Abstract
The use of different drugs in clinical practice has enhanced the importance of pharmaco-EEG (P-EEG) studies in recent years.
The first part of this chapter will discuss the general and methodological aspects of P-EEG.
In the second part, EEG characteristics of individual drugs (antiepileptic and non-antiepileptic drugs) will be described.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Pharmaco-EEG
- Antiepileptic drugs
- Anxiolytics
- Antipsychotics
- Antidepressants
- Anesthetics
- Antibiotics
- Recreational drugs
1 Pharmaco-Electroencephalography: History, Methodology, and Basic Principles
Pharmaco-electroencephalography (P-EEG) is a non-invasive tool used to assess the effects of drugs on the central nervous system by processing the EEG signals, directly revealing the spontaneous synchronized postsynaptic neuronal activity of the cortex with high temporal resolution [1].
The basis of the P-EEG can be dated back to 1931, when Hans Berger first experienced the effects of subcutaneous cocaine on the alpha rhythm that he had just discovered. Over the last few years, in line with the technological evolution and the introduction of the quantitative analysis of EEG, P-EEG has become increasingly important, especially for its various applications in clinical and experimental fields.
Although it is well known that EEG activity is affected by many substances acting on the central nervous system, the interest in increasing this knowledge and the best methodology by which to assess it are relatively recent.
EEG can be considered a sensitive and reproducible biomarker in different conditions, such as in the early detection of cognitive impairment [2], localization of epileptogenic foci, physiopathologic characterization of sleep and sleep disorders, evaluation of the depth of anesthesia, etc. Similarly, EEG could be used as a biomarker of the effects of specific drugs on the CNS to classify psychotropic drugs, evaluate drug-to-drug interactions, and monitor the side effects and toxicity. Moreover, the use of quantitative methods for data processing and statistical data analysis provides a description of the direct and indirect effects of active compounds on brain functions, thus generating pharmacodynamics outcome measures which, together with pharmacokinetic data, may be used to study the pharmacodynamic-pharmacokinetic relationships [3]. Thus, EEG can be useful for all phases of clinical research on drug effects.
The study of P-EEG is complex, as it is affected by a high inter- and intraindividual variability and it should be adapted to the clinical and experimental needs for which it is required (comparison studies, case-control studies, evaluations on healthy patients, large-scale experimental studies vs. single patient evaluations, etc.).
In all cases, before the evaluation, a meticulous medical history is essential to detect all the possible variables that may affect the EEG activity. Physiological anamnesis is important to obtain information about developmental milestones, irregularities of the menstrual cycle, type of work, sleep-wake cycle, and usual behaviors during the day: for example, to evaluate the effect of a drug on arousal, it is important to know if the patient has slept sufficiently the night before the registration and, in general, how is his sleep-wake cycle. It’s necessary to ask the patient if he smokes cigarettes, drinks coffee, and/or makes use of ethanol or other psychotropic substances for therapeutic or recreational use, because of the well-known effects of these substances on the CNS.
With regard to the recording methods, many guidelines have been drafted over the years, trying to standardize data acquisition and processing techniques among EEG laboratories: the final purpose should be the identification of a shared and comparable analytical algorithm beyond interindividual and interlaboratory differences and, if possible, the individuation of peculiar EEG features of specific drugs.
The latest guidelines from the International Pharmaco-EEG Society (IPEG) summarise the requirements for the recording and computerized evaluation of P-EEG data in humans.
A detailed description of the methods and techniques of acquisition, processing, and statistical analysis of the EEG signal is beyond the scope of this chapter and, therefore, we refer to the full text of the guidelines [3].
The recording should be performed in a quiet environment and the patient should be relaxed. A configuration of 21 electrodes according to the international 10–20 system is usually enough: however, it is possible to add further electrodes to study the activity of specific cortical areas and, eventually, to make a P-EEG brain map. Electrooculography is necessary, to identify and exclude ocular artifacts, while electrocardiogram monitors cardiac activity and indirectly highlights the patient’s state during the recording.
The recording must be performed with open and closed eyes for a sufficient time: guidelines recommend a vigilance-controlled EEG for 5 min followed by a resting EEG recording with closed eyes for 5–15 min. The variable duration of the latter depends on the purpose of the registration: sessions of 5 min (with a minimum of 2-min artifact-free signal) are sufficient to quantify EEG activity and to demonstrate pharmacological effects on spectral parameters, while longer recordings are necessary to evaluate the effects of drugs on vigilance and wakefulness (or sleepiness) [3,4,5].
Data processing provides the representation in time and frequency domain, the latter indispensable for spectral analysis, to evaluate EEG band power (absolute and relative), Peak Power Frequency (PPF), Main Dominant Frequency (MDF), Spectral Edge Frequency (SEF), and Median Frequency (MF). Time domain EEG parameters are useful to evaluate the effect of specific anesthetic drugs on brain activity: among them, Burst Suppression Ratio (BSR) is used as an indirect index of the level of anesthesia.
A reliable assessment of the EEG effects of a drug cannot forget considering the status of the basal EEG, necessary to make comparisons between basal and drug-induced activity. Thus, more recordings at specific time points should be performed.
Although different substances may be responsible for the same EEG pattern and despite the large interindividual variability, some EEG features may be considered characteristic and sometimes peculiar of specific drugs.
2 Effects of Drugs on EEG
2.1 Antiepileptic Drugs (AEDs)
AEDs can induce EEG changes, sometimes not detectable by the simple qualitative analysis and whose evaluation is often far from easy. This is due to several reasons: the principal is that epilepsy is a chronic disease which involves the rearrangement of brain networks in addition to the epileptic focus, and this influences the EEG activity. Moreover, epilepsy is a dynamic pathology and it may involve changes in EEG over time, regardless of the patient’s treatment. Persons with epilepsy often take more than one antiepileptic drug, and their EEG tracings may be modified by several substances. To avoid these confounding factors, many studies on antiepileptic drugs EEG changes has been conducted in healthy volunteers. However, even in this case, there are some limitations, above all the time-limited therapy and the low dosages. Therefore, it is clear that EEG modifications induced by AEDs are still not totally defined and sometimes controversial [6, 7].
On the basis of literature data, the modifications induced by AED will be briefly described, subdividing them into two topics: the effects on the background activity and the effects on the ictal and interictal epileptiform activity.
2.1.1 Effects of AEDs on Background Activity
The main old-generation AEDs are barbiturates (PB), diphenylhydantoin (DPH), carbamazepine (CBZ), valproic acid (VPA), and benzodiazepines (BDZs).
