Abstract
Over the last decade, there has been considerable effort to standardize the definition of acute kidney injury (AKI) in pediatric patients. This has led to a clearer understanding of the incidence of childhood AKI as well as which populations appear to be at highest risk for disease development. It is now well established that AKI is a common occurrence in hospitalized children, particularly those who are critically ill. In addition, there is emerging evidence that AKI is associated with poorer short-term and long-term outcomes. Currently, there are no directed therapies that hasten renal recovery in affected patients. Treatment is largely supportive with severe cases requiring initiation of renal replacement therapy.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Acute kidney injury (AKI)
- Pediatric RIFLE (pRIFLE)
- AKIN
- KDIGO
- Renal replacement therapy
- Pediatrics
- Childhood
- Chronic kidney disease (CKD)
1 Introduction
Acute kidney injury (AKI) is classically defined as an abrupt decrease in glomerular filtration rate (GFR), often associated with derangements in metabolic and volume balance.
Recent efforts to standardize AKI definitions have led to a more a robust understanding of populations at risk for AKI as well as the impact on those affected with respect to clinical outcomes. It is now well established that AKI is a common occurrence in hospitalized children, both in the intensive care unit and general inpatient setting. In addition, there is emerging evidence that AKI of any severity confers a higher risk of morbidity and mortality in the short-term as well as an increased likelihood of developing chronic kidney disease (CKD) over the long-term. This chapter provides an overview of the current understanding of pediatric AKI with respect to diagnosis, epidemiology, treatment, and outcomes.
2 Diagnosis of AKI: Definitions and Limitations
Multiple definitions and classification schema for AKI have been developed for use in adults (see Chap. 2), all of which have been studied for use in pediatrics. The RIFLE (risk, injury, failure, loss, end-stage kidney disease) criterion was developed by the Acute Dialysis Quality Initiative group in 2004 [1] in an attempt to standardize the definition of AKI by stratifying patients based on changes in serum creatinine and/or urine output. The pediatric RIFLE (pRIFLE) criteria were adapted from the RIFLE criteria in 2007 [2] and used changes in estimated glomerular filtration as calculated with the Schwartz formula rather than changes in serum creatinine to stratify severity. Subsequently, pRIFLE has been studied and validated primarily in critically ill children [2,3,4] and children who have undergone cardiac surgery [5, 6]. In general, pRIFLE has been shown to be a useful classification system for not only diagnosing AKI but also for providing prognostic information with respect to morbidity and mortality in those affected.
More recently, the Acute Kidney Injury Network (AKIN) modified the RIFLE criteria to include an absolute increase in serum creatinine concentration of ≥0.3 mg/dL from baseline. The AKIN criteria have not been modified specifically for use in children, though have been used in multiple pediatric studies, primarily in the ICU setting [7,8,9]. More recently, the KDIGO definition was published in 2012 and defines and stages AKI according to changes in serum creatinine and urine output [10]. There were no specific adjustments made for children. As it is the newest definition, there are fewer studies using it in children; however, there is a general movement toward adopting this definition, and the most recent, larger-scale studies have used the KDIGO definition. Currently, there is not one universally accepted AKI definition, making comparison of findings across studies challenging. It should be noted that all of the above AKI definitions include urine output criteria. However, due to the difficulty in obtaining accurate measurements of urine output, particularly in retrospective studies, these data are often not available. Thus, there is limited data regarding the etiology, outcomes, and impact of pediatric AKI as defined by urine output . Table 15.1 compares the definitions described.
Clinically, AKI is generally diagnosed following an increase in serum creatinine or a decrease in urine output. Unfortunately, these metrics have significant limitations and result in delayed recognition of AKI, especially in children. Changes in serum creatinine are not timely markers of kidney injury because a sudden drop in GFR to a constant low level is typically reflected by a gradual increase in serum creatinine until the patient reaches a new steady state [11]. In general, patients with more severe AKI take longer to reach a new steady state, which delays determination of the severity of injury [12]. The rate of rise is further altered by factors unrelated to renal function, such as volume of distribution, tubular secretion of creatinine, as well as creatinine generation. Thus, at the time a patient is noted to have AKI, the GFR may be much lower than that estimated using the serum creatinine. The inverse is true as AKI resolves and GFR recovers. The improvement in serum creatinine lags behind and as a result renal function may be underestimated during the phase of renal recovery.
In addition, there is day-to-day and site-to-site variability between serum creatinine levels which complicate interpretation of serum creatinine changes. This is especially problematic in children as there is more variation in patients with lower serum creatinine [13, 14].
