Abstract
Peritoneal mesothelioma (PM) is an uncommon and locally aggressive tumor encompassing a wide spectrum of biological behaviors, from clinically indolent to rapidly fatal disease. PM has been historically treated with debulking (DBK) surgery and/or palliative systemic chemotherapy (sCT), resulting in a median survival of only 1 year in the malignant variants. The biology of this disease has been poorly understood until recent years when mechanisms of resistance to therapy and new potential molecular therapeutic targets have been thoroughly investigated. Pathological and histological classifications of PM are still evolving. The clinical management of these conditions has improved during the last 30 years with the advent of a comprehensive treatment approach involving cytoreductive surgery (CRS) and intraperitoneal drug administration, such as hyperthermic intraperitoneal chemotherapy (HIPEC), resulting in increased patient survival. This review addresses relevant clinical and biological issues of PM, including molecular features, diagnosis, pathology, role of modern systemic and targeted therapies, patient selection for combined surgical treatment, surgical technique, and prognostic factors.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Diffuse malignant peritoneal mesothelioma
- Cytoreductive surgery
- Hyperthemic intraperitoneal chemotherapy (HIPEC)
- Well differentiated papillary peritoneal mesothelioma
- Multicystic peritoneal mesothelioma
21.1 Introduction
Mesothelioma is an uncommon tumor arising from the mesothelial cells lining the pleura, peritoneum, pericardium, and tunica vaginalis layer of testis [1]. Peritoneal mesothelioma (PM) represents about one-fifth to one-third of all forms of mesothelioma. The definition of PM includes a constellation of disease entities with different clinical presentation, biological behavior, and prognosis. Localized PM is uncommon and generally benign. On the contrary, diffuse malignant peritoneal mesothelioma (DMPM) is the commonest and more aggressive variant. Well-differentiated papillary peritoneal mesothelioma (WDPPM) and multicystic peritoneal mesothelioma are exceedingly rare and borderline malignant conditions. In its malignant forms, the disease has been traditionally considered as an end-stage disseminated condition and treated with debulking (DBK) and/or palliative systemic chemotherapy (sCT). Treatment options were mainly palliative and minimally effective. The interest in this disease on part of biological and clinical researchers was poor. Only in recent years, an increasing number of patients with PM have been treated with cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC), resulting in remarkable survival improvements and increased interest in this disease. This chapter reviews several relevant issues regarding the surgical and local-regional management of DMPM and the borderline PM sub-variants.
21.2 Epidemiology of Peritoneal Mesothelioma
Age-adjusted incidence rates in the Surveillance, Epidemiology, and End Results (SEER) database (1973–2003) for DMPM were 1.2 per 1,000,000 person-year in men and 0.8 per 1,000,000 person-year in women. In Europe, crude incidence based on the RARECARE database (1995–2002) for both genders combined was 1.3 per 1,000,000 person-year [2]. In 2008 in Italy, the incidence of DMPM in men and women were 2.6 and 1.2 per 1,000,000 person-year, respectively, with wide variations within the country. Higher rates are reported in smaller areas with widespread past use of asbestos, such as the harbor city of Genoa or Casale Monferrato (age-standardized incidence in men in 1995 was 5.5/1,000,000) (www.ispesl.it\renam\index.asp). An increase of 5–10% in the annual mortality rate will be observed worldwide at least until 2020. The disease has likely already reached its incidence peak in the USA. On the contrary, in Europe and Australia, the peak is expected during this decade [3]. The role of asbestos exposure in DMPM has not been clearly established as in the pleural forms. It is estimated that 58% of men and only 20% of women with DMPM had past asbestos exposure [4]. Therefore, it has been suggested that etiology of DMPM may differ between men and women. Since no asbestos exposure is documented in about 20–40% of DMPM, it has been suggested that other factors may be the determinants. Simian Virus 40 (SV40) is a possible co-factor in mesothelioma oncogenesis, and the hypothesis of a genetic susceptibility with an autosomal dominant pattern is based on observations gathered in Cappadocia [5, 6].
21.3 Molecular Biology
The molecular and cellular mechanisms underlying the proliferative potential and resistance to therapy of DMPM are still poorly understood. The biology of this disease has been thoroughly investigated by clinical and basic science researchers in our institution during the last decade. It has been demonstrated that p16 expression is frequently absent or reduced in DMPM, and EGFR over-expression is more common in peritoneal than pleural forms. However, no correlation with prognosis of over-expression of EGFR, matrix metalloprotease-2 (MMP-2), and MMP-9 was found in patients treated in our center [7, 8].
The Ki-67 is a nuclear antigen expressed during all cellular cycle, except the quiescent (G0) phase. The Ki-67 is an excellent marker of cellular proliferation and tumor aggressiveness. Our group and other groups have shown low Ki-67 expression in DMPM, with a median of 0.6–10% positive cells, but higher expression has been demonstrated to be a strong prognostic factor [8,9,10,11,12]. Analogously, mitotic count is generally low in DMPM, but higher proliferative activity predicts poor prognosis [8].
On the other side, over-expression of cytoprotective factors, such as telomerase activity (TA) and anti-apoptotic mechanisms has been demonstrated in DMPM. TA is expressed in the majority of DMPM and negatively impact prognosis [13]. In DMPM specimens from 38 patients undergoing various therapies; we assessed TA using the telomeric repeat amplification protocol. The alternative lengthening of telomeres (ALT) mechanisms was studied by assaying ALT-associated promyelocytic leukemia nuclear bodies. ALT or TA alone was found in 18.2 and 63.6% of cases, respectively; both ALT and TA were positive in two cases. In the overall series, TA expression was significantly associated with disease relapse (p = 0.018) and cancer-related death (p = 0.045). ALT was not associated with outcome. The prognostic relevance of TA was confirmed in patients uniformly treated by CRS/HIPEC.
Over-expression of cytoprotective factors, including survivin and members of the Inhibitors of apoptosis protein (IAP) family was recently demonstrated by Zaffaroni et al. [14]. The authors have analyzed DMPM proliferative and apoptotic features and tested a survivin knockdown approach in a human DMPM cell line. DMPM cells were transfected with small-interfering RNA (siRNA) targeting survivin mRNA. Survivin expression, growth rate, and ability to undergo spontaneous and drug-induced apoptosis were measured, showing low proliferation rates and poor apoptotic activity in DMPM cells. Survivin was expressed in 91% of cases, and the other IAPs in 69–100%. Transfection of DMPM cells with survivin siRNA resulted in survivin inhibition, decrease in cell growth, and enhancement of spontaneous and drug-induced apoptosis, suggesting that survivin may be a potential target for biological treatments of DMPM.
The above biological features contribute to the lack of effective treatment options in DMPM. We explored novel immunotherapy approaches in an attempt to improve DMPM patients’ survival [15]. We tested CpG-oligodeoxynucleotides (CpG-ODN), synthetic DNA sequences recognized by Toll-like receptor 9 and able to induce innate/adaptive immune response, in two DMPM orthotopic xenografts established in our center, namely MesoII and STO, which properly recapitulate the dissemination pattern of DPMP. Several combined immunodeficiency mice carrying DMPM xenografts were treated at different stages of tumor development with intraperitoneally delivered CpG-ODN1826 for 4 weeks. CpG-ODN1826-induced modulation in the composition of peritoneal immune infiltrate was assessed by flow cytometry. When administered to early-stage tumors (i.e., 4 days after i.p. DMPM cell injection in mice), the agent completely inhibited tumor growth and ascites development (no evidence of tumor masses and ascites in 6/6 mice at necropsy), and also impaired STO tumor uptake and growth (4/6 tumor-free mice; i.p. tumor masses reduced by 94% in the two remaining mice, p = 0.00005). Interestingly, when tested against late-stage STO tumors (i.e., 11 days after i.p. DMPM cell injection in mice), CpG-ODN1826 was still able to reduce the growth of i.p. tumor masses by 66% (p = 0.0009). Peritoneal washings of tumor-bearing mice revealed a strong increase of macrophage infiltration together with a decrease in the presence of B-1 cells and a reduced IgM concentration after CpG-ODN1826 treatment. These data suggest that locally administered CpG-ODN1826 is able to markedly affect the growth of both early- and late-stage DMPM orthotopic xenografts in the absence of severe side effects, and suggest a possible clinical role for the agent in the therapy of DMPM.
An additional line of research has involved the expression of tyrosine kinases receptors (TKRs) [16]. In surgical samples from 20 DMPM patients undergoing CRS/HIPEC in our center, Perrone analyzed TKRs and TKRs downstream pathways, with mTOR and its effectors S6 and 4EBP1, through biochemical and mutational analysis and fluorescent in situ hybridization (FISH). Activation/phosphorylation was shown in 90% of cases for EGFR, in 75% of cases for PDGFRB, and 45% of cases for PDGFRA by immunoprecipitation/Western blot technique. In 100% of cases, no EGFR, PDGFRA, and PDGFRB mutation and gene amplification were demonstrated. AKT, ERK1/2 mTOR, S6, and 4EBP1 were most highly expressed and activated. No mutations of PI3KCA, PTEN, KRAS, and BRAF were seen. The ligand and heterodimerization-dependent activation/expression of EGFR and PDGFRB were demonstrated. Taken together, these findings strongly suggest the potential of TKR receptors and their downstream effectors as targets for molecularly tailored treatments. Based on the concurrent activation of TKR and their downstream effectors, we have designed a clinical-biological study to test the combination TKRs and mTOR inhibitors. In a further analysis, we evaluated the EGFR inhibitor gefinitib, the mTOR inhibitor RAD001, and the multiple TKR inhibitor sorafenib in a DMPM cell line: gefitinib and RAD001 alone showed poor cytotoxic activity; sorafenib had a stronger effect on cellular proliferation and sequential treatment with RAD001 followed by sorafenib-induced a marked synergistic effects in DMPM cells [16].
