Abstract
Malignant Pleural Mesothelioma (MPM) is an aggressive disease characterized by chemoresistance and few therapeutic options. First-line platinum-pemetrexed chemotherapy represents the current standard of care, and no indication is available for second-line treatments. So far, no targeted therapies proved to significantly impact the natural history of this neoplasm, thus reinforcing the need for new targets and drugs in MPM. In this chapter, we will focus on targeted therapy against molecular mechanisms implied in MPM carcinogenesis, progression, and apoptosis resistance. We will describe clinical trials testing the efficacy of biological agents targeting tyrosine kinase receptors signaling, PI3K-AKT-mTOR and FAK pathways, cell cycle regulation, and apoptosis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
17.1 Introduction
Malignant Pleural Mesothelioma (MPM) is fatal disease characterized by chemoresistance and poor prognosis [1]. Since 2003, when a platinum-based chemotherapy plus pemetrexed was introduced as standard first-line therapy [2], no significant improvements in MPM management have been done. To date, no indications for second-line therapies after first-line failure are available [3]. In the last years, many efforts have been directed to the identification of anticancer therapies able to target tumor-related molecular changes. Targeted therapies may improve cancer management in terms of both patients’ prognosis and quality of life, because of the higher specificity and the lower toxicity profile compared to most cytotoxic drugs. The identification of key molecular targets in MPM represents a hard challenge because MPM pathogenesis is not completely known. This neoplasia is characterized by low mutational load, but recurrent somatic mutations in tumor suppressor genes [4]. Moreover, the three histologic subtypes are characterized by different biological and clinical behaviors, increasing the need to develop personalized therapeutic approaches. Here, we focus on potential molecular targets and specific targeted therapies under clinical investigation in MPM.
17.1.1 NF2/Merlin
NF2 is a tumor suppressor gene frequently altered in MPM [5,6,7]. Recent studies performed in a large series of MPM specimens using high-throughput technologies (whole-exome sequencing, RNA-seq) confirmed high frequency of NF2 alteration including mutations and copy number variations [8,9,10]. Of note, sarcomatoid subtypes carried higher rate of NF2 mutation compared to epithelioid ones [9].
NF2 gene encodes for merlin protein, a tumor suppressor blocking several signal transduction pathways involved in cell proliferation, survival, and metabolism. Wild-type merlin is regulated by post-translational modifications defining its conformational status and activity. It is inactivated through the phosphorylation at Serine 518 by cAMP-dependent kinase (PKA) and activated by the myosin phosphatase MYPT1-PP1 [11]. As a consequence, deregulation of merlin can occur in the absence of NF2 gene mutation [12]. Indeed, mRNA overexpression of CPI-17 (phosphatase inhibitor of 17 kDa), a cellular inhibitor of MYPT1-PP1, has been detected in mesothelioma tumor samples carried wild-type NF2, suggesting that merlin is completely inactivated in MPM [13].
17.1.1.1 NF2/Merlin and Hippo Pathway
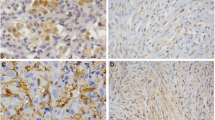
Merlin controls cell proliferation and viability through the regulation of the Hippo pathway, a signal transduction cascade including the proteins: MST1/2 Kinases (Mammalian STE20-like protein kinase 1/2), MST1/2 coactivator SAV1(Salvador1), LATS1/2 Kinases (Large Tumor Suppressor Kinases 1/2), and LATS1/2 coactivator MOB1 (Mps one-binder l) [14]. Merlin-dependent activation of the Hippo pathway results in the phosphorylation and inactivation of YAP (Yes associated protein), a cofactor essential for TEAD (TEA domain family member) transcriptional activity. YAP/TEAD complex activates the transcription of genes involved in cell proliferation, cell growth, and inhibition of apoptosis [15] (Fig. 17.1). In MPM, Hippo pathway deregulation seems to be related mainly to merlin loss of function [16, 17], although concomitant mutations of NF2 and LATS2 genes have been reported [9, 18]. Immunohistochemistry analysis performed on MPM cell lines and tumor tissues revealed strong nuclear localization of YAP in a high percentage of samples [16, 19, 20] and YAP knockdown in MPM cells resulted in the inhibition of cell growth, motility, and invasive abilities [21]. Altogether, these observations highlight the strong link existing between YAP hyper-activation and MPM uncontrolled growth, suggesting that YAP may be a potential candidate for MPM-targeted therapies. A drug screening performed using the Johns Hopkins library identified the small-molecule Verteporfin (VP) (Visudyne, Novartis) as a YAP inhibitor [22]. VP is an FDA (Food and Drug Administration)-approved photosensitizer drug used for the treatment of neovascular macular degeneration. In addition to its photosensitizer properties, VP has light-independent ability in inducing YAP conformational change and in blocking YAP/TEAD interaction [23]. The potential of VP as anticancer drug is under investigation in phase I/II clinical trials in different human cancers, including breast and pancreatic cancers, brain tumors, and pleural malignancies (www.clinicaltrials.gov, NCT02939274, NCT03067051, NCT00002647; NCT02702700). As regard MPM, encouraging results have been obtained in in vitro studies demonstrating VP-dependent reduction of cell proliferation, cell viability, and cell invasion in MPM cell lines [18, 20].
Merlin regulates Hippo pathway activation. Merlin blocks TEAD transcriptional activity (left panel): following growth arrest signals, merlin recruits LATS1/2 and MOB1 in the cytoplasm at the membrane level. MST1/2 phosphorylates LATS1/2 and MOB1 activating LATS1/2 that, in turn, phosphorylates YAP; phospho-YAP binds 14-3-3 and is retained into the cytoplasm. Into the nucleus, merlin inhibits CRL4 DCAF1, the E3 ubiquitin ligase implied in LATS1/2 degradation. Loss of merlin (right panel) results in YAP/TEAD association and activation of transcription. Verteporfin induces YAP conformational change inhibiting YAP/TEAD interaction. LATS Large Tumor Suppressor Kinases 1/2, MOB Mps one-binder l, MST 1/2 Mammalian STE20-like protein kinase1/2, SAV salvador, YAP Yes-associated protein, TEAD TEA domain family member, CRL4 cullin4A-RING E3 ubiquitin ligase, DCAF1 DDB1- and CUL4-associated factor1, VP Verteporfin
17.1.1.2 NF2/Merlin and mTOR Pathway
PI3K-AKT-mTOR is a signal transduction pathway involved in cell proliferation, protein synthesis, glucose metabolism, apoptosis resistance, angiogenesis, and invasion. Activation of PI3K-AKT-mTOR passes through RTKs (Tyrosine Kinase Receptors) activation or G-Protein Coupled Receptors (GPCRs)-dependent RAS induction [24]. mTOR (mammalian target of rapamycin) is a serine/threonine kinase included in two protein complexes: the rapamycin-sensitive mTORC1 (mammalian target of rapamycin complex 1) and the rapamycin-insensitive mTORC2. mTORC1 induces mRNA translation, protein synthesis, and nucleotide production and negatively regulates autophagy and mTORC2 [25]; mTORC2 regulates protein kinases activity including AKT [26]. Physiological inhibitors of PI3K-AKT-mTOR pathway are the phosphatase and tensin homolog PTEN and merlin [27] (Fig. 17.2).
