Abstract
Resistant hypertension (HTN) is defined as uncontrolled blood pressure ≥ 130/80 mm Hg despite treatment with adequate dosages of three or more antihypertensive medications, one of which is a diuretic or requiring a regimen of four or more medications for control. As is evident from the definition, controlling blood pressure is a challenge in this population. This lack of blood pressure control puts these patients at additional cardiovascular risk compared to the nonresistant hypertensive populations. It is well known and established that lowering blood pressure translates in lower risk of cardiovascular morbidity and mortality and is the cornerstone of the management of HTN. It is thus concerning that blood pressure-lowering trials in patients with resistant HTN have not uniformly translated in improved outcomes. This chapter will encompass definition of resistant HTN and factors that make blood pressure more resistant to treatment, together with the role of physical fitness, exercise, and cardiorespiratory fitness on lowering blood pressure, morbidity, and mortality in this subgroup of hypertensives.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Hypertension (HTN) is the most common treatable risk factor for cardiovascular (CV) disease. Lowering blood pressure (BP) has been the most pivotal intervention in decreasing CV morbidity and mortality not just in patients with isolated HTN but also in hypertensives with comorbidities like type 2 diabetes mellitus (DM2), dyslipidemia, chronic kidney disease (CKD), and other established CV diseases like coronary artery disease and cerebrovascular disease.
The direct association between BP levels and CV events has been known since the initial Framingham Heart Study reports in the 1950s showing a strong association between HTN and outcomes including myocardial infarction, congestive heart failure, strokes, and kidney disease [1]. The benefit of lowering BP with medications to improve CV outcomes and mortality has been recognized since Dr. Edward Freis’ landmark Department of Veterans Affairs Cooperative Study [2]. Great advances have been made since then in managing HTN with resulting improved outcomes. However, there remains a group of treated hypertensives that continues to be at high risk in spite of these advances. These are patients with resistant HTN in whom either BP remains uncontrolled ≥130/80 mm of Hg despite being treated simultaneously with optimal dosages of ≥3 antihypertensive medications, one of which is a diuretic, or in whom BP may be controlled but who require ≥4 or more antihypertensive agents. It should be noted that this is the new definition of resistant HTN per the latest guidelines formulated in 2017, prior to which resistant HTN was said to be present when BP was ≥140/90 using the above parameters [3]. Whether this lack of control is a result of poor drug combinations or non-compliance, the fact remains that approximately 15–30% of the treated HTN population can be classified as having resistant HTN [4]. Patients with resistant HTN remain at an even higher risk for CV outcomes, renal outcomes, and all-cause mortality compared to patients who do not have resistant HTN [5] and have been a focus of the HTN community for the past several years. This increased CV risk due to resistant HTN has been shown in many studies. Daugherty et al., for example, reported that adverse CV outcomes were 50% higher in the resistant HTN group, driven mostly by chronic kidney disease [5]. In general, however, it is estimated that there is an over twofold higher risk of CV events in patients with resistant HTN compared to all patients being newly treated for HTN [3]. In one study the all-cause mortality was 40% higher in women with apparent resistant HTN compared to the nonresistant cohort [6]. Additionally, getting BP under control with polypharmacy does not necessarily afford the expected protection against CV outcomes in resistant hypertensive patients. This was evident in a large Kaiser Permanente study which showed that the highest number of events occurred in the group of patients in whom BP was controlled but with four or more antihypertensive medications. This group of patients indeed had an even worse outcome than the group of patients who had uncontrolled BP with three antihypertensive medications [7].
Thus it is imperative to investigate interventions other than drug therapy to determine if additional methods can be identified which could help improve prognosis of patients with resistant HTN. Modalities other than medications have been studied in RH with mixed results. Some of these have been invasive procedures aiming to modify neurogenic or hormonal factors known to adversely impact BP. However, two such interventions, carotid baroreceptor stimulation and renal nerve denervation, were found to be either not widely applicable [8] or ineffective in controlled double blind randomized trials [9].
The impact of cardiorespiratory fitness (CRF) on BP has been studied in varied populations including normotensives, prehypertensives, and hypertensives [10]. Regularly performed exercise leading to improvements in CRF has been shown to lower blood pressure in patients with prehypertension, HTN, and even resistant HTN [10]. Large and well-conducted epidemiologic studies have also shown an inverse and graded association between CRF and mortality in the general hypertensive population [11]. However, it is not known if increased CRF can attenuate mortality risk in patients with resistant HTN. This chapter will discuss the factors associated with and those that predispose to the development of RH and factors that make BP more resistant to treatment, together with the impact of physical activity (PA), exercise, and CRF on lowering BP, morbidity, and mortality in patients with resistant HTN.
