Abstract
Treatment of advanced stage melanoma has recently undergone a revolutionary change. Prior to 2011 dacarbazine and interleukin-2 were the only treatment options with both demonstrating no impact on overall survival. However, the experience with and results with IL-2 therapy have stimulated development of novel immunotherapies in this disease. IL-2 was the first immunotherapy to be approved for patients with metastatic melanoma and produced durable complete remissions in about 6% of patients. The accompanying toxicity, however, limited the widespread use of IL-2 therapy. In contrast, interferon-alpha despite its important role in the adjuvant setting, never showed a significant response rate or any survival benefit in patients with stage IV disease.
Currently, due to the highly successful revival of immunotherapy with the development of immune checkpoint inhibitors targeting CTLA4 and PD1 on T-lymphocytes, the exploration of cytokines such as IL-2, IFN-a and others, now in conjunction with immune checkpoint inhibition or adoptive cell therapy has been rejuvenated in this disease.
This chapter summarizes the development and use of cytokines as single agents or in combination in the treatment of patients with advanced metastatic melanoma.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Interleukin-2
Interleukin-2 (IL-2) was the first biologic therapy approved by the US Food and Drug Administration for the treatment of patients with metastatic melanoma. The approval in 1998 was based on the collective experience with high-dose IL-2 that resulted in clinical response rates of 16%, including complete responses in 6%, many of which were durable (Atkins et al. 1999, 2000). Similar response rates were noted in patients with metastatic renal cell carcinoma, the only other cancer type for which high-dose IL-2 is currently approved (Fyfe et al. 1996).
IL-2 is a hormone produced by lymphocytes and was first described as a T cell growth factor in 1976 (Morgan et al. 1976). The first clinical use was in 1983 when Bindon and colleagues treated two patients with melanoma with natural IL-2, derived from stimulated normal lymphocytes (Bindon et al. 1983). Lotze and colleagues treated AIDS and cancer patients with IL-2 that was derived from Jurkat, a human T cell line (Lotze et al. 1984, 1985). Because of the limited availability of IL-2, small doses were used in these early studies and no anti-tumor responses were observed. These studies did however demonstrate that IL-2 was capable of modulating the immune system and was worthy of further study. The discovery of the gene for IL-2 (Taniguchi et al. 1983) and the production of recombinant IL-2 resulted in large quantities of IL-2 for clinical trials.
Initial studies evaluating different doses of administration of IL-2 defined the maximal tolerated intravenous dose to be 2.16 × 104 IU/kg/h when given by continuous infusion and 7.2 × 106 IU/kg by a single bolus injection (Lotze et al. 1985, 1986b). Because laboratory models predicted that tumor responses correlated with dose intensity (Papa et al. 1986), early studies by Rosenberg and colleagues utilized the highest tolerable intravenous bolus dose that could be repeatedly administered for 10–15 doses every 8 h (Rosenberg et al. 1985). This regimen of 600,000 or 720,000 IU/kg/dose given intravenously every 8 h became known as high-dose IL-2; with the 600,000 IU/kg/dose being the FDA approved regimen.
Pharmacology of IL-2
Currently the only commercially available IL-2 in the US is Proleukin® (Aldesleukin), produced initially by the Cetus Oncology Division of Chiron and now by Novartis, and licensed to Prometheus. Proleukin® varies from natural IL-2 in that it is non-glycosylated, the cysteine at amino acid position 125 has been replaced by serine and it lacks the N-terminal alanine. This recombinant IL-2 has been shown to be biologically and functionally similar to natural IL-2 (Rosenberg et al. 1984; Doyle et al. 1985). Following intravenous administration, IL-2 is rapidly cleared from the circulation according to a two-compartment model (Lotze et al. 1985; Konrad et al. 1990; Yang and Rosenberg 1997). The initial clearance (α distribution) has a half-life (t1/2) of 7–13 min consistent with a rapid egress of IL-2 into the extravascular space. Subsequently, a longer clearance (β clearance) with a t1/2 of 60–96 min is consistent with a slower release from the extravascular space back into the plasma compartment. Studies with subcutaneous IL-2 administration have shown lower peak serum levels than intravenous IL-2 and the levels remain fairly constant for 8–10 h (Yang and Rosenberg 1997; Konrad et al. 1990; Gustavson et al. 1989). Clearance of IL-2 from the body is primarily through metabolism in the kidneys.
Immunologic Activity of IL-2
Immunologic changes can be measured early following the systemic administration of IL-2. Lymphopenia develops within minutes of a single dose of IL-2 (Lotze et al. 1985; Thompson et al. 1988; Boldt et al. 1988; Punt et al. 1992; Sondel et al. 1988; Macfarlane et al. 1995). The lymphopenia is profound and persists while patients are receiving IL-2; it is thought to be secondary to margination and egress of lymphocytes into the extravascular space. Twenty-four to 36 h after discontinuation of IL-2, there is a rebound lymphocytosis of 2 to 70-fold above baseline which persists for 2–7 days; this rebound is dose and schedule dependent (Sosman et al. 1988; Macfarlane et al. 1995; Punt et al. 1992; Thompson et al. 1988).
Lymphokine activated killer (LAK) precursors and natural killer (NK) activity are lost from the circulation within 15 min of a single (bolus) dose of intravenous IL-2 (Lotze et al. 1985; Salvo et al. 1992). One to 2 days after discontinuation of IL-2 (bolus or continuous infusion), in vitro cytolysis of radiolabeled Daudi and K562 cell targets rebounds above baseline in a dose and schedule dependent fashion (Lotze et al. 1985; Thompson et al. 1988; Sosman et al. 1988; Gratama et al. 1993; Rosenthal et al. 1988). PBMC have decreased proliferative responses to IL-2, mitogens and soluble antigens during IL-2 therapy, and rebound after IL-2 discontinuation (Lotze et al. 1985; Rosenthal et al. 1988; Wiebke et al. 1988; Kradin et al. 1989). Repetitive IL-2 administration results in lymphocyte activation as demonstrated by the expression of the CD25 IL-2 receptor (Lotze et al. 1985, 1987; Thompson et al. 1988; Gratama et al. 1993) or HLA-DR expression (Thompson et al. 1988; Gratama et al. 1993) on the cell surface. Soluble IL-2 receptors (shed from the cell surface) are increased in the serum (Lotze et al. 1987; Urba et al. 1990; Smith et al. 2003). At the tissue level, profound lymphocytic infiltrates have been documented in a variety of organs and tumors (Kragel et al. 1990; Rubin et al. 1989; Cohen et al. 1987). After IL-2 therapy, patients can develop immediate hypersensitivity (IH) to skin test recall antigens (Kradin et al. 1989), however, delayed type hypersensitivity (DTH) responses are depressed (Kradin et al. 1989; Wiebke et al. 1988).
B cell numbers decrease with IL-2 infusion (Wiebke et al. 1988; Thompson et al. 1987; Sondel et al. 1988) and return to baseline several days following discontinuation of IL-2; they do not rebound to the same extent as T cells (Wiebke et al. 1988). B cells products such as IgG, IgM, and IgA are moderately decreased during IL-2 infusion (Wiebke et al. 1988; Rosenthal et al. 1988; Kradin et al. 1989) and return to normal or higher after stopping IL-2. This phenomenon may be in part due to redistribution changes secondary to fluid shifts characteristic of the vascular leak syndrome typically seen with IL-2 administration (see below). Tetanus specific IgG is increased during IL-2 therapy following tetanus reimmunization, suggesting that B cell function is preserved (Rosenthal et al. 1988). Anti-IL-2 antibodies are frequent following intravenous IL-2 administration (Thompson et al. 1987; Allegretta et al. 1986; Sarna et al. 1994) and are generally non-neutralizing. Non-neutralizing antibodies have also developed after subcutaneous IL-2 administration (Atzpodien et al. 1990a). Neutralizing antibodies to IL-2 have been observed following subcutaneous administration of IL-2 with interferon β (Krigel et al. 1988) and in patients with renal cell cancer receiving subcutaneous IL-2 (Whitehead et al. 1990). Serum sickness has not been observed (Sarna et al. 1994; Atkins et al. 1986) and the clinical implications of anti-IL-2 antibody development are unknown.
Neutrophil counts have not been generally affected by IL-2. Severe neutropenia during or shortly after IL-2 therapy is rare (Sosman et al. 1988; Ettinghausen et al. 1987; Rosenberg et al. 1994). Neutrophils may be increased in the first 24 h of IL-2 along with a shift to immature forms (Macfarlane et al. 1995; Jablons et al. 1990). However, transient neutrophil dysfunction occurs as noted by decreased Fc receptor expression and decreased chemotaxis (Jablons et al. 1990; Klempner et al. 1990), and may contribute to an increased risk of catheter related bacterial infections seen with IL-2 therapy.
Many cytokines, including TNFα, IFNγ, GM-CSF, M-CSF, G-CSF, IL-5, IL-6, IL-8, and IL-10, have been shown to increase in the serum following IL-2 administration (Punt et al. 1992; Salvo et al. 1992; Konrad et al. 1992; Weidmann et al. 1992; Mier et al. 1988; Jablons et al. 1989; Gemlo et al. 1988; Tritarelli et al. 1991; Schaafsma et al. 1991; Tilg et al. 1993, 1995; van Haelst Pisani et al. 1991). This cytokine cascade has been implicated in many of the observed side effects of IL-2 administration.
Systemic Effects of IL-2
All major organ systems can be affected by IL-2 and much of the etiology of the side effects can be traced to a capillary leak syndrome (reviewed in (Schwartzentruber 2000)). The intensity of side effects is determined by the dose and schedule of IL-2 administration, but all regimens have the capacity of producing similar toxicities. For any given dose, continuous infusion IL-2 (over 24 h) is more toxic than the same dose given by bolus infusion (Thompson et al. 1988). Hence, the greatest dose intensity per cycle of treatment can be achieved by intermittent bolus dosing. The scant evidence of clinical benefit of low doses of IL-2 when used as a single agent and laboratory evidence in favor of dose intensity (Papa et al. 1986) have supported the continued use of the high-dose regimen. As experience has been gained, the incidence of side effects of high-dose IL-2 has diminished considerably (Kammula et al. 1998). It is clear that with careful patient selection and properly trained clinicians, the mortality from this therapy is extremely low (less than 1%) (Kammula et al. 1998). Another component of this improved safety profile is a decrease in the median number of IL-2 doses given per cycle from 13 to 8 at some centers, which has been accomplished without apparent sacrifice in clinical activity (Kammula et al. 1998).
High-dose IL-2 (600,000 or 720,000 IU/kg) is given by intravenous bolus injection every 8 h. The treatment schema generally consists of two cycles of a maximum of 14 doses each, separated by a rest period of 10–14 days. Two cycles of treatment are generally referred to as one course; complete evaluation for clinical response is performed after every course or approximately every 2 months while on therapy. Re-treatment is offered at 2–3 month intervals to patients who show evidence of clinical response and is continued as long as the disease continues to diminish. Patients achieving a complete response generally receive one additional course of treatment after complete disappearance of disease if they are able to tolerate further IL-2. Ninety-one percent of patients with metastatic melanoma that responded to high-dose IL-2 achieved at least a partial response after one course of therapy; there were no responders among patients who did not respond in the first two courses and continued to receive a third course of IL-2 (Lindsey et al. 2000). Therefore, as most tumor shrinkage is seen after one course of IL-2, and treatment tolerance and number of doses administered decrease with successive courses of IL-2 (Marroquin et al. 2000), patients with stable disease (either non-responders or following an initial response) rarely benefit from receiving more than 2 courses of therapy.
The side effects associated with IL-2 administration affect nearly every organ system and can range from mild to potentially life threatening symptoms. The duration of each cycle of treatment is determined by each patient’s tolerance of side effects, which may vary in intensity and time of onset with each successive cycle. As the side effects are generally reversible by holding treatment, emphasis is placed on determining the safety of proceeding with therapy. This mandates that careful assessments be performed prior to each dose of IL-2. Doses may be withheld to allow for recovery of side effects, many of which follow a cyclical pattern following the dose; however, dosage reductions are not performed. Withheld doses are not replaced and despite dose interruptions, treatment does not extend beyond the scheduled 5-day (maximum 14 doses) treatment cycle. A delay of 24 h or more between doses is generally an indication to discontinue that particular cycle of treatment.
Practical guidelines for the safe administration of high-dose IL-2 have been published (Schwartzentruber 2001). The process begins with careful patient selection. Patients should not have major cardiac, pulmonary, renal, hepatic or medical illnesses and should have a good performance status (ECOG 0 or 1). It is important to screen for occult cardiac disease and for this reason, everyone 50 years of age or older should undergo cardiac stress testing. Evidence of ischemic heart disease is a contraindication to high-dose IL-2. Generally patients with active brain metastases or impending spinal cord compression are not good candidates for high-dose IL-2. Published clinical pathways offer practical help in the assessment of patients before, during and after IL-2 administration (Mavroukakis et al. 2001). Due to the complexity of treatment, high-dose IL-2 is generally administered by doctors and nurses that have received special training in its administration and are familiar with its use.
Following high-dose intravenous bolus injection, the first manifestations of IL-2 side effects can begin with fever and chills within 2–4 h of receiving the first dose (Schwartzentruber 2000). The scheduled administration of antipyretics is necessary to control these side effects. Moderate hypotension and tachycardia develop 2–3 h after the first dose of IL-2 and will persist for the remainder of the treatment. As the end of the cycle nears, additional fluids and vasopressors may be needed to maintain hemodynamic stability. Oliguria frequently develops in the first 24 h and requires additional fluids to restore urine output to a minimum safe level of 20 cc per hour or about 160 cc per 8 h period. The use of fluids to maintain renal perfusion and minimize hypotension, contribute to peripheral edema, pulmonary congestion and weight gain. Patients may gain 10–15 pounds of water weight during treatment and the use of diuretics after IL-2 dosing is stopped is important to initiate the return to baseline weight. When treating hypotension and oliguria with fluids, it is important to limit fluid boluses to 1.5 l of crystalloid per day in addition to maintenance requirements because fluids compound the manifestation of the capillary leak syndrome. Nausea, vomiting and diarrhea are frequent gastrointestinal side effects and become most pronounced near the end of the treatment cycle. These can typically be controlled with aggressive use of anti-emetics and anti-diarrheals. Dermatitis with erythema, desquamation and subsequent pruritis is frequent and requires diligent application of topical moisturizers and frequently oral antipyretics. Neurologic side effects such as confusion, disorientation, agitation or restlessness occur in up to 20% of patients. This side effect can progress even in the absence of additional treatment; therefore, this represents an indication for withholding therapy in order to prevent the onset of neurologic consequences that can delay treatment recovery and discharge. Progressive transient elevations in creatinine, hyperbilirubinemia and thrombocytopenia are frequent laboratory abnormalities observed, but largely do not require intervention. Cardiac arrhythmias including atrial flutter or fibrillation can occur near the end of treatment, and are usually an indication to stop treatment for that cycle. Myocarditis presenting with elevations of CPK MB or troponin is seen in up to 5% of patients, occurs at the end of the cycle of treatment (frequently during the recovery phase) and is generally asymptomatic. While this toxicity does not preclude subsequent cycles of IL-2, care should be taken that the enzyme elevations return to normal and there is no associated cardiac dysfunction prior to discharge from the hospital. Prior to subsequent administration of IL-2, cardiac evaluation must demonstrate complete recovery of function.