PB was the first AED on the market, since 1912. It is still a widely used drug, both in mono- and in polytherapy, for the treatment of focal and/or generalized epilepsies. At low dosages, PB typically induces an increase in rapid EEG rhythms (15–35 Hz), more evident in the anterior regions than in lesional areas. At higher dosages, a progressive slowing of the alpha rhythm and a corresponding increase in theta-delta activity can be observed. Acute administration of high dosages of barbiturates can induce a pattern of burst suppression, which may result in a pattern of cortical suppression (Fig. 45.1).
Among the older-generation AEDs, DPH induces mainly a slowing of alpha rhythm and an increase in slow theta-delta activity, even at therapeutic dosages and in the absence of clinical signs of toxicity. In case of overdose, a paroxysmal, hypersynchronous delta activity may occur.
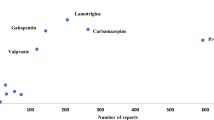
It was reported that CBZ may cause slowing of background EEG. The correlation between the entity of slowing and the serum concentration of CBZ is controversial: some studies found significant correlations between the percentage of delta, theta and alpha 2 power bands and serum levels of CBZ [8]. In particular, with the increase of serum concentration of CBZ, the percentage of power progressively increased in the theta band, while it decreased in the alpha 2 band (Fig. 45.2). The percentage of theta and alpha 2 power was found to reach maximum and minimum levels, respectively, when the peak values of serum concentration of CBZ were attained [9]. Therefore, it can be affirmed that CBZ induces a slowing of the background activity through a mechanism not fully clarified, but similar to that of some tricyclic antidepressants (TCA) with which CBZ shares the biochemical structure (Fig. 45.3).
EEG recorded in a 42-year-old female patient after a single dose of 2400 mg of carbamazepine. The patient was poorly reactive to external stimuli and the EEG showed a global slowing of the background activity with sequences of monomorphic and rhythmic delta potentials, prevalent in the medium-anterior areas
At therapeutic dosages, VPA does not determine qualitative EEG modifications. However, the quantitative EEG analysis also showed a slight slowing of the alpha rhythm and an equally slight increase in both theta and beta bands. It has also been demonstrated that VPA causes a decrease in the synchronization of delta and theta bands in patients with generalized epilepsy. Toxic dosages of VPA produce diffuse delta activity, which in the case of VPA encephalopathy become hypersynchronous and paroxysmal, with superimposed spikes and bi-triphasic waves. Burst suppression pattern, secondary to VPA-induced hyperammonemic encephalopathy, is also described [10]. Furthermore, studies of topographic analysis in the frequency domain, conducted in patients with normal EEG treated in monotherapy with VPA, demonstrated that VPA (wich has multiple actions on sodium and calcium channel as well as on GABA turnover) decreased the low gamma range (30-40 Hz), while CBZ, a sodium-channel modulator, altered brain topography in the 50–60 Hz [11].
When used chronically at therapeutic dosages, BDZs (diazepam, lorazepam, nitrazepam, clonazepam, clobazam, etc.) induce the appearance of a characteristic fast activity of medium/low amplitude, generally bilateral and symmetric and more prominent in the anterior areas. Also in this case, the overdose of BDZ induces, in addition to the fast activity, a slow diffuse abnormalities (Fig. 45.4).
The newAEDs generation seems to have a better safety profile than the older ones, but an overlapping therapeutic efficacy. Those currently available are vigabatrin (VGB), felbamate (FBM), gabapentin (GBP), lamotrigine (LTG), tiagabine (TGB), topiramate (TPM), oxcarbazepine (OXC), levetiracetam (LEV), pregabalin (PGB), zonisamide (ZNS), lacosamide (LCM), eslicarbazepine acetate (ESL), and perampanel (PER). Nevertheless, of the aforementioned drugs, some are currently underused for relevant adverse events (VGB, FBM), or for low antiepileptic efficacy (PGB, GBP, TGB).
Among the new AEDs, OXC (a member of dibenzazepine family as CBZ) induces a slowing of alpha rhythm and an increase in the power of the slow bands, but less than CBZ; an increase of delta and theta activities and a slight slowdown of alpha rhythm is also caused by TPM and GBP [12].
LTG is a phenyltriazine derivative which acts through inhibition of voltage-activated sodium channels and possibly calcium channels, preventing the release of glutamate [13]. It seems to have an EEG activating effect: in persons with epilepsy, it increases the fast frequencies (alpha and beta), decreases the slow frequencies (theta-delta), and also increases the reactivity of the alpha rhythm and the power of the beta band during the performance of attention tests. It has also recently been shown that LTG induces a reduction in thalamocortical synchronization functions in patients with generalized epilepsy, thus reducing the absolute power of the slow bands [14, 15]. However, topographic analysis in the frequency domain has demonstrated that LTG, as CBZ, induces significant power decrease in gamma band at 50-60 Hz (11).
LEV binds synaptic vesicle protein 2A, inhibits calcium release from intraneuronal stores and, thus, excessive synchronized neuronal activity [16]. It does not seem to induce any modification of the background EEG activity; however, the appearance of a burst suppression pattern, in a patient with a postanoxic coma, has been described in a case of LEV overdose [17].
ESL and LCM bind voltage-dependent sodium channels at an inactive state and prolong it reducing the channel firing, while PER is a selective noncompetitive AMPA receptor antagonist. Currently, there are no available literature data about their effect on the background EEG activity: according to our clinical experience, ESL does not seem to induce any changes.
In conclusion, the low or absent impact on background activity of new AEDs could reflect their better tolerability than old AEDs, with scarce repercussions on cognitive profile.
2.1.2 Effects of AEDs on Ictal and Interictal Epileptiform Activity
BDZs usually have a drastic and positive effect on ictal epileptic activity, especially if it is generalized, and for this reason they represent the first-line treatment of the status epilepticus. Their action on interictal activity is less relevant, especially if it is focal (Fig. 45.5a–c).
(a) Generalized nonconvulsive status epilepticus recorded in a 64-year-old male patient; (b, c) 5 and 10 min after i.v. bolus of lorazepam 4 mg administration, the epileptiform activity was almost completely replaced by a diffuse, low-amplitude, fast activity although isolated sharp waves complexes persist followed by bursts of sleep spindles at 14 Hz
Chronic treatment with barbiturates (PB) has a good effect on both ictal and interictal activity, and acute treatment is used for the management of status epilepticus (second-line therapy).
DPH generally has a positive effect on epileptic activity, both in acute (it is considered a second-line drug for the treatment of status epilepticus) and in chronic administration, while the effects on interictal activity are more controversial. However, rare cases in which high-dose DPH has increased ictal activity, also evolving to status epilepticus, have been described.