21.4 Pathology of Peritoneal Mesothelioma
The correct pathological diagnosis of PM is necessary as a variety of other abdominal and pelvic malignancies may present with peritoneal seeding. For example, the majority of patients with papillary serous ovarian cancer do have peritoneal seeding. A high index of suspicion is needed on the part of the pathologist to properly integrate clinical, morphological, and immunostaining findings in order to recognize PM.
Tumors arising from the mesothelial cells lining the abdominal cavity demonstrate a wide spectrum of biological aggressiveness [17]. Adenomatoid tumor and solitary fibrous tumor are truly benign lesions that very unlikely recur after simple excision. The former is a solitary asymptomatic lesion which most often involves genital region peritoneum in reproductive-aged women. Solitary fibrous tumor affects primarily men in their sixth decade [18]. The multicystic variant of PM (MCPM) and well-differentiated papillary variant of PM (WDPPM) are uncommon entities with uncertain malignant potential. At the other extreme, DMPM is a rapidly lethal malignancy, with a median survival of only 1 year when treated with standard therapies. Borderline mesotheliomas and DMPM attract more interest on the part of the medical community and pose substantial problems in the clinical practice.
Classification of PM according to clinical presentation, biological behavior, and pathological features is shown in Table 21.1.
21.4.1 Diffuse Malignant Peritoneal Mesothelioma
DMPM is macroscopically characterized by multiple variably sized grey-white nodules throughout the abdominal cavity. As the disease progresses, the nodules become confluent to form plaques, masses, bowel encasement, or uniformly cover the peritoneal surfaces. Abundant effusion is often present.
Similar to its more frequent pleural counterpart, DMPM is classified as epithelial, sarcomatoid, or biphasic (mixed) [19]. However, the incidence of biphasic tumors is lower than in pleural disease, and pure sarcomatoid DMPM is rare. Epithelial DMPM is composed of polygonal, oval, or cuboidal cells exhibiting cytonuclear features and architectural formations ranging from well-differentiated to anaplastic/pleomorphic appearance. Sarcomatoid tumors and the sarcomatoid component of biphasic DMPM consist of spindle cells arranged in fascicle or storiform pattern [20, 21].
Epithelial DMPM can be further categorized according to the patterns of the epithelial component. The tubulopapillary pattern is one of the most common patterns. It consists of a mixture of small tubules and papillary structures with fibro-vascular cores lined by bland flat, cuboidal, or polygonal cells. The solid pattern consists of nests, cords, or sheets of round, oval, or polygonal cells with abundant eosinophilic cytoplasm and round, vesicular nuclei with prominent nucleoli. The adenomatoid (micro-glandular), acinar, clear-cell, deciduoid, signet-ring cell, small-cell, and rhabdoid patterns are rare [18,19,20,21].
Sarcomatoid DMPM may demonstrate anaplastic, giant-cell, and desmoplastic features, or osteosarcomatous/chondrosarcomatous areas. Atypical histiocytoid-appearing cells within an intense lymphoplasmacytic infiltrate can be seen.
Lymph-node metastases within and outside the abdominal cavity can occur even at the initial manifestation of DMPM. Node involvement has been reported in 7–14% of patients undergoing extensive cytoreductive surgery. By contrast, metastatic disease outside the abdominal cavity is uncommon, except for direct invasion of pleural spaces through the diaphragm [22].
21.4.2 Multicystic and Well-Differentiated Papillary Peritoneal Mesothelioma
Both of these rare disease entities generally affect reproductive-aged women with no history of asbestos exposure and show indolent clinical behaviors. MCPM is often associated with previous abdominal surgery, inflammation, or endometriosis. However, early recurrences requiring multiple surgical interventions, transformation into truly malignant disease, lymph-node involvement, and even death have been described. This, along with the reported clear evidence of diffuse disease distribution throughout the peritoneum and invasion into peritoneal surfaces, suggest that MCPM and WDPPM should be considered as borderline or low-malignant potential conditions, rather than benign tumors [23, 24].
At macroscopic examination, MCPM forms multiple variably sized thin-walled cysts involving primarily the pelvis, but often spreading throughout the abdominal cavity. Microscopically, these cysts are separated by fibrous/adipose septa, and lined by single layers of flattened to cuboidal cells with no or little atypia. WDPPM is characterized by multiple small nodules and, at microscopic level, by well-developed papillary structures with fibrovascular core. The papillae are covered by bland cuboidal cells. Mitoses and atypia are rarely present. The differential diagnosis of WDPPM from the histologically similar but more aggressive tubulopapillary epithelial DMPM is important [25].
21.4.3 Diagnosis and Pathologic Assessment
According to the consensus of expert pathologists from the International Mesothelioma Interest Group (Chicago, IL, October 2006), the diagnosis of DMPM must always be based on an adequate biopsy in the context of appropriate clinical, radiological, and surgical findings [18]. Cytology still plays a limited role in the primary diagnosis, despite the increased accuracy of immunohistochemical and ultrastructural techniques.
The objectives of the pathological workup are:
-
Separating benign from malignant mesothelial proliferations.
-
Differentiating DMPM from other metastatic or primary peritoneal malignancies.
-
Defining the histological sub-variant and other relevant prognostic determinants.
The first step for the diagnosis is hematoxylin–eosin staining. Demonstration of stromal invasion into visceral or parietal peritoneum (or beyond) is the key feature in the differential diagnosis with reactive mesothelial proliferations. However, invasion must be carefully differentiated from entrapment, and the distinction between the rare desmoplastic DMPM and reactive fibrosis may be difficult [25, 26].
Any gastrointestinal carcinoma and, in women, ovarian, primary peritoneal, and, more rarely, lobular breast carcinoma should be considered for the differential diagnosis of epithelial DMPM. The differential diagnosis for sarcomatoid DMPM includes sarcoma and other spindle cells neoplasms, such as sarcomatoid renal carcinoma and, particularly for biphasic DMPM, synovial sarcoma [18]. Since no immunohistochemical marker is entirely specific and sensitive for mesothelioma, the standard is to use panels of positive and negative markers. Mesothelioma is characterized by positive staining for EMA, calretinin, Wilms tumor-1 antigen, cytokeratin 5/6, HBME-1, podoplanin, and mesothelin. Depending on the tumor being considered in the differential diagnosis, CEA, Leu-M1, Ber-Ep4, claudine, B72.3, Bg8, and MOC-31 can be used as negative marker (see Table 21.2) [18,19,20,21,22]. Electron microscopy may help in difficult cases [27].
To date, PM lacks of a grading system. However, histomorphologic parameters can be used to estimate survival. Biphasic/sarcomatoid histology and MCPM/WDPPM have poorer and better prognosis, respectively, than epithelial DMPM. However, the low incidence of biphasic/sarcomatoid and borderline mesotheliomas restricts the clinical utility of this variable.
An exhaustive clinicopathological analysis of 62 patients undergoing comprehensive treatment at the Washington Cancer Institute revealed that nuclear and nucleolar size (rated by a four-tiered score) correlated with survival [28]. Clinical data from our Institution demonstrated that both pathologically involved lymph nodes and inadequate nodal sampling correlate with poor prognosis. Accordingly, careful examination of lymph nodes that drain the visceral and parietal peritoneum is recommended, including bilateral iliac, right gastroepiploic, and ileocolic nodes [22]. Proliferative activity has been reported to be useful for prognostic stratification. It may be quantified either by means of mitotic count or immunohistochemical staining with Ki-67 antigen, an excellent marker of cellular proliferation. Proliferative activity is generally low in PM, but higher rates correlate with poor outcome [7,8,9,10,11].
21.5 Diagnosis of Peritoneal Mesothelioma
DMPM growth is characterized by peritoneal seeding, eventually leading to death due to bowel encasement, obstruction, and intractable ascites. Patients are usually diagnosed at an advanced disease stage.
21.5.1 Clinical Presentation
The initial symptoms of DMPM were prospectively recorded in 51 patients treated at the Washington Cancer Institute [4]. Patients were categorized into three groups: about one-third of them presented with abdominal distention, another one-third with abdominal pain, and the remaining with combined symptoms of distention, pain, and other findings. The investigators designated these three types as a “wet type” presenting with symptoms of malignant ascites causing an increase in abdominal girth, a “dry-painful type” presenting with a focal mass seen at computed tomography (CT) scan usually causing pain, and a “combined type” characterized by both pain and ascites.
