Abstract
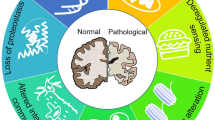
An increasing number of persons live for nine or more decades and enjoy the benefits of a well-functioning brain until the end of their life. In that respect, the cognitive performance in later life and the quality maintenance of the brain are amazing biological phenomena. Since most nerve cells are generated during pregnancy and have to survive an active lifetime, the brain has to be endowed with a maintenance machinery of surprising long-term quality. During successful, that is, non-pathological, aging in most brain regions, there is very little or no evidence for a decrease in numbers of neurons. In some brain structures, a limited reduction of nerve cells may occur, but it is generally conceived that aging and aging-related cognitive impairments are not the result of massive cell loss but rather the result of synaptic changes, receptor dysfunction or signaling deficits, and metabolic decline. Besides, nerve cell loss during normal aging may be compensated by synaptogenesis, dendritic branching, or in certain brain structures like dentate gyrus by neurogenesis from progenitor stem cells. Yet most human individuals suffer from a mild but life-disturbing condition we call aging-related memory impairment (AMI). In this chapter, some of the mechanisms will be shortly explored that are considered to be causal to non-pathological deterioration of cognitive faculties. In particular several cellular and molecular neuronal changes will be addressed that occur during aging, the consequences for interneuronal communication and membrane potential, the blood supply to the brain and cerebrovascular condition, and some observations on the protective neuroimmune system of the brain.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
- 5-hydroxytryptamine
- Afterhyperpolarization (AHP)
- Aging-related memory impairment (AMI)
- Amyloid precursor protein (APP)
- Axonal aberrations
- BDNF (brain-derived neurotrophic factor)
- Brain aging
- Abolishment of LTP
- Axonal aberrations
- Brain microvessels
- Calcium homeostasis
- Cerebral blood flow
- Cognitive dysfunction
- Cortical microvascular decline
- Degenerative changes
- Hippocampal volumetric loss
- Innate inflammatory system
- Memory impairment
- Nervous tissue
- Blood flow in
- Neuroinflammatory processes
- Neuronal loss
- Neuronal membrane
- Changes of
- Neurotransmitter systems
- Synaptic plasticity
- CAMKIV gene
- Cholesterol
- Gamma-aminobutyric acid (GABA)
- Microglia
- Morris water maze (MWM)
- Neurotransmitter serotonin
- Synaptic plasticity
- Voltage-dependent calcium channels (VDCC)
Brief History
An increasing number of persons live for nine or more decades and enjoy the benefits of a well-functioning brain until the end of their life. In that respect, the cognitive performance in later life and the quality maintenance of the brain are amazing biological phenomena. Since most nerve cells are generated during pregnancy and have to survive an active lifetime, the brain has to be endowed with a maintenance machinery of surprising long-term quality. During successful, that is, non-pathological, aging in most brain regions, there is very little or no evidence for a decrease in numbers of neurons. In some brain structures, a limited reduction of nerve cells may occur, but it is generally conceived that aging and aging-related cognitive impairments are not the result of massive cell loss but rather the result of synaptic changes, receptor dysfunction or signaling deficits, and metabolic decline. Besides, nerve cell loss during normal aging may be compensated by synaptogenesis, dendritic branching, or in certain brain structures like dentate gyrus by neurogenesis from progenitor stem cells. Yet most human individuals suffer from a mild but life-disturbing condition we call aging-related memory impairment (AMI). In this chapter, some of the mechanisms will be shortly explored that are considered to be causal to non-pathological deterioration of cognitive faculties. In particular several cellular and molecular neuronal changes will be addressed that occur during aging, the consequences for interneuronal communication and membrane potential, the blood supply to the brain and cerebrovascular condition, and some observations on the protective neuroimmune system of the brain.
