Abstract
Hirschsprung-associated enterocolitis (HAEC) was described in 1886 by Harald Hirschsprung and is the most feared complication of Hirschsprung disease. HAEC is clinically characterized by abdominal distension, fever, and diarrhea, although there can be a variety of other associated symptoms, including colicky abdominal pain, lethargy, and the passage of bloodstained stools. HAEC can occur preoperatively or postoperatively, is the presenting symptom of HSCR in up to 25% of infants, and carries an overall incidence ranging from 20% to 60%. This chapter reviews our current understanding of HAEC pathophysiology, risk factors, diagnosis, and treatment. Areas of current research or controversy and topics for future investigation are presented.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Hirschsprung disease
- Hirschsprung’s disease
- Enterocolitis
- HAEC
- Microbiota
- Microbiome
- Mucosal immunity
- Motility
- Dysmotility
- Intestinal barrier
- Diagnosis
- Treatment
- Therapy
13.1 Introduction
Hirschsprung disease (HSCR, Online Mendelian Inheritance in Man #142623) is a common cause of neonatal bowel obstruction and was first described in 1886 by Harald Hirschsprung [42]. HSCR can lead to the feared complication of Hirschsprung-associated enterocolitis (HAEC), which is the condition that, in retrospect, Hirschsprung originally described. Broadly, HAEC is clinically characterized by abdominal distension, fever, and diarrhea, although there can be a variety of other associated symptoms, including colicky abdominal pain, lethargy, and the passage of bloodstained stools. At the time of his original description, Hirschsprung presented two children with constipation from birth who died after developing marked abdominal distension and loose stools; these would become the first reported cases of HAEC. Although the concept of HAEC was alluded to in the literature in 1950 by Burnard, Fisher and Swenson in 1956, and Dorman in 1957, it was not until 1962 that Bill and Chapman presented the first definitive description of the condition [11, 13, 22, 25].
HAEC can occur preoperatively or postoperatively and is the presenting symptom of HSCR in up to 25% of infants [26, 39, 63, 66]. The incidence of enterocolitis ranges from 20% to 60% [6, 24, 26, 30, 38]. HAEC can occur at any time from the neonatal period onwards into adulthood and can be independent of the medical management or surgical procedure performed. Recurrent HAEC can occur even in the presence of a diverting colostomy and is termed “diversion enterocolitis” [49, 73].
Currently, the diagnosis of HAEC is predominantly based on clinical judgment. This has led to highly variable reports in the incidence rates of HAEC, ranging from 25% to 30% in recent series to as high as 60% in the past. Preoperative incidence is estimated at 6%–60%, and postoperative incidence ranges from 25% to 42% [23, 38, 77]. The overall mortality rate associated with HAEC ranges from 1% to 10%, with the majority of deaths occurring in newborns prior to definitive operation [63]. These newborn infants are at the highest risk of mortality among patients with HAEC. It is unclear whether these infants have higher mortality rates due to a delay in diagnosis, immature immune responses, or some other mechanism. Fortunately, the mortality rate appears to be declining over time, likely due to increasing recognition of this devastating complication. This includes earlier diagnosis of HSCR and HAEC and initiation of therapies such as rectal decompression, vigorous fluid resuscitation, and antibiotic therapy.
However, despite the improvement in mortality rates in HAEC, the morbidity has a profound impact on prolonged hospitalization with a mean of 13 days (ranging from 6 to 29 days). Teitelbaum et al. found that neonates with HAEC have a mortality rate of 5% and a morbidity rate of 30%, and their hospitalization is twice as long as neonates without HAEC [76]. The medical management of HSCR children with HAEC is 2.5 times costlier than of those without HAEC. Moreover, HSCR patients who develop HAEC have worse long-term bowel function than those who never develop HAEC, possibly secondary to inflammatory changes to the ENS [63].
In this chapter, we will review our current understanding of HAEC pathophysiology, risk factors, diagnosis, and treatment. We will additionally present areas of current research or controversy and topics for future investigation.
13.2 Pathophysiology
Despite multiple investigations and numerous theories, a complete understanding of the etiology of HAEC is still elusive. There are currently four prevailing theories regarding the etiology of HAEC: (1) dysmotility, (2) intestinal barrier function, (3) impaired mucosal immunity, and (4) abnormal microbiota.
13.2.1 Historical Considerations
Multiple small series or case reports have put forth etiologic considerations for HAEC.
In 1973, Ament and Bill presented the case of a 6-year-old boy with chronic enterocolitis following surgery for HSCR [3]. Clinical investigations revealed the presence of a sucrase-isomaltase deficiency, and the child recovered on a low sucrose diet. This led to the postulation that non-obstructed HAEC is caused by an inborn error of metabolism. It is important to note that this has not been replicated and that Ament and Bill acknowledged that the boy was an Eskimo and that 10% of Greenland Eskimos are sucrose-intolerant.
Berry and Frazer in 1968 suggested that HAEC is initiated by a sensitivity reaction similar to a Shwartzman reaction caused by intraluminal organisms invading the submucosa [9]. They injected endotoxin directly into the exteriorized rabbit bowel proximal to an obstruction and produced enterocolitis in six of nine animals.
A single case was reported by Lloyd-Still and Demers of HAEC with fulminant unresponsive diarrhea which revealed high PgE1 levels [47]. In response to cholestyramine, a 12-fold decrease in prostaglandin E (PgE) levels in the colostomy fluid was detected. It was postulated that increased PgE activity, enterotoxin, and bile acid malabsorption may be involved in HAEC.
In 1988 Wilson-Storey et al. postulated that defective white cell function may be a predisposing factor for HAEC [94]. White cell counts were analyzed in nine patients with HSCR, of whom five developed HAEC and ten age-matched controls. Their data showed statistically significant differences between the neutrophil count in those with HAEC, HSCR, and controls. This relative neutropenia worsened in three patients during and after an episode of HAEC. The authors also postulated that white cells in HAEC patients are “sluggish” in response to the inflammation.
While these series have not been confirmed in the basic science laboratory or larger clinical series, it is important to consider that there may be component contributions from these types of observations to the multifactorial process of HAEC.
13.2.2 Dysmotility
One of the earliest proposed causes for HAEC was impaired intestinal motility leading to functional obstruction with either subsequent bacterial stasis, overgrowth and translocation, or distension and ischemia [11, 74, 75]. Bill and Chapman argued that partial mechanical obstruction was involved in the pathogenesis of HAEC causing mechanical dilatation of the proximal bowel leading to fecal loading and stasis resulting in further dilatation and thus mucosal ischemia and bacterial invasion which was cured by colostomy [11]. This suggests that enterocolitis only occurs in dilated ganglionic proximal bowel. However, this theory does not explain the enterocolitis that occurs in distal colon with a defunctioning proximal stoma, the occurrence of enterocolitis in postoperative patients, or histological evidence of enterocolitis in aganglionic bowel [67, 72].