VPA, at therapeutic dosages, has an excellent effect on the generalized ictal and interictal activity and it is currently also used for acute administration in the status epilepticus as second-line therapy. The SANAD (Standard and New Antiepileptic Drugs) study reported that valproate was the most effective and best-tolerated first-line AED for patients with Idiopatic Generalized Epilepsy (IGE), including juvenile myoclonic epilepsy (JME), when it was compared to LTG and TPM [18].
The efficacy of LEV in both focal and generalized ictal discharges has been demonstrated. In particular, it has been reported that LEV reduces the photoparoxysmal response and controls the generalized discharges in juvenile myoclonic epilepsy, so that it may be considered a first choice drug in this rare type of epilepsy [19]. Moreover, our experience with LEV, conducted on a series of patients with generalized epilepsy and with very frequent epileptic discharges, showed a less homogeneous response, more evident when LEV is administered as an add-on therapy. LEV was often able to reduce the average duration of generalized discharges, but not to suppress them or significantly reduce their frequency: in some cases, paradoxically, the discharges have appeared even less prolonged, but more numerous in 24 h [20].
LTG is a generally well-tolerated drug with a broad spectrum of actions, and it is often preferred to VPA, especially in young women, for the treatment of IGE with generalized tonic-clonic and absence seizures. Nevertheless, some studies have reported aggravation of JME with LTG [21], while others have documented an amelioration of seizures in this type of epilepsy [22, 23]. A reduction of photoparoxysmal response was described for both focal and generalized ictal and interictal epileptic activity. In particular, LTG seems to allow a better localization of the epileptic focus by limiting its diffusion.
TPM is a widely used drug, especially for the treatment of IGE. Based on the current limited available data, TPM seems to be better tolerated than VPA, but there were no more benefits in terms of efficacy in TPM compared with VPA [24]. Mecarelli and colleagues performed a study on the clinical and EEG effects of TPM in patients with epilepsy and healthy volunteers. They observed that, in patients with epilepsy, the TPM induced EEG changes consisted of increased delta and theta activities and decreased activity in the fast bands. This recognizable TPM-induced EEG pattern was again evident in the healthy volunteers, in whom they also detected a significant reduction in the alpha rhythm. Their results confirm that TPM needs to be introduced gradually, while patients undergo close neuropsychological and neurophysiological monitoring to detect adverse sedative and cognitive effects. The EEG correlate of these events seems to be an increased activity in the slower frequency bands [25].
LCM is used for the treatment of focal onset seizures (both in mono as add-on therapy) and as second-line therapy for the treatment of status epilepticus [26,27,28]. Moreover, LCM treatment has shown effective anti-epileptogenic properties in the pilocarpine model of mesial temporal lobe epilepsy in rats: these effects were accompanied by decreases in interictal spike rates in the hippocampus [29].
ESL and PER are two new, well-tolerated, third-generation AEDs: their clinical efficacy on focal onset and generalized seizures are demonstrated, also for drug-resistant epilepsies, and this is reflected in a reduction of epileptic EEG discharges.
2.2 Anxiolytic Drugs
Anxiolytic drugs are essentially represented by BDZs (diazepam, clobazam, clonazepam, nitrazepam, lorazepam, etc.), whose effects on EEG have already been described in the section dedicated to the AEDs (some of these molecules are indeed used also in the treatment of epilepsy, especially in emergency). Typically, the chronic use of BDZs induces a more or less marked increase in the EEG fast frequencies, predominant in the anterior areas, associated with a slight decrease in the alpha activity and a mild increase in theta frequencies (higher in the case of BDZs with a more important hypnotic effect). Chronic assumption of BDZs for insomnia induce sleep changes consisting in an increase of total sleep duration and a decrease of sleep latency and night awakenings. However, from a macrostructural point of view, a reduction in the duration of the REM sleep and of the NREM stages 3 and 4 occurs. An increase in K complexes and spindles in NREM stage 2 has also been reported [30].
2.3 Antidepressants
Tricyclic antidepressants (TCAs) typically induce an increase of the beta frequencies, a slowing of the alpha activity and a dose-dependent increase in the diffuse theta-delta activities.
Furthermore, numerous studies have been carried out to validate the role of EEG as a biomarker for the response to antidepressant drugs in different psychiatric diseases: in bipolar disorder, for example, some studies suggest that the alpha wavelet power in occipital areas and the alpha asymmetry between anterior and posterior areas could be considered a reliable marker of treatment response [31, 32]. In major depression, other evidences reported no differences in occipital alpha power and in frontal alpha asymmetry. even though a gender and drug class interaction effect was found in frontal alpha asymmetry; right dominant frontal alpha asymmetry in women only was associated with a favorable response to escitalopram and sertraline [33]. Finally, EEG-derived biomarkers as changes in the activity of frequency bands and hemispheric alpha asymmetry, have all been shown to predict response to a various antidepressants [34].
Bupropion is an antidepressant well-known for its effects to lower seizure threshold, as demonstrated by several studies: it would cause the appearance of specific epileptiform graphoelements on EEG (sharp waves, spikes or focal slowings), more frequently in women [35]. Additionally, in contrast with other antidepressants that suppress the REM sleep, bupropion lengthens the REM latency and increases the total REM density [36].
With few exceptions, Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) decrease REM sleep and suppressed cortical spectral power in experimental models and in healthy and depressed patients. Studies on animal models have shown that duloxetine, as well as vortioxetine, increases vigilance (measured as time awake), yet their effects on brain rhythms were markedly different. Vortioxetine (at a dosage corresponding to 80% serotonin transporter occupancy) significantly increases theta, alpha and gamma power, whereas duloxetine (at the same level of serotonin transporter occupancy), has no effects on theta and gamma power, but decreass alpha power. Besides, the fact that vortioxetine elicited increase of hippocampal and pyramidal neuron firing and frontal cortical gamma oscillatory power in rats [37] indicates that the cellular framework for activating cortical neurons and eliciting gamma is engaged [38,39,40]. Duloxetine also seems to cause changes in left-frontal qEEG cordance after 1 week of treatment in a pilot sudy on fibromyalgia [41]. The stability of alpha power and asymmetry differences between responders and non-responders to SSRI, suggests that they represent a reasonable positive predictive factors to response to treatment [42].
The use of SSRIs or SNRIs seems generically to be associated with a low risk of epileptic seizure, however twofold in respect to nonusers. Current use of low-dosage TCAs seems not to be associated with seizures; moreover the risk of seizure would be higher at the beginning of the treatment than in longer-term treatment and among patients with major depression [43, 44].
