Abstract
Diverticular disease affects one in three people over the age of 60 in Western countries and the incidence appears to be increasing. Up to a quarter of these patients will develop diverticulitis. Most cases of diverticulitis are uncomplicated and respond to conservative medical therapy but complications such as free perforation, abscess or fistula may require emergency intervention.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Diverticular disease affects one in three people over the age of 60 in Western countries and the incidence appears to be increasing. Up to a quarter of these patients will develop diverticulitis. Most cases of diverticulitis are uncomplicated and respond to conservative medical therapy but complications such as free perforation, abscess or fistula may require emergency intervention.
A percentage of patients managed conservatively at initial presentation will require subsequent elective sigmoid resection. Indications for this procedure have evolved over recent years. Previous guidelines suggested that sigmoid colectomy was indicated after two or more attacks of diverticulitis. This approach has been challenged, with recent natural history data suggesting that the majority of patients will not suffer recurrent attacks [1]. As a result, the number of attacks of recurrent diverticulitis is no longer considered a dogmatic indication for surgery [2]. Rather, the decision to operate for recurrent acute diverticulitis is determined on an individual basis, considering the level of symptoms and the patient’s age and comorbidity. Though the natural history data are somewhat controversial, most surgeons maintain a lower threshold for operation after a conservatively managed episode of complicated diverticulitis, recommending surgery after the initial complicated episode.
Laparoscopic colectomy has been utilised for over two decades. A number of large, randomised controlled trials of laparoscopic colectomy for cancer have demonstrated short-term benefits for patient recovery [3]. To date, there have been no randomised trials of laparoscopic colectomy for diverticular disease, although non-randomised evidence supports its efficacy and safety in selected patients [4]. The laparoscopic approach can be more technically challenging with diverticular disease than with malignant disease because of the recurrent inflammation and fibrosis. Significant experience in laparoscopic surgery and appropriate patient selection are required to maintain the benefits of the laparoscopic approach with acceptably low morbidity rates.
This chapter describes laparoscopic sigmoid colectomy performed for recurrent diverticulitis. There is some variation in reported techniques for this procedure, such as the approach to left colonic mobilisation, the level of vascular ligation and the necessity of splenic flexure mobilisation. These controversies are discussed in the text but it is important for the surgeon to be adept in all these techniques, as the pathology encountered in diverticular disease may necessitate altering or combining these approaches intraoperatively in order to ensure successful completion of the procedure laparoscopically.
9.1 Procedure
A Fleet enema is given preoperatively, rather than full oral bowel preparation. Intrathecal morphine injection is performed prior to induction of general anaesthesia. Thromboprophylaxis is provided with thromboembolism-deterrent (TED) stockings, sequential compression devices and then subcutaneous low molecular weight heparin at 6 h after the intrathecal morphine injection.
The patient is placed in the modified Lloyd-Davies position on a suction beanbag to ensure secure immobilisation on the operating table during subsequent intraoperative Trendelenburg tilt. It is important that the hips are not flexed, so that the right thigh does not impede the laparoscopic instruments during left colonic and splenic flexure mobilisation. The laparoscopic tower is positioned near the patient’s left foot and, for simplicity and consistency, the necessary cables and tubing are all run off the left leg.
Capnoperitoneum is achieved using an infraumbilical open Hasson technique. A 12-mm trocar is placed in the right iliac fossa 3–4 cm superior and medial to the anterior superior iliac spine, usually lateral to the inferior epigastric vessels, which must be avoided during trocar placement. Two 5-mm trocars are placed: one in the left paraumbilical region and the other on the right, one handbreadth superior and slightly medial to the 12-mm trocar, as demonstrated in Fig. 9.1. Additional 5-mm trocars can be placed in the suprapubic region or epigastric region as required. An epigastric trocar will facilitate splenic flexure mobilisation in particular, entering the lesser sac when reflecting the gastrocolic omentum (see Fig. 9.5). A suprapubic trocar will allow further retraction, if necessary, both in the pelvis and when dissecting around the inferior mesenteric artery (IMA).
The operating surgeon is positioned on the patient’s right side; the first assistant, operating the camera, is positioned to the left of the operating surgeon. At least one further monitor at the patient’s left shoulder is also useful. The authors recommend the use of a 30° scope as it provides a superior view at several critical points during the laparoscopic procedure.