Age-Related Memory Impairment Affects Mainly Effortful Processing but Spares Automatic Cognitive Processing Mechanisms
Aging is generally accompanied by a deterioration of many body systems and functions, including the brain and cognition. Aging-related memory impairment (AMI) is a well-recognized but relatively poorly defined phenomenon, partly because this decline has not one unitary cause. It is not characterized by global cognitive deterioration, but instead is rather specific. In general, aging spares automatic processing but not effortful processing. AMI needs to be distinguished from the pathological forms of dementia. During non-pathological, normal aging-related decline of human cognition, the speed of cognitive processes slows down as compared to younger people. Typical memory hick-ups such as forgetting names (word-finding difficulties), the place you put your keys or in what magazine you read something interesting (source memory failures), promises, and appointments made and learning new associations between items (such as a name with a face) typically increase in people over 40 and belong to the domain of declarative memory. Many of these functions are functionally linked to the prefrontal cortex (PFC) situated in the frontal lobe and the hippocampus situated in the medial temporal lobe. Although in itself not alarming, AMI usually is troublesome for the affected individual and negatively affects the quality of life. Moreover, the brain mechanisms underlying this non-pathological decline in cognition can set in motion or speed up developments toward pathological and eventually devastating cognitive conditions. For this reason, AMI is an increasing biomedical concern worldwide, also since the vast majority of individuals aged over 75 experience AMI.
It is a striking finding that some aged individuals show severe impairments in cognitive functions, whereas others of the same age perform as well as young adults, even up to ages well over 100 (the successful centenarians). People in this group age “successfully,” and they, apparently, have some protection against AMI and beyond. This is referred to as having “cognitive brain reserve,” which, to some extent, depends on specific genetic components. More importantly, these people typically have led an active life, either physically or mentally (and usually both). Based on these observations, the role of physical exercise and the underlying neurobiological mechanisms and substrates in preventing cognitive decline receives ample attention in gerontology. In particular the mechanisms involved are studied in mammalian animal models, mainly in rats, mice, rabbits, and monkeys.
Next to a decline in declarative memory, age-related dysfunctions in navigational skills are well documented in humans. This usually occurs later in life than the mild declarative memory deficits mentioned above. Aged individuals are typically less flexible in adapting acquired behavior to novel situations: they behave more routine-like as compared to younger people. This is referred to as loss of behavioral flexibility, characterized by more routine-like behavior mediated at large by the striatum.
Younger and older individuals perform rather similarly on simple cognition tasks requiring working memory (the temporary storage and processing of information) depending on the PFC. However, when executive functions such as memory updating are required, performance on working memory tasks is severely impaired in the elderly. In order to compensate, elderly recruit more PFC areas (which are often also more strongly activated, called PFC overactivation). Under the same performance level of an easy task, PFC activity is higher in old brain than in young brain. If the task is getting more difficult, young people increase PFC activity much more than old people can do. Hence, level of performance drops in the elderly. Keeping out irrelevant information or deleting irrelevant information is more difficult at old age (less inhibitory control). Next to working memory or short-term memory, aging can have great effects on long-term memory, mainly due to reduced encoding (largely caused by inadequate PFC activation and hence a reduced neural representation needed for proper information encoding). Older adults generally show weaker activation in the medial temporal lobe, and specifically in the hippocampus, the brain region primarily involved in the generation of new (long-term) memories.
More general observations made by brain imaging technologies revealed characteristic alterations in aged brain functioning related to cognitive performance. Age-related reductions in hemispheric asymmetry in older adults are often observed. By this phenomenon, information processing is less specific due to loss of regional specialization. This is true too during PFC overactivation, although initially this can be a successful compensation for cognition. In contrast to PFC overactivation, reduced activation in more posterior regions is often found, called the posterior-anterior shift in brain aging. Signal-to-noise ratios are decreased in the aging brain, which thus leads to less distinct neural representations. Finally, many MRI studies have shown that the aged human brain declines in white matter content. The loss of myelinated fibers may contribute to reduced information processing speed, reduced neuronal network complexity, and cognitive dysfunction.
Cognitive Decline and Its Underlying Mechanisms Can Be Investigated Well in Mammals as Model for the Study of Human Cognitive Dysfunction
Age-related memory impairment is also observed in a wide variety of mammalian species, including rat, mouse, rabbit, and monkey. In these species and in humans, only a small subset of genes undergoes similar changes, serving as a potential common indicator of biological aging. Like in humans, particularly working memory/executive functions and declarative/spatial memory are affected. The brain regions predominantly involved in these two categories are the PFC and hippocampus, respectively, with (sub)region-specific vulnerability. The genetic changes in these areas point to a genetic underpinning for this region specificity.