The ENS participates in host defense by modulation of secretory function and propulsion of luminal contents, thereby diluting and purging pathogens [71, 91]. The role of intestinal motility in the pathogenesis of inflammatory bowel disease is well described, with acute episodes of intestinal inflammation in Crohn’s disease associated with decreased motility [10, 59]. It has been noted, in the EdnrB NCC−/− model, decreased neuronal density in the ganglionated bowel [96]. Further, there is a shift in neurotransmitter phenotypes, with overrepresentation of nitrergic (relaxation) neurons and underrepresentation of cholinergic (contractility) neurons. Similar findings have recently been published in the EdnrB −/− model and confirmed in human tissues, with a positive correlation between increased nitrergic neurons and postoperative enterocolitis [16].
13.2.3 Intestinal Barrier Dysfunction
The intestinal barrier plays a critical role in maintaining host health. Clinically the voluminous amount of mucus produced during HAEC is quite obvious and dramatic. Goblet cells produce mucus, which helps to maintain epithelial integrity by serving as a scaffold for bactericidal and bacteriostatic proteins. Abnormalities in mucin production, therefore, may contribute to the pathogenesis of HAEC.
In 1981, Akkary et al. studied rectal biopsies of HSCR patients and found a marked increase in the volume of mucin compared to control tissues [1]. Teitelbaum et al. hypothesized that HSCR involves an alteration in the composition of mucin in the colon, such that there is mucin retention and crypt dilation [76]. They proposed a histologic grading system which is unique to HSCR and cystic fibrosis. When they excluded patients with trisomy 21, whose histologic findings were often inconsistent with their clinical features, this grading system found that 100% of patients with HAEC had grade 3 or higher. Even though this system is not ideal for clinical use given the uneven distribution of histologic changes in resected specimens, it does demonstrate how the mucosa becomes susceptible to pathogens through local inflammatory responses.
A study of mucin turnover showed that HSCR patients who developed HAEC had turnover rates sevenfold lower than HSCR patients who did not develop HAEC [5]. Additionally, Hirschsprung’s patients also have decreased MUC-2, the predominant mucin expressed in the human colon; MUC-2 is nondetectable in patients with HAEC [12, 51]. This may suggest an intrinsic problem that could allow for bacterial adherence and translocation. Finally, Thiagarajah et al. compared tissue from HSCR patients and the distal colon of EdnrB −/− mice and found increased goblet cell numbers when compared to controls [81]. They then used trans-epithelial resistance measurements to assess for functional differences and noted that trans-epithelial resistance and fecal dehydration were increased in the distal colon of EdnrB −/− mice. Additionally, they found increased mucus viscosity and therefore impaired particle diffusion in null mice.
Overall the evidence has not proven whether mucin alteration is due to the underlying aganglionic condition or a result of the enterocolitis. However, the balance of data supports the concept that the mucin variations are an expression of an altered mucosal barrier and the underlying aganglionic process itself [51]. Taken together, these findings suggest that alterations in mucus production and function may play a role in the development of HAEC.
13.2.4 Impaired Mucosal Immunity
Abnormal leukocyte function has been implicated in the development of HAEC.
Secretory IgA immunoglobulin provides a major immunological barrier in the gastrointestinal tract. IgA is the predominant immunoglobulin at all levels in the intestinal tract, both in the lumen and within the wall. Albanese et al. have shown that secreted IgA binds to bacteria and prevents bacterial translocation across an intact segment of viable intestinal tissue [2]. In the late 1980s, Wilson-Storey et al. conducted a series of studies which demonstrated that patients affected by HSCR have impaired transfer of secretory IgA across the GI mucosa [92, 94]. Specifically, they noted that although HSCR patients had increased IgA in their buccal mucosal tissue, there was a significant decrease of secretory IgA in the saliva. Similarly, the plasma cells in the lamina propria of the bowel were found to have significant increased levels of IgA, IgM, and IgG in HAEC bowel compared to non-HAEC bowel [44]. Those same HAEC patients were found to have decreased luminal IgA, suggesting decreased production or impaired transport into the lumen.
The most common genetic defects associated with HSCR are mutations of rearranged during transfection (Ret) and endothelin receptor B (EdnrB), which are both required for NCC migration and ENS formation [4]. Piebald mice, which have a naturally occurring EdnrB mutation, demonstrate congenital megacolon with absent distal ganglion cells and hence are an excellent model for HSCR [87]. A number of studies have established mucosal secretory function in HAEC in these animals [31, 32]. Two distinct patterns of mortality occur with the majority of mice (64%) characterized by becoming unwell acutely with evidence of acute enterocolitis at 3–4 weeks and then dying quickly or dying between 9 and 11 weeks due to ileus with massive abdominal distension and megacolon. Interestingly two different immunological responses were evident. Those with a more acute history had acute splenitis and a severe diffuse lymphocytic response in the intestinal submucosa and lamina propria with a significantly raised level of IgA in contrast to controls and the late death group. The late death group had increased plasma cell distribution within the deep layer of the lamina propria only. This increased level of plasma cell infiltration in the ganglionic segment of the colon in the early death group implies that the local antigenic stimulation is the principal pathological event. Interestingly, the finding of decreased luminal IgA has also been observed in EdnrB NCC−/− mice, in which EdnrB is deleted only in neural crest cells which form the ENS [34]. The EdnrB NCC−/− mouse develops colorectal aganglionosis and HAEC similar to human HSCR. A recent study showed not only that luminal IgA is reduced but that this finding is specific to the gut, with normal levels of bronchial and nasal IgA observed in these animals [34]. Overall it appears that IgA production by plasma cells is either normal or impaired and that transport into the lumen is further impaired [52].
Mucosal neuroendocrine (NE) cells mediate intestinal function through synthesis and storage of neuroendocrine neuropeptides and biogenic amines which act as chemical messengers [88]. Soeda et al. demonstrated that NE cells are increased in the aganglionic segment of bowel in HSCR as opposed to the ganglionated bowel and normal controls [69]. They noted a marked reduction in NE cells in ganglionated bowel in HAEC compared to those without. These diminished NE cells may represent an impaired immune response or a deficiency which may facilitate the initialization of inflammation [70]. This impaired immune response theory is echoed in trisomy 21. The combination of HSCR and trisomy 21 is associated with a higher incidence of enterocolitis, with 50% of patients with trisomy 21 and HSCR developing HAEC in contrast to 29% among the normal population [4]. Infants with trisomy 21 have an intrinsic immune deficiency due to both decreased cytotoxic T lymphocytes and derangement in humoral function which may explain their increased risk of HAEC [56].