To mobilise the left colon commencing with a lateral approach, the patient is positioned in Trendelenburg and tilted to the right. Congenital adhesions of the sigmoid colon to the lateral abdominal wall are divided. The authors favour an ultrasonic dissector, although scissors, monopolar diathermy or other energy devices can be utilised for dissection during this procedure. Using atraumatic bowel graspers the sigmoid colon is retracted medially, allowing identification of the left ureter (Fig. 9.2). The sigmoid mesocolon is dissected off the retroperitoneum medial to the left ureter. This dissection is continued to the descending colon along the white line of Toldt and into the avascular plane between the mesocolon and Gerota’s fascia. The descending colon should be manipulated both anteriorly and medially to assist with retraction of the small bowel. In the cephalad direction, the descending colon is mobilised as far as the splenic flexure. As the dissection proceeds medially, the operator identifies the lateral aspect of the IMA and preserves the sympathetic nerve branches running just posterior and lateral to this artery.
In the setting of diverticular disease, an inflammatory phlegmon or dense fibrosis can make identification of the left ureter at the pelvic brim difficult. In this situation, the operator should commence mobilisation in the least affected area, at either the descending colon or the lateral aspect of the mesorectum in the pelvis. Alternatively, mobilisation can be commenced using a medial to lateral approach, as demonstrated in Fig. 9.3.
To commence the medial dissection, the assistant retracts the rectosigmoid junction anteriorly and to the left, to apply tension to the medial aspect of the sigmoid mesocolon. The small bowel must be positioned in the left upper quadrant. The sacral promontory is identified and the peritoneum is incised anterior to this promontory and just posterior to the IMA. The peritoneal incision is continued just posterior to the IMA towards its origin. The line of this incision is relatively parallel to the axis of the aorta from the pelvic brim to the IMA origin.
With the peritoneum incised, placing the grasper under the IMA and lifting it anteriorly permits dissection deep to the IMA, ensuring that the sympathetic nerves fall back and remain in the retroperitoneum. This dissection will eventually communicate with the lateral dissection, where the left ureter can be identified once again in the retroperitoneum.
Depending on the extent of resection, the IMA can be taken high, proximal to the left colic arterial branch or at a level distal to this. High ligation requires dissection to near the origin of the IMA (Fig. 9.4). If this mobilisation has been adequate, the IMA should be able to be elevated to a right angle from the aorta. Once again, care must be taken not to damage the sympathetic nerve plexuses. A window is created in the mesocolon between the IMA and inferior mesenteric vein (IMV). This manoeuvre can be challenging; careful blunt dissection with right-angle forceps around the IMA origin can facilitate the creation of the window. Appropriate use of the 30° scope is also beneficial at this point. The IMA is divided with an endoscopic vascular stapling device. Endoloop® ligatures (Ethicon Endo-Surgery) should be available in the operating theatre and the surgeon should grasp the proximal stump of the vessel prior to releasing the stapler. If the unusual situation arises that haemostatic control of the vessel has not been adequate with stapling, on releasing the stapler, an Endoloop can be applied immediately. Alternative methods of securing the IMA include haemostatic clips or energy devices. It is the authors’ opinion that endoscopic staplers or clips, used correctly, provide more reliable haemostasis than currently available energy devices.
The IMV lies in the tissue lateral to the divided IMA. The IMV is dissected to near the inferior border of the pancreas. To complete this dissection, mobilisation of the duodeno-jejunal flexure medially will facilitate exposure. Once again a window is created lateral to the IMV and division performed using an endoscopic vascular stapling device.
In cases requiring less extensive colonic resection, it may be possible to divide the IMA distal to the left colic artery. At this level, the IMV will still be running closely opposed to the IMA and both vessels can be controlled in a single firing of an endoscopic vascular stapler.
Prior to commencing splenic flexure mobilisation, the operating table should be returned to level with the right tilt maintained. The first assistant should move between the patient’s legs and grasp the transverse colon to the left of the middle colic vessels, retracting it inferiorly. The operating surgeon then reflects the omentum superiorly and enters the lesser sac, dissecting the omentum off the transverse colon to the splenic flexure (Fig. 9.5a). A further 5-mm port placed in the epigastrium may facilitate this manoeuvre (see Fig. 9.1). Dissection of the phrenocolic attachments is then continued around the splenic flexure until the dissection eventually communicates with the lateral dissection on Gerota’s fascia. Placing the patient in reverse Trendelenburg at this point may assist with exposure. Further attachments at the lateral aspect of the lesser sac are divided until the splenic flexure is completely mobile (Fig. 9.5b). The ultrasonic dissector will often need to be switched between the right iliac fossa port and the left para-umbilical port to complete this manoeuvre.