Factors Associated with Resistant Hypertension
Resistant HTN can be present in patients without any additional factors; however, certain conditions are likely to be associated with it [12]. Conditions commonly associated with a higher prevalence of resistant HTN are older age, obesity, smoking, obstructive sleep apnea (OSA), DM2, left ventricular hypertrophy (LVH), and CKD. However, there are several other factors and conditions that can render HTN difficult to control including use of excessive sodium, alcohol, certain medications, and secondary forms of HTN associated with endocrine disorders, central nervous system tumors, and coarctation of aorta [13]. An effort should always be made to identify the treatable forms of HTN during initial evaluation of all hypertensive patients based on history, physical examination, and focused laboratory testing and imaging. It has been shown that addressing these risk factors for resistant HTN helps in lowering BP and the benefits of exercise in these populations have been substantiated by several studies, albeit not all in patients with resistant HTN. The next section focuses on the effect of physical activity (PA), exercise training, and/or CRF on certain risk factors of resistant HTN.
Effect of PA and CRF on Risk Factors for Resistant Hypertension
Age
RH is most common in older hypertensives [12]. In this group uncontrolled systolic BP is the main problem. Additionally, older hypertensives generally have other risk factors which increase the susceptibility to develop RH. Even in the absence of additional risk factors, aging contributes to arterial stiffness and decreased aortic compliance [12, 14], which predispose to additional cardiovascular risks. Studies of effect of exercise on central hemodynamics in elderly patients with RH are not available; however, McDonnell et al. [15] have demonstrated that regular exercise is associated with lower systolic BP, diastolic BP, and large artery stiffness in older individuals. A limitation in treating elderly patients with HTN, especially in situations requiring polypharmacy for several concomitant illnesses, is the risk of orthostatic hypotension, which predisposes to syncope, falls, and injuries. Taking this into consideration, the role of moderate- to high-intensity exercise to facilitate control of BP and thereby decrease the requirement for pharmacological therapy is critical in elderly hypertensives. Beneficial effects of exercise in elderly have been validated by many studies, and it is recommended that exercise be implemented in elderly to manage HTN [16,17,18,19,20,21,22,23].
Obstructive Sleep Apnea
It has been long known that OSA increases the risk of CV events. Association of OSA with HTN is also well established, and it is recommended that patients with treatment-resistant HTN be screened for OSA [24]. Increased arterial stiffness has been shown to be present in patients with OSA even in the absence of HTN. In a study of 1921 subjects, patients with moderate to severe OSA had higher brachial-ankle pulse wave velocity at baseline, and severity of OSA predicted future severity of arterial stiffness [25]. There are several other pathological changes precipitated by OSA which can facilitate the development of RH. Some of these changes are secondary to periods of hypoxia caused by OSA leading to activation of endothelin and sympathetic nervous systems [26, 27], which can lead to the development of RH. Exercise intervention studies in OSA patients with RH are lacking; however, regularly performed aerobic exercises have been shown to decrease BP in hypertensive patients with OSA [24].
Diabetes Mellitus
Diabetic patients have a higher risk of having RH. A number of pathophysiologic processes could be contributing to it. Elia et al. [28] in a prospective study reported that DM2 patients had significantly higher pulse wave velocity (PWV) compared to nondiabetics. This risk was nine times higher in uncontrolled diabetics than in nondiabetics. As stated above hypertensive LVH is a risk factor for RH. Coexistence of DM2 with HTN further increases the risk for increase in LV mass, LV dysfunction, and arterial stiffness [29]. While exercise intervention studies focusing only on diabetic patients with RH are not available, exercise training in diabetic hypertensives has been reported to improve not just BP and diabetic control but also endothelial function and left ventricular diastolic function [30]. In a meta-analysis reviewing the effects of supervised exercise on BP and lipid levels in high-risk diabetic patients with HTN and dyslipidemia, 42 trials with 2808 patients were included. Results showed that structured exercise was associated with lowering of systolic BP, diastolic BP, and low-density lipoprotein cholesterol and an increase in high-density lipoprotein cholesterol [31]. Exercise intervention studies in diabetics with RH should be a field for future research.
