Abstract
The aggregation, hyperphosphorylation, and accumulation of the microtubule-associated protein tau is a hallmark for several neurodegenerative diseases, including Alzheimer’s disease. These diseases are known as tauopathies. In tauopathies, the tau protein becomes hyperphosphorylated and forms intracellular neurofibrillary tangles visualized within dystrophic neurites and cell bodies. Evidence suggests that some tau aggregates can become extracellular where they potentially propagate between cells and induce tau pathology in previously unaffected cells. The amount of tau pathology correlates well with the load of neurofibrillary tangles, synaptic loss, and functional decline in humans as well as in transgenic mouse models of tauopathy. Several active and passive immunization studies targeting tau in transgenic mouse models have shown reduced tau pathology, although the mechanism(s) underlying these effects is not clear. In this chapter, we review the recent active and passive immunization strategies targeting tau in mouse models and our understanding of potential mechanisms underlying the effects seen.
Access provided by CONRICYT – Journals CONACYT. Download protocol PDF
Similar content being viewed by others
Key words
1 Tau Protein and Neurodegenerative Disease
The microtubule-associated protein tau stabilizes microtubules and promotes axonal transport. In neurons, it is found mainly in axons, but it is also expressed in astrocytes and oligodendrocytes. In the adult human brain, tau is encoded by the gene MAPT (microtubule-associated protein tau) on chromosome 17q21. It has six splice isoforms. The presence or absence of exons 2 and 3, encode a region in the N-terminus, creating 0, 1, or 2N regions. Exon 10 encodes one of four microtubule binding repeat sequences, and its presence or absence creates 4 repeat (4R) or 3 repeat (3R) tau [1, 2]. Tau is thus referred to by the number of N and R sequences, e.g., 1N3R.
Aggregation and accumulation of amyloid-β (Aβ) and tau are pathological hallmarks of Alzheimer’s disease (AD). In the disease, specific posttranslational modifications of tau occur. Hyperphosphorylation and hyperacetylation are described in aggregated forms of tau, such as neurofibrillary tangles (NFTs) , although it is not clear if these are primary or secondary events in the process of tau aggregation. In normal aging, NFTs containing tau occur in virtually all brains in certain regions, including CA1 of the hippocampus and entorhinal cortex. However, after Aβ deposition begins to occur in the neocortex , the process is associated with progression of tauopathy to the neocortex in AD [3]. Strong data supports the idea that Aβ aggregation somehow drives progression of tau aggregation and its associated neurodegeneration that occurs in AD, but the mechanism is unknown. In certain forms of frontotemporal dementia (FTD), progressive supranuclear palsy (PSP), corticobasal degeneration (CBD), and Pick’s disease, tau aggregates and forms NFTs and is hyperphosphorylated even in the absence of Aβ aggregation [4]. In some inherited cases of FTD, mutations in the MAPT gene also cause tau aggregation, NFTs, and tau hyperphosphorylation. These diseases are collectively termed tauopathies [4].
2 Active Immunization with Tau Peptides
Analogous to targeting of Aβ [5], multiple active and passive immunization strategies against tau have been tested in mouse models of tauopathy. The data from these studies are summarized in Tables 1 and 2. In initial active immunization studies on tau, investigators immunized wild-type female C57Bl/6 mice expressing only murine tau with recombinant human tau protein administered intraperitoneally. This caused encephalomyelitis accompanied by the formation of apparent NFTs in wild-type mice [6]. True NFTs have typically not been found in wild-type mice in the absence of human tau expression. The same group then used a human transgenic tau model expressing double mutant K257T/P301S tau alone in which one-half of the animals had induced inflammation at 6–7 weeks of age by administration of myelin oligodendrocyte glycoprotein. These two groups were subcutaneously injected at 4 months of age with three tau peptides mixed together—(Tau195-213 [P202/205], Tau207-220 [P212/214], and Tau224-238 [P231])—that contained phosphorylation sites recognized by the AT8, AT100, and AT180 monoclonal antibodies that stain pathological tau. Immunized mice showed decreased tau pathology and neurofibrillary tangle burden by Gallyas staining, and decreased phosphorylated forms of tau as recognized by immunostaining with the AT8 and AT180 antibodies. In addition, immunized mice showed increased lectin positive microglial staining compared to controls. The astrocytic burden was unaffected [7].
In another study, phospho-tau peptide (Amino acids 379–408, with pSer 396 and 404) containing the PHF1 phospho-tau epitope antibody), was subcutaneously injected in the JNPL3 (P301L tau transgenic mouse) model. Control mice received aluminum adjuvant alone. One group of mice was treated from 2 until 5 months of age and another group from 2 until 8 months of age. At the end of the treatment, both 5 and 8 month old mice went through a battery of sensorimotor tests before sacrifice. Quantitative immunostaining with the anti-tau antibodies MC1 and PHF1 showed reduced tau pathology in the dentate gyrus, motor cortex, and brainstem regions. Western blotting showed increased soluble phospho-tau and no difference in insoluble phospho-tau. Treated mice showed improvement in rotarod, transverse beam, and maximum velocity tests. This treatment was more effective at the earlier time point of 5 months of age as compared to the later 8 month time point [8]. The same group also immunized mice expressing human tau under the control of the normal tau promoter that were crossed with PS1 transgenic mice (htau/PS1) mice [9]. Mice were immunized with the tau peptide 379–408 containing the PHF1 tau antibody epitope pSer 396 and 404. The htau/PS1 mice were obtained by crossing htau mice expressing all 6 isoforms of tau on a mouse tau knockout background [10] with a model carrying the M146L presenilin mutation that causes a form of dominantly inherited AD [11]. The mice received intraperitoneal injections , with three injections every 2 weeks beginning at 3–4 months of age with subsequent administration at monthly intervals. Control groups received aluminum adjuvant alone. Immunotherapy reduced PHF1 reactive tau pathology compared to controls as assessed by immunostaining in the piriform cortex. Soluble PHF1 reactive tau levels were decreased by Western blot, but there was no difference in insoluble phospho-tau levels compared to controls. No difference in microgliosis or astrogliosis was noted. However immunized mice showed improvement in the radial arm maze and closed field symmetrical maze tests compared to control groups [9].