Schematic representation of TKRs-induced pathways. Growth factors binding to their specific receptors induce intracytoplasmanic phosphorylation and activation of TKRs. TKRs transduce their signals mainly through PI3K-AKT-mTOR pathway and MAPK (Mitogen-Activated Protein Kinase) pathway and are mainly implicated in cell proliferation and survival. PI3K-AKT-mTOR pathway: activated PI3K induces AKT phosphorylation and activation. AKT activates mTORC1 that in turn induces mRNA translation and protein synthesis. mTORC1 inhibits mTORC2. Activated mTORC2 regulates the activity of several protein kinases including AKT. Merlin and PTEN are negative regulators of PI3K-AKT-mTOR pathway. Tivantinib inhibits the kinase domain of c-MET receptor; imatinib mesylate inhibits PDGFR; erlotinib and gefitinib inhibit EGFR. Everolimus inhibits mTORC1; apitolisib inhibits mTORC1, mTORC2, and PI3K; Afuresertib inhibits AKT. HGF Hepatocyte Growth Factor, c-MET mesenchymal–epithelial transition protein, PGF platelet-derived growth factor, PDGFR platelet-derived growth factor receptor, EGF epithermal growth factor, EGFR epithermal growth factor receptor, PTEN phosphatase and tensin homolog, PI3K phosphatidylinositide 3 kinase, mTORC1/2 mammalian target of rapamycin complex 1/2, RAS rat sarcoma (small GTPase), RAF rapidly accelerated fibrosarcoma, MEK mitogen-activated protein kinase kinase, ERK extracellular signal-regulated kinase
Aberrant activation of PI3K/AKT/mTOR pathway is a hallmark of many cancers including MPM [28, 29]. In MPM, recurrent NF2 mutations [8,9,10], loss of PTEN [30], or gain of function mutations of PI3K or AKT [8] are reported to be responsible for mTOR pathway activation. In recent years, rapamycin or rapamycin-derived (rapalog) inhibitors have been used to inhibit mTORC1; among them, the most studied were sirolimus (rapamycin), temsirolimus (CCI-779), and everolimus (RAD001, Novartis Pharmaceuticals). Preclinical studies strongly encouraged the use of rapalogs in MPM. Indeed, Lopez-Lagos et al. [31] demonstrated that merlin null cells showed mTORC1 activation and higher sensitivity to rapamycin treatment compared to merlin-expressing cells. Moreover, Pignochino and coworkers observed anticancer activity of everolimus in MPM cell lines and mouse xenograft models. Of note, everolimus strongly synergized with sorafenib (a multi-kinase inhibitor) [32]. Unfortunately, phase II trials evaluating everolimus activity in unselected MPM patients (www.clinicaltrials.gov; NCT00770120; NCT01024946) showed no clinical efficacy [33]. Probably, the lack of efficacy of everolimus-based therapy in MPM was due to the wide spectrum of PI3K/AKT activities as well as the loss of mTORC1 negative regulation of mTORC2. To overcome low efficacy of mTORC1 inhibitors, the dual PI3K and mTORC1/2 inhibitor apitolisib (Genentech) was assessed in clinical trials. Although the promising response rate of MPM patients is in phase I trial (www.clinicaltrials.gov, NCT00854152; [34]), the drug revealed high toxicity profile in metastatic renal cell carcinoma phase II trials (www.clinicaltrials.gov, NCT01442090; [35] (Table 17.1). Encouraging results were obtained with another AKT inhibitor: Afuresertib (Novartis, Pharmaceuticals). In vitro preclinical study demonstrated that afuresertib strongly inhibited cell growth and clonogenic activity of MPM cell lines, induced cell cycle arrest, and acted in cooperation with cisplatin in inducing MPM apoptosis [36]. Of note, phase I clinical trial of Afuresertib in multiple myeloma showed promising results [37], encouraging further assessment of this drug for the treatment of other cancers including MPM.
17.1.1.3 NF2/Merlin and FAK
Cell anchorage to Extracellular Matrix (ECM) triggers signal transduction pathways involved in cell growth, survival, motility, and invasiveness [38]. A central role in transducing these signals is carried out by the Focal Adhesion Kinase (FAK). FAK is a non-receptor cytoplasmic tyrosine kinase consisting of four domains: N-terminal FERM domain (regulatory domain), catalytic domain, proline-rich domain, and C-terminal focal adhesion domain. It is activated by Integrin Receptors, Growth Factor and Cytokine Receptors [38] (Fig. 17.3). FAK overexpression and deregulation has been described in several types of cancers, and it was linked to uncontrolled tumor growth and metastasis [38]. FAK acts mainly at the membrane levels, but Nuclear Localization Sequence (NLS) in the FERM domain has also been described [39], supporting the hypothesis that FAK may have a role in genes regulation. Small-molecule FAK inhibitors were extensively used both in preclinical studies and in clinical trials. These drugs consist mainly of selective ATP-competitive inhibitors of FAK (e.g., VS-4718, GSK2256098), although some of them target both FAK and its homolog PYK2 (e.g., VS-6062, VS-6063). In vitro results obtained using VS-4718 (Verastem) and VS-6062 (Verastem) in several types of cancer showed a strong activity of FAK inhibitors in reducing cell growth, motility, invasiveness, and metastatic potential [40]. Moreover, VS-4718 was able to deplete tumor suppressive microenvironment [41], while VS-6062 blocked TGF-β-dependent epithelial-to-mesenchymal transition and showed antiangiogenic effects [40]. As regard MPM, in vitro studies using FAK inhibitors revealed a link between merlin expression and anti-FAK therapy sensitivity. Indeed, MPM cell lines expressing merlin were more resistant to VS-4718 in respect of MPM cells characterized by loss of merlin. Shapiro et al. hypothesized that in merlin null cells, the loss of merlin-dependent signals derived from cell-to-cell contact may increase signals derived from cell-to-ECM contact, resulting in a hyper-activation of FAK [42]. In line with this hypothesis, reintroduction of merlin, in merlin null MPM cells, decreased FAK expression levels, FAK phosphorylation, and consequently cell invasiveness [43]. Although the strong preclinical evidence supporting the role of merlin as predictive biomarker for anti-FAK therapy, a phase II, double-blind, randomized, placebo-controlled trial aimed at determining the activity of VS-6063 (Defactinib, Verastem) in MPM, based on merlin status, showed no efficacy and was stopped (www.clinicaltrials.gov; COMMAND NCT01870609). A possible explanation of this failure was provided by Kato et al. that in their work identified E-cadherin as additional predictive biomarker for anti-FAK therapy in merlin null MPM. Using a large panel of MPM cell lines, they demonstrated that the expression levels of E-cadherin mRNA in merlin null cells significantly correlated with VS-4718 resistance, suggesting that evaluation of both markers may be useful for the selection of MPM patients suitable for anti-FAK therapy. Importantly, they also demonstrated that MPM patients characterized by low expression levels of merlin and E-cadherin mRNA showed the poorest overall survival [44]. An additional small-molecule FAK inhibitor tested in clinical trial was GSK2256098 (GlaxoSmithKline). GSK2256098 showed strong efficacy in reducing cell growth, anchorage-independent cell growth, survival, motility, and invasiveness both in vitro and in vivo [45, 46]. The first pharmacokinetic and pharmacodynamic study of GSK2256098 administered as single agent in advanced solid tumors included 29 MPM patients (46% of total patients enrolled) (www.clinicaltrials.gov, NCT01138033). Preliminary results showed a tolerable safety profile and antitumor activity in both merlin null and merlin-expressing MPM. Evaluation of PFS (progression free survival) revealed a greater efficacy in those patients characterized by merlin null status (23.4 weeks merlin null vs 10.9 merlin-positive patients), encouraging the stratification of patients based on merlin expression [47]. Finally, a clinical trial evaluating the efficacy of combined therapy using GSK2256098 and trametinib (a MAPK pathway inhibitor) in MPM is ongoing and preliminary results are promising (www.clinicaltrials.gov, NCT01938443) [48] (Table 17.1).