There are many interventions and medications that help control the side effects of IL-2 (Schwartzentruber 2001). Though steroids abrogate many of these toxicities, they are not used because of the possibility of interfering with the anti-tumor response (Vetto et al. 1987; Mier et al. 1990). When a cycle of treatment is stopped, most side effects rapidly reverse and patients can be discharged from the hospital 1–3 days after discontinuation of IL-2.
Clinical Efficacy of High-Dose IL-2 Alone
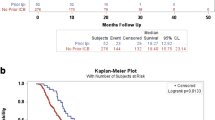
Currently high-dose IL-2 given by intravenous bolus injection is an FDA approved regimen for treatment of patients with metastatic melanoma. High-dose IL-2 has resulted in an overall clinical response rate of 15–16% in patients with metastatic melanoma (Table 1). The combined experience in the US has demonstrated a complete response rate of 6.3% in 270 patients and a partial response rate of 9.6% (Atkins et al. 2000). The median duration of all responses was 8.9 months, with the median not yet reached for complete responses (range of 2.5 to greater than 122 months) and the median for partial responses lasting 5.9 months (range of 1.5 to greater than 111 months) (Fig. 1). In this report, the median duration of complete response was at least 59 months, and 59% of complete responders remained in complete response. Of note, no patients exhibiting response lasting longer than 30 months experienced a relapse, suggesting that such patients may exhibit long term freedom from melanoma recurrence (Figs. 2, 3, and 4).
Kaplan-Meier estimate of response durations for patients with metatatic melanoma achieving complete and partial responses or both (Atkins et al. 2000)
The largest single institution experience in the US, the National Cancer Institute, observed very similar response rates in 182 patients (Rosenberg et al. 1998b) to those reported in the above combined series of 270 (80% of the NCI patients were included in the combined report). Ten of 12 patients achieving a complete response at the NCI, remained in complete response from 12 to greater than 148 months. Complete responses have been observed at all sites, including visceral and cutaneous/subcutaneous sites. Previous treatment with low-dose IL-2 or biochemotherapy has not precluded response to high-dose IL-2 as demonstrated in 2 series with 15–19% response rates after failure of these prior therapies (Weinreich and Rosenberg 2002; Tarhini et al. 2007). On the other hand, the response rate in patients who received prior interferon alpha therapy was somewhat less than in patients without such prior treatment (13% vs. 21%, p = 0.084) (Weinreich and Rosenberg 2002).
Patients who relapse after achieving a response to high-dose IL-2, are generally not retreated because they rarely respond again. In a series of 33 patients with melanoma who relapsed after responding to various IL-2-based regimens, only 1 responded to the same treatment (Lee et al. 1998). Specifically, none of the 8 patients that initially responded to high-dose IL-2 alone re-responded to that treatment. However, 4 patients re-responded to IL-2 when given with tumor infiltrating lymphocytes (Lee et al. 1998).
A more contemporary series was published several years ago and reported the outcomes of 208 patients treated with high-dose IL-2 at one of two centers, MD Anderson Cancer Center (MDACC) and Beth Israel Deaconess Medical Center (BIDMC), between 2003 and 2009 (Joseph et al. 2012a). The vast majority, 88%, had Stage IV (as opposed to unresectable Stage III) disease as well as a normal LDH (79%). The response rate was similar to the historical datasets, with complete responses and partial responses occurring in 6% and 13% of patients, respectively. Additionally, with a median follow up of 2.5 years in surviving patients, the median progression free survival was 104 days and median overall survival 22.8 months. Further, the estimated 5-year survival was 39%. A second, contemporary multicenter study, enrolled 170 patients treated with standard of care high-dose IL-2 from 2009 to 2014 at 15 centers within the Cytokine Working Group (Sullivan et al. 2016). The complete and partial response rates of 5.4% and 13.3%, respectively, were similar to other historical and contemporary cohorts. The median progression free and overall survival were 2.5 and 21.3 months and, more importantly, the 2-year rate of being progression free was 12.4%. Finally, a multicenter series, also reporting on 170 patients with metastatic melanoma from the PROCLAIM database, reported complete and partial response rates of 5% and 10%, respectively, with a median overall survival of 19.6 months with over 43 months median follow up (Alva et al. 2016). Of note, the overall survival data with all three of these datasets, which are non-overlapping, are remarkably similar and far better than historical data, likely reflecting the general improvements in therapy for these patients over the past decade.
Clinical Efficacy of Alternate Doses, Routes and Schedules of IL-2 Alone
In order to avoid the toxicity of high-dose IL-2, lower doses of IL-2 given by a variety of routes, doses and schedules have been explored in many phase I/II studies (Table 2). The different designs of these studies and the small numbers of patients they include make it difficult to draw meaningful conclusions about clinical efficacy. Bolus IL-2 given 3 days per week (as opposed to every 8 h) (Whitehead et al. 1991; Quan and Quan 2003) or manufactured by Hoffman La-Roche (Sparano et al. 1993) or given in low doses (Marolda et al. 1987) has not appeared to be as effective as high-dose bolus IL-2. No complete responses were seen in these studies. The initial use of PEG-IL-2 (polyethylene glycol modified IL-2) to prolong the circulating half-life of IL-2 did not show superior activity to high-dose IL-2 alone in a randomized trial, resulting in a response rate of 11% in 35 treated patients (Yang et al. 1995).
The highest doses of IL-2 given by continuous intravenous infusion (12–18 MIU/m2/day) in 5 small series of patients (15–31 patients each) have resulted in clinical response rates of 6–33% (Perez et al. 1991; Dillman et al. 1997; Legha et al. 1996; Hidalgo et al. 1996; Dorval et al. 1992). The collective experience with high-dose IL-2 alone administered primarily by continuous infusion in Europe has demonstrated an overall response rate of 15% in 117 patients (Keilholz and Eggermont 2000). The median survival in this study was 7.5 months, which appears lower than the 12 month median survival reported for patients treated with high-dose bolus IL-2 in the initial U.S. experience (Atkins et al. 2000). Lower doses of continuous infusion IL-2 or prolonged duration of infusion (up to 90 days) have not consistently resulted in higher response rates (Richards et al. 1988; Creekmore et al. 1989; Engelhardt et al. 1997; Quan et al. 2005; Goldstein et al. 1989; Oliver et al. 1989; Vlasveld et al. 1992, 1994; Caligiuri et al. 1991).
In contrast to its frequent use in patients with renal cell carcinoma, subcutaneous IL-2 has been infrequently used to treat patients with metastatic melanoma and there is very little evidence of clinical activity (Atzpodien et al. 1990a; Stein et al. 1991; Angevin et al. 1995; Tagliaferri et al. 1998; Ahmed et al. 1996; Leahy et al. 1992). The largest study with subcutaneous administration of IL-2 in 133 patients noted an overall response rate of 4% and concluded that survival was inferior to a similar regimen combined with histamine (Agarwala et al. 2002). There is also very little experience with intramuscular and intralymphatic administration of IL-2 and there have been no reported clinical responses when given by these routes (Urba et al. 1990; Sarna et al. 1994; Galvani et al. 1992). Intraperitoneal IL-2 (Lotze et al. 1986a) was evaluated in the early studies of IL-2 and was not continued because of the technical challenges and side effects associated with that route of administration. The novel approach of delivering IL-2 into the splenic artery (Klasa et al. 1990; Thatcher et al. 1989) resulted in clinical responses only when combined with high doses of bolus IL-2 intravenously (4 of 31 patients, 13%), but yielded no complete responses (Thatcher et al. 1989). Intracranial administration of IL-2 has no reported clinical responses (Heimans et al. 1991; List et al. 1992; Rosener et al. 1993; Samlowski et al. 1993). The direct injection of IL-2 into a tumor metastasis or the surrounding tissue has resulted in complete or partial regression of 50–90% of the injected lesions without evidence of systemic response (Lotze et al. 1986b; Radny et al. 2003; Green et al. 2007; Gutwald et al. 1994). Delivery of IL-2 directly to tumors in the lung by the inhalational route (with concurrent dacarbazine) has resulted in regression of pulmonary lesions in 13 of 27 (48%) patients but no responses in metastatic sites outside the lung (Enk et al. 2000).
One of the most striking observations that emerges from the reports of IL-2 alone when used in regimens other than by high-dose bolus, is the paucity of reports of complete and durable responses. Randomized trials to support this observation have not been performed in patients with melanoma; however, such a trial comparing high-dose IL-2 to lower doses of IL-2 in patients with metastatic kidney cancer has been reported (Yang et al. 2003). This trial clearly demonstrated lower toxicity of these alternate regimens but also lower clinical response rates and in particular, fewer complete and/or durable responses.
With the development of newer immunotherapies that target immune checkpoints such as cytotoxic T-lymphocyte associated antigen 4 (CTLA-4), programmed death 1 receptor (PD-1) and its ligand (PD-L1) (See chapter “Checkpoint Inhibitors in the Treatment of Metastatic Melanoma”), there has been renewed interest in other active immunotherapy approaches such as cytokines. One of these has been the exploration of IL-2 modifications to favor T-effector/NK cell activity without T-regulatory activation. The most developed of these approaches has been a novel pegylation technique that culminates in a molecule of 6 polyethylene glycol (PEG) moieties and IL-2. After introduction into the patient, the PEGs are irreversibly cleaved one by one and lead to the conversion of the 6-PEG-IL-2 prodrug, known as NKTR-214, into a biologically active 2-PEG-IL-2 or 1-PEG-IL-2 molecule that purportedly preferentially binds to T-effector and/or NK cell IL-2 receptors as opposed to T regulatory cell IL-2 receptors (Charych et al. 2016, 2017). In the tumor microenvironment, this leads to an influx of effector cells, as well as a compensatory expression by the tumor of PD-L1. NKTR-214 as a single-agent was not associated with responses in any of the 28 patients, including 7 with melanoma, in the dose-escalation phase I study monotherapy trial (Bernatchez et al. 2017). However, in serial biopsies, there was evidence of an influx of PD-1, CD8 dual positive T cells, setting the stage for potential combination therapy with anti-PD-1/PD-L1 monoclonal antibodies (described below).
Clinical Efficacy of IL-2 Combined with Interferon Alpha
A variety of routes, doses and schedules combining IL-2 and interferon alpha have been evaluated in primarily phase I/II studies (Table 3). Only one randomized trial has been performed and it compared the efficacy of IL-2 plus interferon alpha to IL-2 alone (Sparano et al. 1993). In this study, high-dose IL-2 (Hoffman La-Roche, Nutley, NJ) response rates (5%) were no different than bolus IL-2 at a slightly lower dose combined with interferon alpha (10% response rate). The largest single study evaluating escalating doses of bolus IL-2 (Hoffman La-Roche) and interferon alpha in 82 patients resulted in overall response rates of 24% (Marincola et al. 1995b). It appeared that higher doses of each cytokine resulted in higher response rates but the higher toxicity at those doses made them impractical. Similar observations were made in a separate study in which the response rate in 17 patients was 41% but the cardiac and neurologic toxicity of this regimen was excessive (Kruit et al. 1996). A less intense regimen by the same investigators reduced these toxicities but also resulted in a drop in response rate in 25 patients to 20% (Kruit et al. 1996). Bolus IL-2 given three times weekly or at lower doses combined with intramuscular or subcutaneous interferon resulted in clinical response rates of 29% and 16% respectively (Budd et al. 1992; Karp 1998) and were not clearly superior to IL-2 alone. Escalating bolus doses or 2 h intravenous infusions of IL-2 have not shown enhanced activity (Sznol et al. 1990; Huberman et al. 1991).
Many studies have evaluated continuous intravenous infusion IL-2 along with interferon administered subcutaneously or intramuscularly. The three largest studies with continuous infusion IL-2 involved 27, 66 and 51 patients, and demonstrated response rates of 18%, 11% and 16% respectively (Keilholz et al. 1993; Oldham et al. 1992; Kruit et al. 1995). Investigators in Europe piloted a regimen of decrescendo IL-2 in order to reduce toxicity and observed a response rate of 41% in 27 patients (Keilholz et al. 1993). The experience with this regimen of interferon alpha and decrescendo IL-2 was not confirmed in a larger EORTC series of 66 patients exhibiting a response rate of 18% (Keilholz et al. 1997) or in 21 patients in a US study in which no responses were seen (Eton et al. 2000). Other smaller series of continuous intravenous IL-2 with interferon have not demonstrated superiority (Pichert et al. 1991; Thomas et al. 1992; Veelken et al. 1992; Maxwell et al. 1993; Whitehead et al. 1993; Eton et al. 1996; Mittelman et al. 1990; Bukowski et al. 1990; Lee et al. 1989; Bergmann et al. 1990) to reported results with the high dose bolus IL-2 regimen. Outpatient regimens of subcutaneous IL-2 and subcutaneous or intramuscular interferon are generally the least toxic and have yielded response rates of 0–18% (Hidalgo et al. 1996; Atzpodien et al. 1990b; Vuoristo et al. 1994; Gause et al. 1996; Rosso et al. 1992; De Braud et al. 1993; Castello et al. 1993).
The lessons learned from all of these studies were that combining IL-2 and interferon alpha generally resulted in additive toxicities preventing their use at full doses due to unacceptable toxicity. When lower doses of each cytokine were used to reduce toxicity, clinical response rates were not clearly improved over those of high-dose IL-2 alone. In particular, the complete responses characteristic of high-dose bolus IL-2 administration were less frequently observed. Hence, with the added toxicities of the combined regimens and no clear response advantage, the combination of IL-2 and interferon alpha has not been widely used outside of the context of biochemotherapy regimens) that combined IL-2 +/− interferon alpha with dacarbazine and/or cisplatin-based cytotoxic chemotherapy. While these approaches showed higher response rates and median PFS compared to chemotherapy alone in patients with stage IV melanoma, they largely failed to improve median OS (Atkins et al. 2008) and, therefore, have largely been abandoned.