Left Ventricular Hypertrophy
LVH is a known risk factor of poorer cardiovascular outcomes and mortality in hypertensives. Risk of having resistant HTN is higher in hypertensives who have LVH [12]. Fernando et al. reported that regression of electrocardiographic LVH in patients with RH is protective against a composite endpoint of cardiovascular events, CV mortality, and all-cause mortality [32]. Studies in RH with LVH have shown that exercise training can help lower BP, decrease medication requirement, and even lead to regression of LVH in some cases. In a study of 46 African-American patients with severe HTN and LVH, patients were assigned to a 16-week exercise training or a control group. Exercise training was effective in lowering BP, decreasing antihypertensive medications, and decreasing LVH [33]. No exercise related or other adverse events were noted in the study. These patients were on multiple antihypertensive medications, and several met the criteria for RH. Based on these studies, it is evident that exercise has a role in managing patients with RH and regression of LVH in these patients results in improved CV and mortality outcomes.
Chronic Kidney Disease
RH is commonly seen in patients with CKD. There are several factors in CKD patients with RH that can make BP difficult to control including sodium and water retention. Arterial stiffness is also enhanced in patients with CKD; hence the increase in volume from sodium and water retention is not able to be accommodated adequately. This effect is further exacerbated in CKD patients since eGFR is decreased and the increased volume cannot be handled appropriately. Aortic stiffness, which is seen with aging in hypertensives, is further enhanced by the presence of CKD, together with aortic calcification. These changes result in an increase in pulse pressure, PWV, central aortic pressures, and risk of developing LVH. These are known features of patients with RH which are further exacerbated by the presence of CKD. Arterial stiffness and calcification have additional adverse CV effects. Baroreceptor compensatory reflexes may be blunted in patients with decreased carotid compliance secondary to local structural changes, leading to rise in BP and limiting efforts to control it [12]. It is known that it is difficult to control blood pressure in the presence of CKD with most patients requiring three or more antihypertensive medications for control [34]. While exercise has been shown to benefit several conditions that are associated with and/or predispose to the risk of developing CKD as discussed above, not all studies have shown a favorable effect of exercise training in lowering BP in CKD hypertensives. In a group of 150 patients with stage 2–4 CKD and HTN without DM2, Barcellos et al. randomized 76 patients to exercise and 74 to a control group, with a primary aim of assessing change in eGFR and secondary aims of studying effects on weight, systolic BP, diastolic BP, functional capacity, and metabolic parameters [35]. Following 16 weeks of aerobic and resistance training, no between-group differences were noted in BP, eGFR, body weight, or lipid profile. Significant improvements were, however, noted in hs-CRP, fasting glucose, and functional capacity in the exercise group. In another small study of 11 diabetic, obese patients with stage 2–4 CKD on medical management, 7 patients were randomized to aerobic exercise [36]. The exercise consisted of 6 weeks of exercise training preceding 18 weeks of supervised home exercise. At the end of this 24-week study, only a nonsignificant decrease in systolic BP was noted. While in these studies the effect on BP was disappointing, it should not discourage future research to study the role of PA, exercise, and CRF in the management of these patients. This is especially important since no specific, large-scale studies have been done to prospectively assess the role of exercise training or CRF in managing RH in CKD patients and this field remains open for future research in these high-risk patients.
Central Aortic Pressures in Resistant Hypertension
Several risk factors associated with a higher prevalence of resistant HTN are also associated with structural changes in the aorta which lead to increase in central aortic blood pressures [12]. Increasing age leads to stiffening of the aorta [14] which is associated with decreased compliance and distensibility. Changes in distensibility of the aorta with age are likely secondary to decreases in elastic fibers and increase in collagen [37] and vascular smooth muscle cells [38].
