Abstract
There has been great controversy as to what differentiates infection of the urinary tract from mere colonization. The term colonization may be considered obsolete, or, it may be viewed as a clinical scenario on the same continuum as infection. The urinary tract is a sterile medium, and therefore, any presence of bacteria in the urine should be regarded as an infection, regardless of symptomatology. The requirement of delineation between asymptomatic and symptomatic bacteriuria occurs at the level of whether treatment is warranted or not. The additional presence of a catheter adds another level of complexity to the clinical equation. Catheter-associated urinary tract infections are the leading cause of secondary nosocomial bacteremia. An estimated 20 % of hospital-acquired bacteremias arise from the urinary tract, and the mortality associated with this condition is about 10 %. This chapter will seek to increase the understanding of the definitions, epidemiology, etiology (including risk factors and microbiology), pathogenesis, clinical presentation, diagnosis, treatment (including information on antimicrobial drug resistance), complications, and prevention of urinary tract infections.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Urinary tract infection
- Urinary tract colonization
- Asymptomatic bacteriuria
- Catheter-associated urinary tract infection
- Pyuria
- Sterile pyuria
- Cystitis
- Pyelonephritis
- Candiduria
- Funguria
Introduction
There has been great controversy as to what differentiates infection of the urinary tract from mere colonization. The term colonization may be considered obsolete, or, it may be viewed as a clinical scenario on the same continuum as infection. The urinary tract is a sterile medium , and therefore, any presence of bacteria in the urine should be regarded as an infection, regardless of symptomatology. The requirement of delineation between asymptomatic and symptomatic bacteriuria occurs at the level of whether treatment is warranted or not. The additional presence of a catheter adds another level of complexity to the clinical equation. Catheter-associated urinary tract infections are the leading cause of secondary nosocomial bacteremia. An estimated 20 % of hospital-acquired bacteremias arise from the urinary tract, and the mortality associated with this condition is about 10 %. This chapter will seek to increase the understanding of the definitions, epidemiology, etiology (including risk factors and microbiology), pathogenesis, clinical presentation, diagnosis, treatment (including information on antimicrobial drug resistance), complications, and prevention of urinary tract infections.
Definitions
Urinary tract infection (UTI), in patients without a bladder catheter, is defined as the presence of symptomatology in combination with a positive urine culture, containing at least 105 colony-forming units (CFU) per milliliter with the isolation of fewer than two microorganisms.
Catheter-associated urinary tract infection (CAUTI) must contain at least 103 CFU/mL, with the urine sample being obtained with an aseptic technique.
Asymptomatic bacteriuria is defined as isolation of a specified quantitative count of bacteria in an appropriately collected urine specimen from an individual without symptoms or signs (e.g., the absence of fever greater than 38 °C, suprapubic tenderness or costovertebral angle pain or tenderness) of urinary tract infection [1].
For women, asymptomatic bacteriuria is defined as two consecutive clean-catch voided urine specimens with isolation of the same organism in quantitative counts of at least 105 CFU/mL [2].
For men, asymptomatic bacteriuria is defined as a single clean-catch voided urine specimen with one bacterial species isolated in counts of at least 105 CFU/mL in the absence of symptoms [2]. The presence of pyuria (at least 10 leukocytes/mm3 of uncentrifuged urine) is insufficient for the diagnosis of bacteriuria [3].
Symptomatic catheter-related bacteriuria is defined as the presence of fever greater than 38 °C, suprapubic tenderness, costovertebral angle tenderness, or otherwise unexplained systemic symptoms (e.g., malaise, altered mental status, hypotension, metabolic acidosis, respiratory alkalosis, or a systemic inflammatory response syndrome), together with one of the following:
-
Urine culture with greater than 105 CFU/mL irrespective of urinalysis
-
Urine culture with greater than 103 CFU/mL with evidence of pyuria (urinalysis positive for leukocyte esterase and/or nitrite, microscopic pyuria or presence of microbes seen on the Gram stain of unspun urine) [4].
Patients who have had indwelling urinary catheters within the past 48 h (even if they are not in place at the time of infection) are considered to have catheter-associated UTI if they meet these definitions.
In asymptomatic catheterized men or women, bacteriuria is defined as a single catheterized specimen with isolation of a single organism in quantitative counts of at least 102 CFU/mL [2].
Infections of the urinary tract include cystitis (infection of the urinary bladder, or the lower urinary tract), pyelonephritis (infection of the kidney, or the upper urinary tract), or both. Prostatitis, inflammation of the prostate gland, is a separate but similar clinical entity that is beyond the scope of this chapter.
Emphysematous urinary tract infections are infections (cystitis, pyelitis, or pyelonephritis) of the lower or upper urinary tract associated with gas formation.
A urinary tract infection involving a healthy, ambulatory woman with no history suggestive of anatomical or functional urinary tract abnormality is termed as uncomplicated.
A urinary tract infection becomes complicated when it is associated with another underlying condition that increases the risk of treatment failure . These conditions include diabetes, pregnancy, symptoms for at least a week prior to seeking medical attention, hospital-acquired infection, urinary tract obstruction, presence of urinary tract hardware (e.g., indwelling urethral catheter, stent, nephrostomy tube, or urinary diversion), recent urinary tract instrumentation, functional or anatomical urinary tract abnormality, history of childhood urinary tract infection, or renal transplantation. In addition, any urinary tract infection in a male, by definition, is considered to be complicated because they are more likely to be associated with anatomic abnormalities (e.g., bladder outlet obstruction secondary to prostatic hypertrophy or recent instrumentation), and may require surgical intervention to prevent further complications.
Infection with a multidrug resistant organism is also considered complicated, although these patients are not at a higher risk of treatment failure so long as an appropriate antibiotic, based on susceptibility profiles, is used.
Acute complicated pyelonephritis is the progression of an upper urinary tract infection to emphysematous pyelonephritis, renal corticomedullary abscess, perinephric abscess, or papillary necrosis.
The distinction between reinfection and relapse is difficult to make and is arbitrarily defined. A recurrent infection is called a relapse if the infecting strain is the same as the prior infection, and the recurrence occurs within 2 weeks of treatment completion for the prior infection. A recurrent infection is called a reinfection if the infection recurs more than 2 weeks after treatment completion, regardless of the nature of the uropathogenic strain. If there is a documented sterile urine culture between the two infections, and the patient is off antibiotics, the recurrence is also called a reinfection.
Epidemiology
Urinary tract infections are the most common bacterial infection encountered in the ambulatory setting. They accounted for 8.6 million visits nationally in 2007, with 84 % of those cases involving women. By age 32, half of women have had at least one urinary tract infection [5].
For sexually active young women, symptomatic UTI carries a high incidence. Increased risk is seen with recent sexual intercourse, recent spermicide use, and a personal history of UTI [6]. Cystitis also occurs in postmenopausal women [7]. Recurrent uncomplicated UTIs are seen even with anatomic and physiologic urinary tract normality. Acute pyelonephritis is less common than acute cystitis. Recurrent pyelonephritis in healthy women is uncommon. Infections with Escherichia coli (E. coli) in particular tend to recur within the first 6 months [8].
The prevalence of asymptomatic bacteriuria among healthy women tends to increase with age. It affects approximately 1 % of schoolgirls and more than 20 % among women over the age of 80 years. This also tends to correlate with sexual activity [9]. Greater prevalence is seen in premenopausal married women than nuns of the same age [10]. There is no significant difference between pregnant (2 %) and nonpregnant (7 %) women [11]. Asymptomatic bacteriuria generally has a transient (rarely lasting longer than a few weeks) in young healthy women.
Diabetic women have a three- to fourfold higher prevalence (8–15 %), with a correlation seen between the duration and presence of long-term diabetic sequelae. Duration of diabetes more than 10 years has a relative risk of 2.6. Insulin use also appears to carry an increased risk with a relative risk of 3.7 [12].
In pregnancy, bacteriuria occurs in 2–7 %, especially in multiparous women. This prevalence is similar to that seen in nonpregnant women. The organisms are also similar in species and virulence between pregnant and nonpregnant women [13]. Bacteriuria is commonly seen in the first month of pregnancy [14]. Acute cystitis occurs in 1–2 % of pregnant women. There is a greater likelihood among pregnant women for bacteriuria to progress to pyelonephritis. Up to 30–40 % of pregnant women with untreated asymptomatic bacteriuria will develop symptomatic UTI, including pyelonephritis. This risk is reduced by 70–80 % if the bacteriuria is treated [15].