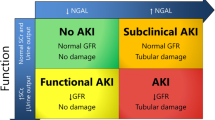
3 Novel Biomarkers for the Diagnosis of AKI
Over the last decade, there has been considerable effort dedicated to the discovery and characterization of novel biomarkers that may allow for increased sensitivity and specificity for the detection of AKI (see Chap. 3). A number of these biomarkers, including neutrophil gelatinase-associated lipocalin (NGAL), kidney injury molecule-1 (KIM-1), interleukin-18 (IL-18), and liver-type fatty acid binding protein (L-FABP), have been studied in the pediatric population. Some of the most important early studies characterizing these biomarkers in humans included pediatric patients at risk for AKI in the setting of cardiac corrective or palliative surgery. In many respects, this cohort represents an ideal population to study given the ability to recruit subjects prospectively and closely approximate the timing of AKI onset. Early studies suggested that some of these biomarkers had superior performance characteristics for the early detection of AKI. For example, Mishra et al. [15] reported that urinary NGAL levels in excess of 50 mc/L 2 h after cardiopulmonary bypass (CBP) were predictive of development of AKI, diagnosed by increased serum creatinine 24–72 h after CPB with a nearly perfect under the receiver-operating characteristic curve of 0.998 (sensitivity 1.00, specificity 0.98). Secondary analyses of a subset of samples from Mishra’s original study demonstrated that urinary IL-18 [16], KIM-1 [17], and L-FABP [18] were also early predictive biomarkers of AKI after CPB, though with less robust performance characteristics than NGAL. Numerous additional studies have further characterized candidate AKI biomarkers in a variety of pediatric populations including premature infants, newborns, critically ill older children, and those exposed to nephrotoxins.
Despite the work described above, serum creatinine remains the metric most widely used clinically to diagnose AKI. There remains optimism that further efforts toward biomarker discovery and validation will eventually enable earlier diagnosis of AKI, ultimately leading to improved outcomes. The inclusion of diverse pediatric populations in future research in this area will be critically important. It is quite likely that biomarker profiles in children with or at risk for AKI will vary depending on age and stage of development and will prove quite distinct from those in adults, particularly those with significant comorbidities (diabetes, hypertension, etc.).
4 Pediatric AKI Etiology and Risk Factors
A comparison of historical and more recent studies of AKI in children indicates a clear shift in AKI etiology over the last two to three decades. Data from the 1980s–1990s suggest that AKI was most commonly caused by primary renal disease, including hemolytic uremic syndrome (HUS) and glomerulonephritis , with secondary causes of renal disease, including sepsis and burns, which is less common [19, 20]. Over time, secondary causes of AKI have become increasingly more common. In a single-center study, Williams et al. [21] noted a sharp increase of oncologic diagnoses as a cause of AKI from 1978–1988 when compared to 1988–1998 (8% vs. 17%) with HUS simultaneously becoming less common (38% vs. 22%). Studies performed more recently clearly demonstrate that this trend has continued and that AKI in childhood is now most commonly caused by some other systemic illness (sepsis, cardiac disease, oncologic disease) and medically related therapies (ECMO, surgery, nephrotoxic medications) as opposed to primary kidney disease [2, 22,23,24]. It is likely that with improvements in critical care more children are surviving to develop AKI, explaining the evolution in terms of underlying etiology.
Today, it is clear that sicker children are at increased risk for AKI. Multiple studies have shown that illness severity (often as measured by the pediatric risk of mortality [PRISM] score) is associated with AKI [2, 25,26,27]. In burn patients, higher body surface area (BSA) was associated with increased AKI risk [25]. Other risk factors include sepsis [2, 25, 28], hematologic/malignant diagnoses [29], and cardiac surgery (with more complex cardiac surgeries being associated with increased risk) [30]. Not surprisingly, children receiving longer courses of aminoglycosides [29] and those receiving increasing number of nephrotoxic medications concomitantly [31] have an increased risk of AKI.
In adults, there are clear data that preexisting CKD increases risk for developing AKI; however, there are limited prospective studies in children, and retrospective studies have yielded conflicting results. That being said, given the reduced renal reserve present in those with CKD, it seems logical that those with CKD would be at a higher risk for AKI in the setting of intercurrent illness, nephrotoxic medication exposure, and/or surgical intervention.
5 Epidemiology of Pediatric AKI and Short-Term Outcomes
Determining the epidemiology of AKI in children is complicated by the different criteria used to define AKI as well as lack of available baseline serum creatinine values in many of the populations studied. The reported incidence of AKI varies by population and definition. The most studied pediatric patient population is those who are critically ill. There is increasing recognition that infants should be considered as a distinct population. Epidemiology of this population will be reviewed separately.
Wide ranges in the incidence of AKI (10–82%) have been reported in critically ill children using pRIFLE criteria [2, 4, 27]. Multiple studies have demonstrated that AKI as defined by pRIFLE criteria is associated with increased mortality (which generally increases with stage of AKI) and increased length of stay, even after adjusting for illness severity and other known risk factors [2,3,4, 25, 32]. These studies also generally report that there is increased need for renal replacement therapy (RRT) with increasing stages of AKI.