It has been long known that in patients on antihypertensive therapy, cardiovascular risk remains elevated if central blood pressures are not controlled even if brachial pressures are within normal limits. In the Conduit Artery Function Evaluation (CAFE) study, the effects of two different combinations of antihypertensive therapies on changes in central aortic pulse pressures and hemodynamics were compared in 2199 patients to assess the impact on outcomes. At the end of follow-up, control of brachial systolic BP was similar in both groups, but central aortic pressure was lower in the group treated with amlodipine with possible addition of perindopril versus those treated with atenolol with possible addition of bendroflumethiazide. Lower central aortic pulse pressure was found to be significantly and directly associated with cardiovascular outcomes and renal events [39]. In a meta-analysis of 17 studies with a total of 15,877 patients who had a mean follow-up 7.7 years, predictive value of aortic PWV for CV events and all-cause mortality was assessed [40]. Authors reported that in patients with high PWV, the relative risk of total CV events was 2.26 (95% confidence interval: 1.89–2.70, 14 studies). Cardiovascular mortality was 2.02 (95% confidence interval: 1.68 to 2.42, 10 studies) and all-cause mortality 1.90 (95% confidence interval: 1.61 to 2.24, 11 studies). Patients with HTN and other established cardiovascular diseases had an even higher relative risk of cardiovascular event rate and mortality with increased aortic PWV. An increase of 1 m/s in aortic PWV increased the risks for all endpoints by 14–15%, and with a 1 standard deviation increase in aortic PWV, the risk for all endpoints rose by 42–42%. There are no long-term, prospective, randomized studies in this population to assess the long-term effect of exercise on abnormal aortic pressure indices in patients with RH. However, a study utilizing high-intensity interval training (HIIT) in high-risk hypertensive patients has shown some benefit as described in the next section.
High-Intensity Interval Training in Resistant Hypertension
The recommendations for PA and exercise to improve the risk factors of CV disease are PA spread over a several days per week to equal about 200 min per week. These recommendations are based on the beneficial effects of exercise on outcomes as assessed by PA questionnaires and/or objectively measured CRF. However, some studies have shown that shorter durations of higher-intensity exercise may help high-risk patients by having a favorable effect on central aortic pressures. Elevated central aortic pressure is an independent predictor of poorer outcomes in hypertensive patients, and it is known to be elevated in patients with resistant HTN [41]. In 50 high-risk patients with metabolic syndrome, effects of durations and frequencies of high-intensity interval training (HIIT) on aortic pressure were assessed. It was reported that only 4 min of HIIT, performed thrice a week, with a weekly volume of 12 min, performed for 16 weeks, was able to decrease aortic reservoir pressure [42]. Effects of HIIT in RH have not been explored and remain an open factor to investigate in future research.
Effect of Exercise and CRF on Resistant Hypertension
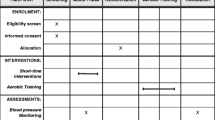
Effect of exercise in lowering BP has been evaluated by some investigators. In these studies, the prior definition to define RH was used which was BP of ≥140/90 mm Hg despite treatment with adequate dosages of three or more antihypertensive medications, one of which is a diuretic or requiring a regimen of four or more medications for control and not the new cutoff of ≥130/80 mm Hg. Dimeo et al. evaluated ambulatory BP and pulse wave analysis to assess arterial compliance and cardiac index in 50 patients with RH. Patients were randomized to exercise for 8–12 weeks on a treadmill or to a control group. Exercise intensity was monitored by serum lactate levels with a target of 2.0 ± 0.5 mmol/L. Exercise was effective in significantly lowering ambulatory daytime systolic and diastolic BP, and this reduction was seen during exertion as well. Exercise training also resulted in increased exercise capacity based on changes in maximal oxygen uptake and lactate curves. This study, however, did not show any change in arterial compliance and cardiac index [43].
In an interesting trial, Guimaraes et al. studied the effect of exercising in heated water on 24-h ambulatory BP parameters in patients with RH [44]. A total of 32 patients met the protocol enrollment criteria, of whom 16 were randomized to heated water exercise and 16 to a control group. Patients randomized to the active arm exercised for 60 min, thrice a week for 12 weeks in a pool heated to 32 °C, by walking and performing calisthenic exercises. No change in activity was recommended for the control group. In the control group, there was a significant increase noted in 24-h systolic and diastolic BP and daytime and nighttime diastolic BP. In contrast, in the active group, heated pool exercises significantly decreased office BP by 36/12 mm Hg together with a significant decrease in 24-h daytime and nighttime systolic BP and diastolic BP parameters.
Effect of CRF on Mortality in Patients with Resistant Hypertension
The protective effect of exercise against mortality in the general hypertensive patients has been shown in many studies. A review of literature which included 48,625 men and 47,625 women, with a minimum 1 year of follow-up, showed that both cardiovascular and all-cause mortality were inversely related to PA in all the studies. The authors reported that hypertensives who participated in any level of PA had a 16–67% reduced risk of CV mortality, whereas the inactive group had an over twofold increase risk of mortality [45].