For young healthy adult men, the incidence of symptomatic UTI (5–8 UTIs per year per 10,000 young to middle-aged men) is much lower than that in women. Asymptomatic bacteriuria is rare among healthy young males [16]. The prevalence rises to 6–15 % among men over the age of 75 years [17]. The presence of diabetes does not confer any additional risk of asymptomatic bacteriuria among males.
Candiduria is becoming increasingly common, with nosocomial UTIs due to Candida species being 22 % between 1986 and 1989 to almost 40 % between 1992 and 1997 [18]. Many of these patients were asymptomatic; therefore, a distinction between infection versus colonization could not be delineated [19].
Indwelling bladder catheters confer a significant ris k of bacteriuria. Patients develop bacteriuria at a rate of 3–10 % per day of catheterization [20]. The clinical significance of catheter-associated asymptomatic bacteriuria is not known. About 10–25 % of patients will be symptomatic [21].
Urinary tract infections encompass almost half of infectious complications of renal transplantation [22]. The incidence of UTI following transplantation has been reduced with improvements in surgical procedures, greater attention to rapid catheter removal, refinements in immunosuppressive therapy, and routine administration of antibiotic prophylaxis [23].
Etiology
Many different variables are responsible for the causation of urinary tract infections. Sexual intercourse, diaphragm-spermicide use, and a history of recurrent UTIs are strong and independent risk factors [6]. There is an increased risk for approximately 24 h post-coitus. Increased sexual intercourse frequency correspondingly increases risk of infection. Having a new sexual partner within the past year increases risk [24].
Spermicide-coated condom use increases risk, as does recent antimicrobial use, even if used for UTI treatment [25]. Antimicrobials (beta-lactams are more heavily implicated than trimethoprim-sulfamethoxazole) lead to an alteration of urogenital flora, especially Lactobacillus. A lack of Lactobacilli in the vaginal flora predisposes to UTI as these organisms competitively exclude uropathogens through epithelial adhesion. Lactobacilli also produce lactic acid which lowers the vaginal pH, creating an inhospitable environment for uropathogens. They also produce bacteriocins and surfactants, and are involved in H2O2 production, in combination with chloride and myeloperoxidase in the vagina. Lactobacilli loss can also be caused by menopause (leading to a loss of estrogen and increased vaginal pH) and bacterial vaginosis [26].
Another identified risk factor is having the first UTI before the age of 15 years. Despite widespread thought that bathroom hygiene and wiping habits are associated with increased risk for UTIs, there has been no data to support this claim [24].
The use insulin and longer diabetes duration (greater than 10 years) confer an increased risk. Diabetics do not exhibit a different microbial profile compared to non-diabetics [12]. Diabetes mellitus and urinary tract obstruction (mainly papillary necrosis and ureteral calculi) confer an increased risk for emphysematous UTIs [27].
Anatomical and urologic differences may also account for infections and recurrences. These include obstruction, stone formation, indwelling catheters, scarring, trauma, fistula formation, urinary incontinence, presence of a cystocele, post-void residual urine, a history of UTI before attaining menopause, and non-secretor status (discussed in Pathogenesis section) [28]. Neurogenic bladder carries an increased risk due to altered urodynamics and microtrauma from repeated intermittent catheterizations.
Specific risk factors identified for UTIs in men include insertive anal intercourse and lack of circumcision [29].
Risk factors for catheter-associated bacteriuria or UTI include female gender, diabetes mellitus, prolonged catheterization, bacterial colonization of the drainage bag, and errors in catheter care [30].
The microbes implicated in uncomplicated cystitis and pyelonephritis are mainly Escherichia coli (75–95 %), with occasional other Enterobacteriaceae (such as Proteus mirabilis and Klebsiella pneumoniae), and Staphylococcus saprophyticus . Other Gram-negative and Gram-positive organisms are rarely isolated in uncomplicated infections [31].
Complicated UTIs involve a larger microbial spectrum , including the aforementioned pathogens, along with Pseudomonas, Serratia, Providencia, Enterococci, Staphylococci, and fungi. Organisms leading to complicated infections are more prone to exhibit antimicrobial drug resistance patterns [32]. Risk factors for progression to complicated pyelonephritis include urinary tract obstruction, urologic dysfunction, antibiotic resistant pathogen(s), and diabetes (particularly for emphysematous pyelonephritis and papillary necrosis).
Emphysematous infections are usually due to E. coli or Klebsiella pneumoniae [27]. Candida is a rare cause [33].
If organisms such as Lactobacilli, Enterococci, Group B Streptococci, and coagulase-negative Staphylococci (excluding Staphylococcus saprophyticus) are isolated in otherwise healthy individuals, contamination of the urine specimen is a reasonable conclusion. However, if these cultures are seen in symptomatic women when found in voided midstream urine at high counts with pure growth, they can be considered pathogenic [5].
Funguria is common among hospitalized patients and is generally benign. Invasive kidney infection is unusual, but difficult to treat. Risk factors for funguria included urinary tract drainage devices, prior antibiotic use, diabetes, urinary tract pathology, and malignancy. Common fungal isolates in the urine are Candida species (predominantly Candida albicans and Candida glabrata). A variety of other fungi can rarely involve the kidney as a result of disseminated infection. These include Aspergillus, Fusarium, Trichosporon, Mucorales (Rhizopus, Mucor), Dematiaceous molds, Cryptococcus neoformans, Histoplasma capsulatum, Coccidioides, Blastomyces dermatitidis, Paracoccidioides brasiliensis, Sporothrix schenckii, and Penicillium marneffei.
Risk factors for UTI in transplant patients include the same risk factors that apply to the general population, in addition to additional factors related to the transplantation itself. Risk factors unrelated to transplantation include advanced age, female gender, reflux kidney disease prior to transplantation, and diabetes mellitus. Risk factors directly related to transplantation include deceased donor kidney, kidney–pancreas transplant, retransplantation, antithymocyte globulin administration, urinary bladder catheterization, allograft rejection and subsequent increased immunosuppression, and ureteral stent placement [22].
Renal transplant patients exhibit many differences in microbial patterns. In general, infections are caused by Gram-negative organisms, predominantly E. coli. The other Gram-negative uropathogens that have been isolated include Pseudomonas aeruginosa, Enterobacter cloacae, Klebsiella pneumoniae, Klebsiella oxytoca, Serratia marcescens, Stenotrophomonas maltophilia, Citrobacter freundii, Proteus mirabilis, Achromobacter xylosoxidans, Acinetobacter baumannii, and Morganella morganii. Because of the common practice of administering antibiotic prophylaxis among transplant recipients, these organisms tend to exhibit increased resistance patterns [34]. Fungal UTIs occur in 5–11 % of transplant recipients with UTI, with Candida albicans being the most common cause. Other species include Candida tropicalis, Candida glabrata, and Candida krusei [35].
Pathogenesis
The pathogenesis of urinary tract infections involves a complex balance and interaction between a variety of factors. The main factors implicated include host-related factors (such as innate factors, urinary tract abnormalities, and behavioral factors) and pathogen-related factors (such as virulence).
Humans have a built-in normal defense mechanism against urinary tract infections. The mechanical force of urine flow helps expel any existing organisms from the genitourinary system. Superficial umbrella cells in the bladder will exfoliate in response to bacteria binding to surface uroplakins (a type of membrane protein). Underlying cells will rapidly differentiate into superficial facet cells [36, 37].
There is also an innate immune response to urinary tract infections. There are antimicrobial peptides , such as beta-defensin 1 and cathelicidin LL-37, in urine that bind and disrupt bacterial membranes. Elements involved in host iron sequestration include lactoferrin, transferrin, and lipocalin-2. Tamm-Horsfall protein, or uromodulin, is responsible for binding and blocking bacterial fimbriae. Bladder and kidney cells are capable of upregulating cytokines and chemokines in response to bacteria, of which interleukin (IL) 8 appears to be a key factor by functioning as a neutrophil attractant. There are also a variety of Toll-like receptors (TLR) that recognize different patterns as part of the host response. TLR1 and TLR2 recognize lipopeptides, TLR4 recognizes fimbriae and lipopolysaccharides, and TLR5 recognizes flagellin. These Toll-like receptors upregulate NFkB that subsequently increases the production of IL-6 and IL-8 [36, 37].
