Abstract
This is a first-hand description of the discovery by the author that the blood coagulation mechanism of Limulus polyphemus, the horseshoe crab, was exquisitely sensitive to bacterial endotoxins. The author recognized the potential usefulness of this observation and utilized his data to provide the basis for the invention of the Limulus amebocyte lysate (LAL) test for the detection of bacterial endotoxin. The great superiority, both in sensitivity and ease of use, of the Limulus amebocyte lysate test to the then utilized rabbit pyrogen test (RPT) eventually resulted in its official approval. Subsequently, the LAL test became and remains the international standard for the detection of bacterial endotoxins in parenteral drugs, intravenous fluids, and implanted biomedical devices.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
1 Introduction
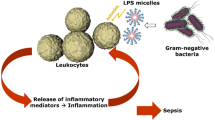
In 1956, Dr. Frederik B. Bang, a Professor at the Johns Hopkins University School of Hygiene and Public Health, reported his studies of the effects of bacterial infection in Limulus polyphemus, the horseshoe crab in the no longer published Bulletin of the Johns Hopkins Hospital [1]. Dr. Bang had undertaken these studies because of his observation that one horseshoe crab had become ill after it had been injected with bacteria present in sea water, which is known to contain significant numbers of Gram-negative bacteria. He noted that due to the infection the blood of the animal had subsequently become uncoagulable, in marked contrast to the coagulation that is uniformly observed when blood is removed from Limulus. He cultured the bacterium from this animal and when reinjected into other Limuli, this bacterium, which was shown to be a Gram-negative rod, caused intravascular coagulation and death. The same effect was produced by a heat stable extract of this bacterium, prepared by heating and disrupting the bacteria. This technique is the traditional method for the production of crude bacterial endotoxin. He also noted that the level of circulating amebocytes was reduced in these animals, and that the amebocytes were degranulated [1]. Pertinently, these effects were not produced by extracts of pneumococci, staphylococci or streptococci, all of which are Gram-positive bacteria. The similarity between the reaction observed in Limuli and the generalized Shwartzman reaction, which is caused by multiple injections of bacterial endotoxin, was obvious.
Bang’s initial observations were put aside for almost 10 years, until 1963, when Dr. Bang discussed his data with Dr. C. Lockard Conley, then the director of the Hematology Division at The Johns Hopkins University School of Medicine and Hospital. Dr. Bang and Dr. Conley decided that if a hematologist carried out investigations with Dr. Bang, an effective collaboration would result. I was then a Research Fellow in Dr. Conley’s hematology division, in the midst of carrying out experiments based on the Shwartzman reaction and also studying platelet function. Because of my interests in these two areas, and the effects of bacterial endotoxin on platelets and blood coagulation, Dr. Conley suggested that I join Dr. Bang for a Summer of research at the Marine Biological Laboratory (MBL) in Woods Hole, Massachusetts, which I did in 1963, never having previously heard of, much less seen, a horseshoe crab. Experiments were initially designed to determine similarities between Limulus amebocytes, the only type of circulating blood cell in the horseshoe crab (Fig. 1.1), and human platelets.
2 Early Observations and Test Development
I was quickly able to demonstrate that cell-free plasma from Limulus would not clot [2], but learning more about amebocytes and coagulation initially proved difficult because samples of blood which were liquid when I left the laboratory in the evening were solidly clotted by the next morning. None of the standard anticoagulants used to prevent the coagulation of human blood, i.e., sodium citrate, EDTA, or heparin, were effective in preventing Limulus blood from clotting [2, 3]. Puzzled by this, I considered the possibility of contamination of the samples either by bacteria or a bacterial component, and when samples were drawn into sterile and pyrogen-free glass tubes, the latter being considered only because of my ongoing studies of the effects of bacterial endotoxin on blood coagulation, Limulus blood did not clot. We were then able to demonstrate that the coagulation system, or at least some of its components, were released from amebocytes [2]. Importantly, Limulus plasma which contained cellular components, i.e., factors derived from the circulating amebocytes, could be gelled by bacterial endotoxin, using either a heat stable component from the Vibrio species that Dr. Bang had isolated in 1957 or E. coli endotoxin. An extract of a pathogenic Gram-positive marine bacterium had no effect [2]. The rate of coagulation was dependent on the concentration of endotoxin, and we suggested that an enzymatic mechanism was involved [2]. Importantly, it was then demonstrated that the entire blood coagulation mechanism of Limulus was contained in the amebocytes [2]. Dr. Erik Murer and I subsequently determined that the granules of amebocytes contained the entire blood coagulation mechanism of the horseshoe crab [4].
