Abstract
The drastic reduction in the circulating levels of estrogens along the menopausal transition triggers a list of symptoms, where hot flashes (HF) constitute a frequently reported episode. Women describe hot flashes as a sudden feeling of heat affecting the upper body, trunk, head, and neck and spreading upwards or, less frequently, downwards. The whole phenomenon is described as a heat wave, which is accompanied by sweating and reddening of the skin, and that persists for short intervals, of minutes or even seconds. HF present during day and night and, when intense enough, affect the quality of sleep and provoke frequent waking-up episodes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
18.1 Introduction
The drastic reduction in the circulating levels of estrogens along the menopausal transition triggers a list of symptoms, where hot flashes (HF) constitute a frequently reported episode. Women describe hot flashes as a sudden feeling of heat affecting the upper body, trunk, head, and neck and spreading upwards or, less frequently, downwards. The whole phenomenon is described as a heat wave , which is accompanied by sweating and reddening of the skin, and that persists for short intervals, of minutes or even seconds. HF present during day and night and, when intense enough, affect the quality of sleep and provoke frequent waking-up episodes.
The prevalence of HF changes as a function of a series of variables, including the ethnic origin, climate, diet, the attitude to women’s role regarding reproduction, etc. (for a review, see [1]). Also, the intensity varies, with some women reporting only night sweats or very slight forms, which do not alter the quality of life.
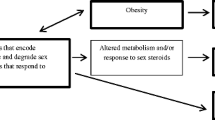
One interesting feature of HF is the accompanying vascular reactivity, which has been taken by investigators to use the more general and descriptive designation of vasomotor symptoms (VMS). Indeed, HF develop an initial vasodilation, occurring as a response to the heat wave, and are followed by subsequent vasoconstriction. These changes have been connected by some authors with altered function of the autonomic nervous system and associated with metabolic dysfunctions [2]. Accordingly, the question has been raised of whether a link might exist between susceptibility to VMS and the risk for cardiovascular disease (CVD).
The connections between HF and CVD, two apparently different categories, might be based in the well-known association between endothelial dysfunction and atherosclerotic risk, as shown in the 1980s and 1990s of the past century [3]. Based on those assumptions, pioneering work by British investigators showed that women suffering VMS had altered vasomotor responses, specifically diminished response to cold [4, 5], and increased blood flow in the upper limb during flushing episodes [6]. In a more recent study, Sassarini et al. found that subcutaneous vessels of women who flushed had a greater response to both endothelium-dependent and endothelium-independent vasodilator stimuli [7] than matched controls. Of specific interest, flushers had lower levels of high-density lipoprotein cholesterol (HDL-C) and apoA1 and higher levels of intercellular adhesion molecule-1 (ICAM-1). These changes have contributed to the conception that HF might be related with cardiovascular risk. Those changes might have an impact in cardiovascular risk and, secondarily, in other systems in the body.
18.2 Central Nervous System and HF
Women with HF do not appear to have lower levels of circulating estrogens than asymptomatic postmenopausal women, although the issue has not been adequately investigated. The main limiting factor is methodological, because very sensitive technology is required to adequately discriminate estrogen concentration when it is already low. In any case, and whichever the conditioning factor, the increased blood flow in the skin of women with HF involves neural mechanisms, either the reduction of the sympathetic-dependent constrictor action or the increase in the sympathetic cholinergic-dependent vasodilator activity.
There are abundant data suggesting that the narrowing of the thermoneutral zone in symptomatic women is associated with increased central noradrenergic activation. For example, neurons in the arcuate nucleus of symptomatic women are hypertrophied and show an increased expression of neurokinin B and kisspeptin (Fig. 18.1). The changes have been observed in female monkeys subjected to ovariectomy (for a review, see [8]). These neurons are involved in the regulation of GnRH pulses as well as in the induction of puberty.
There is hypertrophy of neurons expressing KiSS-1, NKB, substance P, dynorphin, and ERa mRNA in the infundibular nucleus concomitant with the decline of estrogens during menopause. Kisspeptin and NKB stimulate GnRH gene expression. With permission from Rance N. Peptides 2009; 30:111. Permission conveyed through Copyright Clearance Center, Inc.
It is of interest that work with rodent models has shown that projections of these neurons extend to the median preoptic nucleus, a crucial element in the CNS pathway regulating heat dissipation. All those neurons express the neurokinin-3 receptor (NK3R), which has been shown a role in the HF phenotype. Indeed, a recent clinical trial has made evident that women treated with an antagonist to the NK3R experiment a reduction in the number and severity of HF [9].