Clinical Efficacy of IL-2 Combined with Other Cytokines, Immune Modulators, Antibodies or Vaccines
When IL-2 has been combined with various cytokines such as GM-CSF (Smith et al. 2003; Ridolfi et al. 2001), interferon β (Krigel et al. 1988), interferon γ (Weiner et al. 1991; Viens et al. 1992; Kim et al. 1996; Margolin et al. 1992; Taylor et al. 1992), IL-1 β (Triozzi et al. 1995), IL-4 (Olencki et al. 1996), IL-12 (Gollob et al. 2003), or TNF α (Rosenberg et al. 1989; Negrier et al. 1992; Krigel et al. 1995; Dillman et al. 1993) no obvious increase in clinical response rates have been observed above that observed historically with IL-2 alone (Table 4). Similarly, the combination of IL-2 and various immune modulators such as cyclophosphamide (Rosenberg et al. 1989; Mitchell et al. 1988; Lindemann et al. 1989; Verdi et al. 1992; Oldham et al. 1991), famotidine (Quan et al. 2006), flavone acetic acid (Thatcher et al. 1990; O’reilly et al. 1993; Holmund et al. 1995), histamine (Agarwala et al. 2002; Hellstrand et al. 1994; Lindner et al. 2004; Schmidt et al. 2002; Middleton et al. 2007), levamisole (Ahmed et al. 1996; Creagan et al. 1997), melatonin (Lissoni et al. 1994, 1997), radiation (Lange et al. 1992; Safwat et al. 2005), SRL 172 (Mycobacterium vaccae) (Nicholson et al. 2003) or taurolidine (O’brien et al. 2006) have not improved the clinical activity of IL-2 (Table 5). Monoclonal antibodies such as 9.2.27 (Rosenberg et al. 1989), ch14.18 (Albertini et al. 1997), 14.G2a (Albertini et al. 1996), R24 (Bajorin et al. 1990; Soiffer et al. 1997; Nasi et al. 1997; Alpaugh et al. 1998), ch14.14 plus R24 (Choi et al. 2006) or anti-CD3 (Sosman et al. 1993; Hank et al. 1995; Sosman et al. 1995; Buter et al. 1993) when combined with IL-2 have failed to significantly augment the response rate of IL-2 as well (Table 6).
An apparent increase in clinical activity was noted when high-dose IL-2 was combined with gp100:209–217 (210 M) peptide vaccine in a phase II trial of 31 patients, resulting in a 42% response rate (Rosenberg et al. 1998a). Three phase II studies using slightly different schedules of high dose IL-2 combined with this vaccine in 39–42 patients each produced response rates of 13–24% (Sosman et al. 2008). This strategy was subsequently studied in a randomized multi-institutional phase III trial comparing vaccine plus IL-2 to high-dose IL-2 alone. The results of this trial showed a near tripling of response rate (16% versus 6%) in patients treated with vaccine plus high-dose IL-2, but the low rate of response in the control arm limits the impact and applicability of these findings (Schwartzentruber et al. 2011).
As described above, inhibitors of immune checkpoints have demonstrated activity in and become FDA-approved for the treatment of patients with advanced melanoma (Hodi et al. 2010). The first of these developed was the anti-CTLA-4 monoclonal antibody ipilimumab, however the anti-PD1 antibodies pembrolizumab and nivolumab followed soon after (Robert et al. 2015a, b). While combination studies have been or are being performed, there is data on the sequencing of immune checkpoint inhibitors and high-dose IL-2 that helps to determine the potential for sequencing of IL-2 with other therapies. The first report involved the safety of interleukin-2 following ipilimumab come out of the National Cancer Institute (NCI) (Smith et al. 2007). Of 22 patients treated with IL-2 following ipilimumab, three developed bowel perforation; this in contrast to the four perforations in 198 patients treated at the NCI with ipilimumab from 2002 to 2005 and eight out of 1797 patients treated with high-dose IL-2 there from 1998 to 2002. A more contemporary series published in 2016, reported on 52 patients treated with high-dose IL-2 after ipilimumab compared to 276 patients treated with IL-2 without prior ipilimumab (Buchbinder et al. 2016). Efficacy was similar, specifically related to overall survival from IL-2 commencement; however two episodes of severe GI-toxicity occurred including one death from bowel perforation in the group receiving high-dose IL-2 following ipilimumab therapy. In another study, the efficacy of ipilimumab after IL-2 was evaluated in a subset (48) of 208 patients treated with high-dose IL-2 from 2003 to 2009 (Joseph et al. 2012a). In these 48 patients subsequently treated with ipilimumab, the clinical benefit of ipilimumab, was similar to contemporary reports of ipilimumab benefit. Specifically, the response rate was approximately 16% with a median progression and overall survival of 2.5 and 12 months, respectively.
The initial study that combined ipilimumab with high-dose IL-2 resulted in a response rate of 22% in 36 patients (Maker et al. 2005), which was seemingly not different than expected with IL-2 alone. However, following the FDA-approval of ipilimumab in 2011, it remained an unsettled question as to whether high-dose IL-2 could be safely given with ipilimumab and whether the combination may be associated with improved outcomes. This study could not be completed due to the emergence of the anti-PD-1 antibodies as superior first line agents in patients with metastatic melanoma. The data from the 46 patients enrolled onto the phase I portion of the ipilimumab plus interleukin-2 study showed that the combination was tolerable and not associated with undue or unexpected toxicity. There remains great excitement in combining high-dose IL-2 with the immune checkpoint inhibitors, specifically anti-PD-1 antibodies, and trials are underway (NCT03476174).
In 2017, the first data from the trial combining NKTR-214 and nivolumab was presented and updated at the 2018 American Society of Clinical Oncology Meeting (Diab et al. 2017, 2018). The initial 11 melanoma patients did remarkably well, with confirmed response in seven and disease control rate, a RECIST-defined response (complete or partial) or stable disease, in ten of 11. With more patients treated (28 reported to be eligible for response), the response rate fell to 50% (14 of 28) and disease control rate to 71% (20 of 28). This trial is ongoing and larger trials based on these preliminary results are being planned (see chapter “Novel Immunotherapies and Novel Combinations of Immunotherapy for Metastatic Melanoma”).
Clinical Efficacy of IL-2 Combined with Targeted Therapy
With the emergence of BRAF-targeted therapy as a useful and life-prolonging strategy for patients with BRAF mutant metastatic melanoma a number of trials were launched to combine BRAF inhibitors with immunotherapy. Preclinical and early clinical studies suggested that BRAF inhibitor therapy was associated with a number of changes in the melanoma tumor microenvironment that might enhance tumor responsiveness to immunotherapy (Boni et al. 2010; Cooper et al. 2013; Frederick et al. 2013). Specifically, antigen presentation increases, immunosuppressive cytokines go down, T cell clonality increases, and an influx of T cells are seen. Building on these findings, a trial of vemurafenib plus high-dose IL-2 was launched in 2012 (NCT01683188) (Mooradian et al. 2018). This trial closed after enrolling six of a planned 43 patients. Two thirds responded, but no long-term durable responses where seen.
Agents to Reduce the Toxicity of IL-2
The safety of high-dose bolus IL-2 has improved as experience with this regimen has grown (Kammula et al. 1998). The diminished intensity of side effects of high-dose IL-2 has also correlated with a decrease in the number of IL-2 doses given in each cycle in some institutions. Despite the reduction of toxicity, this therapy remains a very intensive inpatient regimen. A variety of concomitant medications such as paracetamol, indomethacin and antiemetics are routinely used to control the common side effects of IL-2 (Schwartzentruber 2001). Various other agents have been studied with the hope of ameliorating toxicity. One such example are corticosteroids which have reduced the side effects of IL-2 (Vetto et al. 1987; Mier et al. 1990). However, steroids have abrogated the therapeutic benefit of IL-2 in mice (Papa et al. 1986) and the concomitant use of steroids with IL-2 is strongly discouraged. Patients should be warned not to use steroids either systemically or topically after receiving IL-2 therapy. Agents which have not been clinically beneficial at reducing IL-2 toxicity in patients with melanoma have included: soluble tumor necrosis factor receptor (Trehu et al. 1996; Du Bois et al. 1997), soluble IL-1 receptor (Mcdermott et al. 1998), lisofylline (Margolin et al. 1997), C1 esterase inhibitor (Ogilvie et al. 1994), and CNI-1493 (Atkins et al. 2001). Low dose dopamine induced recovery of impaired renal function in patients receiving continuous infusion IL-2 (Palmieri et al. 1993) but was not significantly beneficial when used prophylactically in a randomized trial of high-dose IL-2 (Cormier et al. 1997). Taurolidine when used in combination with a decrescendo regimen of continuous infusion IL-2 appeared to enhance tolerability in 11 patients (O’brien et al. 2006). N-Monomethyl-l-Arginine has demonstrated antihypotensive activity in patients with metastatic renal cell carcinoma receiving IL-2 (Kilbourn et al. 2000) and has been evaluated in patients with melanoma receiving high-dose IL-2, without clear clinical benefit despite having apparent antihypotensive effects (Richard Sherry, personal communication).
Predictors of Clinical Response
The ability to predict which patients will respond to IL-2 therapy is desirable since treatment and toxicity could then be spared of those who are not likely to respond. This is particularly important, given that emergence of more effective therapies to treat advanced melanoma, including BRAF targeted therapy and immune checkpoint inhibitors. Basically, there needs to be compelling evidence to support the use of high-dose IL-2 to forego frontline therapy with the more recently approved agents, and the identification of predictive biomarkers to select patients with a high likelihood of therapeutic response is critical. Traditionally, there have been no in-vitro predictors of response (reviewed in (Schwartzentruber 1993)). ECOG performance status of “0” and not having received prior systemic therapies were factors associated with higher clinical response in 270 patients receiving high-dose IL-2 (Atkins et al. 1999). Similarly, patients who received no prior immunotherapy were more likely to have a complete response to IL-2 than patients who received prior immunotherapy (Rosenberg et al. 1998b). One report found a significant association of expression of HLA-DQ1 tissue type with clinical response (Rubin et al. 1995), but a larger study of 272 patients found no association between HLA type and response to IL-2 (Marincola et al. 1995a). This latter study did find a correlation between HLA-DR3 and –DR4 alleles and decreased tolerance to IL-2.
Patients with only cutaneous and subcutaneous metastases have a 50% response rate to high-dose IL-2 which is higher than the 15% rate observed in patients with disease at any other site (Chang and Rosenberg 2001; Phan et al. 2001; Royal et al. 1996). The importance of site of disease was confirmed by French investigators; they also found that high levels of C-reactive protein before therapy was associated with a poor response to IL-2 (Tartour et al. 1996). The majority of patients, however, do not have disease confined to the skin or subcutaneous tissue, and sites of disease and measurements of serum markers have not been used to exclude people from therapy.
Though various treatment-related parameters have been associated with higher clinical response, none has been useful in selecting patients for therapy or altering the therapy in progress. For example, responders have received more doses of IL-2 and developed a greater rebound lymphocytosis than non-responders (Rosenberg et al. 1998b; Phan et al. 2001; Royal et al. 1996). Circulating regulatory T cells (CD4+ CD25+) have decreased following administration of high-dose IL-2 but only in those patients achieving a clinical response to therapy (Cesana et al. 2006). Post-treatment biopsy of metastatic lesions has demonstrated greater HLA-DR antigen expression and T cell infiltrate in regressing lesions than in non-responding lesions (Rubin et al. 1989). Autoimmune hypothyroidism (Phan et al. 2001; Krouse et al. 1995) and vitiligo (Phan et al. 2001; Rosenberg and White 1996) have occurred more frequently in responders than non-responders suggesting that tumor response may be similarly mediated by the induction of an autoimmune reaction against the tumor cells. In general, whether these changes are a function of duration of treatment and follow-up rather than a true association with response (i.e. these toxicities take time to evolve and responders receive more courses of treatment and are followed longer than non-responders) may never be settled.
More recently, patients with an elevated LDH were identified as being uniquely unlikely to respond or have long-term benefit from high-dose IL-2, but this appears to be consistent with the general thinking that patients with a better performance status and less aggressive disease will do better whereas those with a poor performance status and/or aggressive disease will do worse.
Research to discover better biomarkers that will predict responsiveness to high-dose IL-2 has been ongoing, and newer technologies are being used to aide in this discovery. For example, the analysis of tumor DNA for activating mutations for BRAF has been standard of care since the approval of vemurafenib, a potent and specific BRAF inhibitor, since 2011 (Flaherty et al. 2010) (See chapter “Targeted Therapies for BRAF-Mutant Metastatic Melanoma”). However, only 45–50% of patients with cutaneous melanoma have a tumor harboring such a mutation and approximately a quarter have mutations in NRAS, which like BRAF, constitutively activates the mitogen activated protein kinase (MAPK) pathway when mutated (See chapter “Molecularly Targeted Therapy for Patients with BRAF Wild-Type Melanoma”). Interestingly, the presence or absence of a BRAF mutation is not associated with improved responsiveness to high-dose IL-2; however, the presence of an NRAS mutation was, in an analysis of 103 patients with mutational testing available (Joseph et al. 2012b). This has not been validated in larger studies, but is an intriguing finding. In a smaller analysis of 49 patients, gene expression profiling was performed on archived, pretreatment tumors and a GEP enriched with immune-related genes was associated with a higher response rate than in those with an alternative GEP (Sullivan et al. 2016). Building upon this work, the IL-2 Select Melanoma trial was launched with a plan to prospectively validate this GEP approach as a predictive marker of benefit in patients with melanoma treated with high-dose IL-2. From 2009 to 2014, 170 patients were enrolled and RNA sequencing was able to be performed on pretreatment, archival blocks from 101 patients. Application of the prior gene expression classification with immune genes was modestly associated with response (normalized enrichment score of −1.70, p value <0.001, false discovery rate 0.004). At the time of presentation in 2016, the DNA sequencing data was not completed (Sullivan et al. 2016).
Analysis of blood analytes, such as serum LDH, is another possible strategy to identify predictive biomarkers of response. As mentioned above, an elevated LDH is associated with poorer outcomes to high-dose IL-2, although this is true for nearly every therapy for melanoma, and thus is likely more of a prognostic factor than a truly predictive one. A comprehensive analysis of potential blood-based biomarkers identified serum vascular endothelial growth factor (VEGF) and fibronectin as negative predictors of benefit to high-dose IL-2 in patients with melanoma (Sabatino et al. 2009). The IL-2 Select study also captured pretreatment serum in an attempt to validate the predictive value of these biomarkers. These studies are ongoing.
Other Cytokines for Therapy of Metastatic Melanoma
To date, the most efficacious cytokine for the treatment of metastatic melanoma has been high-dose IL-2. IFNα also has activity, but quite modestly in the treatment of metastatic melanoma. Even when combined with anti-PD1 at the maximum tolerated dose of pegylated-IFN-a, clinical activity was at most very modest (Atkins et al. 2018). Other cytokines that have been tested as single agents include: IL-4 (Margolin et al. 1994), IL-6 (Weber et al. 1993, 1994; Sosman et al. 1997), IL-7 (with vaccine) (Rosenberg et al. 2006), IL-12 (Bajetta et al. 1998; Atkins et al. 1997; Gollob et al. 2000; Alatrash et al. 2004), IL-21 (Davis et al. 2007), GM-CSF (Rao et al. 2003), M-CSF (Sanda et al. 1992; Cole et al. 1994; Robertson et al. 2006), and IL-15 (Conlon et al. 2015) (Table 7). None of these has demonstrated significant clinical activity as single agents at the doses tested. There is very limited experience with IL-18; 1 partial responder was noted in a phase I study in 6 patients with metastatic melanoma (Robertson et al. 2006). NKTR-214, the pegylated IL-2 has no single agent activity (see above), but may synergize with anti-PD1 in patients with metastatic melanoma and kidney cancer. More recently, pegylated human recombinant IL-10 or pegilodecakin (AM0010), which stimulates and expands cytotoxic CD8 T cells and inhibits inflammatory CD4 T cells, has been studied as single agent treatment in patients with metastatic solid cancers (Naing et al. 2016). Clinical activity was described in a patient with uveal melanoma and patients with renal cell carcinoma. Pegilodecakin is now being investigated in combination with anti-PD1.