In another study, pR5 mice that express human P301L tau under the control of Thy 1.2 promoter were immunized with a 12 amino acid peptide of Tau 395–406 containing the PHF1 epitope pS396 and pS404. Three different age groups of 4, 8 and 18 months of age were immunized intraperitoneally with tau peptide linked to keyhole limpet hemocyanin (KLH) . Tau-KLH was dissolved in PBS and emulsified with complete or incomplete Freund’s adjacent at 1:1 ratio. Control mice received KLH with complete Freund’s adjacent. Immunostaining showed reduced phosphorylated tau in the amygdala and CA1 regions. In addition, increased astrogliosis was observed in older age group mice. No anti-tau antibodies were found inside neurons of treated pR5 mice [12].
Troquier et al. used THY-Tau22 transgenic mice, which develop hippocampal neurofibrillary tangle-like inclusions at 3–6 months of age. Tau peptide vaccine containing phospho-Ser422 was injected peritoneally at 3 months of age. Control mice received adjuvant alone. The first two injections were administered every 2 weeks, followed by injections given monthly. There was no effect on phosphorylated tau species stained by the anti-tau antibodies AT100 and pS422 in the hippocampal CA1 region. In the biochemical analysis, insoluble tau was decreased by AT100 and pS422 detection. Following active immunization, an increase in tau levels was observed in the blood. Cognitive improvement was also observed in immunized mice in the Y-maze test [13]. Taken together, active immunization with different tau peptides has reduced tau pathology and improved behavior in human tau transgenic mice. However, compared to results with Aβ vaccination, the effects on pathology and behavior do not appear to be as strong, and the underlying mechanism(s) remains unknown.
3 Passive Immunization by Using Anti-Tau Antibodies
In an initial passive immunization study, JNPL3 and P301S tau transgenic mice (at age 2–3 months, prior to the onset of tau pathology) were administered the PHF1 anti-tau monoclonal antibody [14] or the conformation specific antibody MC1 [15] intraperitoneally at 15 mg/kg three times a week for 2 months followed by 10 mg/kg twice a week for the next 2 months. P301S mice were given 15 mg/kg of antibody twice weekly. PHF1 recognizes phospho tau at pSer396/404 on both normal tau and disease-associated tau. MC1 recognizes tau only in a pathological conformation. Both treatments reduced insoluble tau levels [16]. Phospho-tau was reduced in both the brainstem and spinal cord. Treated mice showed improvement in the rotarod test. No alteration in activation of microglia or astrocytes was observed in treated vs. control mice [16]. In another passive immunization study with JNPL3 tau transgenic mice, the PHF1 antibody was intraperitoneally administered for 13 weeks from 2 to 3 months of age, i.e., prior to the onset of pathology in this model. As compared to IgG control treated mice, the tau antibody treated mice showed decreased PHF1 tau pathology in the dentate gyrus. While a decrease in insoluble phospho-tau was observed, there was no change in total insoluble tau levels as measured by Western blot. Treated mice also performed better in the transverse beam task, and similar degrees of micro- and astrogliosis was observed in treated vs. control mice [17].
In another study, d’Abramo et al. treated female JNPL3 mice animals with intraperitoneal injections of either the MC1 or DA31 anti-tau antibodies of 10 mg/kg weekly from 3 to 7 months of age and compared these with saline treated mice. Another group of mice received MC1 weekly from 7 to 10 months of age. P301L mice sacrificed at 7 months of age or treated with saline from 7 months until 10 months were used as control groups. The MC1 antibody reduced soluble and insoluble tau in the forebrain of P301L Tau mice compared to the DA31 treated mice. Mice treated with the MC1 antibody from 7 to 10 months showed decreased phospho-tau immunostaining as assessed by the anti-tau antibodies CP13 and RZ3 in the hippocampal CA1 region. In addition, decreased phosphorylated, insoluble tau was noted in the forebrain of treated mice [18].
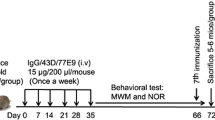
A recent study assessed the effects of that administration of a single dose of 1 or 30 μg of an anti-tau oligomeric monoclonal antibody (TOMA) by intracerebroventricular or intravenous injection in 8 month old JNPL3 mice. A control group received nonspecific IgG–rhodamine and wild type mice received saline injections. Four days after intracerebroventricular injection with TOMA, mice showed improved performance on the rotarod [19]. Tau oligomers were reduced as assessed by Western blot and immunofluorescence assays, with no change in monomeric tau. Four to six days after intravenous injection of the TOMA antibody there was improved performance of mice on both the rotarod and Y-maze task. The investigators also noted an increase in tau oligomers in the periphery following peripheral administration of TOMA [19].
Our group [20] hypothesized that anti-tau antibodies might function by blocking cell to cell spread of a pathological form of tau. We first screened antibodies that blocked the ability of extracellular tau aggregates to seed intracellular tau. We then chose antibodies with various efficacies in blocking tau seeding and tested them in vivo. P301S Tau transgenic mice were treated with one of three different anti-tau antibodies (HJ8.5, HJ9.3, and HJ9.4), a control antibody, or phosphate-buffered saline with infusion into the lateral ventricles for 3 months, beginning at 6 months of age. Each anti-tau antibody targets a different, non-phosphorylated tau epitope. Quantitative immunostaining showed that all three monoclonal anti-tau antibodies strongly reduced the abnormally phosphorylated tau stained by the AT8 phospho-tau antibody in different brain regions. Two of three anti-tau antibodies reduced insoluble tau levels from cortical brain tissues as assessed by biochemical analysis. This treatment also significantly reduced pathological seeding activity in the treated soluble brain lysates of P301S mice compared to control groups. Of the three antibodies tested, HJ8.5 and HJ9.4 significantly improved memory deficits in a conditioned fear test [20]. These experiments were consistent with a mechanism of action based on binding extracellular tau aggregates.
In a follow-up study, the most potent antibody, HJ8.5 in the prior study, was further studied assessed with peripheral administration (intraperitoneal). Two different doses of HJ8.5, 10 mg/kg or 50 mg/kg, were administered weekly to 6 month old male P301S mice for three months. HJ8.5 at 50 mg/kg strongly reduced insoluble tau levels compared to controls. Interestingly, both doses of antibody resulted in decreased cortical and hippocampal brain atrophy compared to the control treated P301S mice. Both doses of HJ8.5 treatment reduced hippocampal CA1 cell layer stained with the p-tau antibody AT8 as well as Thio-S positive tau aggregates in piriform cortex and amygdala. Mice treated with HJ8.5 at 50 mg/kg showed a decrease in motor/sensorimotor deficits compared to control group. Moreover, HJ8.5 treatment resulted in a dose-dependent increase of tau in plasma [21]. All the above studies support the idea that anti-tau antibodies should considered as a potential treatment for tauopathies.