In a more recent series of 81 DMPM Italian patients, ascites, abdominal pain, and asthenia were the most frequent symptoms, followed by weight loss, anorexia, abdominal mass, fever, diarrhea, and vomiting; 13% of patients presented with abdominal hernia. Systemic symptoms, such as thrombocytosis and anemia were present in 73% of cases. About 25% of female patients came to medical attention due to non-specific gynecological symptoms [29].
21.5.2 Circulating Tumor Markers
Circulating tumor markers that could be used as an adjunct to clinical and radiological assessment would be valuable tools in the initial evaluation of peritoneal dissemination of unknown origin. Literature data on serum markers of DMPM are scarce. In 2006, our group reported CA125 above normal limits in 53.3% and CA15.3 in 48.5% of 60 patients undergoing CRS/HIPEC. On the contrary, CEA and CA19.9 were mostly normal. Also, serial CA125 measurements paralleled with tumor growth or regression after CRS/HIPEC, and preoperative CA125 showed borderline prognostic significance only among patients not previously treated with sCT [30]. More recently, we have assessed the diagnostic and prognostic role of mesothelin and osteopontin (which are markers currently used in pleural mesothelioma) [31]. Mean mesothelin levels were 7.84 ng/dl (SD = 5.14) in DMPM group and 3.00 ng/dl (SD = 1.25) in control group (p = 0.001). Mean CA19.9 levels were 5.3 ng/dl (SD = 4.7) and 61.96 ng/dl (SD = 112.5) in the two groups (p = 0.008). No statistical difference was seen for osteopontin (p = 0.738), CEA (p = 0.081), CA125 (p = 0.600), and CA15.3 (p = 0.365). The area under the receiver operating characteristic (AUC-ROC) curves was 0.836 for CA19.9, 0.812 for mesothelin, 0.793 for CEA, and lower for CA125 (0.652), osteopontin (0.531), and CA15.3 (0.481). Using diagnostic cut-offs selected by ROC methodology, mesothelin attained 100% specificity and 100% positive predictive value in the differential diagnosis of DMPM and peritoneal disseminations of unknown origin. These data suggest that serum mesothelin, in combination with negative CEA and CA19.9, would be especially useful during the early assessment, in order to shorten the current diagnostic delay of DMPM. Additionally, osteopontin correlated with survival at multivariate analysis (hazard rate 6.46; 95% CI 1.81–23.05; p = 0.004), suggesting that it might be a prognostic marker to select DMPM patients for aggressive treatment approaches.
21.5.3 Imaging Studies
Contrast-enhanced CT scan is currently the preferred diagnostic radiological tools for DMPM. CT features of PM have been defined as “dry” and “wet,” with the dry appearance consisting of peritoneal-based lesions and the wet appearance consisting of ascites, irregular, or nodular peritoneum thickening and an omental mass that may scallop or directly invade adjacent abdominal viscera (see Fig. 21.1) [32, 33]. The two clinical types, wet or dry-painful type, correspond well to these different CT appearances. In the wet type, there is little or no evidence of solid tumor. The CT/radiologic presentation of the dry-painful type may disclose several mass lesions, but often there is a dominant mass isolated to one part of the abdomen.
Yan examined the CT imaging of a series of 33 patients with PM and described the presence of pleural abnormalities in 8 out of 33 patients (24%), 91% of patients having involvement of the greater omentum, 97% of patients having pelvic involvement, and 66% of patients having ascites. This predominant central abdominal and pelvic disease burden observed may be the characteristic pattern of disease presentation [34].
The CT appearance of cystic PM can be a contrast to the CT appearance of DMPM. Despite a severe distortion of the abdominal and pelvic space by fluid-filled cysts and ascites, there is no disruption of intestinal function or segmental bowel obstruction. Small bowel compartmentalization may be seen [34].
CT scan is also useful in patient selection for a comprehensive surgical approach. Thirty-nine CT scan parameters were statistically analyzed to determine their association with the likelihood to perform an adequate surgical cytoreduction (residual lesions ≤ 2.5 cm), that is a predominant prognostic variable. Seven patients (64%) undergoing suboptimal cytoreduction and two patients (11%) undergoing adequate cytoreduction had a tumor mass > 5 cm in the epigastric region (p = 0.004). In 9 patients (82%) of the suboptimal group and 2 (11%) of the adequate cytoreductive surgery group, CT scans showed loss of normal architecture of the small bowel and its mesentery (p < 0.001) (see Fig. 21.2). In a composite analysis, none of the patients with tumor mass >5 cm in the epigastric region and loss of normal architecture of the small bowel and its mesentery had adequate cytoreduction. Patients who lacked these two preoperative CT scan findings had a 94% probability of an adequate cytoreduction [35].
Contrast-enhanced abdominal- pelvic CT scan showing massive disease involvement of the small bowel and its mesentery, with loss of the normal anatomical architecture. This radiological picture is associated with a very low probability to obtain an adequate surgical cytoreduction. This patient is a poor surgical candidate
The role of fluorine-18 fluorodeoxyglucose (18F-FDG)-PET has been recently tested in 9 patients with MCPM and 14 with Epithelioid PM. PET scan showed mild focal uptake in 1 of 8 cases of MCPM, and was positive in 12 of 14 cases of Epithelioid PM. Sensitivity, specificity, and accuracy were 86%, 89%, and 87%, respectively (p = 0.002). Multicystic histology was significantly associated with lower SUV (p = 0.006). SUV was significantly associated with PFS in epithelioid PM (p = 0.028) [36].
21.5.4 Laparoscopy
Esophagogastroduodenoscopy and colonoscopy may exclude a primary gastrointestinal malignancy. A diagnostic laparoscopy is a tool to perform biopsies, especially when there is no tumor deposit amenable to imaging-guided percutaneous biopsy, due to the unfavorable anatomic sites or small volume disseminated disease. Diagnostic laparoscopy can also provide an opportunity to evaluate the peritoneal disease burden and to assess the feasibility of optimal cytoreductive surgery. However, an important caveat accompanies the recommendation for laparoscopy in the diagnosis of PM. In outpatient follow-up, port site recurrence is frequently observed at trocar sites. It is recommended to limit the trocar sites along the linea alba.
In a series of 33 patients with DMPM who underwent CRS/HIPEC, we assessed laparoscopy effectiveness in predicting complete cytoreduction (residual tumor nodules ≤2.5 mm). At preliminary laparoscopy, peritoneal disease was considered amenable for complete CRS in 30 of 33 patients (91%). In this group, cytoreduction was complete in 29 patients and incomplete in one patient. Cytoreduction was grossly incomplete in the remaining three patients who were deemed not amenable for complete CRS. Our data suggest that laparoscopy can integrate clinical and radiological information in the selection process of patients with DMPM for combined treatment [37].
21.6 Treatment of Peritoneal Mesothelioma
Historically, PM has been treated by palliative or debulking surgery. Systemic/intraperitoneal chemotherapy and abdominal irradiation have been used in malignant variants. These treatments were disappointing, resulting in a median survival of about 12 months (Table 21.3). In the last two decades, the approach to PM radically changed with the introduction of a surgical treatment with curative intent. PM remains confined within the peritoneal surfaces of the abdominal cavity for most of its history. Lymph node and extra-abdominal metastases appear to develop later in the course of disease progression. This is the rationale base supporting a comprehensive local-regional approach to treat DMPM with CRS and intraeritoneal administration of chemotherapic drugs including the most commonly used methodology named hyperthermic intraperitoneal chemotherapy (HIPEC) direct targeting the disease, achieving peritoneal disease control, and prolonged disease-free survival. CRS may be seen as a tool to maximize response to intraperitoneal chemotherapy, because the penetration depth in tumor tissue of locally delivered drugs is only 2–3 mm [47]. On the other side, the role of local-regional chemotherapy is to preserve the macroscopically complete surgical response by eradicating microscopic residual disease.
21.6.1 Systemic Therapies
Due to its rarity and inherent difficulties of radiologic assessment, few studies of sCT have been conducted in DMPM. A variety of systemic drugs has been extrapolated from pleural mesothelioma treatment. The most commonly used agents were cisplatin, gemcitabine, doxorubicin, and pemetrexed. Historical Dana-Farber Cancer Institute and Brigham and Women’s Hospital’s series of 180 mesothelioma patients (37 with PM) reported a median survival of 15 months following various palliative sCT [48]. A randomized cancer and leukemia group B (CALGB) trial comparing cisplatin and mitomycin with cisplatin and doxorubicin in 79 patients with pleural or PM reported an overall response rate of 26% with median time-to-failure of 3.6–8.8 months according to different schedules [49]. More recent studies have demonstrated improved outcomes with pemetrexed in combination with cisplatin/carboplatin. In the expanded access program, 109 patients with DMPM were treated with pemetrexed or pemetrexed-containing sCT. Response rates for the combination of cisplatin/carboplatin with pemetrexed appeared to be higher than pemetrexed alone (24.1% versus 12.5%). One-year survival was 57.4% versus 41.5% [50]. Pemetrexed is a multi-targeted antifolate that inhibits thymidylate synthase (TS), dihydrofolate reductase (DHFR), and glycinamide ribonucleotide formyltransferase (GARFT) was approved for use in pleural mesothelioma based on results of a phase III trial [51]. Activity of pemetrexed in PM was observed in two expanded access programs (EAPs) which allowed access to pemetrexed for eligible patients prior to its regulatory approval in pleural mesothelioma, suggesting a role for pemetrexed-based combinations in DMPM [50, 52].