Summary
The first clinical responses with high-dose IL-2 were observed in patients with metastatic melanoma during the mid-1980s. High-dose IL-2 was approved for this disease by the US Food and Drug Administration in 1998. About half of the clinical responses are complete and durable, lasting in excess of 5 years. Lower doses of IL-2, combinations of IL-2 with other cytokines and immune modulators or the use of various other interleukins have not achieved the level of clinical activity of high-dose IL-2. Much has been learned about the management of the side effects of IL-2 and how to safely administer this agent (Schwartzentruber 2001). When administered by properly trained physicians and nurses, this treatment is safe and can be effective in some patients with metastatic melanoma.
Experience with IL-2 based therapy has established that immune modulation does have a role in the treatment of patients with metastatic melanoma, and this knowledge served as the basis for the development of the current more clinically applicable immune therapies.
References
Agarwala SS, Glaspy J, O’day SJ, Mitchell M, Gutheil J, Whitman E, Gonzalez R, Hersh E, Feun L, Belt R, Meyskens F, Hellstrand K, Wood D, Kirkwood JM, Gehlsen KR, Naredi P (2002) Results from a randomized phase III study comparing combined treatment with histamine dihydrochloride plus interleukin-2 versus interleukin-2 alone in patients with metastatic melanoma. J Clin Oncol 20:125–133
Ahmed FY, Leonard GA, A’hern R, Taylor AE, Lorentzos A, Atkinson H, Moore J, Nicolson MC, Riches PG, Gore ME (1996) A randomised dose escalation study of subcutaneous interleukin 2 with and without levamisole in patients with metastatic renal cell carcinoma or malignant melanoma. Br J Cancer 74:1109–1113
Alatrash G, Hutson TE, Molto L, Richmond A, Nemec C, Mekhail T, Elson P, Tannenbaum C, Olencki T, Finke J, Bukowski RM (2004) Clinical and immunologic effects of subcutaneously administered interleukin-12 and interferon alfa-2b: phase I trial of patients with metastatic renal cell carcinoma or malignant melanoma. J Clin Oncol 22:2891–2900
Albertini MR, Gan J, Jaeger P, Hank JA, Storer B, Schell K, Rivest T, Surfus J, Reisfeld RA, Schiller JH, Sondel PM (1996) Systemic interleukin-2 modulates the anti-idiotypic response to chimeric anti-GD2 antibody in patients with melanoma. J Immunother Emphasis Tumor Immunol 19:278–295
Albertini MR, Hank JA, Schiller JH, Khorsand M, Borchert AA, Gan J, Bechhofer R, Storer B, Reisfeld RA, Sondel PM (1997) Phase IB trial of chimeric antidisialoganglioside antibody plus interleukin 2 for melanoma patients. Clin Cancer Res 3:1277–1288
Allegretta M, Atkins MB, Dempsey RA, Bradley EC, Konrad MW, Childs A, Wolfe SN, Mier JW (1986) The development of anti-interleukin-2 antibodies in patients treated with recombinant human interleukin-2 (IL-2). J Clin Immunol 6:481–490
Alpaugh RK, Von Mehren M, Palazzo I, Atkins MB, Sparano JA, Schuchter L, Weiner LM, Dutcher JP (1998) Phase IB trial for malignant melanoma using R24 monoclonal antibody, interleukin-2/alpha-interferon. Med Oncol 15:191–198
Alva A, Daniels GA, Wong MK, Kaufman HL, Morse MA, Mcdermott DF, Clark JI, Agarwala SS, Miletello G, Logan TF, Hauke RJ, Curti B, Kirkwood JM, Gonzalez R, Amin A, Fishman M, Agarwal N, Lowder JN, Hua H, Aung S, Dutcher JP (2016) Contemporary experience with high-dose interleukin-2 therapy and impact on survival in patients with metastatic melanoma and metastatic renal cell carcinoma. Cancer Immunol Immunother 65:1533–1544
Angevin E, Valteau-Couanet D, Farace F, Dietrich PY, Lecesne A, Triebel F, Escudier B (1995) Phase I study of prolonged low-dose subcutaneous recombinant interleukin-2 (IL-2) in patients with advanced cancer. J Immunother Emphasis Tumor Immunol 18:188–195
Atkins MB, Gould JA, Allegretta M, Li JJ, Dempsey RA, Rudders RA, Parkinson DR, Reichlin S, Mier JW (1986) Phase I evaluation of recombinant interleukin-2 in patients with advanced malignant disease. J Clin Oncol 4:1380–1391
Atkins MB, Robertson MJ, Gordon M, Lotze MT, Decoste M, Dubois JS, Ritz J, Sandler AB, Edington HD, Garzone PD, Mier JW, Canning CM, Battiato L, Tahara H, Sherman ML (1997) Phase I evaluation of intravenous recombinant human interleukin 12 in patients with advanced malignancies. Clin Cancer Res 3:409–417
Atkins MB, Lotze MT, Dutcher JP, Fisher RI, Weiss G, Margolin K, Abrams J, Sznol M, Parkinson D, Hawkins M, Paradise C, Kunkel L, Rosenberg SA (1999) High-dose recombinant interleukin 2 therapy for patients with metastatic melanoma: analysis of 270 patients treated between 1985 and 1993. J Clin Oncol 17:2105–2116
Atkins MB, Kunkel L, Sznol M, Rosenberg SA (2000) High-dose recombinant interleukin-2 therapy in patients with metastatic melanoma: long-term survival update. Cancer J Sci Am 6(Suppl 1):S11–S14
Atkins MB, Redman B, Mier J, Gollob J, Weber J, Sosman J, Macpherson BL, Plasse T (2001) A phase I study of CNI-1493, an inhibitor of cytokine release, in combination with high-dose interleukin-2 in patients with renal cancer and melanoma. Clin Cancer Res 7:486–492
Atkins MB, Hsu J, Lee S, Cohen GI, Flaherty LE, Sosman JA, Sondak VK, Kirkwood JM, Eastern Cooperative Oncology, G (2008) Phase III trial comparing concurrent biochemotherapy with cisplatin, vinblastine, dacarbazine, interleukin-2, and interferon alfa-2b with cisplatin, vinblastine, and dacarbazine alone in patients with metastatic malignant melanoma (E3695): a trial coordinated by the Eastern Cooperative Oncology Group. J Clin Oncol 26:5748–5754
Atkins MB, Hodi FS, Thompson JA, Mcdermott DF, Hwu WJ, Lawrence DP, Dawson NA, Wong DJ, Bhatia S, James M, Jain L, Robey S, Shu X, Homet Moreno B, Perini RF, Choueiri TK, Ribas A (2018) Pembrolizumab plus pegylated interferon alfa-2b or ipilimumab for advanced melanoma or renal cell carcinoma: dose-finding results from the phase Ib KEYNOTE-029 study. Clin Cancer Res 24:1805–1815
Atzpodien J, Korfer A, Evers P, Franks CR, Knuver-Hopf J, Lopez-Hanninen E, Fischer M, Mohr H, Dallmann I, Hadam M et al (1990a) Low-dose subcutaneous recombinant interleukin-2 in advanced human malignancy: a phase II outpatient study. Mol Biother 2:18–26
Atzpodien J, Korfer A, Franks CR, Poliwoda H, Kirchner H (1990b) Home therapy with recombinant interleukin-2 and interferon-alpha 2b in advanced human malignancies. Lancet 335:1509–1512
Bajetta E, Del Vecchio M, Mortarini R, Nadeau R, Rakhit A, Rimassa L, Fowst C, Borri A, Anichini A, Parmiani G (1998) Pilot study of subcutaneous recombinant human interleukin 12 in metastatic melanoma. Clin Cancer Res 4:75–85
Bajorin DF, Chapman PB, Wong G, Coit DG, Kunicka J, Dimaggio J, Cordon-Cardo C, Urmacher C, Dantes L, Templeton MA et al (1990) Phase I evaluation of a combination of monoclonal antibody R24 and interleukin 2 in patients with metastatic melanoma. Cancer Res 50:7490–7495
Bergmann L, Weidmann E, Mitrou PS, Runne U, Keilholz U, Bartsch HH, Franks CR (1990) Interleukin-2 in combination with interferon-alpha in disseminated malignant melanoma and advanced renal cell carcinoma. A phase I/II study. Onkologie 13:137–140
Bernatchez CH, Haymaker CL, Hurwitz ME, Kluger HM, Tetzlaff MT, Jackson N, Gergel I, Tagliaferri MA, Zalevsky J, Hoch U, Fanton C, Iacucci E, Aung S, Imperiale M, Liao E, Bentebibel SE, Tannir NM, Hwu P, Sznol M, Diab A (2017) Effect of a novel IL-2 cytokine immune agonist (NKTR-214) on proliferating CD8+T cells and PD-1 expression on immune cells in the tumor microenvironment in patients with prior checkpoint therapy. J Clin Oncol 35(suppl; abstr 2545)
Bindon C, Czerniecki M, Ruell P, Edwards A, Mccarthy WH, Harris R, Hersey P (1983) Clearance rates and systemic effects of intravenously administered interleukin 2 (IL-2) containing preparations in human subjects. Br J Cancer 47:123–133
Boldt DH, Mills BJ, Gemlo BT, Holden H, Mier J, Paietta E, Mcmannis JD, Escobedo LV, Sniecinski I, Rayner AA et al (1988) Laboratory correlates of adoptive immunotherapy with recombinant interleukin-2 and lymphokine-activated killer cells in humans. Cancer Res 48:4409–4416
Boni A, Cogdill AP, Dang P, Udayakumar D, Njauw CN, Sloss CM, Ferrone CR, Flaherty KT, Lawrence DP, Fisher DE, Tsao H, Wargo JA (2010) Selective BRAFV600E inhibition enhances T-cell recognition of melanoma without affecting lymphocyte function. Cancer Res 70:5213–5219
Buchbinder EI, Gunturi A, Perritt J, Dutcher J, Aung S, Kaufman HL, Ernstoff MS, Miletello GP, Curti BD, Daniels GA, Patel SP, Kirkwood JM, Hallmeyer S, Clark JI, Gonzalez R, Richart JM, Lutzky J, Morse MA, Sullivan RJ, Mcdermott DF (2016) A retrospective analysis of high-dose interleukin-2 (HD IL-2) following Ipilimumab in metastatic melanoma. J Immunother Cancer 4:52
Budd GT, Murthy S, Finke J, Sergi J, Gibson V, Medendorp S, Barna B, Boyett J, Bukowski RM (1992) Phase I trial of high-dose bolus interleukin-2 and interferon alfa-2a in patients with metastatic malignancy. J Clin Oncol 10:804–809
Bukowski RM, Murthy S, Sergi J, Budd GT, Mckeever S, Medendorp SV, Tubbs R, Gibson V, Finke J (1990) Phase I trial of continuous infusion recombinant interleukin-2 and intermittent recombinant interferon-alpha 2a: clinical effects. J Biol Response Mod 9: 538–545
Buter J, Janssen RA, Martens A, Sleijfer DT, De Leij L, Mulder NH (1993) Phase I/II study of low-dose intravenous OKT3 and subcutaneous interleukin-2 in metastatic cancer. Eur J Cancer 29A:2108–2113
Caligiuri MA, Murray C, Soiffer RJ, Klumpp TR, Seiden M, Cochran K, Cameron C, Ish C, Buchanan L, Perillo D et al (1991) Extended continuous infusion low-dose recombinant interleukin-2 in advanced cancer: prolonged immunomodulation without significant toxicity. J Clin Oncol 9:2110–2119
Castello G, Comella P, Manzo T, Napolitano M, Parziale AP, Galati MG, Daponte A, Casaretti R, Celentano E, Comella G (1993) Immunological and clinical effects of intramuscular rIFN alpha-2a and low dose subcutaneous rIL-2 in patients with advanced malignant melanoma. Melanoma Res 3:43–49
Cesana GC, Deraffele G, Cohen S, Moroziewicz D, Mitcham J, Stoutenburg J, Cheung K, Hesdorffer C, Kim-Schulze S, Kaufman HL (2006) Characterization of CD4+CD25+ regulatory T cells in patients treated with high-dose interleukin-2 for metastatic melanoma or renal cell carcinoma. J Clin Oncol 24:1169–1177
Chang E, Rosenberg SA (2001) Patients with melanoma metastases at cutaneous and subcutaneous sites are highly susceptible to interleukin-2-based therapy. J Immunother 24:88–90
Charych DH, Hoch U, Langowski JL, Lee SR, Addepalli MK, Kirk PB, Sheng D, Liu X, Sims PW, Vanderveen LA, Ali CF, Chang TK, Konakova M, Pena RL, Kanhere RS, Kirksey YM, Ji C, Wang Y, Huang J, Sweeney TD, Kantak SS, Doberstein SK (2016) NKTR-214, an engineered cytokine with biased IL2 receptor binding, increased tumor exposure, and marked efficacy in mouse tumor models. Clin Cancer Res 22:680–690
Charych D, Khalili S, Dixit V, Kirk P, Chang T, Langowski J, Rubas W, Doberstein SK, Eldon M, Hoch U, Zalevsky J (2017) Modeling the receptor pharmacology, pharmacokinetics, and pharmacodynamics of NKTR-214, a kinetically-controlled interleukin-2 (IL2) receptor agonist for cancer immunotherapy. PLoS One 12:e0179431
Choi BS, Sondel PM, Hank JA, Schalch H, Gan J, King DM, Kendra K, Mahvi D, Lee LY, Kim K, Albertini MR (2006) Phase I trial of combined treatment with ch14.18 and R24 monoclonal antibodies and interleukin-2 for patients with melanoma or sarcoma. Cancer Immunol Immunother 55:761–774
Cohen PJ, Lotze MT, Roberts JR, Rosenberg SA, Jaffe ES (1987) The immunopathology of sequential tumor biopsies in patients treated with interleukin-2. Correlation of response with T-cell infiltration and HLA-DR expression. Am J Pathol 129:208–216
Cole DJ, Sanda MG, Yang JC, Schwartzentruber DJ, Weber J, Ettinghausen SE, Pockaj BA, Kim HI, Levin RD, Pogrebniak HW et al (1994) Phase I trial of recombinant human macrophage colony-stimulating factor administered by continuous intravenous infusion in patients with metastatic cancer. J Natl Cancer Inst 86:39–45
Conlon KC, Lugli E, Welles HC, Rosenberg SA, Fojo AT, Morris JC, Fleisher TA, Dubois SP, Perera LP, Stewart DM, Goldman CK, Bryant BR, Decker JM, Chen J, Worthy TA, Figg WD Sr, Peer CJ, Sneller MC, Lane HC, Yovandich JL, Creekmore SP, Roederer M, Waldmann TA (2015) Redistribution, hyperproliferation, activation of natural killer cells and CD8 T cells, and cytokine production during first-in-human clinical trial of recombinant human interleukin-15 in patients with cancer. J Clin Oncol 33:74–82