2.4 Antipsychotics
Chronic administration of first-generation antipsychotic drugs (chlorpromazine, haloperidol, etc.) at therapeutic dosages induces typical EEG changes: slowdown of the alpha rhythm, increase of theta-delta activity, decrease of beta1 and increase of beta2 bands. Acute intoxication may induce a paroxysmal, widespread delta activity, up to EEG coma patterns.
These drugs could also lower the seizure threshold and, therefore, induce epileptic seizures (especially in already epileptic patients) and, in the most severe cases, also status epilepticus.
Haloperidol determines extremely unpredictable EEG activity, as reported by controversial literature data: while some studies have indicated an increase of alpha and beta power [45], others reported a decrease of alpha power [46].
Among atypical antipsychotics, clozapine was one of the most investigated: it has been demonstrated that chronic treatment with clozapine decreases relative alpha power and mean beta/total spectrum frequency and increases absolute delta/theta power [47]. Moreover, among antipsychotic drugs, clozapine seems to be the most responsible for seizures occurrence: Centorrino et al. further confirmed clozapine’s impact on brain electrical activity by conducting a large study on the EEG findings among 323 hospitalized psychiatric patients who were given various antipsychotic medications. The results showed EEG abnormalities, majorly consisting in theta and delta slowings, in 47.1% of clozapine-treated patients, in 38.5% of those treated with olanzapine, in 28% of the risperidone group, and in none of those under quetiapine treatment [48].
As regard to EEG changes induced by lithium carbonate, an increase of beta, theta and delta absolute power was reported [49, 50]. However, it is very interesting to note that in a study of 27 patients affected by bipolar disorder and treated with lithium carbonate, only those who didn’t respond to therapy had EEG abnormalities, thus suggesting that the presence of EEG abnormalities may be a biomarker of the lack of therapeutic response [42, 51].
2.5 Anesthetics
The Bispectral Index System (BIS) is one of the most widely used EEG parameters during anesthesia, providing information about its level. BIS monitoring uses a single sensor applied in the frontotemporal region, and the EEG signal is converted into a numerical value ranging from 0 (deeply unconscious patient with isoelectric wave) to 100 (awake patient). Originally, BIS monitoring was validated to monitor the depth of anesthesia in patients undergoing surgery (avoiding intraoperative awareness). Clinical studies are currently focusing on the use of BIS in the assessment of the state of consciousness during sedation schemes in patients admitted to ICU, to avoid oversedation [52, 53]. Nevertheless, qualitative EEG is however often required to assess the depth of anesthesia in intensive care units. Regardless of the indications for the EEG execution, the basic principle is the same: anesthetics induce oscillations that alter or disrupt the oscillations produced by the brain during normal information processing; these aesthesia-induced oscillations are readily visible in the electroencephalogram [54].
The effects of anesthetics on EEG depend on several factors: pharmacodynamic characteristics of the drug; molecular and neural circuit mechanisms of the anesthetic drug; dose administered and plasmatic concentration and metabolism.
The characteristic EEG patterns of some of the most commonly used anesthetics, in relation to their action on CNS, are described in this section.
2.5.1 Propofol
Propofol hyperpolarizes and inhibits postsynaptic neurons through its binding to postsynaptic GABAA receptors. Since the drug is highly liposoluble and the GABAergic inhibitory interneurons are widely distributed in the CNS (cortex, thalamus, brainstem and spinal cord), the action of propofol is carried out at multiple levels. In particular, propofol reduces excitatory inputs from the thalamus to the cerebral cortex by enhancing GABAergic inhibition on the reticular nuclei; it induces GABAergic inhibition of cortical pyramidal neurons; it inhibits arousal by acting on the reticular nuclei and on the inputs from brainstem to hypothalamic nuclei. These actions correspond to specific EEG patterns that, according to the depth of sedation and to the rate of drug administration (bolus vs. continuous infusion), are distinguished by: diffuse low-amplitude fast-activity, anteriorization of the background alpha rhythm, appearance of a widespread slow activity that progressively reduces in frequency and increases in amplitude (theta and delta), “burst suppression” pattern, and electrocortical inactivity (Fig 45.6). When propofol is administered as an induction bolus, patients, in particularly elderly patients, can show the burst suppression pattern immediatly [55].
In addition to its action on the brainstem circuits, propofol also induces unconsciousness through its effects on the thalamocortical and cortico-cortical circuits, which is likely to be expressed through topographic modifications of the alpha rhythm (anteriorization) and appearance of incoherent theta-delta activity.
The appearance of these two simultaneous patterns would suggest the lack of cortical reception of the inputs from the thalamic relay nuclei. As the effects of the propofol bolus recede, EEG evolves into slow-delta oscillation and alpha oscillation patterns. The transition time from slow oscillations or burst suppression into a combined slow oscillation and alpha oscillation patterns depends on how strong the effect of the propofol bolus had been. Even if no additional propofol is administered after the first bolus, it can take several minutes for the transition to occur [48, 56].
2.5.2 Dexmedetomidine
Dexmedetomidine alters the arousal mainly hyperpolarizing the α2-adrenergic presynaptic receptors (α2:α1 selectivity of 1600:1) of the locus coeruleus, thus reducing the release of norepinephrine. Hyperpolarization of the locus coeruleus results in the loss of inhibition on the hypothalamic preoptic area, leading to activation of the GABAergic inputs to the brainstem structures (ventral periaqueductal gray, dorsal raphe nuclei, locus coeruleus, lateral dorsal tegmental nucleus and the pedunculopontine tegmental nucleus). These actions lead to decreased arousal by inhibition of the arousal centers. The activation of hypothalamic inhibitory circuits would be involved in the early stages of NREM sleep. Sedation induced by dexmedetomidine is also enhanced by the reduction of presynaptic norepinephrine release that contributes to the loss of excitatory inputs from the locus coeruleus to the basal forebrain, the thalamus intralaminar nuclei, the cortex and then the thalamocortical connections. The EEG during sedation shows a delta pattern mixed with potentials similar to the spindles of NREM sleep (oscillations at 9–15 Hz that appear at intervals of 1–2 s). The progressive increase in sedation corresponds to the transition to a slower EEG (slow-delta) pattern, similar to that of the deeper phases of NREM sleep [57, 58] (Fig. 45.7).
Both propofol and dexmedetomidine act by inhibiting thalamocortical connections; however, propofol action, even at the same sedation levels, is more effective than dexmedetomidine on these circuits (Fig. 45.8).