Urinary tract infections in women generally originate with fecal flora that colonize the vaginal introitus. These organisms then ascend the urethra to enter the bladder. Alterations in the normal vaginal flora, especially a decrease in H2O2-producing lactobacilli, can predispose to introital colonization with E. coli. Pyelonephritis is a result of pathogen ascent to the kidneys through the ureters. Underlying host and microbial factors that lead to progression from cystitis to pyelonephritis are not well understood at this time. Pyelonephritis may be caused by seeding of the kidneys as a result from bacteremia or from bacteria present in the lymphatic system [26].
There is a predisposition for developing pyelonephritis in pregnancy. This may be related to pregnancy-related anatomic changes in the urinary tract, such as increased pressure on the bladder from the enlarging gravid uterus, and an increase in ureteral size due to smooth muscle relaxation. The immunosuppression of pregnancy may also play a role, including lower mucosal IL-6 levels and serum antibody responses to E. coli antigens [38].
Recurrences, in general, follow the same basic principles as sporadic infection . Recurrences due to the same bacterial strain may be due to reinfection, with the source being a remnant uropathogen reservoir in the bladder epithelium from a prior infection. This may be related to intracellular bacterial communities and quiescent intracellular reservoirs [39]. There is evidence of clonal invasion of epithelial cells in biofilm structures. This allows the bacteria to evade host defenses. Antibiotics are not capable of penetrating these structures well. The majority of cystitis recurrences are reinfections . The initial pathogenic strain can persist in the fecal flora after being eliminated from the urinary tract. E. coli strains can be responsible for recurrent UTIs 1–3 years later, although most recurrences occur within the first 3 months [40].
Women with recurrent infections have an increased susceptibility to vaginal colonization with uropathogens. This is partially due to a greater tendency for uropathogenic coliforms to adhere to the uroepithelium in women with a history of recurrences when compared to women without recurrent infections [41]. Genetic determinants also play a role. The non-secretor and the P1 phenotypes have higher expression among females with recurrent UTI and recurrent pyelonephritis, respectively. Uroepithelial cells from women who are non-secretors of ABH blood group antigens have stronger adherence of uropathogenic E. coli when compared with cells from secretors [42]. The non-secretors also express unique glycolipid receptors that bind uropathogenic E. coli. The IL-8 receptor (IL8R or CXCR1) is another implicated genetic factor. IL-8 promotes neutrophil migration across infected uroepithelium [43].
Asymptomatic bacteriuria and symptomatic urinary tract infection are significantly less common in men when compared to women. This is because of inherent anatomical differences in men, namely the longer urethral length, drier periurethral environment (with subsequent less frequent bacterial colonization), and prostatic fluid’s antibacterial properties.
The lack of symptoms with asymptomatic bacteriuria may be related to the specific pathogen, the host, or both. When comparing asymptomatic bacteriuria, cystitis, and pyelonephritis, the microbiology is similar. There may be some strains that exhibit subtle adaptations that promote pathogenesis. In order for symptomatic infection to occur, bacteria irreversibly attach to the urinary tract via fimbrial adhesins . Some strains with reduced fimbrial expression grow more rapidly, which then leads to asymptomatic bacteriuria [44]. The strains implicated in asymptomatic bacteriuria might be less virulent, and therefore, may not constitute true pathogens and are unlikely to progress to serious infection [45]. Because of this, it is postulated that colonization with “uroprotective” bacterial strains (especially strains of E. coli) may protect against infection from invasive uropathogens [46]. Host factors that may be implicated in asymptomatic bacteriuria may be related to lower levels of neutrophil Toll-like receptor 4 (TLR4) expression . TLR4 is responsible for the mucosal response to E. coli, and its inactivation can lead to a carrier state resembling asymptomatic bacteriuria [47].
Bacterial adhesion to mucosal or urothelial cells is an important determinant of bacterial virulence. Infection in the urinary tract is partly related to the bacteria’s ability to adhere and colonize other locations (e.g., the gut, perineum, urethra, bladder, and kidneys) [48]. Adhesion is especially of interest when infections occurs in an anatomically normal urinary tract, but it also plays a significant role in recurrent cystitis and catheter-associated infections [49].
Uropathogenic Enterobacteriaceae are electronegative and too small to overcome repulsion by the net negative charge of epithelial cells. Therefore, bacterial adhesion cannot happen in the absence of fimbrial or other non-fimbrial surface adhesion systems, which have favorable electrical charge and promote adhesion via hydrophobicity [50].
Bacterial virulence does not appear to be related to antimicrobial drug resistance.
Virulence of uropathogenic E. coli appears to be related to several O-serotypes (O1, O2, O4, O6, O7, O16, O18, and O75) [51]. While they only comprise 28 % of normal fecal flora isolates, they are the culprit in 80 % of pyelonephritis cases, 60 % of cystitis cases, and 30 % of asymptomatic bacteriuria cases [52].
The presence of adhesins on the tip of bacterial fimbriae (also known as pili) and on the bacterial surface (non-fimbrial adhesins) is the most important factor in E. coli uropathogenicity. Most adhesins are lectins that recognize binding site conformations from oligosaccharide sequences on the epithelial cell surface [53].
Two major fimbrial adherence systems (PAP and SFA) have been identified in E. coli strains associated with urinary tract infections. The PAP adhesin is found on the tip of P fimbriae. The term P fimbriae relates to the PAP adhesin’s ability to recognize the human digalactoside P blood group determinants on human erythrocytes and urothelial cells, that then facilitates increased adhesion. This plays an important role in host susceptibility to infection. Epithelial binding and invasion appears to be accomplished by Dr fimbriae [53].
Non-fimbrial adhesins include many different proteins, including AFA and the AT (autotransporter) family of trimeric proteins. Two of these latter proteins have structural similarity to the E. coli K12 antigen 43 (Ag43a), which promotes biofilm growth. Its expression is associated with long-term E. coli bladder colonization. UpaG is another non-fimbrial adhesin that binds to the epithelium, mediates cell aggregation, and relates to biofilm formation [54].
The frequency of PAP, SFA, and AFA operons is approximately 75 %, 25 %, and 10 %, respectively in pyelonephritis; 45, 20, and 12 % in cystitis; and 24, 27, and 0 % in asymptomatic bacteriuria [55]. Virtually all young females with a normal urinary tract and pyelonephritis have been found to have at least one adhesin system [56].
Because of the aforementioned findings, patients with UTI who are infected with non-uropathogenic (non-fimbrial) bacteria should undergo further investigations to detect a structural defect (e.g., intermittent reflux, neuromuscular bladder dysfunction, or bladder neck obstruction) leading to infection [56].
Apart from the presence of adhesins , bacterial fimbriae also appear to have other virulence properties that are responsible for development of infection, but these are not yet well defined. Other virulence factors include the presence of flagellae (which are responsible for motility), hemolysin production (which form pores in the epithelial cell membrane and lead to inflammation, damage, and hemorrhage), and aerobactin production (which is necessary for iron uptake in the iron-deficient urinary tract). CNF1 appears to play a role in adherence and invasion, and can stimulate bladder cell apoptosis [51].
Escherichia coli is capable of evading host defense mechanisms, as well. Its type 1 fimbriae make the siderophore enterobactin, which is neutralized by the host protein lipocalin-2. The bacteria can glycosylate enterobactin into salmochelin, which lipocalin-2 cannot recognize. E. coli can also synthesize factors that blunt cytokine responses and help resist free radicals. It can also produce immunosuppressants such as SisA and SisB [36, 37].
Escherichia coli may also have an effect on ureteral peristalsis. Multiple strains of E. coli were tested. Non-uropathogenic strains had no significant effect on ureteral motility. However, uropathogenic strains demonstrated some effect, from 9.47 to 96.7 % ureteral dysmotility over 8 h. This effect is postulated to be related to the FimH adhesin on the end of type 1 fimbriae [57].
Proteus mirabilis has its own armamentarium of virulence factors, including urease production, hemolysin production, IgA protease production, iron acquisition, flagellae, and fimbriae. Urease hydrolyzes urea to ammonia and carbon dioxide. Ammonia combines with hydrogen to form ammonium. This leads to urine alkalinization with the urine pH being frequently above 7.0 and can even reach as high as 9.0. The alkalinity promotes precipitation of phosphate, carbonate, and magnesium, which form struvite stones and then large staghorn calculi. These stones contain a mixture of proteinaceous matrix, leukocytes, struvite, and bacteria. Because the stone is Proteus-contaminated, it becomes a permanent source of bacteria. It also leads to urinary stasis, which then furthers bacterial multiplication, urinary alkalinization, and deposition of new struvite layers. Hemolysin in Proteus species works in a similar fashion to Escherichia species in that it leads to epithelial cell inflammation, damage, and hemorrhage. Another entity, Proteus toxic agglutinin, remains anchored on the bacterial surface and leads to bacterial auto-agglutination. This process is directly toxic to bladder and kidney cells [58].