Depending on the extent of resection required, mobilisation of the splenic flexure may not be mandatory although it is usually required. In patients with distal sigmoid disease and a redundant sigmoid and descending colon, sufficient length of bowel for tension-free anastomosis to the upper rectum can be achieved without splenic flexure mobilisation.
Attention is now returned to the pelvic brim. The first assistant resumes his or her original position and the patient is once again placed in Trendelenburg with right tilt. The rectosigmoid is grasped and retracted anteriorly and to the left. Using an open atraumatic grasper, the upper mesorectum is elevated, opening the extrafascial plane and the upper rectum is dissected in this plane, preserving the hypogastric nerves (Fig. 9.6). The dissection is continued around to the lateral aspects of the mesorectum. To expose the left lateral aspect, the rectosigmoid will need to be retracted to the right and posteriorly. The left ureter should be clearly re-identified at this point. The mesorectum is transected using the ultrasonic dissector to produce a clean muscular tube suitable for transection.
To minimise recurrence, the surgeon must ensure that the point of distal transection is at a point on the rectum where there is healthy, non-inflamed bowel. This point is usually at the upper rectum, which is identified by the coalescence of the taeniae coli at the pelvic brim. An articulating endoscopic stapling device is introduced through the right iliac fossa port and positioned across the upper rectum (Fig. 9.7). With adequate preparation of the rectum, a 45-mm device will usually be sufficient to transect the upper rectum with a single firing. Extensive inflammation or fibrosis may necessitate more distal transection of the rectum. In this situation, the stapler can be introduced through a 12-mm suprapubic port, transecting the rectum in the sagittal plane.
Rectal transection can be performed through a Pfannenstiel incision created for specimen extraction using conventional open stapling devices or a hand-sewn technique. In the authors’ opinion, a superior view is achieved laparoscopically, allowing a more satisfactory double-stapled anastomosis. Adequate exposure to perform the anastomosis through the incision generally requires it to be extended well beyond the 4–5 cm required for specimen extraction.
Following intracorporeal rectal transection, a small incision is created to exteriorise and resect the colon, and then prepare the proximal end for anastomosis (Fig. 9.8). For this purpose, the authors prefer a short (4–5 cm) Pfannenstiel incision, although left iliac fossa incisions are also commonly described.
A plastic wound retractor maximises exposure through this small incision and also provides wound protection. Following placement of the retractor and exteriorisation of the mobilised colon, the remaining mesocolon is divided from the point of transection of the IMA to the point chosen for transection in the left colon.
The exact level of proximal transection chosen will depend on the degree of involvement with diverticular disease. There is no evidence that more extensive resections prevent recurrence, but from a pragmatic point of view, the resection does need to extend to a point where there is a relative paucity of diverticula, to allow a satisfactory anastomosis to be performed. Therefore, cases of extensive left colonic involvement will require resection well onto the descending colon, necessitating the full left colonic mobilisation described to this point. The blood flow in the marginal artery is checked prior to ligation of this vessel to ensure that adequate pulsatile flow is present.
Following division of the bowel at the appropriate point, the anvil of a circular stapling device is secured using a purse-string suture.
As mentioned, the laparoscopic view of the colorectal anastomosis is generally superior to that obtained through a Pfannenstiel incision, so the authors prefer to complete the anastomosis intracorporeally.
The colon is replaced in the abdominal cavity and held using a grasper introduced through a right-sided trocar. The plastic retractor is sealed and capnoperitoneum is reinstituted. With the patient in Trendelenburg, a satisfactory laparoscopic view of the pelvis is obtained. A second assistant introduces the circular stapling device per rectum and manipulates it under laparoscopic vision to the rectal staple line. The spike of the stapling device should be brought through the rectum immediately adjacent to (but not directly through) the rectal staple line. The surgeon must carefully check the orientation of the colon prior to anastomosis, ensuring that there has not been a 360° rotation during manipulation. Grasping the anvil of the stapler with a laparoscopic grasper prior to reinstitution of the capnoperitoneum, as described, will help maintain the correct orientation of the colon. With the correct orientation confirmed, the components of the stapler are engaged and anastomosis completed (Fig. 9.9).