Neurophysiological mechanisms of propofol (a) and dexmedetomidine and clonidine (b) actions in the brain. (a) Propofol enhances GABAergic transmission in the cortex and at the inhibitory projections from the POA to the arousal centers. (b) Dexmedetomidine-induced loss of consciousness through NE-mediated inhibition of the POA and decreased noradrenergic signaling in the thalamus and cortex. Clonidine-induced analgesia through enhanced inhibitory activity in the descending pain pathway. Abbreviations: 5HT serotonin, ACh acetylcholine, DA dopamine, DR dorsal raphe, DRG dorsal root ganglia, GABA gamma-aminobutyric acid, GABAA GABA receptor subtype A, AGal galanin, His histamine, ILN intralaminar nucleus of the thalamus, LC locus coeruleus, LDT laterodorsal tegmental area, LH lateral hypothalamus, NE norepinephrine, PAF peripheral afferent fiber, PN projection neuron, POA preoptic area, PPT pedunculopontine tegmental area, RVM rostral ventral medulla, TMN tuberomammillary nucleus, vPAG ventral periaqueductal gray. (Modified from Brown EN, Purdon PL, Van Dort CJ. General Anesthesia and Altered States of Arousal: A Systems Neuroscience Analysis. Annual Review of Neuroscience. 2011; 34:601–628, with permission)
2.5.3 Ketamine
Ketamine binds N-Metil-D-Aspartate (NMDA) receptors in the brain and in the spinal cord. At low-to-moderate dosages, ketamine blocks inputs to inhibitory interneurons and it allows downstream excitatory neurons to become disinhibited or more active: this clinically results in hallucinations. As the dosage of ketamine is increased, the NMDA receptors on the excitatory glutamatergic neurons are also blocked, with loss of consciousness.
Given the preference of ketamine for NMDA receptors on inhibitory interneurons, whose inhibition results in increased cerebral metabolic rate, cerebral blood flow and hallucinations, ketamine is associated with an active EEG pattern. When ketamine is administered alone in a low dosage, EEG shows fast oscillations in the high beta and a low gamma range, at between 25 and 32 Hz. Compared with propofol and dexmedetomidine, ketamine slow oscillations are less regular [54].
Summarizing, in the earlier stages of continuous anesthesia, we can observe a typical widespread - or prevalent in anterior areas - beta 1 or alpha EEG activity, defined as WAR (Widespread Anteriorly maximum Rhythmic pattern). The frequency of this anesthetic pattern tends to decrease in correlation with the depth of the anesthesia. In association with this pattern, we can often observe anterior - usually diphasic - slow waves, lasting about 1 s, isolated or in short sequences (Anteriorly maximum Intermittent Slow, AIS). Then, a slower activity, predominant in posterior and temporal areas and characterized by widespread delta potentials (Widespread Persistent Slow, WPS), can occur completely, replacing the WAR. When the rate of anesthetics is too high, the slow activity decreases in amplitude and it is progressively replaced by burst suppression pattern and, then, by electrocerebral inactivity.
2.6 Recreational Drugs and Toxic Substances
2.6.1 Cannabinoids
The principal psychoactive constituent in cannabinoids is D9-tetrahydrocannabinol (THC) [59, 60]. The CB1 receptor (CB1R) is one of the most abundant G-protein-coupled receptors in the central nervous system, with high densities in areas such as the cerebral cortex, basal ganglia, hippocampus, and cerebellum [61]. CB1Rs are primarily located presynaptically and their activation (by either endogenous or exogenous cannabinoids) inhibits the release of other neurotransmitters, such as gamma-aminobutyric acid (GABA) and glutamate, by decreasing Ca2+ influx via the inhibition of adenylate cyclase and N-type Ca2+ channels [62]. In the cerebral cortex and hippocampus, this neuromodulation principally occurs in networks of cholecystokinin-containing GABAergic interneurons [63]; thus, it appears that CB1Rs may function as a molecular “brake,” regulating the timing and release of GABA and other neurotransmitters [64]. In vitro and in vivo animal studies have shown that CB1Rs modulate gamma (30–80 Hz) and theta (4–7 Hz) bands synchronized oscillations in networks of GABAergic interneurons in the cerebral cortex and hippocampus [65]. The effects of CBD on EEG activity are different if we consider an acute or chronic use.
The occasional use of hashish and marijuana does not seem to induce visible EEG changes. Quantitative EEG studies have rather evidenced that the chronic use of marijuana reduces the power of the alpha and beta bands in the posterior areas. During abstinence, an increase of the power of alpha band in the frontal areas have been observed.
2.6.2 Psychostimulant Substances
In general, low dosages of psychostimulant substances increase the power of alpha and beta frequencies and decrease the amplitude and magnitude of the slow frequencies (delta and theta), causing an EEG desynchronization with clear prevalence of the fast components.
The effect of cocaine on EEG was first studied by Berger in 1931. After acute administration, cocaine determines an increase of the power of the beta band with decrease and desynchronization of alpha band. Quantitative EEG studies demonstrate that cocaine-addicted male subjects show substantially significat deficits of low-frequency activity and significant excess of alpha activity. Furthermore, cocaine can induce epileptiform abnormalities and epileptic seizures up to status epilepticus [66].
Morphine and heroin generally induce a dose-dependent slowing of the alpha rhythm and an increase both in the theta and the beta bands. Acute intoxication may lead to a coma state with the related EEG patterns [66].
2.6.3 Ethanol
EEGs of ethanol abusers are poorly synchronized, with reduction of the alpha and increase of fast frequencies. With regard to EEG modifications induced by ethanol abuse, it is extremely difficult to distinguish between those alcohol-related and those due to concomitant factors (cortical atrophy after a long period of intoxication, systemic diseases, concomitant use of other drugs, etc.). Quantitative EEG studies have demonstrated a decrease in the power of alpha, theta and delta bands (characteristic of chronic brain damage) and an increase in the power of beta band (due to cortical hyperexcitability state) (Fig. 45.9). During the abuse, but also after suspension (abstinence), interictal epileptic abnormalities can be observed, even with epileptic seizures and/or status epilepticus [66].
2.7 Antibiotics
Although the association between seizures and antibiotics has been known since long time, recent literature reviews suggest that this association can be actually considered low or very low (evidence Class III–IV). However, numerous reports underline an increased risk of provoked epileptic seizures, especially with unsubstituted penicillins, fourth-generation cephalosporins, imipenem, and ciprofloxacin, in combination with renal dysfunction, brain lesions and epilepsy. During administration of these antibiotics in patients with particular predispositions, close monitoring of serum levels is suggested [67].
The risk of seizures is mainly related to the concomitance of other medical conditions that may alter the clearance and/or the bioavailability of the drug. The drug’s ability to cross the blood-brain barrier (BBB) and/or damage to the BBB is another important risk factor for seizures.
