Abstract
Blepharoptosis occurs from congenitally or acquired mechanical, neurogenic, myogenic, or traumatic etiologies leading to drooping of the upper eyelid. Ptosis in elderly patients most commonly presents as dehiscence of the levator aponeurosis insertion and thinning of the aponeurotic fibers [1]. The aponeurotic repair of ptosis, originally described by Everbrush in 1883, grew in popularity in 1975 after Jones reported a new technique resecting a portion of the flaccid aponeurotic tissue [2]. The technique continued to be modified over time as the role of the disinsertion of the levator aponeurosis in involutional ptosis was more clearly understood [3].
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- External levator resection
- External levator advancement
- Levator aponeurosis
- Involutional ptosis
- Ptosis
- Congenital ptosis
- Small incision
- Blepharoptosis
Introduction
Blepharoptosis occurs from congenitally or acquired mechanical, neurogenic, myogenic, or traumatic etiologies leading to drooping of the upper eyelid. Ptosis in elderly patients most commonly presents as dehiscence of the levator aponeurosis insertion and thinning of the aponeurotic fibers [1]. The aponeurotic repair of ptosis , originally described by Everbrush in 1883, grew in popularity in 1975 after Jones reported a new technique resecting a portion of the flaccid aponeurotic tissue [2]. The technique continued to be modified over time as the role of the disinsertion of the levator aponeurosis in involutional ptosis was more clearly understood [3].
The most common surgical approaches of symptomatic involutional levator aponeurotic blepharoptosis include anterior approaches with the levator aponeurosis advancement or resection, tarsoaponeurectomy, modified small-incision levator repair, and posterior approaches with a conjunctival Müller’s muscle resection. The aim of these procedures targets reattaching the levator aponeurosis to the tarsal plate. This chapter aims to discuss the anterior surgical approaches for blepharoptosis including external levator advancement, levator resection, and small-incisional surgery.
Preoperative Evaluation
A careful history of trauma, duration of symptoms, progression, variation, and severity of ptosis should be documented to help assess the etiology of ptosis. Common complaints include decrease in peripheral vision, heaviness, forehead fatigability, or constant brow elevation and droopy eyelids. Prior ocular history should encompass previous eyelid or intraocular surgery, recurrent intravitreal injections, and surgical glaucoma history of trabeculectomy or glaucoma drainage implant device. Theoretical concern of placement of sutures through the palpebral conjunctiva or alteration of the eyelid margin could result in possible glaucoma drainage implant exposure, erosion, or bleb failure.
A thorough assessment and treatment of patients with dry eye complaints should be completed prior to surgery. All patients should be aware that dry eyes may occur or become more noticeable after surgery due to greater ocular surface exposure that may lead to increased tear film evaporation . Postoperatively, patients may benefit from a regimen of preservative-free artificial tears and eyelid hygiene . Patients with poor corneal integrity, lagophthalmos, or severe dry eyes despite medical management may experience worsening of symptoms after surgery and thus may wish to defer surgery or have a more conservative elevation. Punctal plugs or permanent punctal cautery before or after surgery can aid in patients with severe dry eye syndrome and corneal punctate keratopathy .
Clinical features to document include the location of the eyelid crease, presence of excess dermatochalasis or an epicanthal fold (Fig. 3.1), degree of ptosis, vertical palpebral fissure, marginal distance reflex, levator function, obstruction of pupil in downgaze (Fig. 3.2), fatigability, and Hering’s law. Complete obstruction of the pupil in downgaze, or less than 1 mm of vertical palpebral fissure in reading position, typically qualifies as visually significant.
Levator function is measured with a ruler held to the eyelid margin while the patient looks down and then in extreme upgaze, measuring the distance of maximal levator excursion in millimeters. It is important to eliminate the use of the frontalis muscle with the examiner’s hand to prevent the patient from using the forehead to elevate the eyelid (Fig. 3.3).