A decline in episodic memory (the “what, where, when” memory or the memory of autobiographical events or source memory mediated by the PFC) is a hallmark of normal cognitive aging, and deficits increase with increasing age. Age-related working memory deficits due to PFC hypo-activity have been shown in rats too. As such, reduced PFC functioning in aged animals largely mimics the situation in aged humans.
Rodent spatial memory is best studied in spatial memory tasks such as the Morris water maze (MWM) , the eight-arm radial maze, and the T or Y maze. In the latter, the shift from hippocampal to striatal learning and loss of behavioral flexibility can be monitored. Old mice perform similarly as young mice during the acquisition in a two-arm reference memory task (Y maze with one arm consistently baited), but are impaired during reversal training (subsequently with the other arm consistently baited) (Fig. 1). This AMI is caused by the differential engagement of the hippocampus and striatum: young mice use the hippocampus which is highly flexible during reversal learning, whereas old animals try to solve the task via the less flexible striatum. They do so because of aging-related hippocampal dysfunction.
Aged mice are specifically impaired in spatial reversal learning, reflecting a loss in behavioral flexibility. The mice entered the Y maze from a start box (s) and were trained for 7 days (six trials per day, with one arm choice allowed per trial) to locate the food reward (F) in the left arm. All mice started at approximately 50 % chance level of choosing the correct arm, and over time young and aged mice mastered the task equally well. Then during reversal training, the food reward was relocated to the right arm. It took aged mice significantly more trials than young mice to master this part of the test (Modified from Havekes et al. (2011))
Spatial memory performance depends on hippocampal place cells, which are neurons responding to specific locations within a spatial environment. When aged rats initially explore a new environment, place cells in the hippocampal fields CA1 and CA3 form place fields (spatial maps) similarly in size as seen in young rats. However, when old rats repeatedly traverse the same environment, the place fields do not expand to the extent that occurs in young rats. This deficit in place field plasticity, based on NMDA-receptor-dependent synaptic plasticity underlying the formation of networks of hippocampal principal cells, contributes to reduced spatial memory performance. Besides spatial map formation, spatial map stability is also reduced in the aged hippocampus. In addition, old rats retrieve the wrong spatial map more frequently than young rats upon reentry of an environment, which can be viewed as a memory retrieval failure. The spatial maps in CA3 tend to generalize environments more in old rats, by which minor spatial alterations in landmarks and cues are ignored.
Clearly, hippocampus-dependent memory is specifically impaired in aged individuals. The hippocampus is needed for the formation of new (declarative) memories and to acquire and retain information critical for successful navigation through space combined with the formation of associative memories. Spatial memory deficits have been consistently reported in aged animals, including monkeys, dogs, rats, and mice. For this reason, the neurobiological substrate of AMI has largely focused on the hippocampus. The new memories have to be consolidated into long-term memory sites in the neocortex. The exact nature of the hippocampus-neocortex interactions is not well understood, but the hippocampus has to “reactivate” previous activity patterns necessary for long-term storage. This replay occurs during quiet periods and sleep. In aged rats, the correct sequence of firing of hippocampal neurons is less preserved, which may contribute to overall memory impairment in aged rats.
Within the rodent hippocampus, the dentate gyrus is particularly vulnerable to the effects of aging, with a characteristic reduction in rate of neurogenesis. Although neurogenesis declines with age, it has not been clearly demonstrated that neurogenesis correlates with learning abilities in (aged) rodents. Some data indicate that a correlation between neurogenesis, aging, and learning does exist by which the aged impaired individuals have the least neurogenesis. Like in rodents, the generation of new nerve cells is dramatically reduced in the aged human dentate gyrus.
Mechanisms of Brain Aging
Many neuronal mechanisms remain more or less similar in young and aged brain. However, there are some specific, aging-related alterations in the old brain directly linked to impaired cognitive performance. Even in the course of normal aging, the overall brain shows a certain degree of atrophy, which results in a decrease in brain weight and volume and a decrease in the level of proteins. From 50 to 90 years of age, the loss of brain weight is approximately 2–3 % per decade. An increase in ventricular volume and the total amount of cerebrospinal fluid indicates a reduction in the volume of brain tissue during aging. With the aid of magnetic resonance imaging (MRI), the shrinkage of different brain areas can readily be followed. Especially the involution size of the hippocampus was repeatedly matched successfully to AMI in humans. The primary question is how neuronal atrophy affects the structure and function of different parts of the neuron, i.e., the synapses, the neurites (axons and dendrites), and size and integrity of the cell bodies. These changes are thought to underlie AMI and will be briefly discussed below.