In the international EAP, 109 patients with chemo-naïve or previously treated surgically unresectable DMPM received pemetrexed alone or with cisplatin or carboplatin. Response rate and 1-year survival rate were 18.7 and 47.4%, respectively. Combination chemotherapy was well-tolerated [50]. In the USA EAP, 73 patients with chemo-naïve or previously treated surgically unresectable PM received 6 cycles of pemetrexed alone or combined with cisplatin. Response rates were 26, 19.2, and 29.8% in the overall population, pemetrexed and pemetrexed/cisplatin groups, respectively. Median survival was 13.1 months for patients who received pemetrexed with cisplatin and 8.7 months for pemetrexed alone [52]. In a phase II study, 6 cycles of pemetrexed (500 mg/m2 on day 8) plus gemcitabine (1250 mg/m2 on days 1 and 8) were evaluated in 20 chemo-naïve patients. Response rate was 15%, median time to disease progression was 10.4 months, and median overall survival (OS) was 26.8 months. However, toxicity from this treatment was significant, including one treatment-related death. Grade 3–4 neutropenia and febrile neutropenia were observed in 60 and 10% of patients, respectively [53].
There are isolated reports of the role of whole-abdominal radiation. However, this treatment such a treatment is highly associated with morbidity. Nonetheless a series of patients treated with surgery, HIPEC, and whole abdominal radiation was reported to achieve improved disease-free survival [54].
Limited data are available to guide the use of sCT in combination with CRS/HIPEC in the adjuvant or neoadjuvant setting. Since CRS/HIPEC does not achieve complete cytoreduction in all patients and recurrence is common even after complete cytoreduction [55], sCT is given in combination with intraperitoneal chemotherapy by several groups. We have retrospectively analyzed data from our institutional prospective database regarding 116 DMPMs treated with CRS/HIPEC from 1995 to 2011. Sixty cases had preoperative sCT, 30 had postoperative sCT, and 26 had no sCT. Platinum and pemetrexed were given to 55 cases. Preoperative sCT was not associated with complete cytoreduction or severe morbidity. There was no significant difference in survival among preoperative, postoperative, and no sCT groups, suggesting that operative and long-term outcomes were not influenced by perioperative CT. Only a weak correlation was seen between use of perioperative platinum and pemetrexed and improved survival. However, the potential bias associated with the retrospective study design has to be taken into account [56].
In a recent study, 126 DMPM patients undergoing CRS/HIPEC from 1991 to 2014, at 20 French tertiary centers were divided into four groups: (1) preoperative sCT; (2) postoperative sCT; (3) perioperative (both pre and postoperative sCT; (4) no sCT. At multivariate analysis, preoperative sCT was associated with worse survival (HR = 2.30; 95% CI = 1.07–4.94; p = 0.033), with no impact on treatment toxicity [57]. In summary, sCT with pemetrexed and cisplatin should be considered in patients with surgically unresectable DMPM. Carboplatin may be a reasonable alternative to cisplatin in elderly patients and those with poor performance, given its better safety profile. No conclusive data are available regarding perioperative sCT in patients undergoing CRS/HIPEC.
21.7 Cytoreductive Surgery and Intraperitoneal Chemotherapy
CRS for peritoneal tumors was developed by Sugarbaker who described six peritonectomy procedures to surgically remove all of the peritoneal linings of the abdominopelvic cavity [47]. The loose attachment of parietal peritoneum allows for stripping of the serosal layers by means of bilateral diaphragmatic, anterior abdominal wall, pelvic peritonectomy, and plus omental bursa stripping. Greater and lesser omentectomy are usually performed for both oncologic reasons and to facilitate intra-abdominal drug circulation. Because visceral peritoneum is more intimately attached to underlying structures, tumor implants on visceral surfaces require organ resections, except for liver and pancreatic capsulectomy. Figure 21.3 shows the amount of disease as it can be seen during the early phase of the CRS procedure in a typical case of high-volume DMPM. Figure 21.4 is an intraoperative picture of the same patient showing large disease involving pelvic peritoneum, uterus, sigmoid colon, and both ovaries. Massive disease involving the sub-hepatic/perigastric region is displayed in Fig. 21.5.
Intraoperative picture of the same patient as in Fig. 21.3, showing large disease massively involving the pelvic peritoneum, uterus, sigmoid colon, and both ovaries
The adaptation of the original technique to DMPM is still a challenge, and several modifications have been undertaken. In the next paragraphs, CRS procedures performed in our center are described (see Table 21.4), with a focus on the modifications emerged during a 20-year experience, and a special attention on the most debated issues.
21.7.1 Importance of Complete Cytoreduction
The current literature consistently supports the notion that CRS must be aimed at removing all visible tumors. The completeness of cytoreduction (CCR) is classified at the end of the surgical phase according to Sugarbaker, as CCR-0 (macroscopically complete); CCR-1 (residual disease ≤2.5 mm in any region); CCR-2 (residual disease >2.5 mm and ≤25 mm), and CCR-3 (residual disease >25 mm) [58]. Numerous studies have stratified survival on the basis of this surgical endpoint, and CCR is the major prognostic factor in all PSM [59]. Near complete cytoreduction, leaving behind millimetric residual tumor may be pursued only when complete cytoreduction is not feasible, in order to preserve organ functions postoperatively. We have demonstrated the survival advantage of macroscopically complete cytoreduction, over minimal residual disease in 70 patients with DMPM undergoing CCR-0 or CCR-1 and HIPEC by analyzing clinicopathological factors correlating to disease progression in 13 abdominopelvic regions [55]. Residual tumor ≤ 2.5 mm (versus non-visible tumor) was the only independent risk factor for disease progression in epigastric region (p = 0.047), upper ileum (p = 0.029), upper jejunum (p = 0.034), and lower jejunum (p = 0.002). Before our study, the definition of optimal cytoreduction for DMPM was controversial as other authors suggested that a residual disease up to 25 mm could be adequate. On the contrary, we demonstrated that minimal residual disease, compared with macroscopically complete cytoreduction, correlated to failure in critical anatomical areas, and supporting the need for maximal cytoreductive surgical efforts. The final results of macroscopically complete CRS are shown in Fig. 21.6. The results of complete CRS in the sub-hepatic region and pelvis are shown in Figs. 21.7 and 21.8.
Final results at the end of the surgical cytoreduction. All the macroscopic disease has been completely resected. The entire parietal peritoneum has been removed. Complete peritonectomy of both aspects of the mesentery has been performed, together with radical greater omentectomy and round and falciform liver ligament resection
Sub-hepatic region after macroscopically complete surgical cytoreduction in the same patient as Fig. 21.5. Both the greater and lesser gastric curvature have been made clear of tumor, sparing the blood supply through the left gastric artery. The gall bladder has been removed and the serosal layer covering the hepato-duodenal ligament has been dissected
Complete surgical cytoreduction in the pelvic region. The peritoneum has been surgically removed from the anterior aspect of the bladder, and lateral and posterior pelvic walls. The bladder is suspended to show the sigmoid colon, proximal rectum, and vaginal stump. No sigmoid colon resection has been performed in this case. The peritoneum of the Douglas pouch has been surgically removed. Both ureters, iliac arteries, and veins have been dissected and preserved. Bilateral iliac and obturatory lymphnodes have been removed
21.7.2 Complete Versus Selective Parietal Peritonectomy
Parietal peritonectomy is generally limited to surfaces involved by visible tumor, as well as organ resections, to preserve sufficient postoperative function. We have reported that systematic complete parietal peritonectomy (including both macroscopically involved and normal surfaces) regardless of disease distribution is associated with better survival in DMPM because of its biological characteristics and dissemination pattern with frequent microscopic (not visible) peritoneal disease. In a retrospective matched case-control study, we compared 30 patients with DMPM undergoing selective parietal peritonectomy with 30 matched controls undergoing routine complete parietal peritonectomy. Median overall survival was 29.6 months in the selective peritonectomy group and not reached in the complete peritonectomy group; 5-year overall survival was 40.0% and 63.9%, respectively (p = 0.027). At multivariate analysis, complete versus selective peritonectomy was recognized as an independent prognostic factor, along with complete cytoreduction, negative lymph nodes, epithelial histology, and lower MIB-1 labeling index. Morbidity rates were not different between groups. Furthermore, pathologic examination detected disease involvement on parietal surfaces with no evident tumor at surgical exploration in 12 of 24 patients undergoing complete parietal peritonectomy [60].