2.7.1 Penicillins
The prevalence of seizures in patients receiving penicillin G or oxacillin is estimated to be 3.2 per 1000 patients [68]. Studies on animal models suggest that symptomatic seizures may derive from the interaction of penicillin with GABA, leading to a reduction of GABAergic inhibition allowing excitatory cortical afferents to trigger epileptiform bursts [69, 70].
However, the risk of epileptic seizures varies among the different molecules. As a matter of fact, the association between amoxicillin and clavulanic acid is not related to the risk of seizures, probably because of the inability to cross the blood-brain barrier and the poor ability to bind the GABAA receptor. Nevertheless, some case reports have described specific EEG abnormalities associated with amoxicillin (intermittent generalized short bursts of beta-frequency polyspikes alternated to frontal intermittent rhythmic delta activity (FIRDA) bursts during wakefulness) [71].
On the other hand, cases of nonconvulsive status epilepticus after piperacillin/tazobactam treatment have been reported [72].
2.7.2 Cephalosporins
The risk of seizures has been also reported for cephalosporins. All generations may cause seizures but cefepime and cefazoline are the most involved. Cephalosporins may induce encephalopathy with different EEG patterns characterized by several kinds of diffuse abnormalities—especially in fronto-central areas—from diffuse triphasic waves [73, 74] to continuous or intermittent bursts of generalized, high-voltage, 1 to 2 Hz sharp-wave or sharp and slow-wave activity [75]. The mechanism proposed of the cephaloporins-induced seizures is the dose-dependent inhibition of the GABAA receptors function [76].
2.7.3 Carbapenems
Carbapenems are able to penetrate the BBB, with effective treatment of CNS infections. This property, however, may promote seizure induction. Seizure induction could be caused by the structural similarity of the b-lactam ring with the GABA neurotransmitter, enabling carbapenems to interact at the GABAA receptor and act as a GABA antagonist [77]. Anecdotal cases of encephalopathy caused by imipenem are reported. EEG abnormalities described are diffuse slowing of background activity and intermittent multifocal or generalized epileptiform discharges (rhythmic spikes, polyspikes, sharp waves, spike wave, and sharp-and-slow wave complexes), accompanied by a diffuse low-voltage 10–25 Hz activity. In addition, a generalized photoparoxysmal response induced by intermittent photic stimulation at 20–25 Hz was observed [78].
2.7.4 Fluoroquinolones
Animal models suggest that fluoroquinolones inhibit GABAergic transmission by blocking the intracerebral GABAA receptors at a specific binding site [79]. Fluoroquinolone-associated neurotoxicity may manifest as seizures, delirium, or encephalopathy, and some cases of encephalopathy related to these drugs are reported. In a case report of a nonconvulsive status epilepticus due to levofloxacin, EEG revealed a continuous slow electrical activity with frequent generalized atypical spike-and-wave discharges prevalent in the anterior regions [80].
References
Jobert M, Wilson FJ. Advanced analysis of Pharmaco-EEG data in humans. Neuropsychobiology. 2015;72:165–77.
Babiloni C, Vecchio F, Lizio R, et al. Resting state cortical rhythms in mild cognitive impairment and Alzheimer’s disease: electroencephalographic evidence. J Alzheimers Dis. 2011;26(Suppl 3):201–14.
Jobert M, Wilson FJ, Ruigt GSF, et al. Guidelines for the recording and evaluation of Pharmaco-EEG data in man: the international Pharmaco-EEG society (IPEG). Neuropsychobiology. 2012;66:201–20.
Jobert M, Schulz H, Jahnig P. On the choice of recording duration in pharmaco-EEG studies. Neuropsychobiology. 1995;32:106–14.
Olbrich S, Mulert C, Karch S, et al. EEG vigilance and BOLD effect during simultaneous EEG/fMRI measurement. Neuroimage. 2009;45:319–32.
Salinsky MC, Oken BS, Morehead L. Intraindividual analysis of antiepileptic drug effects on EEG background rhythms. Electroencephalogr Clin Neurophysiol. 1994;90:186–93.
Salinsky MC, Oken BS, Storzbach D, Dodrill CB. Assessment of CNS effects of antiepileptic drugs by using quantitative EEG measures. Epilepsia. 2003;44:1042–50.
Marciani MG, Gigli GL, Stefanini F, et al. Effect of carbamazepine on EEG background activity and on interictal epileptiform abnormalities in focal epilepsy. Int J Neurosci. 1993;70:107–16.
Wu X, Xiao CH. Quantitative pharmaco-EEG of carbamazepine in volunteers and epileptics. Clin Electroencephalogr. 1996;27:40–5.
Cherian KA, Legatt AD. Burst suppression pattern on electroencephalogram secondary to Valproic acid-induced Hyperammonemic encephalopathy. Pediatr Neurol. 2017;73:88–91.
Arzy S, Allali G, Brunet D. Antiepileptic drugs modify power of high EEG frequencies and their neural generators. Eur J Neurol. 2010;17:1308–12.
Mecarelli O, Vicenzini E, Pulitano P, et al. Clinical, cognitive, and neurophysiologic correlates of short-term treatment with carbamazepine, oxcarbazepine, and levetiracetam in healthy volunteers. Ann Pharmacother. 2004;38:1816–22.
Nicholson A, Appleton RE, Chadwick DW, Smith DF. The relationship between treatment with valproate, lamotrigine, and topiramate and the prognosis of then idiopathic generalized epilepsies. J Neurol Neurosurg Psychiatry. 2004;75:75–9.
Clemens B, Ménes A, Piros P, et al. Quantitative EEG effects of carbamazepine, oxcarbazepine, valproate, lamotrigine, and possible clinical relevance of the findings. Epilepsy Res. 2006;70:190–9.
Clemens B, Piros P, Bessenyei M, Hollody K. Lamotrigine decreases EEG synchronization in a use-dependent manner in patients with idiopathic generalized epilepsy. Clin Neurophysiol. 2007;118:910–7.
Lyseng-Williamson KA. Levetiracetam: a review of its use in epilepsy. Drugs. 2011;71:489–514.
Bouchier B, Demarquay G, Guérin C, André-Obadia N, Gobert F. Marked EEG worsening following Levetiracetam overdose: how a pharmacological issue can confound coma prognosis. Clin Neurol Neurosurg. 2017;152:1–4.
Schomer DL. In: Lopes da Silva FH, editor. Niedermeyer’s electroencephalography: basic principles, clinical applications and related fields. New York: Oxford University Press; 2018.
Marson AG, Al-Kharusi AM, Alwaidh M, et al. The SANAD study of effectiveness of valproate, lamotrigine, or topiramate for generalized and unclassifiable epilepsy: an unblinded randomized controlled trial. Lancet. 2007;369:1016–26.
