Abstract
Posttraumatic stress disorder (PTSD) is a mental disorder that sometimes develops after exposure to a life-threatening, psychologically traumatic event. Reflecting empirical advances relevant to the neurobiology and cognitive neuroscience of PTSD, this chapter will focus on PTSD as a neurobehavioral syndrome. We begin by describing PTSD, including a brief review of its clinical presentation and underlying neuropathology. We next review the neurocognitive characteristics of the disorder, common neuropsychological approaches to its assessment, and key clinical considerations in conducting neuropsychological evaluations when PTSD is a possible diagnosis. The chapter additionally addresses treatment implications, concluding with family and social considerations.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Posttraumatic stress disorder (PTSD) is a mental disorder that sometimes develops after exposure to a life-threatening, psychologically traumatic event. Reflecting empirical advances relevant to the neurobiology and cognitive neuroscience of PTSD, this chapter will focus on PTSD as a neurobehavioral syndrome. We begin by describing PTSD, including a brief review of its clinical presentation and underlying neuropathology. We next review the neurocognitive characteristics of the disorder, common neuropsychological approaches to its assessment, and key clinical considerations in conducting neuropsychological evaluations when PTSD is a possible diagnosis. The chapter additionally addresses treatment implications, concluding with family and social considerations.
Description of the Disorder
Diagnostic Criteria and Prevalence
Although numerous psychosocial and biological factors increase the risk of developing PTSD following exposure to a psychologically traumatic event [1,2,3,4,5], PTSD is unique among psychiatric disorders in that the diagnosis cannot be made without exposure to an environmental event (i.e., the trauma event). The fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) [6] defines a traumatic event as one in which a person “experienced, witnessed, or was confronted with an event or events that involved actual or threatened death or serious injury, or a threat to the physical integrity of self or others” (Criterion A1) and had a subjective response that involved “intense fear, helplessness, or horror” in adults or “disorganized or agitated behavior” in children (Criterion A2). Epidemiological studies indicate that at least one of every two Americans (ages 15–54) have been exposed over the course of their lifetimes to a psychologically traumatic event and the majority of those exposed have faced two or more traumas in their lifetime [7].
As defined by DSM-IV, symptoms are grouped into three symptom criteria: (1) reexperiencing of the traumatic event (e.g., nightmares, physiological and emotional responsivity to trauma reminders); (2) avoidance of external reminders or thoughts associated with the trauma and numbing of general responsiveness (e.g., inability to have loving feelings); and (3) hyperarousal (e.g., concentration impairment, hypervigilance to threat, difficulty in sleeping). Factor analytic studies, however, suggest that a four-factor solution in which avoidance symptoms are separated from numbing and other symptoms may be more appropriate [8, 9]. DSM-IV additionally requires that symptoms endure for at least 1 month and cause clinically significant distress or functional impairment. Despite the frequency of trauma exposure, only about 25% of individuals confronted with trauma develop core PTSD symptoms [10]. The lifetime prevalence of PTSD among US adults has been estimated to be 6.8% [7]. Not surprisingly, prevalence is higher in at-risk populations such as combat veterans [11,12,13,14], inner-city children [15], and mass violence survivors [16].
Course and Associated Clinical Features
Course. PTSD typically begins with symptom emergence immediately following the traumatic event [17, 18], although it is possible for symptoms to have a delayed onset. Whereas a subset of individuals recover within a few months [19], PTSD can persist for decades or even for an individual’s lifetime [20]. For example, approximately 90% of National Comorbidity Study (NCS) participants retrospectively reported that their PTSD symptoms were still present at 3 months, more than 70% continued to experience symptoms 1 year following the traumatic event, and more than one-third of the sample continued to experience PTSD symptoms 10 years or more, including those individuals who had received treatment [7]. Symptoms may also be cyclical, waxing and waning over time.
Comorbidities. PTSD rarely occurs in isolation from other emotional and behavioral symptoms. Kessler et al. [7], for example, reported that 88% of men and 79% of women with a lifetime diagnosis of PTSD met criteria for at least one other psychiatric diagnosis. Most common among these comorbid disorders are alcohol and substance use, mood, and non-PTSD anxiety disorders [21] (see Brady et al. for a review). Comorbidity rates of PTSD with other anxiety disorders (e.g., generalized anxiety disorder, panic disorder, simple phobia) ranged in the NCS from 7.3 to 31.4%, and lifetime prevalence rates of alcohol and drug use disorders were 51.9 and 34.5%, respectively, for men and 27.9 and 26.9%, respectively, for women with histories of PTSD [7]. Rates of comorbid major depression are likewise high, typically ranging from 30 to 50% (see [18]), with rates as high as 77% in treatment-seeking populations [22].
Traumatic stress exposures and PTSD also have been linked to health problems, such as cardio-and cerebrovascular disease, depressed immune functioning, pain disorders, increased health complaints, and decrements in health-related functioning [23,24,25]. Subsets of individuals diagnosed with PTSD may also experience physiological sleep abnormalities [26,27,28,29], potentially further damaging somatic, emotional, and cognitive health. Although some health problems may result from health risk behaviors such as increased tobacco use [28], as described below, others may be a direct consequence of neurobiological alterations.
Neurobiological Basis of PTSD
When confronted with life threat, the body responds with a state of physiological arousal, including acute increases in stress-related neurotransmitters and neuropeptides, such as corticotropin-releasing factor, norepinephrine, serotonin, dopamine, endogenous benzodiazepines, and endogenous opiates [30]. Although this response often serves an adaptive function in the immediate context of danger by facilitating actions that promote survival (i.e., “flight or fight” responses), the chronic dysregulation of these systems is believed to play an important role in both the pathogenesis and the maintenance of PTSD [31, 32] and is distinct from the pattern of neurobiological abnormalities associated with other stress-related psychiatric disorders such as anxiety and depression [32]. Unlike the profile of attenuated responsivity associated with habituation and adaptation to chronic stress [33] and major depression [34], PTSD is associated with exaggerated neurobiological responsiveness to cues (now often harmless) of the original trauma [30] and the general sensitization of several neurobiological systems [32, 35]. This sensitization in turn can lead to over-responsiveness to subsequent stress and fear cues. Over time, the cumulative biological strain produced by repeated stress responses, known as “allostatic load,” [36] can accelerate pathophysiology, including neuroimmune suppression and possibly neuronal damage.
Of particular relevance to the neuropsychology of PTSD is the dysregulation of the noradrenergic system, hypothalamic–pituitary–adrenal (HPA) axis, and serotonergic system [35]. These systems are believed to influence brain functioning in regions involved in the fear response, including the prefrontal cortex (PFC), amygdala, hippocampus, dorsal raphe nucleus, and locus coeruleus. In short, the combined dysregulation of these systems is thought to result in dampened prefrontal and hippocampal functioning and reduced medial prefrontal inhibition of the amygdala, a limbic structure central to fear-based emotion. Multiple reviews of the vast neurobiological literature relevant to PTSD are available [30, 35, 37,38,39,40].
Neuroimaging Findings
In this section, we present a brief overview of findings from structural and functional neuroimaging studies relevant to three critical brain regions (amygdala, medial prefrontal cortex, hippocampus) thought to be involved in the pathophysiology of PTSD. Several extensive reviews of these literatures are available [41,42,43,44,45].
Structural Imaging and Magnetic Resonance Spectroscopy (MRS)
Volumetric studies generally have revealed smaller hippocampal volumes in participants diagnosed with PTSD as compared to both no-PTSD trauma-exposed [43, 46,47,48,49] and non-trauma-exposed [43, 46,47,48, 50, 51] participants, although this finding has not been uniform [52], especially when samples with more recent trauma exposure were examined [53,54,55]. Gilbertson et al. [56] suggested that hippocampal volume may be a vulnerability for PTSD, rather than a consequence of the disorder, based on the finding that both the trauma-exposed and the non-trauma-exposed “co-twins” of veterans with PTSD showed smaller hippocampal volumes than non-PTSD trauma-exposed veterans and their non-exposed co-twins. Moreover, hippocampal volumetric differences may not become apparent until adulthood (see [43] for a review) and are not necessarily associated with neurocognitive performances, including on tasks of learning and memory [57]. Paralleling the volumetric findings, MRS studies examining the relative concentration of select compounds within the hippocampus have suggested that PTSD is associated with decreased neuronal health in the hippocampus [52, 58, 59].
A growing number of structural imaging studies have begun to examine the PFC and amygdala in relation to PTSD. In a meta-analysis of structural brain abnormalities in PTSD, Karl and colleagues [43] found significantly smaller left amygdala volumes in adults with PTSD compared to both healthy and trauma-exposed controls and significantly smaller anterior cingulate cortex compared to trauma-exposed controls. Not all studies examining amygdala volumes, however, have revealed differences between PTSD-diagnosed trauma survivors and comparison samples [47, 51, 53,54,55]. In contrast, those measuring frontal cortex volumes have revealed reduced volumes of the frontal cortex in PTSD [54, 60, 61], including decreased volumes in medial PFC structures [62,63,64,65] and reduced cortical thickness in much of the frontal gyri [66].
Functional Imaging
Functional neuroimaging studies of PTSD typically have demonstrated that individuals with PTSD, relative to comparison samples, show heightened amygdala responsivity and deactivation or decreased activation of the hippocampal, anterior cingulate, and orbital frontal cortex in response to symptom provocation such as that elicited by combat sounds and traumarelated words [67,68,69], script-driven imagery [70,71,72,73,74], and administration of yohimbine, an alpha-2 adrenergic receptor antagonist [75]. A similar pattern has surfaced in studies using cognitive activation paradigms such as encoding and retrieval of threat-related words [76], the emotional Stroop task [77], and presentation and memory of emotional facial expressions [78,79,80]. Relationships between activation in the amygdala and medial prefrontal cortex in response to traumatic imagery [74, 81] and fear-related stimuli [80] suggest that these two structures are functionally related in PTSD.
Summary and Related Literatures
Although beyond the scope of this chapter, there is also significant evidence of electrophysiological abnormalities in PTSD suggestive of neural processing abnormalities to both neutral and trauma-relevant stimuli [82]. Taken together, multiple methodologies provide converging evidence of biological, physiological, and neuroanatomical abnormalities associated with PTSD that would be expected to be associated with neuropsychological impairment.
Neuropsychological Functioning in PTSD
Empirical Findings
In this section, we review the now sizable literature on clinical neuropsychological test performances in PTSD and organize our review by domains commonly assessed in clinical neuropsychological evaluations, emphasizing those domains with the strongest empirical bases. Other recent reviews are also available [83,84,85,86,87].
Intellectual functioning. PTSD in both children [88] and adults [89,90,91,92,93,94,95,96] is associated with lower estimated and omnibus IQ scores as compared to no-PTSD trauma-exposed and non-exposed comparison groups. Likewise, correlational studies indicate an inverse relationship between PTSD and intellectual performance, even after controlling for stressor severity [90, 94, 97]. Few studies have examined intellectual functioning comprehensively with multi-faceted tasks, but those that have suggested that performance on verbal, as compared to visual–spatial, intellectual tasks may be more strongly associated with PTSD status [88, 90, 95]. In children, intellectual performance decrements have been associated with both early trauma exposure [98] and cortisol-induced neuronal loss associated with trauma exposure [55].
