Abstract
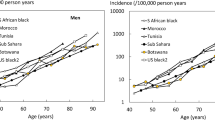
Fractures of the proximal part of the femur, hip fractures, are common and costly. The number of hip fractures has increased in all western countries during recent decades. This has occurred mainly because of an increase in the number of elderly people and also due to an increase in the risk for hip fracture among the oldest persons. Due to an increase in ageing population all over the world there will be a geographical shift in the occurrence of hip fractures. The incidence rates of hip fractures are higher in white populations than in others and vary by geographical region. Age adjusted incidence rates of hip fracture by gender are higher in Scandinavia than in North America and lower in countries of Southern Europe. The absolute number of hip fractures in each region is determined not only by ethnic composition, but also by the size of the population and its age distribution. In 1990 one third of all hip fractures in the world occurred in Asia despite lower incidence rates among Asians. Almost half of the fractures occurred in Europe, North America and Oceania. These populations are smaller but older. It was estimated in the beginning of the 1990s that 323 million people aged 65 years and over were living around the world. This has been estimated to increase to 1555 million by the year 2050.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
The Future Problem
Fractures of the proximal part of the femur, hip fractures, are common and costly. The number of hip fractures has increased in all western countries during recent decades. This has occurred mainly because of an increase in the number of elderly people and also due to an increase in the risk for hip fracture among the oldest persons [1–5]. Due to an increase in ageing population all over the world there will be a geographical shift in the occurrence of hip fractures. The incidence rates of hip fractures are higher in white populations than in others and vary by geographical region. Age adjusted incidence rates of hip fracture by gender are higher in Scandinavia than in North America and lower in countries of Southern Europe [6, 7]. The absolute number of hip fractures in each region is determined not only by ethnic composition, but also by the size of the population and its age distribution. In 1990 one third of all hip fractures in the world occurred in Asia despite lower incidence rates among Asians. Almost half of the fractures occurred in Europe, North America and Oceania. These populations are smaller but older. It was estimated in the beginning of the 1990s that 323 million people aged 65 years and over were living around the world. This has been estimated to increase to 1555 million by the year 2050 [8]. The increase will be especially high in Africa, Asia, South America and the Eastern Mediterranean regions. In USA demographic changes alone will more than double the number of hip fractures from 238,000 1986 to 512,000 in the year 2040 [8]. In another publication [9] the 340,000 hip fractures around year 2000 will increase to 650,000 in the year 2050. It has been calculated that the now close to two million hip fractures in the world could rise to over six million in the year 2050. Of these then 71 % is calculated to be in Africa, Asia, South America or the eastern Mediterranean region [10].
Already today hip fractures are highly resource consuming and strenuous for the organisation of medical care. Optimised methods for operation and rehabilitation along with preventive measures are necessary to cope with this increasing problem, otherwise it can become overwhelming.
Fracture Types
Hip fractures consist of different types in the proximal femur. It is very important whether the fracture is located in the femoral neck (cervical fracture, intracapsular) or through the parts of the proximal femur which constitute muscle insertions (trochanteric fractures, extracapsular) because both the treatment and the cause of healing are different [11]. Cervical fractures are best classified into undisplaced (Garden I and II) or displaced (Garden III and IV) [12]. Other sub-grouping has proven difficult to reproduce [13]. The trochanteric fractures are for routine use best classified into two-fragmented fractures (stable) or multi-fragment fractures (unstable). The baso-cervical fractures are a transition form between cervical and trochanteric fractures. They are usually treated as trochanteric fractures, but can in some cases have healing complications similar to the cervical ones. Sub-trochanteric fractures are more comminuted and include the area down to 5 cm below the trochanter minor.
The blood supply to the femoral head is often damaged after cervical fractures, because the vessels either penetrate within the marrow cavity or are positioned sub-periosteally on the femoral neck. Varying degree of vascular damage caused at the fracture moment will give varying amount of healing complications. The extracapsular trochanteric fractures have good vascular supply and few healing complications. Some of them are however very shattered with stability problems. Different systems for a more detailed classification of the fractures exist, but these are best suited for specialised research projects, as the reproducibility has been a major problem. In the Swedish national registration of hip fractures (RIKSHÖFT) Table 38.1 shows the fracture types registered based on 170,000 cases.