If unilateral or asymmetric ptosis is present and the ptotic eyelid manually lifted, the contralateral eyelid may become droopy, consistent with Hering’s law of equal innervation. If the contralateral eyelid droops enough to approach the visual axis, this would suggest that bilateral ptosis surgery should be performed. Beard’s classification of levator function has historically served as a surgical guideline for the degree of ptosis: with good levator function categorized as 8–16 mm of eyelid excursion, fair 5–7 mm, and poor being ≤4 mm of levator function [4]. For patients with fair to good levator function, aponeurotic advancement or repair serves as a good surgical option. Patients with mild to moderate ptosis (1–3 mm) that elevates after instillation of a drop of 2.5% or 10% phenylephrine on the ptotic side may be suitable for a posterior conjunctival Müller’s muscle resection (CMMR) . However, in instances where the ptosis is more severe or the patient has failed prior conjunctivomüllerectomy, additional elevation with an anterior levator approach may result in better outcomes and more subtle contour adjustments. Although some surgeons have performed repeat conjunctival Müller’s muscle resection with reportedly good results, the algorithms and outcomes may be less predictable. Myogenic (such as in chronic progressive external ophthalmoplegia, myotonic dystrophy, myasthenia gravis, or oculopharyngeal dystrophy) or involutional ptosis with poor levator function will often require a more conservative approach to minimize postoperative complications of dry eye syndrome, lagophthalmos, or exposure keratopathy.
Eyebrow ptosis and eyebrow asymmetry must be corrected concurrently with levator repair as patients postoperatively may otherwise perceive asymmetry or lack of ptosis improvement despite elevation of the actual margin-reflex distance (Fig. 3.4). Patients with frontalis muscle preference, raising one side of the forehead more prominently, may mask underlying eyebrow ptosis but may also feel that that side is more “open” after bilateral levator surgery. Excessive skin or dermatochalasis with concurrent ptosis should be assessed by taping up the excess skin or gently rolling the skin back with a cotton applicator to obtain accurate measurements of the upper eyelid crease position, vertical fissure height, and levator function.
For insurance authorization, clinical photographs and visual field defects showing substantial superior visual field constriction can aid in approval of surgical intervention and should be checked with the individual insurance prior to surgery. Conversations about patient expectations, postoperative care, and surgical risks that include bruising, bleeding, infection, asymmetry, need for additional surgery, recurrence, scarring, and loss of vision should also be thoroughly discussed.
Surgical Techniques and Variations
External Levator Aponeurosis Advancement
The goal of the external levator advancement , also called a levator repair , is to reattach the levator aponeurosis to its anatomic position along the anterior surface of tarsal plate, without resection of levator tissue. The indications for external levator advancement are generally for ptosis with fair to good levator excursion of at least 6 mm. Contraindications for external levator advancement include ptosis with poor or absent levator function. External levator advancement has achieved excellent outcomes with postoperative satisfaction as high as 80–94% with reoperation rates in 8–10% of patients [5]. When compared to the posterior approach conjunctivomüllerectomy (CMMR), both groups have been shown to perform equally in effectiveness [6].
Although surgical variations exist, in general, the eyelid incision is marked prior to local anesthetic infiltration, as this could stretch the soft tissues or cause ecchymosis that affects the accuracy of the eyelid markings. The surgical incision line is typically marked within the natural eyelid crease at 8–12 mm above the eyelid margin for females, 7–9 mm for males, and 4–6 mm for Asian eyelids (Fig. 3.5). Local infiltration of lidocaine 2% with 1:100,000 epinephrine, with or without a longer acting agent such as marcaine, is injected along the incision line to provide hemostasis and analgesia. It is important to inject no more than 1–1.5 mL of anesthetic in each eyelid and to place the same volume between the two sides, as larger and asymmetric volumes can cause temporary paresis of the levator and Müller muscles and thus make the dynamic intraoperative adjustment of eyelid height unreliable.