Earlier work using archival records suggests a directional relationship in which higher IQ serves a protective role following trauma exposure, reducing risk of PTSD [94]. Gilberston et al. [99] provided additional support for this hypothesis by examining twin pairs composed of one Vietnam War-exposed and one non-exposed brother. Intellectual performance did not differ between trauma-exposed brothers and their non-exposed co-twins. Instead, no-PTSD exposed brothers and their non-exposed co-twins performed more proficiently on intellectual tasks than both exposed brothers with PTSD and their non-exposed co-twins. A recent study of combat veterans using archival data, however, suggests that this relationship may be more complex: pre-exposure intellectual performance appeared to be protective against development of PTSD symptoms only at lower levels of trauma severity [100]. Using combat exposure as an index of combat severity, at lower levels of combat exposure, pre-exposure intellectual scores were negatively correlated with post-exposure PTSD symptom levels. In contrast, at higher levels of trauma exposure, pre-combat intellectual performances were not significantly associated with post-exposure PTSD severity.
New learning and memory. Anterograde memory on episodic, declarative memory tasks is perhaps the most thoroughly examined neuropsychological domain in the PTSD literature. Although several studies have yielded negative findings regarding the relationship of PTSD to anterograde memory functioning [101,102,103], the majority of studies have found that both children [104, 105] and adults [89,90,91, 93, 96, 106,107,108,109,110,111,112,113,114,115,116,117] with PTSD perform less proficiently than those without PTSD on one or more measures of learning or memory, with initial acquisition being the most frequently impaired aspect of memory dysfunction. There is also evidence of heightened sensitivity to proactive [118] and retroactive [96, 115, 117] interference in persons with PTSD. Whether PTSD is associated with degraded retention of newly learned information over longer delayed intervals is more ambiguous. Whereas PTSD was associated with less proficient memory retention in select studies [107], several studies failed to reveal PTSD-related deficits in memory retention [89, 91, 115, 119,120,121].
Two recent independent meta-analyses have attempted to address inconsistencies across studies through the advantages gained by pooling data. Both found that PTSD was associated with less proficient performance on verbal memory tasks. Brewin et al. [122] found small to moderate effect sizes for PTSD diagnostic status across different civilian and military trauma samples. The association between PTSD and memory impairment, which were more pronounced on verbal as compared to non-verbal memory tasks, could not be attributed to head injury and did not differ significantly according to immediate versus delayed recall conditions. Johnsen and Asbjornsen [111] extended these findings in a meta-analysis of immediate verbal memory performance, likewise finding a moderate effect size for PTSD diagnostic status. The effect was larger in military as compared to interpersonal trauma samples and when specific memory instruments (Wechsler Memory Scale subtests and the Rey Auditory Verbal Learning Test, as compared to the California Verbal Learning Test) were used.
Autobiographical memory. In addition to anterograde memory deficits, PTSD is associated with autobiographical memory abnormalities. On autobiographical memory tasks that require recall of a specific memory in response to a cue word, trauma survivors with PTSD, as compared to trauma-exposed participants without PTSD, are more likely to produce “over-general” memories (i.e., reflecting categories of events rather than a specific event) [123,124,125,126]. Overgeneral memory recall appears to be particularly pronounced for emotionally positive memories [124, 125, 127], suggesting a possible emotion-based cognitive bias. Although beyond the scope of this chapter, considerable controversy exists regarding whether traumatic autobiographical memories are encoded differently than non-traumatic memories or whether they differ only in the severity of impairment [128,129,130,131,132].
Attentional, executive, and prefrontal functioning. Despite the inclusion of concentration difficulties as a core PTSD diagnostic feature, PTSD does not appear to be associated with a general concentration deficit but instead appears to be associated with a specific pattern of attentional deficits. PTSD-related performance decrements have been documented repeatedly on working memory and divided attention tasks [89, 91, 95, 133, 134] and to a lesser extent [135] on tasks of sustained attention [96, 115, 136,137,138]. In contrast, some aspects of attention, such as shift of set (as measured by card sorting and visual selective attention tasks) and focus of attention (as measured by letter cancellation and the standard Stroop) appear to be relatively impervious to PTSD in non-elderly adults [93, 96, 115, 116, 136, 138,139,140,141], although PTSD-related deficits on card sorting tasks have been documented in elderly former prisoners of war [142] and children [104].
Contemporary neuroanatomical conceptualizations of PTSD implicate dysfunction of the prefrontal cortex, especially regarding its inhibitory functions. Consistent with this notion, PTSD has been shown to be associated with cognitive disinhibition [115, 140] and perseveration [99, 143]. Also suggesting prefrontal dysfunction, Vasterling et al. [116] found that, as compared to combat-exposed veterans without PTSD and non-combat-exposed veterans, Vietnam veterans with PTSD displayed relative performance deficits in olfactory recognition, a task sensitive to orbitofrontal integrity [144].
Language, visual–spatial, and motor functioning. The few studies examining basic language, visual– spatial, and motor functions in PTSD have failed to reveal PTSD-related deficits [145, 146] with the exception of performances on those tasks with a strong executive component, such as complex figural copying [92, 139, 147, 148], word list generation [104, 108, 118], and motor sequencing [92, 93]. Error analysis of clinical visuo-constructive tasks [149] and performance patterns on experimental visuo-spatial tasks [150] have also revealed PTSD-related deficits in processing local, as compared to global, stimulus attributes and distal contextual elements.
Summary. The existing literature indicates subtle, yet specific, cognitive deficits on tasks with significant executive demands (e.g., strategic learning, working memory, and inhibition tasks). Consistent with neuroimaging [46, 152], electrophysiological [153], and behavioral [149, 151] data implicating a cerebral asymmetry favoring the non-dominant hemisphere, neuropsychological studies of PTSD point to a modality-specific deficit in processing verbally mediated information. Although much of the neuropsychological literature relevant to PTSD is derived from non-elderly adult samples, existing studies of children and older adults suggest that the observed neuropsychological deficits are relatively consistent across the lifespan, although age may interact with PTSD such that the performance of older individuals possibly reflects aspects of both PTSD and aging [154, 155]. With rare exception [94, 99, 100], few studies have attempted to examine causal direction between cognitive dysfunction and PTSD in humans, leaving it an area ripe for further exploration via prospective methodology.
Implications for Clinical Evaluation
In our experience, PTSD referrals for neuropsychological evaluation typically center on requests to rule out alternative etiologies (e.g., degenerative disease, traumatic brain injury, cerebrovascular disease) for cognitive dysfunction and/or to document the extent of cognitive dysfunction associated with PTSD. Neuropsychological evaluation of PTSD patients can be used to inform treatment planning, including cognitive rehabilitation efforts. Occasionally, neuropsychologists also are referred cases in which the primary diagnosis of PTSD is not yet established or requires confirmation.
Confirming or establishing a PTSD diagnosis. As summarized in previous sections, empirical findings reveal that PTSD is associated with a pattern of mild cognitive deficits that are not necessarily specific to the disorder. Therefore, the primary diagnosis of PTSD is not made on the basis of neurocognitive testing, but instead requires the use of psychological assessment methods developed specifically for PTSD diagnosis. At its most basic level, the PTSD evaluation includes solicitation of the trauma event(s), assessment of the full range of PTSD symptoms and their linkage to the trauma event(s), and documentation of the duration and functional impact of the symptoms. State-of-the-art assessments typically incorporate multiple methods, including interview-based and paper-and-pencil self-report measures, allowing the examiner to capitalize on the strengths of each, while mitigating the relative weaknesses of each. An excellent summary of these measures can be found on the Department of Veterans Affairs National Center for PTSD website (www.ncptsd.va.gov).
Commonly employed structured interviews include measures focused solely on PTSD such as the Clinician-Administered PTSD Scale (CAPS) [156], Structured Interview for PTSD [157], the PTSD Symptom Scale Interview [158], and the PTSD Module of the Structured Clinical Interview for DSM-IV [159]. The CAPS is often considered the “gold standard” due to its inclusion of trauma assessment, linkage of symptoms to trauma events, assessment of associated features, and assessment of functional impact. Self-report measures often focus on symptom assessment and include those that are DSM-congruent, such as the PTSD Checklist [160], Davidson Trauma Scale [161], Impact of Events Scale – Revised [162], and the Posttraumatic Diagnostic Scale [163], as well as those that are considered less face valid because they do not show one-to-one DSM symptom correspondence but as a result may be less specific to PTSD [164]. Examples of the latter group include the Mississippi Scale for Combat-Related Posttraumatic Stress Disorder [165], Los Angeles Symptom Checklist [166], Penn Inventory for Posttraumatic Stress Disorder [167], and the Trauma Symptom Inventory [168].
A smaller subset of measures with demonstrated psychometric properties have been designed for use with young trauma patients. Examples include the Clinician-Administered PTSD Scale for Children and Adolescents [169], Trauma Symptom Checklist for Children [170], Posttraumatic Stress Disorder Semi-Structured Interview and Observation Record [171], and the Child Post-Traumatic Stress Disorder Reaction Index [172]. Detailed discussions of the strengths and weaknesses of various adult and child assessment measures and approaches can be found elsewhere [173,174,175,176].
Assessment of comorbid conditions and other contributory factors. As described earlier, PTSD commonly is associated with other psychiatric and somatic disorders. Complicating the primary diagnosis, overlap in symptom criteria (e.g., concentration difficulties) between PTSD and other psychiatric (e.g., depression) and somatic (e.g., post-concussion syndrome) disorders often create diagnostic ambiguities. Comorbid conditions also potentially impact cognitive performance both directly and indirectly (through other mediating factors). For example, when accompanied by certain comorbidities (e.g., depression), trauma survivors may be at greater risk for suicidal and other harmful behaviors [177], some of which (e.g., gunshots wounds to the head, drug overdoses resulting in coma) may result in lasting neuropsychological impairment. Further, pharmacological treatment of PTSD and associated conditions may result in iatrogenic effects that either enhance or impair cognitive functioning, depending on the specific agent [178,179,180,181,182]. Finally, certain comorbidities (e.g., alcohol use disorders, depression, traumatic brain injury, sleep disturbance) may influence neuropsychological performance directly [134, 183,184,185,186].