4 Propagation of Tau
In AD and other tauopathies, tau pathology starts in a particular brain region and then progresses or spreads to other regions that are anatomically connected. Normally, monomeric tau is closely associated with microtubules. Yet monomeric tau under physiological conditions is released into both the interstitial fluid (ISF) and CSF, and tau aggregates may also be present in the ISF [22]. Tau antibodies that enter the CNS could thus be targeting extracellular tau aggregates as well as monomeric tau. What is the evidence that extracellular tau aggregates are important in disease pathogenesis? In cultured cells, tau aggregates can be released into the extracellular space, and these aggregates have been shown to be transferred to neighboring cells [23, 24]. In vivo injection of the brain extracts from human mutant P301S tau mice into the hippocampus and cerebral cortex of ALZ17 mice, which express the longest form of the wild type human four repeat isoform and never develop tau deposits, induced tau pathology, with spread of the pathology from sites of injection to neighboring brain regions [25]. Isolation of tau oligomers from Alzheimer’s disease brains by immunoprecipitation followed by injection into the wild type C57BL/6 mice was found to induce tau aggregation by seeding endogenous murine tau, and to induce tau pathology at distant sites after prolonged incubation [26]. Two independent research groups showed in similar animal models that by restricting the expression of P301L tau in the entorhinal cortex, tau aggregates spread to neighboring cells and also synaptically connected regions in the hippocampus [27, 28]. In young mice, tau pathology was limited to the entorhinal cortex. However, in aged mice, tau aggregates spread to the synaptically connected granular layer of the dentate gyrus, CA region of the hippocampus, and the cingulate cortex. Infusion of synthetic fibrils of recombinant full length human tau with P301S mutation into the hippocampus of the young P301S tau transgenic mice induced rapid formation of neurofibrillary tangle-like inclusions at the injection sites. The pathology spread to synaptically connected regions in a time and dose-dependent manner [29], although it is difficult to exclude spreading of the inoculum itself. Following injection of brain extract from tauopathies such as AD into the hippocampus and cerebral cortex of ALZ17 mice, there was induction of tau inclusions. Human tauopathy brain extracts injected into non-transgenic 3 month old C57BL/6 mice also resulted in the formation of tau inclusions. Furthermore, induced pathology in mouse brain could induce more pathology upon reinjection into a next generation of mice [30]. Finally, a recent study found that stably expressed tau repeat domain will propagate distinct amyloid conformations in a clonal fashion in culture [31]. Reintroduction of tau from these lines into naive cells reestablished identical clones. Further, the two “artificial” tau strains produced in vitro induced distinct pathologies in vivo as determined by successive inoculations into three generations of transgenic mice. Immunopurified tau from these mice created the original strains in culture. Finally, the cell culture system enabled isolation of multiple disease-associated strains from tauopathy patients. Together with other studies, this demonstrates that some form(s) of tau has essential characteristics of a prion. The studies above clearly indicate that tau aggregates formed in one region propagate a specific tau conformation to neighboring neuronal cells. It may be that certain anti-tau antibodies are able to block or decrease this process.
Tau seeding and spreading appears to be mediated by specific conformations of tau protein. For proteins that aggregate in neurodegenerative diseases, including tau, specific conformations may determine patterns of both spreading pathology and toxicity. Small aggregates of pathogenic proteins, termed oligomers , are generally more neurotoxic than the insoluble mature fibrils [32]. Therefore, it may be very important to target such species to create the most effective immunotherapy . As mentioned earlier, passive immunization studies targeting different phosphorylation or pathological forms of the tau have been shown to reduce tau pathology. However, most effects do not appear overly robust in animal models using this strategy, indicating that we need to better understand antibody mechanisms, particularly those of antibodies that have strong effects. The best treatment results to date appear to have been accomplished with anti-tau antibodies that do not specifically target a phosphorylated or acetylated form of tau but can recognize a host of different forms [20, 21]. To best design anti-tau immunotherapy approaches, understanding these effects will be critical.
5 Tau Species to Be Targeted
Tau is hyperphosphorylated in neurodegenerative conditions, and phosphorylated tau is present in paired helical filaments and NFTs. In a Drosophila model , it was shown that neurodegeneration occurs even in the absence of NFTs [33] and that the presence of NFTs in mouse neurons does not always mark dying or sick cells [34, 35]. It may be that particular aggregated forms of tau are key in eliciting neurodegeneration, but this is not known.
It has recently been shown that tau can misfold into specific conformational states and epigenetically propagate multiple amyloid conformations in clonal cell lines and in vivo [31]. Therefore, tau conformers can be in distinct tau aggregated forms or “strains” may predominate in patients with different types of tauopathies. Different tau antibodies are likely to differentially bind to these different strains or tau conformations. Therefore, in immunotherapy , a key may be to choose antibodies that can either target multiple conformations or to target very specific conformations associated with a particular disease. In both active and passive immunization, by selecting pathological forms of tau peptides in active immunization or utilizing antibodies targeting pathological tau or tau oligomers, there was reduction of tau pathology and also improvement in behavioral deficits in tau transgenic mouse models (Tables 1 and 2). Of the studies published to date, infusion of anti-tau antibodies directly into the lateral ventricle of the brain appear to have had the greatest effect in decreasing tau pathology versus other treatments in transgenic mice [20]. Interestingly, all the 3 anti-tau antibodies used in this study appeared to immunoprecipitate unique forms of tau species from brain lysates of transgenic mice as assessed by atomic force microscopy [20]. This indicates that different anti-tau antibodies may differentially recognize unique tau conformations. Depending on the location within the brain that such antibodies can access, the antibodies may sequester soluble or aggregated forms of tau in the extracellular or intracellular space and might also prevent monomeric tau from forming oligomeric or fibrillar species. While some studies suggest that anti-tau antibodies access the cytoplasm [17, 36, 37], this has not been observed in other studies [16, 18–20].