Histological evidence of enterocolitis consists of a number of features including crypt abscesses, leukocyte aggregates, ulceration, and Paneth cell metaplasia [31]. Paneth cells are normally present in the small bowel and secrete lysozymes which digest the bacterial wall membranes. Their presence in HAEC colon suggests an attempt at reinforcement of the mucosal immunity. ICAM-1 is a cell surface intercellular adhesion glycoprotein which is involved in leukocyte recruitment when inflammation occurs. Kobayashi et al. have demonstrated that ICAM-1 shows increased expression in the endothelium of both the ganglionated and aganglionic bowels in patients with HAEC [45]. This emphasizes the importance of endothelial cell activation in HAEC pathogenesis. Elhalaby et al. postulated that the occurrence of a single episode of HAEC can alter intrinsic intestinal immunity by causing a chronic change to the mucosa to an increased risk of further episodes [24]. This would help to explain the lower but real recurrence rate of HAEC following a “diversion” colostomy or a successful pull-through.
Splenic lymphopenia is also thought to contribute to an etiology of impaired immunity. This was first described in the EdnrB −/− mouse model by Cheng et al. [18]. These animals have abnormal splenic architecture and reduced total lymphocytes in the spleen. Specifically, they have a relative reduction in B as compared to T lymphocytes, as well as a negative correlation between splenic lymphocyte counts and intestinal inflammation on histologic analysis. This finding was confirmed in the EdnrB NCC−/− model, with the additional discovery of a decrease in marginal zone B lymphocytes, suggesting impaired B lymphocyte development or trafficking from the spleen to the Peyer’s patches of the small intestine [34]. Another group attempted to understand the contribution of the EdnrB genotype to the clinical expression of HAEC by performing bone marrow transplants from EdnrB animals to Rag2 −/− recipients and inducing bowel obstruction in wild-type animals [27]. They concluded that stress from obstruction resulted in similar lymphocyte alterations to those seen in HAEC models. However, they found that after surgical relief of obstruction, EdnrB −/− mice still carried a 40% risk of developing HAEC [97].
13.2.5 Abnormal Microbiota
Infectious etiologies have been linked to enterocolitis by a number of studies. Clostridium difficile was reported by Thomas et al. when high titers of the toxin were detected in four of six patients with HAEC [83]. They further detected the cytopathic toxin in 7 of 13 (54%), and C. difficile was isolated in 77% of children with HAEC [82]. In the control groups, C. difficile was isolated in 18% of those with HSCR and in 30% of children without. The authors postulated that the toxin was pathogenetic due to the incidence of toxin in the feces, the magnitude of the toxin levels, and the isolation rates for C. difficile which were significantly higher in HAEC patients than in those without HAEC or even HSCR. The possibility that HAEC could prevent the development of a “benign” colonic bacterial flora and aggressively treating C. difficile could improve this made this a very exciting theory. However, this has not been proven on subsequent investigations: 50% of all patients with HSCR have C. difficile, and there is no variation in incidence between before and after surgery [37]. Wilson-Storey et al. demonstrated a broad spectrum of organisms present in the stools with no significant difference in the Clostridium carriage rate between those with HAEC and those without HAEC or normal controls [93]. After an episode of enterocolitis, 70% of patients with HAEC have C. difficile present as opposed to 42% of those without HAEC. It is postulated that after the initiation of the enterocolitis episode, alteration in mucosal immunity allows C. difficile to flourish. Although it may not be causative, it may complicate the colitis. Pseudomembranous colitis with stools positive for C. difficile is rare and has been reported in four patients with a 50% mortality despite vancomycin therapy [8].
While several organisms have been found to be associated with HAEC (including C. difficile, E. coli, and rotavirus), none has been demonstrated to be causative. In the last 5 years, two mouse model studies have shed light on the relationship between host microbiome and development of HAEC.
Using the EdnrB −/− mouse model, Ward et al. demonstrated increasing microbiome diversity over 24 days, with a greater increase in HSCR mice versus wild type [86]. They identified clusters of microbiota in each group, showing that wild-type and HSCR mice had distinct microbiomes. Further, HSCR mice were found to have higher levels of Bacteroidetes and Firmicutes than controls. Similarly, Pierre et al. found evidence of comparable microbiomes between HSCR mice and controls early in the neonatal period, with divergence of the microbiota between HSCR and controls as the onset of HAEC approached [62]. HSCR mice expressed increased Bacteroidetes and Clostridium species, and E. coli was found only in HSCR mice. Both of these studies also showed decrease in Lactobacillus over time in HSCR mice. Another group used the EdnrB −/− model of HSCR/HAEC to demonstrate that survival could be extended to 36 days by changing to a liquid diet and the addition of oral antibiotics, further supporting a role for the microbiome in the development of HAEC [17].
Approaches to HAEC using genomics have also contributed to knowledge about alterations in the microbiome of HAEC patients. DeFilippo et al. used amplified ribosomal DNA restriction analysis to demonstrate distinct changes in the microbiota of a single child as he progressed from pre-enterocolitis through the acute episode and onto resolution [21]. Yan et al. used this technique in two patients with HAEC and two without and found different bacterial clustering in the patients with HAEC as compared to those without [95]. Recent studies are beginning to investigate a potential role for alterations in the fungal communities of the gut and their contribution to HAEC pathogenesis [29].
13.2.6 Summary
Impaired mucosal immunity, abnormal microbiota, intestinal barrier dysfunction, and dysmotility all appear to contribute to the pathogenesis of HAEC. ENS dysfunction can result in microbiome dysbiosis through impaired motility. When followed by impaired intestinal barrier function and an abnormal immune response, HAEC develops. This stepwise model is the target of current research endeavors by multiple groups (Fig. 13.1).
13.3 Risk Factors
Many risk factors for HAEC have been identified. These factors include delay in the initial diagnosis of HSCR, gender, a family history of HSCR, and the presence of trisomy 21. Delays in the diagnosis of HSCR lead to a higher incidence of enterocolitis as the presenting condition [79]. In the neonatal period, the incidence of HAEC increases from 11% in the first week of life to 24% after.
The best-established risk factor for HAEC is trisomy 21 [14, 65, 79]. Patients with Down syndrome have been shown to have almost double the incidence of HAEC compared to other children with HSCR. The combination of HSCR and trisomy 21 is associated with a higher incidence of postoperative morbidity, prolonged hospitalization, and poor long-term bowel function. Infants with trisomy 21 have an intrinsic immune deficiency due to both decreased cytotoxic T lymphocytes and derangement in humoral function [56] which may explain their increased risk of HAEC. Of patients with trisomy 21, ~50% develop HAEC as opposed to 29% in the normal population [53, 65].
Other risk factors include family history of HSCR, male sex, delay in diagnosis of HSCR, and other genetic syndromes. There is growing evidence that genetic mutations may have a role in predisposition to HAEC: one study noted that 2/3 patients with HAEC had variants of integrin-β2, which is involved in cell surface-mediated signaling and has been associated with chronic colitis conditions [55]. Some have also postulated that the occurrence of a single episode of HAEC can alter intrinsic intestinal immunity leading to an increased risk of further episodes [24].
There has been conflicting evidence on whether or not the length of disease is related to recurrent HAEC, with longer disease involvement postulated to have a higher rate of recurrence [11, 24, 26, 43]. Studies have shown that HAEC is significantly more common in patients with aganglionic segments longer than the sigmoid [24, 43]. Neonates with total colonic aganglionosis may present with perforation of the ganglionic bowel. However, some studies on this condition have found no difference as regards length of the aganglionic bowel [11, 14, 26].