As such, clinical neuropsychological evaluation of PTSD requires assessment of comorbid conditions (e.g., depression), health risk behaviors (e.g., suicide attempts, excessive alcohol consumption), and contextual factors (e.g., concurrent pharmacological treatment, sleep) that potentially complicate interpretation of the assessment data. When such complicating factors occur, it becomes important to document the timeline of their onset relative to the onset and course of PTSD as well as any neuropsychological deficits. For example, knowing the chronology of substance abuse in relation to the onset of cognitive impairment and PTSD symptoms may help determine that cognitive decline began only after substance use increased. This information in turn can be used to project prognosis under a range of different circumstances (e.g., once substance use is discontinued). Preliminary evidence that neurodevelopmental disorders (e.g., attention deficit hyperactivity disorder) may be associated with increased risk of PTSD [91,92,93] also highlights the need to assess mental disorders that predate PTSD onset. Likewise, neurobehavioral disorders (e.g., dementia) with onset postdating trauma exposure may be associated with recurrence or exacerbation of PTSD symptoms [187].
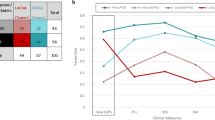
As an example of a complex clinical constellation, we highlight traumatic brain injury (TBI) occurring in the context of PTSD. TBI may have considerable overlap with PTSD in regard to neuropsychological deficits [188,189,190,191,192,193,194,195,196,197,198], associated somatic symptoms [199, 200], and underlying neural abnormalities [201, 202]. Depending on the relative severity of the two disorders, the overlap between PTSD and TBI on these dimensions can make differentiation of the relative contributions of each to neuropsychological deficits challenging [203]. Perhaps of greater relevance to the patient’s day to day functioning, however, is that TBI may exacerbate existing PTSD and depression symptoms in trauma survivors [204,205,206], complicating the clinical presentation. In such cases, it becomes essential to understand the recency of the TBI(s), the onset of PTSD relative to the TBI(s), the relative severity of each disorder, and the degree to which there may be other complicating factors (e.g., headaches) that influence current cognitive status and the course and prognosis of neuropsychological deficits.
Neurobehavioral Instrument Selection
As with neuropsychological evaluation of most disorders, we recommend incorporating at least cursory assessment of a broad range of cognitive domains, evaluating domains anticipated to be sensitive to PTSD diagnosis as well as those not expected to be affected. This approach allows evaluation of both confirmatory and disconfirmatory evidence of the hypothesized etiology of neuropsychological dysfunction and facilitates detection of non-PTSD etiologies. Screening multiple domains additionally identifies potential cognitive strengths that can be utilized to help compensate for observed deficits. Because the empirical literature suggests that PTSD-related deficits are relatively subtle, we recommend more comprehensive assessment of domains thought to be impaired in PTSD (e.g., learning, memory, inhibitory functions) using tasks that are reasonably challenging. Unfortunately, research examining neuropsychological functioning in PTSD only rarely has included assessment of effort, but the clinical context necessitates evaluation of cognitive effort for interpretation of the results. In the following paragraphs, we integrate findings from the empirical literature in considering clinical test selection in the two domains most commonly found to differ according to PTSD diagnosis (i.e., learning/memory and attention/executive functioning).
Learning and memory. Although both visual–spatial and verbal–auditory learning and memory deficits have been found to be associated with PTSD diagnosis, deficits have been more commonly documented on verbal–auditory tasks, and effect sizes appear larger on verbal–auditory as compared to visual–spatial tasks [122], suggesting that learning and memory should be assessed in both modalities. As with any disorder, it is typically useful to include both single- and multiple-exposure tasks, and to include tasks that assess both initial registration and retention. Although PTSD-related deficits have been observed on delayed recall [106], they less commonly have been observed when retention is computed relative to initial acquisition [91, 115, 116, 119, 154], suggesting that computation of difference scores or retention ratios may be clinically informative. Similarly, empirical findings indicating that PTSD is associated with heightened sensitivity to proactive and retroactive interference [115, 117, 118] suggest that tasks incorporating interference trials may provide clinically useful information.
The memory deficits associated with PTSD have been conceptualized as stemming in part from difficulties related to strategic learning [132, 207], highlighting the potential utility of administering tasks that vary in their demands on self-initiated strategy. For example, it may be helpful to compare performance on tasks with unrelated stimuli (placing additional burden on strategic memory processes) to performance on tasks in which there is an underlying categorical structure (demanding less strategic processing). Finally, we recommend analyzing errors (e.g., perseverations, intrusions) in memory assessments, given the mounting evidence that executive components of memory encoding and retrieval may be central to the memory deficit observed in PTSD.
Attentional and executive functions. One of the most theoretically interesting neuropsychological findings in PTSD (i.e., decreased response inhibition) may also be among the most clinically significant. The failure to gate information and regulate emotions strikes at the heart of PTSD with direct implications for the development and maintenance of the disorder. Specifically, it may be that frontally mediated deficits in inhibitory regulation influence how patients with PTSD process, encode, and retrieve trauma events and related memories [132]. Similarly, regulatory deficits of the limbic system have far-reaching implications for how emotions are experienced and managed. Therefore, we recommend that evaluation of attention/executive functions in PTSD include at a minimum a thorough assessment of response inhibition. Because the full extent of executive and attentional deficits associated with PTSD is not yet fully understood (especially in terms of their interactions with developmental stage), neuropsychological evaluation of PTSD ideally will include a broad range of attention and executive tasks.
Summary. Neuropsychological evaluation of the PTSD patient poses specific challenges. Whereas there are observable group-level deficits on neurobehavioral measures, they are likely to be mild and difficult to interpret at the individual level. In addition, a number of other potential contributory factors (e.g., other medical conditions, medications, comorbid substance abuse) may complicate the clinical picture. However, even subtle deficits may have a significant impact on daily functioning [148]. Moreover, as described below under the “Treatment Implications” section, such deficits may also have as yet undocumented effects on treatment response, suggesting that neuropsychological evaluation of PTSD offers information of potential value to the overall clinical management of the patient.
The Emotional Stroop Paradigm
As suggested by the previous section, the performance deficits on standardized clinical neuropsychological tests that accompany PTSD are typically mild and overlap to some extent with comorbid disorders. In contrast to standardized neuropsychological assessment instruments, experimental information processing, electrophysiological, and functional imaging studies have yielded results suggesting that some types of information processing abnormalities may be specific to PTSD, especially when trauma-relevant stimuli are employed. In this section, we highlight the emotional Stroop task, an experimental paradigm that has been particularly robust in detecting information processing biases to trauma-relevant stimuli in PTSD [208]. Although we anticipate that functional imaging and electrophysiological paradigms will continue to generate findings that will move the field closer toward understanding the neuropsychology of PTSD, we focus on the emotional Stroop task because of its extensive empirical history and, because it does not require specialized equipment, its potential feasibility and widespread accessibility. The functional imaging literature has been reviewed briefly in previous sections, and comprehensive reviews of the electrophysiological and cognitive information processing PTSD literatures are available elsewhere [82, 209, 210].
The emotional Stroop is a variant of the Stroop color-naming task [211], in which respondents are shown color-congruent (e.g., the word “red” printed in red ink) and color-incongruent (e.g., the word “red” printed in blue ink) words and asked to name as quickly as possible the color of ink in which the word is printed. In the classic Stroop, respondents are slower to name color-incongruent words than color-congruent words [211]. The emotional Stroop variation modifies the paradigm by varying the emotional valence and relevance of the words (e.g., “chair” as a neutral word, “combat” as a trauma-relevant word for combat veterans). Slower naming of any particular class of words is interpreted as an attentional bias (i.e., an attentional preference or “pull”) to the particular semantic category.
Relative to non-trauma-exposed and trauma-exposed individuals without PTSD, individuals with PTSD are slower to color-name trauma-related words as compared to emotionally neutral words or emotional words that are unrelated to their trauma [208, 212,213,214,215,216]. This attentional bias is thought to occur when the mild threat inherent to the semantic content of trauma words interferes with normal functioning and diverts cognitive resources to the threat-related information [208]. Attentional bias to trauma words in PTSD has been documented across a range of trauma populations, including rape victims [212, 213], combat veterans [214, 215, 217], and motor vehicle accident survivors [218, 219].
Although attentional biases to threat words on the Stroop have been well replicated, there continue to be several factors that limit its application as a clinical task. First, whereas idiographic lists are not required to show an effect, the trauma words nonetheless need to be generally related to the respondent’s trauma experience to elicit an effect. Thus, prior to clinical use, different versions of the task must be developed to accommodate diverse trauma populations. Second, and likely related to the diversity of stimuli necessary across trauma populations, clinical normative data do not yet exist. Such normative data will be critical, as biases to emotionally relevant words are not absolute but are instead relative to normal controls. Finally, theoretical debate continues regarding the parameters in which the emotional Stroop effect is most likely to occur and the degree to which it reflects automatic (i.e., involuntary and without conscious awareness or effort) versus strategic (i.e., requiring cognitive effort) processing [208, 220,221,222].
In sum, the emotional Stroop and other information processing paradigms continue to generate findings that elucidate the cognitive processes that underlie the development and perpetuation of PTSD (e.g., through reinforcement of fear networks) and explain PTSD symptoms such as hypervigilance and decreased concentration. Moreover, because of the specificity of attentional bias to threat-relevant information, some of these paradigms also hold potential for future clinical application; however, the field awaits further development of these tasks prior to widespread clinical implementation.
Treatment Implications
There are a number of psychosocial and psychopharmacological interventions used to treat PTSD. Below, we discuss the neuropsychological relevance of some of the more common of these interventions.
Pharmacological Treatment
Several psychotropic medications have been employed in the treatment of PTSD, including selective serotonin reuptake inhibitors (SSRIs), other antidepressants (e.g., tricyclics, monoamine oxidase inhibitors), anti-psychotic medications, and antiepileptic medications [180, 223]. However, the only two pharmacological agents approved by the US Food and Drug Administration specifically for treatment of PTSD are the SSRIs sertraline, and paroxetine [224]. Likewise, the Department of Veterans Affairs/Department of Defense Guidelines (VA/DOD) [225], the American Psychiatric Association [226], and the International Society of Traumatic Stress Studies (ISTSS) [227] endorsed SSRIs as the initial choice for the pharmacological treatment of PTSD. SSRIs impact multiple neurotransmitter systems [e.g., serotonin, glutamate, and gamma-aminobutyric acid (GABA)] that are thought to potentially impact cognitive functioning by improving inhibition of distracting recollections [223]. Supporting this hypothesis, preliminary evidence from single group designs suggests that SSRIs used in the treatment of PTSD may enhance performance on anterograde memory tasks [228] and alter neural activation from pre- to post-treatment in frontal, limbic, and paralimbic regions, particularly among treatment responders [229].
Psychotherapy
Psychological treatment approaches for PTSD include but are not limited to exposure-based interventions, cognitive–behavioral therapy, psychodynamic therapy, supportive counseling, anxiety management, and eye movement desensitization and reprocessing (EMDR). Of the many treatment approaches available, exposure-based and cognitive–behavioral interventions have been identified as the most efficacious in the treatment of PTSD [230,231,232], with exposure-based therapy named as the treatment of choice by the Institutes of Medicine [233].