Proteus mirabilis produces at least 4 fimbrial types that do not appear to be requisite for causing infection. At least 2 fimbrial systems may contribute to colonization , namely the MR/P fimbriae for bladder and kidney infection; and the PMF fimbriae for bladder infection. UCA fimbriae bind epithelial cells and can target a variety of surface receptors. ATF fimbriae is another structure that appears to be expressed optimally at room temperature, and may play a role in the organism’s survival outside of the urinary tract. ZapA is a zinc metalloprotease that cleaves IgG, IgA, complement, and antimicrobial peptides [58].
A particular phenotype termed “swarm cell differentiation ,” characterized by the formation of very long flagellae, appears to facilitate ascent into the urinary tract [59].
Staphylococcus saprophyticus is a common cause of cystitis in young sexually active women. It rarely leads to pyelonephritis. This organism adheres strongly to the urothelium apparently because of a lactosamine residue [60].
Microorganisms have uptake and transport systems that steal essential metals from the host. The most important metals that have been identified are iron and zinc. Iron is critical for a variety of host processes. Zinc plays a key role in metalloprotease activity and piliation. The host sequesters these nutrients as a defense mechanism. However, bacteria are able to generate siderophores in order to harvest iron [36, 37].
The pathogenesis of funguria is not as well understood. Fungal multiplication is commonly found within the kidney, a phenomenon which does not appear to occur in any other organ. It is not known whether fungi preferentially localize in the kidney or are cleared from other organs more efficiently. The pathogenesis of fungal renal infection appear to be related to the attachment of fungi to endothelial surfaces and penetration into tissue. The presence of yeast in the capillary beds of the kidneys elicits an inflammatory response. The yeasts survive only if they are able to penetrate the capillary walls and invade the interstitium. Invasion is expedited by attachment of the fungi via adherence mechanisms to the capillary walls. Pseudohyphal and hyphal forms facilitate penetration through the capillary walls. Ascending infection of the kidneys appears to be related to vesicoureteral reflux of fungi from the bladder [61].
Catheter-associated urinary tract infections may be extraluminal or intraluminal. Extraluminal infections occur with bacterial entry into the bladder along the biofilm that forms around the catheter in the urethra. Intraluminal infections occur due to urinary stasis because of drainage failure, or due to drainage bag contamination with subsequent ascending infection. Extraluminal infections are more common than intraluminal [62].
The organisms that cause urinary tract infections in a hospital or nursing home are usually of different species and often have greater antibiotic resistance profiles when compared to pathogens seen in the general community. Ambulatory patients with indwelling catheters tend to acquire uropathogens similar to those seen in hospitalized patients. These organisms may lack some virulence factors that allow the usual uropathogen to adhere to uroepithelial cells, but they can still easily access the bladder via the catheter. Upper urinary tract infection is also an important consequence of CAUTIs [63].
Clinical Presentation
There is a crucial distinction to be made when evaluating a patient with bacteriuria—whether they are symptomatic or not. This distinction will serve to determine whether treatment is warranted. Many patients with bacteriuria will be asymptomatic, and may not always require antibiotic treatment. Symptomatic patients, on the other hand, will always require treatment. This will be further discussed later.
Patients with cystitis have dysuria, frequency, urgency, suprapubic pain/discomfort, and/or hematuria [64].
Patients with pyelonephritis may or may not complain of the symptoms associated with cystitis, in addition to fever, chills, flank pain, costovertebral angle tenderness, nausea, and/or vomiting. Symptoms may mimic pelvic inflammatory disease. On rare occasions, acute pyelonephritis may manifest as acute kidney injury, sepsis, multiple organ dysfunction syndrome (MODS) , and/or shock [64].
Patients with emphysematous cystitis most commonly present with abdominal pain. Emphysematous pyelonephritis and emphysematous pyelitis are indistinguishable from severe acute pyelonephritis based on presentation. The symptoms may present suddenly or may evolve over 2–3 weeks.
Complicated pyelonephritis may present as weeks to months of malaise, fatigue, nausea, or abdominal pain.
Chronic pyelonephritis is an uncommon cause of chronic tubulointerstitial disease, usually associated with a chronically obstructing calculus or vesicoureteral reflux, in which patients again present with weeks to months of insidious non-specific symptoms.
Patients with indwelling catheters are rarely symptomatic. Even when faced with fever, urinary symptoms, and leukocytosis, it can be difficult to attribute these to an active UTI [21].
Funguria is a common occurrence in the presence of indwelling catheters. When asymptomatic, the presence of yeasts generally reflect colonization . Infected patients may have dysuria, frequency, and suprapubic discomfort. When present, symptoms of fungal kidney involvement may include flank pain, costovertebral angle tenderness, abdominal pain, and/or abdominal tenderness [65].
Symptoms of urinary tract infection in pregnancy are no different from the nonpregnant population.
Patients in the extremes of age may have subtle symptoms . Elderly patients with indwelling catheters often have atypical presentations of infection. The clues to the presence of infection may be the development of fever or otherwise unexplained systemic manifestations compatible with infection, such as altered mental status, delirium, fall in blood pressure, metabolic acidosis, tachypnea, and respiratory alkalosis. However, fever may not be present [21].
In renal transplant patients, urinary tract infection usually occurs within the first year after transplantation. Now, due to multiple factors (routine administration of prophylactic antibiotics, refinements in immunosuppression, improvements in surgical techniques, and greater attention to early catheter removal post-operatively), more patients are presenting with UTI after the first year of transplantation. Patients can present with either uncomplicated cystitis (without pyelonephritis of allograft or native kidney and without sepsis) or pyelonephritis involving either the native kidney or allograft. Symptoms are generally comparable to non-transplant patients [34]. Occasionally, patients may lack all clinical manifestations of UTI because of immunosuppression and denervation of the renal allograft [66].
Diagnosis
Clinical history is of the utmost importance in diagnosis of uncomplicated cystitis or pyelonephritis along with clinical manifestations mentioned above. The likelihood of cystitis is more than 50 % in a woman with any of the symptoms of urinary tract infection presented above (clinical manifestations section) but the probability of urinary tract infection is usually greater than 90 % in a woman presenting with dysuria and frequency in the absence of vaginal discharge or irritation [3, 64].
Physical examination is another important entity and should consist of evaluation for fever, costovertebral angle tenderness, and complete abdominal examination including signs of guarding and rigidity. Complete pelvic exam should also be considered in cases where vaginitis or urethritis is present. In addition, testing for pregnancy is crucial in women of child bearing age presenting with symptoms of urinary tract infection.
Further assessment with laboratory diagnostic testing includes urinalysis and urine culture with susceptibility information. Urinalysis with microscopy or dipstick is acceptable depending on inpatient versus outpatient setting and is a quick and cheap diagnostic tool complimenting urine culture. However, urinalysis without a urine culture is also considered adequate for diagnosing uncomplicated cystitis if clinical symptoms are indicative of urinary tract infection unless there is strong suspicion for antimicrobial resistance or other confounding features including indwelling catheters, anatomic abnormalities, history of renal transplant, and clinical signs/symptoms indicating complicated cystitis with pyelonephritis.
Routine imaging studies are not indicated for diagnosing acute uncomplicated cystitis but may be required in certain complicated cases, recurrent UTIs, and pyelonephritis.
The most important aspect of urinalysis is searching for pyuria when evaluating a patient for urinary tract infection. Lack of pyuria on urinalysis should strongly instigate the clinician to look for alternative diagnosis as pyuria is present in nearly all patients presenting with acute cystitis or pyelonephritis [67].
Evaluating an unspun midstream voided urine sample with a hemocytometer is the most precise technique of assessing for pyuria. A positive result is reported with ≥10 leukocytes/microL [3].
Presence of white blood cell casts in the urine is indicative of upper tract infection. Red blood cells are common in UTI setting but uncommon in urethritis or vaginitis and therefore are helpful to the clinician when making treatment decisions. Hematuria, on the other hand, is neither an indication for longer therapy nor is a predictor for more severe infection.