Using AKIN criteria , incidences are typically slightly lower than with pRIFLE, ranging from 33 to 65% in critically ill patients [32,33,34]. There is less data regarding the incidence of AKI in critically ill children using KDIGO criteria, but there are several large, good-quality studies. Selewski et al. found an incidence of 24.5% in a combined pediatric intensive care unit (PICU)/cardiac intensive care unit (CICU) cohort [26], and Sutherland et al. found an incidence of 42% in a PICU population [33]. For both KDIGO and AKIN definitions, AKI in PICU patients was associated with increased mortality and length of stay even in multivariate analysis. Increases in mortality are particularly impressive when using KDIGO criteria . Selewski [26] and Sutherland [33] reported an increased mortality in those with AKI when compared with those without AKI from 1.1% to 11.1% and 2.3% to 15.3%, respectively. There is only one large-scale prospective study of AKI in the pediatric ICU (PICU) population, which is the AWARE study that included 32 PICUs worldwide. Kaddourah et al. defined AKI using KDIGO criteria and found an overall incidence of 26.9% (15.3% stage 1, 6.3% stage 2, and 5.3% stage 3). Severe AKI (stage 2 or 3) was associated with increased risk of death (OR 2.41–5.14) after adjustment for illness severity score (PRISM-III, PIM-2, or PELOD depending on the center). Stage 1 was not associated with increased mortality, but any AKI was (OR ranging from 1.87 to 3.91 depending on illness severity score.) Patients with stage 1 AKI had longer ICU stays and longer mechanical ventilation than those with no AKI [35].
There is less data regarding the incidence and outcomes of AKI in the noncritically ill or general pediatric population. Logically, one would expect a lower incidence than in critically ill children; however, the incidence still appears to be significant. Patients receiving ≥72 h of aminoglycosides had an AKI incidence of 56% using pRIFLE and 45.2% using AKIN criteria [34]. A similar study of patients administered aminoglycosides reported incidences of 33% using pRIFLE and 20% using AKIN [29]. In a retrospective review of hospitalized children at higher risk for AKI (defined as having a baseline creatinine within 3 months before hospital admission), Sutherland and colleagues [33] reported an overall incidence of 51.1% using pRIFLE, 37.3% using AKIN, and 40.3% using KDIGO . Surprisingly, the incidence of AKI in the ICU and non-ICU population was similar across all definitions (pRIFLE, 51.3% vs. 51.0%; AKIN, 39.9% vs. 37.6%; KDIGO, 42% vs. 40.5%). There was no significant association between AKI and mortality in the non-ICU population; however, AKI was associated with longer lengths of stay across all definitions, and lengths of stay increased with AKI stage, except that patients with pRIFLE stage 3 was shorter than those with stage 2. An additional study which used ICD-9 diagnosis codes in a nationally representative sample of noncritically ill hospitalized children reported a much lower incidence of 0.39% [24]. This dramatic difference in reported incidence is likely related to the fact that many patients who meet criteria for AKI don’t receive an appropriate diagnosis. In one study of noncritically ill children receiving nephrotoxins, 58% more patients were classified as having AKI using pRIFLE criteria when compared to ICD-9 codes [36], suggesting that strict reliance on administrative data to identify cases of AKI in retrospective studies is unreliable.
6 Special Population: Neonates
There is emerging consensus that neonates should be considered separately from other children due to differences in renal physiology after birth and during the first few months of life as well as the potential for interruption of nephrogenesis in premature infants. Nephrogenesis begins at week 5 of gestation with a full complement of nephrons typically achieved reached by 34–36 weeks [37]. There are limited studies of kidneys of premature infants, but those that exist suggest that prematurity, IUGR, and AKI all result in decreased nephrogenesis and that former premature infants are at increased risk for CKD, proteinuria, and hypertension as they age. The normal GFR in term neonates at birth is 10–20 mL/min/1.73 m2 and increases to 30–40 mL/min/1.73 m2 by 2 weeks of life. The initial GFR is lower and improves more slowly in preterm infants [38]. In addition, immediately after birth, the infant’s serum creatinine reflects maternal creatinine. Thus, interpreting changes in creatinine can be challenging in the neonatal period, and this population may require different standards to diagnose AKI.
AKI appears to be quite common in neonatal intensive care unit (NICU) patients . Studies of very low and extremely low birth weight infants (defined as birth weight of <1500 g and < 1000 g, respectively) reported incidences between 12.5 (using an alternative definition of urine output <1 mL/kg/h for at least 24 h or serum creatinine >1.5 mg/dL) and 39.8% (using KIDGO definition) [39, 40]. Two studies of newborns undergoing therapeutic cooling for treatment of significant perinatal asphyxia reported incidences of 38% using KDIGO and 41.7% using AKIN [41, 42]. Extracorporeal membranous oxygenation (ECMO) is also associated with AKI as defined by RIFLE criteria with one study suggesting an incidence of 64% [43]. The incidence of AKI defined by AKIN is also high in newborns and infants requiring cardiac corrective or palliative surgery, with rates reported as high as 62% in those <28 days [44] and 52% in those <90 days [45]. Other reported risk factors include low birth weight, low gestational age, maternal and infant NSAID use, and sepsis as well as the presence of signs of perinatal stress including low APGARs, low cord pH, asystole, and intubation at birth [46,47,48,49,50]. As in older children, outcomes for infants with AKI appear to be worse after adjustment for confounders with studies showing increased mortality, hospital length of stay, and increased likelihood of abnormal brain MRI at 7–10 days of life [39, 42, 46, 49, 51, 52].