6 Potential Mechanism in Blocking Extracellular Tau Spread/Toxicity
In contrast to Aβ that is secreted and forms extracellular plaques, tau forms primarily intracellular amyloids. However, in vivo microdialysis indicates that tau is released from cells under physiological conditions. Moreover, tau is present in relatively high levels in the ISF of wild-type mice at concentrations of ~50 ng/ml—even in the absence of neurodegeneration or injury [22]. Studies from cultured cells have shown that certain forms of tau can escape cells and spread in a prion like manner to neighboring cells. Such secretion of tau into the extracellular space from neurons is independent of cell death [38, 39]. In addition, recent studies showed that tau release by neurons is regulated by excitatory neuronal activity [40, 41]. It is not yet clear whether under either normal or pathological conditions tau aggregates are also secreted into the brain extracellular space along with monomers via similar mechanisms. Once the tau aggregates are released from the cells into the extracellular space, they may sequester monomeric tau [22]. These extracellular aggregates could be taken up by adjacent cells or connected cells or may be taken up by the same cells and increase the intracellular burden of aggregated tau.
Blocking of tau aggregates that are more prone to initiate seeding activity in adjacent cells or promote the clearance of extracellular tau conformers by microglia, neurons, or other cells may be important mechanisms in tau immunotherapy. While the study by Yanamandra et al. (2013) suggests that anti-tau antibodies may block spreading of extracellular tau seeds from one cell to another, this has not yet been definitively proven. If an antibody is able to target forms of extracellular tau seeds or conformers, there can be several possible fates of the tau protein, as discussed in the following section. In addition, it is possible that extracellular forms of tau are toxic. Targeting these forms, independent of blocking spreading per se, could potentially lead to beneficial effects on synaptic/neuronal function.
7 Clearance of Tau and Tau Aggregates
7.1 Neurons
If an anti-tau antibody binds extracellular tau, the anti-tau antibody/tau complex might still be taken up by neurons. There are two main protein degradation systems present in cells (including neurons), namely the proteasomal and lysosomal systems. The proteasome mainly degrades soluble and short lived ubiquitinated proteins. Lysosome-mediated degradation mediates multiple mechanisms including macroautophagy [42]. Non-functional misfolded proteins can be cleared for the purpose of detoxification by either of these systems.
Certain neurons express high affinity FcγR1 receptors on their membrane [43, 44]. The low affinity Fc receptors FcγII and FcγIII are not expressed in neurons and are exclusively expressed in microglia in brain [44–46]. High affinity FcγRI receptors recognize the Fc domain of IgG and can initiate antibody uptake [47]. If the antibody enters the cytoplasm via this mechanism, it could then bind cytosolic tau aggregates and initiate its clearance by lysosomal pathways. In such a location, it could also theoretically bind to cytosolic antibody receptor TRIM21 and trigger antibody/tau degradation by the proteasome and initiate signaling pathways of the innate immune system [48, 49]. With the knowledge that tau can be present in the extracellular space, one study suggests that antibody bound to extracellular tau aggregates can be taken up by the neurons in a clathrin-dependent Fcγ receptor mediated endocytosis and further degraded by proteolytic enzymes in lysosomes [36, 37]. In contrast, recent studies using tau antibodies targeting extracellular tau species showed no detectable amount of uptake of anti-tau antibodies into neurons [18, 19] or non-neuronal cells in vitro [20]. Further in vitro and in vivo work will be required to sort out the role of neurons in uptake, degradation, and seeding of tau in the presence and absence of different anti-tau antibodies.
7.2 Microglia and Astrocytes
In neurodegenerative disease and other tauopathies, tau aggregation is linked to the activation of microglia and astrocytes in transgenic mouse models [50–54]. Microglia and astrocytes are phagocytic in nature. Once anti-tau antibodies in vivo sequester extracellular tau aggregates, their metabolic fate is not yet clear. Passive immunization with anti-Aβ antibodies has been noted to reduce microgliosis chronically [55] though acute application of anti-Aβ antibodies can lead to rapid microglial activation if the antibodies bind aggregated Aβ and have an intact Fc domain [56]. Microglia express low affinity FcγII and FcγIII receptors in the cytoplasm and on the surface of the cells. These receptors are not present on astrocytes. These receptors have the potential to recognize antibody/tau aggregate complexes and initiate the multiple immune effector pathways including antibody mediated cellular uptake, phagocytosis, and release of inflammatory mediators [57]. Antibody mediated clearance of extracellular α-synuclein was showed to occur mainly in microglia through Fcγ receptors and not in neuronal cells or astrocytes [46]. Certain antibodies against amyloid-β were shown to trigger microglial cells to clear plaques through Fc receptor-mediated phagocytosis and subsequent peptide degradation [58]. In temporal neocortex of Alzheimer’s patients, the size distribution of dense-core plaques was proportional to the microglial response but not to the astrocyte response. However, plaque-associated reactive astrocytes may be protecting neurons form surrounding plaques [59]. The role of astrocytes in tau pathology in the presence or absence of anti-tau antibodies is not yet clear. Astrocytes may be activated indirectly by antibody/tau complexes and activate microglial release of some inflammatory signals or cytokines.
In some anti-tau immunotherapies that have been tested by using anti-pathological tau antibodies, no change in activation of microglia or astrocytes was found [16, 17]. After 3 months of anti-tau antibody administration into tau transgenic mice, activated microglia were reduced in proportion to the reduction of tau pathology in treated mice [20]. This is also consistent with a study in which several months of passive immunization with anti-Aβ antibodies showed reduced Aβ plaques and reduced microgliosis [60]. In cases in which there is reduction of microgliosis upon passive administration of anti-tau antibodies, this could simply reflect lower levels of tau aggregation due to the anti-tau antibody therapy. In BV2-murine cultured immortalized microglial-like cells, anti-tau antibody increased the uptake of tau aggregates compared to control conditions. However, no difference in uptake of tau aggregates in presence or absence of anti-tau antibody was noted using primary neurons [21]. Using in vivo models, whether and how microglia and astrocytes play a role in anti-tau antibody mediated tau clearance still remains an open question.