FAK pathway: integrin or RTK-mediated activation of FAK involves recruitment of different proteins including talin, paxillin RHOGEF, and Src. Activated FAK induces cell cycle progression through RAS/ERK1/2 pathway, inhibits apoptosis through RAS/ERK1/2 and PI3K/AKT pathways, promotes cell migration and invasion through PI3K/AKT/mTOR pathway and activation of p300CAS. VS-4718, VS-6063, and GSK2256098 are ATP-competitive FAK inhibitors that block FAK autophosphorylation. ECM extracellular matrix, RTKs Tyrosine Kinase Receptors, FAK Focal Adhesion Kinase, RHOGEF Rho guanine nucleotide exchange factor, ERK1/2 extracellular signal-regulated kinase 1/2, PI3K phosphatidylinositide 3 kinase, mTOR mammalian target of rapamycin, p130Cas p130 Crk-associated substrate, MMPs matrix metalloproteases
17.1.2 Tyrosine Kinase Receptors
Tyrosine Kinase Receptors (TKRs) are important class of transmembrane receptors transducing growth factor signals. The binding of growth factors with specific TKRs activates transduction pathways such as MAPKs (Mitogen Activated Protein Kinases), PI3K/AKT, Phospholipase Cγ (PLCγ), and Protein Kinases C (PKC), and regulates cell proliferation, survival, migration, invasion, and angiogenesis (Fig. 17.2). Oncogenic role of gain of function TKRs mutations or TKRs overexpression has been described in several types of cancers, and an important role in MPM carcinogenesis has been shown for c-MET (mesenchymal–epithelial transition protein), Platelet-Derived Growth Factor Receptor (PDGF), and Epidermal Growth Factor Receptors (EGFRs) (Fig. 17.2) [28].
EGFR overexpression has been detected in about 50% of MPM patients [49, 50]. Erlotinib (Tarceva, Genentech Inc.) and gefitinib (Iressa, Astra Zeneca Pharmaceuticals) are Tyrosine Kinase Inhibitors (TKIs) targeting specifically the intracytoplasmic catalytic domain of EGFR. These drugs have been successfully introduced in the treatment of NSCLC, where the response is strictly related to the presence of gain of function mutations in exons 19 and 21 of the EGFR gene [51]. Despite this, phase II clinical trials conducted in untreated mesothelioma patients failed to show activity with both erlotinib and gefitinib [50, 52], probably because EGFR mutations in MPM are infrequent [53] (Table 17.1).
c-MET is a tyrosine kinase receptor activated by the binding with Hepatocyte Growth Factor (HGF). HGF/MET signaling involved mainly the activation of PI3K/AKT pathway [54]. Overexpression of c-MET in mesothelioma tumors has been described, especially in epithelioid subtypes [55], and seemed to be related to mir-34 b/c silencing [56]. Moreover, mesothelioma patients expressed higher serum levels of HGF compared to healthy subjects [57]. These results encouraged the investigation of c-MET inhibitors in mesothelioma clinical trials. Tivantinib (ARQ 197), an orally bioavailable small-molecule c-MET inhibitor, was tested in phase II trial for the treatment of malignant mesothelioma previously treated (www.clinicaltrials.gov, NCT01861301). While in hepatocellular carcinoma the anticancer activity of tivantinib was related to c-MET overexpression [58], results of this trial showed disease control only in peritoneal mesothelioma group and no correlation with c-MET expression or mutation [59]. On the other hand, in MPM preclinical models, tivantinib showed low activity used as single agent, but synergistic antitumor activity in association with pemetrexed [60] or PI3K/mTOR inhibitors [61]. To date, phase I-Ib trial testing the efficacy of tivantinib plus carboplatin/pemetrexed as first-line therapy for malignant pleural mesothelioma and non-small cell lung cancer is ongoing (www.clinicaltrials.gov, NCT02049060) and results are awaited (Table 17.1).
PDGF is a growth factor inducing proliferation of mesothelioma cells. Its receptor is expressed in two different isoforms (PDGFRα and PDGFRβ). Normal mesothelial cells express PDGFRα, while mesothelioma tumors express high levels of PDGFRβ [51]. Imatinib mesylate (STU 571, Gleevec, Novartis), an inhibitor of tyrosine kinase associated with PDGFR, c-Kit and BCR-ABL fusion protein, was tested in several trials both as single-agent and combined therapies. Phase II trials showed no results when imatinib was administered as single agent [62, 63]; in a phase I study designed to determine the maximum-tolerated dose of imatinib mesylate in association to cisplatin and pemetrexed on 17 MPM patients, the combination was not well tolerated discouraging further examination [64]; finally, phase II trial aimed at assessing the antitumoral activity of a combination of imatinib mesylate and gemcitabine in patients with unresectable malignant mesothelioma expressing either PDGFR or c-Kit is ongoing (www.clinicaltrials.gov, NCT02303899) (Table 17.1).
Failure of TKIs in MPM treatment can be caused by the concomitant activation of different TKRs (MET; EGFR; PDGFR). For example, high percentage of MPM tumors and cell lines (70%) showed simultaneous overexpression of c-MET and EGFR and preclinical models revealed a synergistic antitumor activity using crizotinib (c-MET kinase inhibitor) and afatinib (EGFR inhibitor) [65]. Multi-targeted TKIs have been developed. Vandetanib (ZD6474, Zactima, Astra Zeneca Pharmaceuticals), an oral inhibitor of EGFR, VEGFR and RET tyrosine kinases, showed strong anticancer activity in MPM cell lines acting both inhibiting RET-dependent cell survival and VEGFR-dependent angiogenesis [66], and strongly enhancing carboplatin/pemetrexed cytotoxicity [67]. Despite this, its efficacy as single agent in vandetanib versus vinorelbine randomized phase II trial in 25 patients with inoperable or relapsed malignant mesothelioma showed disappointing results (www.clinicaltrials.gov; NCT00597116). Dasatinib (BMS354825, Sprycel, Bristol-Myers) targets BCR-ABL fusion protein and inhibits signals derived from PDGFR and Src family of non-receptor tyrosine kinase [68]. Single-agent dasatinib assessed in second-line or neoadjuvant setting showed high toxicity profile without anticancer efficacy [69, 70] (Table 17.1). These negative results highlight the need to test further TKI combinations and to identify reliable predictive biomarkers to select those patients suitable for specific therapies.
17.1.3 Apoptosis Dysregulation
Dysregulation of apoptotic pathway is a feature of MPM. O’kane et al., analyzing 54 MPM tumor samples that consist of both sarcomatoid and epithelioid subtypes, revealed overexpression of the antiapoptotic proteins BCL-2, BCL-XL, and Mcl-1 and downregulation of the proapoptotic Bad, Bax, and Bid. Most important, percentage of patients overexpressing BCL-XL and under-expressing Bad and Bid was significantly higher in sarcomatoid than in epithelioid subtypes [71]. Overexpression of caspase inhibitors XIAP (X-Linked Inhibitor Of Apoptosis) and survivin in MPM specimens has also been reported [72].