21.7.3 Lymph Node Assessment
The importance of nodal sampling and its impact on outcome has been shown to be important in DMPM. In our experience, negative lymph nodes are independent predictor of improved survival, after adjustment for other prognostic variables. In our study, negative nodes, as compared to positive or non-assessed nodes, were associated with increased survival. Since then, we use to perform careful nodal sampling during CRS for DMPM. Although node positivity ultimately bears a poorer outcome and is unlikely to be modified through extended lymphadenectomy, an approach to standardized lymph node sampling would assist in disease staging [22].
21.7.4 Small-Bowel Mesentery Cytoreduction
The involvement of the small-bowel mesentery by neoplastic cells is regulated by factors, such as cell biological aggressiveness and peritoneal features, such as the presence of a relatively low density of lymphatic lacunae, stomata, and milky spots [59]. With low or moderately aggressive malignancies, this typically results in sparing of small bowel surfaces or isolated small tumor implants, that can be locally resected. Conversely, high-grade malignant tumors may massively involve small bowel and its mesentery, thus hampering an adequate cytoreduction. In intermediate-grade tumors, small-to-medium-sized nodules and plaques are observed on the mesentery surface up to the transition line between the mesentery and the small bowel, with minimal deep tissue invasion. In these circumstances, we perform a partial or a complete peritonectomy on both sides of the mesentery. The serosal layer may be stripped up to the limits of bowel wall by either blunt or sharp dissection. It is important to avoid any vascular injury (especially close to the small bowel), as it could result in disruption to the blood supply. This procedure is made easier by finding the space between the serosal layer and the mesenteric fat tissue; it is possible at that time to use the fingers to perform a complete mesenteric peritonectomy by blunt dissection. In our experience, no major surgical complication appeared to be related to the mesenteric peritonectomy, except for a moderate prolongation of postoperative ileus [61]. In Fig. 21.6, the final results of complete parietal peritonectomy with complete mesentery peritonectomy are shown.
21.7.5 Intraperitoneal Perioperative Chemotherapy
Local-regional chemotherapy is performed either as intra-operative hyperthermic intraperitoneal chemotherapy (HIPEC), or normothermic early intraperitoneal chemotherapy (EPIC) [59]. The pharmacological advantage of intraperitoneal administration consists in higher local-regional drug concentration with minimal systemic toxicity. Intra-operative or early postoperative time settings allow optimal distribution of chemotherapeutic agents before the development of postoperative adhesions and tumor cell entrapment in scar tissue, which can contribute to disease recurrence. Additionally, mild hyperthermia (41–43 °C) has a direct cytotoxic effect, increases the efficacy of antiblastic agents, such as mitomycin-C and platinum compounds, as well as their penetration into tumor tissue.
HIPEC techniques vary widely among centers, in terms of closed versus open abdomen technique, drug(s), drug dosage, target temperature, duration, flow rate, type, and volume of carrier solutions. However, no technical variation has demonstrated an advantage in comparative trials. The choice of drugs is based on their clinical efficacy and pharmacokinetics variables, such as hydrophilic properties, high molecular weight to limit passage through the peritoneal-plasma barrier, high plasma clearance, and mechanisms of action potentiated by hyperthermia. Also, only cell cycle phase non-specific agents are indicated for this single-shot treatment. Currently, cisplatin alone or cisplatin in combination with doxorubicin are often used to treat DMPM.
When performing EPIC, the administration of normothermic antiblastic agents is started immediately after surgery using a peritoneal Tenckhoff catheter or a subcutaneous port, and continued for 1–5 days. Generally, 2–4 closed suction drains placed at surgery are maintained closed for 23 h and opened for 1 h a day, to take out the perfusate solution. Drugs with a high rate of hepatic extraction and no significant heat enhancement may be used for EPIC, such as 5-fluoruracil, doxorubicin, or taxanes [61].
A treatment protocol of adjuvant bidirectional chemotherapy with intraperitoneal pemetrexed combined with intravenous cisplatin has been developed at the Washington Cancer Institute. Peritoneal ports are placed at the time of CRS/HIPEC. The treatment consists of pemetrexed 500 mg/m2 given intraperitoneally and cisplatin 50 mg/m2 given intravenously simultaneously on day 1 of every 21-day cycle for 6 cycles. Nine of 10 patients were reported to be able to complete all 6 cycles of therapy without delays or dose modifications. One patient developed a catheter infection after 3 cycles and required catheter removal. He was switched to intravenous pemetrexed and cisplatin for 1 cycle, then a new peritoneal catheter was placed and the remaining 2 cycles were completed. Mild fatigue, nausea, and abdominal pain were observed [62].
21.8 Results of Treatment and Prognostic Factors
Treatment results of DMPM have been reported by a small number of referral centers only in recent years, but this disease has become a classical CRS/HIPEC indication. The most relevant literature series are reported in Table 21.5. Median survival ranged from 30 to 92 months and it appears to improve with growing experience, as the most recent updates report median survival of 4–5 year and more. One French, one American, and one International multi-institutional series have been published, collecting 249, 211, and 405 patients, respectively [68, 69, 73]. The International study was sponsored by the Peritoneal Surface Oncology Group International (PSOGI) and included patients treated in eight centers from 1989 to 2009. Major operative morbidity of 46%, mortality of 2%, median survival of 53 months, and 5-year survival of 47% were reported [68].
We reported operative long-term outcomes for 108 patients treated with complete CRS/HIPEC (post-cytoreductin residual disease ≤2.5 mm). Treatment-related morbidity and mortality were 38.9% and 1.9%, respectively. Median survival was 63.2 months. Interestingly, there were 19 (43.6%) actual survivors of the 39 patients with potential follow-up >7 years, suggesting that patients surviving >7 years may be cured. On multivariate analysis, epithelioid histology and negative lymph node correlated with both overall survival and progression-free survival [11].
Several predictive factors for overall survival in patients with DMPM have been identified. Consistently with the notion that HIPEC penetration depth in residual tumor tissue is only a few millimeters, complete cytoreduction is mandatory for successful treatment [47]. Achievement of CCR-0/1 cytoreduction is highly dependent on the extent of peritoneal disease, involvement of crucial anatomic regions, and tumor aggressiveness [30]. Outcomes from numerous studies have supported this finding: disease stage based on percutaneous coronary interventions (PCI) was identified as a prognostic factor by Yan [74], Schaub et al. created a nomogram to predict survival that was partly based on PCI [75]. Magge found similar finding with lower PCI being predictive of increased survival [71]. Male sex and older age have been also associated with poorer prognosis [69, 71, 76].
Significant pathological and biological prognostic factors reported in the literature are summarized in Table 21.6. One of the most consistent factors is the histological type. Significantly, worse outcomes have been reported for sarcomatoid and biphasic DMPM than the epithelioid subtype [11, 68, 75]. Both Schaub and Alexander further sub-categorized the epithelioid subtype into tumors with significant solid component as a marker for worse outcomes, as compared with epithelioid DMPM with a tubule-papillary pattern [69, 75]. Magge showed that there may be no benefit from CRS-HIPEC in the sarcomatoid and biphasic groups, with a median survival of 10.5 versus 51.5 months for epithelioid DMPM [71]. On the contrary, a recent PSOGI registry study reported better results, with a median survival of 7.8 years in patients with biphasic histology undergoing CCR-0 cytoreduction, thus suggesting that biphasic DMPM should not be considered as an absolute contraindication [78].
The prognostic impact of lymph-node metastases has been reported in both single center and multi-institutional series [11, 68, 74]. Individual studies have also identified mitotic rate [8, 11, 79], GLUT-1 expression [80], preoperative CA-125 [30, 75], telomere maintenance mechanisms [13], estrogen receptors [81], BCL2 [77], MUC-1 [82], BAP1, NF2, CDKN2A [83], PD-L1 [80], and preoperative thrombocytosis [84] as predictors of survival.
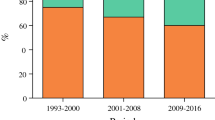
We recently developed an algorithm by means of conditional inference tree model [9]. This model relies on pre-cytoreduction PCI and tumor proliferative index measured by Ki-67 using immunohistochemistry. Three prognostic subsets were defined: (I) Ki-67 ≤ 9%; (II) Ki-67 > 9% and PCI 17; and (III) Ki-67 > 9% and PCI > 17. The median OS for subsets I, II, and III were, 86.6, 63.2, and 10.3 months, respectively. The model had an acceptable discriminant capacity with a bootstrap-corrected Harrell c-index of 0.74 (see Fig. 21.9).
21.8.1 Low-Grade Peritoneal Mesotelioma
MCPM and WDPM are rare variants of mesothelioma. In a few centers, these disease entities have been treated by CRS/HIPEC due to their tendencies to give multiple local-regional recurrences and reported potential to evolve into truly malignant DMPM. In 2007, we reported a series of four women with MPM and eight with WDPPM undergoing cytoreduction and close-abdomen HIPEC with cisplatin and doxorubicin. Seven of them were treated for recurrent disease after previous debulking. After a median follow-up of 27 months (range 6–94), 5-year overall and progression-free survival were 90.0% and 79.7%, respectively. Transition of typical WDPPM to malignant biphasic mesothelioma was documented in one patient who died of disease progression following incomplete cytoreduction and HIPEC. We were able to calculate median progression-free survival of 24 months (range 2–87) following previous debulking surgery in 7 patients (one operation in five patients, two operations in one, and four operations in one), that was statistically worse than the corresponding figure after CRS/HIPEC in the same patients (p = 0.0156) [24].