Specchio N, Boero G, Michelucci R, et al. Effects of levetiracetam on EEG abnormalities in juvenile myoclonic epilepsy. Epilepsia. 2008;49:663–9.
Pro S, Vicenzini E, Pulitano P, et al. Effects of levetiracetam on generalized discharges monitored with ambulatory EEG in epileptic patients. Seizure. 2009;18:133–8.
Biraben A, Allain H, Scarabin J, Schück S, Edan G. Exacerbation of juvenile myoclonic epilepsy with lamotrigine. Neurology. 2000;55:1758.
Morris G, Hammer A, Kustra R, Messenheimer J. Lamotrigine for patients with juvenile myoclonic epilepsy following prior treatment with valproate: results of an open-label study. Epilepsy Behav. 2004;5:509–21.
Machado RA, García VF, Astencio AG, Cuartas VB. Efficacy and tolerability of lamotrigine in juvenile myoclonic epilepsy in adults: a prospective, unblinded randomized controlled trial. Seizure. 2013;22:846–55.
Liu J, Wang LN, Wang YP. Topiramate monotherapy for juvenile myoclonic epilepsy. Cochrane Database Syst Rev. 2017;4:CD010008.
Mecarelli O, Piacenti A, Pulitano P, et al. Clinical and electroencephalographic effects of topiramate in patients with epilepsy and healthy volunteers. Clin Neuropharmacol. 2001;24:284–9.
Misra UK, Dubey D, Kalita J. Comparison of lacosamide versus sodium valproate in status epilepticus: a pilot study. Epilepsy Behav. 2017;76:110–3.
Zhu LN, Chen D, Xu D, Tan G, Wang HJ, Liu L. Newer antiepileptic drugs compared to levetiracetam as adjunctive treatments for uncontrolled focal epilepsy: an indirect comparison. Seizure. 2017;51:121–32.
d’Orsi G, Pascarella MG, Martino T, et al. Intravenous lacosamide in seizure emergencies: observations from a hospitalized in-patient adult population. Seizure. 2016;42:20–8.
Behr C, Lévesque M, Ragsdale D, Avoli M. Lacosamide modulates interictal spiking and high-frequency oscillations in a model of mesial temporal lobe epilepsy. Epilepsy Res. 2015;115:8–16.
Manconi M, Ferri R, Miano S, et al. Sleep architecture in insomniacs with severe benzodiazepine abuse. Clin Neurophysiol. 2017;128:875–81.
Jernajczyk W, Gosek P, Latka M, Kozlowska K, Święcicki Ł, West BJ. Alpha wavelet power as a biomarker of antidepressant treatment response in bipolar depression. Adv Exp Med Biol. 2017;968:79–94.
Bruder GE, Sedoruk JP, Stewart JW, McGrath PJ, Quitkin FM, Tenke CE. Electroencephalographic alpha measures predict therapeutic response to a selective serotonin reuptake inhibitor antidepressant: pre-and post-treatment findings. Biol Psychiatry. 2008;63:1171–7.
Arns M, Bruder G, Hegerl U, et al. EEG alpha asymmetry as a gender-specific predictor of outcome to acute treatment with different antidepressant medications in the randomized iSPOT-D study. Clin Neurophysiol. 2016;127:509–19.
Baskaran A, Milev R, McIntyre RS. The neurobiology of the EEG biomarker as a predictor of treatment response in depression. Neuropharmacology. 2012;63:507–13.
Macaluso M, Zackula R, D’Empaire I, Baker B, Liow K, Preskorn SH. Twenty percent of a representative sample of patients taking bupropion have abnormal, asymptomatic electroencephalographic findings. J Clin Psychopharmacol. 2010;30:312–7.
Ott GE, Rao U, Lin KM, Gertsik L, Poland RE. Effect of treatment with bupropion on EEG sleep: relationship to antidepressant response. Int J Neuropsychopharmacol. 2004;7:275–81.
Leiser SC, Pehrson AL, Robichaud PJ, Sanchez C. Multimodal antidepressant vortioxetine increases frontal cortical oscillations unlike escitalopram and duloxetine–a quantitative EEG study in rats. Br J Pharmacol. 2014;171:4255–72.
Pehrson AL, Leiser SC, Gulinello M. Treatment of cognitive dysfunction in major depressive disorder—a review of the preclinical evidence for efficacy of selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors and the multimodal-acting antidepressant vortioxetine. Eur J Pharmacol. 2015;753:19–31.
Dale E, Zhang H, Leiser SC, et al. Vortioxetine (Lu AA21004) disinhibits pyramidal cell output and enhances theta rhythms and long-term plasticity in the hippocampus. Eur Neuropsychopharmacol. 2013;23:S394.
Riga MS, Celada P, Sanchez C, Artigas F. Role of 5-HT3 receptors in the mechanism of action of the investigational antidepressant vortioxetine. Eur Neuropsychopharmacol. 2013;23:S393–4.
Hunter AM, Leuchter AF, Cook IA, et al. Brain functional changes and duloxetine treatment response in fibromyalgia: a pilot study. Pain Med. 2009;10:730–8.
Bruder GE, Sedoruk JP, Steward JW. EEG alpha measures predict therapeutic response to an SSRI antidepressant: pre and post treatment findings. Biol Psychiatry. 2008;63:1171–7.
Bloechliger M, Ceschi A, Rüegg S, et al. Risk of seizures associated with antidepressant use in patients with depressive disorder: follow-up study with a nested case–control analysis using the clinical practice research datalink. Drug Saf. 2016;39:307.
Wu C, Liu HY, Tsai HJ, Liu SK. Seizure risk associated with antidepressant treatment among patients with depressive disorders: a population-based case-crossover study. J Clin Psychiatry. 2017;78:e1226–32.
Liem-Moolenaar M, Gray FA, de Visser SJ, et al. Psychomotor and cognitive effects of a single oral dose of talnetant (SB223412) in healthy volunteers compared with placebo or haloperidol. J Psychopharmacol. 2010;24:73–82.
Yoshimura M, Koenig T, Irisawa S, et al. A pharmaco-EEG study on antipsychotic drugs in healthy volunteers. Psychopharmacology (Berl). 2007;191:995–1004.
Knott V, Labelle A, Jones B, Mahoney C. Quantitative EEG in schizophrenia and in response to acute and chronic clozapine treatment. Schizophr Res. 2001;50:41–53.
Centorrino F, Price BH, Tuttle M, et al. EEG abnormalities during treatment with typical and atypical antipsychotics. Am J Psychiatry. 2002;159:109–15.