In 2012, Askenazi and Jetton [53] proposed a standardized classification system for neonatal AKI based on the KDIGO definition. The neonatal modified KDIGO criteria are described in Table 15.2. In 2013, a group of neonatologists and pediatric nephrologists reached consensus that this definition represented a reasonable starting point to provide standardization for future studies. Utilization of this definition moving forward will help facilitate comparison of findings across studies.
7 Management of Pediatric AKI
To date, there is no clear evidence that any intervention decreases the likelihood of children developing AKI or hastens recovery from it. As a result, treatment is generally supportive and involves removing or treating any known triggers of AKI and attempting to avoid added renal injury. Avoiding further nephrotoxin exposure and ensuring adequate renal perfusion are important to avoid further damage and to promote renal recovery. In addition, meticulous attention to fluid status with strict monitoring of intake and output and daily weights is helpful to prevent volume excess. Prompt reduction of fluid rates in children with oliguria/anuria is critical as even modest degrees of volume overload may contribute to respiratory or cardiac compromise due to smaller body size.
There is a growing body of evidence that volume excess contributes to poor outcomes in critically ill children who require renal replacement therapy (RRT). Multiple small, single-center studies of PICU patients undergoing continuous renal replacement therapy (CRRT) have shown that patients who do not survive AKI tend to have a higher percent fluid overload, but multivariate analysis including illness severity scores has generally showed borderline association [54,55,56]. Two larger studies reported more compelling results. A prospective study of 297 children undergoing CRRT at 13 centers showed an adjusted odds ratio (OR) mortality of 1.03 (1.01–1.05) for fluid overload, suggesting a 3% increase in mortality for each 1% fluid overload. When fluid overload was dichotomized into <20% and ≥20%, the adjusted OR was 8.5 [57]. This was corroborated by a retrospective single-center study of 190 children undergoing CRRT in which a multivariate analysis showed that percent fluid overload was associated with mortality. Hazard ratio for death was also increased, even when adjusted for timing of CRRT initiation and illness severity score [58]. Some of these studies also suggest that earlier initiation of CRRT may be associated with improved survival. Further research is needed to better understand optimal timing of CRRT initiation and what degree of fluid overload requires RRT initiation.
Once a patient is determined to have severe AKI, they may require RRT for solute clearance as well as fluid removal. Indications for initiation include fluid overload, electrolyte or acid-base derangements refractory to medical therapy, and symptomatic uremia. Patients may also require RRT for removal of nephrotoxins such as CT contrast, which can further exacerbate AKI. The treatment modality of choice depends on patient characteristics as well as center expertise. In patients who are more stable and are likely to tolerate more rapid fluid shifts, intermittent hemodialysis (IHD) is an option. This modality provides the most efficient clearance and is most amenable to running without anticoagulation. Traditionally, it is initiated in a stepwise fashion with progressively increased urea reduction on successive days to avoid dialysis disequilibrium syndrome. The length of treatment time depends on patient size, access, and clearance desired. When patients are acutely ill, HD treatments are generally provided daily.
If patients are less stable or are unlikely to tolerate more rapid fluid shifts, CRRT is often a better choice for RRT. Short-term clearance is lower with CRRT due to lower blood and dialysate flows, but over time, CRRT can be adjusted to provide comparable clearance to HD, and fluid removal can be continuously adjusted, which permits optimizing provision of nutrition and transfusions. CRRT can provide clearance through diffusion and/or convection, and modalities and protocols are institution dependent. Close attention to electrolyte balance is critical as pateints can develop hypokalemia and hypophosphatemia depending on dialysate solutions and replacement fluids. Also, medications need to be dosed appropriately for all forms of RRT, especially antibiotics and sedation.
Pediatric-specific considerations for both IHD and CRRT include catheter selection, blood flow rate, and treatment time, all of which are determined by patient size and clinical stability. In addition attention must be paid to the priming solution. Options include saline, albumin, or blood. In small patients, if the extracorporeal circuit volume is more than 10% of the patient’s estimated blood volume, the circuit should be primed with blood to prevent hemodilution leading to instability. In unstable patients who do not require priming with blood, priming with albumin may be of utility. In most other patients, saline can be used for priming. Generally, anticoagulation for RRT is provided with citrate or heparin. Other agents are available for those with complicating factors precluding the use of heparin. Occasionally, in patients with coagulopathies, CRRT can be provided without anticoagulation though circuit survival may be compromised in this setting.