17.1.3.1 Apoptosis Dysregulation and HDAC Inhibitors
Histone deacetylases are 18 different enzymes divided into four classes based on functional criteria [73]. They control a plethora of cellular function including cell cycle arrest, apoptosis, angiogenesis, and immunomodulation regulating the activity of both histones and nonhistone proteins, such as p53, NF-kB, HSP90, and HIF-1alpha [74]. HDAC inhibitors include a wide spectrum of natural and synthetic compounds [75], and are classified as pan-deacetylase inhibitors, including vorinostat (Suberoylanilide Hydroxamic Acid-SAHA: Zolinza, Merck), panobinostat (LBH589; Farydak, Novartis), belinostat (PXD101; Beleodaq, Spectrum Pharmaceuticals), and trichostatin A, and class-specific inhibitors such as butyrate and valproate (inhibit class I and IIa HDACs) and SBHA (suberohydroxamic acid) (inhibits HADC 1 and 3) [73]. In MPM cell lines, downregulation of BCL-XL was implicated in butyrate-induced apoptosis [76], and in SBHA sensitization to TNF-Related Apoptosis-Inducing Ligand (TRAIL) [77]. Sensitization to TRAIL treatment was also obtained with panobinostat that acted inhibiting the expression of XIAP and increasing caspases’ activation [78]. Vandermeers et al. demonstrated increased apoptosis induction combining cisplatinum and pemetrexed treatment with both valproate and SAHA. Anticancer efficacy of valproate plus cisplatinum/pemetrexed therapy was also validated in an epithelioid in vivo model [79]. In MPM, HDAC inhibitors have been tested in clinical trials both as single agent and combined therapy (Table 17.1). Oral vorinostat, an FDA-approved drug for the treatment of cutaneous T-cell lymphoma, was tested in a phase III, double-blind, randomized, placebo-controlled trial (www.clinicaltrials.gov; NCT00128102). Six hundred and sixty-one mesothelioma patients progressed after platinum plus pemetrexed treatment were included in the study. Results of this phase III study showed no improvement in Overall Survival (OS) in vorinostat versus placebo-treated group [80]. Negative results were also obtained with belinostat in a phase II study in which 13 MPM patients were included for second-line treatment and received intravenous infusion of the drug. The study was stopped for lack of efficacy [81]. On the contrary, a phase II trial aimed at evaluating oral valproate administration plus doxorubicin for refractory or recurrent mesothelioma after platinum-based first-line therapy showed encouraging response rate (16%) and disease control (36%). Among 45 MPM patients enrolled into the study, the best response was observed in those patients with good performance status at the time of protocol inclusion [82].
17.1.3.2 Apoptosis Dysregulation and Proteasome Inhibitors
Proteasome is a multiprotein complex responsible for proteins degradation and homeostasis. Bortezomib (Velcade) is a potent proteasome inhibitor, approved by FDA for multiple myeloma treatments. It is able to activate intrinsic apoptosis mainly blocking the degradation of IKB (Inhibitor KB) and consequently the activation of the pro-survival NF-kB (nuclear factor kappa-light-chain-enhancer of activated B cells) pathway [83].
In MPM preclinical studies, the ability of bortezomib to induce apoptosis was confirmed [84]. Of note, a strong synergizing activity was reported when bortezomib was administrated in combination with carboplatin/pemetrexed therapy [85]. Despite this, clinical evaluation of bortezomib in MPM patients failed to reach satisfactory results. Phase II trial designed to evaluate the efficacy of bortezomib as single agent in first- and second-line setting showed no activity, discouraging further evaluations [86]; phase II study aimed at evaluating the efficacy of first-line therapy combining cisplatin and bortezomib did not fulfill the primary endpoint (progression-free survival rate at 18 weeks >67.5%) and showed higher toxicity than cisplatin/pemetrexed (or raltitrexed) therapy [87] (Table 17.1).
17.1.3.3 Apoptosis Dysregulation and MicroRNAs
MicroRNAs (miRNAs) are short, noncoding, RNAs that targeting sequence-specific mRNAs are implied in post-transcriptional regulation of genes expression. Based on their target mRNAs, microRNAs can act as oncogenes or tumor suppressor genes. Dysregulation of miRNAs expression has been described in many malignancies, including cancers. In MPM mir-34b/c, mir-16 and mir-193a-3p are downregulated. These miRNAs are implied in the regulation of pro-survival and antiapoptotic pathways [56, 88,89,90]. TargomiRs are minicells loaded with specific microRNAs (EDVs—EnGeneIC Dream Vector) representing a reliable delivery system for in vivo administration. Mir-16 mimic encapsulated in an EGFR-targeted EDVs was successfully tested in MPM xenograft model [89] paving the way for clinical assessment. Van Zandwijk et al. conducted a phase I, open-label, dose-escalation study aimed at testing safety and activity of mir-16-loaded minicells in patients with recurrent pleural mesothelioma previously treated (Table 17.1). Twenty-six MPM patients were enrolled into the study. 5 × 109 TargomiRs per week were well tolerated and revealed early signs of antitumor activity detected by CT and PET-CT (5% of patients had partial response and 68% of patients had stable disease). However, Targomir activity could not be clearly attributed to mir-16 targeting because the evaluation of mir-16 silencing on post-treatment biopsies has not been performed [91]. Nevertheless, results of the study are encouraging and warrant further clinical investigations.
17.1.4 Cell Cycle Regulation
Molecular pathogenesis of MPM is characterized by frequent deletion of CDKN2A gene. CDKN2A encodes p14/ARF and p16/INK4A proteins. p16/INK4a plays an important role in the regulation of the G1/S cell cycle checkpoint; it inhibits the activity of Cyclin-Dependent Kinases (CDKs) 4/6 preventing the phosphorylation of RB (Retinoblastoma protein) and thus G1/S cell cycle progression [51] (Fig. 17.4). Low expression of p16/INK4a significantly correlated with chemotherapy resistance and worse survival of MPM patients [92], suggesting that MPM patients carrying p16 deletion may benefit from CDK inhibitor-based therapy. CDK4/6 inhibitors (such as palbociclib and ribociclib) are under investigation in several tumors. These drugs mimic p16 activity preventing RB phosphorylation [93]. Palbociclib (PD-033299; Pfizer) is an oral available, potent CDK4/6 inhibitor characterized by a mild toxicity profile. It was approved by FDA for the treatment of estrogen-positive metastatic breast cancer. Of note, palbociclib showed efficacy in MPM cell lines when associated with PI3K inhibitors [94], but clinical trials aimed at testing its efficacy in MPM patients has not been performed yet.
Apoptotic pathways are represented on the left. TNF (Tumor Necrosis Factor)-related ligands trigger extrinsic apoptosis. Genotoxic agents induce mitochondrial intrinsic apoptosis through p53 phosphorylation and activation. Proapoptotic proteins are represented in green. Antiapoptotic proteins are represented in red. The role of p14ARF and p16INK4a proteins in the cell cycle regulation is represented on the right. p14ARF inhibits MDM2 and subsequently induces p53 accumulation and activation. p16INK4a inactivates cyclinD/CDK4/6 complex preventing the phosphorylation and inactivation of Rb, thus inducing G1/S cell cycle arrest. Palbociclib and ribociclib inhibit CDK4/6. FADD Fas-associated protein death domain, procasp/casp procaspase/caspase, BCL2 B-cell lymphoma 2, BCLXL B-cell lymphoma extra-large, MCL1 myeloid cell leukemia 1, BAX BCL2-associated X protein, BAK BCL2 Antagonist Killer, APAF1 apoptotic protease activating factor-1, c-IAP cellular inhibitor of apoptosis, XIAP X-linked inhibitor of apoptosis, MDM2 mouse double minute 2, CDK4/6 cyclin-dependent kinase 4/6, RB retinoblastoma protein
The efficacy of ribociclib (LEE01; Novartis) is under evaluation in solid tumor, including MPM. Phase II open-label, nonrandomized clinical trial including patients characterized by aberrant expression of CDK4/6, cyclin D1/3, or p16 is ongoing (www.clinicaltrials.gov; NCT02187783) (Table 17.1).
p14/ARF controls both cell cycle progression and apoptosis activation inhibiting MDM2 (Mouse Double Minute 2), the E3 ubiquitin ligase responsible for p53 degradation (Fig. 17.4). In p53 wild-type tumors, p14/ARF activity can be bypassed using small-molecule p53 activators such as Nutlin 3a, an inhibitor of MDM2-p53 interaction [95]. Nutlin 3a showed greater activity in those tumor characterized by over-activation of MDM2 [96]. This is of particular interest in MPM because MDM2 overexpression was reported in tumor samples, especially in sarcomatoid and biphasic subtypes [97]. In MPM preclinical studies, Nutlin 3a caused p53-dependent G1/S cell cycle arrest inducing p21 increase [98] also in ZL34 and MSTO-211H cell lines not expressing p14/ARF [92, 99]. Moreover, p53 activation was able to decrease the antiapoptotic protein survivin. However, in the absence of strong apoptotic stimuli, Nutlin 3a did not induce MPM cell death but strongly synergized with rhTRAIL-dependent apoptosis [98]. Clinical trial aimed at testing the activity of RG7112 (Roche), a Nutlin 3a analog optimized for clinical use, showed promising activity in leukemias [100] but modest responses and high toxicity in solid tumors [101]. A more potent nutlin analog, RG7388 (Roche) (idasanutlin) [102], is in phase III trial in relapsed/refractory AML (Acute Myeloblastic Leukemia) (www.clinicaltrials.gov; NCT02545283) encouraging future assessment in MPM both as single agent and combined therapy.