Cognitive–behavioral interventions target modification of negative or distorted thoughts attached to trauma experiences, with the goal of generating more realistic explanations and thoughts associated with the trauma and trauma experience. Such modifications could be reasoned to require both the inhibition of maladaptive thoughts and sufficient cognitive flexibility to reappraise thoughts and memories. In addition, the degree to which trauma memories can be retrieved and modified may be important to treatment, especially when exposure is included in the intervention. Although not directly measuring neurocognitive functioning, recent neuroimaging studies have demonstrated that activation levels of the amygdala and anterior cingulate cortex [234, 235] and anterior cingulate volumes [236] helped predict treatment response for cognitive–behavioral and exposure therapies, raising the question of whether associated cognitive functions also may be useful in predicting treatment response to common psychological PTSD interventions. Supporting this notion, Wild and Gur [237] reported that more proficient verbal encoding and recall performances at pre-treatment were associated with better PTSD treatment outcomes.
EMDR is a multi-phase treatment incorporating trauma visualization, simultaneous lateral eye movements, and the coupling of positive cognitions with trauma visualization [238], with the latter repeated until the patient reports a high level of belief in the positive cognition [239]. Thus, like exposure-based interventions and some forms of CBT, EMDR incorporates an exposure component. Significant debate exists regarding the incremental benefits of EMDR over other exposure-based interventions, and the underlying mechanism of change (i.e., imagined exposure, ocular movement) is not well understood [239,240,241].
Preliminary work suggests that cognitive– behavioral and other psychological interventions may alter neural functioning. Sutherland and Bryant reported improved recollection of specific memories and reduced recollection of overgeneral, categorical memories following cognitive–behavioral treatment, as well as reduced bilateral amygdala and anterior cingulate activation [126]. Although not measuring neuropsychological outcomes, in a randomized trial, Lindauer et al. likewise demonstrated changes in neural activation in frontal and paralimbic regions following brief eclectic psychotherapy as compared to a wait-list control condition [242].
Family Considerations
Neuropsychological evaluations often consider how disorders impact the family. In PTSD, emotional, and possibly cognitive, dysfunction may lead to significant disruptions of social and family functioning. PTSD patients have the most difficulty in their closest relationships, such as those with a partner or significant other and children. In intimate relationships, trauma survivors with PTSD report lower levels of marital satisfaction [243, 244], poor cohesion and expressiveness [244, 245], high levels of conflict, which sometimes include physical aggression [246,247,248], and less intimacy and sexual satisfaction [246, 249, 250]. In turn, their partners report significant marital problems and often show somatic symptoms, anxiety, depression, and insomnia [244, 251, 252].
Regarding relationships with their children, trauma survivors suffering PTSD, particularly those who experience high levels of PTSD numbing and avoidance symptoms, have poorer parent–child relationships and less satisfaction with parenting [253, 254]. Children who have a parent with PTSD live in households with significantly higher conflict and lower cohesiveness [245, 252]. These children are also more likely to have behavioral problems [244] and are at a greater risk for mental disorders, including PTSD [255]. Some literature suggests that partners and children may exhibit secondary PTSD in which family members take on some symptoms of PTSD [256,257,258,259].
These negative family outcomes are relevant not only to the family member but also to the patient, especially in light of robust findings that social support is a key resource and determinant of mental health outcomes for those suffering from PTSD [260, 261]. Because social relationships may be affected adversely by PTSD symptoms, without intervention, individuals with PTSD may find themselves in a downward spiral in which one of the most valuable resources (i.e., social support) is less likely to be available. This reduction of social resources leads to ineffective coping behaviors (e.g., avoidance and isolation), which further deplete available resources, thus continuing the cycle. Therefore, in clinical settings, it is critical to assess family and social resources available to patients with PTSD. Fortunately, a number of interventions are emerging that may be particularly promising to address social dysfunction within intimate partner and family relationships [262,263,264].
Conclusions
Neuropsychological research, along with converging evidence from neurobiological, neuroimaging, and electrophysiological studies, suggests that the neural underpinnings of PTSD are integral to the disorder. Neuropsychological abnormalities include impairment of executive aspects of attention, sustained attention, learning, and memory. Performance on verbally mediated tasks, including IQ and anterograde memory tasks, is less likely to be proficient among trauma survivors who develop PTSD as compared to those who do not. The pattern of results is consistent with neuroanatomical models of PTSD that emphasize the prefrontal cortex and limbic/paralimbic areas, including the amygdala and the hippocampus. There is much about PTSD as a neurobehavioral disorder, however, that remains unresolved. For example, the degree to which neurobiological and neuropsychological abnormalities represent predispositional factors versus sequelae of trauma exposure is uncertain. Likewise, the extent to which comorbidity and treatment-related factors contribute to neuropsychological dysfunction in PTSD is not fully resolved. Inconsistencies in measurement and sampling methodology across studies have not permitted sufficient replication to create a highly delineated neuropsychological profile, although recent meta-analytic and longitudinal studies have begun to help address some of these issues. Finally, the addition of clinical neuropsychological measures within clinical trial research represents a particularly exciting application of neuropsychology. Inclusion of such assessment tools, both as outcome measures and as potential predictors of treatment response, will potentially have significant impact on the care of patients with PTSD.
References
Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. 2000;68:748–66.
McFarlane AC, Yehuda R. Risk factors for the acute biological and psychological response to trauma. In: Yehuda R, editor. Risk factors for posttraumatic stress disorder. Washington, DC: American Psychiatric Association; 1999. pp. 163–90.
Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull. 2003;129:52–73.
Yehuda R. Biological factors associated with susceptibility to posttraumatic stress disorder. Can J Psychiatry/La Revue Canadienne de Psychiatrie. 1999;44:34–39.
Vogt DS, King DW, King LA. Risk pathways for PTSD: making sense of the literature. In: Friedman MJ, Keane TM, Resick PA, editors. Handbook of PTSD: science and practice. New York, NY: Guilford Press; 2007. pp. 99–115.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994.
Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the national comorbidity survey. Arch Gen Psychiatry. 1995;52:1048–60.
King DW, Leskin GA, King LA, Weathers FW. Confirmatory factor analysis of the clinician-administered PTSD Scale: evidence for the dimensionality of posttraumatic stress disorder. Psychol Assess. 1998;10:90–96.
Simms LJ, Watson D, Doebbeling BN. Confirmatory factor analyses of posttraumatic stress symptoms in deployed and nondeployed veterans of the Gulf War. J Abnorm Psychol. 2002;111:637–47.
Green BL. Psychosocial research in traumatic stress: an update. J Trauma Stress. 1994;7:341–62.
Dohrenwend BP, Turner JB, Turse NA, et al. The psychological risks of Vietnam for U.S. veterans: a revisit with new data and methods. Science. 2006;313:979–82.
Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351:13–22.
Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295:1023–32.
Kulka RA, Schlenger WE, Fairbank JA, et al. Trauma and the Vietnam war generation: report of findings from the National Vietnam Veterans Readjustment Study. Philadelphia, PA: Brunner/Mazel; 1990.
Silva RR, Alpert M, Munoz DM, et al. Stress and vulnerability to posttraumatic stress disorder in children and adolescents. Am J Psychiatry. 2000;157:1229–35.
de Jong JT, Komproe IH, Van Ommeren M, et al. Lifetime events and posttraumatic stress disorder in four postconflict settings. JAMA. 2001;286:555–62.
Flouri E. Post-traumatic stress disorder (PTSD): what we have learned and what we still have not found out. J Interpers Violence. 2005;20:373–79.
Shalev AY. What is posttraumatic stress disorder? J Clin Psychiatry. 2001;62(Suppl 17):4–10.
Breslau N. Outcomes of posttraumatic stress disorder. J Clin Psychiatry. 2001;62(Suppl 17):55–9.
Yule W. Posttraumatic stress disorder in the general population and in children. J Clin Psychiatry. 2001;62(Suppl 17):23–8.
Brady KT, Killeen TK, Brewerton T, Lucerini S. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J Clin Psychiatry. 2000;61(Suppl 7):22–32.
Brown TA, Campbell LA, Lehman CL, et al. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. J Abnorm Psychol. 2001;110:585–99.
Schnurr PP, Green BL. Trauma and health: physical health consequences of exposure to extreme stress. Washington, DC: American Psychological Association; 2004.
Taft CA, Stern AS, King LA, King DW. Modeling physical health and functional health status: the role of combat exposure, posttraumatic stress disorder, and personal resource attributes. J Trauma Stress. 1999;12:2–23.
Vasterling JJ, Schumm J, Proctor SP, et al. Posttraumatic stress disorder and health functioning in a non-treatment-seeking sample of Iraq war veterans: a prospective analysis. J Rehabil Res Dev. 2008;45:347–58.
Breslau N, Roth T, Burduvali E, et al. Sleep in lifetime posttraumatic stress disorder: a community-based polysomnographic study. Arch Gen Psychiatry. 2004;61:508–16.
Mellman TA, Kulick-Bell R, Ashlock LE, Nolan B. Sleep events among veterans with combat-related posttraumatic stress disorder. Am J Psychiatry. 1995;152:110–15.
Schnurr PP, Spiro A 3rd. Combat exposure, posttraumatic stress disorder symptoms, and health behaviors as predictors of self-reported physical health in older veterans. J Nerv Ment Dis. 1999;187:353–59.
Singareddy RK, Balon R. Sleep in posttraumatic stress disorder. Ann Clin Psychiatry. 2002;14:183–90.
Bremner JD, Southwick SM, Charney DS. The neurobiology of posttraumatic stress disorder: an integration of animal and human research. In: Saigh PA, Bremner JD, editors. Posttraumatic stress disorder: a comprehensive text. Needham Heights, MA: Allyn & Bacon; 1999. pp. 103–43.
Charney DS, Deutch AY, Krystal JH, et al. Psychobiologic mechanisms of posttraumatic stress disorder. Arch Gen Psychiatry. 1993;50:295–305.
Yehuda R, McFarlane AC. Conflict between current knowledge about posttraumatic stress disorder and its original conceptual basis. Am J Psychiatry. 1995;152:1705–13.
Selye H. The stress of life. New York, NY: McGraw-Hill; 1956.
Siever LJ, Davis KL. Overview: toward a dysregulation hypothesis of depression. Am J Psychiatry. 1985;142:1017–31.
Southwick SM, Rasmusson A, Barron J, Arnsten A. Neurobiological and neurocognitive alterations and PTSD: a focus on norepinephrine, serotonin, and the HPA axis. In: Vasterling JJ, Brewin CR, editors. The neuropsychology of PTSD: biological, cognitive, and clinical perspectives. New York, NY: Guilford Press; 2005.
McEwen BS. Allostasis and allostatic load: implications for neuropsychopharmacology. Neuropsychopharmacology. 2000;22:108–24.
Bonne O, Grillon C, Vythilingam M, et al. Adaptive and maladaptive psychobiological responses to severe psychological stress: implications for the discovery of novel pharmacotherapy. Neurosci Biobehav Rev. 2004;28:65–94.