18.3 HF and Risk of Cardiovascular Disease
The link between vascular tone and atherosclerosis initiation and progression has raised questions about an association between HF and cardiovascular risk. The studies showing a differential response of vascular reactivity in women with HF [4, 6, 7], added to alterations in the lipidogram and higher levels of ICAM-1, have fed the hypothesis of a higher cardiovascular risk in women with HF. Subsequent cross-sectional American studies, like the Study of Women’s Health Across the Nation (SWAN), have confirmed association of VMS with established cardiovascular risk factors, like altered lipidogram or hypertension [10, 11].
Meanwhile, post hoc analyses from other American studies, like the Women’s Health Initiative (WHI) and the Heart and Estrogen/Progestin Replacement Study (HERS), showed that the association between hormone therapy (HT) and risk for CVD was modified not only by age but also by HF [12, 13]. Since then, several groups of investigators have increased their interest into the topic and have provided a wealth of extremely valuable data.
In a cross-sectional study, Lambrinoudaki et al. found that the carotid intima-media thickness (IMT), a recognized biomarker of atherosclerosis, was increased in women with HF as compared with matched controls of women with no or mild HF. The association was independent from well-known cardiovascular risk factors or circulating estrogen levels [14].
The SWAN study, which includes women who have been followed longitudinally for several years, has provided a wealth of interesting data. Subclinical parameters, including vascular reactivity or atherosclerosis imaging at the carotid (IMT) or the coronary (coronary artery calcium, CAC), have been explored and contrasted with the HF phenotype. Both cross-sectional and longitudinal studies, led by the group of R Thurston at the University of Pittsburg, have confirmed the association of VMS with subclinical atherosclerosis indicators (for a review, see [15]). Furthermore, longitudinal studies have disclosed that duration of VMS was more clearly determining the association with CVD risk indicators, the association being then replicated in other big cardiovascular studies, like the Women’s Ischemia Syndrome Evaluation (WISE) [16]. These data are consistent with studies that along the latter years have shown an association between the fall in estrogens and initial steps of atherosclerosis, such as endothelial function parameters [17].
In a more sophisticated step, Thurston and cols have prospectively followed a group of 300 non-smoking midlife women in the MsHeart Study. VMS were recorded with the use of electronic digital diaries and physiologic monitoring with appropriate sensors. The study confirmed that VMS were related with IMT values and plaque identification, and that the association was above traditional CV risk factors or circulating estrogens [18].
18.4 Conclusion
Evidence in favor of VMS as marker of cardiovascular vulnerability accumulates as a result of studies from different groups. Despite so, the key question of the pathophysiological link remains elusive. Some data suggest that it is the VMS during the early menopause that seem determinant. This hypothesis agrees with recent data giving relevance to the lipid changes during the initiation of menopause transition as a key determinant variable for later IMT increase [19]. The assumption might be that, if the menopausal transition seems a vulnerability window, and changes in lipids and other cardiovascular risk factors seem to occur in association with VMS during that period, a potential link might exist. Parallel to lipid changes, some studies have found that alterations in the control mechanisms in the autonomic nervous system, with increased sympathetic or reduced parasympathetic control of heart rate variability, occur during HF. Those changes in the autonomic system have been linked with cardiovascular risk [20]. But, still, the association of VMS with those lipid or nervous system changes is not clearly understood.
Another option might consider the sequence of altered vascular wall reactivity leading to atherosclerosis, an interpretation already maintained for years to explain the estrogenic protective role. There are abundant data showing the association of VMS with vascular reactivity dysfunctions, but, still, more consolidated evidence is required.
References
Llaneza P. Clinical symptoms and quality of life: hot flashes and mood. In: Menopause, a comprehensive approach. New York, NY: Springer; 2017.
Archer DF, Sturdee DW, Baber R, de Villiers TJ, Pines A, Freedman RR, Gompel A, Hickey M, Hunter MS, Lobo RA, Lumsden MA, MacLennan AH, Maki P, Palacios S, Shah D, Villaseca P, Warren M. Menopausal hot flushes and night sweats: where are we now? Climacteric. 2011;14(5):515–28.
Ross R. Atherosclerosis--an inflammatory disease. N Engl J Med. 1999;340(2):115–26.
Rees MC, Barlow DH. Absence of sustained reflex vasoconstriction in women with menopausal flushes. Hum Reprod. 1988;3(7):823–5.
Brockie JA, Barlow DH, Rees MC. Menopausal flush symptomatology and sustained reflex vasoconstriction. Hum Reprod. 1991;6(4):472–4.
Ginsburg J, Hardiman P, O’Reilly B. Peripheral blood flow in menopausal women who have hot flushes and in those who do not. BMJ. 1989;298(6686):1488–90.
Sassarini J, Fox H, Ferrell W, Sattar N, Lumsden MA. Vascular function and cardiovascular risk factors in women with severe flushing. Clin Endocrinol (Oxf). 2011;74(1):97–103.