The effect of PA, exercise, and CRF on mortality in patients with RH has not been evaluated in prospective, randomized, controlled studies. However, the association of CRF with all-cause mortality in patients with RH was studied by our group in African-American patients with RH [46]. From a group of 9968 patients, 1276 men were identified as having RH based on the prior definition of BP ≥140/90 mm Hg on three antihypertensive medications, one of which was a diuretic or use of >4 antihypertensive medications. All these patients had undergone an exercise tolerance test (ETT) at the Department of Veterans Affairs Medical Center in Washington, DC. To eliminate the confounding effect of age on exercise capacity, patients were categorized in four age-specific CRF groups according to the peak metabolic equivalents (METs) reached on a standard Bruce protocol. The mean follow-up was 9.5 ± 4.2 years during which an inverse relationship was noted between all-cause mortality and CRF, with mortality being the highest in the least-fit group and slowest in the high-fit group. In comparison to the least-fit group, mortality was 21% lower in the low-fit group, 36% lower in the moderate-fit group, and 62% lowest in the high-fit group (Fig. 9.1). This reduction was statistically significant in the moderate- and high-fit groups. With an increase in each MET in exercise capacity, the mortality rate decreased by 18%. This study did have limitations in that it included only African-Americans, male patients who had access to full, unrestricted medical management under the Veterans Affairs Medical Center umbrella. Thus, the results may not be generalizable to females, non-veterans, and patients of other racial backgrounds. Another limitation was that the analysis was based on data collected at baseline, and any changes in medications, level of CRF, and other lifestyle factors could not be taken into consideration. Nonetheless, these findings are gratifying considering the difficulty in altering the risk of CV events and all-cause mortality in RH patients, despite medical therapy as discussed earlier in this chapter. The study population had multiple CV risk factors (Table 9.1) and still benefited from having improved CRF.
The study also revealed a statistically lower systolic BP in the high-fit group (Table 9.2) which is an important finding, considering the difficulty in controlling BP in this group of patients.
It is also noteworthy that the METs achieved by the moderate-fit and high-fit groups were only 7.1 + 0.9 METs and 8.8 + 1.1 METs, respectively (Fig. 9.1).
This is a level that is likely to be easily achieved by most patients with RH as it is equivalent to just a 30–40-min brisk walk on most days of the week. To date no pharmacological study has shown an impact on mortality in RH population. Hence, it is gratifying to have a study supporting the inverse association of improved CRF with all-cause mortality in a subset of patients with RH. Future studies will likely validate the findings of this study and make the results generalizable to the general resistant hypertensive population.
Summary and Conclusions
RH is a disease that often defies control even with polypharmacy. This lack of BP control, at times, may be a pseudo-resistance to treatment, since it could be because of inadequate dosages or poor combinations of antihypertensive medications, non-compliance with therapy, or unhealthy lifestyles that interfere with BP control. Nevertheless, the result is that resistant hypertensives remain a high-risk population. They disproportionately utilize healthcare funds due to cost of medications, need for more frequent medical evaluations, and management of sequelae of RH. As discussed above it is not uncommon for these patients to have additional CV risk factors and comorbidities, like DM2, dyslipidemia, CKD, LVH, and obesity, which further increase the risk of future CV events. Increasing CRF has been shown to improve many of these coexisting cardiovascular indices and their related outcomes, in several studies [46, 47].
The role of improving CRF in complicated hypertensive patients is pivotal in managing not only HTN but also coexisting risk factors and conditions. As discussed above the degree of fitness, as measured by CRF, to realize CV and mortality, benefits are achievable for most patients, being equivalent to a 30–40-min brisk walk on most days of the week. This simple habit will have a beneficial effect not just on BP but also on other coexisting cardiovascular risk factors and decrease the global burden of CV outcomes including all-cause mortality. To date several studies have endorsed the role of PA, exercise, and CRF in decreasing morbidity and mortality in hypertensives with and without coexisting conditions. Such large, prospective, randomized, long-term studies are lacking in RH. Available studies, however, have verified the role of PA and exercise training in positively modifying the pathological vascular changes that are seen in RH including increased PWV and high central aortic pressure. Exercise training has been shown to regress LVH in patients with resistant HTN. Lastly, there is a strong inverse relationship between CRF and all-cause mortality in patients with RH.