The anastomotic “doughnuts” are checked, confirming that both contain an intact ring of the full thickness of the intestinal wall. The integrity of the anastomosis is routinely checked by leak testing. The pelvis is filled with normal saline and air is insufflated into the rectum whilst occluding the bowel above the anastomosis. If an air leak is identified the anastomosis must be carefully inspected to identify its exact source. The options to deal with a leak include oversewing the staple line in that area or redoing the anastomosis. In the setting of a major leak or other associated technical problems, the anastomosis may need to be completely taken down and reanastomosis performed. More often, the staple line can be oversewn at the point of the leak with several interrupted sutures. Following the repair, the leak test is repeated. Even if the subsequent leak test is negative, the authors routinely perform a temporary defunctioning ileostomy to protect an anastomosis that has required repair in this fashion.
Following anastomosis, the abdomen is inspected to ensure haemostasis is satisfactory. Assessment of tension on the anastomosis is best performed with the patient level, as steep Trendelenburg can produce a false impression that the anastomosis is under tension. The surgeon should also take particular care to ensure that the small bowel has not worked its way between the neo-descending colon and the retroperitoneum, as this can be a cause of early postoperative small bowel obstruction. Drains are not routinely used for intraperitoneal anastomosis.
The trocars are removed. The 12-mm trocar sites are closed at the fascial level with 0 absorbable suture but the 5-mm trocar sites are not routinely closed (Fig. 9.10). The Pfannenstiel incision is closed in layers.
The patient is managed postoperatively according to enhanced recovery principles. These include early oral feeding, mobilisation and minimal intravenous fluids, with the goal of discharge at postoperative day 3–4.
9.2 Results
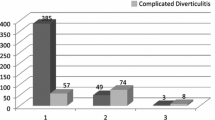
Laparoscopic sigmoid colectomy is now widely employed in the setting of diverticular disease. Nevertheless, there are no randomised trials to support its use. A meta-analysis of 19,608 patients from non-randomised studies demonstrated reduced infective, pulmonary, gastrointestinal and cardiovascular complications and a shorter hospital stay with laparoscopic surgery [4]. A more recent multicentre, prospective study comparing laparoscopic and open sigmoid colectomy for diverticular disease also showed reduced complications and hospital stay after laparoscopic surgery [5]. Selection bias is likely to have played a significant role in the outcomes in these non-randomised studies, enhancing the results seen in the laparoscopic groups.
Studies have consistently demonstrated that operative time is significantly longer for laparoscopic surgery and conversion rates are approximately 15%. Given the evidence from randomised colorectal cancer trials that patients undergoing conversion have a worse outcome, patient selection for a laparoscopic approach in diverticular disease is crucial to minimise conversion rates and morbidity.
The surgeon must be aware of the possibility of significant inflammation and fibrosis associated with the diverticular disease, especially after complicated attacks involving abscess, perforation or fistula. This can produce technical challenges in laparoscopic colectomy. Surgery for diverticular disease is commonly more technically difficult than that required for colon cancer because of the repeated episodes of inflammation leading at times to dense fibrosis and scarring. If this situation is anticipated from preoperative imaging and colonoscopy, an open approach may be more suitable. Intraoperatively, fibrosis can cause particular difficulty with identification of the left ureter, as shown in Fig. 9.2. This is a critical step in the procedure; if ureteric identification is not possible despite the manoeuvres suggested, conversion to an open procedure will be necessary. If difficulty with this step is anticipated, insertion of ureteric catheters may be useful.
Hand-assisted laparoscopic surgery has been advocated in difficult diverticular resections. This approach may facilitate dissection in experienced hands and can be used as a planned approach from the commencement of the procedure. Caution should be exercised in the use of a hand port by surgeons inexperienced in hand-assisted laparoscopic surgery in an attempt to avoid conversion. In this setting, introduction of a hand port may simply prolong the procedure and delay the eventual conversion.
This chapter has described sigmoid colectomy for recurrent diverticulitis performed in an elective setting. In the acute setting, with perforated diverticulitis and peritonitis, surgical options include lavage or resection with or without anastomosis. Several series document successful outcomes after simple laparoscopic lavage without resection in cases of generalised peritonitis [6]. However, doubt remains about which patients can be safely selected for this approach, and the gold standard remains resection. Primary anastomosis can be performed after resection in selected patients but those who are unwell, with sepsis and faecal peritonitis, will require Hartmann’s procedure. In the acute setting, laparoscopic Hartmann’s procedure is rarely performed. One small case series has reported successful outcomes [7] but most surgeons would advocate an open procedure in this setting with severe inflammation, peritonitis and systemic sepsis.