There is no evidence that the type of pull-through or presence of stoma after pull-through is related to the incidence of postoperative HAEC [64]. Swenson reported an HAEC incidence of 21% after pull-through in a 40-year follow-up [67]. However, Wildhaber et al. demonstrated no correlation between the incidence of HAEC and the type of pull-through performed [90]. Others have noted similar findings [64, 84, 89]. Additionally, no increase in HAEC has been found in the postoperative period after a primary pull-through without stoma formation [15].
After pull-through surgery, known risk factors for HAEC include anastomotic leak or stricture and postoperative intestinal obstruction secondary to adhesive disease. These increase the relative risk of HAEC by nearly threefold [36, 77]. Finally, although HAEC does occur with a diverting colostomy/enterostomy, its incidence appears substantially lower.
13.4 Diagnosis
The presentation of HAEC is highly variable in both symptoms and severity [35]. Due to the difficulty in making a definitive diagnosis and potential for morbidity or mortality with late diagnosis and treatment, most practitioners make a presumptive diagnosis and initiate therapy. Classic manifestations include abdominal distension, fever, and diarrhea. The broad spectrum of presentations is nonspecific, however, and likely contributes to the variable incidence of HAEC observed in the literature.
Mild cases may present with fever, mild distension, and diarrhea, mimicking viral gastroenteritis. More severe cases may include lethargy, rectal bleeding, and obstipation. In the neonate, the classical presentation consists of a history of constipation from birth associated with occasional loose foul-smelling stools and progressive abdominal distension [24, 30]. Among neonates with HSCR, 16%–33% present with diarrhea. The presence of diarrhea is pathognomonic of enterocolitis which occurs in 93% of patients with HAEC. Vomiting rarely occurs in HAEC. A markedly distended hyperresonant abdomen occurs in 32%–83%, vomiting in 9%–76%, pyrexia in 12%–54%, and less commonly rectal bleeding in 5%–9% of patients with HAEC.
Rectal examination, either by digit or soft catheter, is both diagnostic and therapeutic, resulting in a characteristically explosive foul smelly stool and gaseous decompression which once witnessed is never forgotten. Patients after a pull-through operation or those with a diverting stoma will present in the same fashion. The significant morbidity associated with HAEC occurs with the toxic megacolon which is characterized by bilious vomiting, fever, dehydration, marked abdominal distension, and signs of shock. Fortunately, bowel perforation is a rare complication occurring in only 2%–3% of patients [24].
Current diagnostic practice involves excluding other causes of colitis such as necrotizing enterocolitis in the infant and infectious colitis in older children. Stool studies and Clostridium difficile testing can be helpful to rule out the latter. Although in the majority of patients the diagnosis can be made easily on clinical evaluation, certain radiographic findings have been associated with HAEC in the context of a suspicious clinical history (Fig. 13.2). Simple anterior-posterior and lateral decubitus abdominal radiographs can show thickening of the bowel wall, mucosal irregularity (“sawtooth” appearance), dilated bowel loops, air-fluid levels, “cutoff” sign in the rectosigmoid colon, pneumatosis, pneumoperitoneum, and evidence of toxic megacolon (grossly dilated colonic loop) (Fig. 13.3). Contrast enema should be avoided during episodes of HAEC due to the risk of perforation.
Contrast enema characteristics of Hirschsprung disease and Hirschsprung-associated enterocolitis. Contrast enema demonstrating loss of the normal rectosigmoid ratio, where the sigmoid is expected to be larger in diameter than the rectum, in Hirschsprung disease. Also note colonic distension, speculation, edema, and mucosal nodularity (“sawtooth” appearance) of the distal rectum, indicative of active enterocolitis. Contrast enemas should be avoided during episodes of HAEC due to the risk of perforation
A major barrier in the care of Hirschsprung patients has been the lack of a standardized method for diagnosing enterocolitis. In 2009, a large group of gastroenterologists and surgeons participated in a Delphi process to generate a diagnostic scoring system for HAEC [20, 60]. Using history, physical exam findings, laboratory findings, and imaging, they arrived at a 16-item list. Each item was assigned 1–2 points, with a summed score of 10 or greater being diagnostic of HAEC. Despite multidisciplinary expert input into the development of this definition, it was not designed for and has not been put into widespread clinical use. Recently, another collaborative reviewed the medical records of 116 children across 5 centers using the 16 Delphi criteria to create a more clinically useful scoring system [28]. The most common positive criteria included distended abdomen (31%), diarrhea with explosive stool (24%), diarrhea with foul-smelling stool (23%), and lethargy (19.8%). On multivariate analysis, diarrhea with explosive stool, decreased peripheral perfusion, lethargy, and dilated loops of bowel were independently associated with suspected HAEC episodes. Based on the calculated sensitivities and specificities for each score point, they demonstrated that a cutoff score of 4 points maximized the sensitivity (83.7%) and specificity (98.6%) in diagnosing HAEC. Using the same patient cohort, they then devised a new risk score based on these four criteria. However, this scoring system has not yet been prospectively verified.
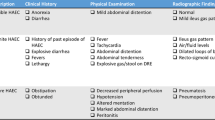
The American Pediatric Surgery Association’s (APSA) Hirschsprung Disease Interest Group also proposed a staging system for HAEC [35]. This system classifies HAEC into three stages based on many of the same history, physical exam, and radiologic features and is aimed toward aiding in both the diagnosis and management of HAEC (Table 13.1). However, it is hampered by the same primary weakness of the Delphi criteria – it relied on expert opinion in its development. There is an ongoing need to establish an evidence-based diagnosis and grading system for HAEC.
13.5 Treatment
There is currently no evidence-based, standard-of-care guideline or algorithm for the treatment of HAEC. Therapy is nonspecific and aimed at treating symptoms rather than a known etiology. Fluid resuscitation and correction of electrolyte abnormalities are critical in initial management. Additional management strategies may include dietary changes, antibiotics, rectal irrigations, and intensive care unit admission.
13.5.1 Acute Illness
Treatment regimens should be tailored to the providers’ clinical judgment of the severity of disease. The APSA HSCR interest group published guideline for the treatment of HAEC based on their diagnostic guidelines (Table 13.2) [35]. Three grades of disease severity are defined as suspected HAEC (grade 1), definite HAEC (grade 2), and severe HAEC (grade 3).
The APSA guidelines recommend that a patient with grade 1 HAEC may be safely treated as an outpatient with oral metronidazole and oral hydration. The optimal dosing, frequency, and duration of antibiotics for HAEC have not been determined. Rectal irrigations (washouts) can be considered in patients with abdominal distension or incomplete evacuation. Shim and Swenson recommended the use of a flatus or rectal tube to enable colonic decompression [68]. Rectal washouts are performed using a large-bore soft catheter with multiple side holes. The tube is well lubricated and advanced into the colon. In preoperative HAEC, the tube should be passed into the transition zone if technically possible. Repeated tube decompression and gentle rectal washouts with 10 mL/kg aliquots of warm or room-temperature normal saline make a significant clinical impact on these patients.