The diagnosis of a hip fracture is made by ordinary x-ray. On these pictures also the fracture type is classified. It also gives information about circumstances that can influence the choice of operation method, i.e. earlier performed operations. It can also disclose a pelvic fracture, which is a common differential diagnosis for pain from the hip area in elderly patients after a fall. All patients with pain from the hip after a fall, who have a normal, ordinary x-ray should be furthering diagnosed with MRI. It can usually disclose undisplaced hip fractures with risk of displacement and potential functional problems. It is also good for diagnosing undisplaced pelvic fractures, which are not uncommon in the pelvic rami in these age groups. If there is no access to MRI also a CT can disclose fractures, but not totally dismiss the suspicion. Scintigraphy performed after a couple of days can strengthen the fracture suspicion if positive with a localised high uptake. In lack of all these facilities mobilisation with weight bearing under supervision is a possibility with repeated x-ray check-ups, but it is a rather costly way of treatment as the patient usually has to be put into a hospital ward. MRI has proven particularly valuable for acute diagnosing of undisplaced fractures, which are not possible on ordinary x-ray. On the STIR-sequence an increased signal in the bone marrow is seen and on T1-weighted pictures the fracture oedema is seen as a dark line against a light background of trabecular bone marrow.
Already in the pre-operative course increased attention should be given to the pain relief of the patient, prevention of pressure sores and an early handling for rapid operation. The treatment should aim at operation as soon as possible, immediate mobilisation on the next day with full weight bearing as much as can be tolerated from pain, but no limitations in weight bearing due to fear of instability in the osteosynthesis. Only in certain very comminuted pertrochanteric or subtrochanteric fractures non-weight bearing should be recommended. In the other cases, particularly the femoral neck fractures, an early weight bearing is a test of the stability of the osteosynthesis and a failure can then be rapidly followed with a re-osteosynthesis or with a hip arthroplasty.
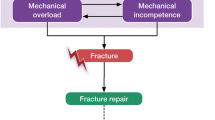
For the fracture types listed above the two major controversial areas are the displaced femoral neck fractures and the trochanteric multifragment fractures in combination with subtrochanteric fractures. The cervical displaced fractures are a combined biological and biomechanical problem due to the influence of the blood supply to the healing whereas the trochanteric/subtrochanteric fractures are predominantly a biomechanical stability problem due to the good vascularisation of the bone fragments. There are different philosophies for the treatment of these different fracture types, which will be further discussed below. It is possible to determine the circulation to the femoral head with high accuracy with the use of scintimetry, but this is resource consuming and also tends to delay the operation. MRI, probably with contrast, will possibly in the future become available, as a routine tool for the choice of operation method for femoral neck fractures, but these techniques are not yet developed.
Cervical Fractures
The blood supply to the femoral head after a cervical fracture has a decisive importance for the healing. The healing complications after a cervical fracture consist either of re-dislocation (early change of position) or pseudarthrosis (non-healing) or segmental collapse (femoral head necrosis after a healed fracture) [14–16]. A segmental collapse is thus re-building of the femoral head after vascular damage and needs a healed fracture for the vessels to grow in. At present there is no practical useful method to determine the blood circulation pre-operatively. The degree of dislocation of the fracture on an ordinary x-ray picture is not prognostically sufficiently accurate. Preoperative scintimetry is resource consuming, depending on the positioning of the leg and delays the operation. MRI is not yet developed for this purpose. The goal for the future and a very important area for research is to be able to prognosticate the healing complications already pre-operatively and based on that choose the primary method for operation. Patients with a good blood supply to the femoral head should then get a primary osteosynthesis and those with a clearly bad circulation instead a primary arthroplasty. In waiting for this diagnostic possibility the choice of operation method will be dependent on the grade of dislocation seen on the x-ray picture combined with the age of the patient, the patient’s other medical conditions and her functional level pre-fracture.
Undisplaced Cervical Fractures
These have little or no displacement of the fracture and usually very little risk for vascular damage to the femoral head and thereby little healing complications. This group of cervical fractures contains the Garden groups I and II [12]. Primary operation with osteosynthesis is advocated all over the world. The most used methods are either two or more parallel screws or two hook pins. The screws mostly differ by modifications of the configuration of the screwing in the top part [11, 17]. A few centres have tried not to operate some undisplaced fractures [18]. This leads to increased risks of dislocation and thereby a prognostic deterioration for the healing. Non-operative treatment also demands non-weight bearing and increased check-ups, both clinically and with radiography. It is a much safer method to operate the fracture and allow the patient full immediate weight bearing [19].
Displaced Cervical Fractures
These fractures have been the area of continuous disagreement for the last half century. Slowly more agreement is reached. There is a geographical difference internationally concerning the treatment principles for the displaced cervical fractures. In Scandinavia, particularly in Sweden and Norway, primary osteosynthesis has been performed in all cases with displaced cervical fractures. The basic philosophy has been to perform a small, quick and for the patient less burdening operation first and in the case of a healing complication later as a secondary procedure do a well-planned arthoplasty. This is usually then performed as a total hip arthroplasty where both the femoral and the acetabular parts are exchanged. It is an undisputed fact that the best long-term result after a femoral neck fracture is a healed fracture and preservation of the patient’s own femoral head provided no segmental collapse appears. This will give no future problems. An arthroplasty always has the risk of dislocation in the short time perspective and in the long run the risk of loosening and for the hemi-arthroplasties also by the years deterioration of the acetabular cartilage. When a patient has been operated with an osteosynthesis and 2 years has passed since the fracture and this is healed without complications, there is little risk of further problems from this hip [11, 20]. Some patients however never regain the full functional level that they had before the fracture. The complications after an arthroplasty increase after 5–10 years and this risk has to be balanced against the expected remaining lifetime for the patient [21]. Therefore arthroplasty is used mainly in elderly patients with clearly displaced fractures.