The incision can be made with a #15 blade scalpel, CO2 laser, and monopolar or radiofrequency cautery through the skin and orbicularis oculi . In patients in whom dry eyes or postoperative exposure may be a concern, or who have less levator function, the orbicularis muscle can be left intact without excision (if a skin blepharoplasty is concurrently performed) in order to facilitate eyelid closure (Fig. 3.6). Posterior to the preseptal orbicularis muscle lies the multilayered translucent orbital septum, and prolapse of the underlying preaponeurotic fat can be noted with gentle pressure on the globe. The orbital septum is then carefully opened to avoid injury to the underlying levator complex, and excessive preaponeurotic fat can be clamped with a curved hemostat and debulked or thermally shrunk with cautery. Gentle pushing with cotton-tipped applicators can also release the many fine septal attachments over the levator complex up toward Whitnall’s ligament. Often the levator muscle itself may demonstrate significant rarefication or fatty infiltration of the normal muscle (Fig. 3.7). The anterior superior tarsal surface is also dissected clean, taking care to minimize pretarsal dissection along the inferior half of the tarsus that could lead to postoperative eyelash ptosis (Fig. 3.8). Next, 2–3 sutures through the levator aponeurosis and partial-thickness superior tarsus with 6-0 Prolene or 5-0 nylon suture are placed above the central pupil, or at the lateral and medial limbus, to create the desired eyelid height and contour (Fig. 3.9). Typically, the suture is passed starting from the musculoaponeurotic junction to behind the levator muscle (anterior to Müller’s muscle), through the tarsus horizontally, and then back up behind the levator to exit several millimeters adjacent to the first pass. The suture is then cinched temporarily on the anterior surface of the levator aponeurosis. Note that placing the tarsal sutures too low in the tarsal plate may result in peaking of the eyelid margin, or eyelid margin ectropion off the globe surface. Therefore, the sutures should typically be passed in horizontal lamellar fashion through the upper one-third of the tarsus (Fig. 3.10). The eyelid should always be everted after each tarsal pass, to confirm that the suture is not exiting full-thickness, which would result in corneal abrasions (Fig. 3.11). Fine adjustments are made with the patient alert without sedation and sitting up to ensure adequate eyelid height and symmetry, as well as a natural curved contour without lateral retraction. Having the patient sitting up also allows for the natural forehead and eyebrow ptosis to manifest which affects the dynamics of the eyelid position. Eyelid closure should also demonstrate negligible lagophthalmos, or the sutures would need to be loosened. The sutures can be loosened to lower the medial or lateral margin, or tightened further to elevate the eyelid as desired, and then permanently tied without further cinching down the knot. The incision is closed with several interrupted eyelid crease reformation and orbicularis sutures with 6-0 polyglactin, followed by a running skin suture with 6-0 nylon or fast-absorbing plain gut suture.
Small-Incision External Levator Repair
While a longer skin excision allows for complete visualization of the upper eyelid anatomy, the benefits of a smaller incision are to decrease the operative area, resulting in less scarring, ecchymosis, edema, incidence of hematoma, as well as less anesthetic and surgical time [7]. Indications and contraindications are similar to those for external levator advancement , with patients with ptosis of good to fair levator function having best outcomes. Initially popularized by Lucarelli and Lemke in 1999, their outcomes using small-incision external levator surgery demonstrated effective eyelid correction without significant postoperative complications [8]. When compared to the traditional full external levator approach, the small-incisional technique has been shown to produce similar results with shorter operating times [9]. This approach is also an ideal option for those who have had prior blepharoplasty, or do not need skin removal such as if deep superior sulci are present (Fig. 3.12), in reoperations, or for those concerned about lengthy scarring.
Using a cotton-tipped applicator to assess the eyelid elevation at multiple sites, a small 8 mm skin incision is marked in the eyelid crease at the location that achieves best eyelid contour, followed by 0.5–1.0 mL of local infiltrative anesthesia (Fig. 3.13). The surgical steps are the same, but overall the operative field is more confined, which may be more technically challenging for less experienced surgeons. With retraction of the skin edges, dissection down through the pretarsal orbicularis allows for exposure of the superior tarsus (Fig. 3.14). Some surgeons prefer to further release the levator complex from the underlying Müller muscle, although this is not required. Using a spatulated needle on a 6-0 Prolene suture or a 5-0 nylon suture, the suture is passed starting from the musculoaponeurotic junction under the levator muscle, horizontally through partial-thickness superior tarsus, followed by passing the needle superiorly in the plane between the levator and Müller’s muscle to exit at the musculoaponeurotic junction and temporarily tied (Fig. 3.9). If the eyelid requires less elevation based on the preoperative margin-reflex distance, the suture can be placed lower than the musculoaponeurotic junction or higher on the tarsus to minimize the length of the hangback suture. Adjusting the suture tension with the patient in an upright position allows the eyebrows to rest in their natural position and more accurately reflect the eyelid height. An additional suture can be placed for contour if needed, even within the small incision. Once the eyelid height and contour are optimized, the suture can be clamped just under the knot with a needle driver to prevent the knot from cinching down further when tying down the suture permanently, which would thus inadvertently elevate the eyelid (Fig. 3.15). Eyelid crease reformation sutures are not required with this approach.
