Abstract
Stroke is a leading cause of upper-limb impairment and a motivating factor behind the development of robotic technologies for arm assessment and rehabilitation. The shoulder is one of the most complex joints in the body and a potential source of human-exoskeleton misalignment. This paper presents histograms of shoulder displacement during 18 activities of daily living (ADLs) and demonstrates the shoulder joint translations that must be accommodated if misalignment is to be avoided during natural reach and grasp movements of the arm.
This work is supported by NSF Award#1532239 and the Eunice Kennedy Shiver NICHD of the NIH Award#K12HD073945. Content is the sole responsibility of the authors and does not necessarily represent the views of either NSF or NIH.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
- Shoulder Displacement
- Activities Of Daily Living (ADL)
- Robotic Exoskeleton
- Upper-limb Impairment
- Functional ADLs
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
The development of exoskeleton orthoses for functional assessment is an area of growing interest in the field of rehabilitation robotics. One of the motivating factors behind this growth is a steady increase in the number of individuals living with post-stroke mobility impairment [1]. Although the mortality rate of stroke has declined as hospitals improve early therapeutic strategies, the cost of care is increasing [2] driven by a growing and aging global population [3]. Further complicating the situation, growth in the patient population is outpacing that of therapeutic professions, putting increased strain on the medical system, and calling for more efficient methods of assessment and rehabilitation.
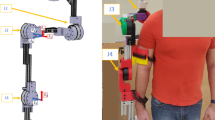
Exoskeletons offer a means for precise and quantifiable movement for both therapeutic and diagnostic use when properly sized and adjusted. In order to mitigate the risk of injury and of inaccuracy of measurement, it is important that the exoskeleton joints remain adequately aligned with the anatomical joints of the human wearer. In a healthy shoulder, articulation is achieved via combination of 4 joints: the glenohumeral (GH), acromioclavicular (AC), and sternoclavicular (SC) synovial joints, and a scapulothoracic (ST) ‘false’ joint formed by musculature between the scapula and thoracic cage (Fig. 1). Together the four joints of the shoulder provide the greatest mobility of any joint complex in the human body, and as a result present a significant design challenge in the development of anthropomorphic exoskeleton arms.
Shoulder mechanisms are often simplified to three intersecting revolute joints to form a stationary spherical joint [4]. This simplification has generally been assumed appropriate but can lead to misalignment and unnatural movement from the patient in specific regions of the workspace, depending on the combination and orientation of exoskeleton joints selected [5].
This paper presents data and analysis of shoulder kinematics recorded from 18 activities of daily living (ADLs). The data is plotted in histograms for the complete set, as well as for task subsets including eating and drinking, functional ADLs, reaching, and hygiene tasks. In the end, we posit that the results justify the assertion of the importance of including shoulder translation to enabling natural movement in exoskeleton devices.
2 Methods
2.1 ADL Data
The database of ADL motion captures used in this analysis was collected in a previous study [6]. Subjects preformed ADL tasks including, reaching, functional tasks, eating/drinking, and hygiene tasks. The kinematic motions for 24 ADL’s were captured for six subjects whose age ranged from 20 to 41 years. Further details regarding the testing setup and all recorded ADL actions can be found in the original publication [6]. During ADL recordings, a VICON motion capture system maps the locations of visual markers on a patient to an internal kinematic model and exports both Euler angle rotations for rigid bodies representing the arm, and Cartesian locations of the centers of rotation of the shoulder, elbow, and wrist. Only Cartesian position data is used in this analysis. To study shoulder motion, an ideal motion capture dataset would account for torso motion by using markers to track and subtract it from overall shoulder motion. Unfortunately, this was not the case with the available dataset, which was generated without this study in mind. To obtain a reference for the required ROM of Pandora’s Box, tasks which may have involved trunk motion and significant reaching were removed from consideration to focus on shoulder displacement only. The heights of subject’s and their resulting shoulder displacement distributions were compared for all actions. No significant variation was observed, indicating that height differences alone were not enough to cause an individual’s recordings to include more trunk motion.