Internationally in many western countries the primary choice for a displaced femoral neck fracture is to perform an arthroplasty. This basic principle has been to treat all patients with arthroplasty to avoid healing complications in some. The treatment philosophy is now modified and an increasing amount of primary osteosyntheses is performed above all in relatively younger patients and those with less severe dislocation. Many studies have shown somewhat increased mortality after primary arthroplasty compared to primary osteosynthesis [11, 21, 22]. At the same time studies have shown a higher need of re-operation after the primary osteosynthesis within the first 2 years after the fracture compared to after a primary arthroplasty. The complications after a primary arthroplasty develop later and also a re-arthroplasty is a bigger operation and has more inherited complications than a secondary arthroplasty after a failed primary osteosynthesis [17].
The international literature shows that healing problems due to vascular damage of the femoral head by the displaced cervical fracture leads to non-union in 10–30 % of the cases and segmental collapse in further 10–20 % of cases. With an optimised osteosynthesis technique the healing complications (both non-union and segmental collapse) has been limited to in total 20–25 % for the displaced cervical fractures [20, 23].
Primary arthroplasty results in dislocation in around 4 % of the cases with hemi-arthroplasty and in 10 % with total hip arthroplasty. Infection consists of 2–5 %. Following a hemi-arthroplasty around 20 % of the cases in the long run develop wear and deterioration of the acetabular cartilage. Loosening is expected in around 10 % of the cases. Fracture in connection with the arthroplasty amount to 2–4 %. Re-operation with arthroplasty after a primary osteosynthesis has been reported to 20–30 % of the displaced cervical fractures. A major re-operation within the first years after a primary arthroplasty is expected to be needed in around 10 % of the cases. These are then rather complicated operations [11, 17, 21].
Unipolar hemiarthroplasty or a total hip replacement give better functional results within the first 2 years than a primary osteosynthesis. A total hip arthroplasty or a bipolar hemiarthroplasty probably gives better functional results after 2 years than a unipolar hemiarthroplasty. Cemented stem gives better outcome than uncemented. Uncemented cup is not recommended to these osteoporotic patients [11, 16].
Randomised studies have been performed both in Sweden and abroad to improve the criteria for the choice between a primary osteosynthesis and a primary arthroplasty [24–27]. Most of these studies have shown relatively high number of complications for osteosynthesis when compared with previously published consecutive series during the last decades [20, 23]. A differentiated treatment protocol results in fewer re-operations [15, 16, 28–30].
Based on the results of these randomised studies the treatment policy in Sweden has changed during the last decade so the most displaced fractures in elderly patients now in increasing amount receive a primary arthroplasty. A primary arthroplasty is advocated if the cervical fracture is clearly displaced with lack of continuity both on the frontal and the side view, particularly in patients with high degree of osteoporosis. Also the patient should have been walking prior to the fracture. The age should be above 70–75 years, where biological age is more important than chronological. Irrespective of the patient’s age the primary arthroplasty is recommended in cases with disease to the hip joint such as rheumatoid arthritis or a pathological fracture secondary to malignancy or other destruction of the hip joint; e.g. after infection. Also a lately diagnosed fracture is indicated for arthroplasty, particularly if the scintimetry has shown a low uptake. Arthrosis in the fractured hip joint is also an indication for primary arthroplasty. The primary arthroplasty is however not recommended in patients with severe dementia, bedridden patients or patients with bad muscular function due to the increased risk of dislocation.
The tendency internationally now aims at a differentiated treatment protocol according to the principles given above. In waiting for better diagnostic possibilities of the circulation to the femoral head, the principles indicated will probably result in that two thirds of the displaced cervical fractures will be operated with primary osteosynthesis and the other third with a primary arthroplasty, then preferably a bipolar with cemented stem.
Timing of Operation
Hip fracture patients should be operated as soon as practically possible. Directly life threatening conditions must of course have priority before the hip fractures, but these elderly patients will have a prolonged rehabilitation and functional less optimal result if the time between arrival to hospital and operation is unnecessarily delayed. This in turn leads to more complications and inactivity in these elderly persons. It can also generate increased nursing needs with great economic consequences. The goal is to operate the patient on the day of arrival and at latest within 24 h. If the patient is operated with osteosynthesis within 6 h from the fracture it has been shown that the risk for blood circulation disturbance to the femoral head and thereby following healing complications diminish [31].