7.3 Peripheral Sink and Cerebrospinal Fluid
Peripheral administration of anti-Aβ antibodies in PDAPP transgenic mice reduces Aβ burden. One mechanism that may account for part of this effect is by facilitating Aβ efflux or clearance from the brain to the periphery in a “peripheral sink” type of mechanism [61–63]. Anti-Aβ antibodies were also shown to sequester extracellular soluble Aβ in the central nervous system to potentially further block its aggregation [61, 64]. It is thought that antibodies cannot effectively penetrate cells and directly access cytoplasmic proteins under normal circumstances. In tau immunotherapy, it is also possible that anti-tau antibodies can sequester extracellular tau species effectively in the brain, not allowing prion-like spreading of tau to seed tau in adjacent cells. Antibodies to tau could thus promote tau monomer and aggregate clearance via binding to tau in the extracellular space and promoting efflux of tau antibody/tau complexes via the brain ISF and CSF into the periphery [65, 66]. It is also possible that anti-tau antibody in the periphery could accelerate CNS to plasma efflux of tau via bulk flow or blood–brain barrier mediated mechanisms as proposed with the peripheral sink Aβ hypothesis. As the mechanism(s) by which tau can exit the CNS to the periphery have not yet been worked out, future experiments will need to address these issues.
8 Summary
Active and passive immunization of tau has shown promising results in reducing tau pathology and improving brain dysfunction, indicating that these approaches should be further considered as therapeutic strategies for tauopathies. In immunotherapy studies, tau antibodies may be targeting tau species in either the extracellular or intracellular space and promoting tau clearance by multiple pathways. Extracellular tau clearance may be mediated by microglial, astrocytic, or neuronal mediated uptake followed by lysosomal degradation. It is also interesting to consider the possibility of antibody mediated clearance of tau monomer and aggregate via CSF and ISF flow into the periphery, as well as tau clearance via a “peripheral sink” mechanism. In this scenario, antibodies could promote tau efflux into the peripheral blood stream without requiring antibody entry into the CNS. We have summarized several possible mechanisms of anti-tau antibody-mediated clearance of tau in Fig. 1. While studies suggest that some of these mechanisms may be operative, it is not yet clear which of these is the most important. We suggest that the choice of antibody is likely critical to see the best possible efficacy. Our own data suggests that targeting all forms of tau species and blocking the prion-like propagation of pathological forms of tau into adjacent cells may be most important. However, much more work needs to be done in this area to better understand the underlying mechanism(s) of these potentially very promising effects.
Possible clearance mechanisms of tau aggregates by antibodies : In disease conditions, different forms of tau aggregates can be released into the extracellular space and propagate into neighboring cells to induce the aggregation of intracellular tau (Shown in left panel). Under therapeutic conditions (right panel), anti-tau antibodies trap tau aggregates in the extracellular space and induce clearance by different mechanisms, possibly via astrocytes (A), microglia (B) or neuronal mediated clearance mechanisms (C). (D) Anti-tau antibodies could also promote efflux of tau from central nervous system by crossing the blood–brain barrier and binding tau in the CNS, promoting clearance via ISF/CSF flow ultimately into the plasma. It is also possible that anti-tau antibodies present in the blood can somehow increase the normal efflux of tau from CNS to plasma
References
Goode BL, Feinstein SC (1994) Identification of a novel microtubule binding and assembly domain in the developmentally regulated inter-repeat region of tau. J Cell Biol 124(5):769–782
Gustke N, Trinczek B, Biernat J, Mandelkow EM, Mandelkow E (1994) Domains of tau protein and interactions with microtubules. Biochemistry 33(32):9511–9522
Musiek ES, Holtzman DM (2012) Origins of Alzheimer’s disease: reconciling cerebrospinal fluid biomarker and neuropathology data regarding the temporal sequence of amyloid-beta and tau involvement. Curr Opin Neurol 25(6):715–720. doi:10.1097/WCO.0b013e32835a30f4
Mandelkow EM, Mandelkow E (2012) Biochemistry and cell biology of tau protein in neurofibrillary degeneration. Cold Spring Harb Perspect Med 2(7):a006247. doi:10.1101/cshperspect.a006247, Pii: a006247
Brody DL, Holtzman DM (2008) Active and passive immunotherapy for neurodegenerative disorders. Annu Rev Neurosci 31:175–193. doi:10.1146/annurev.neuro.31.060407.125529
Rosenmann H, Grigoriadis N, Karussis D, Boimel M, Touloumi O, Ovadia H, Abramsky O (2006) Tauopathy-like abnormalities and neurologic deficits in mice immunized with neuronal tau protein. Arch Neurol 63(10):1459–1467. doi:10.1001/archneur.63.10.1459, Pii: 63/10/145
Boimel M, Grigoriadis N, Lourbopoulos A, Haber E, Abramsky O, Rosenmann H (2010) Efficacy and safety of immunization with phosphorylated tau against neurofibrillary tangles in mice. Exp Neurol 224(2):472–485. doi:10.1016/j.expneurol.2010.05.010, Pii: S0014-4886(10)00168-8