2.2 Calculation of Shoulder Displacement and Plotting
The ADL data set provided shoulder positions in terms of Cartesian coordinates with respect to a global origin. For each ADL action, a shoulder origin was established as the mean position of the shoulder in the first 10 motion capture frames. The shoulder displacement for each frame is then the absolute difference of the shoulder’s recorded position and the shoulder origin. A Euclidean norm is used to calculate the magnitude of shoulder displacement for each frame, and displacement histograms are generated. Recordings began when an audible cue signaled subjects to initiate motion by moving their hand away from the designated rest position. This process introduces a bias toward arm configurations near the starting position due to delay between recording start time and subject motion. To limit this bias, a velocity trigger is applied. The trigger removes from consideration any data frames in which the moving average filtered velocity of the hand was recorded to be less than a threshold velocity. The threshold was set to 50 mm/s which was determined to be appropriate as it is well below the observed typical velocity of hand motion and above the noise level on the smoothed hand velocity signal.
3 Results
The magnitudes of shoulder displacement are used to generate a histogram showing the displacement of the shoulder for the full available ADL dataset (Fig. 2). The histogram utilizes PDF normalization, meaning the total area of the boxes sums to 100, and fifty bins which are each .5 cm wide over the 25-cm range.
Each ADL action subgroup was then separated to generate histograms which enable comparison of action subgroups (Fig. 3). Again, PDF normalization is used, and each histogram uses fifty bins .4 cm in width over the 20-cm range.
4 Conclusion
Proper exoskeleton kinematic alignment is required to achieve reasonably natural motion of a patient and is therefore essential to the effectiveness of post-stroke impairment evaluation devices. Distributions of shoulder displacement during ADL activities show that deviations of 10–15 cm from initial shoulder position occur regularly. Action subgroups show mostly consistent ranges with reaching actions having the widest distribution and hygiene actions showing an expected peak at 5 cm of displacement due to those tasks being concentrated on actions in which the hand was often near the subject’s head. From these results it can be seen that disallowing shoulder movement can influence a patient’s volitional movement and may impact the safety and/or effectiveness of therapy and assessment. Consequently, exoskeleton devices should implement this shoulder movement to improve alignment and allow natural motion for the patient.
References
Seshadri, S., et al.: The lifetime risk of stroke: estimates from the Framingham study. Stroke 37(2), 345–350 (2006)
Yacoub, H.A., Al-Qudah, Z.A., Khan, H.M.R., Farhad, K., Ji, A.B.-H., Souayah, N.: Trends in outcome and hospitalization cost among adult patients with acute ischemic stroke in the United States. J. Vasc. Interv. Neurol. 8(2), 19–23 (2015)
ONU: World population, ageing. Suggest. Cit. United Nations, Dep. Econ. Soc. Aff. Popul. Div. World Popul. Ageing, United Nat, no. ST/ESA/SER.A/390, p. 164 (2015)
Klopčar, N., Lenarčič, J.: Kinematic model for determination of human arm reachable workspace. Meccanica 40(2), 203–219 (2005)
Lo, H.S., Xie, S.Q.: Exoskeleton robots for upper-limb rehabilitation: state of the art and future prospects. Med. Eng. Phys. 34(3), 261–268 (2012)
Perry, J.C., Powell, J.M., Rosen, J.: Isotropy of an upper limb exoskeleton and the kinematics and dynamics of the human arm. Appl. Bion. Biomech. 6(2), 175–191 (2009)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this paper
Cite this paper
Bitikofer, C.K., Hill, P.W., Wolbrecht, E.T., Perry, J.C. (2019). Analysis of Shoulder Displacement During Activities of Daily Living and Implications on Design of Exoskeleton Robotics for Assessment. In: Masia, L., Micera, S., Akay, M., Pons, J. (eds) Converging Clinical and Engineering Research on Neurorehabilitation III. ICNR 2018. Biosystems & Biorobotics, vol 21. Springer, Cham. https://doi.org/10.1007/978-3-030-01845-0_96
Download citation
DOI: https://doi.org/10.1007/978-3-030-01845-0_96
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-01844-3
Online ISBN: 978-3-030-01845-0
eBook Packages: EngineeringEngineering (R0)