Charney DS, Deutch AY, Southwick SM, Krystal JH. Neural circuits and mechanisms of posttraumatic stress disorder. In: Friedman MJ, Charney DS, Deutch AY, editors. Neurobiological and clinical consequences of stress: from normal adaptation to posttraumatic stress disorder. Philadelphia, PA: Lippincott-Raven; 1995. pp. 271–87.
Rasmusson AM, Vythilingam M, Morgan CA 3rd. The neuroendocrinology of posttraumatic stress disorder: new directions. CNS Spectr. 2003;8(651–656):665–657.
Yehuda R. Current status of cortisol findings in posttraumatic stress disorder. Psychiatr Clin North Am. 2002;25(341–68):vii.
Francati V, Vermetten E, Bremner JD. Functional neuroimaging studies in posttraumatic stress disorder: review of current methods and findings. Depress Anxiety. 2007;24:202–18.
Grossman R, Buchsbaum MS, Yehuda R. Neuroimaging studies in post-traumatic stress disorder. Psychiatr Clin N Am. 2002;25:317–40.
Karl A, Schaefer M, Malta LS, et al. A meta-analysis of structural brain abnormalities in PTSD. Neurosci Biobehav Rev. 2006;30:1004–31.
Rauch SL, Shin LM, Phelps EA. Neurocircuitry models of posttraumatic stress disorder and extinction: human neuroimaging research – past, present, and future. Biol Psychiatry. 2006;60:376–82.
Shin LM, Rauch SL, Pitman RK. Structural and functional anatomy of PTSD: findings from neuroimaging research. In: Vasterling JJ, Brewin CR, editors. Neuropsychology of PTSD: biological, cognitive, and clinical perspectives. New York, NY: Guilford Press; 2005. pp. 59–82.
Bremner JD, Vythilingam M, Vermetten E, et al. MRI and PET study of deficits in hippocampal structure and function in women with childhood sexual abuse and posttraumatic stress disorder. Am J Psychiatry. 2003;160:924–32.
Gurvits TV, Shenton ME, Hokama H, et al. Magnetic resonance imaging study of hippocampal volume in chronic, combat-related posttraumatic stress disorder. Biol Psychiatry. 1996;40:1091–99.
Kitayama N, Vaccarino V, Kutner M, et al. Magnetic resonance imaging (MRI) measurement of hippocampal volume in posttraumatic stress disorder: a meta-analysis. J Affect Disord. 2005;88:79–86.
Stein MB, Koverola C, Hanna C, et al. Hippocampal volume in women victimized by childhood sexual abuse. Psychol Med. 1997;27:951–59.
Bremner JD, Randall P, Scott TM, et al. MRI-based measurement of hippocampal volume in patients with combat-related posttraumatic stress disorder. Am J Psychiatry. 1995;152:973–81.
Bremner JD, Randall P, Vermetten E, et al. Magnetic resonance imaging-based measurement of hippocampal volume in posttraumatic stress disorder related to childhood physical and sexual abuse – a preliminary report. Biol Psychiatry. 1997;41:23–32.
Schuff N, Neylan TC. Lenoci MA et al. Decreased hippocampal N-Acetylaspartate in the absence of atrophy in posttraumatic stress disorder. Biol Psychiatry. 2001;50:952–59.
Bonne O, Brandes D, Gilboa A, et al. Longitudinal MRI study of hippocampal volume in trauma survivors with PTSD. Am J Psychiatry. 2001;158:1248–51.
Carrion VG, Weems CF, Eliez S, et al. Attenuation of frontal asymmetry in pediatric posttraumatic stress disorder. Biol Psychiatry. 2001;50(12):943–51.
De Bellis M, Keshavan MS, Clark D, et al. Developmental traumatology part II: brain development. Biol Psychiatry. 1999;45:1271–84.
Gilbertson MW, Shenton ME, Ciszewski A, et al. Smaller hippocampal volume predicts pathologic vulnerability to psychological trauma. Nat Neurosci. 2002;5:1242–47.
Lindauer RJ, Olff M, van Meijel EP, et al. Cortisol, learning, memory, and attention in relation to smaller hippocampal volume in police officers with posttraumatic stress disorder. Biol Psychiatry. 2006;59:171–77.
Freeman TW, Cardwell D, Karson CN, Komoroski RA. In vivo proton magnetic resonance spectroscopy of the medial temporal lobes of subjects with combat-related posttraumatic stress disorder. Magn Reson Med. 1998;40:66–71.
Menon PM, Nasrallah HA, Lyons JA, et al. Single-voxel proton MR spectroscopy of right versus left hippocampi in PTSD. Psychiatry Res. 2003;123:101–08.
De Bellis MD, Keshavan MS, Shifflett H, et al. Brain structures in pediatric maltreatment-related posttraumatic stress disorder: a sociodemographically matched study. Biol Psychiatry. 2002;52:1066–78.
Fennema-Notestine C, Stein MB, Kennedy CM, et al. Brain morphometry in female victims of intimate partner violence with and without posttraumatic stress disorder. Biol Psychiatry. 2002;52:1089–101.
Kasai K, Yamasue H, Gilbertson MW, et al. Evidence for acquired pregenual anterior cingulate gray matter loss from a twin study of combat-related posttraumatic stress disorder. Biol Psychiatry. 2008;63:550–56.
Rauch SL, Shin LM, Segal E, et al. Selectively reduced regional cortical volumes in post-traumatic stress disorder. Neuroreport. 2003;14:913–16.
Woodward SH, Kaloupek DG, Streeter CC, et al. Decreased anterior cingulate volume in combat-related PTSD. Biol Psychiatry. 2006;59:582–87.
Yamasue H, Kasai K, Iwanami A, et al. Voxel-based analysis of MRI reveals anterior cingulate gray-matter volume reduction in posttraumatic stress disorder due to terrorism. Proc Natl Acad Sci USA. 2003;100:9039–43.
Geuze E, Westenberg HG, Heinecke A, et al. Thinner prefrontal cortex in veterans with posttraumatic stress disorder. Neuroimage. 2008;41:675–81.
Bremner JD, Staib LH, Kaloupek D, et al. Neural correlates of exposure to traumatic pictures and sound in Vietnam combat veterans with and without posttraumatic stress disorder: a positron emission tomography study. Biol Psychiatry. 1999;45:806–16.
Driessen M, Beblo T, Mertens M, et al. Posttraumatic stress disorder and fMRI activation patterns of traumatic memory in patients with borderline personality disorder. Biol Psychiatry. 2004;55:603–11.
Liberzon I, Taylor SF, Amdur R, et al. Brain activation in PTSD in response to trauma-related stimuli. Biol Psychiatry. 1999;45:817–26.
Bremner JD, Narayan M, Staib LH, et al. Neural correlates of memories of childhood sexual abuse in women with and without posttraumatic stress disorder. Am J Psychiatry. 1999;156:1787–95.
Lanius RA, Williamson PC, Densmore M, et al. Neural correlates of traumatic memories in posttraumatic stress disorder: a functional MRI investigation. Am J Psychiatry. 2001;158:1920–22.
Liberzon I, Britton JC, Phan KL. Neural correlates of traumatic recall in posttraumatic stress disorder. Stress. 2003;6:151–56.
Rauch SL, van der Kolk BA, Fisler RE, et al. A symptom provocation study of posttraumatic stress disorder using positron emission tomography and script-driven imagery. Arch Gen Psychiatry. 1996;53:380–87.
Shin LM, Orr SP, Carson MA, et al. Regional cerebral blood flow in the amygdala and medial prefrontal cortex during traumatic imagery in male and female Vietnam veterans with PTSD. Arch Gen Psychiatry. 2004;61:168–76.
Bremner JD, Innis RB, Ng CK, et al. Positron emission tomography measurement of cerebral metabolic correlates of yohimbine administration in combat-related posttraumatic stress disorder. Arch Gen Psychiatry. 1997;54:246–54.
Bremner JD, Vythilingam M, Vermetten E, et al. Neural correlates of declarative memory for emotionally valenced words in women with posttraumatic stress disorder related to early childhood sexual abuse. Biol Psychiatry. 2003;53:879–89.
Shin LM, Whalen PJ, Pitman RK, et al. An fMRI study of anterior cingulate function in posttraumatic stress disorder. Biol Psychiatry. 2001;50:932–42.
Dickie EW, Brunet A, Akerib V, Armony JL. An fMRI investigation of memory encoding in PTSD: influence of symptom severity. Neuropsychologia. 2008;46:1522–31.
Rauch SL, Whalen PJ, Shin LM, et al. Exaggerated amygdala response to masked facial stimuli in posttraumatic stress disorder: a functional MRI study. Biol Psychiatry. 2000;47:769–76.
Shin LM, Wright CI, Cannistraro PA, et al. A functional magnetic resonance imaging study of amygdala and medial prefrontal cortex responses to overtly presented fearful faces in posttraumatic stress disorder. Arch Gen Psychiatry. 2005;62:273–81.
Gilboa A, Shalev AY, Laor L, et al. Functional connectivity of the prefrontal cortex and the amygdala in posttraumatic stress disorder. Biol Psychiatry. 2004;55:263–72.
Metzger LJ, Gilbertson MW, Orr SP. Electrophysiology of PTSD. In: Vasterling JJ, Brewin CR, editors. Neuropsychology of PTSD: biological, cognitive, and clinical perspectives. New York, NY: Guilford Press; 2005. p. 83–102.
Danckwerts A, Leathem J. Questioning the link between PTSD and cognitive dysfunction. Neuropsychol Rev. 2003;13:221–35.
De Bellis MD, Hooper SR, Sapia JL. Early trauma exposure and the brain. In: Vasterling JJ, Brewin CR, editors. Neuropsychology of PTSD: biological, cognitive, and clinical perspectives. New York, NY: Guilford Press; 2005. pp. 153–77.
Horner MD, Hamner MB. Neurocognitive functioning in posttraumatic stress disorder. Neuropsychol Rev. 2002;12:15–30.
MacDonald HZ, Vasterling JJ, Rasmusson A. Neuropsychological underpinnings of PTSD in children and adolescents. In: Ardino V, editor. Post-traumatic syndromes in children and adolescents. London: Wiley–Blackwell, in press.
Vasterling JJ, Brailey K. Neuropsychological findings in adults with PTSD. In: Vasterling JJ, Brewin CR, editors. Neuropsychology of PTSD: biological, cognitive, and clinical perspectives. New York, NY: Guilford Press; 2005. pp. 178–207.
Saigh PA, Yasik AE, Oberfield RA, et al. The intellectual performance of traumatized children and adolescents with or without posttraumatic stress disorder. J Abnorm Psychol. 2006;115:332–40.
Brandes D, Ben-Schachar G, Gilboa A, et al. PTSD symptoms and cognitive performance in recent trauma survivors. Psychiatry Res. 2002;110:231–38.
Gil T, Calev A, Greenberg D, et al. Cognitive functioning in post-traumatic stress disorder. J Trauma Stress. 1990;3:29–45.