As with perforation, the other complicated presentations of diverticulitis are not well suited to a laparoscopic approach. Most diverticular abscesses are dealt with by percutaneous drainage. If this approach is not suitable, laparoscopy is unlikely to be a viable alternative. Colovesical fistulas are managed by resection of the involved sigmoid colon and repair of what is usually a small bladder defect. This procedure is feasible laparoscopically, although the fistula itself may be best dealt with through a Pfannenstiel incision or hand port. Hence laparoscopic sigmoid colectomy for diverticular disease is presently most appropriate in the elective setting when surgery has been deemed necessary for recurrent diverticulitis.
9.3 Conclusions
Significant variation in the technique of laparoscopic sigmoid colectomy remains for all pathologies. This variation was highlighted in a recent survey of 292 surgeons performing laparoscopic colectomy, which found strong consensus in only 1 of 20 technical details [8]. Contentious points included the approach to mobilisation of the left colon (lateral versus medial), the necessity of splenic flexure mobilisation, the optimal timing of ligation of the IMA and the technique of anastomosis.
A standard approach to sigmoid colectomy has been presented here but the nature of the pathology in diverticular disease may require adaptation of this approach to deal with significant inflammation and fibrosis. For example, the laparoscopic surgeon embarking on diverticular resection should be sufficiently experienced to be adept at both lateral and medial laparoscopic approaches to the left colon, as a combination of both may be required.
The key point in the resection for diverticulitis is the removal of the diseased sigmoid colon. It is not necessary to resect all proximal diverticula but simply to identify a segment of colon with sufficiently few diverticula to permit safe colorectal anastomosis. In contrast, the distal resection must be to the level of at least the upper rectum, as leaving distal sigmoid has been shown to produce higher recurrence rates. The rectum must be pliable and free of inflammation; in cases of distal sigmoid involvement, transection at the level of the mid or even low rectum may be necessary.
With appropriate patient selection and surgeon experience, laparoscopic sigmoid colectomy is a feasible and safe procedure that has potential benefits for patient recovery. Advances in technology and operative technique are likely to continue the increased adoption of this technique in the future.
References
Eglinton T, Nguyen T, Raniga S, et al. Patterns of recurrence in patients with acute diverticulitis. Br J Surg. 2010;97:952–7.
Rafferty J, Shellito P, Hyman NH, et al. Practice parameters for sigmoid diverticulitis. Dis Colon Rectum. 2006;49:939–44.
Schwenk W, Haase O, Neudecker J, et al. Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev. 2005;2005:CD003145.
Purkayastha S, Constantinides VA, Tekkis PP, et al. Laparoscopic vs. open surgery for diverticular disease: a meta-analysis of nonrandomized studies. Dis Colon Rectum. 2006;49:446–63.
Alves A, Panis Y, Slim K, et al. French multicentre prospective observational study of laparoscopic versus open colectomy for sigmoid diverticular disease. Br J Surg. 2005;92:1520–5.
Afshar S, Kurer MA. Laparoscopic peritoneal lavage for perforated sigmoid diverticulitis. Color Dis. 2012;14:135–42.
Agaba EA, Zaidi RM, Ramzy P, et al. Laparoscopic Hartmann’s procedure: a viable option for treatment of acutely perforated diverticulitis. Surg Endosc. 2009;23:1483–6.
Neudecker J, Bergholz R, Junghans T, et al. Laparoscopic sigmoidectomy in Germany--a standardised procedure? Langenbeck’s Arch Surg. 2007;392:573–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Eglinton, T.W., Frizelle, F.A. (2019). Laparoscopic Sigmoid Colectomy for Diverticular Disease. In: Parker, M., Hohenberger, W. (eds) Lower Gastrointestinal Tract Surgery: Vol.1, Laparoscopic procedures. Springer Surgery Atlas Series. Springer, Cham. https://doi.org/10.1007/978-3-030-05240-9_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-05240-9_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-05239-3
Online ISBN: 978-3-030-05240-9
eBook Packages: MedicineMedicine (R0)