Commercially available dipsticks are used to detect the presence of leukocyte esterase which is an enzymatic product of leukocytes indicating pyuria. Dipsticks also detect for nitrite, a by-product of Enterobacteriaceae which convert urinary nitrate to nitrite.
Leukocyte esterase may also be used to look for >10 leukocytes per high power field which has sensitivity of 75–96 % and specificity of 94–98 % [68]. Furthermore, the presence of nitrite is appreciably sensitive and specific for detecting ≥105 CFU of Enterobacteriaceae per mL of urine but it does not have acceptable sensitivity to detect for other organisms. Consequently, negative results should not be taken for granted [69]. Further caution should be used when interpreting positive nitrite results because false positive nitrite tests can result when compounds that can make urine red are involved, such as bladder analgesic phenazopyridine or ingestion of beats.
The dipstick exam is useful in assessing for UTI when positive for either leukocyte esterase or nitrite with sensitivity of 75 % and a specificity of 82 % [64]. However, positive or negative dipstick results cannot accurately rule in or rule out a UTI because the clinical history along with presenting signs and symptoms of an individual patient is always considered more reliable.
Obtaining a proper urine culture may also be required when evaluating a patient with suspected UTI as treatment with antibiotics is considered. This has been increasingly more important in the face of increasing prevalence of antimicrobial resistance amid uropathogens . It is also crucial to obtain a urine culture when dealing with a complicated UTI [70]. For instance, urine culture with susceptibility testing should be performed in all patients presenting with signs and symptoms of acute pyelonephritis [71]. Furthermore, a urine culture should be obtained for susceptibility data of uropathogens if a patient is suffering from recurrent UTIs or symptoms persist after completing a course of antibiotics. A voided midstream urine specimen should be obtained for best results.
Treatment and Resistance
Treatment guidelines presented in this section are intended for treating uncomplicated acute cystitis and pyelonephritis . Complicated cystitis and pyelonephritis therapy guidelines are not covered in this chapter as they are beyond the scope of this text.
Treatment of UTI is based on the severity of the infection . A key decision point in selecting an appropriate antibiotic regimen is whether a cystitis or pyelonephritis is present. Antibiotic selection for treatment of acute cystitis further depends on certain key factors that include resistance profiles of uropathogens, efficacy of selected antimicrobial agent along with its side effect profile, drug availability, and cost [72].
Some of the commonly suggested antimicrobial agents for the treatment of acute cystitis are as follows:
Nitrofurantoin: Nitrofurantoin monohydrate/macrocrystals with suggested dose of 100 mg twice daily has reported efficacy rate of 90–95 % when used for 5–7 days orally according to randomized trials [73].
Special consideration: Nitrofurantoin is contraindicated in patients with creatinine clearance of <60 mL/min.
Trimethoprim-sulfamethoxazole (TMP-SMX): TMP-SMX with suggested dose of 160/800 mg (one double strength tablet) twice daily has reported efficacy rate of 86–100 % when used for 3–7 days orally according to randomized trials [74]. TMP-SMX should be dose adjusted at 50 % of recommended dose for patients with creatinine clearance of 15–30 mL/min.
Special consideration: Trimethoprim-sulfamethoxazole is contraindicated in patients with creatinine clearance of less than 15 mL/min.
Fosfomycin: Fosfomycin trometamol has reported efficacy rate of 91 % when given 3 g as a single dose according to one randomized trial [75]. However, it is considered inferior in efficacy when compared to other first-line agents suggested for treatment of acute cystitis [76].
Pivmecillinam: Pivmecillinam with suggested dose of 400 mg twice daily has reported efficacy of 55–82 % when given for 3–7 days orally according to randomized trials [77]. Evidently, it has lower clinical efficacy when compared to the other agents mentioned above. Pivmecillinam is currently not available in the USA.
Pyelonephritis is a more severe infection compared to cystitis and therefore requires special attention and selection of broader-spectrum antimicrobial agents. Definitive treatment of pyelonephritis is generally based on susceptibility profiles of causative microbes. However, empiric choice of antimicrobial agents is again based on the severity of illness. One important decision point in treating pyelonephritis is whether to initiate inpatient treatment (which generally requires intravenous antibiotics) or if outpatient treatment with oral antibiotics is adequate.
Outpatient management of pyelonephritis is deemed appropriate for patients who have mild to moderate illness (with mild symptoms and low grade fever) that can be treated with oral antibiotic and oral hydration [78].
Oral fluoroquinolones are the cornerstone of outpatient empiric therapy for patients with acute uncomplicated pyelonephritis. There has been ongoing concern for increasing resistance of uropathogens to currently available fluoroquinolones but clinical efficacy remains high when these antibiotics are used in accordance with susceptibility profiles [79].
For outpatient empiric treatment of pyelonephritis , the commonly suggested oral fluoroquinolones are ciprofloxacin and levofloxacin. For example, 500 mg of ciprofloxacin orally twice daily for 7 days or 1000 mg of extended release oral ciprofloxacin for 7 days are suggested regimens. Alternatively, 750 mg of oral levofloxacin for 5–7 days is also acceptable.
Of note, fluoroquinolones are contraindicated in pregnancy. Therefore, when fluoroquinolones are used for treatment or prophylaxis in women in the reproductive age group, an effective contraception should be advised. Other serious side effects of fluoroquinolones include prolonged QTc interval in patients with certain cardiac conditions and risk of tendon rupture.
Albeit, final selection of oral antibiotic is then based on susceptibility profiles of the infection causing organisms and side effect profiles of antimicrobial agents selected.
On the contrary, inpatient management is mandatory for patients with pyelonephritis who present with more severe illness demonstrating high fever, hemodynamic instability, and inability to take adequate oral hydration or medications due to marked nausea/vomiting, excessive pain, and pregnancy. Empiric intravenous antibiotic therapy should be initiated promptly which is then tailored as susceptibility data becomes available. Commonly suggested intravenous antibiotics include fluoroquinolones, aminoglycosides, extended-spectrum cephalosporins, extended-spectrum penicillins, as well as carbapenems depending on the severity of the infection, other complicating factors, and prevalence of local resistance [5].
Moreover, when extended-spectrum beta-lactamase (ESBL ) producing microbes are involved, intravenous carbapenems should be the choice for antibiotics [80].
Hospitalized patients receiving intravenous antibiotics should be monitored closely and should be switched to appropriate oral agents when significant clinical improvement is evident and patients are able to tolerate oral hydration as well as medications [81].
Most of the discussion on diagnosis and treatment so far has been devoted to urinary tract infections in women because asymptomatic bacteriuria and symptomatic urinary tract infections are much less common in men due to longer urethral length, relatively dry periurethral environment leading to lower frequency of colonization around the urethra and antibacterial properties of prostatic fluid [82].
Traditionally, all urinary tract infections in men between the age of 15 and 50 have been deemed complicated because most UTIs occur in infants and the elderly that have urologic anomalies, such as bladder outlet obstruction, or men with neurogenic bladders leading to altered urinary dynamics and microtrauma from intermittent catheterization, and urologic procedures. Nevertheless, clinical diagnosis and treatment of uncomplicated cystitis and pyelonephritis in men with normal urinary systems is comparable to diagnosis and treatment in women for all practical purposes.
There are some special circumstances where screening for and treating asymptomatic bacteriuria in men between the ages of 15 and 50 may be justified as well. These special considerations include transurethral resection of the prostate or other urologic procedures that put the patient at risk of bactremia with instrumentation causing mucosal bleeding which can lead to sepsis and septic shock [2, 29].
Men with recurrent cystitis additionally warrant special consideration and evaluation for prostatitis with focus on physical examination and may require digital rectal examination for further management. In addition, the possibility of urethritis should be considered in young sexually active men presenting with UTI symptoms.
Imaging studies are also not routinely needed for diagnosing uncomplicated acute cystitis and pyelonephritis in men but may be helpful in certain circumstances.