17.2 Conclusions
Although clinical evaluation of targeted therapies in MPM found a strong rationale in several molecular alterations characterizing this neoplasia, clinical trials aimed at evaluating the efficacy of biologic agents targeting key oncogenic pathways did not achieve the expected results [28]. A possible explanation of this failure may lie in the lack of driver mutations, which instead characterize other types of cancers. Indeed, while TKIs are ineffective in MPM, EGFR-mutated NSCLC is particularly suited to anti-EGFR therapies, so that these treatments entered in clinical practice. Loss of tumor suppressor genes results in the simultaneous dysregulation of different downstream pathways. For example, loss of NF2/merlin triggers cell proliferation through Hippo, PI3K-ATK-mTOR, and FAK pathways. In this context, targeting a single transduction pathway has shown to be ineffective to abrogate the proliferative pressure of cancer cells. These negative results highlight the need to better understand MPM biology. A comprehensive evaluation of cellular features, their interconnections, and their relationships with tumor microenvironment may help to develop novel therapeutic approaches aimed at targeting multiple key signals simultaneously.
References
Tsao AS, Wistuba I, Roth JA, Kindler HL. Malignant pleural mesothelioma. J Clin Oncol Off J Am Soc Clin Oncol. 2009;27(12):2081–90. Epub 2009/03/04.
Vogelzang NJ, Rusthoven JJ, Symanowski J, Denham C, Kaukel E, Ruffie P, et al. Phase III study of pemetrexed in combination with cisplatin versus cisplatin alone in patients with malignant pleural mesothelioma. J Clin Oncol Off J Am Soc Clin Oncol. 2003;21(14):2636–44. Epub 2003/07/16.
Kindler HL, Ismaila N, Armato SG 3rd, Bueno R, Hesdorffer M, Jahan T, et al. Treatment of malignant pleural mesothelioma: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol Off J Am Soc Clin Oncol. 2018;36(13):1343–73. Epub 2018/01/19.
Sekido Y. Genomic abnormalities and signal transduction dysregulation in malignant mesothelioma cells. Cancer Sci. 2010;101(1):1–6. Epub 2009/10/02.
Sekido Y, Pass HI, Bader S, Mew DJ, Christman MF, Gazdar AF, et al. Neurofibromatosis type 2 (NF2) gene is somatically mutated in mesothelioma but not in lung cancer. Cancer Res. 1995;55(6):1227–31. Epub 1995/03/15.
Cheng JQ, Lee WC, Klein MA, Cheng GZ, Jhanwar SC, Testa JR. Frequent mutations of NF2 and allelic loss from chromosome band 22q12 in malignant mesothelioma: evidence for a two-hit mechanism of NF2 inactivation. Genes Chromosomes Cancer. 1999;24(3):238–42. Epub 1999/08/19.
Baser ME, De Rienzo A, Altomare D, Balsara BR, Hedrick NM, Gutmann DH, et al. Neurofibromatosis 2 and malignant mesothelioma. Neurology. 2002;59(2):290–1. Epub 2002/07/24.
Lo Iacono M, Monica V, Righi L, Grosso F, Libener R, Vatrano S, et al. Targeted next-generation sequencing of cancer genes in advanced stage malignant pleural mesothelioma: a retrospective study. J Thorac Oncol. 2015;10(3):492–9. Epub 2014/12/17.
Bueno R, Stawiski EW, Goldstein LD, Durinck S, De Rienzo A, Modrusan Z, et al. Comprehensive genomic analysis of malignant pleural mesothelioma identifies recurrent mutations, gene fusions and splicing alterations. Nat Genet. 2016;48(4):407–16. Epub 2016/03/02.
Hylebos M, Van Camp G, Vandeweyer G, Fransen E, Beyens M, Cornelissen R, et al. Large-scale copy number analysis reveals variations in genes not previously associated with malignant pleural mesothelioma. Oncotarget. 2017;8(69):113673–86. Epub 2018/01/27.
Petrilli AM, Fernandez-Valle C. Role of Merlin/NF2 inactivation in tumor biology. Oncogene. 2016;35(5):537–48. Epub 2015/04/22.
Sato T, Sekido Y. NF2/Merlin inactivation and potential therapeutic targets in mesothelioma. Int J Mol Sci. 2018;19(4):988. Epub 2018/03/29.
Thurneysen C, Opitz I, Kurtz S, Weder W, Stahel RA, Felley-Bosco E. Functional inactivation of NF2/merlin in human mesothelioma. Lung Cancer. 2009;64(2):140–7. Epub 2008/10/07.
Yu FX, Zhao B, Guan KL. Hippo pathway in organ size control, tissue homeostasis, and cancer. Cell. 2015;163(4):811–28. Epub 2015/11/07.
Felley-Bosco E, Stahel R. Hippo/YAP pathway for targeted therapy. Translational Lung Cancer Res. 2014;3(2):75–83. Epub 2015/03/26.
Murakami H, Mizuno T, Taniguchi T, Fujii M, Ishiguro F, Fukui T, et al. LATS2 is a tumor suppressor gene of malignant mesothelioma. Cancer Res. 2011;71(3):873–83. Epub 2011/01/20.
Sekido Y. Inactivation of Merlin in malignant mesothelioma cells and the Hippo signaling cascade dysregulation. Pathol Int. 2011;61(6):331–44. Epub 2011/05/28.
Tranchant R, Quetel L, Tallet A, Meiller C, Renier A, de Koning L, et al. Co-occurring mutations of tumor suppressor genes, LATS2 and NF2, in malignant pleural mesothelioma. Clin Cancer Res. 2017;23(12):3191–202. Epub 2016/12/23.
Meerang M, Berard K, Friess M, Bitanihirwe BK, Soltermann A, Vrugt B, et al. Low Merlin expression and high Survivin labeling index are indicators for poor prognosis in patients with malignant pleural mesothelioma. Mol Oncol. 2016;10(8):1255–65. Epub 2016/07/06.
Zhang WQ, Dai YY, Hsu PC, Wang H, Cheng L, Yang YL, et al. Targeting YAP in malignant pleural mesothelioma. J Cell Mol Med. 2017;21(11):2663–76. Epub 2017/05/05.
Mizuno T, Murakami H, Fujii M, Ishiguro F, Tanaka I, Kondo Y, et al. YAP induces malignant mesothelioma cell proliferation by upregulating transcription of cell cycle-promoting genes. Oncogene. 2012;31(49):5117–22. Epub 2012/01/31.
Liu-Chittenden Y, Huang B, Shim JS, Chen Q, Lee SJ, Anders RA, et al. Genetic and pharmacological disruption of the TEAD-YAP complex suppresses the oncogenic activity of YAP. Genes Dev. 2012;26(12):1300–5. Epub 2012/06/09.
Gibault F, Corvaisier M, Bailly F, Huet G, Melnyk P, Cotelle P. Non-Photoinduced biological properties of Verteporfin. Curr Med Chem. 2016;23(11):1171–84. Epub 2016/03/17.