Cooper ZA, Frederick DT, Juneja VR, Sullivan RJ, Lawrence DP, Piris A, Sharpe AH, Fisher DE, Flaherty KT, Wargo JA (2013) BRAF inhibition is associated with increased clonality in tumor-infiltrating lymphocytes. Oncoimmunology 2:e26615
Cormier JN, Hurst R, Vasselli J, Lee D, Kim CJ, Mckee M, Venzon D, White D, Marincola FM, Rosenberg SA (1997) A prospective randomized evaluation of the prophylactic use of low-dose dopamine in cancer patients receiving interleukin-2. J Immunother 20: 292–300
Creagan ET, Rowland KM Jr, Suman VJ, Kardinal CG, Marschke RF Jr, Marks RS, Maples WJ (1997) Phase II study of combined levamisole with recombinant interleukin-2 in patients with advanced malignant melanoma. Am J Clin Oncol 20:490–492
Creekmore SP, Harris JE, Ellis TM, Braun DP, Cohen II, Bhoopalam N, Jassak PF, Cahill MA, Canzoneri CL, Fisher RI (1989) A phase I clinical trial of recombinant interleukin-2 by periodic 24-hour intravenous infusions. J Clin Oncol 7:276–284
Davis ID, Skrumsager BK, Cebon J, Nicholaou T, Barlow JW, Moller NP, Skak K, Lundsgaard D, Frederiksen KS, Thygesen P, Mcarthur GA (2007) An open-label, two-arm, phase I trial of recombinant human interleukin-21 in patients with metastatic melanoma. Clin Cancer Res 13:3630–3636
De Braud F, Biganzoli L, Bajetta E, Colleoni M, Zampino MG (1993) Subcutaneous low-dose interleukin-2 plus alpha interferon in advanced malignant melanoma. Tumori 79:187–190
Diab A, Tannir NM, Bernatchez C, Haymaker CL, Bentebibel SE, Curti BD, Wong MK, Gergel I, Tagliaferri MA, Zalevsky J, Hoch U, Aung S, Imperiale M, Cho DC, Tykodi SS, Puzanov I, Kluger HM, Hurwitz ME, Hwu P, Sznol MA (2017) Phase 1/2 study of a novel IL-2 cytokine, NKTR-214, and nivolumab in patients with select locally advanced or metastatic solid tumors. ASCO Annual Meeting, Chicago. J Clin Oncol 35(suppl; abstr e14040)
Diab A, Hurwitz ME, Cho DC, Papadimitrakopoulou V, Curti BD, Tykodi SS, Puzanov I, Ibrahim NK, Tolaney SM, Tripathy D, Gao J, Siefker-Radtke AO, Clemens W, Tagliaferri MA, Gettinger SN, Kluger HM, Larkin JM, Grignani G, Sznol M, Tannir NM (2018) NKTR-214 (CD122-biased agonist) plus nivolumab in patients with advanced solid tumors: Preliminary phase 1/2 results of PIVOT. ASCO Annual Meeting, Chicago. J Clin Oncol 36(suppl; abstr 3006)
Dillman RO, Church C, Oldham RK, West WH, Schwartzberg L, Birch R (1993) Inpatient continuous-infusion interleukin-2 in 788 patients with cancer. The National Biotherapy Study Group experience. Cancer 71:2358–2370
Dillman RO, Wiemann MC, Vandermolen LA, Bury MJ, Depriest C, Church C (1997) Hybrid high-dose bolus/continuous infusion interleukin-2 in patients with metastatic melanoma: a phase II trial of the Cancer Biotherapy Research Group (formerly the National Biotherapy Study Group). Cancer Biother Radiopharm 12:249–255
Dorval T, Mathiot C, Chosidow O, Revuz J, Avril MF, Guillaume JC, Tursz T, Brandely M, Pouillart P, Fridman WH (1992) IL-2 phase II trial in metastatic melanoma: analysis of clinical and immunological parameters. Biotechnol Ther 3:63–79
Doyle MV, Lee MT, Fong S (1985) Comparison of the biological activities of human recombinant interleukin-2(125) and native interleukin-2. J Biol Response Mod 4:96–109
Du Bois JS, Trehu EG, Mier JW, Shapiro L, Epstein M, Klempner M, Dinarello C, Kappler K, Ronayne L, Rand W, Atkins MB (1997) Randomized placebo-controlled clinical trial of high-dose interleukin-2 in combination with a soluble p75 tumor necrosis factor receptor immunoglobulin G chimera in patients with advanced melanoma and renal cell carcinoma. J Clin Oncol 15:1052–1062
Engelhardt M, Wirth K, Mertelsmann R, Lindemann A, Brennscheidt U (1997) Clinical and immunomodulatory effects of repetitive 2-day cycles of high-dose continuous infusion IL-2. Eur J Cancer 33:1050–1054
Enk AH, Nashan D, Rubben A, Knop J (2000) High dose inhalation interleukin-2 therapy for lung metastases in patients with malignant melanoma. Cancer 88: 2042–2046
Eton O, Talpaz M, Lee KH, Rothberg JM, Brell JM, Benjamin RS (1996) Phase II trial of recombinant human interleukin-2 and interferon-alpha-2a: implications for the treatment of patients with metastatic melanoma. Cancer 77:893–899
Eton O, Buzaid AC, Bedikian AY, Smith TM, Papadopoulos NE, Ellerhorst JA, Hibberts JL, Legha SS, Benjamin RS (2000) A phase II study of “decrescendo” interleukin-2 plus interferon-alpha-2a in patients with progressive metastatic melanoma after chemotherapy. Cancer 88:1703–1709
Ettinghausen SE, Moore JG, White DE, Platanias L, Young NS, Rosenberg SA (1987) Hematologic effects of immunotherapy with lymphokine-activated killer cells and recombinant interleukin-2 in cancer patients. Blood 69:1654–1660
Flaherty KT, Puzanov I, Kim KB, Ribas A, Mcarthur GA, Sosman JA, O’dwyer PJ, Lee RJ, Grippo JF, Nolop K, Chapman PB (2010) Inhibition of mutated, activated BRAF in metastatic melanoma. N Engl J Med 363: 809–819
Frederick DT, Piris A, Cogdill AP, Cooper ZA, Lezcano C, Ferrone CR, Mitra D, Boni A, Newton LP, Liu C, Peng W, Sullivan RJ, Lawrence DP, Hodi FS, Overwijk WW, Lizee G, Murphy GF, Hwu P, Flaherty KT, Fisher DE, Wargo JA (2013) BRAF inhibition is associated with enhanced melanoma antigen expression and a more favorable tumor microenvironment in patients with metastatic melanoma. Clin Cancer Res 19:1225–1231
Fyfe GA, Fisher RI, Rosenberg SA, Sznol M, Parkinson DR, Louie AC (1996) Long-term response data for 255 patients with metastatic renal cell carcinoma treated with high-dose recombinant interleukin-2 therapy. J Clin Oncol 14:2410–2411
Galvani DW, Walton S, Davies JM, Owen RR, Carr R, Cawley JC, Sells RA (1992) Endolymphatic delivery of IL2 in patients with melanoma and lymphoma. Biotherapy 4:251–255
Gause BL, Sznol M, Kopp WC, Janik JE, Smith JW 2nd, Steis RG, Urba WJ, Sharfman W, Fenton RG, Creekmore SP, Holmlund J, Conlon KC, Vandermolen LA, Longo DL (1996) Phase I study of subcutaneously administered interleukin-2 in combination with interferon alfa-2a in patients with advanced cancer. J Clin Oncol 14:2234–2241
Gemlo BT, Palladino MA Jr, Jaffe HS, Espevik TP, Rayner AA (1988) Circulating cytokines in patients with metastatic cancer treated with recombinant interleukin 2 and lymphokine-activated killer cells. Cancer Res 48:5864–5867
Goldstein D, Sosman JA, Hank JA, Weil-Hillman G, Moore KH, Borchert A, Bechhofer R, Storer B, Kohler PC, Levitt D et al (1989) Repetitive weekly cycles of interleukin 2: effect of outpatient treatment with a lower dose of interleukin 2 on non-major histocompatibility complex-restricted killer activity. Cancer Res 49:6832–6839
Gollob JA, Mier JW, Veenstra K, Mcdermott DF, Clancy D, Clancy M, Atkins MB (2000) Phase I trial of twice-weekly intravenous interleukin 12 in patients with metastatic renal cell cancer or malignant melanoma: ability to maintain IFN-gamma induction is associated with clinical response. Clin Cancer Res 6:1678–1692
Gollob JA, Veenstra KG, Parker RA, Mier JW, Mcdermott DF, Clancy D, Tutin L, Koon H, Atkins MB (2003) Phase I trial of concurrent twice-weekly recombinant human interleukin-12 plus low-dose IL-2 in patients with melanoma or renal cell carcinoma. J Clin Oncol 21:2564–2573
Gratama JW, Bruin RJ, Lamers CH, Oosterom R, Braakman E, Stoter G, Bolhuis RL (1993) Activation of the immune system of cancer patients by continuous i.v. recombinant IL-2 (rIL-2) therapy is dependent on dose and schedule of rIL-2. Clin Exp Immunol 92:185–193
Green DS, Bodman-Smith MD, Dalgleish AG, Fischer MD (2007) Phase I/II study of topical imiquimod and intralesional interleukin-2 in the treatment of accessible metastases in malignant melanoma. Br J Dermatol 156:337–345
Gustavson LE, Nadeau RW, Oldfield NF (1989) Pharmacokinetics of teceleukin (recombinant human interleukin-2) after intravenous or subcutaneous administration to patients with cancer. J Biol Response Mod 8:440–449
Gutwald JG, Groth W, Mahrle G (1994) Peritumoral injections of interleukin 2 induce tumour regression in metastatic malignant melanoma. Br J Dermatol 130:541–542
Hank JA, Albertini M, Wesly OH, Schiller JH, Borchert A, Moore K, Bechhofer R, Storer B, Gan J, Gambacorti C et al (1995) Clinical and immunological effects of treatment with murine anti-CD3 monoclonal antibody along with interleukin 2 in patients with cancer. Clin Cancer Res 1:481–491
Heimans JJ, Wagstaff J, Schreuder WO, Wolbers JG, Baars JW, Polman CH, Scharenberg JG, Scheper RJ, Palmer PA, Franks CR (1991) Treatment of leptomeningeal carcinomatosis with continuous intraventricular infusion of recombinant interleukin-2. Surg Neurol 35:244–247
Hellstrand K, Naredi P, Lindner P, Lundholm K, Rudenstam CM, Hermodsson S, Asztely M, Hafstrom L (1994) Histamine in immunotherapy of advanced melanoma: a pilot study. Cancer Immunol Immunother 39:416–419
Hidalgo OF, Aramendia JM, Alonso G, Foncillas JG, Brugarolas A (1996) Results of two sequential phase II studies of interleukin-2 (IL2) in metastatic renal cell carcinoma and melanoma: high-dose continuous intravenous IL2 infusion and subcutaneous IL2 administration in combination with alpha interferon. Rev Med Univ Navarra 40:6–12
Hodi FS, O’day SJ, Mcdermott DF, Weber RW, Sosman JA, Haanen JB, Gonzalez R, Robert C, Schadendorf D, Hassel JC, Akerley W, van den Eertwegh AJ, Lutzky J, Lorigan P, Vaubel JM, Linette GP, Hogg D, Ottensmeier CH, Lebbe C, Peschel C, Quirt I, Clark JI, Wolchok JD, Weber JS, Tian J, Yellin MJ, Nichol GM, Hoos A, Urba WJ (2010) Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med 363:711–723
Holmund JT, Kopp WC, Wiltrout RH, Longo DL, Urba WJ, Janik JE, Sznol M, Conlon KC, Fenton RG, Hornung R et al (1995) A phase I clinical trial of flavone-8-acetic acid in combination with interleukin 2. J Natl Cancer Inst 87:134–136
Huberman M, Bering H, Fallon B, Tessitore J, Sonnenborn H, Paul S, Zeffren J, Levitt D, Groopman J (1991) A phase I study of an outpatient regimen of recombinant human interleukin-2 and alpha-2a-interferon in patients with solid tumors. Cancer 68: 1708–1713
Jablons DM, Mule JJ, Mcintosh JK, Sehgal PB, May LT, Huang CM, Rosenberg SA, Lotze MT (1989) IL-6/IFN-beta-2 as a circulating hormone. Induction by cytokine administration in humans. J Immunol 142: 1542–1547
Jablons D, Bolton E, Mertins S, Rubin M, Pizzo P, Rosenberg SA, Lotze MT (1990) IL-2-based immunotherapy alters circulating neutrophil Fc receptor expression and chemotaxis. J Immunol 144:3630–3636
Joseph RW, Eckel-Passow JE, Sharma R, Liu P, Parker A, Jakob J, Buchbinder E, Bassett RL, Davies MA, Hwu P, Atkins MB, Sullivan RJ (2012a) Characterizing the clinical benefit of ipilimumab in patients who progressed on high-dose IL-2. J Immunother 35:711–715
Joseph RW, Sullivan RJ, Harrell R, Stemke-Hale K, Panka D, Manoukian G, Percy A, Bassett RL, Ng CS, Radvanyi L, Hwu P, Atkins MB, Davies MA (2012b) Correlation of NRAS mutations with clinical response to high-dose IL-2 in patients with advanced melanoma. J Immunother 35:66–72
Kammula US, White DE, Rosenberg SA (1998) Trends in the safety of high dose bolus interleukin-2 administration in patients with metastatic cancer. Cancer 83: 797–805
Karp SE (1998) Low-dose intravenous bolus interleukin-2 with interferon-alpha therapy for metastatic melanoma and renal cell carcinoma. J Immunother 21:56–61
Keilholz U, Eggermont AM (2000) The role of interleukin-2 in the management of stage IV melanoma: the EORTC melanoma cooperative group program. Cancer J Sci Am 6(Suppl 1):S99–S103
Keilholz U, Scheibenbogen C, Tilgen W, Bergmann L, Weidmann E, Seither E, Richter M, Brado B, Mitrou PS, Hunstein W (1993) Interferon-alpha and interleukin-2 in the treatment of metastatic melanoma. Comparison of two phase II trials. Cancer 72:607–614
Keilholz U, Goey SH, Punt CJ, Proebstle TM, Salzmann R, Scheibenbogen C, Schadendorf D, Lienard D, Enk A, Dummer R, Hantich B, Geueke AM, Eggermont AM (1997) Interferon alfa-2a and interleukin-2 with or without cisplatin in metastatic melanoma: a randomized trial of the European Organization for Research and Treatment of Cancer Melanoma Cooperative Group. J Clin Oncol 15:2579–2588
Kilbourn RG, Fonseca GA, Trissel LA, Griffith OW (2000) Strategies to reduce side effects of interleukin-2: evaluation of the antihypotensive agent NG-monomethyl-l-arginine. Cancer J Sci Am 6(Suppl 1):S21–S30
Kim CJ, Taubenberger JK, Simonis TB, White DE, Rosenberg SA, Marincola FM (1996) Combination therapy with interferon-gamma and interleukin-2 for the treatment of metastatic melanoma. J Immunother Emphasis Tumor Immunol 19:50–58
Klasa RJ, Silver HK, Kong S (1990) In vivo induction of lymphokine-activated killer cells by interleukin-2 splenic artery perfusion in advanced malignancy. Cancer Res 50:4906–4910