In 1965, after having completed my two-year hematology research fellowship (1962–1964) and having been the Chief Resident in Medicine (1964–1965) at the Yale-New Haven Medical Center in New Haven, CT, I became a member of the faculty of the Hematology division at Hopkins. I returned to Woods Hole in the Summer of 1965, the second of many Summers at the MBL, where I subsequently served as member of the Board of Trustees (1988–1993). I then used N-ethylmaleimide (NEM) to prepare washed amebocytes, from which lysates, free of any plasma factors, could be prepared [5]. The conditions for this step were critical, since it was necessary to not only prevent the amebocytes from aggregating but to then be able to successfully wash and lyse them.
During this period, we described the preparation of Limulus amebocyte lysate and the basic characteristics of the Limulus amebocyte lysate (LAL) test for bacterial endotoxins [5]. Fig. 1.2 shows the author bleeding an adult horseshoe crab. Note the total absence of any of the now required conditions for the bleeding of horseshoe crabs for the preparation of GMP certified lysate. It should also be emphasized that bleeding was performed in a standard research laboratory, with the windows usually open, no temperature controls, and high humidity as the result of sea water continuously running into an open tank and splashing onto the laboratory floor. Despite these conditions, the author bled hundreds of animals without ever producing a contaminated batch of amebocytes, which provided the sole basis for a highly sensitive test for bacterial endotoxins.
Dr. Jack Levin bleeding a horseshoe crab in his laboratory at the Marine Biological Laboratory, Woods Hole, MA (circa 1970). Blood flows via a needle directly from the cardiac sinus into an endotoxin-free siliconized flask which contains a warmed solution of N-ethyl maleimide (NEM). NEM prevents the amebocytes from aggregating. Limulus blood is blue because it contains a high concentration of hemocyanin, the oxygen carrying protein in the plasma
The gel clot endpoint is shown in Fig. 1.3. The change from a clear liquid to an opaque gel is obvious. Interestingly, although this gel is very stable if undisturbed, if the tube is shaken, the gel will not reform but rather becomes a viscous mass of similarly opaque particulate material. Since the rate of the reaction between bacterial endotoxin and Limulus amebocyte lysate is dependent upon the concentration of endotoxin, one can quantitatively determine the concentration of endotoxin by measuring the rate of increase in optical density (Fig. 1.4) [5] or light scattering (Fig. 1.5) [6]. These three initially described endpoints remain the basis for the endpoints currently in commercial use. The insert in Fig. 1.4 established that the reaction between bacterial endotoxin and amebocyte lysate was enzymatic. Subsequent studies from our laboratory elaborated the enzymatic nature of the reaction [7,8,9]. Ours was the first report of an enzymatic blood coagulation mechanism in an invertebrate and it was established that serine proteases played an important role in the enzymatic reaction [10].
Increase in optical density after addition of different concentrations of E. coli endotoxin. The rate of increase in optical density was dependent upon the concentration of endotoxin. The semi-log plot (insert) indicates that the reaction between Limulus amebocyte lysate and endotoxin is enzymatic. (From Ref. [5], with permission.)
Rate of increase in light scattering after addition of bacterial endotoxin from E. coli. The concentration of endotoxin is shown in μg/ml. As the concentration of endotoxin decreased, the rate of increase in light scattering decreased. (From Ref. [6], with permission.)
Critical to the acceptance of a new bioassay is the demonstration that the assay, e.g., the Limulus test, correlated with other established assays for endotoxin. Although this was eventually demonstrated (Table 1.1), some skepticism remained because the much greater sensitivity of the Limulus amebocyte lysate (LAL) test in comparison to the other available bioassays made it impossible to directly compare the results of the LAL test with other assays at the lowest concentrations of endotoxin which LAL could detect.