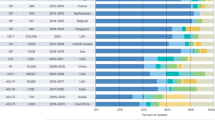
Finally, growing uropathogen resistance can present a considerable challenge when selecting antimicrobial agents. Microbial resistance patterns vary significantly depending on geographic location and this is mostly true for E. coli. For instance, multiple studies show that resistance rates are higher amongst medial centers in the USA when compared to Canadian medical centers [83]. Resistance rates as high as greater than 20 % have been reported in many regions for trimethoprim (with or without sulfamethoxazole). Resistance for fluoroquinolones has been reported close to 10 % in most parts of North America [84]. Furthermore, ciprofloxacin resistance rates have been reported to have increased from 3 to 17 % between the years of 2000 and 2010 [79]. First and second generation oral cephalosporins are reported to have less than 10 % resistance. Nitrofurantoin is reported to have good in vitro activity in all regions generally [85]. Based on this reported data, the agents with least resistance may be used for empiric therapy in uncomplicated urinary infections caused by E. coli.
Complications
Recurrent uncomplicated urinary tract infections are relatively common in otherwise young, healthy woman even with normal anatomical and physiological urinary tracts. There have been no reported long-term complications including renal disease, permanent urinary tract injury, or other sequela leading to long-term health problems from recurrent UTIs in absence of anatomic or functional abnormalities of the urinary tract.
Patients presenting with complicated (please refer to the definitions section above for definition of complicated UTI) urinary tract infections leading to pyelonephritis can have a number of dire complications that require a special attention. Acute complicated pyelonephritis for instance can lead to sepsis, multi-organ system failure, shock, and acute renal failure. Moreover, progression of acute complicated pyelonephritis can lead to such complications as renal corticomedullary abscess, perinephric abscess, emphysematous pyelonephritis, or papillary necrosis. Some important risk factors for more advanced disease with progression to complicated pyelonephritis include urinary tract obstruction, urinary dysfunction, infection with multi-drug resistance uropathogens, and diabetes. Diabetes alone is a significant risk factor particularly for emphysematous pyelonephritis and papillary necrosis. Patients presenting with complicated acute pyelonephritis associated symptoms therefore should alert a clinician to diagnose and treat this potentially life threatening condition with a sense of urgency.
Prevention
Recurrent UTIs in women could present a significant burden and increase the risk of developing antibiotic resistance.
A number of behavioral interventions have been suggested that may be helpful in preventing recurrent UTIs in women. However, many of these behavioral interventions have not been sufficiently studied and tested clinically. Clinicians and patients arguably hold strong biases about the usefulness of these behavioral interventions and therefore it is important to consider them as tools of preventing UTIs that may help in limiting the use of antibiotics.
For instance, use of spermicides (especially coupled with diaphragms) in sexually active woman has been suggested to increase the risk of recurrent UTIs. These women should be counseled on the association between UTIs and use of spermicides during sexual intercourse. Avoiding the usage of spermicide consisting products is expected to reduce the risk of recurrent UTIs.
Another popular behavioral intervention often suggested is an early postcoital voiding and generous fluid intake to increase the frequency of micturition.
Furthermore, decreasing the frequency of sexual intercourse or complete abstinence are also commonly suggested strategies for preventing recurrent UTIs but may not be very practical.
Cranberry juice has also been widely used by patients for prevention of recurrent UTIs. A few laboratory studies have suggested that cranberry juice may inhibit adherence of urinary tract microbes to uroepithelial cells [85]. However, most clinical studies reported on clinical efficacy of cranberry juice have been suboptimal and limited (due to lack of power or other design limitations) [86]. Routine use of cranberry juice is not recommended clinically. Additionally, cranberry juice may also put patients at risk of unwanted gastrointestinal side effects such as gastroesophageal reflux as demonstrated by some studies [87].
Prophylactic antibiotics are a reasonable option in patients with recurrent UTIs who do not wish to undergo behavioral interventions such as changing their mode of contraception or other behavioral modifications. Antibiotic prophylaxis should be considered especially in patients who suffer two or more symptomatic recurrent UTIs within 6 months and/or three or more within 12 months period [88]. Antibiotic prophylaxis in patients with these characteristics has been proven to be an effective way of preventing recurrent UTIs [89]. Nevertheless, due to the concern for increasing antibacterial resistance , prophylactic antibiotics should be used conservatively. They should be reserved for patients exhibiting discomfort and more serious UTIs.
Conclusion/Summary
Urinary tract infection is defined as a combination of symptoms and positive urine culture containing at minimal 105 colony forming units per milliliter of urine with isolation of less than two microorganisms in a patient without a bladder catheter.
On the other hand, catheter-associated urinary tract infection must contain at least 103 CFU/mL, with the urine sample obtained by an aseptic technique.
Asymptomatic bacteriuria is defined as isolation of a significant count of bacteria in an appropriately collected urine specimen from a patient without any signs or symptoms of UTI.
Urinary tract infection is considered complicated when it is associated with other conditions that increase the risk of treatment failure. Such conditions include diabetes, pregnancy, symptoms lasting 1 week or longer prior to starting medical treatment, hospital-acquired infections, urinary tract obstruction, presence of hardware, recent instrumentation, functional or anatomical abnormality, history of childhood UTIs, and renal transplantation.
The prevalence of asymptomatic bacteriuria among healthy women tends to increase with age. Symptomatic UTIs are more prevalent in sexually active young women. Prevalence of UTIs is three-to-fourfold higher in diabetic women.
Asymptomatic bacteriuria is rare among young healthy men, and the incidence of symptomatic UTIs is much lower than that in women.
Pyelonephritis is a more serious infection than cystitis as it includes the upper urinary tract infection involving the kidney(s).
Some of the strong independent etiologic risk factors for UTIs include history of recurrent UTIs, receptive sexual intercourse, and diaphragm-spermicide use. Other risk factors include, having first UTI before the age of 15, diabetes, anatomical or functional urinary tract abnormalities, indwelling urinary catheters, and recent instrumentation.
Among uropathogens, E. coli is the most commonly implicated uropathogen responsible for majority of UTIs. Severity of infections depends on variety of host factors, virulence, and antibiotic resistance properties of uropathogens.
Patients with symptomatic cystitis could present with a variety of symptoms including dysuria, increased urinary frequency, urgency, suprapubic pain/discomfort, and hematuria.
Patients with pyelonephritis on the contrary may or may not present with symptoms commonly associated with cystitis but may exhibit fever, chills, flank pain, costovertebral angle tenderness, nausea, and/or vomiting.
Clinical history is immensely important in diagnosis of uncomplicated cystitis or pyelonephritis. Laboratory studies with urinalysis and urine culture also provide valuable information in diagnosis and treatment of UTIs. Routine imaging studies are not indicated for diagnosing acute uncomplicated cystitis but may be required in certain complicated cases and pyelonephritis.
Treatment of UTI is based on the severity of the infection. Appropriate antibiotic regimen is selected based on whether it is cystitis or pyelonephritis.
Treatment of acute cystitis further depends on resistance profiles of uropathogens, efficacy of selected antimicrobial agent along with its side effect profile, drug availability, and cost. Treatment of pyelonephritis generally requires inpatient therapy with intravenous antibiotics.
Growing antibiotic resistance among uropathogens presents a special challenge when selecting antimicrobial agents.
Behavioral interventions may be helpful in reducing the risk of recurrent UTIs but may not be very practical and more studies are needed to prove their clinical efficacy.
Prophylactic antibiotics may be a reasonable option in patients with recurrent UTIs that do not wish to undergo behavioral interventions but because of concern for increasing antibacterial resistance, prophylactic antibiotics should be used conservatively.
References
www.cdc.gov/nhsn/pdfs/pscManual/7pscCAUTIcurrent.pdf. Accessed 04 Jan 2010.
Nicolle LE, Bradley S, Colgan R, Rice JC, Schaeffer A, Hooton TM. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis. 2005;40(5):643.
Stamm WE. Measurement of pyuria and its relation to bacteriuria. Am J Med. 1983;75(1B):53.
Hooton TM, Bradley SF, Cardenas DD, Colgan R, Geerlings SE, Rice JC, Saint S, Schaeffer AJ, Tambayh PA, Tenke P, Nicolle LE, Infectious Diseases Society of America. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010;50(5):625.
Hooton TM. Clinical practice. Uncomplicated urinary tract infection. N Engl J Med. 2012;366(11):1028–37. doi:10.1056/NEJMcp1104429.
Hooton TM, Scholes D, Hughes JP, Winter C, Roberts PL, Stapleton AE, Stergachis A, Stamm WE. A prospective study of risk factors for symptomatic urinary tract infection in young women. N Engl J Med. 1996;335(7):468.