For grade 2 cases, inpatient or outpatient management is left to the provider’s clinical judgment. Dietary restriction options include clear liquids or nothing by mouth. Broad-spectrum antibiotics and rectal irrigations/washouts are recommended.
Patients with severe cases of HAEC (grade 3) should be strongly considered for intensive care unit admission, bowel rest, broad-spectrum antibiotics, and rectal irrigations. These patients may require proximal diversion if there is failure to improve with nonoperative management. Clinical deterioration in the neonate, particularly those with long-segment disease, in which washouts have a high failure rate, may require an emergency decompression and diversion.
13.5.2 Recurrent HAEC
Treatment of recurrent HAEC begins with identifying the underlying cause. The workup for underlying etiology begins with assessing for causes of obstructive symptoms [46]. Anatomic etiologies can be identified with contrast enema, physical examination under anesthesia, and rectal biopsies to confirm the presence of ganglionated bowel. Anatomic abnormalities such as anastomotic stricture, transition zone pull-through, or Duhamel spur should be treated surgically. Redo pull-through operations when appropriate appear to be as effective as primary procedures in terms of continence and stooling frequency and can decrease episodes of HAEC [78].
After excluding anatomic etiologies, non-relaxation of the internal anal sphincter should be considered. The use of botulinum injections for the treatment of postoperative HAEC has shown some promising results. In one study, 14 of 18 patients with persistent constipation, obstructive symptoms, or recurrent HAEC showed improvement in bowel function, and 5 of these had improvement that lasted longer than 6 months [54]. Multiple studies have shown a reduction in hospitalizations for HAEC following botulinum injections [61]. However, it is difficult to predict which patients will respond, and long-term outcomes have not been well studied.
Posterior myotomy/myectomy (POMM) can also be considered in children with recurrent episodes of HAEC 1–2 years after pull-through operation [19]. Although there has been some success in small trials, there have been mixed results regarding functional outcomes [40, 48, 64, 89]. An advantage to POMM is that redo pull-through can still be performed in the event that myectomy is not successful. Finally, end ileostomy or colostomy (diversion) can be considered as a last resort.
13.5.3 Prophylactic Measures
After pull-through surgery, some surgeons recommend routine anal dilations. Gao et al. reported an enterocolitis rate of 2/34 (6%) after using routine dilations for 3 months after surgery [33]. However, recent data questions these findings. A review by Temple et al. compared rates of stricture development and enterocolitis among children with HSCR and anorectal malformation undergoing either weekly calibration of the anastomosis by a surgeon or daily dilation by parents and observed no differences [80]. A separate review of HSCR patients had similar findings [7].
Concerns over the mortality rate due to fulminant enterocolitis in the postoperative period led Marty et al. to suggest routine postoperative rectal washout to decrease both the incidence and the severity of episodes of enterocolitis following definitive surgery [50]. They recommend a policy of rectal irrigation performed by the parents commencing 2 weeks following surgery twice daily for 3 months followed by once daily for 3 months. This policy reduced their incidence of HAEC from 36% (34 of 95 patients) to 10% (4 of 40 patients). A Spanish study of 37 children with HSCR treated between 1978 and 2005 found similar results [58].
Further research is needed to investigate what role probiotics might play in the prevention of HAEC. In one study, children undergoing surgery for HSCR were randomized to probiotic versus placebo postoperatively; this study did not show differences in HAEC rates between the two groups [23]. In contrast, another group similarly randomized patients and treated them for 4 weeks [85]. The probiotic group had reduced incidence and severity of HAEC over the following 3 months. A recent meta-analysis concluded that probiotics do not reduce the risk of HAEC [57].
13.6 Conclusion and Future Directions
HAEC remains a diagnostic and therapeutic challenge, despite recent advances in our understanding of the pathophysiology. Current research is focusing on a number of avenues including patient-specific microbiome analysis and targeted probiotic therapy and use of stem cell therapy to restore bowel function in HSCR [41]. Further studies on the underlying mechanisms of disease, accurate methods of diagnosis, and optimal treatment strategies will be needed in order to improve our ability to care for HSCR patients with HAEC.
References
Akkary S, Sahwy E, Kandil W, Hamdy MH. A histochemical study of the mucosubstances of the colon in cases of Hirschsprung’s disease with and without enterocolitis. J Pediatr Surg. 1981;16(5):664–8.
Albanese CT, Smith SD, Watkins S, Kurkchubasche A, Simmons RL, Rowe MI. Effect of secretory IgA on transepithelial passage of bacteria across the intact ileum in vitro. J Am Coll Surg. 1994;179(6):679–88.
Ament ME, Bill AH. Persistent diarrhea due to sucrase-isomaltase deficiency in a postoperative child with Hirschsprung’s disease. J Pediatr Surg. 1973;8(4):543–5.
Amiel J, Sproat-Emison E, Garcia-Barcelo M, Lantieri F, Burzynski G, Borrego S, Pelet A, Arnold S, Miao X, Griseri P, Brooks AS, Antinolo G, de Pontual L, Clement-Ziza M, Munnich A, Kashuk C, West K, Wong KK-Y, Lyonnet S, Chakravarti A, Tam PK-H, Ceccherini I, Hofstra RMW, Fernandez R, Hirschsprung Disease Consortium. Hirschsprung disease, associated syndromes and genetics: a review. J Med Genet. 2008;45(1):1–14.
Aslam A, Spicer RD, Corfield AP. Turnover of radioactive mucin precursors in the colon of patients with Hirschsprung’s disease correlates with the development of enterocolitis. J Pediatr Surg. 1998;33(1):103–5.
Austin KM. The pathogenesis of Hirschsprung’s disease-associated enterocolitis. Semin Pediatr Surg. 2012;21(4):319–27.
Aworanti O, Hung J, McDowell D, Martin I, Quinn F. Are routine dilatations necessary post pull-through surgery for Hirschsprung disease? Eur J Pediatr Surg. 2013;23(5):383–8.
Bagwell CE, Langham MR Jr, Mahaffey SM, Talbert JL, Shandling B. Pseudomembranous colitis following resection for Hirschsprung’s disease. J Pediatr Surg. 1992;27(10):1261–4.
Berry CL, Fraser GC. The experimental production of colitis in the rabbit with particular reference to Hirschsprung’s disease. J Pediatr Surg. 1968;3(1):36–42.
Bickelhaupt S, Pazahr S, Chuck N, Blume I, Froehlich JM, Cattin R, Raible S, Bouquet H, Bill U, Rogler G, Frei P, Boss A, Patak MA. Crohn’s disease: small bowel motility impairment correlates with inflammatory-related markers C-reactive protein and calprotectin. Neurogastroenterol Motil. 2013;25(6):467–73.