Levator Resection via External Approach
Indications for levator resection include patients with congenital, myogenic, or neurogenic severe ptosis with poor to fair levator function, often with structurally maldeveloped or abnormal levator muscles (Fig. 3.16). Levator resection surgery through the skin can result in greater eyelid elevation, as the levator aponeurosis and muscle are first resected and then further advanced to the tarsal surface [4]. Patients with good levator function should undergo levator advancement or posterior approach surgeries, and those with near-absent levator function require frontalis suspension surgery (frontalis sling). An external levator resection should also be used cautiously in Asian patients as an undesirable eyelid crease or double crease may be created.
The technique was initially described in 1953 by Johnson, with further modifications by Beard and others [9, 10]. Based on the degree of ptosis and measured levator function, many algorithms have been proposed to determine the amount of levator resection necessary (Table 3.1) [4, 11, 12]. Generally speaking, each quantitative technique serves as a guideline but each surgery requires individualization. In addition, it is often difficult to accurately measure levator function in children, which is reflected in the wide range of measurements seen in algorithms. This approach is primarily useful for congenital ptosis, often with fair or decreased levator function, as anterior levator resection can result in predictable eyelid elevation and clearance of the visual axis postoperatively [11, 13].
A major benefit of this technique in children, or adults with limited cooperation, is that the patient does not need to be awake during surgery for intraoperative suture adjustments. Contraindications would be the presence of a poor Bell’s reflex or elevator palsy that would limit upgaze and thus risk corneal integrity after surgery. Using the charts to determine the amount of resection, the levator aponeurosis and most of the levator muscle are excised, with horizontal mattress sutures placed just above the incision line so that the residual muscle stump can be advanced to the superior tarsus. Maximal or supramaximal levator aponeurosis resection involves removal up to or above Whitnall’s ligament, respectively, and is reserved for cases of severe ptosis with poor levator function [14]. External levator resection differs from an external levator advancement as the levator complex is actually excised, compared to imbricated, with reattachment to the superior tarsal plate.
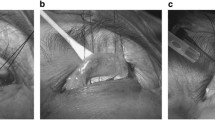
When performing a levator resection, a traction suture at the gray line of the eyelid margin can provide inferior traction to facilitate dissection. The orbital septum is opened and the entire levator aponeurosis dissected horizontally off the tarsus. Dissection is continued superiorly toward the fornix in a plane behind the levator muscle or encompassing both the levator and Müller muscles depending on surgeon preference (Fig. 3.17). The medial and lateral horns of the levator aponeurosis are incised vertically and widely toward the fornix, taking care to avoid injury to the lacrimal gland and avoid narrowing the proximal muscle base (Fig. 3.18). The elevated tissue is placed in a Berke ptosis clamp and the desired amount of tissue resection marked on the muscle with a surgical marker (Fig. 3.19). If more than 25–30 mm needs to be excised based on the severity of ptosis and decreased levator function, this may sometimes result in a resection that extends up to or past Whitnall’s ligament (Fig. 3.20). Prior to transecting the muscle at the markings, it is useful to secure the remaining portion of levator with sutures, such as 6-0 Prolene mattress sutures, so that the proximal stump does not retract and become difficult to locate after cutting. These sutures pass horizontally through the anterior superior tarsus to advance the levator muscle and elevate the eyelid. Alternatively, several 5-0 or 6-0 double-armed sutures (Prolene, nylon, chromic gut) can be first passed horizontally through the upper tarsus, and each of the suture arms passed upward behind the levator to exit at or just above the resection markings (Fig. 3.21). The double-armed sutures are tied as horizontal sutures to advance the levator muscle, followed by resection of the excess muscle (Fig. 3.22). Typically the desired eyelid margin height at the end of the procedure should rest at or above the superior limbus.
If the elevated eyelid creates a fold of skin over the margin that causes mechanical eyelash ptosis or entropion, then a thin strip of skin should be excised. The eyelid crease is reformed by suturing the orbicularis oculi muscle from the superior and inferior incision to the edge of the levator complex, followed by skin closure. Patients and families should be aware that postoperative lagophthalmos is not uncommon, but rather expected, following this technique, and therefore aggressive lubrication with tears and nighttime gel is often necessary.
Postoperative Care
Cold wet compresses applied frequently for the first 48 hours and mild analgesics help control postoperative pain. Patients should be instructed to call for severe deep, aching pain or visual loss that may be an early manifestation of an orbital hemorrhage . Antibiotic ointment is applied on the sutures three times a day for 1 week, which may blur vision temporarily. Nonabsorbable skin sutures , if used, should be removed approximately 5–10 days after surgery. Artificial tears can be used for mild ocular irritation or dry eye symptoms. Exercise and heavy lifting or bending are also avoided for 1 week after surgery to minimize bleeding complications.