Gilbertson MW, Gurvits TV, Lasko NB, et al. Multivariate assessment of explicit memory function in combat veterans with posttraumatic stress disorder. J Trauma Stress. 2001;14:413–31.
Gurvits TV, Gilbertson MW, Lasko NB, et al. Neurologic soft signs in chronic posttraumatic stress disorder. Arch Gen Psychiatry. 2000;57:181–86.
Gurvits TV, Lasko NB, Schachter SC, et al. Neurological status of Vietnam veterans with chronic posttraumatic stress disorder. J Neuropsychiatry Clin Neurosci. 1993;5:183–88.
Macklin ML, Metzger LJ, Litz BT, et al. Lower precombat intelligence is a risk factor for posttraumatic stress disorder. J Consult Clin Psychol. 1998;66:323–26.
Vasterling JJ, Brailey K, Constans JI, et al. Assessment of intellectual resources in Gulf War veterans: relationship to PTSD. Assessment. 1997;4:51–59.
Vasterling JJ, Duke LM, Brailey K, et al. Attention, learning, and memory performances and intellectual resources in Vietnam veterans: PTSD and no disorder comparisons. Neuropsychology. 2002;16:5–14.
McNally RJ, Shin LM. Association of intelligence with severity of posttraumatic stress disorder symptoms in Vietnam Combat veterans. Am J Psychiatry. 1995;152:936–38.
Koenen KC, Moffitt TE, Caspi A, et al. Domestic violence is associated with environmental suppression of IQ in young children. Dev Psychopathol. 2003;15:297–311.
Gilbertson MW, Paulus LA, Williston SK, et al. Neurocognitive function in monozygotic twins discordant for combat exposure: relationship to posttraumatic stress disorder. J Abnorm Psychol. 2006;115:484–95.
Thompson WW, Gottesman II. Challenging the conclusion that lower preinduction cognitive ability increases risk for combat-related post-traumatic stress disorder in 2,375 combat-exposed Vietnam War veterans. Mil Med. 2008;173:576–82.
Neylan TC, Lenoci M, Rothlind J, et al. Attention, learning, and memory in posttraumatic stress disorder. J Trauma Stress. 2004;17:41–46.
Pederson CL, Maurer SH, Kaminski PL, et al. Hippocampal volume and memory performance in a community-based sample of women with posttraumatic stress disorder secondary to child abuse. J Trauma Stress. 2004;17:37–40.
Zalewski C, Thompson W, Gottesman II. Comparison of neuropsychological test performance in PTSD, generalized anxiety disorder, and control Vietnam veterans. Assessment. 1994;1:133–42.
Beers SR, De Bellis M. Neuropsychological function in children with maltreatment-related posttraumatic stress disorder. Am J Psychiatry. 2002;159:483–86.
Yasik AE, Saigh PA, Oberfield RA, Halamandaris PV. Posttraumatic stress disorder: memory and learning performance in children and adolescents. Biol Psychiatry. 2007;61:382–88.
Bremner JD, Scott TM, Delaney RC, et al. Deficits in short-term memory in posttraumatic stress disorder. Am J Psychiatry. 1993;150:1015–19.
Bremner JD, Randall P, Scott TW, et al. Deficits in short-term memory in adult survivors of childhood abuse. Psychiatry Res. 1995;59:97–107.
Bustamante V, Mellman TA, David D, Fins AI. Cognitive functioning and the early development of PTSD. J Trauma Stress. 2001;14:791–97.
Golier JA, Yehuda R, Lupien SJ, et al. Memory performance in Holocaust survivors with posttraumatic stress disorder. Am J Psychiatry. 2002;159:1682–88.
Jenkins MA, Langlais PJ, Delis D, Cohen R. Learning and memory in rape victims with posttraumatic stress disorder. Am J Psychiatry. 1998;155:278–279.
Johnsen GE, Asbjornsen AE. Consistent impaired verbal memory in PTSD: a meta-analysis. J Affect Disord. 2008;111:74–82.
Moradi AR, Doost HT, Taghavi MR, et al. Everyday memory deficits in children and adolescents with PTSD: performance on the Rivermead Behavioural Memory Test. J Child Psychol Psychiatry. 1999;40:357–61.
Parslow RA, Jorm AF. Pretrauma and posttrauma neurocognitive functioning and PTSD symptoms in a community sample of young adults. Am J Psychiatry. 2007;164:509–15.
Sachinvala N, Von Scotti H, McGuire M, et al. Memory, attention, function, and mood among patients with chronic posttraumatic stress disorder. J Nerv Ment Dis. 2000;188:818–23.
Vasterling JJ, Brailey K, Constans JI, Sutker PB. Attention and memory dysfunction in posttraumatic stress disorder. Neuropsychology. 1998;12:125–33.
Vasterling JJ, Brailey K, Sutker PB. Olfactory identification in combat-related posttraumatic stress disorder. J Trauma Stress. 2000;13:241–53.
Yehuda R, Keefe RSE, Harvey PD, et al. Learning and memory in combat veterans with posttraumatic stress disorder. Am J Psychiatry. 1995;152:137–39.
Uddo M, Vasterling JJ, Brailey K, Sutker PB. Memory and attention in combat-related post-traumatic stress disorder (PTSD). J Psychopathol Behav Assess. 1993;15:43–53.
Jelinek L, Jacobsen D, Kellner M. Verbal and nonverbal memory functioning in posttraumatic stress disorder. J Clin Exp Neuropsychol. 2006;28:940–48.
Stein MB, Hanna C, Vaerum V, Koverola C. Memory functioning in adult women traumatized by childhood sexual abuse. J Trauma Stress. 1999;12:527–34.
Yehuda R, Golier JA, Harvey PD, et al. Relationship between cortisol and age-related memory impairments in Holocaust survivors with PTSD. Psychoneuroendocrinology. 2005;30:678–87.
Brewin CR, Kleiner JS, Vasterling JJ, Field AP. Memory for emotionally neutral information in posttraumatic stress disorder: a meta-analytic investigation. J Abnorm Psychol. 2007;116:448–63.
Dalgleish T, Rolfe J, Golden A-M, et al. Reduced autobiographical memory specificity and posttraumatic stress: exploring the contributions of impaired executive control and affect regulation. J Abnorm Psychol. 2008;117:236–41.
McNally RJ, Lasko NB, Macklin ML, Pitman RK. Autobiographical memory disturbance in combat-related posttraumatic stress disorder. Behav Res Ther. 1995;33:619–30.
McNally RJ, Litz BT, Prassas A, Shin LM. Emotional priming of autobiographical memory in post-traumatic stress disorder. Cogn Emot. 1994;8:351–67.
Sutherland K, Bryant RA. Autobiographical memory in posttraumatic stress disorder before and after treatment. Behav Res Ther. 2007;45:2915–23.
Schönfeld S, Ehlers A, Böllinghaus I, Rief W. Overgeneral memory and suppression of trauma memories in posttraumatic stress disorder. Memory. 2007;15:339–52.
Christianson S. Emotional stress and eyewitness memory: a critical review. Psychol Bull. 1992;112:284–309.
Conway MA. Memory and the self. J Mem Lang. 2005;53:594–628.
Golden A-M, Dalgleish T, Mackintosh B. Levels of specificity of autobiographical memories and of biographical memories of the deceased in bereaved individuals with and without complicated grief. J Abnorm Psychol. 2007;116:786–95.
Safer MA, Christianson S, Autry MW, Österlund K. Tunnel memory for traumatic events. Appl Cogn Psychol. 1998;12:99–117.
Verfaellie M, Vasterling JJ. Memory in PTSD: a neurocognitive approach. In: Shiromani P, Keane TM, LeDoux J, editors. Neurobiology of PTSD. Totowa, NJ: Humana Press; 2009. pp. 105–132.
Beckham JC, Crawford AL, Feldman ME. Trail making test performance in Vietnam combat veterans with and without posttraumatic stress disorder. J Trauma Stress. 1998;11:811–9.
Meewisse ML, Nijdam MJ, de Vries GJ, et al. Disaster-related posttraumatic stress symptoms and sustained attention: evaluation of depressive symptomatology and sleep disturbances as mediators. J Trauma Stress. 2005;18:299–302.
Golier J, Yehuda R, Cornblatt B, et al. Sustained attention in combat-related posttraumatic stress disorder. Integr Physiol Behav Sci. 1997;32:52–61.
Jenkins MA, Langlais PJ, Delis DA, Cohen RA. Attentional dysfunction associated with posttraumatic stress disorder among rape survivors. Clin Neuropsychol. 2000;14:7–12.
McFarlane AC, Weber DL, Clark CR. Abnormal stimulus processing in posttraumatic stress disorder. Biol Psychiatry. 1993;34:311–20.
Veltmeyer MD, Clark CR, McFarlane AC, et al. Integrative assessment of brain and cognitive function in post-traumatic stress disorder. J Integr Neurosci. 2005;4:145–59.
Barrett DH, Green ML, Morris R, et al. Cognitive functioning and posttraumatic stress disorder. Am J Psychiatry. 1996;153:1492–94.
Leskin LP, White PM. Attentional networks reveal executive function deficits in posttraumatic stress disorder. Neuropsychology. 2007;21:275–84.
Twamley EW, Hami S, Stein MB. Neuropsychological function in college students with and without posttraumatic stress disorder. Psychiatry Res. 2004;126:265–74.
Sutker PB, Vasterling JJ, Brailey K, Allain AN. Memory, attention, and executive deficits in POW survivors: contributing biological and psychological factors. Neuropsychology. 1995;9:118–25.
Koenen KC, Driver KL, Oscar-Berman M, et al. Measures of prefrontal system dysfunction in posttraumatic stress disorder. Brain Cogn. 2001;45:64–78.
Savic I, Bookheimer SY, Fried I, Engel J Jr. Olfactory bedside test: a simple approach to identify temporo-orbitofrontal dysfunction. Arch Neurol. 1997;54:162–68.
Crowell TA, Kieffer KM, Siders CA. Neuropsychological findings in combat-related posttraumatic stress disorder. Clin Neuropsychol. 2002;16:310–21.
Sullivan K, Krengel M, Proctor SP, et al. Cognitive functioning in treatment-seeking Gulf War veterans: pyridostigmine bromide use and PTSD. J Psychopathol Behav Assess. 2003;25:95–103.
Gurvits TV, Lasko NB, Repak AL, et al. Performance on visuospatial copying tasks in individuals with chronic posttraumatic stress disorder. Psychiatry Res. 2002;112:263–68.
Stein MB, Kennedy CM, Twamley EW. Neuropsychological function in female victims of intimate partner violence with and without posttraumatic stress disorder. Biol Psychiatry. 2002;52:1079–88.
Vasterling JJ, Rogers C, Kaplan E. Qualitative block design analysis in posttraumatic stress disorder. Assessment. 2000;7:217–26.