Bill A, CHapman N. The enterocolitis of Hirschsprung’s disease: its natural history and treatment. Am J Surg. 1962;103:70–4.
Buisine MP, Devisme L, Savidge TC, Gespach C, Gosselin B, Porchet N, Aubert JP. Mucin gene expression in human embryonic and fetal intestine. Gut. 1998;43(4):519–24.
Burnard ED. Hirschsprung’s disease in infancy. Br Med J. 1950;1(4646):151–6.
Caniano DA, Teitelbaum DH, Qualman SJ. Management of Hirschsprung’s disease in children with trisomy 21. Am J Surg. 1990;159(4):402–4.
Carcassonne M, Guys JM, Morrison-Lacombe G, Kreitmann B. Management of Hirschsprung’s disease: curative surgery before 3 months of age. J Pediatr Surg. 1989;24(10):1032–4.
Cheng LS, Schwartz DM, Hotta R, Graham HK, Goldstein AM. Bowel dysfunction following pullthrough surgery is associated with an overabundance of nitrergic neurons in Hirschsprung disease. J Pediatr Surg. 2016;51(11):1834–8.
Cheng Z, Dhall D, Zhao L, Wang HL, Doherty TM, Bresee C, Frykman PK. Murine model of Hirschsprung-associated enterocolitis. I: phenotypic characterization with development of a histopathologic grading system. J Pediatr Surg. 2010;45(3):475–82.
Cheng Z, Wang X, Dhall D, Zhao L, Bresee C, Doherty TM, Frykman PK. Splenic lymphopenia in the endothelin receptor B-null mouse: implications for Hirschsprung associated enterocolitis. Pediatr Surg Int. 2011;27(2):145–50.
Coran AG, Teitelbaum DH. Recent advances in the management of Hirschsprung’s disease. Am J Surg. 2000;180(5):382–7.
Dalkey N, Helmer O. An experimental application of the Delphi method to the use of experts. Manag Sci. 1963;9(3):458–67.
De Filippo C, Pini-Prato A, Mattioli G, Avanzini S, Rapuzzi G, Cavalieri D, Di Paola M, Stefanini I, Ceccherini I, Mavilio D, Lionetti P, Jasonni V. Genomics approach to the analysis of bacterial communities dynamics in Hirschsprung’s disease-associated enterocolitis: a pilot study. Pediatr Surg Int. 2010;26(5):465–71.
Dorman GW. Hirschsprung’s disease; a lethal problem in early infancy. AMA Arch Surg. 1957;75(6):906–13.
El-Sawaf M, Siddiqui S, Mahmoud M, Drongowski R, Teitelbaum DH. Probiotic prophylaxis after pullthrough for Hirschsprung disease to reduce incidence of enterocolitis: a prospective, randomized, double-blind, placebo-controlled, multicenter trial. J Pediatr Surg. 2013;48(1):111–7.
Elhalaby EA, Coran AG, Blane CE, Hirschl RB, Teitelbaum DH. Enterocolitis associated with Hirschsprung’s disease: a clinical-radiological characterization based on 168 patients. J Pediatr Surg. 1995;30(1):76–83.
Fisher JH, Swenson O. Hirschsprung’s disease during infancy. Surg Clin North Am. 1956:1511–5.
Foster P, Cowan G, Wrenn EL. Twenty-five years’ experience with Hirschsprung’s disease. J Pediatr Surg. 1990;25(5):531–4.
Frykman PK, Cheng Z, Wang X, Dhall D. Enterocolitis causes profound lymphoid depletion in endothelin receptor B- and endothelin 3-null mouse models of Hirschsprung-associated enterocolitis. Eur J Immunol. 2015a;45(3):807–17.
Frykman PK, Kim S, Wester T, Nordenskjöld A, Kawaguchi A, Hui TT, Teitelbaum DH, Granström AL, Rogatko A, HAEC Collaborative Research Group (HCRG). Critical evaluation of the Hirschsprung-associated enterocolitis (HAEC) score: a multicenter study of 116 children with Hirschsprung disease. J Pediatr Surg. 2018;53(4):708–17.
Frykman PK, Nordenskjold A, Kawaguchi A, Hui TT, Granstrom AL, Cheng Z, Tang J, Underhill DM, Iliev I, Funari VA, Wester T, H. C. R. Group. Characterization of bacterial and fungal microbiome in children with Hirschsprung disease with and without a history of Enterocolitis: a multicenter study. PLoS One. 2015b;10(4):e0124172.
Frykman PK, Short SS. Hirschsprung-associated enterocolitis: prevention and therapy. Semin Pediatr Surg. 2012;21(4):328–35.
Fujimoto T. Natural history and pathophysiology of enterocolitis in the piebald lethal mouse model of Hirschsprung’s disease. J Pediatr Surg. 1988a;23(3):237–42.
Fujimoto T, Reen DJ, Puri P. Inflammatory response in enterocolitis in the piebald lethal mouse model of Hirschsprung’s disease. Pediatr Res. 1988;24(2):152–5.
Gao Y, Li G, Zhang X, Xu Q, Guo Z, Zheng B, Li P, Li G. Primary transanal rectosigmoidectomy for Hirschsprung’s disease: preliminary results in the initial 33 cases. J Pediatr Surg. 2001;36(12):1816–9.
Gosain A, Barlow-Anacker AJ, Erickson CS, Pierre JF, Heneghan AF, Epstein ML, Kudsk KA. Impaired cellular immunity in the murine neural crest conditional deletion of Endothelin receptor-B model of Hirschsprung’s disease. PLoS One. 2015;10(6):e0128822.
Gosain A, Frykman PK, Cowles RA, Horton J, Levitt M, Rothstein DH, Langer JC, Goldstein AM, American Pediatric Surgical Association Hirschsprung Disease Interest Group. Guidelines for the diagnosis and management of Hirschsprung-associated enterocolitis. Pediatr Surg Int. 2017;33(5):517–21.
Hackam DJ, Filler RM, Pearl RH. Enterocolitis after the surgical treatment of Hirschsprung’s disease: risk factors and financial impact. J Pediatr Surg. 1998;33(6):830–3.
Hardy SP, Bayston R, Spitz L. Prolonged carriage of Clostridium difficile in Hirschsprung’s disease. Arch Dis Child. 1993;69(2):221–4.
Haricharan RN, Seo J-M, Kelly DR, Mroczek-Musulman EC, Aprahamian CJ, Morgan TL, Georgeson KE, Harmon CM, Saito JM, Barnhart DC. Older age at diagnosis of Hirschsprung disease decreases risk of postoperative enterocolitis, but resection of additional ganglionated bowel does not. J Pediatr Surg. 2008;43(6):1115–23.
Harrison MW, Deitz DM, Campbell JR, Campbell TJ. Diagnosis and management of Hirschsprung’s disease. A 25 year perspective. Am J Surg. 1986;152(1):49–56.