Apart from being strenuous for the patient due to pain and immobilisation a delay of the operation is associated with increased morbidity and mortality. A delay of more than 24 h between arrival to hospital and osteosynthesis of the fracture has shown association to increased mortality. Lower mortality has been shown when the operation was performed within 12 h. If a delay is unavoidable the time should be used to improve the general condition of the patient, particularly the fluid balance [16, 17, 21].
Practical Considerations at Operation
Osteosynthesis for cervical fractures is performed with the use of a fracture table allowing traction under the image intensifier. Preferably a biplanar image intensifier is used. It is wise to supervise the transferring of the patient to the fracture table, as the injured leg has to be treated with great care to prevent fracture displacement occurring or damage to the retinacular vessels. A manual traction on the leg straightening it out during transfer is advisable. Also to reduce the risk of pressure sores padding should be applied to any area of pressure such as around the feet, sacrum and groin. The uninjured leg should be flexed and abducted as much as possible. Positioning of the image intensifier is easier if the hip and knee are flexed to 90° on the uninjured side (Fig. 38.1). A displaced cervical fracture is reduced by longitudinal traction followed by inward rotation. A biplanar image intensifier has the advantage that after positioning of the equipment no further movements of the stand or tube are necessary, which thereby avoids jeopardising the draping and thereby the sterility. The shifting between the views is done on the monitor with a foot pedal, which considerably saves operation time. Also the easy rapid shifting between the positions increases the precision in the positioning of the osteosynthesis material. The importance for the circulation to the femoral head of a low traumatic operating technique has been proven [32]. The channel should be pre-drilled and hammering in of osteosynthesis material avoided. Also impaction of the fracture by hammering increases the damage of the circulation to the femoral head. The best way to achieve compression in the fracture is by the patient’s own muscle forces at weight bearing. For undisplaced fractures early surgery will allow aspiration of any haematoma within the joint capsule. This may reduce the risk of avascular necrosis caused by ischaemia from a tamponade effect on the intracapsular vessels. Cervical fractures are operated with parallel pins or screws to allow axial compression along the axis of the femoral neck perpendicular to the fracture line when the patient is weight bearing. This is a physiological way of compressing the fracture. To prevent slipping out of the osteosynthesis material they are either threaded as screws or have a hook that can be pressed out through a central canal. To facilitate parallel positioning most devices are cannulated and have instruments to enable parallel placement. The most commonly used methods of fixation are two or three parallel cancellous screws, two parallel hook pins or a dynamic hip screw. The blood circulation to the femoral head via the capsule vessels along the femoral neck is vulnerable. Sudden forceful movements of the hip during reduction or excessive traction causing fracture diastasis may damage the femoral head circulation. The fracture is usually reduced by applying traction to the outstretched leg, followed by internal rotation. These manoeuvres should be checked throughout the procedure in both the lateral and the anterior-posterior radiograph using the image intensifier which should have a large field of view and a good resolution facility. The reduction manoeuvre is begun by using the fracture table to apply gentle traction to the leg, progressively while checking in the AP radiograph. Traction is applied until the medial parts of the femoral neck, the calcar region, are approximated with anatomical contact between the bone ends. Next, the lateral view is obtained and the foot is rotated inwards until the dorsal angulation of the femoral neck fracture has been counteracted. This part of the manoeuvre can be likened to closing an open book. The aim is to restore the alignment of the femoral neck such that a straight line can be drawn to bisect the femoral head, trochanteric region and shaft. It is essential that there is no residual fracture angulation, as this will increase the risk of re-displacement of the fracture. Quite frequently there is need to apply more than 90° of inward rotation to achieve reduction. Small corrections with ab-adduction and sometimes elevation of the leg may also be needed to obtain an anatomical reduction. Following the reduction maneuver it is advisable to slacken the traction somewhat. This allows some impaction to occur at the fracture site and reduces the risk of the femoral head rotating during drilling.
Open reduction is very seldom indicated. Only in very young patients it can be tried and then combined with insertion of a pedicle graft consisting of a piece of bone with a muscle bridge which is implanted into the fracture site. In all middle aged and older patients the alternative is rather a total hip arthroplasty if there is inability to obtain an adequate closed reduction. This is also advisable if the fracture is more than 1 week old or if there is early re-displacement following internal fixation.