Klempner MS, Noring R, Mier JW, Atkins MB (1990) An acquired chemotactic defect in neutrophils from patients receiving interleukin-2 immunotherapy. N Engl J Med 322:959–965
Konrad MW, Hemstreet G, Hersh EM, Mansell PW, Mertelsmann R, Kolitz JE, Bradley EC (1990) Pharmacokinetics of recombinant interleukin 2 in humans. Cancer Res 50:2009–2017
Konrad MW, Dewitt SK, Bradley EC, Goodman G, Groves EC, Hersh EM, Krigel RL, Rudolph A (1992) Interferon-gamma induced by administration of recombinant interleukin-2 to patients with cancer: kinetics, dose dependence, and correlation with physiological and therapeutic response. J Immunother (1991) 12: 55–63
Kradin RL, Kurnick JT, Preffer FI, Dubinett SM, Dickersin GR, Pinto C (1989) Adoptive immunotherapy with IL-2 results in the loss of delayed-type hypersensitivity responses and the development of immediate hypersensitivity to recall antigens. Clin Immunol Immunopathol 50:184–195
Kragel AH, Travis WD, Feinberg L, Pittaluga S, Striker LM, Roberts WC, Lotze MT, Yang JJ, Rosenberg SA (1990) Pathologic findings associated with interleukin-2-based immunotherapy for cancer: a postmortem study of 19 patients. Hum Pathol 21:493–502
Krigel RL, Padavic-Shaller KA, Rudolph AR, Litwin S, Konrad M, Bradley EC, Comis RL (1988) A phase I study of recombinant interleukin 2 plus recombinant beta-interferon. Cancer Res 48:3875–3881
Krigel RL, Padavic-Shaller K, Toomey C, Comis RL, Weiner LM (1995) Phase I study of sequentially administered recombinant tumor necrosis factor and recombinant interleukin-2. J Immunother Emphasis Tumor Immunol 17:161–170
Krouse RS, Royal RE, Heywood G, Weintraub BD, White DE, Steinberg SM, Rosenberg SA, Schwartzentruber DJ (1995) Thyroid dysfunction in 281 patients with metastatic melanoma or renal carcinoma treated with interleukin-2 alone. J Immunother Emphasis Tumor Immunol 18:272–278
Kruit WH, Goey SH, Calabresi F, Lindemann A, Stahel RA, Poliwoda H, Osterwalder B, Stoter G (1995) Final report of a phase II study of interleukin 2 and interferon alpha in patients with metastatic melanoma. Br J Cancer 71:1319–1321
Kruit WH, Punt CJ, Goey SH, De Mulder PH, Gratama JW, Eggermont AM, Bolhuis RL, Stoter G (1996) Dose efficacy study of two schedules of high-dose bolus administration of interleukin 2 and interferon alpha in metastatic melanoma. Br J Cancer 74:951–955
Lange JR, Raubitschek AA, Pockaj BA, Spencer WF, Lotze MT, Topalian SL, Yang JC, Rosenberg SA (1992) A pilot study of the combination of interleukin-2-based immunotherapy and radiation therapy. J Immunother (1991) 12:265–271
Leahy MG, Pitfield D, Popert S, Gallagher CJ, Oliver RT (1992) Phase I study comparing continuous infusion of recombinant interleukin-2 by subcutaneous or intravenous administration. Eur J Cancer 28A:1049–1051
Lee KH, Talpaz M, Rothberg JM, Murray JL, Papadopoulos N, Plager C, Benjamin R, Levitt D, Gutterman J (1989) Concomitant administration of recombinant human interleukin-2 and recombinant interferon alpha-2A in cancer patients: a phase I study. J Clin Oncol 7:1726–1732
Lee DS, White DE, Hurst R, Rosenberg SA, Yang JC (1998) Patterns of relapse and response to retreatment in patients with metastatic melanoma or renal cell carcinoma who responded to interleukin-2-based immunotherapy. Cancer J Sci Am 4:86–93
Legha SS, Gianan MA, Plager C, Eton OE, Papadopoulous NE (1996) Evaluation of interleukin-2 administered by continuous infusion in patients with metastatic melanoma. Cancer 77:89–96
Lindemann A, Hoeffken K, Schmidt RE, Diehl V, Kloke O, Gamm H, Hayungs J, Oster W, Boehm M, Franks CR et al (1989) A multicenter trial of interleukin-2 and low-dose cyclophosphamide in highly chemotherapy-resistant malignancies. Cancer Treat Rev 16(Suppl A): 53–57
Lindner P, Rizell M, Mattsson J, Hellstrand K, Naredi P (2004) Combined treatment with histamine dihydrochloride, interleukin-2 and interferon-alpha in patients with metastatic melanoma. Anticancer Res 24:1837–1842
Lindsey KR, Rosenberg SA, Sherry RM (2000) Impact of the number of treatment courses on the clinical response of patients who receive high-dose bolus interleukin-2. J Clin Oncol 18:1954–1959
Lissoni P, Barni S, Cazzaniga M, Ardizzoia A, Rovelli F, Brivio F, Tancini G (1994) Efficacy of the concomitant administration of the pineal hormone melatonin in cancer immunotherapy with low-dose IL-2 in patients with advanced solid tumors who had progressed on IL-2 alone. Oncology 51:344–347
Lissoni P, Fumagalli L, Paolorossi F, Rovelli F, Roselli MG, Maestroni GJ (1997) Anticancer neuroimmunomodulation by pineal hormones other than melatonin: preliminary phase II study of the pineal indole 5-methoxytryptophol in association with low-dose IL-2 and melatonin. J Biol Regul Homeost Agents 11:119–122
List J, Moser RP, Steuer M, Loudon WG, Blacklock JB, Grimm EA (1992) Cytokine responses to intraventricular injection of interleukin 2 into patients with leptomeningeal carcinomatosis: rapid induction of tumor necrosis factor alpha, interleukin 1 beta, interleukin 6, gamma-interferon, and soluble interleukin 2 receptor (Mr 55,000 protein). Cancer Res 52: 1123–1128
Lotze MT, Robb RJ, Sharrow SO, Frana LW, Rosenberg SA (1984) Systemic administration of interleukin-2 in humans. J Biol Response Mod 3: 475–482
Lotze MT, Matory YL, Ettinghausen SE, Rayner AA, Sharrow SO, Seipp CA, Custer MC, Rosenberg SA (1985) In vivo administration of purified human interleukin 2. II. Half life, immunologic effects, and expansion of peripheral lymphoid cells in vivo with recombinant IL 2. J Immunol 135:2865–2875
Lotze MT, Custer MC, Rosenberg SA (1986a) Intraperitoneal administration of interleukin-2 in patients with cancer. Arch Surg 121:1373–1379
Lotze MT, Matory YL, Rayner AA, Ettinghausen SE, Vetto JT, Seipp CA, Rosenberg SA (1986b) Clinical effects and toxicity of interleukin-2 in patients with cancer. Cancer 58:2764–2772
Lotze MT, Custer MC, Sharrow SO, Rubin LA, Nelson DL, Rosenberg SA (1987) In vivo administration of purified human interleukin-2 to patients with cancer: development of interleukin-2 receptor positive cells and circulating soluble interleukin-2 receptors following interleukin-2 administration. Cancer Res 47:2188–2195
Macfarlane MP, Yang JC, Guleria AS, White RL Jr, Seipp CA, Einhorn JH, White DE, Rosenberg SA (1995) The hematologic toxicity of interleukin-2 in patients with metastatic melanoma and renal cell carcinoma. Cancer 75:1030–1037
Maker AV, Phan GQ, Attia P, Yang JC, Sherry RM, Topalian SL, Kammula US, Royal RE, Haworth LR, Levy C, Kleiner D, Mavroukakis SA, Yellin M, Rosenberg SA (2005) Tumor regression and autoimmunity in patients treated with cytotoxic T lymphocyte-associated antigen 4 blockade and interleukin 2: a phase I/II study. Ann Surg Oncol 12:1005–1016
Margolin KA, Doroshow JH, Akman SA, Leong LA, Morgan RJ, Raschko J, Somlo G, Mills B, Goldberg D, Sniecinski I (1992) Phase I trial of interleukin-2 plus gamma-interferon. J Immunother (1991) 11:50–55
Margolin K, Aronson FR, Sznol M, Atkins MB, Gucalp R, Fisher RI, Sunderland M, Doroshow JH, Ernest ML, Mier JW et al (1994) Phase II studies of recombinant human interleukin-4 in advanced renal cancer and malignant melanoma. J Immunother Emphasis Tumor Immunol 15:147–153
Margolin K, Atkins M, Sparano J, Sosman J, Weiss G, Lotze M, Doroshow J, Mier J, O’boyle K, Fisher R, Campbell E, Rubin J, Federighi D, Bursten S (1997) Prospective randomized trial of lisofylline for the prevention of toxicities of high-dose interleukin 2 therapy in advanced renal cancer and malignant melanoma. Clin Cancer Res 3:565–572
Marincola FM, Shamamian P, Rivoltini L, Salgaller M, Cormier J, Restifo NP, Simonis TB, Venzon D, White DE, Parkinson DR (1995a) HLA associations in the antitumor response against malignant melanoma. J Immunother Emphasis Tumor Immunol 18:242–252
Marincola FM, White DE, Wise AP, Rosenberg SA (1995b) Combination therapy with interferon alfa-2a and interleukin-2 for the treatment of metastatic cancer. J Clin Oncol 13:1110–1122
Marolda R, Belli F, Prada A, Villani F, Gambacorti-Passerini C, Galazka A, Parmiani G, Cascinelli N (1987) A phase I study of recombinant interleukin 2 in melanoma patients. Toxicity and clinical effects. Tumori 73:575–584
Marroquin CE, White DE, Steinberg SM, Rosenberg SA, Schwartzentruber DJ (2000) Decreased tolerance to interleukin-2 with repeated courses of therapy in patients with metastatic melanoma or renal cell cancer. J Immunother 23:387–392
Mavroukakis SA, Muehlbauer PM, White RL Jr, Schwartzentruber DJ (2001) Clinical pathways for managing patients receiving interleukin 2. Clin J Oncol Nurs 5:207–217
Maxwell W, Mcdevitt J, Reid I, Sharpe I, Feighery C, Tanner WA, Emmons R, Monson JR (1993) Changes in immunological parameters during interleukin 2 and interferon 2 alpha treatment of recurrent renal cell carcinoma and malignant melanoma. Eur J Surg Oncol 19:265–272
Mcdermott DF, Trehu EG, Mier JW, Sorce D, Rand W, Ronayne L, Kappler K, Clancy M, Klempner M, Atkins MB (1998) A two-part phase I trial of high-dose interleukin 2 in combination with soluble (Chinese hamster ovary) interleukin 1 receptor. Clin Cancer Res 4:1203–1213
Middleton M, Hauschild A, Thomson D, Anderson R, Burdette-Radoux S, Gehlsen K, Hellstrand K, Naredi P (2007) Results of a multicenter randomized study to evaluate the safety and efficacy of combined immunotherapy with interleukin-2, interferon-{alpha}2b and histamine dihydrochloride versus dacarbazine in patients with stage IV melanoma. Ann Oncol 18:1691–1697
Mier JW, Vachino G, Van Der Meer JW, Numerof RP, Adams S, Cannon JG, Bernheim HA, Atkins MB, Parkinson DR, Dinarello CA (1988) Induction of circulating tumor necrosis factor (TNF alpha) as the mechanism for the febrile response to interleukin-2 (IL-2) in cancer patients. J Clin Immunol 8:426–436
Mier JW, Vachino G, Klempner MS, Aronson FR, Noring R, Smith S, Brandon EP, Laird W, Atkins MB (1990) Inhibition of interleukin-2-induced tumor necrosis factor release by dexamethasone: prevention of an acquired neutrophil chemotaxis defect and differential suppression of interleukin-2-associated side effects. Blood 76:1933–1940
Mitchell MS, Kempf RA, Harel W, Shau H, Boswell WD, Lind S, Bradley EC (1988) Effectiveness and tolerability of low-dose cyclophosphamide and low-dose intravenous interleukin-2 in disseminated melanoma [corrected]. J Clin Oncol 6:409–424
Mittelman A, Huberman M, Puccio C, Fallon B, Tessitore J, Savona S, Eyre R, Gafney E, Wick M, Skelos A et al (1990) A phase I study of recombinant human interleukin-2 and alpha-interferon-2a in patients with renal cell cancer, colorectal cancer, and malignant melanoma. Cancer 66:664–669
Mooradian MJ, Reuben A, Prieto PA, Hazar-Rethinam M, Frederick DT, Nadres B, Piris A, Juneja V, Cooper ZA, Sharpe AH, Corcoran RB, Flaherty KT, Lawrence DP, Wargo JA, Sullivan RJ (2018) A phase II study of combined therapy with a BRAF inhibitor (vemurafenib) and interleukin-2 (aldesleukin) in patients with metastatic melanoma. Oncoimmunology 7:e1423172
Morgan DA, Ruscetti FW, Gallo R (1976) Selective in vitro growth of T lymphocytes from normal human bone marrows. Science 193:1007–1008
Naing A, Papadopoulos KP, Autio KA, Ott PA, Patel MR, Wong DJ, Falchook GS, Pant S, Whiteside M, Rasco DR, Mumm JB, Chan IH, Bendell JC, Bauer TM, Colen RR, Hong DS, Van Vlasselaer P, Tannir NM, Oft M, Infante JR (2016) Safety, antitumor activity, and immune activation of pegylated recombinant human interleukin-10 (AM0010) in patients with advanced solid tumors. J Clin Oncol 34:3562–3569
Nasi ML, Meyers M, Livingston PO, Houghton AN, Chapman PB (1997) Anti-melanoma effects of R24, a monoclonal antibody against GD3 ganglioside. Melanoma Res 7(Suppl 2):S155–S162
Negrier MS, Pourreau CN, Palmer PA, Ranchere JY, Mercatello A, Viens P, Blaise D, Jasmin C, Misset JL, Franks CR et al (1992) Phase I trial of recombinant interleukin-2 followed by recombinant tumor necrosis factor in patients with metastatic cancer. J Immunother (1991) 11:93–102
Nicholson S, Guile K, John J, Clarke IA, Diffley J, Donnellan P, Michael A, Szlosarek P, Dalgleish AG (2003) A randomized phase II trial of SRL172 (Mycobacterium vaccae) +/− low-dose interleukin-2 in the treatment of metastatic malignant melanoma. Melanoma Res 13:389–393
O’brien GC, Cahill RA, Bouchier-Hayes DJ, Redmond HP (2006) Co-immunotherapy with interleukin-2 and taurolidine for progressive metastatic melanoma. Ir J Med Sci 175:10–14
Ogilvie AC, Baars JW, Eerenberg AJ, Hack CE, Pinedo HM, Thijs LG, Wagstaff J (1994) A pilot study to evaluate the effects of C1 esterase inhibitor on the toxicity of high-dose interleukin 2. Br J Cancer 69:596–598