Peritoneal dialysis (PD) is another option for RRT in AKI. It is often the modality of choice in infants due to the challenges of placing a large catheter for hemodialysis and challenges maintaining blood flows necessary for dialysis machines. In addition, infants typically require a blood prime for both HD and CRRT, which can result in sensitization, complicating future transplantation. PD eliminates this blood exposure, allows gradual fluid removal, and does not require anticoagulation. The challenges of PD include catheter leakage (which is more common when initiated in the acute setting) and lack of precise control over fluid removal and clearance. When PD is initiated acutely, lower dwell volumes are employed to avoid leaking around the catheter prior to healing. In this setting, solute clearance through PD is not as efficient as that achieved with HD or CRRT . PD is contraindicated in patients with recent abdominal surgery or infection and is relatively contraindicated in patients with VP shunts.
Given the described advantages and limitations of each modality, the modality of dialysis for those with AKI should be determined based on the above-noted factors, the local expertise and resources available, and the expected length of therapy required whenever possible.
8 Long-Term Outcomes
There is limited information about long-term outcomes of children after AKI, though emerging reports suggest significant chronic sequelae. Mammen et al. [59] showed an incidence of chronic kidney disease (CKD), defined as estimated GFR <60 mL/min/1.73 m2 and/or albuminuria, of 10.3% at 1–3-year follow-up. Another 46.8% were deemed at risk for CKD due to findings of more mild reductions in GFR (60–90 mL/min/1.72 m2), hypertension, and/or hyperfiltration. The study was small (n = 126), but there were no differences between those with CKD and those without in terms of underlying diagnoses, severity of illness scores, or nephrotoxin exposure. Patients with more severe AKI (AKIN stage 3) demonstrated an increased trend toward CKD development, though this did not reach statistical significance. There were significantly more patients who required dialysis that developed CKD. Askenazi [60] and colleagues reported 3–5-year outcomes of a cohort of children who developed AKI at a single center between 1998 and 2001. Of 174 patients who survived to hospital discharge, 32 subsequently died, and 16 developed end-stage renal disease. Of the 126 remaining survivors, 29 (23%) were recruited to participate in a study to assess renal injury. Of these children, 59% had at least one sign of chronic renal injury, including microalbuminuria (31%), hyperfiltration (31%), decreased GFR (14%), and hypertension (21%). Of concern, a pediatric nephrologist was involved in the care of only 35% of patients with evidence of chronic renal injury. These small, relatively short-term follow-up studies not only indicate that children with a history of AKI are at significantly increased risk for developing CKD over time but also suggest they are likely under-recognized and not being followed appropriately for such complications. Larger prospective studies are necessary to confirm these findings.
Conclusion
AKI is common in hospitalized children and associated with poorer outcomes, including increased mortality in ICU patients and increased length of stay in ICU and non-ICU patients. In addition, childhood survivors of childhood AKI are at high risk for complications including CKD, hypertension, and proteinuria. Future investigations should include established standardized definitions of pediatric AKI to further clarify at-risk populations and long-term outcomes. It will be important to study children from a variety of populations, as AKI susceptibility and recovery is very likely to be unique depending on age, developmental stage, as well as the presence of preexisting comorbidities.
References
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute Dialysis Quality Initiative w. Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8(4):R204–12. https://doi.org/10.1186/cc2872.
Akcan-Arikan A, Zappitelli M, Loftis LL, Washburn KK, Jefferson LS, Goldstein SL. Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int. 2007;71(10):1028–35. https://doi.org/10.1038/sj.ki.5002231.
Bresolin N, Bianchini AP, Haas CA. Pediatric acute kidney injury assessed by pRIFLE as a prognostic factor in the intensive care unit. Pediatr Nephrol. 2013;28(3):485–92. https://doi.org/10.1007/s00467–012–2357–8.
Schneider J, Khemani R, Grushkin C, Bart R. Serum creatinine as stratified in the RIFLE score for acute kidney injury is associated with mortality and length of stay for children in the pediatric intensive care unit. Crit Care Med. 2010;38(3):933–9. https://doi.org/10.1097/CCM.0b013e3181cd12e1.
dos Santos El Halal MG, Carvalho PR. Acute kidney injury according to pediatric RIFLE criteria is associated with negative outcomes after heart surgery in children. Pediatr Nephrol. 2013;28(8):1307–14. https://doi.org/10.1007/s00467–013–2495–7.
Ricci Z, Di Nardo M, Iacoella C, Netto R, Picca S, Cogo P. Pediatric RIFLE for acute kidney injury diagnosis and prognosis for children undergoing cardiac surgery: a single-center prospective observational study. Pediatr Cardiol. 2013;34(6):1404–8. https://doi.org/10.1007/s00246–013–0662-z.
Bagga A, Bakkaloglu A, Devarajan P, Mehta RL, Kellum JA, Shah SV, et al. Improving outcomes from acute kidney injury: report of an initiative. Pediatr Nephrol. 2007;22(10):1655–8. https://doi.org/10.1007/s00467–007–0565–4.
Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11(2):R31. https://doi.org/10.1186/cc5713.