Positioning of Two Hook Pins or Screws
Commonly used screws are the Garden screws, Asnis screws, Uppsala screws and AO screws. In Sweden and Norway the Hansson hook pins are widely spread. The screws and pins usually are about 7 mm in diameter and inserted parallel to each other. The aim is to create a three point fixation, where the first point is the entry hole for the firm lateral cortical bone, the second point is the pin lying on the calcar inferiorly or posteriorly within the medullary cavity of the neck and the third at the subcondral bone plate (Fig. 38.2). The lateral skin incision should be extended distally from a point about 2 cm distal to the greater trochanter for a length of about 5 cm. The exact positioning of the incision is best located using a guide wire or other radiopaque object on the skin surface and screening with an image intensifier in the AP view. After skin incision a guide wire is introduced. The inferior pin should be inserted through a drill hole at the level of the middle/lower part of the lesser trochanter. If the drill hole is situated distal to this point there is increased risk of fracture of the femur through the distal hole. The distal pin should rest along the calcar femorale and go up into the femoral head until 2–3 mm from the joint line (Fig. 38.3). While introducing the Kirschner wire the position is repeatedly checked with an image intensifier in the AP and lateral planes. On the lateral view the guide wire should appear within the centre of the femoral head and neck. The second, proximal guide wire is then placed in a position parallel to the first one. It should be as spread apart as possible from the lower one in the femoral neck. When three screws are used, for example of Asnis type [33], a triangular pattern is recommended for undisplaced or impacted intracapsular fractures. For displaced fractures four screws in a diamond pattern is suggested. This is said to give better rotatory stability. Impaction along the femoral neck combined with a minor rotation gives somewhat angulation of the osteosynthesis material, but still allows further impaction when two pins are used (Fig. 38.4).
Considerations at Arthroplasty
The hip fracture patient is usually a woman with osteoporosis and short statue. Extra care should be taken not to cause perforation of the acetabulum by reaming for a total hip arthroplasty or by causing a femoral shaft fracture. Smaller sizes of the arthroplasty are usually needed. Postoperative direct weight bearing should be allowed and postoperative restriction should be kept to a minimum. Capsulectomy should be avoided to prevent postoperative dislocation and a posteriolateral exposure is usually favoured due to limited tissue dissection needed, which give shorter operation times and less blood loss. The abductors are not damaged by this approach and there is a lower risk of femoral penetration. This exposure has been said to have a somewhat higher risk of dislocation and the sciatic nerve must be carefully watched to prevent damage. Anteriolateral approach is possible to have a lower risk of dislocation, but has the disadvantage of a greater tissue dissection and a more restricted access for positioning of straight long stem arthroplasties. If a hemiarthroplasty is to be used special care is necessary not to damage the acetabular cartilage. Forceful movements and hammering should be avoided and the femur is preferably prepared only by handheld reamers. Cementation of the femoral shaft gives better results than the uncemented classical Austin-Moore prosthesis. There is concern about less tolerance of these elderly patients to the cementation procedure so pulse and blood pressure should preferably be monitored and excessive pressure should be avoided even if modern cementing techniques are recommended. There is a risk of cardiac arythmia and low blood pressure during the insertion of the cement. To prevent this a venting catheter to allow air to escape from the femur during cementation and cortisone intravenously have been tried. There are no regular studies to approve this.
Depending on the patient’s biological age and activity level before the fracture different types of arthroplasty are chosen. Usually an ordinary one block hemiartroplasty is chosen for the oldest and most disabled patients, whereas a bipolar hemiarthroplasty is used for somewhat younger and fit patients and a total hip arthroplasty is given to the youngest and healthiest patients [16, 34].
Trochanteric Fractures
In trochanteric fractures the circulation to both bone ends is undamaged and healing complications are much less usual than for the cervical fractures. Instead osteoporosis increases the risk of fragmentation in trochanteric fractures. A minor part of the trochanteric fractures can be so comminuted that early direct weight bearing is hindered. The most widely spread operation method is a sliding screw plate (Fig. 38.5). It is a method that is fairly easy to teach on a large scale and has few complications. Modern metal techniques withstands metal fatigue unless in cases with longstanding pseudarthrosis where a metal plate fracture can occur, usually after 6–12 months. During the last decade short intramedullary devices have been introduced as alternatives to the screw plate (Fig. 38.4). The postulated advantages are shorter operation time, less bleeding due to other exposure and a biomechanically shorter lever arm for weight bearing on the osteosynthesis material. Randomised studies have not shown any superior results of these intramedullary devices compared to the ordinary extramedullary screw plate. In some cases a significantly increased risk of femoral shaft fracture has been shown. Inadequate reaming of the femur is normally the cause, in conjunction with excessive force when inserting the nail. An alternative reason may be that the lateral cortical bone around the lag screw is not load protected by a barrel, as with the screw plate. A fissure in this area may more readily extend. The main indications for intramedullary fixation are low trochanteric fractures, hip fractures with associated femoral shaft fracture and pathological extracapsular fractures.
There is also a modification of the side plate that allows sliding along the femoral shaft combined with that along the femoral neck to impact the fracture more anatomically [35]. The results on consecutive series seem promising with a lowered cut out of the screw in the femoral head (Fig. 38.6).