Vanhaesebroeck B, Guillermet-Guibert J, Graupera M, Bilanges B. The emerging mechanisms of isoform-specific PI3K signalling. Nat Rev Mol Cell Biol. 2010;11(5):329–41. Epub 2010/04/10.
Julien LA, Carriere A, Moreau J, Roux PP. mTORC1-activated S6K1 phosphorylates Rictor on threonine 1135 and regulates mTORC2 signaling. Mol Cell Biol. 2010;30(4):908–21. Epub 2009/12/10.
Janku F, Yap TA, Meric-Bernstam F. Targeting the PI3K pathway in cancer: are we making headway? Nat Rev Clin Oncol. 2018;15(5):273–91. Epub 2018/03/07.
Li W, Cooper J, Karajannis MA, Giancotti FG. Merlin: a tumour suppressor with functions at the cell cortex and in the nucleus. EMBO Rep. 2012;13(3):204–15. Epub 2012/04/07.
Stahel RA, Weder W, Felley-Bosco E, Petrausch U, Curioni-Fontecedro A, Schmitt-Opitz I, et al. Searching for targets for the systemic therapy of mesothelioma. Ann Oncol. 2015;26(8):1649–60. Epub 2015/02/28.
Cedres S, Ponce-Aix S, Pardo-Aranda N, Navarro-Mendivil A, Martinez-Marti A, Zugazagoitia J, et al. Analysis of expression of PTEN/PI3K pathway and programmed cell death ligand 1 (PD-L1) in malignant pleural mesothelioma (MPM). Lung Cancer. 2016;96:1–6. Epub 2016/05/03.
Agarwal V, Campbell A, Beaumont KL, Cawkwell L, Lind MJ. PTEN protein expression in malignant pleural mesothelioma. Tumour Biol. 2013;34(2):847–51. Epub 2012/12/18.
Lopez-Lago MA, Okada T, Murillo MM, Socci N, Giancotti FG. Loss of the tumor suppressor gene NF2, encoding merlin, constitutively activates integrin-dependent mTORC1 signaling. Mol Cell Biol. 2009;29(15):4235–49. Epub 2009/05/20.
Pignochino Y, Dell’Aglio C, Inghilleri S, Zorzetto M, Basirico M, Capozzi F, et al. The combination of sorafenib and everolimus shows antitumor activity in preclinical models of malignant pleural mesothelioma. BMC Cancer. 2015;15:374. Epub 2015/05/09.
Ou SH, Moon J, Garland LL, Mack PC, Testa JR, Tsao AS, et al. SWOG S0722: phase II study of mTOR inhibitor everolimus (RAD001) in advanced malignant pleural mesothelioma (MPM). J Thorac Oncol. 2015;10(2):387–91. Epub 2015/01/23.
Dolly SO, Wagner AJ, Bendell JC, Kindler HL, Krug LM, Seiwert TY, et al. Phase I study of Apitolisib (GDC-0980), dual Phosphatidylinositol-3-kinase and mammalian target of Rapamycin kinase inhibitor, in patients with advanced solid Tumors. Clin Cancer Res. 2016;22(12):2874–84. Epub 2016/01/21.
Powles T, Lackner MR, Oudard S, Escudier B, Ralph C, Brown JE, et al. Randomized open-label phase II trial of Apitolisib (GDC-0980), a novel inhibitor of the PI3K/mammalian target of Rapamycin pathway, versus Everolimus in patients with metastatic renal cell carcinoma. J Clin Oncol Off J Am Soc Clin Oncol. 2016;34(14):1660–8. Epub 2016/03/10.
Yamaji M, Ota A, Wahiduzzaman M, Karnan S, Hyodo T, Konishi H, et al. Novel ATP-competitive Akt inhibitor afuresertib suppresses the proliferation of malignant pleural mesothelioma cells. Cancer Med. 2017;6(11):2646–59. Epub 2017/09/30.
Spencer A, Yoon SS, Harrison SJ, Morris SR, Smith DA, Brigandi RA, et al. The novel AKT inhibitor afuresertib shows favorable safety, pharmacokinetics, and clinical activity in multiple myeloma. Blood. 2014;124(14):2190–5. Epub 2014/07/31.
Sulzmaier FJ, Jean C, Schlaepfer DD. FAK in cancer: mechanistic findings and clinical applications. Nat Rev Cancer. 2014;14(9):598–610. Epub 2014/08/08.
Lim ST, Mikolon D, Stupack DG, Schlaepfer DD. FERM control of FAK function: implications for cancer therapy. Cell Cycle. 2008;7(15):2306–14. Epub 2008/08/05.
Roy-Luzarraga M, Hodivala-Dilke K. Molecular pathways: endothelial cell FAK-A target for cancer treatment. Clin Cancer Res. 2016;22(15):3718–24. Epub 2016/06/05.
Serrels A, Lund T, Serrels B, Byron A, McPherson RC, von Kriegsheim A, et al. Nuclear FAK controls chemokine transcription, Tregs, and evasion of anti-tumor immunity. Cell. 2015;163(1):160–73. Epub 2015/09/26.
Shapiro IM, Kolev VN, Vidal CM, Kadariya Y, Ring JE, Wright Q, et al. Merlin deficiency predicts FAK inhibitor sensitivity: a synthetic lethal relationship. Sci Transl Med. 2014;6(237):237ra68. Epub 2014/05/23.
Poulikakos PI, Xiao GH, Gallagher R, Jablonski S, Jhanwar SC, Testa JR. Re-expression of the tumor suppressor NF2/merlin inhibits invasiveness in mesothelioma cells and negatively regulates FAK. Oncogene. 2006;25(44):5960–8. Epub 2006/05/03.
Kato T, Sato T, Yokoi K, Sekido Y. E-cadherin expression is correlated with focal adhesion kinase inhibitor resistance in Merlin-negative malignant mesothelioma cells. Oncogene. 2017;36(39):5522–31. Epub 2017/05/30.
Zhang J, He DH, Zajac-Kaye M, Hochwald SN. A small molecule FAK kinase inhibitor, GSK2256098, inhibits growth and survival of pancreatic ductal adenocarcinoma cells. Cell Cycle. 2014;13(19):3143–9. Epub 2014/12/09.
Thanapprapasr D, Previs RA, Hu W, Ivan C, Armaiz-Pena GN, Dorniak PL, et al. PTEN expression as a predictor of response to focal adhesion kinase inhibition in uterine cancer. Mol Cancer Ther. 2015;14(6):1466–75. Epub 2015/04/03.
Soria JC, Gan HK, Blagden SP, Plummer R, Arkenau HT, Ranson M, et al. A phase I, pharmacokinetic and pharmacodynamic study of GSK2256098, a focal adhesion kinase inhibitor, in patients with advanced solid tumors. Ann Oncol. 2016;27(12):2268–74. Epub 2016/10/14.
Arkenau H-T, Gazzah A, Plummer R, Blagden SP, Mak G, Soria J-C, et al. A phase Ib dose-escalation study of GSK2256098 (FAKi) plus trametinib (MEKi) in patients with selected advanced solid tumors. J Clin Oncol. 2015;33(15_suppl):2593.
Dazzi H, Hasleton PS, Thatcher N, Wilkes S, Swindell R, Chatterjee AK. Malignant pleural mesothelioma and epidermal growth factor receptor (EGF-R). Relationship of EGF-R with histology and survival using fixed paraffin embedded tissue and the F4, monoclonal antibody. Br J Cancer. 1990;61(6):924–6. Epub 1990/06/01.
Govindan R, Kratzke RA, Herndon JE 2nd, Niehans GA, Vollmer R, Watson D, et al. Gefitinib in patients with malignant mesothelioma: a phase II study by the cancer and Leukemia group B. Clin Cancer Res. 2005;11(6):2300–4. Epub 2005/03/25.