Heikkinen M, Rintala R, Luukkonen P. Long-term anal sphincter performance after surgery for Hirschsprung’s disease. J Pediatr Surg. 1997;32(10):1443–6.
Heuckeroth RO. Hirschsprung disease – integrating basic science and clinical medicine to improve outcomes. Nat Rev Gastroenterol Hepatol. 2018;15(3):152–67.
Hirschsprung H. Stuhltragheit neugeborener infolge von dilatation and hypertrophies des colons. Jahrb Kinderheilkd. 1887;27:1–42.
Ikeda K, Goto S. Diagnosis and treatment of Hirschsprung’s disease in Japan. An analysis of 1628 patients. Ann Surg. 1984;199(4):400–5.
Imamura A, Puri P, O’Briain DS, Reen DJ. Mucosal immune defence mechanisms in enterocolitis complicating Hirschsprung’s disease. Gut. 1992;33(6):801–6.
Kobayashi H, Hirakawa H, Puri P. Overexpression of intercellular adhesion molecule-1 (ICAM-1) and MHC class II antigen on hypertrophic nerve trunks suggests an immunopathologic response in Hirschsprung’s disease. J Pediatr Surg. 1995;30(12):1680–3.
Langer JC, Rollins MD, Levitt M, Gosain A, Torre L, Kapur RP, Cowles RA, Horton J, Rothstein DH, Goldstein AM. American Pediatric Surgical Association Hirschsprung Disease Interest Group. Guidelines for the management of postoperative obstructive symptoms in children with Hirschsprung disease. Pediatr Surg Int. 2017;33(5):523–6.
Lloyd-Still JD, Demers LM. Hirschsprung’s enterocolitis, prostaglandins, and response to cholestyramine. J Pediatr Surg. 1978;13(4):417–8.
Marty TL, Matlak ME, Hendrickson M, Black RE, Johnson DG. Unexpected death from enterocolitis after surgery for Hirschsprung’s disease. Pediatrics. 1995;96(1 Pt 1):118–21.
Marty TL, Seo T, Matlak ME, Sullivan JJ, Black RE, Johnson DG. Gastrointestinal function after surgical correction of Hirschsprung’s disease: long-term follow-up in 135 patients. J Pediatr Surg. 1995;30(5):655–8.
Marty TL, Seo T, Sullivan JJ, Matlak ME, Black RE, Johnson DG. Rectal irrigations for the prevention of postoperative enterocolitis in Hirschsprung’s disease. J Pediatr Surg. 1995;30(5):652–4.
Mattar AF, Coran AG, Teitelbaum DH. MUC-2 mucin production in Hirschsprung’s disease: possible association with enterocolitis development. J Pediatr Surg. 2003;38(3):417–21; discussion 417-421
Medrano G, Cailleux F, Guan P, Kuruvilla K, Barlow-Anacker AJ, Gosain A. B-lymphocyte-intrinsic and -extrinsic defects in secretory immunoglobulin A production in the neural crest-conditional deletion of endothelin receptor B model of Hirschsprung-associated enterocolitis. FASEB J. 2019:fj201801913R. https://doi.org/10.1096/fj.201801913R.
Menezes M, Puri P. Long-term clinical outcome in patients with Hirschsprung’s disease and associated Down’s syndrome. J Pediatr Surg. 2005;40(5):810–2.
Minkes RK, Langer JC. A prospective study of botulinum toxin for internal anal sphincter hypertonicity in children with Hirschsprung’s disease. J Pediatr Surg. 2000;35(12):1733–6.
Moore SW, Sidler D, Zaahl MG. The ITGB2 immunomodulatory gene (CD18), enterocolitis, and Hirschsprung’s disease. J Pediatr Surg. 2008;43(8):1439–44.
Nair MP, Schwartz SA. Association of decreased T-cell-mediated natural cytotoxicity and interferon production in Down’s syndrome. Clin Immunol Immunopathol. 1984;33(3):412–24.
Nakamura H, Lim T, Puri P. Probiotics for the prevention of Hirschsprung-associated enterocolitis: a systematic review and meta-analysis. Pediatr Surg Int. 2018;34(2):189–93.
Nunez R, Torres A, Agulla E, Moreno C, Marin D, Santamaria JI. Rectal irrigation and bowel decontamination for the prevention of postoperative enterocolitis in Hirschsprung’s disease. Cir Pediatr. 2007;20(2):96–100.
Ohama T, Hori M, Fujisawa M, Kiyosue M, Hashimoto M, Ikenoue Y, Jinno Y, Miwa H, Matsumoto T, Murata T, Ozaki H. Downregulation of CPI-17 contributes to dysfunctional motility in chronic intestinal inflammation model mice and ulcerative colitis patients. J Gastroenterol. 2008;43(11):858–65.
Pastor AC, Osman F, Teitelbaum DH, Caty MG, Langer JC. Development of a standardized definition for Hirschsprung’s-associated enterocolitis: a Delphi analysis. J Pediatr Surg. 2009;44(1):251–6.
Patrus B, Nasr A, Langer JC, Gerstle JT. Intrasphincteric botulinum toxin decreases the rate of hospitalization for postoperative obstructive symptoms in children with Hirschsprung disease. J Pediatr Surg. 2011;46(1):184–7.
Pierre JF, Barlow-Anacker AJ, Erickson CS, Heneghan AF, Leverson GE, Dowd SE, Epstein ML, Kudsk KA, Gosain A. Intestinal dysbiosis and bacterial enteroinvasion in a murine model of Hirschsprung’s disease. J Pediatr Surg. 2014;49(8):1242–51.
Pini-Prato A, Rossi V, Avanzini S, Mattioli G, Disma N, Jasonni V. Hirschsprung’s disease: what about mortality? Pediatr Surg Int. 2011;27(5):473–8.
Polley TZ, Coran AG, Wesley JR. A ten-year experience with ninety-two cases of Hirschsprung’s disease. Including sixty-seven consecutive endorectal pull-through procedures. Ann Surg. 1985a;202(3):349–55.
Quinn FM, Surana R, Puri P. The influence of trisomy 21 on outcome in children with Hirschsprung’s disease. J Pediatr Surg. 1994;29(6):781–3.
Rescorla FJ, Morrison AM, Engles D, West KW, Grosfeld JL. Hirschsprung’s disease. Evaluation of mortality and long-term function in 260 cases. Arch Surg. 1992;127(8):934–41; discussion 941–932
Sherman JO, Snyder ME, Weitzman JJ, Jona JZ, Gillis DA, O’Donnell B, Carcassonne M, Swenson O. A 40-year multinational retrospective study of 880 Swenson procedures. J Pediatr Surg. 1989;24(8):833–8.
Shim WK, Swenson O. Treatmentof congenital megacolon in 50 infants. Pediatrics. 1966;38(2):185–93.
Soeda J, O’Briain DS, Puri P. Mucosal neuroendocrine cell abnormalities in the colon of patients with Hirschsprung’s disease. J Pediatr Surg. 1992;27(7):823–7.
