Abstract
There are three accessory glands of the male genital system: the seminal vesicles, the prostate, and the bulbourethral glands. The seminal vesicles are paired structures on the posterolateral aspect of the base of the bladder, which secrete fluid that will form part of the semen. Aberrations of the proper development of the seminal vesicles can be seen during fetal life, and can occur in association with other genitourinary tract anomalies, owing to the close embryological origin of these complex tissues. Therefore, knowledge of the normal development and histological appearance of the seminal vesicle during fetal life can be useful. This chapter reviews the embryology of the seminal vesicles and highlights the histological features of the fetal seminal vesicles at various points in gestation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
There are three accessory glands of the male genital system : the seminal vesicles, the prostate , and the bulbourethral glands . The seminal vesicles are paired structures on the posterolateral aspect of the base of the bladder. Their main function is to secrete fluid that will form part of the semen; secretions of the seminal vesicles contain nutrients for the spermatozoa (such as fructose), as well as other proteins, enzymes, and mucus [1]. Because spermatozoa are not yet developed in fetal life, the physiological functions of the seminal vesicles are not necessary for the maintenance of life, but proper development of all the components of the male genital tract is important for future fertility. Aberrations of the proper development of the seminal vesicles, such as agenesis, fusion, duplication, hypoplasia, diverticulum, and cysts [2], can be seen during fetal life and can occur in association with other genitourinary tract anomalies, owing to the close embryological origin of these complex tissues. Therefore, knowledge of the normal development and histologic appearance of the seminal vesicle during fetal life can be useful. This chapter reviews the embryology of the seminal vesicles and highlights the histologic features of the fetal seminal vesicles at various points in gestation.
Embryology
The three accessory glands of the male genital system—the seminal vesicles, the prostate , and the bulbourethral glands—originate at the most caudal end of the mesonephric duct , where it joins the endodermally derived pelvic urethra. The seminal vesicles begin to develop in the 10th–12th weeks as bilateral, dorsolateral outpouchings from the mesonephric duct proximal to the prostatic outpouchings, at the angle between the vertical and horizontal portions of the duct [3, 4]. By the 13th week, the outpouchings enlarge, and distal constrictions are visible. These represent the beginning of the developing ejaculatory ducts [4], which will receive both the ampulla of the distal vas deferens and the ipsilateral seminal vesicle. Further development of the seminal vesicles occurs in fetal life, as described below.
Histology
General Overview
The overall appearance of the seminal vesicle is that of a coiled, tubular structure. The wall is composed of an epithelial layer, lamina propria , and muscularis . The mucosa of the adult seminal vesicle is extensively folded and alveolus-like [5]. These mucosal convolutions do begin to develop in fetal life and appear fairly significant by term, but they do not reach the complexity seen in adulthood. The mature seminal vesicle epithelium consists of a layer of luminal columnar, secretory cells with microvilli and an underlying layer of basal cells . Adult columnar epithelial cells contain lipofuscin pigment [5], which is not a feature seen in fetal seminal vesicles. The lamina propria is the connective-tissue layer beneath the basement membrane of the epithelium; it contains connective-tissue elements and blood vessels. The outer coat of the mature seminal vesicle comprises a thin, external longitudinal smooth-muscle layer and a thicker, internal circular smooth-muscle layer [5].
Second Trimester
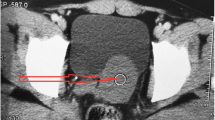
By 15 weeks gestation, the seminal vesicle anlage becomes “kinked” and consists of a medial, horizontal portion and a lateral, vertical portion [4]. In the early midtrimester, the lumen of the seminal vesicle shows only occasional diverticula, folds, or outpouchings; significant folding of the epithelium has not yet occurred (Figs. 13.1 and 13.2). The surrounding mesenchyme appears to be undifferentiated and consists of haphazardly arranged spindle-shaped cells (see Fig. 13.2). Later in the midtrimester, the seminal vesicle is more coiled, and the lumen develops more epithelial convolutions, which are especially noticeable in the distal half (Fig. 13.3) [4]. In addition, the mesenchyme surrounding the lumen matures, and early formation of the lamina propria and muscularis is seen (Fig. 13.4). The epithelium appears as a simple columnar type or a pseudostratified columnar type (Fig. 13.5).
Seminal vesicle at 17 weeks gestation. The architecture of the seminal vesicles (SV) appears to be similar to the ampulla of the vas deferens (V). The lumen shows minimal outpouchings. The surrounding mesenchyme is immature, with little definitive smooth-muscle differentiation (hematoxylin and eosin (H&E), 4×)
Seminal vesicle at 24 weeks gestation. This low-power image shows the overall architecture of the seminal vesicle, with increased coiling. The epithelium also shows increased outpouchings. The surrounding mesenchyme appears to show two indistinct layers: an inner, less-differentiated mesenchyme layer (lamina propria ) and the outer layer, showing more smooth-muscle differentiation (muscularis ) (H&E, 4×)
Third Trimester
In the early third trimester, the coiling of the seminal vesicle and folding of the epithelium increases (Fig. 13.6). The surrounding muscularis thickens and takes on a more eosinophilic appearance as smooth-muscle differentiation also increases. The lamina propria is distinct beneath the epithelium, containing tightly packed spindle cells without eosinophilia in their cytoplasm (Fig. 13.7). The epithelium may still appear pseudostratified, but the formation of two distinct layers can be seen as some cells along the basement membrane take on the appearance of basal cells (Fig. 13.8). As the third trimester progresses toward term, the epithelial folding increases to involve the majority of the organ, with the most prominent folding seen at term (Figs. 13.9, 13.10, 13.11, and 13.12). The epithelial differentiation into basal and columnar cells also becomes more apparent late in gestation.
References
Huggins C, Scott W, Heinen JJ. Chemical composition of human semen and of the secretions of the prostate and seminal vesicles. Am J Phys. 1942;136:467–73.
Arora SS, Breiman RS, Webb EM, Westphalen AC, Yeh BM, Coakley FV. CT and MRI of congenital anomalies of the seminal vesicles. AJR Am J Roentgenol. 2007;189:130–5.
Schoenwolf GC, Larsen WJ. Larsen’s human embryology. 4th ed. Philadelphia: Churchill Livingstone/Elsevier; 2009.
Brewster SF. The development and differentiation of human seminal vesicles. J Anat. 1985;143:45–55.
Trainer T. Testis and excretory duct system. In: Mills SE, editor. Histology for pathologists. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2012. p. 1003–26.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ernst, L.M., Ruchelli, E.D., Huff, D.S. (2019). Seminal Vesicle. In: Ernst, L., Ruchelli, E., Carreon, C., Huff, D. (eds) Color Atlas of Human Fetal and Neonatal Histology. Springer, Cham. https://doi.org/10.1007/978-3-030-11425-1_13
Download citation
DOI: https://doi.org/10.1007/978-3-030-11425-1_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-11424-4
Online ISBN: 978-3-030-11425-1
eBook Packages: MedicineMedicine (R0)