Outcomes of MPM were also studied as a subgroup analysis from the PSOGI registry. There were 26 patients (6.4%) with a large preponderance of females (n = 20). Following a median follow up of 54 months (range 5–129), all patients treated were alive and free of disease [85]. In our most recent institutional update, we reviewed 19 patients with MCPM who underwent 20 CRS/HIPEC procedures in our center between August 1997 and October 2017. The majority of the patients were females (n = 17, 89%), and mean age was 42. Mean PCI was 15.5 ± 9.9 and total number of procedures performed 6.7 ± 2.6. Major complications occurred in 3 (15%) patients, with no perioperative mortality. After a median of follow-up of 69 months (range 4–220) all patients were alive and four patients had recurrence (21%). Patients with high PCI (defined by median PCI) had shorter recurrence-free survival (106.4 ± 6.6 months versus 125.6 ± 34.1; p = 0.03) [86].
21.8.2 Staging of Peritoneal Mesothelioma
No staging system exists for DMPM, because of its rarity and unique clinical presentation with diffuse disease dissemination throughout the peritoneum, and no primary lesion. As a curative-intent treatment has become available, the international PSOGI registry collecting 292 DMPM patients undergoing CRS/HIPEC has been used to formulate a new tumor-node-metastasis (TNM) staging system [74].
Yan assessed tumor (T) category according to the extent of peritoneal involvement, as scored intraoperatively by PCI. PCI was categorized into T1 (PCI 1–10), T2 (PCI 11–20), T3 (PCI 21–30), and T4 (PCI 30–39). Node (N) and metastasis (M) factors were defined according to the presence versus absence of positive intra-abdominal lymph nodes and hepatic or extra-abdominal involvement. The T1, N0, M0 defined stage 1. T2-3, N0, M0 defined stage 2. T4, N0, M0, and N1 or M1 with any T, defined stage 3. Five-year survival associated with stage I, II, and III was 87, 53, and 29%, respectively. The proposed TNM staging was associated with survival in the multivariate analysis, together with histological subtype, and complete cytoreduction.
Based on the evidence that prognosis of DMPM is predominantly dependent on pathological and biological features, such as histological subtype and proliferative activity, we hypothesized that the prognostic stratification of the recently proposed TNM could be improved by the incorporation of a pathological grading system. We defined pathological grading as follows:
-
Grade 1: mitotic count (MC) ≤ 5/10 high power fields (HPF), or Ki-67 index ≤ 5% (percentage of positive cells among 2000 tumor cells).
-
Grade 2: MC 5–25/10 HPF or Ki-67 index > 5%.
-
Grade 3: MC > 25/10 HPF or Ki-67 index > 25% or presence of any spindle cell component.
Stage grouping was revised as follows: T1-3, N0, M0, G1 defined stage I; T4, N0, M0, G1, or T1-3, N0, M0, G2 defined stage II. Stage III was defined by any of the following: (1) G3; (2) N1; (3) M1; (4) T4, N0, M0, G2.
For stage I, median overall survival was not reached (71.6% at 5-year). For stage II and III, median survival was 39.5 months (95% CI = 34.6–44.4) and 12.6 months (95% CI = 6.8–18.5), respectively. In a Cox multivariable model, modified TNM (hazard ratio (HR) = 2.3, 95% CI = 1.7–3.3; p < 0.001), completeness of cytoreduction (HR = 2.0; 95% CI = 1.4–2.9; p < 0.001), and major complications (HR = 1.7; 95% CI = 1.1–2.8; p = 0.030) independently correlated with survival. The previously proposed TNM was not significant (p = 0.507) [87].
By means of 25 demographic, laboratory, operative, and histopathological variables, Schaub developed a nomogram using machine-learned Bayesian belief networks with stepwise training, testing, and cross-validation to predict prognosis of DMPM patients who underwent CRS/HIPEC. Among 104 patients treated at the National Cancer Institute/NIH, Bethesda, MD, mean PCI was 15, 66% of patients had a CCR-0/1 cytoreduction, and 87% of patients had epithelioid histology. Median follow-up was 49 months (1–195), and 3- and 5-year survival rates were 58 and 46%, respectively. Histological subtype, PCI, and preoperative serum CA-125 had the greatest impact on survival and were included in the nomogram. The mean areas under the ROC curve for the ten-fold cross-validation of the 3- and 5-year models were 0.77 and 0.74, respectively. This nomogram may potentially individualize patient care and prevent CRS in patients unlikely to achieve favorable outcomes [75].
21.9 Conclusion
Even in the absence of controlled data, the current evidence suggests that the comprehensive approach of CRS/HIPEC is now the benchmark against which other treatments have to be evaluated. The optimization of several important clinical issues is still ongoing, including patient selection for treatment, adaptation of CRS techniques to this peculiar disease, and role of integrated systemic and local-regional therapies in the individual patients. CRS/HIPEC and sCT should be applied according to histology, tumor biology, disease stage, and patient condition as follows:
-
CRS/HIPEC is recommended for low-grade PM (WDPM and MCPM) with no need of further treatment.
-
Patients with not resectable or metastatic DMPM, and/or poor general status not allowing major abdominal surgery, should be considered for sCT.
-
Patients with DMPM confined to the peritoneum and not fit for major abdominal surgery or with disease not fully resectable or resectable with extensive surgery conditioning higher risk of postoperative morbidity should be proposed for neoadjuvant sCT. In these patients, CRS/HIPEC should be considered after sCT in case of important response.
-
Patients with DMPM confined to the peritoneum fit for major abdominal surgery, and with disease amenable to complete resection. This is the group of patients in whom CRS HIPEC is indicated as first-line treatment.
We believe that the rarity of this disease entity and complexity of its treatment approaches would make it necessary to be treated these patients in highly qualified referral centers. Novel systemic combination chemotherapy warrants further assessments as an adjunct to intraperitoneally delivered drugs. Basic science research is rapidly evolving and future developments may come from integrating innovative molecular and cellular approaches into comprehensive treatment strategies.
References
Robinson BWS, Lake RA. Advanced in malignant mesothelioma. N Engl J Med. 2005;353:1591–603.
Conti S, Minelli G, Ascoli V, Marinaccio A, Bonafede M, Manno V, Crialesi R, Straif K. Peritoneal mesothelioma in Italy: trends and geography of mortality and incidence. Am J Ind Med. 2015;58:1050–8.
Boffetta P. Epidemiology of peritoneal mesothelioma: a review. Ann Oncol. 2007;18:985–90.
Sugarbaker PH, Welch LS, Mohamed F, Glehen O. A review of peritoneal mesothelioma at the Washington Cancer Institute. Surg Oncol Clin N Am. 2003;12:605–21.
Gazdar AF, Carbone M. Molecular pathogenesis of mesotheliom and its relationship to Simian virus 40. Clin Lung Cancer. 2003;5:177–81.
Roushdy-Hammady I, Siegel J, Emri S, et al. Genetic-susceptibility factor and malignant mesothelioma in the Cappadocian region of Turkey. Lancet. 2001;357:444–5.
Nonaka D, Kusamura S, Baratti D, et al. Diffuse malignant mesothelioma of the peritoneum: a clinicopathological study of 35 patients treated locoregionally at a single institution. Cancer. 2005;104:2181–8.
Borczuk AC, Taub RN, Hesdorffer M, et al. P16 loss and mitotic activity predict poor survival in patients with peritoneal malignant mesothelioma. Clin Cancer Res. 2005;11:3303–8.
Kusamura S, Torres Mesa PA, Cabras A, Baratti D, Deraco M. The role of Ki-67 and pre-cytoreduction parameters in selecting diffuse malignant peritoneal mesothelioma (DMPM) patients for Cytoreductive surgery (CRS) and Hyperthermic Intraperitoneal Chemotherapy (HIPEC). Ann Surg Oncol. 2016;23:1468–73.
Deraco M, Cabras A, Baratti D, Kusamura S. Immunohistochemical evaluation of Minichromosome maintenance protein 7 (MCM7), topoisomerase IIα, and Ki-67 in diffuse malignant peritoneal mesothelioma patients using tissue microarray. Ann Surg Oncol. 2015;22:4344–51.
Baratti D, Kusamura S, Cabras AD, Bertulli R, Hutanu I, Deraco M. Diffuse malignant peritoneal mesothelioma: long-term survival with complete cytoreductive surgery followed by hyperthermic intraperitoneal chemotherapy (HIPEC). Eur J Cancer. 2013;49:3140–8. 8A.L.
Feldman AL, Libutti SK, Pingpank JF, et al. Analysis of factors associated with outcome in patients with malignant peritoneal mesothelioma undergoing surgical debulking and intraperitoneal chemotherapy. J Clin Oncol. 2003;21:4560–7.
Villa R, Daidone MG, Motta R, Venturini L, De Marco C, Vannelli A, Kusamura S, Baratti D, Deraco M, Costa A, Reddel RR, Zaffaroni N. Multiple mechanisms of telomere maintenance exist and differentially affect clinical outcome in diffuse malignant peritoneal mesothelioma. Clin Cancer Res. 2008;14:4134–40.