Soeda J, O’Briain DS, Puri P. Regional reduction in intestinal neuroendocrine cell populations in enterocolitis complicating Hirschsprung’s disease. J Pediatr Surg. 1993;28(8):1063–8.
Spiller RC. Role of nerves in enteric infection. Gut. 2002;51(6):759–62.
Suita S, Taguchi T, Ieiri S, Nakatsuji T. Hirschsprung’s disease in Japan: analysis of 3852 patients based on a nationwide survey in 30 years. J Pediatr Surg. 2005;40(1):197–201; discussion 201-192
Swenson O. Hirschsprung’s disease—a complicated therapeutic problem: some thoughts and solutions based on data and personal experience over 56 years. J Pediatr Surg. 2004;39(10):1449–53.
Swenson O, Davidson FZ. Similarities of mechanical intestinal obstruction and aganglionic megacolon in the newborn infant: a review of 64 cases. N Engl J Med. 1960;262:64–7.
Swenson O, Fisher JH, Scott JE. Diarrhea following rectosigmoidectomy for Hirschsprung’s disease. Surgery. 1960;48:419–21.
Teitelbaum DH, Caniano DA, Qualman SJ. The pathophysiology of Hirschsprung’s-associated enterocolitis: importance of histologic correlates. J Pediatr Surg. 1989;24(12):1271–7.
Teitelbaum DH, Cilley RE, Sherman NJ, Bliss D, Uitvlugt ND, Renaud EJ, Kirstioglu I, Bengston T, Coran AG. A decade of experience with the primary pull-through for hirschsprung disease in the newborn period: a multicenter analysis of outcomes. Ann Surg. 2000;232(3):372–80.
Teitelbaum DH, Drongowski RA, Chamberlain JN, Coran AG. Long-term stooling patterns in infants undergoing primary endorectal pull-through for Hirschsprung’s disease. J Pediatr Surg. 1997;32(7):1049–52; discussion 1052-1043
Teitelbaum DH, Qualman SJ, Caniano DA. Hirschsprung’s disease. Identification of risk factors for enterocolitis. Ann Surg. 1988;207(3):240–4.
Temple SJ, Shawyer A, Langer JC. Is daily dilatation by parents necessary after surgery for Hirschsprung disease and anorectal malformations? J Pediatr Surg. 2012;47(1):209–12.
Thiagarajah JR, Yildiz H, Carlson T, Thomas AR, Steiger C, Pieretti A, Zukerberg LR, Carrier RL, Goldstein AM. Altered goblet cell differentiation and surface mucus properties in Hirschsprung disease. PLoS One. 2014;9(6):e99944.
Thomas DF, Fernie DS, Bayston R, Spitz L, Nixon HH. Enterocolitis in Hirschsprung’s disease: a controlled study of the etiologic role of Clostridium difficile. J Pediatr Surg. 1986;21(1):22–5.
Thomas DF, Fernie DS, Malone M, Bayston R, Spitz L. Association between Clostridium difficile and enterocolitis in Hirschsprung’s disease. Lancet. 1982;1(8263):78–9.
van Leeuwen K, Teitelbaum DH, Elhalaby EA, Coran AG. Long-term follow-up of redo pull-through procedures for Hirschsprung’s disease: efficacy of the endorectal pull-through. J Pediatr Surg. 2000;35(6):829–33; discussion 833-824
Wang X, Li Z, Xu Z, Wang Z, Feng J. Probiotics prevent Hirschsprung’s disease-associated enterocolitis: a prospective multicenter randomized controlled trial. Int J Color Dis. 2015;30(1):105–10.
Ward NL, Pieretti A, Dowd SE, Cox SB, Goldstein AM. Intestinal aganglionosis is associated with early and sustained disruption of the colonic microbiome. Neurogastroenterol Motil. 2012;24(9):874–e400.
Webster W. Aganglionic megacolon in piebald-lethal mice. Arch Pathol. 1974;97(2):111–7.
Wiedenmann B, Waldherr R, Buhr H, Hille A, Rosa P, Huttner WB. Identification of gastroenteropancreatic neuroendocrine cells in normal and neoplastic human tissue with antibodies against synaptophysin, chromogranin a, secretogranin I (chromogranin B), and secretogranin II. Gastroenterology. 1988;95(5):1364–74.
Wildhaber BE, Pakarinen M, Rintala RJ, Coran AG, Teitelbaum DH. Posterior myotomy/myectomy for persistent stooling problems in Hirschsprung’s disease. J Pediatr Surg. 2004;39(6):920–6; discussion 920–926
Wildhaber BE, Teitelbaum DH, Coran AG. Total colonic Hirschsprung’s disease: a 28-year experience. J Pediatr Surg. 2005;40(1):203–6; discussion 206-207
Wiles TJ, Jemielita M, Baker RP, Schlomann BH, Logan SL, Ganz J, Melancon E, Eisen JS, Guillemin K, Parthasarathy R. Host gut motility promotes competitive exclusion within a model intestinal microbiota. PLoS Biol. 2016;14(7):e1002517.
Wilson-Storey D, Scobie WG. Impaired gastrointestinal mucosal defense in Hirschsprung’s disease: a clue to the pathogenesis of enterocolitis? J Pediatr Surg. 1989;24(5):462–4.
Wilson-Storey D, Scobie WG, McGenity KG. Microbiological studies of the enterocolitis of Hirschsprung’s disease. Arch Dis Child. 1990;65(12):1338–9.
Wilson-Storey D, Scobie WG, Raeburn JA. Defective white blood cell function in Hirschsprung’s disease: a possible predisposing factor to enterocolitis. J R Coll Surg Edinb. 1988;33(4):185–8.
Yan Z, Poroyko V, Gu S, Zhang Z, Pan L, Wang J, Bao N, Hong L. Characterization of the intestinal microbiome of Hirschsprung’s disease with and without enterocolitis. Biochem Biophys Res Commun. 2014;445(2):269–74.
Zaitoun I, Erickson CS, Barlow AJ, Klein TR, Heneghan AF, Pierre JF, Epstein ML, Gosain A. Altered neuronal density and neurotransmitter expression in the ganglionated region of Ednrb null mice: implications for Hirschsprung’s disease. Neurogastroenterol Motil. 2013;25(3):e233–44.
Zhao L, Dhall D, Cheng Z, Wang HL, Doherty TM, Bresee C, Frykman PK. Murine model of Hirschsprung-associated enterocolitis II: surgical correction of aganglionosis does not eliminate enterocolitis. J Pediatr Surg. 2010;45(1):206–11; discussion 211-202
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Veras, L.V., Gosain, A. (2019). Hirschsprung-Associated Enterocolitis. In: Puri, P. (eds) Hirschsprung's Disease and Allied Disorders. Springer, Cham. https://doi.org/10.1007/978-3-030-15647-3_13
Download citation
DOI: https://doi.org/10.1007/978-3-030-15647-3_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-15646-6
Online ISBN: 978-3-030-15647-3
eBook Packages: MedicineMedicine (R0)