Asuni AA, Boutajangout A, Quartermain D, Sigurdsson EM (2007) Immunotherapy targeting pathological tau conformers in a tangle mouse model reduces brain pathology with associated functional improvements. J Neurosci 27(34):9115–9129. doi:10.1523/JNEUROSCI.2361-07.2007, pii:27/34/9115
Boutajangout A, Quartermain D, Sigurdsson EM (2010) Immunotherapy targeting pathological tau prevents cognitive decline in a new tangle mouse model. J Neurosci 30(49):16559–16566. doi:10.1523/JNEUROSCI.4363-10.2010, pii: 30/49/16559
Andorfer C, Acker CM, Kress Y, Hof PR, Duff K, Davies P (2005) Cell-cycle reentry and cell death in transgenic mice expressing nonmutant human tau isoforms. J Neurosci 25(22):5446–5454. doi:10.1523/JNEUROSCI.4637-04.2005, pii: 25/22/5446
Duff K, Eckman C, Zehr C, Yu X, Prada CM, Perez-tur J, Hutton M, Buee L, Harigaya Y, Yager D, Morgan D, Gordon MN, Holcomb L, Refolo L, Zenk B, Hardy J, Younkin S (1996) Increased amyloid-beta42(43) in brains of mice expressing mutant presenilin 1. Nature 383(6602):710–713. doi:10.1038/383710a0
Bi M, Ittner A, Ke YD, Gotz J, Ittner LM (2011) Tau-targeted immunization impedes progression of neurofibrillary histopathology in aged P301L tau transgenic mice. PLoS One 6(12), e26860. doi:10.1371/journal.pone.0026860, pii: PONE-D-11-15839
Troquier L, Caillierez R, Burnouf S, Fernandez-Gomez FJ, Grosjean ME, Zommer N, Sergeant N, Schraen-Maschke S, Blum D, Buee L (2012) Targeting phospho-Ser422 by active Tau immunotherapy in the THYTau22 mouse model: a suitable therapeutic approach. Curr Alzheimer Res 9(4):397–405, doi:CAR-EPUB-20120123-019 [pii]
Otvos L Jr, Feiner L, Lang E, Szendrei GI, Goedert M, Lee VM (1994) Monoclonal antibody PHF-1 recognizes tau protein phosphorylated at serine residues 396 and 404. J Neurosci Res 39(6):669–673. doi:10.1002/jnr.490390607
Jicha GA, Weaver C, Lane E, Vianna C, Kress Y, Rockwood J, Davies P (1999) cAMP-dependent protein kinase phosphorylations on tau in Alzheimer’s disease. J Neurosci 19(17):7486–7494
Chai X, Wu S, Murray TK, Kinley R, Cella CV, Sims H, Buckner N, Hanmer J, Davies P, O’Neill MJ, Hutton ML, Citron M (2011) Passive immunization with anti-Tau antibodies in two transgenic models: reduction of Tau pathology and delay of disease progression. J Biol Chem 286(39):34457–34467. doi:10.1074/jbc.M111.229633, pii: M111.229633
Boutajangout A, Ingadottir J, Davies P, Sigurdsson EM (2011) Passive immunization targeting pathological phospho-tau protein in a mouse model reduces functional decline and clears tau aggregates from the brain. J Neurochem 118(4):658–667. doi:10.1111/j.1471-4159.2011.07337.x
d’Abramo C, Acker CM, Jimenez HT, Davies P (2013) Tau passive immunotherapy in mutant P301L mice: antibody affinity versus specificity. PLoS One 8(4):e62402. doi:10.1371/journal.pone.0062402, pii: PONE-D-13-01397
Castillo-Carranza DL, Sengupta U, Guerrero-Munoz MJ, Lasagna-Reeves CA, Gerson JE, Singh G, Estes DM, Barrett AD, Dineley KT, Jackson GR, Kayed R (2014) Passive immunization with Tau oligomer monoclonal antibody reverses tauopathy phenotypes without affecting hyperphosphorylated neurofibrillary tangles. J Neurosci 34(12):4260–4272. doi:10.1523/JNEUROSCI.3192-13.2014, pii: 34/12/4260
Yanamandra K, Kfoury N, Jiang H, Mahan TE, Ma S, Maloney SE, Wozniak DF, Diamond MI, Holtzman DM (2013) Anti-tau antibodies that block tau aggregate seeding in vitro markedly decrease pathology and improve cognition in vivo. Neuron 80(2):402–414. doi:10.1016/j.neuron.2013.07.046, pii: S0896-6273(13)00670-3
Yanamandra K, Jiang H, Mahan TE, Maloney SE, Wozniak DF, Diamond MI, Holtzman DM (2015) Anti-tau antibody reduces insoluble tau and decreases brain atrophy. Ann Clin Transl Neurol 2(3):278–288. doi:10.1002/acn3.176
Yamada K, Cirrito JR, Stewart FR, Jiang H, Finn MB, Holmes BB, Binder LI, Mandelkow EM, Diamond MI, Lee VM, Holtzman DM (2011) In vivo microdialysis reveals age-dependent decrease of brain interstitial fluid tau levels in P301S human tau transgenic mice. J Neurosci 31(37):13110–13117. doi:10.1523/JNEUROSCI.2569-11.2011, pii: 31/37/13110
Guo JL, Lee VM (2011) Seeding of normal Tau by pathological Tau conformers drives pathogenesis of Alzheimer-like tangles. J Biol Chem 286(17):15317–15331. doi:10.1074/jbc.M110.209296, pii: M110.209296
Frost B, Jacks RL, Diamond MI (2009) Propagation of tau misfolding from the outside to the inside of a cell. J Biol Chem 284(19):12845–12852. doi:10.1074/jbc.M808759200, pii: M808759200
Clavaguera F, Bolmont T, Crowther RA, Abramowski D, Frank S, Probst A, Fraser G, Stalder AK, Beibel M, Staufenbiel M, Jucker M, Goedert M, Tolnay M (2009) Transmission and spreading of tauopathy in transgenic mouse brain. Nat Cell Biol 11(7):909–913. doi:10.1038/ncb1901, pii: ncb1901
Lasagna-Reeves CA, Castillo-Carranza DL, Sengupta U, Guerrero-Munoz MJ, Kiritoshi T, Neugebauer V, Jackson GR, Kayed R (2012) Alzheimer brain-derived tau oligomers propagate pathology from endogenous tau. Sci Rep 2:700. doi:10.1038/srep00700
Liu L, Drouet V, Wu JW, Witter MP, Small SA, Clelland C, Duff K (2012) Trans-synaptic spread of tau pathology in vivo. PLoS One 7(2), e31302. doi:10.1371/journal.pone.0031302, pii: PONE-D-11-23353
de Calignon A, Polydoro M, Suarez-Calvet M, William C, Adamowicz DH, Kopeikina KJ, Pitstick R, Sahara N, Ashe KH, Carlson GA, Spires-Jones TL, Hyman BT (2012) Propagation of tau pathology in a model of early Alzheimer’s disease. Neuron 73(4):685–697. doi:10.1016/j.neuron.2011.11.033, pii: S0896-6273(12)00038-4