A basic biomechanical principle for good healing of trochanteric and subtrochanteric fractures is contact between the major weight bearing bone fragments. Rigid fixation systems counteract this and lead to pseudarthrosis and in the long run breakage of the plate due to metal fatigue. At reposition during operation and the following mobilisation and weight bearing good contact is aimed at in the major bone fragments, sometimes to the price of a certain shortening of the leg. The main goal is a rapid healing of the fracture. In some cases increasing pain and too much collapse of the fracture make non-weight bearing necessary. This is also the case if the screw through the femoral neck and head threatens to cut through the subcondral bone into the hip joint (Fig. 38.6). If the patient cannot support the weight bearing with some walking aid such as a walking table, rollator, quatra peds, sticks or crutches some weeks of sitting in a chair might be necessary. In the long run all trochanteric fractures heal, usually within 3–5 months. The development of femoral head necrosis is very rare, but there is some percentage of pseudarthrosis development which is higher if a more rigid fixation system has been used [16].
Dynamic extramedullary osteosynthesis (screw plate) is much better than rigid nail plates [36]. The Ender method, which was previously widely spread in Europe, has in several randomised studies shown inferior results compared to the screw plate [37]. The intramedullary type of osteosynthesis with a screw up through the femoral neck and a short intramedullary rod often with transverse screws through the femoral shaft (the first type was called Gamma nail) has in several randomised comparative studies shown the same risk cut out through the femoral head as the conventional screw plate whereas the intramedullary device has resulted in more re-operations, usually due to fracture at the distal end of the intramedullary nail. The technique is somewhat more demanding to perform [11]. It is however used as the only routine method in some centres in Europe. In the literature there are reports of a frequency of cut out of the femoral screw through the femoral head into the acetabulum with the use of a conventional screw plate in up to 10 % of the cases. This has been diminished to some percent only with the axial screw plate (Medoff plate). Reversed, oblique pertrochanteric fractures are especially suited for this type of osteosynthesis.
Subtrochanteric Fractures
The subtrochaneric fractures have a considerably higher frequency of healing complications compared to the trochanteric ones. This is due to the high mechanical forces acting in this area and that the fractures often are very comminuted which gives inferior stability to the osteosynthesis system. One problem with the conventional screw plate for subtrochanteric fractures is that a distal fracture line transfers the dynamic screw plate to become a more static implant as the fracture is situated below the area for the gliding screw. This leads to complications associated with the static fixations such as delayed healing, pseudarthrosis, breakage of the plate and cutting through of the femoral head by the screw [11, 17]. This has led to an increased use of long intramedullary nails with transverse fixation screws in the distal part and a screw through the femoral head and neck in the proximal part. With this device also very long and comminuted femoral shaft fractures can be handled [16].
Weightbearing and Rehabilitation
The goal after a hip fracture is to rehabilitate the patient to the same functional level as before the fracture [5, 16]. A stable osteosynthesis system or a well-fixed arthroplasty is a pre-requisite for this. The operation should allow direct postoperative weight bearing to start immediately the day after the operation (Fig. 38.7). This is possible for the majority of patients operated with osteosynthesis for femoral neck fractures as well as for those receiving an arthroplasty. The weight bearing by walking gives a physiological impaction of the fracture and stimulates the bone healing process. The rule is immediate postoperative weight bearing. Furthermore elderly patients usually find it difficult to have restricted weight bearing and cannot handle crutches as young patients.
As mentioned above for trochanteric fractures the majority can have full weight bearing whereas a small part of the fractures need more care due to very comminuted fractures. During recent decades successful rehabilitation programs have spread consisting of direct mobilisation in the hospital and continued walking rehabilitation in the patient’s own home [3, 28, 38–46].
Hip Fracture Audit
Due to the increasing burden on the health care system of the osteoporotic fractures in the elderly, particularly the hip fractures, it is very important to know the results of everyday treatment on a national basis of these fractures,. In Sweden, a national registration of hip fracture treatment called RIKSHÖFT was introduced in 1988 [16, 47]. This has spread internationally and in 1995 the Standardised Audit of Hip Fractures in Europe (SAHFE) was started based on the Swedish RIKSHÖFT experience [14].
The pattern of living before fracture and postoperatively up till 4 months after femoral neck (Fig. 38.8) or trochanteric fractures (Fig. 38.9) shows that of those patients coming from own home, the majority had returned there after 2–3 weeks of treatment at the orthopedic department. Actually, the mean hospitalisation time is now just below 10 days. The rest of the patients are rehabilitated through an institution. This is mainly due to other diseases existing before the fracture. Within a month from the fracture the majority of the patients from own home or service house have returned to their previous place of living. Already after 2 months a very stable pattern of rehabilitation is apparent from the graph and at 4 months after the fracture, the majority of the patients are back in their pre-fracture way of living.
