour Res. 2015;51(5):3695–715.
Connolly JM, et al. Estimation of a biofilm-specific reaction rate: kinetics of bacterial urea hydrolysis in a biofilm. NPJ Biofilms Microbiomes. 2015;1:15014.
Ebigbo A, et al. Darcy-scale modeling of microbially induced carbonate mineral precipitation in sand columns. Water Resour Res. 2012;48:W07519.
Ebigbo A, et al. Modelling biofilm growth in the presence of carbon dioxide and water flow in the subsurface. Adv Water Resour. 2010;33(7):762–81.
Steefel CI, DePaolo DJ, Lichtner PC. Reactive transport modeling: an essential tool and a new research approach for the Earth sciences. Earth Planet Sci Lett. 2005;240(3):539–58.
Morris NS, Stickler DJ, McLean RJ. The development of bacterial biofilms on indwelling urethral catheters. World J Urol. 1999;17(6):345–50.
Gustafsson JP. Visual MINTEQ 3.1. 2000. Available from: https://vminteq.lwr.kth.se/.
Parkhurst DL, Appelo CAJ. User’s guide to PHREEQC (Version 2): a computer program for speciation, batch-reaction, one-dimensional transport, and inverse geochemical calculations. In: Water-resources investigations report. 1999.
Ronteltap M, Maurer M, Gujer W. Struvite precipitation thermodynamics in source-separated urine. Water Res. 2007;41(5):977–84.
Nardi A, et al. Interface COMSOL-PHREEQC (iCP), an efficient numerical framework for the solution of coupled multiphysics and geochemistry. Comput Geosci. 2014;69:10–21.
Acknowledgements
This work was supported by the Montana University System Research Initiative (51040-MUSRI2015-03), a grant from Montana NASA EPSCoR Research Infrastructure Development, and the Burroughs Wellcome Fund (grant #1017519). This chapter is dedicated to J.W. (Bill) Costerton and Mark E. Shirtliff who dedicated their lives to biofilm research and teaching.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Espinosa-Ortiz, E.J., Gerlach, R. (2019). Struvite Stone Formation by Ureolytic Biofilms. In: Lange, D., Scotland, K. (eds) The Role of Bacteria in Urology. Springer, Cham. https://doi.org/10.1007/978-3-030-17542-9_6
Download citation
DOI: https://doi.org/10.1007/978-3-030-17542-9_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-17541-2
Online ISBN: 978-3-030-17542-9
eBook Packages: MedicineMedicine (R0)