LAL was prepared by the vigorous disruption of washed amebocytes with unbuffered distilled water. We thoroughly investigated whether LAL was gelled by β-glucans and it was not [11]. The specificity of LAL as prepared in my laboratory is emphasized because subsequently, it was observed that LAL prepared commercially was sensitive to β-glucans. The commercial methods for preparation of amebocyte lysate involve the use of buffers and other additives, and the proprietary nature of the various commercial methods makes it impossible to learn which additives or perhaps pH adjustments resulted in Limulus amebocyte lysate becoming sensitive to β-glucans via active Factor G (Fig. 1.6). It is noteworthy that unbuffered LAL, as prepared in my laboratory, remains stable in liquid form for many years.
3 Official Approval of the Limulus Amebocyte Lysate Test by Federal Agencies
Since the rabbit pyrogen test (RPT) was the well-established official standard for the detection of bacterial endotoxins, a comparison of the LAL test with the RPT was mandatory if the Limulus test was going to be accepted. Thus, such a study was performed by James Cooper, then a graduate student at Hopkins, and myself [12]. This demonstrated that the results of a LAL test could be effectively compared with the RPT (Fig. 1.7). Cooper subsequently introduced the Limulus lysate assay to the FDA. An important major comparison of the Limulus and rabbit pyrogen tests by Mascoli and Weary clearly demonstrated the superiority of the Limulus test, which did not produce a single false negative in almost 30,000 tests, in addition to being much more sensitive than the RPT (Table 1.2). It is pertinent that the period during which these early studies were performed preceded the establishment of endotoxin standards, and thus the official Endotoxin Unit (EU) did not come into existence until after the LAL test became available. In many respects, it was the LAL test which made necessary the establishment of an international endotoxin standard based on biological activity. Prior to this, endotoxin concentrations were described by their weight. Since the biological activity of a given weight of endotoxin depends at least in part on the intrinsic biological activity of the specific endotoxin and its method of preparation, it had been difficult to compare the results of experiments, performed in different laboratories, in which endotoxin was used. However, this problem had been partially managed by the common use of endotoxin from E. coli O55:B5 in many research laboratories.
Gelation of Limulus amebocyte lysate by E. coli or Klebsiella endotoxin vs. rabbit pyrogenicity. Gelation times increased as the concentration of endotoxin decreased. Arrows indicate gelation times of pyrogenic concentrations of endotoxin. Gelation times shorter than the red line correlated with rabbit pyrogenicity; gelation times longer than the blue line (to the right) correlated with non-pyrogenicity. (from Ref. [12], with permission.)
Multiple steps were required to define the methods for the use of the LAL test for release of parenteral drugs and intravenous fluids. Extensive discussions of the approved use of the LAL test occurred at an international conference in Woods Hole, MA in 1981 [13,14,15]. Although the Limulus test was adequately described in 1965, it required almost 20 years for it to be formally announced as being validated as an end-product endotoxin test in the Federal Register (Fig. 1.8). Another more recent summary of the steps required for the validation of the LAL test was published in 2003 [16]. By 1984, there were 8 FDA licensed Limulus lysate manufacturers in the U.S. An amebocyte lysate made in Japan (TAL) from the Asian horseshoe crab, Tachypleus tridentatus was also licensed. However currently there are only 4 licensed commercial sources. A brief history of the commercialization of the Limulus test is available [17]. A detailed summary and overview of the sequence of these events is provided in Table 1.3.
An important early impact of the Limulus test was that for the first time, it was feasible for research laboratories to determine if their reagents had biologically significant concentrations of endotoxin. This was especially important when experimental models were susceptible to the effects of endotoxin. This was often the case [18, 19]. Thus, data from such experimental models were seriously flawed. Importantly, the availability of a highly sensitive and feasible test had an impact on the safety of parenteral drugs and fluids. An early example was the effective clinical use of the Limulus Test to demonstrate that an outbreak of pyrogenic reactions to serum albumin infusions was due to contaminating bacterial endotoxin [20]. The Limulus test has also been used successfully to detect endotoxin in the blood of patients suspected of having endotoxemia [21], as well as in other body fluids.