Pasello G, Favaretto A. Molecular targets in malignant pleural mesothelioma treatment. Curr Drug Targets. 2009;10(12):1235–44. Epub 2009/11/17.
Garland LL, Rankin C, Gandara DR, Rivkin SE, Scott KM, Nagle RB, et al. Phase II study of erlotinib in patients with malignant pleural mesothelioma: a southwest oncology group study. J Clin Oncol Off J Am Soc Clin Oncol. 2007;25(17):2406–13. Epub 2007/06/15.
Mezzapelle R, Miglio U, Rena O, Paganotti A, Allegrini S, Antona J, et al. Mutation analysis of the EGFR gene and downstream signalling pathway in histologic samples of malignant pleural mesothelioma. Br J Cancer. 2013;108(8):1743–9. Epub 2013/04/06.
Gaudino G, Yang H, Carbone M. HGF/met Signaling is a key player in malignant mesothelioma carcinogenesis. Biomedicine. 2014;2(4):327–44. Epub 2014/11/14.
Bois MC, Mansfield AS, Sukov WR, Jenkins SM, Moser JC, Sattler CA, et al. c-Met expression and MET amplification in malignant pleural mesothelioma. Ann Diagn Pathol. 2016;23:1–7. Epub 2016/07/13.
Kubo T, Toyooka S, Tsukuda K, Sakaguchi M, Fukazawa T, Soh J, et al. Epigenetic silencing of microRNA-34b/c plays an important role in the pathogenesis of malignant pleural mesothelioma. Clin Cancer Res. 2011;17(15):4965–74. Epub 2011/06/16.
Jagadeeswaran R, Ma PC, Seiwert TY, Jagadeeswaran S, Zumba O, Nallasura V, et al. Functional analysis of c-Met/hepatocyte growth factor pathway in malignant pleural mesothelioma. Cancer Res. 2006;66(1):352–61. Epub 2006/01/07.
Santoro A, Rimassa L, Borbath I, Daniele B, Salvagni S, Van Laethem JL, et al. Tivantinib for second-line treatment of advanced hepatocellular carcinoma: a randomised, placebo-controlled phase 2 study. Lancet Oncol. 2013;14(1):55–63. Epub 2012/11/28.
Maron SB, Karrison T, Kanteti R, Rao KA, Gandara DR, Koczywas M, et al. ARQ 197 in patients with previously-treated malignant mesothelioma (MM): a phase II trial from the University of Chicago phase II consortium. J Clin Oncol. 2015;33(15_suppl):7511.
Leon LG, Gemelli M, Sciarrillo R, Avan A, Funel N, Giovannetti E. Synergistic activity of the c-Met and tubulin inhibitor tivantinib (ARQ197) with pemetrexed in mesothelioma cells. Curr Drug Targets. 2014;15(14):1331–40. Epub 2014/12/09.
Kanteti R, Dhanasingh I, Kawada I, Lennon FE, Arif Q, Bueno R, et al. MET and PI3K/mTOR as a potential combinatorial therapeutic target in malignant pleural mesothelioma. PLoS One. 2014;9(9):e105919. Epub 2014/09/16.
Porta C, Mutti L, Tassi G. Negative results of an Italian Group for Mesothelioma (G.I.Me.) pilot study of single-agent imatinib mesylate in malignant pleural mesothelioma. Cancer Chemother Pharmacol. 2007;59(1):149–50. Epub 2006/04/26.
Mathy A, Baas P, Dalesio O, van Zandwijk N. Limited efficacy of imatinib mesylate in malignant mesothelioma: a phase II trial. Lung Cancer. 2005;50(1):83–6. Epub 2005/06/14.
Tsao AS, Harun N, Lee JJ, Heymach J, Pisters K, Hong WK, et al. Phase I trial of cisplatin, pemetrexed, and imatinib mesylate in chemonaive patients with unresectable malignant pleural mesothelioma. Clin Lung Cancer. 2014;15(3):197–201. Epub 2014/02/05.
Huang L, Cai M, Zhang X, Wang F, Chen L, Xu M, et al. Combinational therapy of crizotinib and afatinib for malignant pleural mesothelioma. Am J Cancer Res. 2017;7(2):203–17. Epub 2017/03/25.
Ogino H, Yano S, Kakiuchi S, Yamada T, Ikuta K, Nakataki E, et al. Novel dual targeting strategy with vandetanib induces tumor cell apoptosis and inhibits angiogenesis in malignant pleural mesothelioma cells expressing RET oncogenic rearrangement. Cancer Lett. 2008;265(1):55–66. Epub 2008/03/28.
Giovannetti E, Zucali PA, Assaraf YG, Leon LG, Smid K, Alecci C, et al. Preclinical emergence of vandetanib as a potent antitumour agent in mesothelioma: molecular mechanisms underlying its synergistic interaction with pemetrexed and carboplatin. Br J Cancer. 2011;105(10):1542–53. Epub 2011/10/06.
Tsao AS, He D, Saigal B, Liu S, Lee JJ, Bakkannagari S, et al. Inhibition of c-Src expression and activation in malignant pleural mesothelioma tissues leads to apoptosis, cell cycle arrest, and decreased migration and invasion. Mol Cancer Ther. 2007;6(7):1962–72. Epub 2007/07/11.
Dudek AZ, Pang H, Kratzke RA, Otterson GA, Hodgson L, Vokes EE, et al. Phase II study of dasatinib in patients with previously treated malignant mesothelioma (cancer and leukemia group B 30601): a brief report. J Thorac Oncol. 2012;7(4):755–9. Epub 2012/03/20.
Tsao AS, Lin H, Carter BW, Lee JJ, Rice D, Vaporcyan A, et al. Biomarker-integrated Neoadjuvant Dasatinib trial in Resectable malignant pleural mesothelioma. J Thorac Oncol. 2018;13(2):246–57. Epub 2018/01/10.
O'Kane SL, Pound RJ, Campbell A, Chaudhuri N, Lind MJ, Cawkwell L. Expression of bcl-2 family members in malignant pleural mesothelioma. Acta Oncol. 2006;45(4):449–53. Epub 2006/06/09.
Kleinberg L, Lie AK, Florenes VA, Nesland JM, Davidson B. Expression of inhibitor-of-apoptosis protein family members in malignant mesothelioma. Hum Pathol. 2007;38(7):986–94. Epub 2007/03/14.
Khan O, La Thangue NB. HDAC inhibitors in cancer biology: emerging mechanisms and clinical applications. Immunol Cell Biol. 2012;90(1):85–94. Epub 2011/11/30.
Paik PK, Krug LM. Histone deacetylase inhibitors in malignant pleural mesothelioma: preclinical rationale and clinical trials. J Thorac Oncol. 2010;5(2):275–9. Epub 2009/12/26.
Bolden JE, Peart MJ, Johnstone RW. Anticancer activities of histone deacetylase inhibitors. Nat Rev Drug Discov. 2006;5(9):769–84. Epub 2006/09/07.
Cao XX, Mohuiddin I, Ece F, McConkey DJ, Smythe WR. Histone deacetylase inhibitor downregulation of bcl-xl gene expression leads to apoptotic cell death in mesothelioma. Am J Respir Cell Mol Biol. 2001;25(5):562–8. Epub 2001/11/20.
Neuzil J, Swettenham E, Gellert N. Sensitization of mesothelioma to TRAIL apoptosis by inhibition of histone deacetylase: role of Bcl-xL down-regulation. Biochem Biophys Res Commun. 2004;314(1):186–91. Epub 2004/01/13.
Symanowski J, Vogelzang N, Zawel L, Atadja P, Pass H, Sharma S. A histone deacetylase inhibitor LBH589 downregulates XIAP in mesothelioma cell lines which is likely responsible for increased apoptosis with TRAIL. J Thorac Oncol. 2009;4(2):149–60. Epub 2009/01/31.