Ozcakar ZB, Yalcinkaya F, Altas B, Ergun H, Kendirli T, Ates C, et al. Application of the new classification criteria of the Acute Kidney Injury Network: a pilot study in a pediatric population. Pediatr Nephrol. 2009;24(7):1379–84. https://doi.org/10.1007/s00467–009–1158–1.
Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120(4):c179–84. https://doi.org/10.1159/000339789.
Moran SM, Myers BD. Course of acute renal failure studied by a model of creatinine kinetics. Kidney Int. 1985;27(6):928–37.
Waikar SS, Bonventre JV. Creatinine kinetics and the definition of acute kidney injury. J Am Soc Nephrol. 2009;20(3):672–9. https://doi.org/10.1681/ASN.2008070669.
Carobene A, Ceriotti F, Infusino I, Frusciante E, Panteghini M. Evaluation of the impact of standardization process on the quality of serum creatinine determination in Italian laboratories. Clin Chim Acta. 2014;427:100–6. https://doi.org/10.1016/j.cca.2013.10.001.
Komenda P, Beaulieu M, Seccombe D, Levin A. Regional implementation of creatinine measurement standardization. J Am Soc Nephrol. 2008;19(1):164–9. https://doi.org/10.1681/ASN.2007020156.
Mishra J, Dent C, Tarabishi R, Mitsnefes MM, Ma Q, Kelly C, et al. Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker for acute renal injury after cardiac surgery. Lancet. 2005;365(9466):1231–8. https://doi.org/10.1016/S0140–6736(05)74811-X.
Parikh CR, Mishra J, Thiessen-Philbrook H, Dursun B, Ma Q, Kelly C, et al. Urinary IL-18 is an early predictive biomarker of acute kidney injury after cardiac surgery. Kidney Int. 2006;70(1):199–203. https://doi.org/10.1038/sj.ki.5001527.
Han WK, Waikar SS, Johnson A, Betensky RA, Dent CL, Devarajan P, et al. Urinary biomarkers in the early diagnosis of acute kidney injury. Kidney Int. 2008;73(7):863–9. https://doi.org/10.1038/sj.ki.5002715.
Portilla D, Dent C, Sugaya T, Nagothu KK, Kundi I, Moore P, et al. Liver fatty acid-binding protein as a biomarker of acute kidney injury after cardiac surgery. Kidney Int. 2008;73(4):465–72. https://doi.org/10.1038/sj.ki.5002721.
Andreoli SP. Acute renal failure. Curr Opin Pediatr. 2002;14(2):183–8.
Flynn JT. Choice of dialysis modality for management of pediatric acute renal failure. Pediatr Nephrol. 2002;17(1):61–9. https://doi.org/10.1007/s004670200011.
Williams DM, Sreedhar SS, Mickell JJ, Chan JC. Acute kidney failure: a pediatric experience over 20 years. Arch Pediatr Adolesc Med. 2002;156(9):893–900.
Ball EF, Kara T. Epidemiology and outcome of acute kidney injury in New Zealand children. J Paediatr Child Health. 2008;44(11):642–6. https://doi.org/10.1111/j.1440–1754.2008.01373.x.
Hui-Stickle S, Brewer ED, Goldstein SL. Pediatric ARF epidemiology at a tertiary care center from 1999 to 2001. Am J Kidney Dis. 2005;45(1):96–101.
Sutherland SM, Ji J, Sheikhi FH, Widen E, Tian L, Alexander SR, et al. AKI in hospitalized children: epidemiology and clinical associations in a national cohort. Clin J Am Soc Nephrol. 2013;8(10):1661–9. https://doi.org/10.2215/CJN.00270113.
Palmieri T, Lavrentieva A, Greenhalgh D. An assessment of acute kidney injury with modified RIFLE criteria in pediatric patients with severe burns. Intensive Care Med. 2009;35(12):2125–9. https://doi.org/10.1007/s00134–009–1638–6.
Selewski DT, Cornell TT, Heung M, Troost JP, Ehrmann BJ, Lombel RM, et al. Validation of the KDIGO acute kidney injury criteria in a pediatric critical care population. Intensive Care Med. 2014;40(10):1481–8. https://doi.org/10.1007/s00134–014–3391–8.
Slater MB, Anand V, Uleryk EM, Parshuram CS. A systematic review of RIFLE criteria in children, and its application and association with measures of mortality and morbidity. Kidney Int. 2012;81(8):791–8. https://doi.org/10.1038/ki.2011.466.
Plotz FB, Bouma AB, van Wijk JA, Kneyber MC, Bokenkamp A. Pediatric acute kidney injury in the ICU: an independent evaluation of pRIFLE criteria. Intensive Care Med. 2008;34(9):1713–7. https://doi.org/10.1007/s00134–008–1176–7.
Zappitelli M, Moffett BS, Hyder A, Goldstein SL. Acute kidney injury in non-critically ill children treated with aminoglycoside antibiotics in a tertiary healthcare centre: a retrospective cohort study. Nephrol Dial Transplant. 2011;26(1):144–50. https://doi.org/10.1093/ndt/gfq375.