The most common risks of anterior approach levator surgery , besides edema and ecchymosis, include undercorrection, overcorrection, asymmetric eyelid creases, scarring, lagophthalmos and dry eyes, or suboptimal eyelid contour. Although noted immediately after surgery, these are often difficult to distinguish from normal postoperative healing, and thus observation for a month may sometimes be helpful. Reoperation rates for levator advancement surgery have been reported to occur in 8.7% of cases within the first operative year and up to twice as likely to occur in patients undergoing bilateral surgery versus unilateral surgery [5]. On rare occasion, a unilateral surgery may unmask a previously undiagnosed Hering’s effect, such that the contralateral eyelid becomes ptotic postoperatively and requires secondary surgery.
In the first few weeks after surgery, if significant overcorrection or undercorrection is evident and edema is minimal, the incision can be opened in the office and the levator sutures adjusted as needed. Later reoperations, even up to 6 weeks postoperatively, have demonstrated similar adjustment outcomes; therefore, longer observation is reasonable to allow for more healing and spontaneous recovery [15].
Conclusion
Correction of eyelid blepharoptosis can be performed with various surgical techniques.
Anterior approaches with external levator advancement , small-incision levator repair, and levator resection all offer effective long-term outcomes with excellent eyelid height, contour, and function.
References
Anderson RL, Beard C. The levator aponeurosis. Attachments and their clinical significance. Arch Ophthalmol. 1977;95(8):1437–41.
Jones LT, Quickert MH, Wobig JL. The cure of ptosis by aponeurotic repair. Arch Ophthalmol. 1975;93:629–34.
Dortzbach RK, Sutula FC. Involutional blepharoptosis. A histopathological study. Arch Ophthalmol. 1980;98(11):2045–9.
Beard C. The surgical treatment of blepharoptosis: a quantitative approach. Trans Am Ophthalmol Soc. 1966;64:401–87.
McCulley T, Kersten RC, Kulwin DR, et al. Outcome and influencing factors of external levator palpebrae superioris aponeurosis advancement for blepharoptosis. Ophthal Plast Reconstr Surg. 2003;19:388–93.
Ben Simon GJ, Lee S, Schwarcz RM, et al. External levator advancement vs Müller’s muscle-conjunctival resection for correction of upper eyelid involutional ptosis. Am J Ophthalmol. 2005;140(3):426–32.
Baroody M, Holds JB, Sakamoto DK, et al. Small incision transcutaneous levator aponeurotic repair for blepharoptosis. Ann Plast Surg. 2004;52(6):558–61.
Lucarelli MJ, Lemke BN. Small incision external levator repair: technique and early results. Am J Ophthalmol. 1999;127(6):637–44.
Frueh BR, Musch DC, McDonald HM. Efficacy and efficiency of a small-incision, minimal dissection procedure versus a traditional approach for correcting aponeurotic ptosis. Ophthalmology. 2004;111(12):2158–63.
Johnson CC. Blepharoptosis: a general consideration of surgical methods; with the results in 162 operations. Am J Ophthalmol. 1954;38(2):129–62.
Berke RN. Results of resection of the levator muscle through a skin incision in congenital ptosis. Arch Ophthalmol. 1959;61:177.
Henderson JW. Present status of blepharoptosis surgery. Postgrad Med. 1963;33:153–8.
Göncü T, Çakmak S, Akal A, et al. Improvement in levator function after anterior levator resection for the treatment of congenital ptosis. Ophthal Plast Reconstr Surg. 2015;31(3):197–201.
Mauriello JA, Wagner RS, Caputo AR, Natale B, Lister M. Treatment of congenital ptosis by maximal levator resection. Ophthalmology. 1986;93(4):466–9.
Shore JW, Bergin DJ, Garrett SN. Results of blepharoptosis surgery with early postoperative adjustment. Ophthalmology. 1990;97(11):1502–11.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Tran, A.Q., Burkat, C.N. (2019). External Levator Advancement and Resection. In: Cohen, A., Burkat, C. (eds) Oculofacial, Orbital, and Lacrimal Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-14092-2_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-14092-2_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-14090-8
Online ISBN: 978-3-030-14092-2
eBook Packages: MedicineMedicine (R0)