Vandermeers F, Hubert P, Delvenne P, Mascaux C, Grigoriu B, Burny A, et al. Valproate, in combination with pemetrexed and cisplatin, provides additional efficacy to the treatment of malignant mesothelioma. Clin Cancer Res. 2009;15(8):2818–28. Epub 2009/04/09.
Krug LM, Kindler HL, Calvert H, Manegold C, Tsao AS, Fennell D, et al. Vorinostat in patients with advanced malignant pleural mesothelioma who have progressed on previous chemotherapy (VANTAGE-014): a phase 3, double-blind, randomised, placebo-controlled trial. Lancet Oncol. 2015;16(4):447–56. Epub 2015/03/25.
Ramalingam SS, Belani CP, Ruel C, Frankel P, Gitlitz B, Koczywas M, et al. Phase II study of belinostat (PXD101), a histone deacetylase inhibitor, for second line therapy of advanced malignant pleural mesothelioma. J Thorac Oncol. 2009;4(1):97–101. Epub 2008/12/20.
Scherpereel A, Berghmans T, Lafitte JJ, Colinet B, Richez M, Bonduelle Y, et al. Valproate-doxorubicin: promising therapy for progressing mesothelioma. A phase II study. Eur Respir J. 2011;37(1):129–35. Epub 2010/06/10.
Fennell DA, Chacko A, Mutti L. BCL-2 family regulation by the 20S proteasome inhibitor bortezomib. Oncogene. 2008;27(9):1189–97. Epub 2007/09/11.
Sartore-Bianchi A, Gasparri F, Galvani A, Nici L, Darnowski JW, Barbone D, et al. Bortezomib inhibits nuclear factor-kappaB dependent survival and has potent in vivo activity in mesothelioma. Clin Cancer Res. 2007;13(19):5942–51. Epub 2007/10/03.
Gordon GJ, Mani M, Maulik G, Mukhopadhyay L, Yeap BY, Kindler HL, et al. Preclinical studies of the proteasome inhibitor bortezomib in malignant pleural mesothelioma. Cancer Chemother Pharmacol. 2008;61(4):549–58. Epub 2007/05/25.
Fennell DA, McDowell C, Busacca S, Webb G, Moulton B, Cakana A, et al. Phase II clinical trial of first or second-line treatment with bortezomib in patients with malignant pleural mesothelioma. J Thorac Oncol. 2012;7(9):1466–70. Epub 2012/08/17.
O’Brien ME, Gaafar RM, Popat S, Grossi F, Price A, Talbot DC, et al. Phase II study of first-line bortezomib and cisplatin in malignant pleural mesothelioma and prospective validation of progression free survival rate as a primary end-point for mesothelioma clinical trials (European Organisation for Research and Treatment of Cancer 08052). Eur J Cancer. 2013;49(13):2815–22. Epub 2013/06/25.
Williams M, Kirschner MB, Cheng YY, Hanh J, Weiss J, Mugridge N, et al. miR-193a-3p is a potential tumor suppressor in malignant pleural mesothelioma. Oncotarget. 2015;6(27):23480–95. Epub 2015/07/01.
Reid G, Pel ME, Kirschner MB, Cheng YY, Mugridge N, Weiss J, et al. Restoring expression of miR-16: a novel approach to therapy for malignant pleural mesothelioma. Ann Oncol. 2013;24(12):3128–35. Epub 2013/10/24.
Truini A, Coco S, Genova C, Mora M, Dal Bello MG, Vanni I, et al. Prognostic and therapeutic implications of MicroRNA in malignant pleural mesothelioma. MicroRNA. 2016;5(1):12–8. Epub 2016/01/29.
van Zandwijk N, Pavlakis N, Kao SC, Linton A, Boyer MJ, Clarke S, et al. Safety and activity of microRNA-loaded minicells in patients with recurrent malignant pleural mesothelioma: a first-in-man, phase 1, open-label, dose-escalation study. Lancet Oncol. 2017;18(10):1386–96. Epub 2017/09/06.
Jennings CJ, Murer B, O'Grady A, Hearn LM, Harvey BJ, Kay EW, et al. Differential p16/INK4A cyclin-dependent kinase inhibitor expression correlates with chemotherapy efficacy in a cohort of 88 malignant pleural mesothelioma patients. Br J Cancer. 2015;113(1):69–75. Epub 2015/06/10.
O’Leary B, Finn RS, Turner NC. Treating cancer with selective CDK4/6 inhibitors. Nat Rev Clin Oncol. 2016;13(7):417–30. Epub 2016/04/01.
Bonelli MA, Digiacomo G, Fumarola C, Alfieri R, Quaini F, Falco A, et al. Combined inhibition of CDK4/6 and PI3K/AKT/mTOR pathways induces a synergistic anti-tumor effect in malignant pleural mesothelioma cells. Neoplasia. 2017;19(8):637–48. Epub 2017/07/14.
Urso L, Calabrese F, Favaretto A, Conte P, Pasello G. Critical review about MDM2 in cancer: possible role in malignant mesothelioma and implications for treatment. Crit Rev Oncol Hematol. 2016;97:220–30. Epub 2015/09/12.
Tovar C, Graves B, Packman K, Filipovic Z, Higgins B, Xia M, et al. MDM2 small-molecule antagonist RG7112 activates p53 signaling and regresses human tumors in preclinical cancer models. Cancer Res. 2013;73(8):2587–97. Epub 2013/02/13.
Pasello G, Urso L, Mencoboni M, Grosso F, Ceresoli GL, Lunardi F, et al. MDM2 and HIF1alpha expression levels in different histologic subtypes of malignant pleural mesothelioma: correlation with pathological and clinical data. Oncotarget. 2015;6(39):42053–66. Epub 2015/11/07.
Urso L, Cavallari I, Silic-Benussi M, Biasini L, Zago G, Calabrese F, et al. Synergistic targeting of malignant pleural mesothelioma cells by MDM2 inhibitors and TRAIL agonists. Oncotarget. 2017;8(27):44232–41. Epub 2017/06/01.
Hopkins-Donaldson S, Belyanskaya LL, Simoes-Wust AP, Sigrist B, Kurtz S, Zangemeister-Wittke U, et al. p53-induced apoptosis occurs in the absence of p14(ARF) in malignant pleural mesothelioma. Neoplasia. 2006;8(7):551–9. Epub 2006/07/27.
Andreeff M, Kelly KR, Yee K, Assouline S, Strair R, Popplewell L, et al. Results of the phase I trial of RG7112, a small-molecule MDM2 antagonist in leukemia. Clin Cancer Res. 2016;22(4):868–76. Epub 2015/10/16.
Burgess A, Chia KM, Haupt S, Thomas D, Haupt Y, Lim E. Clinical overview of MDM2/X-targeted therapies. Front Oncol. 2016;6:7. Epub 2016/02/10.
Ding Q, Zhang Z, Liu JJ, Jiang N, Zhang J, Ross TM, et al. Discovery of RG7388, a potent and selective p53-MDM2 inhibitor in clinical development. J Med Chem. 2013;56(14):5979–83. Epub 2013/07/03.
Jackman DM, Kindler HL, Yeap BY, Fidias P, Salgia R, Lucca J, et al. Erlotinib plus bevacizumab in previously treated patients with malignant pleural mesothelioma. Cancer. 2008;113(4):808–14.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Urso, L., Pasello, G. (2019). Targeted Therapies in Mesothelioma. In: Ceresoli, G., Bombardieri, E., D'Incalci, M. (eds) Mesothelioma. Springer, Cham. https://doi.org/10.1007/978-3-030-16884-1_17
Download citation
DOI: https://doi.org/10.1007/978-3-030-16884-1_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-16883-4
Online ISBN: 978-3-030-16884-1
eBook Packages: MedicineMedicine (R0)