Gilbertson MW, Williston SK, Paulus LA, et al. Configural cue performance in identical twins discordant for posttraumatic stress disorder: theoretical implications for the role of hippocampal function. Biol Psychiatry. 2007;62:513–20.
Vasterling JJ, Duke LM, Tomlin H, et al. Global-local visual processing in posttraumatic stress disorder. J Int Neuropsychol Soc. 2004;10:709–18.
Villarreal G, Hamilton DA, Petropoulos H, et al. Reduced hippocampal volume and total white matter volume in posttraumatic stress disorder. Biol Psychiatry. 2002;52:119–25.
Metzger LJ, Paige SR, Carson MA, et al. PTSD arousal and depression symptoms associated with increased right-sided parietal EEG asymmetry. J Abnorm Psychol. 2004;113:324–29.
Yehuda R, Golier JA, Tischler L, et al. Learning and memory in aging combat veterans with PTSD. J Clin Exp Neuropsychol. 2005;27:504–15.
Yehuda R, Tischler L, Golier JA, et al. Longitudinal assessment of cognitive performance in Holocaust survivors with and without PTSD. Biol Psychiatry. 2006;60:714–21.
Weathers FW, Keane TM, Davidson JR. Clinician-administered PTSD scale: a review of the first ten years of research. Depress Anxiety. 2001;13:132–56.
Davidson J, Smith R, Kudler H. Validity and reliability of the DSM-III criteria for posttraumatic stress disorder. Experience with a structured interview. J Nerv Ment Dis. 1989;177:336–41.
Foa D, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing posttraumatic stress disorder. J Trauma Stress. 1993;6:459–74.
First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV axis I disorders, clinician version. Arlington, VA: American Psychiatric Publishing, Inc; 1997.
Weathers FW, Litz BT, Herman D, et al. The PTSD Checklist (PCL): reliability, validity, and diagnostic utility. San Antonio, TX: Annual Convention of the International Society for Traumatic Stress Studies; 1993.
Davidson JR, Book SW, Colket JT, et al. Assessment of a new self-rating scale for post-traumatic stress disorder. Psychol Med. 1997;27:153–60.
Weiss DS, Marmar CR. The Impact of Event Scale – Revised. In: Wilson J, Keane TM, editors. Assessing psychological trauma and PTSD. New York, NY: Guilford Press; 1996. pp. 399–411.
Foa EB, Cashman L, Jaycox LH, Perry BD. The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychol Assess. 1997;9:445–51.
Weathers FW, Keane TM, King LA, et al. Psychometric theory in the development of posttraumatic stress disorder assessment tools. Assessing psychological trauma and PTSD. New York, NY: Guilford Press; 1997. pp. 98–135.
Keane TM, Caddell JM, Taylor KL. Mississippi Scale for Combat-Related Posttraumatic Stress Disorder: three studies in reliability and validity. J Consult Clin Psychol. 1988;56:85–90.
King LA, King DW, Leskin G, Foy DW. The Los Angeles Symptom Checklist: a self-report measure of posttraumatic stress disorder. Assessment. 1995;2:1–17.
Hammarberg M. Penn Inventory for Posttraumatic Stress Disorder: psychometric properties. Psychol Assess. 1992;4:67–76.
Briere J. Trauma Symptom Inventory Professional manual. Odessa, FL: Psychological Assessment Resources; 1995.
Nader K, Kriegler JA, Blake DD, et al. Clinician Administered PTSD Scale, child and adolescent version. White River Junction, VT: National Center for PTSD; 1996.
Briere J. Trauma Symptom Checklist for children: professional manual. Odessa, FL: Psychol Assess Resources; 1996.
Scheeringa MS, Zeanah CH. PTSD semi-structured interview and observation record for infants and young children. New Orleans, LA: Department of Psychiatry and Neurology, Tulane University Health Sciences Center; 1994.
Frederick C, Pynoos R, Nader K. Child Post-traumatic Stress Disorder Reaction Index. Los Angeles, CA: Trauma Psychiatry Service, University of California at Los Angeles; 1992.
Hawkins SS, Radcliffe J. Current measures of PTSD for children and adolescents. J Pediatr Psychol. 2006;31:420–30.
Keane TM, Brief DJ, Pratt EM, et al. Assessment of PTSD and its comorbidities in adults. In: Friedman MJ, Keane TM, Resick PA, editors. Handbook of PTSD: science and practice. New York, NY: Guilford Press; 2007. pp. 279–305.
Norris FH, Hamblen JL. Standardized self-report measures of civilian trauma and PTSD. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. 2nd ed. New York, NY: Guilford Press; 2004. pp. 63–102.
Stover CS, Berkowitz S. Assessing violence exposure and trauma symptoms in young children: a critical review of measures. J Trauma Stress. 2005;18:707–17.
Oquendo MA, Friend JM, Halberstam B, et al. Association of comorbid posttraumatic stress disorder and major depression with greater risk for suicidal behavior. Am J Psychiatry. 2003;160:580–82.
Bremner JD, Yehuda R. The relationship between cognitive and brain changes in posttraumatic stress disorder. In: Yehuda R, editor. Psychobiology of posttraumatic stress disorders: a decade of progress, vol. 1071. Malden, MA: Blackwell; 2006. pp. 80–6.
Constant EL, Adam S, Gillain B, et al. Effects of sertraline on depressive symptoms and attentional and executive functions in major depression. Depress Anxiety. 2005;21:78–89.
Davis LL, Frazier EC, Williford RB, Newell JM. Long-term pharmacotherapy for post-traumatic stress disorder. CNS Drugs. 2006;20:465–76.
Siepmann M, Grossmann J, Muck-Weymann M, Kirch W. Effects of sertraline on autonomic and cognitive functions in healthy volunteers. Psychopharmacology (Berl). 2003;168:293–98.
Wadsworth EJ, Moss SC, Simpson SA, Smith AP. SSRIs and cognitive performance in a working sample. Hum Psychopharmacol. 2005;20:561–72.
Austin MP, Mitchell P, Wilhelm K, et al. Cognitive function in depression: a distinct pattern of frontal impairment in melancholia? Psychol Med. 1999;29:73–85.
Himanen L, Portin R, Isoniemi H, et al. Longitudinal cognitive changes in traumatic brain injury: a 30-year follow-up study. Neurology. 2006;66:187–92.
Leroi I, Sheppard JM, Lyketsos CG. Cognitive function after 11.5 years of alcohol use: relation to alcohol use. Am J Epidemiol. 2002;156:747–52.
Ravnkilde B, Videbech P, Clemmensen K, et al. The Danish PET/depression project: cognitive function and regional cerebral blood flow. Acta Psychiatr Scand. 2003;108:32–40.
van Achterberg ME, Rohrbaugh RM, Southwick SM. Emergence of PTSD in trauma survivors with dementia. J Clin Psychiatry. 2001;62:206–7.
Chen JK, Johnston KM, Petrides M, Ptito A. Neural sub-strates of symptoms of depression following concussion in male athletes with persisting postconcussion symptoms. Arch Gen Psychiatry. 2008;65:81–9.
Drake AI, Gray N, Yoder S, et al. Factors predicting return to work following mild traumatic brain injury: a discriminant analysis. J Head Trauma Rehabil. 2000;15:1103–12.
Kennedy JE, Jaffee MS, Leskin GA, et al. Posttraumatic stress disorder and posttraumatic stress disorder-like symptoms and mild traumatic brain injury. J Rehabil Res Dev. 2007;44:895–920.
King KA, Hough MS, Vos P, et al. Word retrieval following mild TBI: implications for categorical deficits. Aphasiology. 2006;20:233–45.
Malojcic B, Mubrin Z, Coric B, et al. Consequences of mild traumatic brain injury on information processing assessed with attention and short-term memory tasks. J Neurotrauma. 2008;25:30–7.
Milders M, Fuchs S, Crawford JR. Neuropsychological impairments and changes in emotional and social behaviour following severe traumatic brain injury. J Clin Exp Neuropsychol. 2003;25:157–72.
Moore EL, Terryberry-Spohr L, Hope DA. Mild traumatic brain injury and anxiety sequelae: a review of the literature. Brain Inj. 2006;20:117–32.
Raskin SA, Rearick E. Verbal fluency in individuals with mild traumatic brain injury. Neuropsychology. 1996;10:416–22.
Ryan LM, Warden DL. Post concussion syndrome. Int Rev Psychiatry. 2003;15:310–6.
Vanderploeg RD, Curtiss G, Luis CA, Salazar AM. Long-term morbidities following self-reported mild traumatic brain injury. J Clin Exp Neuropsychol. 2007;29:585–98.
Yang CC, Tu YK, Hua MS, Huang SJ. The association between the postconcussion symptoms and clinical outcomes for patients with mild traumatic brain injury. J Trauma. 2007;62:657–63.
Fear NT, Jones E, Groom M, et al. Symptoms of post-concussional syndrome are non-specifically related to mild traumatic brain injury in UK Armed Forces personnel on return from deployment in Iraq: an analysis of self-reported data. Psychol Med. 2008;39(8):1379–87.
Hoge CW, McGurk D, Thomas JL, et al. Mild traumatic brain injury in U.S. soldiers returning from Iraq. N Engl J Med. 2008;358:453–63.
Bigler ED. Mild traumatic brain injury: causality considerations from a neuroimaging and neuropathology perspective. In: Young G, Kane AW, Nicholson K, editors. Psychological knowledge in court: PTSD, pain, and TBI. New York, NY: Springer Science + Business Media; 2006. pp. 308–34.
Wilde EA, Bigler ED, Hunter JV, et al. Hippocampus, amygdala, and basal ganglia morphometrics in children after moderate-to-severe traumatic brain injury. Dev Med Child Neurol. 2007;49:294–9.
Gaylord KM, Cooper DB, Mercado JM, et al. Incidence of posttraumatic stress disorder and mild traumatic brain injury in burned service members: preliminary report. J Trauma. 2008;64:S200–5, discussion S205–6.
Chemtob CM, Muraoka MY, Wu-Holt P, et al. Head injury and combat-related posttraumatic stress disorder. J Nerv Ment Dis. 1998;186:701–8.
Mollica RF, Henderson DC, Tor S. Psychiatric effects of traumatic brain injury events in Cambodian survivors of mass violence. Br J Psychiatry. 2002;181:339–47.
Vasterling JJ, Constans JI, Hanna-Pladdy B. Head injury as a predictor of psychological outcome in combat veterans. J Trauma Stress. 2000;13:441–51.
Isaac CL, Cushway D, Jones GV. Is posttraumatic stress disorder associated with specific deficits in episodic memory? Clin Psychol Rev. 2006;26:939–55.
Constans JI. Information-processing biases in PTSD. In: Vasterling JJ, CR Brewin, editors. Neuropsychology of PTSD: biological, cognitive, and clinical perspectives. New York, NY: Guilford Press; 2005. pp. 105–30.
Buckley TC, Blanchard EB, Neill WT. Information processing and PTSD: a review of the empirical literature. Clin Psychol Rev. 2000;28:1041–65.