4 End Points for the Detection of Endotoxin
The gel clot was the first endpoint officially approved for the Limulus test. For reasons unknown, it was decided that the gel clot assay had to be read at a single time point, i.e., 1 hour. A solid gel was required for a positive result. Since the reaction between endotoxin and Limulus lysate is enzymatic, it is obvious that a longer incubation time for the readout would result in a marked increase in the sensitivity. Unfortunately, my efforts to convince the FDA to have the gel clot endpoint serially read at multiple time points failed. However, when chromogenic and turbidimetric kinetic methods were introduced, this significant limitation of sensitivity was bypassed. Nevertheless, it should be pointed out that the gel clot end point technique, if not limited to 1 hour, is as sensitive as the chromogenic and turbidimetric kinetic assays (Fig. 1.9) [22].
End points for performance of Limulus test for bacterial endotoxin. Comparison of amidolytic activity quantified by measurement of PNA absorbance or of PNA-DACA Schiff base absorbance with visual gelation method. Amidolytic activity was generated by incubation of Limulus lysate with various concentrations of E. coli endotoxin and quantified with the chromogenic substrate, S-2222. Measurements of absorbance were: free PNA at 405 (•); and PNA-DACA complex at 575 (O). Additional samples also were scored visually after incubation for I day for presence of borderline flocculation(F-), heavy flocculation(F+), or gelation(G). Results of representative experiment are shown. (From Ref. [22], with permission)
5 Conclusion
Serendipity has been defined in a variety of related ways. The term is often used incorrectly to indicate a purely accidental observation or discovery. It is more than that, as illustrated by the definitions shown (Table 1.4). The Limulus test would never have been conceived and then established if during my initial struggles with Limulus blood and its very biologically active amebocytes I had not also been studying the effects of bacterial endotoxin on blood coagulation and platelets in rabbits. Lacking the experience and knowledge of the literature gained from my rabbit experiments, I would never have considered the possibility that the spontaneous aggregation and disruption of Limulus amebocytes, with activation of blood coagulation despite the blood being anticoagulated, was due bacterial endotoxin. In 1960, A. V. Hill wrote “By the methods of comparative physiology, or of experimental biology, by the choice of a suitable organ, tissue or process, in some animal far removed in evolution, we may often throw light upon some function or process in the higher animals, or in man.” [23]. The “basic research” that unexpectedly led to the discovery of the sensitivity of the blood coagulation mechanism in Limulus to bacterial endotoxin and subsequent development of the Limulus test validates Hill’s thoughtful and wise statement.
References
Bang FB. A bacterial disease of Limulus polyphemus. Bull Johns Hopkins Hosp. 1956;98:325–51.
Levin J, Bang FB. The role of endotoxin in the extracellular coagulation of Limulus blood. Bull Johns Hopkins Hosp. 1964;115:265–74.
Levin J, Bang FB. A description of cellular coagulation in the Limulus. Bull Johns Hopkins Hosp. 1964;115:337–45.
Murer EH, Levin J, Holme R. Isolation and studies of the granules of the amebocytes of Limulus polyphemus, the horseshoe crab. J Cell Physiol. 1975;86:533–42.
Levin J, Bang FB. Clottable protein in Limulus: Its localization and kinetics of its coagulation by endotoxin. Thromb Diath Haemorrh. 1968;19:186–97.
Levin J, Tomasulo PA, Oser RS. Detection of endotoxin in human blood and demonstration of an inhibitor. J Lab Clin Med. 1970;75:903–911.
Nakamura S, Levin J. Fractionation of Limulus amebocyte lysate. Characterization of activation of the proclotting enzyme by an endotoxin-mediated activator. Biochim Biophys Acta. 1982;707:217–25.
Nakamura S, Levin J. Endotoxin-mediated Limulus proclotting enzyme activator and detection of a previously undescribed protease (protease N). Biochem Biophys Res Comm. 1982;108:1619–32.
Torano AE, Nakamura S, Levin J. Properties of the clotting enzyme responsible for endotoxin-mediated Limulus coagulation. Thromb Res. 1984;34:407–17.
