Abstract
The present chapter examines segmental resection as a surgical option in the treatment of Crohn’s disease of the large bowel. Segmental resection is feasible only if the disease extent is limited, while total abdominal colectomy is more likely associated with multi-segmental or diffuse disease. However, segmental resection and total abdominal colectomy are associated with comparable risk of both overall disease recurrence and surgical recurrence. Most studies have also indicated that the risk of permanent stoma creation is comparable. Therefore, a segmental resection is generally preferable when the extent of disease is limited. In case of concurrent dysplasia the standard of care remains total proctocolectomy with end ileostomy. Either segmental colectomy or total abdominal colectomy are associated with substantial risk of metachronous cancer or dysplasia and should therefore be considered only in individualized circumstances.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Introduction
Total abdominal colectomy with ileorectal anastomosis is an accepted alternative to total proctocolectomy and end ileostomy in the surgical management of patients with Crohn’s disease of the colon provided that the rectum and anoperineum have minimal or no evidence of active disease [1,2,3]. Segmental colonic resection for the same scenario is an even more conservative option, which could still remove gross disease while allowing improved functional results. It is uncertain however whether a segmental resection actually results in improved functional outcomes and whether it is associated with an increased risk of disease recurrence.
Patient population | Intervention | Comparator | Outcomes studied |
|---|---|---|---|
Patients with Crohn’s colitis and rectal sparing | Segmental resection | Total colectomy | Recurrence rate, functional results |
Search Strategy
A comprehensive literature search of Cochrane Database of Collected Research, EMBASE, MEDLINE, and PubMed was performed to identify all of the English-language publications related to Crohn’s disease, colectomy, recurrence and functional results from 1985 to 2015. Key search terms included the following: “Crohn’s colitis”, “Crohn’s disease of the colon”, “inflammatory bowel disease,” “Crohn’s disease” “surgical treatment”, “colectomy,” “subtotal colectomy”, “total colectomy”, “hemicolectomy”, “segmental colectomy”, “resection of the colon”, “colonic resection”. Studies were excluded if they did not directly contrast segmental resection with total colectomy, failed to measure recurrence and functional results, included patients with ulcerative colitis or familial adenomatous polyposis, or included pediatric patients. Only the most recent study was included if similar studies from the same institution were encountered. The references of the included studies were reviewed to identify additional studies that were incorporated as appropriate.
Results
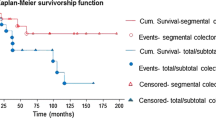
The available evidence indicates that segmental colectomy and total abdominal colectomy for management of Crohn’s disease of the colon are comparable with respect to the risk of recurrence. When assessing surgical recurrence, a few studies have been conducted over a long period of time and their quality is moderate to low (Table 17.1). All of the studies are retrospective and not surprisingly patients treated with segmental colectomy were more likely to have disease localized to a single colonic segment while total abdominal colectomy was more frequently performed when two or more colonic segments were involved. An earlier meta-analysis comparing these surgical approaches in patients with two or more colonic segments indicated that patients undergoing total abdominal colectomy and ileorectal anastomosis experienced a lower reoperation rate, although the difference did not reach statistical significance [4]. Angriman conducted a more recent systematic review, which included data on both surgical recurrence and overall recurrence, and found statistically similar rates when comparing the two operations. An additional subset analysis that focused on patients undergoing surgery after the introduction of biologic medications again confirmed equivalence in the risk of either overall or surgical recurrence [5].
With respect to functional results, one relevant endpoint assessed in the literature is the risk of permanent stoma. Most studies have indicated that the risk for permanent stoma creation is comparable between segmental colectomy and total colectomy, particularly more recent studies [6,7,8]. Earlier studies had suggested that the more conservative segmental colectomy is actually associated with a significant reduction in the risk of permanent stoma creation [9,10,11]. When all eligible studies were evaluated in a systematic review, the incidence of permanent stoma was significantly decreased following segmental colectomy [5].
Despite the putative advantages of preservation of a longer segment of functioning bowel, there is actually limited data on functional outcomes. Andersson reported that patients undergoing segmental colectomy experienced improved anorectal function when assessing a composite score incorporating the ability to pass flatus without leakage, incontinence for loose stools, and soiling [6]. A subsequent study by Kiran assessed the Cleveland Global Quality of Life [12] instrument scores and Short Form Inflammatory Bowel Disease Questionnaire scores, which were both found to be statistically similar between the groups [8].
The management of patients with dysplasia or cancer on the background of Crohn’s disease is a particularly daunting problem. In general, the standard of care in this situation is total proctocolectomy with end ileostomy and either a segmental resection or a total colectomy should be avoided [13]. Kiran identified a 40% rate of remote dysplasia in the resected specimen in the presence of cancer and an incidence of multifocal dysplasia of 44% [14]. A more recent study reported that 40% of patients undergoing segmental colectomy for neoplasm and 35% receiving a subtotal colectomy for the same indication developed metachronous cancer over a mean follow-up of 6.8 years [15]. However, there have been reports of selected patients undergoing conservative, sphincter-saving procedures, ranging from segmental resection to subtotal colectomy, which resulted in acceptable oncologic outcomes. This approach remains highly controversial and has been advocated for individualized cases, such as poor-risk patients and/or cases of preoperative low-grade dysplasia [14]. The techniques of endoscopic detection and management of colorectal dysplasia in Crohn’s disease of the colon continue to evolve and could lead in the future to a decreased number of patients requiring surgery for this particular indication [16].
Recommendations
In patients requiring surgery for Crohn’s disease of the colon, a segmental colectomy is equivalent to a total abdominal colectomy in terms of disease recurrence and risk of permanent stoma creation. If the extent of disease is limited, a segmental resection is therefore preferable. While the preservation of a longer segment of functional large intestine seems to be intuitively desirable, a segmental resection is not associated with substantially documented advantages. For patients requiring surgery for dysplasia, the operation of choice remains total proctocolectomy with end ileostomy.