Jackson SL, Boyko EJ, Scholes D, Abraham L, Gupta K, Fihn SD. Predictors of urinary tract infection after menopause: a prospective study. Am J Med. 2004;117(12):903.
Foxman B, Gillespie B, Koopman J, Zhang L, Palin K, Tallman P, Marsh JV, Spear S, Sobel JD, Marty MJ, Marrs CF. Risk factors for second urinary tract infection among college women. Am J Epidemiol. 2000;151(12):1194.
Hooton TM, Scholes D, Stapleton AE, Roberts PL, Winter C, Gupta K, Samadpour M, Stamm WE. A prospective study of asymptomatic bacteriuria in sexually active young women. N Engl J Med. 2000;343(14):992.
Kunin CM, McCormack RC. An epidemiologic study of bacteriuria and blood pressure among nuns and working women. N Engl J Med. 1968;278(12):635.
Nicolle LE. Asymptomatic bacteriuria: when to screen and when to treat. Infect Dis Clin North Am. 2003;17(2):367.
Boyko EJ, Fihn SD, Scholes D, Abraham L, Monsey B. Risk of urinary tract infection and asymptomatic bacteriuria among diabetic and nondiabetic postmenopausal women. Am J Epidemiol. 2005;161(6):557.
Stenqvist K, Sandberg T, Lidin-Janson G, Orskov F, Orskov I, Svanborg-Edén C. Virulence factors of Escherichia coli in urinary isolates from pregnant women. J Infect Dis. 1987;156(6):870.
Kaitz AL. Urinary concentrating ability in pregnant women with asymptomatic bacteriuria. J Clin Invest. 1961;40:1331.
Smaill F, Vazquez JC. Antibiotics for asymptomatic bacteriuria in pregnancy. Cochrane Database Syst Rev. 2007;18, CD000490.
Lipsky BA. Urinary tract infections in men. Epidemiology, pathophysiology, diagnosis, and treatment. Ann Intern Med. 1989;110(2):138.
Boscia JA, Kobasa WD, Knight RA, Abrutyn E, Levison ME, Kaye D. Epidemiology of bacteriuria in an elderly ambulatory population. Am J Med. 1986;80(2):208.
Sobel JD, Fisher JF, Kauffman CA, Newman CA. Candida urinary tract infections--epidemiology. Clin Infect Dis. 2011;52 Suppl 6:S433.
Richards MJ, Edwards JR, Culver DH, Gaynes RP. Nosocomial infections in medical intensive care units in the United States. National Nosocomial Infections Surveillance System. Crit Care Med. 1999;27(5):887.
Haley RW, Hooton TM, Culver DH, Stanley RC, Emori TG, Hardison CD, Quade D, Shachtman RH, Schaberg DR, Shah BV, Schatz GD. Nosocomial infections in U.S. hospitals, 1975–1976: estimated frequency by selected characteristics of patients. Am J Med. 1981;70(4):947.
Tambyah PA, Maki DG. Catheter-associated urinary tract infection is rarely symptomatic: a prospective study of 1,497 catheterized patients. Arch Intern Med. 2000;160(5):678.
Alangaden GJ, Thyagarajan R, Gruber SA, Morawski K, Garnick J, El-Amm JM, West MS, Sillix DH, Chandrasekar PH, Haririan A. Infectious complications after kidney transplantation: current epidemiology and associated risk factors. Clin Transplant. 2006;20(4):401.
de Souza RM, Olsburgh J. Urinary tract infection in the renal transplant patient. Nat Clin Pract Nephrol. 2008;4(5):252.
Scholes D, Hooton TM, Roberts PL, Stapleton AE, Gupta K, Stamm WE. Risk factors for recurrent urinary tract infection in young women. J Infect Dis. 2000;182(4):1177.
Fihn SD, Boyko EJ, Normand EH, Chen CL, Grafton JR, Hunt M, Yarbro P, Scholes D, Stergachis A. Association between use of spermicide-coated condoms and Escherichia coli urinary tract infection in young women. Am J Epidemiol. 1996;144(5):512.
Gupta K, Stamm WE. Pathogenesis and management of recurrent urinary tract infections in women. World J Urol. 1999;17(6):415.
Huang JJ, Tseng CC. Emphysematous pyelonephritis: clinicoradiological classification, management, prognosis, and pathogenesis. Arch Intern Med. 2000;160(6):797.
Raz R, Gennesin Y, Wasser J, Stoler Z, Rosenfeld S, Rottensterich E, Stamm WE. Recurrent urinary tract infections in postmenopausal women. Clin Infect Dis. 2000;30(1):152.
Hooton TM, Stamm WE. Diagnosis and treatment of uncomplicated urinary tract infection. Infect Dis Clin North Am. 1997;11(3):551.
Platt R, Polk BF, Murdock B, Rosner B. Risk factors for nosocomial urinary tract infection. Am J Epidemiol. 1986;124(6):977.
Echols RM, Tosiello RL, Haverstock DC, Tice AD. Demographic, clinical, and treatment parameters influencing the outcome of acute cystitis. Clin Infect Dis. 1999;29(1):113.
Warren JW. Catheter-associated urinary tract infections. Infect Dis Clin North Am. 1987;1(4):823.
Hildebrand TS, Nibbe L, Frei U, Schindler R. Bilateral emphysematous pyelonephritis caused by Candida infection. Am J Kidney Dis. 1999;33(2), E10.
Valera B, Gentil MA, Cabello V, Fijo J, Cordero E, Cisneros JM. Epidemiology of urinary infections in renal transplant recipients. Transplant Proc. 2006;38(8):2414.
Krcmery S, Dubrava M, Krcmery Jr V. Fungal urinary tract infections in patients at risk. Int J Antimicrob Agents. 1999;11(3–4):289–91.
Nielubowicz GR, Mobley HL. Host-pathogen interactions in urinary tract infection. Nat Rev Urol. 2010;7:430–41.
Stapleton AE. Infect Dis Clin Nor Am. 2013. doi:10.1016/j.idc.2013.10.006.
Sweet RL. Bacteriuria and pyelonephritis during pregnancy. Semin Perinatol. 1977;1(1):25.
Russo TA, Stapleton A, Wenderoth S, Hooton TM, Stamm WE. Chromosomal restriction fragment length polymorphism analysis of Escherichia coli strains causing recurrent urinary tract infections in young women. J Infect Dis. 1995;172(2):440.
Stamm WE, McKevitt M, Roberts PL, White NJ. Natural history of recurrent urinary tract infections in women. Rev Infect Dis. 1991;13(1):77.
Schaeffer AJ, Jones JM, Falkowski WS, Duncan JL, Chmiel JS, Plotkin BJ. Variable adherence of uropathogenic Escherichia coli to epithelial cells from women with recurrent urinary tract infection. J Urol. 1982;128(6):1227.
Sheinfeld J, Schaeffer AJ, Cordon-Cardo C, Rogatko A, Fair WR. Association of the Lewis blood-group phenotype with recurrent urinary tract infections in women. N Engl J Med. 1989;320(12):773.
Godaly G, Proudfoot AE, Offord RE, Svanborg C, Agace WW. Role of epithelial interleukin-8 (IL-8) and neutrophil IL-8 receptor A in Escherichia coli-induced transuroepithelial neutrophil migration. Infect Immun. 1997;65(8):3451.
Roos V, Nielsen EM, Klemm P. Asymptomatic bacteriuria Escherichia coli strains: adhesins, growth and competition. FEMS Microbiol Lett. 2006;262(1):22.
Roos V, Schembri MA, Ulett GC, Klemm P. Asymptomatic bacteriuria Escherichia coli strain 83972 carries mutations in the foc locus and is unable to express F1C fimbriae. Microbiology. 2006;152(Pt 6):1799.
Klemm P, Hancock V, Schembri MA. Mellowing out: adaptation to commensalism by Escherichia coli asymptomatic bacteriuria strain 83972. Infect Immun. 2007;75(8):3688.
Fischer H, Yamamoto M, Akira S, Beutler B, Svanborg C. Mechanism of pathogen-specific TLR4 activation in the mucosa: fimbriae, recognition receptors and adaptor protein selection. Eur J Immunol. 2006;36(2):267.
Mulvey MA. Adhesion and entry of uropathogenic Escherichia coli. Cell Microbiol. 2002;4(5):257.
Reid G, van der Mei HC, Tieszer C, Busscher HJ. Uropathogenic Escherichia coli adhere to urinary catheters without using fimbriae. FEMS Immunol Med Microbiol. 1996;16(3–4):159.