Zaffaroni N, Costa A, Pennati M, De Marco C, Affini E, Madeo M, Erdas R, Cabras A, Kusamura S, Baratti D, Deraco M, Daidone MG. Survivin is highly expressed and promotes cell survival in malignant peritoneal mesothelioma. Cell Oncol. 2007;29:453–66.
De Cesare M, Sfondrini L, Pennati M, De Marco C, Motta V, Tagliabue E, Dera M, Balsari A, Zaffaroni N. CpG-oligodeoxynucleotides exert remarkable antitumor activity against diffuse malignant peritoneal mesothelioma orthotopic xenografts. J Transl Med. 2016;14:25.
Perrone F, Jocollè G, Pennati M, Deraco M, Baratti D, Brich S, Orsenigo M, Tarantino E, De Marco C, Bertan C, Cabras A, Bertulli R, Pierotti MA, Zaffaroni N, Pilotti S. Receptor tyrosine kinase and downstream signalling analysis in diffuse malignant peritoneal mesothelioma. Eur J Cancer. 2010;46:2837–48.
Churg A, Roggli VL, Galateau-Salle F, et al. Tumours of the pleura: Mesothelial tumours. In: Travis WD, Brambilla E, Harris CC, Muller-Hermelink HK, editors. Pathology and genetics of tumours of the lung, pleura, thymus and heart. Lyon: IARC Press; 2004.
Husain AN, Colby TV, Ordóñez NG, et al. Guidelines for pathologic diagnosis of malignant mesothelioma: 2017 update of the consensus statement from the international mesothelioma interest group. Arch Pathol Lab Med. 2018;142:89–108.
Battifora H, McCaughey WTE. Tumours and pseudotumours of the serosal membranes. In: Atlas of tumour pathology 3rd series, fascicle 15. Washington, DC: Armed Forces Institute of Pathology; 1995. p. 15–88.
Roggli VL, Cagle PT. Pleura, pericardium and peritoneum. In: Silverberg SG, DeLellis RA, Frable WJ, LiVolsi VA, Wick MR, editors. Silverberg’s principles and practice of surgical pathology. 4th ed. New York: Churchill-Livingstone/Elsevier; 2006. p. 1005–39.
Attanoos RL, Gibbs AR. Pathology of malignant mesothelioma. Histopathology. 1997;30:403–18.
Baratti D, Kusamura S, Cabras AD, Laterza B, Balestra MR, Deraco M. Lymph node metastases in diffuse malignant peritoneal mesothelioma. Ann Surg Oncol. 2010;17:45–53.
Butnor KJ, Sporn TA, Hammar SP, Roggli VL. Well-differentiated papillary mesothelioma. Am J Surg Pathol. 2001;25:1304–9.
Baratti D, Kusamura S, Nonaka D, Oliva GD, Laterza B, Deraco M. Multicystic and well-differentiated papillary peritoneal mesothelioma treated by surgical cytoreduction and hyperthermic intra-peritoneal chemotherapy (HIPEC). Ann Surg Oncol. 2007;14:2790–7.
Churg A, Colby TV, Cagle P. The separation of benign and malignant mesothelial proliferations. Am J Surg Pathol. 2000;24:1183–200.
Attanoos RL, Griffin A, Gibbs AR. The use of immunohistochemistry in distinguishing reactive from neoplastic mesothelium: a novel use for desmin and comparative evaluation with epithelial membrane antigen, p53, platelet-derived growth factor-receptor, P-glycoprotein and Bcl-2. Histopathology. 2003;43:231–8.
Ordonez NG. Immunohistochemical diagnosis of epithelioid mesothelioma: an update. Arch Pathol Lab Med. 2005;129:1407–14.
Cerruto CA, Brun EA, Chang D, Sugarbaker PH. Prognostic significance of histomorphologic parameters in diffuse malignant peritoneal mesothelioma. Arch Pathol Lab Med. 2006;130:1654–61.
de Pangher V, Recchia L, Cafferata M, et al. Malignant peritoneal mesothelioma: a multicenter study on 81 cases. Ann Oncol. 2010;21:348–53.
Baratti D, Kusamura S, Martinetti A, Seregni E, Oliva DG, Laterza B, Deraco M. Circulating CA125 in patients with peritoneal mesothelioma treated with cytoreductive surgery and intraperitoneal hyperthermic perfusion. Ann Surg Oncol. 2007;14:500–8.
Bruno F, Baratti D, Martinetti A, Morelli D, Sottotetti E, Bonini C, Guaglio M, Kusamura S, Deraco M. Mesothelin and osteopontin as circulating markers of diffuse malignant peritoneal mesothelioma: a preliminary study. Eur J Surg Oncol. 2018;44:792–8.
Park JY, Kim KW, Kwon HJ, et al. Peritoneal mesotheliomas: clinicopathologic features, CT findings, and differential diagnosis. Am J Roentgenol. 2008;191:814–25.
Whitley N, Brenner D, Antman K, Grant D, Aisner J. CT of peritoneal mesothelioma: analysis of eight cases. Am J Roentgenol. 1982;138:531–5.
Yan TD, Haveric N, Carmignani CP, Bromley CM, Sugarbaker PH. Computed tomographic characterization of malignant peritoneal mesothelioma. Tumori. 2005;91:394–400.
Yan TD, Haveric N, Carmignani CP, Chang D, Sugarbaker PH. Abdominal computed tomography scans in the selection of patients with malignant peritoneal mesothelioma for comprehensive treatment with cytoreductive surgery and perioperative intraperitoneal chemotherapy. Cancer. 2005;103:839–49.
Dubreuil J, Giammarile F, Rousset P, et al. The role of 18F-FDG-PET/ceCT in peritoneal mesothelioma. Nucl Med Commun. 2017;38:312–8.
Laterza B, Kusamura S, Baratti D, Oliva GD, Deraco M. Role of explorative laparoscopy to evaluate optimal candidates for cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (HIPEC) in patients with peritoneal mesothelioma. In Vivo. 2009;23:187–90.
Rogoff EE, Hilaris B, Huvos AG. Long-term survival in patients with malignant peritoneal mesothelioma treated with irradiation. Cancer. 1973;32:656–64.
Jones DEC, Silver D. Peritoneal mesothelioma. Surgery. 1979;86:556–60.
Chahinian AP, Pajak TF, Holland JF, et al. Diffuse malignant mesothelioma. Prospective evaluation of 69 patients. Ann Intern Med. 1982;96:746–55.
Antman KH, Osteen R, Klegar K, et al. Early peritoneal mesothelioma: a treatable malignancy. Lancet. 1985;2:977–81.
Kirmani S, Cleary SM, Mowry J, et al. Intracavitary cisplatin for malignant mesothelioma: an update. In: Proc Am Clin Oncol, vol. 7, 1988. (Abstract 1057).
van Gelder T, Hoogsteden HC, Versnel MA, et al. Malignant peritoneal mesothelioma: a series of 19 cases. Digestion. 1989;43:222–7.
Markman M, Kelsen D. Efficacy of cisplatin-based intraperitoneal chemotherapy as treatment of malignant peritoneal mesothelioma. J Cancer Res Clin Oncol. 1992;118:547–50.
Neumann V, Muller KM, Fischer M. Peritoneal mesothelioma-incidence and aetiology. Pathologe. 1999;20:169–76.
Eltabbakh GH, Piver MS, Hempling RE, et al. Clinical picture, response to therapy, and survival of women with diffuse malignant peritoneal mesothelioma. J Surg Oncol. 1999;70:6–12.
Sugarbaker PH. Peritonectomy procedures. Ann Surg. 1995;221:29–42.
Antman K, Shemin R, Ryan L, et al. Malignant mesothelioma: prognostic variables in a registry of 180 patients, the Dana-Farber Cancer Institute and Brigham and Women’s Hospital experience over two decades, 1965-1985. J Clin Oncol. 1988;6:147–53.
Chahinian AP, Antman K, Goutsou M, et al. Randomized phase II trial of cisplatin with mitomycin or doxorubicin for malignant mesothelioma by the cancer and Leukemia group B. J Clin Oncol. 1993;11:1559–65.
Carteni G, Manegold C, Garcia GM, et al. Malignant peritoneal mesothelioma - results from the international expanded access program using pemetrexed alone or in combination with a platinum agent. Lung Cancer. 2009;64:211–8.
Vogelzang NJ, Rusthoven JJ, Symanowski J, et al. Phase III study of pemetrexed in combination with cisplatin versus cisplatin alone in patients with malignant pleural mesothelioma. J Clin Oncol. 2003;21:2636–44.
Jänne PA, Wozniak AJ, Belani CP, et al. Open-label study of pemetrexed alone or in combination with cisplatin for the treatment of patients with peritoneal mesothelioma: outcomes of an expanded access program. Clin Lung Cancer. 2005;7:40–6.