Oldham RK, Stark J, Barth NM, Hoogstraten B, Brown CH, O’connor T, Dupere S, Birch R (1991) Continuous infusion of interleukin-2 and cyclophosphamide as treatment of advanced cancers: a National Biotherapy Study Group Trial. Mol Biother 3:74–78
Oldham RK, Blumenschein G, Schwartzberg L, Birch R, Arnold J (1992) Combination biotherapy utilizing interleukin-2 and alpha interferon in patients with advanced cancer: a National Biotherapy Study Group Trial. Mol Biother 4:4–9
Olencki T, Finke J, Tubbs R, Tuason L, Greene T, Mclain D, Swanson SJ, Herzog P, Stanley J, Edinger M, Budd GT, Bukowski RM (1996) Immunomodulatory effects of interleukin-2 and interleukin-4 in patients with malignancy. J Immunother Emphasis Tumor Immunol 19:69–80
Oliver RT, Crosby D, Nouri A, Scott E, Galazka A (1989) Evaluation of the effect of continuous infusion recombinant interleukin-2 (bioleukin) on peripheral blood leucocytes of patients with terminal malignancy. Br J Cancer 60:934–937
O’reilly SM, Rustin GJ, Farmer K, Burke M, Hill S, Denekamp J (1993) Flavone acetic acid (FAA) with recombinant interleukin-2 (rIL-2) in advanced malignant melanoma: I. Clinical and vascular studies. Br J Cancer 67:1342–1345
Palmieri G, Morabito A, Lauria R, Montesarchio V, Matano E, Memoli B, Libetta C, Rea A, Merola C, Correale P et al (1993) Low-dose dopamine induces early recovery of recombinant interleukin-2--impaired renal function. Eur J Cancer 29A:1119–1122
Papa MZ, Mule JJ, Rosenberg SA (1986) Antitumor efficacy of lymphokine-activated killer cells and recombinant interleukin 2 in vivo: successful immunotherapy of established pulmonary metastases from weakly immunogenic and nonimmunogenic murine tumors of three district histological types. Cancer Res 46: 4973–4978
Parkinson DR, Abrams JS, Wiernik PH, Rayner AA, Margolin KA, Van Echo DA, Sznol M, Dutcher JP, Aronson FR, Doroshow JH et al (1990) Interleukin-2 therapy in patients with metastatic malignant melanoma: a phase II study. J Clin Oncol 8:1650–1656
Perez EA, Scudder SA, Meyers FA, Tanaka MS, Paradise C, Gandara DR (1991) Weekly 24-hour continuous infusion interleukin-2 for metastatic melanoma and renal cell carcinoma: a phase I study. J Immunother (1991) 10:57–62
Phan GQ, Attia P, Steinberg SM, White DE, Rosenberg SA (2001) Factors associated with response to high-dose interleukin-2 in patients with metastatic melanoma. J Clin Oncol 19:3477–3482
Pichert G, Jost LM, Fierz W, Stahel RA (1991) Clinical and immune modulatory effects of alternative weekly interleukin-2 and interferon alfa-2a in patients with advanced renal cell carcinoma and melanoma. Br J Cancer 63:287–292
Punt KC, Jansen RL, De Mulder PH, Batchelor D, Galazka A, Bolhuis RL, Stoter G (1992) Repetitive weekly cycles of 4-day continuous infusion of recombinant interleukin-2: a phase I study. J Immunother (1991) 12:277–284
Quan WD Jr, Quan FM (2003) Outpatient experience with moderate dose bolus interleukin-2 in metastatic malignant melanoma and kidney cancer. J Immunother 26:286–290
Quan W Jr, Ramirez M, Taylor C, Quan F, Vinogradov M, Walker P (2005) Administration of high-dose continuous infusion interleukin-2 to patients age 70 or over. Cancer Biother Radiopharm 20:11–15
Quan WD Jr, Milligan KS, Quan FM, Cuenca RE, Khan N, Liles DK, Walker PR (2006) Continuous infusion interleukin-2 and intravenous famotidine in metastatic melanoma. Cancer Biother Radiopharm 21:607–612
Radny P, Caroli UM, Bauer J, Paul T, Schlegel C, Eigentler TK, Weide B, Schwarz M, Garbe C (2003) Phase II trial of intralesional therapy with interleukin-2 in soft-tissue melanoma metastases. Br J Cancer 89:1620–1626
Rao RD, Anderson PM, Arndt CA, Wettstein PJ, Markovic SN (2003) Aerosolized granulocyte macrophage colony-stimulating factor (GM-CSF) therapy in metastatic cancer. Am J Clin Oncol 26:493–498
Richards JM, Barker E, Latta J, Ramming K, Vogelzang NJ (1988) Phase I study of weekly 24-hour infusions of recombinant human interleukin-2. J Natl Cancer Inst 80:1325–1328
Ridolfi L, Ridolfi R, Ascari-Raccagni A, Fabbri M, Casadei S, Gatti A, Trevisan G, Righini MG (2001) Intralesional granulocyte-monocyte colony-stimulating factor followed by subcutaneous interleukin-2 in metastatic melanoma: a pilot study in elderly patients. J Eur Acad Dermatol Venereol 15:218–223
Robert C, Long GV, Brady B, Dutriaux C, Maio M, Mortier L, Hassel JC, Rutkowski P, Mcneil C, Kalinka-Warzocha E, Savage KJ, Hernberg MM, Lebbe C, Charles J, Mihalcioiu C, Chiarion-Sileni V, Mauch C, Cognetti F, Arance A, Schmidt H, Schadendorf D, Gogas H, Lundgren-Eriksson L, Horak C, Sharkey B, Waxman IM, Atkinson V, Ascierto PA (2015a) Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med 372:320–330
Robert C, Schachter J, Long GV, Arance A, Grob JJ, Mortier L, Daud A, Carlino MS, Mcneil C, Lotem M, Larkin J, Lorigan P, Neyns B, Blank CU, Hamid O, Mateus C, Shapira-Frommer R, Kosh M, Zhou H, Ibrahim N, Ebbinghaus S, Ribas A, Investigators, K (2015b) Pembrolizumab versus Ipilimumab in Advanced Melanoma. N Engl J Med 372:2521–2532
Robertson MJ, Mier JW, Logan T, Atkins M, Koon H, Koch KM, Kathman S, Pandite LN, Oei C, Kirby LC, Jewell RC, Bell WN, Thurmond LM, Weisenbach J, Roberts S, Dar MM (2006) Clinical and biological effects of recombinant human interleukin-18 administered by intravenous infusion to patients with advanced cancer. Clin Cancer Res 12:4265–4273
Rosenberg SA, White DE (1996) Vitiligo in patients with melanoma: normal tissue antigens can be targets for cancer immunotherapy. J Immunother Emphasis Tumor Immunol 19:81–84
Rosenberg SA, Grimm EA, Mcgrogan M, Doyle M, Kawasaki E, Koths K, Mark DF (1984) Biological activity of recombinant human interleukin-2 produced in Escherichia coli. Science 223:1412–1414
Rosenberg SA, Lotze MT, Muul LM, Leitman S, Chang AE, Ettinghausen SE, Matory YL, Skibber JM, Shiloni E, Vetto JT et al (1985) Observations on the systemic administration of autologous lymphokine-activated killer cells and recombinant interleukin-2 to patients with metastatic cancer. N Engl J Med 313:1485–1492
Rosenberg SA, Lotze MT, Yang JC, Aebersold PM, Linehan WM, Seipp CA, White DE (1989) Experience with the use of high-dose interleukin-2 in the treatment of 652 cancer patients. Ann Surg 210:474–484; discussion 484–5
Rosenberg SA, Yang JC, Topalian SL, Schwartzentruber DJ, Weber JS, Parkinson DR, Seipp CA, Einhorn JH, White DE (1994) Treatment of 283 consecutive patients with metastatic melanoma or renal cell cancer using high-dose bolus interleukin 2. JAMA 271:907–913
Rosenberg SA, Yang JC, Schwartzentruber DJ, Hwu P, Marincola FM, Topalian SL, Restifo NP, Dudley ME, Schwarz SL, Spiess PJ, Wunderlich JR, Parkhurst MR, Kawakami Y, Seipp CA, Einhorn JH, White DE (1998a) Immunologic and therapeutic evaluation of a synthetic peptide vaccine for the treatment of patients with metastatic melanoma. Nat Med 4:321–327
Rosenberg SA, Yang JC, White DE, Steinberg SM (1998b) Durability of complete responses in patients with metastatic cancer treated with high-dose interleukin-2: identification of the antigens mediating response. Ann Surg 228:307–319
Rosenberg SA, Sportes C, Ahmadzadeh M, Fry TJ, Ngo LT, Schwarz SL, Stetler-Stevenson M, Morton KE, Mavroukakis SA, Morre M, Buffet R, Mackall CL, Gress RE (2006) IL-7 administration to humans leads to expansion of CD8+ and CD4+ cells but a relative decrease of CD4+ T-regulatory cells. J Immunother 29:313–319
Rosener M, Schwulera U, Menke G, Thrun A, Lissner R, Krauseneck P, Bogdahn U, Martin R (1993) Tolerance and cerebrospinal fluid pharmacokinetics of intrathecally administered human natural interleukin-2: a phase I trial. Eur Cytokine Netw 4:189–195
Rosenthal NS, Hank JA, Kohler PC, Minkoff DZ, Moore KH, Bechhofer R, Hong R, Storer B, Sondel PM (1988) The in vitro function of lymphocytes from 25 cancer patients receiving four to seven consecutive days of recombinant IL-2. J Biol Response Mod 7:123–139
Rosso R, Sertoli MR, Queirolo P, Sanguineti O, Barzacchi MC, Mariani GL, Miglio L, Venturini M, Toma S (1992) An outpatient phase I study of a subcutaneous interleukin-2 and intramuscular alpha-2a-interferon combination in advanced malignancies. Ann Oncol 3:559–563
Royal RE, Steinberg SM, Krouse RS, Heywood G, White DE, Hwu P, Marincola FM, Parkinson DR, Schwartzentruber DJ, Topalian SL, Yang JC, Rosenberg SA (1996) Correlates of response to IL-2 therapy in patients treated for metastatic renal cancer and melanoma. Cancer J Sci Am 2:91–98
Rubin JT, Elwood LJ, Rosenberg SA, Lotze MT (1989) Immunohistochemical correlates of response to recombinant interleukin-2-based immunotherapy in humans. Cancer Res 49:7086–7092
Rubin JT, Day R, Duquesnoy R, Simonis B, Adams S, Lee J, Lotze MT (1995) HLA-DQ1 is associated with clinical response and survival of patients with melanoma who are treated with interleukin-2. Ther Immunol 2:1–6
Sabatino M, Kim-Schulze S, Panelli MC, Stroncek D, Wang E, Taback B, Kim DW, Deraffele G, Pos Z, Marincola FM, Kaufman HL (2009) Serum vascular endothelial growth factor and fibronectin predict clinical response to high-dose interleukin-2 therapy. J Clin Oncol 27:2645–2652
Safwat A, Schmidt H, Bastholt L, Fode K, Larsen S, Aggerholm N, Von Der Maase H (2005) A phase II trial of low-dose total body irradiation and subcutaneous interleukin-2 in metastatic melanoma. Radiother Oncol 77:143–147
Salvo G, Samoggia P, Masciulli R, Boccoli G, Allavena P, Mariani G, Bullo A, Montesoro E, Bulgarini D, Carlini P et al (1992) Interleukin-2 bolus therapy induces immediate and selective disappearance from peripheral blood of all lymphocyte subpopulations displaying natural killer activity: role of cell adhesion to endothelium. Eur J Cancer 28A:818–825
Samlowski WE, Park KJ, Galinsky RE, Ward JH, Schumann GB (1993) Intrathecal administration of interleukin-2 for meningeal carcinomatosis due to malignant melanoma: sequential evaluation of intracranial pressure, cerebrospinal fluid cytology, and cytokine induction. J Immunother Emphasis Tumor Immunol 13:49–54
Sanda MG, Yang JC, Topalian SL, Groves ES, Childs A, Belfort R, De Smet MD, Schwartzentruber DJ, White DE, Lotze MT et al (1992) Intravenous administration of recombinant human macrophage colony-stimulating factor to patients with metastatic cancer: a phase I study. J Clin Oncol 10:1643–1649
Sarna G, Machleder H, Collins J, Bonavida B, Jacobs E, Hawkins R, Golub S, Shau H, Fahey J, Popow J et al (1994) A comparative study of intravenous versus intralymphatic interleukin-2, with assessment of effects of interleukin-2 on both peripheral blood and thoracic-duct lymph. J Immunother Emphasis Tumor Immunol 15:140–146
Schaafsma MR, Falkenburg JH, Landegent JE, Duinkerken N, Osanto S, Ralph P, Kaushansky K, Wagemaker G, van Damme J, Willemze R et al (1991) In vivo production of interleukin-5, granulocyte-macrophage colony-stimulating factor, macrophages colony-stimulating factor, and interleukin-6 during intravenous administration of high-dose interleukin-2 in cancer patients. Blood 78:1981–1987
Schmidt H, Larsen S, Bastholt L, Fode K, Rytter C, von der Maase H (2002) A phase II study of outpatient subcutaneous histamine dihydrochloride, interleukin-2 and interferon-alpha in patients with metastatic melanoma. Ann Oncol 13:1919–1924
Schwartzentruber DJ (1993) In vitro predictors of clinical response in patients receiving interleukin-2-based immunotherapy. Curr Opin Oncol 5:1055–1058
Schwartzentruber DJ (2000) Interleukin-2: clinical applications. Principles of administration and management of side effects. In: Rosenberg SA (ed) Principles and practice of the biologic therapy of cancer. Lippincott Williams & Wilkins, Philadelphia
Schwartzentruber DJ (2001) Guidelines for the safe administration of high-dose interleukin-2. J Immunother 24:287–293
Schwartzentruber DJ, Lawson DH, Richards JM, Conry RM, Miller DM, Treisman J, Gailani F, Riley L, Conlon K, Pockaj B, Kendra KL, White RL, Gonzalez R, Kuzel TM, Curti B, Leming PD, Whitman ED, Balkissoon J, Reintgen DS, Kaufman H, Marincola FM, Merino MJ, Rosenberg SA, Choyke P, Vena D, Hwu P (2011) gp100 peptide vaccine and interleukin-2 in patients with advanced melanoma. N Engl J Med 364: 2119–2127
Smith IJ, Kurt RA, Baher AG, Denman S, Justice L, Doran T, Gilbert M, Alvord WG, Urba WJ (2003) Immune effects of escalating doses of granulocyte-macrophage colony-stimulating factor added to a fixed, low-dose, inpatient interleukin-2 regimen: a randomized phase I trial in patients with metastatic melanoma and renal cell carcinoma. J Immunother 26:130–138
Smith FO, Goff SL, Klapper JA, Levy C, Allen T, Mavroukakis SA, Rosenberg SA (2007) Risk of bowel perforation in patients receiving interleukin-2 after therapy with anti-CTLA 4 monoclonal antibody. J Immunother 30:130