Henninger GR. Lithium carbonate and brain function. Cerebral-evoked potentials, EEG and symptom changes during lithium carbonate treatment. Arch Gen Psychiatry. 1978;35:228–33.
Thau K, Rappelsberger P, Lovrek A, Petsche H, Simhandl C, Topitz A. Effect of lithium on the EEG of healthy males and females. A probability mapping study. Neuropsychobiology. 1989;20:158–63.
Aiyer R, Novakovic V, Barkin RL. A systematic review on the impact of psychotropic drugs on electroencephalogram waveforms in psychiatry. Postgrad Med. 2016;128:656–64.
Avidan MS, Zhang L, Burnside BA, et al. Anesthesia awareness and the bispectral index. N Engl J Med. 2008;358:1097–108.
Kelley SD. Monitoring consciousness: using the bispectral index. 2nd ed. Boulder: Covidien; 2010. p. 6.
Purdon PL, Sampson A, Pavone KJ, Brown EN. Clinical electroencephalography for anesthesiologists part I: background and basic signatures. Anesthesiology. 2015;123:937–60.
Besch G, Liu N, Samain E, et al. Occurrence of and risk factors for electroencephalogram burst suppression during propofol-remifentanil anaesthesia. Br J Anaesth. 2011;107:749–56.
Purdon PL, Pierce ET, Mukamel EA, et al. Electroencephalogram signatures of loss and recovery of consciousness from propofol. Proc Natl Acad Sci U S A. 2013;110:E1142–51.
Akeju O, Kim SE, Vazquez R, et al. Spatiotemporal dynamics of dexmedetomidine-induced electroencephalogram oscillations. PLoS One. 2016;11:e0163431.
Akeju O, Pavone KJ, Westover MB, et al. A comparison of propofol- and dexmedetomidine-induced electroencephalogram dynamics using spectral and coherence analysis. Anesthesiology. 2014;121:978–89.
Devane WA, Dysarz FA, Johnson MR, Melvin LS, Howlett AC. Determination and characterization of a cannabinoid receptor in rat brain. Mol Pharmacol. 1988;34:605–13.
Pertwee RG, Howlett AC, Abood ME, et al. International union of basic and clinical pharmacology. LXXIX. Cannabinoid receptors and their ligands: beyond CB and CB. Pharmacol Rev. 2010;62:588–631.
Glass M, Dragunow M, Faull RL. Cannabinoid receptors in the human brain: a detailed anatomical and quantitative autoradiographic study in the fetal, neonatal and adult human brain. Neuroscience. 1997;77:299–318.
Freund TF, Katona I, Piomelli D. Role of endogenous cannabinoids in synaptic signaling. Physiol Rev. 2003;83:1017–66.
Eggan SM, Melchitzky DS, Sesack SR, Fish KN, Lewis DA. Relationship of cannabinoid CB1 receptor and cholecystokinin immunoreactivity in monkey dorsolateral prefrontal cortex. Neuroscience. 2010;169:1651–61.
Farkas I, Kallo I, Deli L, et al. Retrograde endocannabinoid signaling reduces GABAergic synaptic transmission to gonadotropin-releasing hormone neurons. Endocrinology. 2010;151:5818–29.
Katona I, Sperlagh B, Magloczky Z, et al. GABAergic interneurons are the targets of cannabinoid actions in the human hippocampus. Neuroscience. 2000;100:797–804.
Ceballos NA, Bauer LO, Houston RJ. Recent EEG and ERP findings in substance abusers. Clin EEG Neurosci. 2009;40:122–8.
Sutter R, Ruegg S, Sutter ST. Seizures as adverse events of antibiotic drugs: a systematic review. Neurology. 2015;85:1332–41.
Boston Collaborative Drug Surveillance Program. Drug induced convulsions: report from the Boston Collaborative Drug Surveillance Program. Lancet. 1972;2:677–9.
Van Duijn H, Schwartzkroin PA, Prince DA. Action of penicillin on inhibitory processes in the cat’s cortex. Brain Res. 1973;53:470–6.
Wong RK, Prince DA. Dendritic mechanisms underlying penicillin-induced epileptiform activity. Science. 1979;204:1228–31.
Raposo J, Teotónio R, Bento C, Sales F. Amoxicillin, a potential epileptogenic drug. Epileptic Disord. 2016;18:454–7.
Fernández-Torre JL, Santos-Sánchez C, Pelayo AL. De novo generalised non-convulsive status epilepticus triggered by piperacillin/tazobactam. Seizure. 2010;19:529–30.
Pro S, Randi F, Pulitano P, Vicenzini E, Mecarelli O. Reversible encephalopathy induced by cefoperazone: a case report monitored with EEG. Neurol Sci. 2011;32:465–7.
De Silva DA, Pan AB, Lim SH. Cefepime-induced encephalopathy with triphasic waves in three Asian patients. Ann Acad Med Singapore. 2007;36:450–1.
Martínez-Rodríguez JE, Barriga FJ, Santamaria J, et al. Nonconvulsive status epilepticus associated with cephalosporins in patients with renal failure. Am J Med. 2001;111:115–9.
Sugimoto M, Uchida I, Mashimo T, et al. Evidence for the involvement of GABA(A) receptor blockade in convulsions induced by cephalosporins. Neuropharmacology. 2003;45:304–14.
Miller AD, Ball AM, Bookstaver PB, Dornblaser EK, Bennett CL. Epileptogenic potential of carbapenem agents: mechanism of action, seizure rates, and clinical considerations. Pharmacotherapy. 2011;31:408–23.
Fernández-Torre JL, Velasco M, Gutiérrez R, Fernández-Sampedro M. Encephalopathy secondary to imipenem therapy. Clin EEG Neurosci. 2004;35:100–3.
Green MA, Halliwell RF. Selective antagonism of the GABA(A) receptor by ciprofloxacin and biphenylacetic acid. Br J Pharmacol. 1997;122:584–90.
Mazzei D, Accardo J, Ferrari A, Primavera A. Levofloxacin neurotoxicity and non-convulsive status epilepticus (NCSE): a case report. Clin Neurol Neurosurg. 2012;114:1371–3.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Brienza, M., Pulitano, P., Mecarelli, O. (2019). Effects on EEG of Drugs and Toxic Substances. In: Mecarelli, O. (eds) Clinical Electroencephalography. Springer, Cham. https://doi.org/10.1007/978-3-030-04573-9_45
Download citation
DOI: https://doi.org/10.1007/978-3-030-04573-9_45
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-04572-2
Online ISBN: 978-3-030-04573-9
eBook Packages: MedicineMedicine (R0)