Lex DJ, Toth R, Cserep Z, Alexander SI, Breuer T, Sapi E, et al. A comparison of the systems for the identification of postoperative acute kidney injury in pediatric cardiac patients. Ann Thorac Surg. 2014;97(1):202–10. https://doi.org/10.1016/j.athoracsur.2013.09.014.
Moffett BS, Goldstein SL. Acute kidney injury and increasing nephrotoxic-medication exposure in noncritically-ill children. Clin J Am Soc Nephrol. 2011;6(4):856–63. https://doi.org/10.2215/CJN.08110910.
Kavaz A, Ozcakar ZB, Kendirli T, Ozturk BB, Ekim M, Yalcinkaya F. Acute kidney injury in a paediatric intensive care unit: comparison of the pRIFLE and AKIN criteria. Acta Paediatr. 2012;101(3):e126–9. https://doi.org/10.1111/j.1651–2227.2011.02526.x.
Sutherland SM, Byrnes JJ, Kothari M, Longhurst CA, Dutta S, Garcia P, et al. AKI in hospitalized children: comparing the pRIFLE, AKIN, and KDIGO definitions. Clin J Am Soc Nephrol. 2015;10(4):554–61. https://doi.org/10.2215/CJN.01900214.
Zappitelli M, Parikh CR, Akcan-Arikan A, Washburn KK, Moffett BS, Goldstein SL. Ascertainment and epidemiology of acute kidney injury varies with definition interpretation. Clin J Am Soc Nephrol. 2008;3(4):948–54. https://doi.org/10.2215/CJN.05431207.
Kaddourah A, Basu RK, Bagshaw SM, Goldstein SL, AWARE Investigators. Epidemiology of acute kidney injury in critically ill children and young adults. N Engl J Med. 2017;376(1):11–20. https://doi.org/10.1056/NEJMoa1611391.
Schaffzin JK, Dodd CN, Nguyen H, Schondelmeyer A, Campanella S, Goldstein SL. Administrative data misclassifies and fails to identify nephrotoxin-associated acute kidney injury in hospitalized children. Hosp Pediatr. 2014;4(3):159–66. https://doi.org/10.1542/hpeds.2013–0116.
Hinchliffe SA, Sargent PH, Howard CV, Chan YF, van Velzen D. Human intrauterine renal growth expressed in absolute number of glomeruli assessed by the disector method and Cavalieri principle. Lab Investig. 1991;64(6):777–84.
Vieux R, Hascoet JM, Merdariu D, Fresson J, Guillemin F. Glomerular filtration rate reference values in very preterm infants. Pediatrics. 2010;125(5):e1186–92. https://doi.org/10.1542/peds.2009–1426.
Carmody JB, Swanson JR, Rhone ET, Charlton JR. Recognition and reporting of AKI in very low birth weight infants. Clin J Am Soc Nephrol. 2014;9(12):2036–43. https://doi.org/10.2215/CJN.05190514.
Viswanathan S, Manyam B, Azhibekov T, Mhanna MJ. Risk factors associated with acute kidney injury in extremely low birth weight (ELBW) infants. Pediatr Nephrol. 2012;27(2):303–11. https://doi.org/10.1007/s00467–011–1977–8.
Kaur S, Jain S, Saha A, Chawla D, Parmar VR, Basu S, et al. Evaluation of glomerular and tubular renal function in neonates with birth asphyxia. Ann Trop Paediatr. 2011;31(2):129–34. https://doi.org/10.1179/146532811X12925735813922.
Selewski DT, Jordan BK, Askenazi DJ, Dechert RE, Sarkar S. Acute kidney injury in asphyxiated newborns treated with therapeutic hypothermia. J Pediatr. 2013;162(4):725–9 e1. https://doi.org/10.1016/j.jpeds.2012.10.002.
Zwiers AJ, de Wildt SN, Hop WC, Dorresteijn EM, Gischler SJ, Tibboel D, et al. Acute kidney injury is a frequent complication in critically ill neonates receiving extracorporeal membrane oxygenation: a 14-year cohort study. Crit Care. 2013;17(4):R151. https://doi.org/10.1186/cc12830.
Alabbas A, Campbell A, Skippen P, Human D, Matsell D, Mammen C. Epidemiology of cardiac surgery-associated acute kidney injury in neonates: a retrospective study. Pediatr Nephrol. 2013;28(7):1127–34. https://doi.org/10.1007/s00467–013–2454–3.
Blinder JJ, Goldstein SL, Lee VV, Baycroft A, Fraser CD, Nelson D, et al. Congenital heart surgery in infants: effects of acute kidney injury on outcomes. J Thorac Cardiovasc Surg. 2012;143(2):368–74. https://doi.org/10.1016/j.jtcvs.2011.06.021.