Simon GR, Verschraegen CF, Jänne PA, Langer CJ, Dowlati A, Gadgeel SM, et al. Pemetrexed plus gemcitabine as first-line chemotherapy for patients with peritoneal mesothelioma: final report of a phase II trial. J Clin Oncol. 2008;26:3567–72.
Hesdorffer ME, Chabot JA, Keohan ML, et al. Combined resection, intraperitoneal chemotherapy, and whole abdominal radiation for the treatment of malignant peritoneal mesothelioma. Am J Clin Oncol. 2008;31:49–54.
Baratti D, Kusamura S, Cabras AD, Dileo P, Laterza B, Deraco M. Diffuse malignant peritoneal mesothelioma: failure analysis following cytoreduction and hyperthermic intraperitoneal chemotherapy (HIPEC). Ann Surg Oncol. 2009;16:463–72.
Deraco M, Baratti D, Hutanu I, Bertuli R, Kusamura S. The role of perioperative systemic chemotherapy in diffuse malignant peritoneal mesothelioma patients treated with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Ann Surg Oncol. 2013;20:1093–100.
Kepenekian V, Elias D, Passot G, et al. Diffuse malignant peritoneal mesothelioma: evaluation of systemic chemotherapy with comprehensive treatment through the RENAPE database: multi-institutional retrospective study. Eur J Cancer. 2016;65:69–79.
Jaquet P, Sugarbaker PH. Current methodologies for clinical assessment of patients with peritoneal carcinomatosis. J Exp Clin Cancer Res. 1996;15:49–58.
Baratti D, Kusamura S, Guaglio M, Deraco M. Peritoneal metastases: challenges for the surgeon. Minerva Chir. 2015;70:195–215.
Baratti D, Kusamura S, Cabras AD, Deraco M. Cytoreductive surgery with selective versus complete parietal peritonectomy followed by hyperthermic intraperitoneal chemotherapy in patients with diffuse malignant peritoneal mesothelioma: a controlled study. Ann Surg Oncol. 2012;19:1416–24.
Deraco M, Baratti D, Kusamura S, Laterza B, Balestra MR. Surgical technique of parietal and visceral peritonectomy for peritoneal surface malignancies. J Surg Oncol. 2009;100:321–8.
Bijelic L, Stuart OA, Sugarbaker PH. Adjuvant bidirectional chemotherapy with intraperitoneal pemetrexed combined with intravenous cisplatin for diffuse malignant peritoneal mesothelioma. Gastroenterol Res Pract. 2012;2012:1–6. Article ID 890450.
Blackham AU, Shen P, Stewart JH, et al. Cytoreductive surgery with intraperitoneal hyperthermic chemotherapy for malignant peritoneal mesothelioma: mitomycin versus cisplatin. Ann Surg Oncol. 2010;17:1720–7.
Robella M, Vaira M, Mellano A, et al. Treatment of diffuse malignant peritoneal mesothelioma (DMPM) by cytoreductive surgery and HIPEC. Minerva Chir. 2014;69:9–15.
Elias D, Bedard V, Bouzid T, et al. Malignant peritoneal mesothelioma: treatment with maximal cytoreductive surgery plus intraperitoneal chemotherapy. Gastroenterol Clin Biol. 2007;31:784–8.
Chua TC, Yan TD, Morris DL. Outcomes of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for peritoneal mesothelioma: the Australian experience. J Surg Oncol. 2009;99:109–13.
Gilani SNS, Mehta A, Garcia-Fadrique A, et al. Outcomes of cytoreductive surgery with hyperthermic intraperitoneal chemotherapy for peritoneal mesothelioma and predictors of survival. Int J Hyperth. 2018;34:578–84.
Yan TD, Deraco M, Baratti D, et al. Cytoreductive surgery combined with hyperthermic intraperitoneal chemotherapy for peritoneal mesothelioma—a multi-institutional registry study. J Clin Oncol. 2009;27:6237–42.
Alexander HR Jr, Bartlett DL, Pingpank JF, et al. Treatment factors associated with long-term survival after cytoreductive surgery and regional chemotherapy for patients with malignant peritoneal mesothelioma. Surgery. 2013;153:779–86.
Hommell-Fontaine J, Isaac S, Passot G, et al. Malignant peritoneal mesothelioma treated by cytoreductive surgery and hyperthermic intraperitoneal chemotherapy: is GLUT1 expression a major prognostic factor? A preliminary study. Ann Surg Oncol. 2013;20:3892–8.
Magge D, Zenati MS, Austin F, et al. Malignant peritoneal mesothelioma: prognostic factors and oncologic outcome analysis. Ann Surg Oncol. 2014;21:1159–65.
Ihemelandu C, Bijelic L, Sugarbaker PH. Iterative cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for recurrent or progressive diffuse malignant peritoneal mesothelioma: clinicopathologic characteristics and survival outcome. Ann Surg Oncol. 2015;22:1680–5.
Malgras B, Gayat E, Aoun O, et al. Impact of combination chemotherapy in peritoneal mesothelioma Hyperthermic Intraperitoneal chemotherapy (HIPEC): the RENAPE study. Ann Surg Oncol. 2018;25:3271–9.
Yan TD, Deraco M, Elias D, Glehen O, Levine EA, Moran BJ, Morris DL, Chua TC, Piso P, Sugarbaker PH, Peritoneal Surface Oncology Group. A novel tumor-node-metastasis (TNM) staging system of diffuse malignant peritoneal mesothelioma using outcome analysis of a multi-institutional database. Cancer. 2011;117:1855–63.
Schaub NP, Alimchandani M, Quezado M, et al. A novel nomogram for peritoneal mesothelioma predicts survival. Ann Surg Oncol. 2013;20:555–61.
Cao C, Yan TD, Deraco M, Elias D, Glehen O, Levine EA, Moran BJ, Morris DL, Chua TC, Piso P, Sugarbaker PH, Peritoneal Surface Malignancy Group. Importance of gender in diffuse malignant peritoneal mesothelioma. Ann Oncol. 2012;23:1494–8.
Pillai K, Pourgholami MH, Chua TC, Morris DL. Ki67-BCL2 index in prognosis of malignant peritoneal mesothelioma. Am J Cancer Res. 2013;3:411–23.
Votanopoulos KI, Sugarbaker P, Deraco M, et al. Is cytoreductive surgery with hyperthermic intraperitoneal chemotherapy justified for biphasic variants of peritoneal mesothelioma? Outcomes from the peritoneal surface oncology group international registry. Ann Surg Oncol. 2018;25:667–73.
Krasinskas AM, Borczuk AC, Hartman DJ, et al. Prognostic significance of morphological growth patterns and mitotic index of epithelioid malignant peritoneal mesothelioma. Histopathology. 2016;68:729–37.
Valmary-Degano S, Colpart P, Villeneuve L, et al. Immunohistochemical evaluation of two antibodies against PD-L1 and prognostic significance of PD-L1 expression in epithelioid peritoneal malignant mesothelioma: a RENAPE study. Eur J Surg Oncol. 2017;43:1915–23.
Huang Y, Alzahrani NA, Liauw W, Morris DL. Effects of sex hormones on survival of peritoneal mesothelioma. World J Surg Oncol. 2015;13:210.
Pillai K, Pourgholami MH, Chua TC, Morris DL. MUC1 has prognostic significance in malignant peritoneal mesothelioma. Int J Biol Markers. 2013;28:303–12.
Singhi AD, Krasinskas AM, Choudry HA, et al. The prognostic significance of BAP1, NF2, and CDKN2A in malignant peritoneal mesothelioma. Mod Pathol. 2016;29:14–24.
Li YC, Khashab T, Terhune J, et al. Preoperative thrombocytosis predicts shortened survival in patients with malignant peritoneal mesothelioma undergoing operative Cytoreduction and Hyperthermic Intraperitoneal chemotherapy. Ann Surg Oncol. 2017;24:2259–65.
Chua TC, Yan TD, Deraco M, Glehen O, Moran BJ, Sugarbaker PH. Multi-institutional experience of diffuse intra-abdominal multicystic peritoneal mesothelioma. Br J Surg. 2011;98:60–4.
Nizri E, Baratti D, Guaglio M, et al. Multicystic mesothelioma: operative and long-term outcomes with cytoreductive surgery and hyperthermic intra peritoneal chemotherapy. Eur J Surg Oncol. 2018;44:1100–4.
Baratti D, Kusamura S, Cabras AD, et al. Diffuse malignant peritoneal mesothelioma: incorporation of a simple pathological grading into recently proposed TNM classification improbe out come prediction. In: 9th International Congress on peritoneal Surface malignancies. Amsterdam, ND. 9-11 October 2014.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Deraco, M., Kusamura, S., Guaglio, M., Cabras, A., Nizri, E., Baratti, D. (2019). Peritoneal Mesothelioma: Diagnosis and Management. In: Ceresoli, G., Bombardieri, E., D'Incalci, M. (eds) Mesothelioma. Springer, Cham. https://doi.org/10.1007/978-3-030-16884-1_21
Download citation
DOI: https://doi.org/10.1007/978-3-030-16884-1_21
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-16883-4
Online ISBN: 978-3-030-16884-1
eBook Packages: MedicineMedicine (R0)