Oelschlaeger TA, Dobrindt U, Hacker J. Virulence factors of uropathogens. Curr Opin Urol. 2002;12(1):33.
Johnson JR. Virulence factors in Escherichia coli urinary tract infection. Clin Microbiol Rev. 1991;4(1):80.
Johnson JR, Roberts PL, Stamm WE. P fimbriae and other virulence factors in Escherichia coli urosepsis: association with patients’ characteristics. J Infect Dis. 1987;156(1):225.
Servin AL. Pathogenesis of Afa/Dr diffusely adhering Escherichia coli. Clin Microbiol Rev. 2005;18(2):264.
Valle J, Mabbett AN, Ulett GC, Toledo-Arana A, Wecker K, Totsika M, Schembri MA, Ghigo JM, Beloin C. UpaG, a new member of the trimeric autotransporter family of adhesins in uropathogenic Escherichia coli. J Bacteriol. 2008;190(12):4147.
Le Bouguénec C, Lalioui L, du Merle L, Jouve M, Courcoux P, Bouzari S, Selvarangan R, Nowicki BJ, Germani Y, Andremont A, Gounon P, Garcia MI. Characterization of AfaE adhesins produced by extraintestinal and intestinal human Escherichia coli isolates: PCR assays for detection of Afa adhesins that do or do not recognize Dr blood group antigens. J Clin Microbiol. 2001;39(5):1738.
Meyrier A, Condamin MC, Fernet M, Labigne-Roussel A, Simon P, Callard P, Rainfray M, Soilleux M, Groc A. Frequency of development of early cortical scarring in acute primary pyelonephritis. Kidney Int. 1989;35(2):696.
Floyd RV, et al. Escherichia coli-mediated impairment of ureteric contractility is uropathogenic E. coli specific. J Infect Dis. 2012;206(10):1589–96.
Schulz WA. Uropathogenic bacteria leave a mark. Lab Invest. 2011;91(6):816–8.
Mobley HL, Island MD, Massad G. Virulence determinants of uropathogenic Escherichia coli and Proteus mirabilis. Kidney Int Suppl. 1994;47:S129.
Latham RH, Running K, Stamm WE. Urinary tract infections in young adult women caused by Staphylococcus saprophyticus. JAMA. 1983;250(22):3063.
Barnes JL, Osgood RW, Lee JC, King RD, Stein JH. Host-parasite interactions in the pathogenesis of experimental renal candidiasis. Lab Invest. 1983;49(4):460.
Nickel JC, Costerton JW, McLean RJ, Olson M. Bacterial biofilms: influence on the pathogenesis, diagnosis and treatment of urinary tract infections. J Antimicrob Chemother. 1994;33(Suppl A):31.
Schaberg DR, Haley RW, Highsmith AK, Anderson RL, McGowan Jr JE. Nosocomial bacteriuria: a prospective study of case clustering and antimicrobial resistance. Ann Intern Med. 1980;93(3):420.
Bent S, Nallamothu BK, Simel DL, Fihn SD, Saint S. Does this woman have an acute uncomplicated urinary tract infection? JAMA. 2002;287(20):2701.
Lehner T. Systemic candidiasis and renal involvement. Lancet. 1964;1(7348):1414.
Ramsey DE, Finch WT, Birtch AG. Urinary tract infections in kidney transplant recipients. Arch Surg. 1979;114(9):1022–5.
Wilson ML, Gaido L. Laboratory diagnosis of urinary tract infections in adult patients. Clin Infect Dis. 2004;38:1150.
Pappas PG. Laboratory in the diagnosis and management of urinary tract infections. Med Clin North Am. 1991;75:313.
Eisenstadt J, Washington JA. Diagnostic microbiology for bacteria and yeasts causing urinary tract infections. In: Mobley HL, Warren JW, editors. UTIs: Molecular pathogenesis and clinical management. Washington: ASM Press; 1996. p. 29.
Warren JW, Abrutyn E, Hebel JR, et al. Guidelines for antimicrobial treatment of uncomplicated acute bacterial cystitis and acute pyelonephritis in women. Infectious Diseases Society of America (IDSA). Clin Infect Dis. 1999;29:745.
Gupta K, Hooton TM, Stamm WE. Increasing antimicrobial resistance and the management of uncomplicated community-acquired urinary tract infections. Ann Intern Med. 2001;135:41.
Gupta K, Hooton TM, Naber KG, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011; 52:e103.
McKinnell JA, Stollenwerk NS, Jung CW, Miller LG. Nitrofurantoin compares favorably to recommended agents as empirical treatment of uncomplicated urinary tract infections in a decision and cost analysis. Mayo Clin Proc. 2011;86:480.
Arredondo-García JL, Figueroa-Damián R, Rosas A, et al. Comparison of short-term treatment regimen of ciprofloxacin versus long-term treatment regimens of trimethoprim/sulfamethoxazole or norfloxacin for uncomplicated lower urinary tract infections: a randomized, multicentre, open-label, prospective study. J Antimicrob Chemother. 2004;54:840.
Stein GE. Comparison of single-dose fosfomycin and a 7-day course of nitrofurantoin in female patients with uncomplicated urinary tract infection. Clin Ther. 1999;21:1864.
Fosfomycin for urinary tract infections. Med Lett Drugs Ther. 1997; 39:66.
Ferry SA, Holm SE, Stenlund H, et al. Clinical and bacteriological outcome of different doses and duration of pivmecillinam compared with placebo therapy of uncomplicated lower urinary tract infection in women: the LUTIW project. Scand J Prim Health Care. 2007;25:49.
Ward G, Jorden RC, Severance HW. Treatment of pyelonephritis in an observation unit. Ann Emerg Med. 1991;20:258.
Sanchez GV, Master RN, Karlowsky JA, Bordon JM. In vitro antimicrobial resistance of urinary Escherichia coli isolates among U.S. outpatients from 2000 to 2010. Antimicrob Agents Chemother. 2012;56:2181.
Pitout JD. Infections with extended-spectrum beta-lactamase-producing enterobacteriaceae: changing epidemiology and drug treatment choices. Drugs. 2010;70:313.
Mombelli G, Pezzoli R, Pinoja-Lutz G, et al. Oral vs intravenous ciprofloxacin in the initial empirical management of severe pyelonephritis or complicated urinary tract infections: a prospective randomized clinical trial. Arch Intern Med. 1999;159:53.
Krieger JN, Ross SO, Simonsen JM. Urinary tract infections in healthy university men. J Urol. 1993;149:1046.
Zhanel GG, Hisanaga TL, Laing NM, et al. Antibiotic resistance in Escherichia coli outpatient urinary isolates: final results from the North American Urinary Tract Infection Collaborative Alliance (NAUTICA). Int J Antimicrob Agents. 2006;27:468.
Swami SK, Liesinger JT, Shah N, et al. Incidence of antibiotic-resistant Escherichia coli bacteriuria according to age and location of onset: a population-based study from Olmsted County. Minnesota Mayo Clin Proc. 2012;87:753.
Sobota AE. Inhibition of bacterial adherence by cranberry juice: potential use for the treatment of urinary tract infections. J Urol. 1984;131:1013.
Avorn J, Monane M, Gurwitz JH, et al. Reduction of bacteriuria and pyuria after ingestion of cranberry juice. JAMA. 1994;271:751.
Stapleton AE, Dziura J, Hooton TM, et al. Recurrent urinary tract infection and urinary Escherichia coli in women ingesting cranberry juice daily: a randomized controlled trial. Mayo Clin Proc. 2012;87:143.
Ronald AR, Conway B. An approach to urinary tract infections in ambulatory women. Curr Clin Top Infect Dis. 1988;9:76.
Stamm WE, Hooton TM. Management of urinary tract infections in adults. N Engl J Med. 1993;329:1328.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Science+Business Media New York
About this chapter
Cite this chapter
Singh, R., Multani, A., Cmar, J. (2017). Microbiology of Virulence: Urinary Tract Infection Versus Colonization. In: Gordon, D., Katlic, M. (eds) Pelvic Floor Dysfunction and Pelvic Surgery in the Elderly. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-6554-0_6
Download citation
DOI: https://doi.org/10.1007/978-1-4939-6554-0_6
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-6552-6
Online ISBN: 978-1-4939-6554-0
eBook Packages: MedicineMedicine (R0)