Young NS, Levin J, Prendergast RA. An invertebrate coagulation system activated by endotoxin: evidence for enzymatic mediation. J Clin Invest. 1972;51:1790–7.
Soderhall K, Levin J, Armstrong PB. The effects of β1,3-glucans on blood coagulation and amebocyte release in the horseshoe crab, Limulus polyphemus. Biol Bull. 1985;169:661–74.
Cooper JF, Levin J, Wagner HN Jr. Quantitative comparison of in vitro and in vivo methods for the detection of endotoxin. J Lab Clin Med. 1971;78:138–48.
Munson TE. FDA guideline for validation of the LAL test as an end-product endotoxin test for human and biological fluids. In: Watson SW, Levin J, Novitsky TN, editors. Endotoxins and their detection with the Limulus amebocyte lysate test. New York: Alan R Liss, Inc.; 1982. p. 25–32.
Outschoorn AS. The USP bacterial endotoxin test. In: Watson SW, Levin J, Novitsky TN, editors. Endotoxins and their detection with the Limulus amebocyte lysate test. New York: Alan R Liss, Inc.; 1982. p. 33–8.
Ross VC, Bruch CW. Endotoxin testing of medical devices with LAL: FDA requirements. In: Watson SW, Levin J, Novitsky TN, editors. Endotoxins and their detection with the Limulus amebocyte lysate test. New York: Alan R Liss, Inc.; 1982. p. 39–48.
Levin J, Hochstein HD, Novitsky TJ. Clotting cells and Limulus amebocyte lysate: an amazing analytical tool. In: Shuster Jr CN, Barlow RB, Brockmann HJ, editors. The American horseshoe crab. Cambridge: Harvard University. Press; 2003. p. 310–40.
Cooper JF. Discovery and acceptance of the bacterial endotoxins test. In: McCullough KZ MC, editor. The bacterial endotoxins test: a practical approach. River Grove: Davis Healthcare International Publishing, LLC; 2011. p. 1–14.
Zuckerman KS, Quesenberry PJ, Levin J, Sullivan R. Contamination of erythropoietin by endotoxin: in vivo and in vitro effects on murine erythropoiesis. Blood. 1979;54:146–58.
Gordon T, Milligan SA, Levin J, Thompson JE, Fine JM, Sheppard D. Apparent effect of catalase on airway edema in guinea pigs. Role of endotoxin contamination. Am Rev Respir Dis. 1987;135:854–9.
Hochstein HD, Seligmann EB, Marquina RE, Rivera R. Limulus amebocyte lysate testing of normal serum albumin (human) released in the United States since 1975. Dev Biol Stand. 1975;44:35.
Levin J, Poore E, Young NS, et al. Gram-negative sepsis: detection of endotoxemia with the Limulus test. Ann Int Med. 1972;76:1–7.
Roth RI, Levin J, Behr S. A modified Limulus amebocyte lysate test with increased sensitivity for detection of bacterial endotoxin. J Lab Clin Med. 1989;114:306–11.
Hill AV. Experiments on frogs and men. In: Hill AV, editor. The ethical dilemma of science and other writings. New York: Rockefeller Institute Press; 1960. p. 24–38.
Mascoli CC, Weary ME. Applications and advantages of the Limulus Amebocyte Lysate (LAL) pyrogen test for parenteral injectable products. In: Cohen E, Bang FB, Levin J, et al., editors. Biomedical applications of the horseshoe crab (Limulidae). New York: Alan R. Liss, Inc.; 1979. p. 387–402.
Acknowledgment
The author wishes to thank Dr. Thomas Novitsky for sharing his insights into the years during which Limulus amebocyte lysate transitioned from the research laboratory into commercial development as the Limulus amebocyte lysate (LAL) test for bacterial endotoxins.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Levin, J. (2019). Discovery and Early Development of the Limulus Test. In: Williams, K. (eds) Endotoxin Detection and Control in Pharma, Limulus, and Mammalian Systems. Springer, Cham. https://doi.org/10.1007/978-3-030-17148-3_1
Download citation
DOI: https://doi.org/10.1007/978-3-030-17148-3_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-17147-6
Online ISBN: 978-3-030-17148-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)