Iba M, Guo JL, McBride JD, Zhang B, Trojanowski JQ, Lee VM (2013) Synthetic Tau fibrils mediate transmission of neurofibrillary tangles in a transgenic mouse model of Alzheimer’s-like tauopathy. J Neurosci 33(3):1024–1037. doi:10.1523/JNEUROSCI.2642-12.2013, pii: 33/3/1024
Clavaguera F, Akatsu H, Fraser G, Crowther RA, Frank S, Hench J, Probst A, Winkler DT, Reichwald J, Staufenbiel M, Ghetti B, Goedert M, Tolnay M (2013) Brain homogenates from human tauopathies induce tau inclusions in mouse brain. Proc Natl Acad Sci U S A 110(23):9535–9540. doi:10.1073/pnas.1301175110, pii: 1301175110
Sanders DW, Kaufman SK, DeVos SL, Sharma AM, Mirbaha H, Li A, Barker SJ, Foley AC, Thorpe JR, Serpell LC, Miller TM, Grinberg LT, Seeley WW, Diamond MI (2014) Distinct Tau prion strains propagate in cells and mice and define different tauopathies.. doi:10.1016/j.neuron.2014.04.047, pii: Neuron, doi:S0896-6273(14)00362-6
Haass C, Selkoe DJ (2007) Soluble protein oligomers in neurodegeneration: lessons from the Alzheimer’s amyloid beta-peptide. Nat Rev Mol Cell Biol 8(2):101–112. doi:10.1038/nrm2101, pii: doi:nrm2101
Wittmann CW, Wszolek MF, Shulman JM, Salvaterra PM, Lewis J, Hutton M, Feany MB (2001) Tauopathy in Drosophila: neurodegeneration without neurofibrillary tangles. Science 293(5530):711–714. doi:10.1126/science.1062382, pii: 1062382
Kuchibhotla KV, Wegmann S, Kopeikina KJ, Hawkes J, Rudinskiy N, Andermann ML, Spires-Jones TL, Bacskai BJ, Hyman BT (2014) Neurofibrillary tangle-bearing neurons are functionally integrated in cortical circuits in vivo. Proc Natl Acad Sci U S A 111(1):510–514. doi:10.1073/pnas.1318807111, pii: 1318807111
de Calignon A, Fox LM, Pitstick R, Carlson GA, Bacskai BJ, Spires-Jones TL, Hyman BT (2010) Caspase activation precedes and leads to tangles. Nature 464(7292):1201–1204. doi:10.1038/nature08890, pii: nature08890
Congdon EE, Gu J, Sait HB, Sigurdsson EM (2013) Antibody uptake into neurons occurs primarily via clathrin-dependent Fcgamma receptor endocytosis and is a prerequisite for acute tau protein clearance. J Biol Chem 288(49):35452–35465. doi:10.1074/jbc.M113.491001, pii: M113.491001
Sigurdsson EM (2009) Tau-focused immunotherapy for Alzheimer’s disease and related tauopathies. Curr Alzheimer Res 6(5):446–450, pii: CAR-7
Karch CM, Jeng AT, Goate AM (2012) Extracellular Tau levels are influenced by variability in Tau that is associated with tauopathies. J Biol Chem 287(51):42751–42762. doi:10.1074/jbc.M112.380642, pii: M112.380642
Chai X, Dage JL, Citron M (2012) Constitutive secretion of tau protein by an unconventional mechanism. Neurobiol Dis 48(3):356–366. doi:10.1016/j.nbd.2012.05.021, pii: S0969-9961(12)00207-0
Yamada K, Holth JK, Liao F, Stewart FR, Mahan TE, Jiang H, Cirrito JR, Patel TK, Hochgrafe K, Mandelkow EM, Holtzman DM (2014) Neuronal activity regulates extracellular tau in vivo. J Exp Med 211(3):387–393. doi:10.1084/jem.20131685, pii: jem.20131685
Pooler AM, Phillips EC, Lau DH, Noble W, Hanger DP (2013) Physiological release of endogenous tau is stimulated by neuronal activity. EMBO Rep 14(4):389–394. doi:10.1038/embor.2013.15, pii: embor201315
Ding WX, Yin XM (2008) Sorting, recognition and activation of the misfolded protein degradation pathways through macroautophagy and the proteasome. Autophagy 4(2):141–150, pii: doi:5190
Mohamed HA, Mosier DR, Zou LL, Siklos L, Alexianu ME, Engelhardt JI, Beers DR, Le WD, Appel SH (2002) Immunoglobulin Fc gamma receptor promotes immunoglobulin uptake, immunoglobulin-mediated calcium increase, and neurotransmitter release in motor neurons. J Neurosci Res 69(1):110–116. doi:10.1002/jnr.10271
Andoh T, Kuraishi Y (2004) Direct action of immunoglobulin G on primary sensory neurons through Fc gamma receptor I. FASEB J 18(1):182–184. doi:10.1096/fj.02-1169fje, pii: 02-1169fje
Niu N, Zhang J, Guo Y, Zhao Y, Korteweg C, Gu J (2011) Expression and distribution of immunoglobulin G and its receptors in the human nervous system. Int J Biochem Cell Biol 43(4):556–563. doi:10.1016/j.biocel.2010.12.012, pii: S1357-2725(10)00424-3
Bae EJ, Lee HJ, Rockenstein E, Ho DH, Park EB, Yang NY, Desplats P, Masliah E, Lee SJ (2012) Antibody-aided clearance of extracellular alpha-synuclein prevents cell-to-cell aggregate transmission. J Neurosci 32(39):13454–13469. doi:10.1523/JNEUROSCI.1292-12.2012, pii: 32/39/13454
Ravetch JV, Bolland S (2001) IgG Fc receptors. Annu Rev Immunol 19:275–290. doi:10.1146/annurev.immunol.19.1.275, pii: 19/1/275
McEwan WA, Tam JC, Watkinson RE, Bidgood SR, Mallery DL, James LC (2013) Intracellular antibody-bound pathogens stimulate immune signaling via the Fc receptor TRIM21. Nat Immunol 14(4):327–336. doi:10.1038/ni.2548, pii: ni.2548
Mallery DL, McEwan WA, Bidgood SR, Towers GJ, Johnson CM, James LC (2010) Antibodies mediate intracellular immunity through tripartite motif-containing 21 (TRIM21). Proc Natl Acad Sci U S A 107(46):19985–19990. doi:10.1073/pnas.1014074107, pii: 1014074107
Bellucci A, Westwood AJ, Ingram E, Casamenti F, Goedert M, Spillantini MG (2004) Induction of inflammatory mediators and microglial activation in mice transgenic for mutant human P301S tau protein. Am J Pathol 165(5):1643–1652. doi:10.1016/S0002-9440(10)63421-9, pii: S0002-9440(10)63421-9