Collectively data presented in this chapter establish the significant role of improving physical fitness in decreasing morbidity and all-cause mortality in patients with RH. It is thus imperative that efforts should be made by healthcare professionals to consider providing physical activity and exercise guidance as critical as prescribing medications. They should inform their patients that the best probability of controlling their BP and, perhaps, decreasing their dependence on medications is by adopting a healthy lifestyle. This is an important factor to be considered since RH patients not only require polypharmacy for HTN but also for concomitant medical conditions, like DM2, CKD, CV diseases, and dyslipidemia. Physicians should, however, emphasize to patients adopting positive changes in levels of PA and/or exercise that these changes have to be sustained long term, essentially life long, because benefits of exercise, just like of medications, are only realized with regular use.
Abbreviations
- ABPM:
-
Ambulatory blood pressure monitor
- BP:
-
Blood pressure
- CKD:
-
Chronic kidney disease
- CRF:
-
Cardiorespiratory fitness
- CVD:
-
Cardiovascular disease
- DM2:
-
Type 2 diabetes mellitus
- ETT:
-
Exercise tolerance test
- HIIT:
-
High-intensity interval training
- hs-CRP:
-
High-sensitivity C-reactive protein
- HTN:
-
Hypertension
- LVH:
-
Left ventricular hypertrophy
- METs:
-
Metabolic equivalents
- OSA:
-
Obstructive sleep apnea
- PA:
-
Physical activity
- PWV:
-
Pulse wave velocity
References
Kagan A, Gordon T, Kannel WB, Dawber TR. Blood pressure and its relation to coronary heart disease in the Framingham study; hypertension volume VII. Drug action, epidemiology and hemodynamics. In: Proceedings of the Council for High Blood Pressure Research, American Heart Association. New York: American Heart Association; 1959. p. 53–81.
Principal Investigator, Freis E. Effects of treatment on morbidity and mortality in hypertension: II. Results in patients with diastolic blood pressure averaging 90 through 114 mmHg. JAMA. 1970;213:1143–51.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary. J Am Coll Cardiol. 2017;71:2199. https://doi.org/10.1016/j.jacc.2017.11.005.
Pimenta E, Calhoun DA. Resistant hypertension: incidence, prevalence and prognosis. Circulation. 2012;125(13):1594–6.
Daugherty SL, Powers JD, Magid DJ, Tavel HM, Masoudi FA, Margolis KL, O'Connor PJ, Selby JV, Ho PM. Incidence and prognosis of resistant hypertension in hypertensive patients. Circulation. 2012;125(13):1635–42. https://doi.org/10.1161/CIRCULATIONAHA.111.068064. Epub 2012 Feb 29.
Smith SM, Huo T, Gong Y, Handberg E, Gulati M, Merz CN, Pepine CJ, Cooper-DeHoff RM. Mortality risk associated with resistant hypertension among women: analysis from three prospective cohorts encompassing the Spectrum of Women's heart disease. J Womens Health (Larchmt). 2016;25(10):996–1003.
Sim JJ, Bhandari SK, Shi J, Reynolds K, Calhoun DA, Kalantar-Zadeh K, Jacobsen SJ. Comparative risk of renal, cardiovascular, and mortality outcomes in controlled, uncontrolled resistant, and non-resistant hypertension. Kidney Int. 2015;88(3):622–32.
Zhang J, Zhou S, Xua G. Carotid baroreceptor stimulation: a potential solution for resistant hypertension. Interv Neurol. 2014;2(3):118–22.
Bhatt DL, Kandzari DE, O'Neill WW, D'Agostino R, Flack JM, Katzen BT, Leon MB, Liu M, Mauri L, Negoita M, Sidney A, Cohen SA, Oparil S, Rocha-Singh K, Townsend RR, Bakris GL, for the SYMPLICITY HTN-3 investigators. A controlled trial of renal denervation for resistant hypertension. N Engl J Med. 2014;370:1393–401.
Ben-Sira D, Oliveira JMF. Hypertension in aging: physical activity as primary prevention. Eur Rev Aging Phys Act. 2007;4:85–9.
Faselis C, Doumas M, Pittaras A, Narayan P, Myers J, Tsimploulis A, Kokkinos P. Exercise capacity and all-cause mortality in male veterans with hypertension aged ≥70 years. Hypertension. 2014;64:30–5.