Personal View
The general management principle describing the surgical approach to colonic disease should be to resect only segments of colon that are grossly involved with Crohn’s disease. Therefore, if Crohn’s disease is located in a discrete segment of colon, a segmental resection is preferable. The perioperative complication rate is similar to total colectomy and there are possible functional advantages. There is no evidence that the removal of a longer segment of colon through total abdominal colectomy results in either reduced disease recurrence or increased stoma-free survival. The factors independently associated with disease recurrence and risk of permanent stoma creation do not include a particular restorative procedure, whether segmental resection or total colectomy, but are instead disease-related or patient-related variables such as younger age [18], female sex [19], and concurrent perianal disease [8, 17]. The only operation for large bowel Crohn’s disease that independently minimizes the risk of disease recurrence is total proctocolectomy with end ileostomy, which is obviously not favored by the majority of patients.
In the case of diffuse Crohn’s disease of the colon with rectal sparing or mild proctitis, total abdominal colectomy remains a reasonable surgical option. Under these circumstances segmental colectomy is not feasible. Two segments of disease separated by a short segment of grossly preserved colon should be de facto considered as one single area of disease and therefore should be preferentially treated with one long, encompassing segmental resection. However, if the colitis is distributed in two or more distinctive segments, a total abdominal colectomy is preferable to a double segmental colonic resection.
With respect to dysplasia in the background of Crohn’s disease of the colon, treatment algorithms are evolving with increasing data supporting the safety of endoscopic management as suggested by the SCENIC guidelines [16]. For those patients requiring surgery for dysplasia, any option more conservative then total proctocolectomy and end ileostomy remains oncologically risky and should be considered only in extraordinary, individualized cases.
Abstracted Recommendation
Patients requiring surgery for Crohn’s disease of the large bowel limited to the colon can undergo segmental resection when technically feasible instead of total abdominal colectomy. (strong recommendation based on low and moderate quality evidence).
References
Longo WE, et al. Outcome of ileorectal anastomosis for Crohn’s colitis. Dis Colon Rectum. 1992;35(11):1066–71.
Yamamoto T, Allan RN, Keighley MR. Smoking is a predictive factor for outcome after colectomy and ileorectal anastomosis in patients with Crohn’s colitis. Br J Surg. 1999;86(8):1069–70.
O’Riordan JM, et al. Long-term outcome of colectomy and ileorectal anastomosis for Crohn’s colitis. Dis Colon Rectum. 2011;54(11):1347–54.
Tekkis PP, et al. A comparison of segmental vs subtotal/total colectomy for colonic Crohn’s disease: a meta-analysis. Color Dis. 2006;8(2):82–90.
Angriman I, et al. A systematic review of segmental vs subtotal colectomy and subtotal colectomy vs total proctocolectomy for colonic Crohn’s disease. Color Dis. 2017;19(8):e279–87.
Andersson P, et al. Segmental resection or subtotal colectomy in Crohn’s colitis? Dis Colon Rectum. 2002;45(1):47–53.
Fichera A, et al. Long-term outcome of surgically treated Crohn’s colitis: a prospective study. Dis Colon Rectum. 2005;48(5):963–9.
Kiran RP, et al. The role of primary surgical procedure in maintaining intestinal continuity for patients with Crohn’s colitis. Ann Surg. 2011;253(6):1130–5.
Sanfey H, Bayless TM, Cameron JL. Crohn’s disease of the colon. Is there a role for limited resection? Am J Surg. 1984;147(1):38–42.
Andrews HA, Lewis P, Allan RN. Prognosis after surgery for colonic Crohn’s disease. Br J Surg. 1989;76(11):1184–90.
Makowiec F, et al. Long-term follow-up after resectional surgery in patients with Crohn’s disease involving the colon. Z Gastroenterol. 1998;36(8):619–24.
Kiran RP, et al. Prospective assessment of Cleveland Global Quality of Life (CGQL) as a novel marker of quality of life and disease activity in Crohn’s disease. Am J Gastroenterol. 2003;98(8):1783–9.
Strong S, et al. Clinical practice guideline for the surgical management of Crohn’s disease. Dis Colon Rectum. 2015;58(11):1021–36.
Kiran RP, et al. Dysplasia associated with Crohn’s colitis: segmental colectomy or more extended resection? Ann Surg. 2012;256(2):221–6.
Maser EA, et al. High rates of metachronous colon cancer or dysplasia after segmental resection or subtotal colectomy in Crohn’s colitis. Inflamm Bowel Dis. 2013;19(9):1827–32.
Laine L, et al. SCENIC international consensus statement on surveillance and management of dysplasia in inflammatory bowel disease. Gastroenterology. 2015;148(3):639–651.e28.
Bernell O, Lapidus A, Hellers G. Recurrence after colectomy in Crohn’s colitis. Dis Colon Rectum. 2001;44(5):647–54; discussion 654.
Martel P, et al. Crohn’s colitis: experience with segmental resections; results in a series of 84 patients. J Am Coll Surg. 2002;194(4):448–53.
Polle SW, et al. Recurrence after segmental resection for colonic Crohn’s disease. Br J Surg. 2005;92(9):1143–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Stocchi, L. (2019). The Role of Segmental Resection in Crohn’s Colitis. In: Hyman, N., Fleshner, P., Strong, S. (eds) Mastery of IBD Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-16755-4_17
Download citation
DOI: https://doi.org/10.1007/978-3-030-16755-4_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-16754-7
Online ISBN: 978-3-030-16755-4
eBook Packages: MedicineMedicine (R0)