Ikeda M, Shoji M, Kawarai T, Kawarabayashi T, Matsubara E, Murakami T, Sasaki A, Tomidokoro Y, Ikarashi Y, Kuribara H, Ishiguro K, Hasegawa M, Yen SH, Chishti MA, Harigaya Y, Abe K, Okamoto K, St George-Hyslop P, Westaway D (2005) Accumulation of filamentous tau in the cerebral cortex of human tau R406W transgenic mice. Am J Pathol 166(2):521–531. doi:10.1016/S0002-9440(10)62274-2, pii: S0002-9440(10)62274-2
Sasaki A, Kawarabayashi T, Murakami T, Matsubara E, Ikeda M, Hagiwara H, Westaway D, George-Hyslop PS, Shoji M, Nakazato Y (2008) Microglial activation in brain lesions with tau deposits: comparison of human tauopathies and tau transgenic mice TgTauP301L. Brain Res 1214:159–168. doi:10.1016/j.brainres.2008.02.084, pii: S0006-8993(08)00554-4
Zilka N, Stozicka Z, Kovac A, Pilipcinec E, Bugos O, Novak M (2009) Human misfolded truncated tau protein promotes activation of microglia and leukocyte infiltration in the transgenic rat model of tauopathy. J Neuroimmunol 209(1-2):16–25. doi:10.1016/j.jneuroim.2009.01.013, pii: S0165-5728(09)00020-4
Yoshiyama Y, Higuchi M, Zhang B, Huang SM, Iwata N, Saido TC, Maeda J, Suhara T, Trojanowski JQ, Lee VM (2007) Synapse loss and microglial activation precede tangles in a P301S tauopathy mouse model. Neuron 53(3):337–351. doi:10.1016/j.neuron.2007.01.010, pii: S0896-6273(07)00030-X
Wilcock DM, DiCarlo G, Henderson D, Jackson J, Clarke K, Ugen KE, Gordon MN, Morgan D (2003) Intracranially administered anti-Abeta antibodies reduce beta-amyloid deposition by mechanisms both independent of and associated with microglial activation. J Neurosci 23(9):3745–3751, doi:23/9/3745 [pii]
Bacskai BJ, Kajdasz ST, Christie RH, Carter C, Games D, Seubert P, Schenk D, Hyman BT (2001) Imaging of amyloid-beta deposits in brains of living mice permits direct observation of clearance of plaques with immunotherapy. Nat Med 7(3):369–372. doi:10.1038/85525, pii: 85525
Gessner JE, Heiken H, Tamm A, Schmidt RE (1998) The IgG Fc receptor family. Ann Hematol 76(6):231–248
Bard F, Cannon C, Barbour R, Burke RL, Games D, Grajeda H, Guido T, Hu K, Huang J, Johnson-Wood K, Khan K, Kholodenko D, Lee M, Lieberburg I, Motter R, Nguyen M, Soriano F, Vasquez N, Weiss K, Welch B, Seubert P, Schenk D, Yednock T (2000) Peripherally administered antibodies against amyloid beta-peptide enter the central nervous system and reduce pathology in a mouse model of Alzheimer disease. Nat Med 6(8):916–919. doi:10.1038/78682
Serrano-Pozo A, Muzikansky A, Gomez-Isla T, Growdon JH, Betensky RA, Frosch MP, Hyman BT (2013) Differential relationships of reactive astrocytes and microglia to fibrillar amyloid deposits in Alzheimer disease. J Neuropathol Exp Neurol 72(6):462–471. doi:10.1097/NEN.0b013e3182933788
Wilcock DM, Munireddy SK, Rosenthal A, Ugen KE, Gordon MN, Morgan D (2004) Microglial activation facilitates Abeta plaque removal following intracranial anti-Abeta antibody administration. Neurobiol Dis 15(1):11–20, doi:S0969996103001955 [pii]
Dodart JC, Bales KR, Gannon KS, Greene SJ, DeMattos RB, Mathis C, DeLong CA, Wu S, Wu X, Holtzman DM, Paul SM (2002) Immunization reverses memory deficits without reducing brain Abeta burden in Alzheimer’s disease model. Nat Neurosci 5(5):452–457. doi:10.1038/nn842, pii: nn842
DeMattos RB, Bales KR, Cummins DJ, Dodart JC, Paul SM, Holtzman DM (2001) Peripheral anti-A beta antibody alters CNS and plasma A beta clearance and decreases brain A beta burden in a mouse model of Alzheimer’s disease. Proc Natl Acad Sci U S A 98(15):8850–8855. doi:10.1073/pnas.151261398, pii: 151261398
DeMattos RB, Bales KR, Cummins DJ, Paul SM, Holtzman DM (2002) Brain to plasma amyloid-beta efflux: a measure of brain amyloid burden in a mouse model of Alzheimer’s disease. Science 295(5563):2264–2267. doi:10.1126/science.1067568, pii: 295/5563/2264
Yamada K, Yabuki C, Seubert P, Schenk D, Hori Y, Ohtsuki S, Terasaki T, Hashimoto T, Iwatsubo T (2009) Abeta immunotherapy: intracerebral sequestration of Abeta by an anti-Abeta monoclonal antibody 266 with high affinity to soluble Abeta. J Neurosci 29(36):11393–11398. doi:10.1523/JNEUROSCI.2021-09.2009, pii: 29/36/11393
Abbott NJ (2004) Evidence for bulk flow of brain interstitial fluid: significance for physiology and pathology. Neurochem Int 45(4):545–552. doi:10.1016/j.neuint.2003.11.006, pii: S0197018603002675
Iliff JJ, Wang M, Liao Y, Plogg BA, Peng W, Gundersen GA, Benveniste H, Vates GE, Deane R, Goldman SA, Nagelhus EA, Nedergaard M (2012) A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid beta. Sci Transl Med 4(147):147ra111. doi:10.1126/scitranslmed.3003748, pii: 4/147/147ra111
Acknowledgements
This work was supported by research grants from the Tau consortium and C2N Diagnostics (M.I.D. and D.M.H.).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this protocol
Cite this protocol
Yanamandra, K., Diamond, M.I., Holtzman, D.M. (2016). Active and Passive Immunotherapy Against Tau: Effects and Potential Mechanisms. In: Ingelsson, M., Lannfelt, L. (eds) Immunotherapy and Biomarkers in Neurodegenerative Disorders. Methods in Pharmacology and Toxicology. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-3560-4_9
Download citation
DOI: https://doi.org/10.1007/978-1-4939-3560-4_9
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-3558-1
Online ISBN: 978-1-4939-3560-4
eBook Packages: Springer Protocols