Williams B. The aorta and resistant hypertension. JACC. 2009;53(5):452–4. https://doi.org/10.1016/j.jacc.2008.10.027.
Pimenta E, Gaddam KK, Oparil S. Mechanisms and treatment of resistant hypertension. J Clin Hypertens. 2008;10(3):239–44.
Meyer ML, Tanaka H, Palta P, et al. Correlates of segmental pulse wave velocity in older adults: the atherosclerosis risk in communities (ARIC) study. Am J Hypertens. 2016;29:114–22.
McDonnell BJ, Maki-Petaja KM, Munnery M, Yasmin Wilkinson IB, Cockcroft JR, McEniery CM. Habitual exercise and blood pressure: age dependency and underlying mechanisms. Am J Hypertens. 2013;26(3):334–41.
Kelley GA, Kelley KS. Progressive resistance exercise and resting blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2000;35:838–43.
Xin X, He J, Frontini MG, et al. Effects of alcohol reduction on blood pressure: a meta-analysis of randomized control trials. Hypertension. 2001;38:1112–7.
Hagberg JM, Park JJ, Brown MD. The role of exercise training in the treatment of hypertension: an update. Sports Med. 2000;30:193–206.
Hamdorf PA, Penhall RK. Walking with its training effects on the fitness and activity patterns of 79-91 year old females. Aust NZ J Med. 1999;29:22–8.
Brandão Rondon MU, Alves MJ, Braga AM, et al. Postexercise blood pressure reduction in elderly hypertensive patients. J Am Coll Cardiol. 2002;39:676–82.
Kelley GA, Kelley KS. Aerobic exercise and resting blood pressure in older adults: a meta-analysis review of randomized controlled trials. J Gerontol Ser A Biol Med Sci. 2001;56:M298–303.
Huang G, Thompson CJ, Osness WH. Influence of a 10-week controlled exercise program on resting blood pressure in sedentary older adults. J Appl Res. 2006;6:188–95.
Toth PP. Short-term aerobic exercise in the elderly promotes blood pressure reduction. J Appl Res. 2006;6:186–7.
Mancia G, Laurent S, Gabiti-Rosei E, et al. Reappraisal of European guidelines on hypertension management: a European society of hypertension task force document. J Hypertens. 2009;27:2121–58.
Kim J, Lee SK, Yoon DW, Shin C. Obstructive sleep apnoea is associated with progression of arterial stiffness independent of obesity in participants without hypertension: a KoGES prospective cohort study. Sci Rep. 2018;8(1):8152. https://doi.org/10.1038/s41598-018-26587-y.
Phillips BG, Narkiewicz K, Pesek CA, et al. Effects of obstructive sleep apnea on endothelin-1 and blood pressure. J Hypertens. 1999;17(1):61–6.
Khan A, Patel NK, O'Hearn DJ, Khan S. Resistant hypertension and obstructive sleep apnea. Int J Hypertens. 2013;2013:193010.
Elias MF, Crichton GE, Dearborn PJ, Robbins MA, Abhayaratna WP. Associations between type 2 diabetes mellitus and arterial stiffness: a prospective analysis based on the maine-syracuse study. Pulse (Basel). 2018;5(1–4):88–98. https://doi.org/10.1159/000479560.
Devereux RB, Roamn MJ, Paraniacas M, et al. Impact of diabetes on cardiac structure and function: the strong heart study. Circulation. 2000;101:2271–6.
Stewart KJ. Exercise training and the cardiovascular consequences of type 2 diabetes and hypertension: plausible mechanisms for improving cardiovascular health. JAMA. 2002;288(13):1622–31.
Hayashino Y, Jackson JL, Fukumori N, Nakamura F, Fukuhara S. Effects of supervised exercise on lipid profiles and blood pressure control in people with type 2 diabetes mellitus: a meta-analysis of randomized controlled trials. Diabetes Res Clin Pract. 2012;98(3):349–60. https://doi.org/10.1016/j.diabres.2012.10.004. Epub 2012 Oct 29.
Fernando GF, Cardosa CRL, Fiszman R, Muxfeldt S. Prognostic impact of baseline and serial changes in electrocardiographic left ventricular hypertrophy in resistant hypertension. Am Heart J. 2010;159(5):833–40.