Rance NE, Dacks PA, Mittelman-Smith MA, Romanovsky AA, Krajewski-Hall SJ. Modulation of body temperature and LH secretion by hypothalamic KNDy (kisspeptin, neurokinin B and dynorphin) neurons: a novel hypothesis on the mechanism of hot flushes. Front Neuroendocrinol. 2013;34(3):211–27.
Prague JK, Roberts RE, Comninos AN, Clarke S, Jayasena CN, Nash Z, Doyle C, Papadopoulou DA, Bloom SR, Mohideen P, Panay N, Hunter MS, Veldhuis JD, Webber LC, Huson L, Dhillo WS. Neurokinin 3 receptor antagonism as a novel treatment for menopausal hot flushes: a phase 2, randomised, double-blind, placebo-controlled trial. Lancet. 2017;389(10081):1809–20.
Thurston RC, El Khoudary SR, Sutton-Tyrrell K, Crandall CJ, Gold EB, Sternfeld B, Joffe H, Selzer F, Matthews KA. Vasomotor symptoms and lipid profiles in women transitioning through menopause. Obstet Gynecol. 2012;119(4):753–61.
Jackson EA, El Khoudary SR, Crawford SL, Matthews K, Joffe H, Chae C, Thurston RC. Hot flash frequency and blood pressure: data from the study of women’s health across the nation. J Womens Health (Larchmt). 2016;25(12):1204–9.
Rossouw JE, Prentice RL, Manson JE, Wu L, Barad D, Barnabei VM, Ko M, LaCroix AZ, Margolis KL, Stefanick ML. Postmenopausal hormone therapy and risk of cardiovascular disease by age and years since menopause. JAMA. 2007;297(13):1465–77.
Huang AJ, Sawaya GF, Vittinghoff E, Lin F, Grady D. Hot flushes, coronary heart disease, and hormone therapy in postmenopausal women. Menopause. 2009;16(4):639–43.
Lambrinoudaki I, Augoulea A, Armeni E, Rizos D, Alexandrou A, Creatsa M, Kazani M, Georgiopoulos G, Livada A, Exarchakou A, Stamatelopoulos K. Menopausal symptoms are associated with subclinical atherosclerosis in healthy recently postmenopausal women. Climacteric. 2012;15(4):350–7.
Thurston RC. Vasomotor symptoms: natural history, physiology, and links with cardiovascular health. Climacteric. 2018;2:1–5.
Thurston RC, Johnson BD, Shufelt CL, Braunstein GD, Berga SL, Stanczyk FZ, Pepine CJ, Bittner V, Reis SE, Thompson DV, Kelsey SF, Sopko G, Bairey Merz CN. Menopausal symptoms and cardiovascular disease mortality in the Women’s Ischemia Syndrome Evaluation (WISE). Menopause. 2017;24(2):126–32.
Bechlioulis A, Kalantaridou SN, Naka KK, Chatzikyriakidou A, Calis KA, Makrigiannakis A, Papanikolaou O, Kaponis A, Katsouras C, Georgiou I, Chrousos GP, Michalis LK. Endothelial function, but not carotid intima-media thickness, is affected early in menopause and is associated with severity of hot flushes. J Clin Endocrinol Metab. 2010;95(3):1199–206.
Thurston RC, Chang Y, Barinas-Mitchell E, Jennings JR, Landsittel DP, Santoro N, von Känel R, Matthews KA. Menopausal hot flashes and carotid intima media thickness among midlife women. Stroke. 2016;47(12):2910–5.
Matthews KA, El Khoudary SR, Brooks MM, Derby CA, Harlow SD, Barinas-Mitchell EJ, Thurston RC. Lipid changes around the final menstrual period predict carotid subclinical disease in postmenopausal women. Stroke. 2017;48(1):70–6.
Thurston RC, Christie IC, Matthews KA. Hot flashes and cardiac vagal control: a link to cardiovascular risk? Menopause. 2010;17(3):456–61.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 International Society of Gynecological Endocrinology
About this chapter
Cite this chapter
Hidalgo-Mora, J.J., Dudenko, D., Ruiz-Vega, S., Cano, A. (2019). Symptoms and Hormones: Fine-Tuning Atherosclerotic Risk?. In: Brinton, R., Genazzani, A., Simoncini, T., Stevenson, J. (eds) Sex Steroids' Effects on Brain, Heart and Vessels. ISGE Series. Springer, Cham. https://doi.org/10.1007/978-3-030-11355-1_18
Download citation
DOI: https://doi.org/10.1007/978-3-030-11355-1_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-11354-4
Online ISBN: 978-3-030-11355-1
eBook Packages: MedicineMedicine (R0)