Irrespective of the philosophy chosen for the treatment of hip fractures it is of utmost importance to be able to compare the results from the different treatment programs. Different countries have various traditions both socially and in medical treatment, but internationally comparisons will more rapidly bring out optimised ways of treatment that will be the solution to cope with the increasing amount of hip fractures during the coming decades (see www.rikshoft.se).
References
Jarnlo G-B, Jakobsson B, Ceder L, Thorngren K-G. Hip fracture incidence in Lund, Sweden, 1966-1986. Acta Orthop Scand. 1989;60:278–82. 1. Wallace WA. The increasing incidence of fractures of the proximal femur: an orthopaedic epidemic. Lancet. 1983;i:1413–4.
Zetterberg C, Elmersson S, Andersson GBJ. Epidemiology of hip fractures in Göteborg, Sweden 1940-1983. Clin Orthop Relat Res. 1984;191:278–82.
Jarnlo G-B, Ceder L, Thorngren K-G. Early rehabilitation at home of elderly patients with hip fractures and consumption of resources in primary care. Scand J Prim Health Care. 1984;2:105–12.
Obrant K, Bengnér U, Johnell O, Nilsson B, Sernbo I. Increasing age-adjusted risk of fragility fractures: a sign of increasing osteoporosis in successive generations? Editorial. Calcif Tissue Int. 1989;44:157–67.
Thorngren K-G. Fractures in older persons. Disabil Rehabil. 1994;16:119–26.
Melton III LJ. Differing patterns of osteoporosis across the world. In: Chesnut III CH, editor. New dimensions in osteoporosis in the 1990s. Hong Kong: Excerpta medica Asia; 1991. p. 13–8.
Johnell O, Gullberg B, Allander E, Kanis JA. The apparent incidence of hip fracture in Europé: a study of national register sources (MEDOS Study Group). Osteoporos Int. 1992;2:298–302.
WHO Study Group. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. WHO Technical Report Series No 843. 1994.
Brody JA. Prospects for an ageing population. Nature. 1985;315:463–6.
Cooper C, Campion G, Melton III J. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2:285–9.
Parker MJ, Pryor GA, Thorngren K-G. Handbook of hip fracture surgery. Oxford: Butterworth-Heinemann; 1997. p. 1–145.
Garden RS. Low-angle fixation in fractures of the femoral neck. J Bone Joint Surg. 1961;43-B:647–63.
Frandsen PA, Andersen E, Madsen F, Skjödt T. Garden’s classification of femoral neck fractures: an assessment of inter-observer variation. J Bone Joint Surg. 1988;70-B:588–90.
Parker MJ, Currie CT, Mountain JA, Thorngren K-G. Standardised audit of hip fracture in Europé (SAHFE). Hip Int. 1998;8:10–5.
Thorngren K-G. Hip fractures in the geriatric patient. Natural history, therapeutic approach and rehabilitation potential. In: Stein H, editor. Scientific proceedings SIROT 97. Freund Publishing House Ltd; 1999, 161–70.
Thorngren K-G. Fractures of the femoral neck and proximal femur. In: Bentley G, editor. European surgical orthopaedics and traumatology. Heidelberg: Springer; 2014. p. 2203–68.
Koval KJ, Zuckerman JD. Hip fractures. A practical guide to management. New York: Springer; 2000.
Raaymakers ELFB, Marti RK. Non-operative treatment of impacted femoral neck fractures: a prospective study of 170 cases. J Bone Joint Surg. 1991;73-B:950–4.
Cserhati P, Kazár G, Manninger J, Fekete K, Frenyó S. Nonoperative or operative treatment for displaced femoral neck fractures: a comparative study of 122 non-operative and 125 operatively treated cases. Injury. 1996;27(8):583–8.
Strömqvist B, Nilsson LT, Thorngren K-G. Femoral neck fracture fixation with hook-pins, 2-year results and learning curve in 626 prospective cases. Acta Orthop Scand. 1992;63(3):282–7.
Parker MJ, Pryor GA. Hip fracture management. Boston: Blackwell Scientific Publications; 1993. p. 1–292.
Rodrigues J, Herrara A, Canales V, Serrano S. Epidemiologic factors, mortality and morbidity after femoral neck fractures in the elderly – a comparative study: internal fixation vs hemiarthroplasty. Acta Orthop Belg. 1987;53:472–9.
Rehnberg L, Olerud C. Subchondral screw fixation for femoral neck fractures. J Bone Joint Surg. 1989;71-B:178–80.
Rödén M, Schön M, Fredin H. Primary treatment of displaced femoral neck fractures. Acta Orthop Scand. 1999;70(Suppl 287).
Tidermark J, Ponzer S, Törnkvist H, Svensson O, et al. Internal fixation vs. 1999.