Karl A, Malta LS, Maercker A. Meta-analytic review of event-related potential studies in post-traumatic stress disorder. Biol Psychol. 2006;71:123–47.
Stroop JR. Studies of interference in serial verbal reactions. J Exp Psychol. 1935;18:643–62.
Cassiday KL, McNally RJ, Zeitlin SB. Cognitive processing of trauma cues in rape victims with post-traumatic stress disorder. Cogn Ther Res. 1992;16:283–95.
Foa EB, Feske U, Murdock TB, et al. Processing of threat-related information in rape victims. J Abnorm Psychol. 1991;100:156–62.
Kaspi SP, McNally RJ, Amir N. Cognitive processing of emotional information in posttraumatic stress disorder. Cogn Ther Res. 1995;19:433–44.
McNally RJ, Kaspi SP, Riemann BC, Zeitlin SB. Selective processing of threat cues in posttraumatic stress disorder. J Abnorm Psychol. 1990;99:398–402.
Williams JMG, Mathews A, MacLeod C. The emotional Stroop task and psychopathology. Psychol Bull. 1996;120:3–24.
Constans JI, McCloskey MS, Vasterling JJ, et al. Suppression of attentional bias in PTSD. J Abnorm Psychol. 2004;113:315–23.
Bryant RA, Harvey A. Posttraumatic stress reaction in volunteer fire fighters. Scand J Work Environ Health. 1996;19:121–5.
Buckley TC, Blanchard EB, Hickling EJ. Automatic and strategic processing of threat stimuli: a comparison between PTSD, panic disorder, and nonanxiety controls. Cogn Ther Res. 2002;26:97–115.
Bar-Haim Y, Lamy D, Pergamin L, et al. Threat-related attentional bias in anxious and nonanxious individuals: a meta-analytic study. Psychol Bull. 2007;133:1–24.
Mathews A, MacLeod C. Induced processing biases have causal effects on anxiety. Cogn Emot. 2002;16:331–54.
Mobini S, Grant A. Clinical implications of attentional bias in anxiety disorders: an integrative literature review. Psychother Theory Res Pract Training. 2007;44:450–62.
Friedman MJ. Pharmacological approaches to cognitive deficits associated with PTSD. In: Vasterling JJ, Brewin CR, editors. Neuropsychology of PTSD: biological, cognitive, and clinical perspectives. New York, NY: Guilford Press; 2005. pp. 292–325.
Friedman MJ, Davidson JRT. Pharmacotherapy for PTSD. In: Friedman MJ, Keane TM, Resick PA, editors. Handbook of PTSD: science and practice. New York, NY: Guilford Press; 2007. pp. 376–405.
Department of Veterans Affairs/Department of Defense. VA/DoD clinical practice guideline for the management of post-traumatic stress. Version 1.0. Washington, DC: Veterans Health Administration, Department of Defense; 2004.
American Psychiatric Association. Practice guidelines for the treatment of patients with acute stress disorder and posttraumatic stress disorder. American Psychiatric Association practice guidelines for the treatment of psychiatric disorders: compendium 2006. Arlington, VA: American Psychiatric Association; 2006. pp. 1003–71.
Friedman MJ, Davidson JRT, Mellman TA, Southwick SM. Psychotherapy. In: Foa EB, Keane TM, Friedman MJ, Cohen JA, editors. Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress Studies. New York, NY: Guilford Press; 2004. pp. 84–105.
Vermetten E, Vythilingam M, Southwick SM, et al. Long-term treatment with paroxetine increases verbal declarative memory and hippocampal volume in posttraumatic stress disorder. Biol Psychiatry. 2003;54:693–702.
Seedat S, Warwick J, van Heerden B, et al. Single photon emission computed tomography in posttraumatic stress disorder before and after treatment with a selective serotonin reuptake inhibitor. J Affect Disord. 2004;80:45–53.
Friedman MJ. What might the psychobiology of posttraumatic stress disorder teach us about future approaches to pharmacotherapy? J Clin Psychiatry. 2000;61(Suppl 7):44–51.
Nemeroff CB, Bremner JD, Foa EB, et al. Posttraumatic stress disorder: a state-of-the-science review. J Psychiatr Res. 2006;40:1–21.
Resick PA, Monson CM, Gutner C. Psychosocial treatments for PTSD. In: Friedman MJ, Keane TM, Resick PA, editors. Handbook of PTSD: science and practice. New York, NY: Guilford Press; 2007. pp. 330–58.
Institutes of Medicine. Treatment of PTSD: an assessment of the evidence. Washington, DC: Institutes of Medicine of the National Academies; 2007.
Bryant RA, Felmingham K, Kemp A, et al. Amygdala and ventral anterior cingulate activation predicts treatment response to cognitive behaviour therapy for post-traumatic stress disorder. Psychol Med. 2008;38:555–61.
Felmingham K, Kemp A, Williams L, et al. Changes in anterior cingulate and amygdala after cognitive behavior therapy of posttraumatic stress disorder. Psychol Sci. 2007;18:127–9.
Bryant RA, Felmingham K, Whitford TJ, et al. Rostral anterior cingulate volume predicts treatment response to cognitive–behavioural therapy for posttraumatic stress disorder. J Psychiatry Neurosci. 2008;33:142–6.
Wild J, Gur RC. Verbal memory and treatment response in post-traumatic stress disorder. Br J Psychiatry. 2008;193:254–5.
Shapiro DA. ‘Validated’ treatments and evidence-based psychological services. Clin Psychol (New York). 1996;3:256–9.
Cahill SP, Carrigan MH, Frueh BC. Does EMDR work? and if so, why?: a critical review of controlled outcome and dismantling research. J Anxiety Disord. 1999;13:5–33.
Perkins BR, Rouanzoin CC. A critical evaluation of current views regarding eye movement desensitization and reprocessing (EMDR): clarifying points of confusion. J Clin Psychol. 2002;58:77–97.
McNally RJ. EMDR and mesmerism: a comparative historical analysis. J Anxiety Disord. 1999;13:225–36.
Lindauer RJ, Booij J, Habraken JB, et al. Effects of psychotherapy on regional cerebral blood flow during trauma imagery in patients with post-traumatic stress disorder: a randomized clinical trial. Psychol Med. 2008;38:543–54.
Gold JI, Taft CT, Keehn MG, et al. PTSD symptom severity and family adjustment among female Vietnam veterans. Mil Psychol. 2007;19:71–81.
Jordan BK, Marmar CR, Fairbank JA, et al. Problems in families of male Vietnam veterans with posttraumatic stress disorder. J Consult Clin Psychol. 1992;60:916–26.
Taft CT, Schumm JA, Panuzio J, Proctor SP. An examination of family adjustment among Operation Desert Storm veterans. J Consult Clin Psychol. 2008;76:648–56.
Dekel R, Solomon Z. Marital relations among former prisoners of war: contribution of posttraumatic stress disorder, aggression, and sexual satisfaction. J Fam Psychol. 2006;20:709–12.
Sherman MD, Sautter F, Jackson MH, et al. Domestic violence in veterans with posttraumatic stress disorder who seek couples therapy. J Marital Fam Ther. 2006;32:479–90.
Taft CT, Street AE, Marshall AD, et al. Posttraumatic stress disorder, anger, and partner abuse among Vietnam combat veterans. J Fam Psychol. 2007;21:270–7.
Riggs DS, Byrne CA, Weathers FW, Litz BT. The quality of the intimate relationships of male Vietnam veterans: problems associated with posttraumatic stress disorder. J Trauma Stress. 1998;11:87–101.
Roberts WR. Interpersonal problems of Vietnam combat veterans with symptoms of posttraumatic stress disorder. J Abnorm Psychol. 1982;91:444–50.
Beckham JC, Lytle BL, Feldman ME. Caregiver burden in partners of Vietnam War veterans with posttraumatic stress disorder. J Consult Clin Psychol. 1996;64:1068–72.
Westerink J, Giarratano L. The impact of posttraumatic stress disorder on partners and children of Australian Vietnam veterans. Aust N Z J Psychiatry. 1999;33:340.
Lauterbach D, Bak C, Reiland S, et al. Quality of parental relationships among persons with a lifetime history of posttraumatic stress disorder. J Trauma Stress. 2007;20:161–72.
Samper RE, Taft CT, King DW, King LA. Posttraumatic stress disorder symptoms and parenting satisfaction among a national sample of male Vietnam veterans. J Trauma Stress. 2004;17:311–5.
Yehuda R, Halligan SL, Bierer LM. Relationship of parental trauma exposure and PTSD to PTSD, depressive and anxiety disorders in offspring. J Psychiatr Res. 2001;35:261–70.
Ben Arzi N, Solomon Z, Dekel R. Secondary traumatization among wives of PTSD and post-concussion casualties: distress, caregiver burden and psychological separation. Brain Inj. 2000;14:725–36.
Dirkzwager AJE, Bramsen I, Ader H, van der Ploeg HM. Secondary traumatization in partners and parents of Dutch peacekeeping soldiers. J Fam Psychol. 2005;19:217–26.
Goff BSN, Reisbig AMJ, Bole A, et al. The effects of trauma on intimate relationships: a qualitative study with clinical couples. Am J Orthopsychiatry. 2006;76:451–60.
Solomon Z, Waysman M, Levy G, et al. From front line to home front: a study of secondary traumatization. Fam Process. 1992;31:289–302.
Dirkzwager AJE, Bramsen I, van der Ploeg HM. Social support, coping, life events, and posttraumatic stress symptoms among former peacekeepers: a prospective study. Pers Individ Dif. 2003;34:1545–59.
King LA, King DW, Fairbank JA, et al. Resilience-recovery factors in post-traumatic stress disorder among female and male Vietnam veterans: hardiness, postwar social support, and additional stressful life events. J Pers Soc Psychol. 1998;74:420–34.
Monson CM, Rodriguez BF, Warner R. Cognitive– behavioral therapy for PTSD in the real world: do interpersonal relationships make a real difference? J Clin Psychol. 2005;61:751–61.
Monson CM, Schnurr PP, Stevens SP, Guthrie KA. Cognitive–behavioral couple’s treatment for posttraumatic stress disorder: initial findings. J Trauma Stress. 2004;17:341–4.
Sherman MD, Zanotti DK, Jones DE. Key elements in couples therapy with veterans with combat-related posttraumatic stress disorder. Prof Psychol Res Pr. 2005;36:626–33.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Vasterling, J.J., Grande, L., Graefe, A.C., Alvarez, J.A. (2019). Neuropsychological Assessment of Posttraumatic Stress Disorder (PTSD). In: Armstrong, C., Morrow, L. (eds) Handbook of Medical Neuropsychology. Springer, Cham. https://doi.org/10.1007/978-3-030-14895-9_27
Download citation
DOI: https://doi.org/10.1007/978-3-030-14895-9_27
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-14894-2
Online ISBN: 978-3-030-14895-9
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)