Kokkinos PF, Narayan P, Colleran JA, Pittaras A, Notargiacomo A, Reda D, Papademetrious V. Effects of regular exercise on blood pressure and left ventricular hypertrophy in African American men with severe hypertension. N Engl J Med. 1995;333:1462–7.
Keane WF, Eknoyan G. Proteinuria, albuminuria, risk, assessment, detection, elimination (PARADE): a position paper of the National Kidney Foundation. Am J Kidney Dis. 1999;33:1004–10.
Barcellos FC, Del Vecchio FB, Reges A, Mielke G, Santos IS, Umpierre D, Bohlke M, Hallal PC. Exercise in patients with hypertension and chronic kidney disease: a randomized controlled trial. J Hum Hypertens. 2018;32:397. https://doi.org/10.1038/s41371-018-0055-0.
Leehey DJ, Moinuddin I, Bast JP, Qureshi S, Jelinek CS, Cooper C, Edwards LC, Smith BM, Collins EG. Aerobic exercise in obese diabetic patients with chronic kidney disease: a randomized and controlled pilot study. Cardiovasc Diabetol. 2009;8:62. https://doi.org/10.1186/1475-2840-8-62.
Fritze O, Romero B, Schleicher M, et al. Age-related changes in the elastic tissue of the human aorta. J Vasc Res. 2012;49:77–86.
Amento EP, Ehsani N, Palmer H, et al. Cytokines and growth factors positively and negatively regulate interstitial collagen gene expression in human vascular smooth muscle cells. Arterioscler Thromb. 1991;11:1223–30.
The CAFE Investigators, CAFE Steering Committee and Writing Committee, Williams B, Lacy PS, Thom SM, Cruickshank K, Stanton A, Collier D, Hughes AD, Thurston H, O’Rourke M, for the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT) Investigators. Differential impact of blood pressure–lowering drugs on central aortic pressure and clinical outcomes. Principal results of the conduit artery function evaluation (CAFE) study. Circulation. 2006;113:1213–25.
lachopoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol. 2010;55(13):1318–27.
O’Rourke MF, Safar ME, Adji A. Resistant hypertension and central aortic pressure. J Hypertens. 2014;32(3):699–701.
Ramosa JS, Dalleckb LC, Ramosc MV, Fabio Borranid F, Robertsa L, Gomersalla S, Beethama KS, Diasa KA, Keatinga SE, Fassetta RG, Sharmanf JF, Coombes JS. 12 min/week of high-intensity interval training reduces aortic reservoir pressure in individuals with metabolic syndrome: a randomized trial. J Hypertens. 2016;34:1977–87.
Dimeo F, Pagonas N, Seibert F, Arndt R, Zidek W, Westhoff TH. Aerobic exercise reduces blood pressure in resistant hypertension. Hypertension. 2012;60:653–8.
Guimaraes GV, de Barros Cruz LG, Fernandes-Silva MM, Dorea EL, Bocchi EA. Heated water-based exercise training reduces 24-hour ambulatory blood pressure levels in resistant hypertensive patients: a randomized controlled trial (HEx trial). Int J Cardiol. 2014;172(2):434–41. https://doi.org/10.1016/j.ijcard.2014.01.100. Epub 2014 Jan 24.
Rossi A, Dikareva A, Bacon SL, Daskalopoulou SS. The impact of physical activity on mortality in patients with high blood pressure: a systematic review. J Hypertens. 2012;30(7):1277–88.
Narayan P, Doumas M, Kumar A, Faselis CJ, Myers JN, Pittaras A, Kokkinos PF. Impact of cardiorespiratory fitness on mortality in black male veterans with resistant systemic hypertension. Am J Cardiol. 2017;120(9):1568–71. https://doi.org/10.1016/j.amjcard.2017.07.055. Epub 2017 Jul 31.
Myers J, Prakash M, Froelicher V, et al. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346:793–801.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Narayan, P., Kumar, A. (2019). Role of Physical Activity, Exercise, and Cardiorespiratory Fitness in the Management of Resistant Hypertension. In: Kokkinos, P., Narayan, P. (eds) Cardiorespiratory Fitness in Cardiometabolic Diseases. Springer, Cham. https://doi.org/10.1007/978-3-030-04816-7_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-04816-7_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-04815-0
Online ISBN: 978-3-030-04816-7
eBook Packages: MedicineMedicine (R0)