Soiffer RJ, Chapman PB, Murray C, Williams L, Unger P, Collins H, Houghton AN, Ritz J (1997) Administration of R24 monoclonal antibody and low-dose interleukin 2 for malignant melanoma. Clin Cancer Res 3:17–24
Sondel PM, Kohler PC, Hank JA, Moore KH, Rosenthal NS, Sosman JA, Bechhofer R, Storer B (1988) Clinical and immunological effects of recombinant interleukin 2 given by repetitive weekly cycles to patients with cancer. Cancer Res 48:2561–2567
Sosman JA, Kohler PC, Hank J, Moore KH, Bechhofer R, Storer B, Sondel PM (1988) Repetitive weekly cycles of recombinant human interleukin-2: responses of renal carcinoma with acceptable toxicity. J Natl Cancer Inst 80:60–63
Sosman JA, Weiss GR, Margolin KA, Aronson FR, Sznol M, Atkins MB, O’boyle K, Fisher RI, Boldt DH, Doroshow J et al (1993) Phase IB clinical trial of anti-CD3 followed by high-dose bolus interleukin-2 in patients with metastatic melanoma and advanced renal cell carcinoma: clinical and immunologic effects. J Clin Oncol 11:1496–1505
Sosman JA, Kefer C, Fisher RI, Jacobs CD, Pumfery P, Ellis TM (1995) A phase IA/IB trial of anti-CD3 murine monoclonal antibody plus low-dose continuous-infusion interleukin-2 in advanced cancer patients. J Immunother Emphasis Tumor Immunol 17:171–180
Sosman JA, Aronson FR, Sznol M, Atkins MB, Dutcher JP, Weiss GR, Isaacs RE, Margolin KA, Fisher RI, Ernest ML, Mier J, Oleksowicz L, Eckhardt JR, Levitt D, Doroshow JH (1997) Concurrent phase I trials of intravenous interleukin 6 in solid tumor patients: reversible dose-limiting neurological toxicity. Clin Cancer Res 3:39–46
Sosman JA, Carrillo C, Urba WJ, Flaherty L, Atkins MB, Clark JI, Dutcher J, Margolin KA, Mier J, Gollob J, Kirkwood JM, Panka DJ, Crosby NA, O’boyle K, Lafleur B, Ernstoff MS (2008) Three phase II cytokine working group trials of gp100 (210M) peptide plus high-dose interleukin-2 in patients with HLA-A2-positive advanced melanoma. J Clin Oncol 26:2292–2298
Sparano JA, Fisher RI, Sunderland M, Margolin K, Ernest ML, Sznol M, Atkins MB, Dutcher JP, Micetich KC, Weiss GR et al (1993) Randomized phase III trial of treatment with high-dose interleukin-2 either alone or in combination with interferon alfa-2a in patients with advanced melanoma. J Clin Oncol 11:1969–1977
Stein RC, Malkovska V, Morgan S, Galazka A, Aniszewski C, Roy SE, Shearer RJ, Marsden RA, Bevan D, Gordon-Smith EC et al (1991) The clinical effects of prolonged treatment of patients with advanced cancer with low-dose subcutaneous interleukin-2 [corrected]. Br J Cancer 63:275–278
Sullivan RJ, Hoshida Y, Logan T, Khushalani NI, Giobbie-Hurder A, Margolin KA, Roder J, Bhatt R, Koon H, Olencki T, Hutson T, Curti B, Blackmon S, Mier JW, Roder H, Stewart J, Amin A, Ernstroff M, Clark J, Atkins MB, Kaufman H, Sosman J, Signoretti S, Mcdermott DF (2016) High Dose Interleukin 2 (HD IL-2) Select Trial in Melanoma: A tissue and blood collection protocol to identify predictive biomarkers of response to HD IL-2 in patients with advanced melanoma. Society of Immunotherapy in Cancer Annual Meeting, National Harbor
Sznol M, Mier JW, Sparano J, Gaynor ER, Weiss GR, Margolin KA, Bar MH, Hawkins MJ, Atkins MB, Dutcher JP et al (1990) A phase I study of high-dose interleukin-2 in combination with interferon-alpha 2b. J Biol Response Mod 9:529–537
Tagliaferri P, Barile C, Caraglia M, Guarrasi R, Morelli D, Ricciardi B, Martignetti A, Librera MT, Matano E, Della Vecchia A, Catalano G, Famiani M, Palmieri G, Correale P, Bianco AR (1998) Daily low-dose subcutaneous recombinant interleukin-2 by alternate weekly administration: antitumor activity and immunomodulatory effects. Am J Clin Oncol 21:48–53
Taniguchi T, Matsui H, Fujita T, Takaoka C, Kashima N, Yoshimoto R, Hamuro J (1983) Structure and expression of a cloned cDNA for human interleukin-2. Nature 302:305–310
Tarhini AA, Kirkwood JM, Gooding WE, Cai C, Agarwala SS (2007) Durable complete responses with high-dose bolus interleukin-2 in patients with metastatic melanoma who have experienced progression after biochemotherapy. J Clin Oncol 25:3802–3807
Tartour E, Blay JY, Dorval T, Escudier B, Mosseri V, Douillard JY, Deneux L, Gorin I, Negrier S, Mathiot C, Pouillart P, Fridman WH (1996) Predictors of clinical response to interleukin-2--based immunotherapy in melanoma patients: a French multiinstitutional study. J Clin Oncol 14:1697–1703
Taylor CW, Chase EM, Whitehead RP, Rinehart JJ, Neidhart JA, Gonzalez R, Bunn PA, Hersh EM (1992) A Southwest Oncology Group Phase I study of the sequential combination of recombinant interferon-gamma and recombinant interleukin-2 in patients with cancer. J Immunother (1991) 11:176–183
Thatcher N, Dazzi H, Johnson RJ, Russell S, Ghosh AK, Moore M, Chadwick G, Craig RD (1989) Recombinant interleukin-2 (rIL-2) given intrasplenically and intravenously for advanced malignant melanoma. A phase I and II study. Br J Cancer 60:770–774
Thatcher N, Dazzi H, Mellor M, Ghosh A, Carrington B, Johnson RJ, Loriaux EM, Craig RP (1990) Recombinant interleukin-2 (rIL-2) with flavone acetic acid (FAA) in advanced malignant melanoma: a phase II study. Br J Cancer 61:618–621
Thomas H, Barton C, Saini A, Dalgleish A, Waxman J (1992) Sequential interleukin-2 and alpha interferon for renal cell carcinoma and melanoma. Eur J Cancer 28A:1047–1049
Thompson JA, Lee DJ, Cox WW, Lindgren CG, Collins C, Neraas KA, Dennin RA, Fefer A (1987) Recombinant interleukin 2 toxicity, pharmacokinetics, and immunomodulatory effects in a phase I trial. Cancer Res 47:4202–4207
Thompson JA, Lee DJ, Lindgren CG, Benz LA, Collins C, Levitt D, Fefer A (1988) Influence of dose and duration of infusion of interleukin-2 on toxicity and immunomodulation. J Clin Oncol 6:669–678
Tilg H, Shapiro L, Atkins MB, Dinarello CA, Mier JW (1993) Induction of circulating and erythrocyte-bound IL-8 by IL-2 immunotherapy and suppression of its in vitro production by IL-1 receptor antagonist and soluble tumor necrosis factor receptor (p75) chimera. J Immunol 151:3299–3307
Tilg H, Atkins MB, Dinarello CA, Mier JW (1995) Induction of circulating interleukin 10 by interleukin 1 and interleukin 2, but not interleukin 6 immunotherapy. Cytokine 7:734–739
Trehu EG, Mier JW, Dubois JS, Sorce D, Klempner MS, Epstein M, Dinarello CA, Shapiro L, Kappler K, Ronayne L, Atkins MB (1996) Phase I trial of interleukin 2 in combination with the soluble tumor necrosis factor receptor p75 IgG chimera. Clin Cancer Res 2:1341–1351
Triozzi PL, Kim JA, Martin EW, Young DC, Benzies T, Villasmil PM (1995) Phase I trial of escalating doses of interleukin-1 beta in combination with a fixed dose of interleukin-2. J Clin Oncol 13:482–489
Tritarelli E, Rocca E, Testa U, Boccoli G, Camagna A, Calabresi F, Peschle C (1991) Adoptive immunotherapy with high-dose interleukin-2: kinetics of circulating progenitors correlate with interleukin-6, granulocyte colony-stimulating factor level. Blood 77:741–749
Urba WJ, Steis RG, Longo DL, Kopp WC, Maluish AE, Marcon L, Nelson DL, Stevenson HC, Clark JW (1990) Immunomodulatory properties and toxicity of interleukin 2 in patients with cancer. Cancer Res 50:185–192
van Haelst Pisani C, Kovach JS, Kita H, Leiferman KM, Gleich GJ, Silver JE, Dennin R, Abrams JS (1991) Administration of interleukin-2 (IL-2) results in increased plasma concentrations of IL-5 and eosinophilia in patients with cancer. Blood 78:1538–1544
Veelken H, Rosenthal FM, Schneller F, von Schilling C, Guettler IC, Herrmann F, Mertelsmann R, Lindemann A (1992) Combination of interleukin-2 and interferon-alpha in renal cell carcinoma and malignant melanoma: a phase II clinical trial. Biotechnol Ther 3:1–14
Verdi CJ, Taylor CW, Croghan MK, Dalke P, Meyskens FL, Hersh EM (1992) Phase I study of low-dose cyclophosphamide and recombinant interleukin-2 for the treatment of advanced cancer. J Immunother (1991) 11:286–291
Vetto JT, Papa MZ, Lotze MT, Chang AE, Rosenberg SA (1987) Reduction of toxicity of interleukin-2 and lymphokine-activated killer cells in humans by the administration of corticosteroids. J Clin Oncol 5: 496–503
Viens P, Blaise D, Stoppa AM, Brandely M, Baume D, Olive D, Resbeut M, Delpero JR, Lopez M, Aubert C et al (1992) Interleukin-2 in association with increasing doses of interferon-gamma in patients with advanced cancer. J Immunother (1991) 11:218–224
Vlasveld LT, Rankin EM, Hekman A, Rodenhuis S, Beijnen JH, Hilton AM, Dubbelman AC, Vyth-Dreese FA, Melief CJ (1992) A phase I study of prolonged continuous infusion of low dose recombinant interleukin-2 in melanoma and renal cell cancer. Part I: clinical aspects. Br J Cancer 65:744–750
Vlasveld LT, Horenblas S, Hekman A, Hilton AM, Dubbelman AC, Melief CJ, Rankin EM (1994) Phase II study of intermittent continuous infusion of low-dose recombinant interleukin-2 in advanced melanoma and renal cell cancer. Ann Oncol 5:179–181
Vuoristo M, Jantunen I, Pyrhonen S, Muhonen T, Kellokumpu-Lehtinen P (1994) A combination of subcutaneous recombinant interleukin-2 and recombinant interferon-alpha in the treatment of advanced renal cell carcinoma or melanoma. Eur J Cancer 30A:530–532
Weber J, Yang JC, Topalian SL, Parkinson DR, Schwartzentruber DS, Ettinghausen SE, Gunn H, Mixon A, Kim H, Cole D et al (1993) Phase I trial of subcutaneous interleukin-6 in patients with advanced malignancies. J Clin Oncol 11:499–506
Weber J, Gunn H, Yang J, Parkinson D, Topalian S, Schwartzentruber D, Ettinghausen S, Levitt D, Rosenberg SA (1994) A phase I trial of intravenous interleukin-6 in patients with advanced cancer. J Immunother Emphasis Tumor Immunol 15:292–302
Weidmann E, Bergmann L, Stock J, Kirsten R, Mitrou PS (1992) Rapid cytokine release in cancer patients treated with interleukin-2. J Immunother (1991) 12:123–131
Weiner LM, Padavic-Shaller K, Kitson J, Watts P, Krigel RL, Litwin S (1991) Phase I evaluation of combination therapy with interleukin 2 and gamma-interferon. Cancer Res 51:3910–3918
Weinreich DM, Rosenberg SA (2002) Response rates of patients with metastatic melanoma to high-dose intravenous interleukin-2 after prior exposure to alpha-interferon or low-dose interleukin-2. J Immunother 25:185–187
Whitehead RP, Ward D, Hemingway L, Hemstreet GP 3rd, Bradley E, Konrad M (1990) Subcutaneous recombinant interleukin 2 in a dose escalating regimen in patients with metastatic renal cell adenocarcinoma. Cancer Res 50:6708–6715
Whitehead RP, Kopecky KJ, Samson MK, Costanzi JJ, Natale RB, Feun LG, Hersh EM, Rinehart JJ (1991) Phase II study of intravenous bolus recombinant interleukin-2 in advanced malignant melanoma: Southwest Oncology Group study. J Natl Cancer Inst 83:1250–1252
Whitehead RP, Figlin R, Citron ML, Pfile J, Moldawer N, Patel D, Jones G, Levitt D, Zeffren J (1993) A phase II trial of concomitant human interleukin-2 and interferon-alpha-2a in patients with disseminated malignant melanoma. J Immunother Emphasis Tumor Immunol 13:117–121
Wiebke EA, Rosenberg SA, Lotze MT (1988) Acute immunologic effects of interleukin-2 therapy in cancer patients: decreased delayed type hypersensitivity response and decreased proliferative response to soluble antigens. J Clin Oncol 6:1440–1449
Yang JC, Rosenberg SA (1997) An ongoing prospective randomized comparison of interleukin-2 regimens for the treatment of metastatic renal cell cancer. Cancer J Sci Am 3(Suppl 1):S79–S84
Yang JC, Topalian SL, Schwartzentruber DJ, Parkinson DR, Marincola FM, Weber JS, Seipp CA, White DE, Rosenberg SA (1995) The use of polyethylene glycol-modified interleukin-2 (PEG-IL-2) in the treatment of patients with metastatic renal cell carcinoma and melanoma. A phase I study and a randomized prospective study comparing IL-2 alone versus IL-2 combined with PEG-IL-2. Cancer 76:687–694
Yang JC, Sherry RM, Steinberg SM, Topalian SL, Schwartzentruber DJ, Hwu P, Seipp CA, Rogers-Freezer L, Morton KE, White DE, Liewehr DJ, Merino MJ, Rosenberg SA (2003) Randomized study of high-dose and low-dose interleukin-2 in patients with metastatic renal cancer. J Clin Oncol 21:3127–3132
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this entry
Cite this entry
Haanen, J.B.A.G., Sullivan, R.J., Kirkwood, J.M., Atkins, M.B., Schwartzentruber, D.J. (2020). Cytokines (IL-2, IFN, GM-CSF, etc.) Melanoma. In: Balch, C., et al. Cutaneous Melanoma. Springer, Cham. https://doi.org/10.1007/978-3-030-05070-2_56
Download citation
DOI: https://doi.org/10.1007/978-3-030-05070-2_56
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-05068-9
Online ISBN: 978-3-030-05070-2
eBook Packages: MedicineReference Module Medicine