Rogmark C, Johnell O, Sernbo I and the NOA Study Group. Nail or arthroplasty – a randomized study of displaced cervical hip fractures with 1-year results. Acta Orthop Scand. 1999;70(Suppl 287).
Neander G, Dalén N. Osteosynthesis versus total hip arthroplasty for displaced femoral neck fractures – results after 4 years of a prospective randomized study. Acta Orthop Scand. 1999;70(Suppl 287).
Holmberg S, Thorngren K-G. Consumption of hospital resources for femoral neck fracture. Acta Orthop Scand. 1988;59:377–81.
Thorngren K-G. Optimal treatment of hip fractures. Acta Orthop Scand. 1991;62 Suppl 241:31–4.
Alberts KA, Isacson J, Sandgren B. Femoral neck fractures – fewer secondary hip arthroplasty procedures with a differentiated treatment protocol. Acta Orthop Scand. 1999;70(Suppl 287).
Manninger J, Kazar G, Fekete G, et al. Avoidance of avascular necrosis of the femoral head, following fractures of the femoral neck, by early reduction and internal fixation. Injury. 1985;16:437–48.
Strömqvist B. Femoral head vitality after intracapsular hip fracture: 490 cases studied by intravital tetracycline labeling and Tc-MDP radionuclide imaging. Acta Orthop Scand. 1983;Suppl 200.
Asnis S, Wanek-Sgaglione L. Intracapsular fractures of femoral neck: results of cannulated screw fixation. J Bone Joint Surg. 1994;76A:1793–803.
Kyle RF, Cabanela NE, Russel TA, et al. Fractures of the proximal part of the femur. Instruction course lecture. J Bone Joint Surg Am. 1994;76:924–52.
Medoff RJ, Maes K. A new device for the fixation of unstable pertrochanteric fractures of the hip. J Bone Joint Surg. 1991;73-A:1192–9.
Chinoy MA, Parker MJ. Fixed nail plates versus sliding hip systems for the treatment of trochanteric femoral fractures: a meta analysis of 14 studies. Injury Int J Care Injured. 1999;30:157–63.
Parker MJ, Handoll HHG, Bhonsle S, Gilespie WJ. Ender nails compared with nail or screw plate devices for trochanteric femoral fractures: a meta-analysis of randomised trials. Hip Int. 1999;9(1):41–8.
Ceder L, Thorngren K-G, Wallden B. Prognostic indicators and early home rehabilitation in elderly patients with hip fractures. Clin Orthop. 1980;152:173–84.
Ceder L, Thorngren K-G. Rehabilitation after hip repair (letter). Lancet. 1982;2(8307):1097–8.
Borgquist L, Nordell E, Lindelöw G, Wingstrand H, Thorngren K-G. Outcomed after hip fracture in different health care districts. Rehabilitation of 837 consecutive patients in primary care 1986-88. Scand J Prim Health Care. 1991;9:244–51.
Borgqvist L, Lindelöw G, Thorngren K-G. Costs of hip fractures. Rehabilitation of 180 patients in primary health care. Acta Orthop Scand. 1991;62:39–48.
Holmberg S, Thorngren K-G. Rehabilitation after femoral neck fracture: 3053 patients followed for 6 years. Acta Orthop Scand. 1985;56:305–8.
Snedal J, Thorngren M, Ceder L, Thorngren K-G. Outcome patients with a nailed hip fracture requiring rehabilitation on hospital for chronic care. Scand J Rehabil Med. 1984;16:171–6.
Thorngren M, Nilsson LT, Thorngren K-G. Prognostic-based rehabilitation of hip fractures. Compr Gerontol. 1988;2:12–7.
Jalovaara P, Berglund-Rödén M, Wingstrand H, Thorngren K-G. Treatment of hip fracture in Finland and Sweden. Prospective comparison of 788 cases in three hospitals. Acta Orthop Scand. 1992;63:531–5.
Berglund-Rödén M, Swierstra BA, Wingstrand H, Thorngren K-G. Prospective comparison of hip fracture treatment, 856 cases followed for 4 months in the Netherlands and Sweden. Acta Orthop Scand. 1994;65:287–94.
Thorngren K-G. Experience from Sweden. In: Medical audit. Rationale and practicalities. Cambridge University Press; 1993. p. 365–75.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer-Verlag London
About this chapter
Cite this chapter
Thorngren, KG. (2016). Optimised Treatment of Hip Fractures. In: Poitout, D. (eds) Biomechanics and Biomaterials in Orthopedics. Springer, London. https://doi.org/10.1007/978-1-84882-664-9_38
Download citation
DOI: https://doi.org/10.1007/978-1-84882-664-9_38
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-84882-663-2
Online ISBN: 978-1-84882-664-9
eBook Packages: MedicineMedicine (R0)