Askenazi DJ, Koralkar R, Hundley HE, Montesanti A, Patil N, Ambalavanan N. Fluid overload and mortality are associated with acute kidney injury in sick near-term/term neonate. Pediatr Nephrol. 2013;28(4):661–6. https://doi.org/10.1007/s00467–012–2369–4.
Cataldi L, Leone R, Moretti U, De Mitri B, Fanos V, Ruggeri L, et al. Potential risk factors for the development of acute renal failure in preterm newborn infants: a case-control study. Arch Dis Child Fetal Neonatal Ed. 2005;90(6):F514–9. https://doi.org/10.1136/adc.2004.060434.
Cuzzolin L, Fanos V, Pinna B, di Marzio M, Perin M, Tramontozzi P, et al. Postnatal renal function in preterm newborns: a role of diseases, drugs and therapeutic interventions. Pediatr Nephrol. 2006;21(7):931–8. https://doi.org/10.1007/s00467–006–0118–2.
Koralkar R, Ambalavanan N, Levitan EB, McGwin G, Goldstein S, Askenazi D. Acute kidney injury reduces survival in very low birth weight infants. Pediatr Res. 2011;69(4):354–8. https://doi.org/10.1203/PDR.0b013e31820b95ca.
Mathur NB, Agarwal HS, Maria A. Acute renal failure in neonatal sepsis. Indian J Pediatr. 2006;73(6):499–502.
Askenazi DJ, Griffin R, McGwin G, Carlo W, Ambalavanan N. Acute kidney injury is independently associated with mortality in very low birthweight infants: a matched case-control analysis. Pediatr Nephrol. 2009;24(5):991–7. https://doi.org/10.1007/s00467–009–1133-x.
Sarkar S, Askenazi DJ, Jordan BK, Bhagat I, Bapuraj JR, Dechert RE, et al. Relationship between acute kidney injury and brain MRI findings in asphyxiated newborns after therapeutic hypothermia. Pediatr Res. 2014;75(3):431–5. https://doi.org/10.1038/pr.2013.230.
Jetton JG, Askenazi DJ. Update on acute kidney injury in the neonate. Curr Opin Pediatr. 2012;24(2):191–6. https://doi.org/10.1097/MOP.0b013e32834f62d5.
Foland JA, Fortenberry JD, Warshaw BL, Pettignano R, Merritt RK, Heard ML, et al. Fluid overload before continuous hemofiltration and survival in critically ill children: a retrospective analysis. Crit Care Med. 2004;32(8):1771–6.
Selewski DT, Cornell TT, Blatt NB, Han YY, Mottes T, Kommareddi M, et al. Fluid overload and fluid removal in pediatric patients on extracorporeal membrane oxygenation requiring continuous renal replacement therapy. Crit Care Med. 2012;40(9):2694–9. https://doi.org/10.1097/CCM.0b013e318258ff01.
Selewski DT, Cornell TT, Lombel RM, Blatt NB, Han YY, Mottes T, et al. Weight-based determination of fluid overload status and mortality in pediatric intensive care unit patients requiring continuous renal replacement therapy. Intensive Care Med. 2011;37(7):1166–73. https://doi.org/10.1007/s00134–011–2231–3.
Sutherland SM, Zappitelli M, Alexander SR, Chua AN, Brophy PD, Bunchman TE, et al. Fluid overload and mortality in children receiving continuous renal replacement therapy: the prospective pediatric continuous renal replacement therapy registry. Am J Kidney Dis. 2010;55(2):316–25. https://doi.org/10.1053/j.ajkd.2009.10.048.
Modem V, Thompson M, Gollhofer D, Dhar AV, Quigley R. Timing of continuous renal replacement therapy and mortality in critically ill children*. Crit Care Med. 2014;42(4):943–53. https://doi.org/10.1097/CCM.0000000000000039.
Mammen C, Al Abbas A, Skippen P, Nadel H, Levine D, Collet JP, et al. Long-term risk of CKD in children surviving episodes of acute kidney injury in the intensive care unit: a prospective cohort study. Am J Kidney Dis. 2012;59(4):523–30. https://doi.org/10.1053/j.ajkd.2011.10.048.
Askenazi DJ, Feig DI, Graham NM, Hui-Stickle S, Goldstein SL. 3–5 year longitudinal follow-up of pediatric patients after acute renal failure. Kidney Int. 2006;69(1):184–9. https://doi.org/10.1038/sj.ki.5000032.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Science+Business Media, LLC, part of Springer Nature
About this chapter
Cite this chapter
Hunt, E.A.K., Ferguson, M.A. (2018). Pediatric Acute Kidney Injury: Diagnosis, Epidemiology, and Treatment. In: Waikar, S., Murray, P., Singh, A. (eds) Core Concepts in Acute Kidney Injury. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-8628-6_15
Download citation
DOI: https://doi.org/10.1007/978-1-4939-8628-6_15
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-8626-2
Online ISBN: 978-1-4939-8628-6
eBook Packages: MedicineMedicine (R0)