During Aging, Neurons Rarely Die but Change at the Level of Cytoskeleton, Synapse, and Synthetic Activity Negatively Affecting Synaptic Plasticity
Gene transcription and protein synthesis are needed for the formation of long-term memory. Aberrant changes in gene transcription affect the cognitive abilities of the aged brain: it can either be decreased or increased depending on the brain region and the protein studied. Cognitive performance requires the transcription of immediate early genes (IEGs, including Arc (activity-regulated cytoskeletal gene)), BDNF (brain-derived neurotrophic factor) , and the late gene zif268. IEGs are among the first genes switched on upon neuronal and synaptic stimulation, followed by switching on late genes. Decreased IEG expression has been shown in the aged brain. Moreover, BDNF and its receptors undergo significant age-associated downregulations. Hence, several genes known to be necessary for synaptic plasticity and normal memory functioning are downregulated in the aged brain. Reductions in the amount of protein synthesis in the aged brain contribute to AMI. Along this line reduction in age-related protein synthesis is typically found in rat hippocampus (dentate gyrus but not CA1), nucleus accumbens, and locus coeruleus.
The once generalized “neuronal loss theory of aging” has been disproved by novel cell counting methods based on more reliable mathematical techniques to quantify and estimate total neuron numbers. More classical studies reported some loss of neurons with aging in the neocortex, amygdala, spinal cord, nucleus basalis, corpus striatum/putamen, suprachiasmatic nucleus, inferior olive, and cerebellar Purkinje cells, but more recently it was established that there is no overt loss of neurons during normal aging (except for the Purkinje cells). Hence, the impairment of hippocampal-dependent memory in aged individuals is not due to massive cell death.
As indicated above, if hippocampal volumetric loss occurs, it is primarily caused by neuronal atrophy (shrinkage) rather than by neuronal loss. The number of hippocampal neurons differs neither between young and aged individuals nor between individuals with AMI and cognitively intact old subjects. Age-related functional and behavioral changes are the outcome of other, more subtle, changes that occur in individual neurons or the communication between neurons.
Aging has a profound effect on the integrity of the forebrain fiber patterns that find their origin in general modifying transmitter systems such as the serotonergic, noradrenergic, dopaminergic, and cholinergic cell groups in midbrain and basal forebrain. In particular these midbrain and basal forebrain projection systems to the cortical mantle are prone to the formation of axonal pathologies like fiber swelling and profiles forming grape-like structures. Likewise, such axonal aberrations are also found for cytoskeletal proteins such as neurofilaments (Fig. 2). These aberrant fibers and fiber swelling become progressively pronounced in the course of normal brain aging. Thus, these anomalies of axon pathology are rather ubiquitous in projecting neurons, and they appear to be causally related to hampered axonal transport processes. Since these axonal aberrations also occur in the aged animal brain where the specific neurodegenerative processes that are known from human diseases are absent, these fiber anomalies should be considered as typical for aging per se. It is highly likely that fiber aberrations and neuritic dystrophies are indicators of a shift of balance from successful neuronal maintenance toward loss of restorative capacity of the brain progressively resulting in abundant accumulation of dystrophic structures.
Axonal aberrations (see arrows in panel (a)); fibers stained for neurofilaments in rabbit hippocampus) are large malformations in thin fibers found throughout the aged brain. The number of axonal aberrations, here quantified for the hippocampus (panel (b)), gradually increases with age. Such fiber swellings are common for cortical projection systems that originate from subcortical sources like cholinergic, serotonergic, and noradrenergic cell groups in basal forebrain and brain stem (Data taken from Van der Zee et al. (1997))
Electrical properties remain relatively intact over the lifespan. Hence, firing properties do not differ at large between young and old neurons, but hippocampal connectivity is affected in a region-specific manner with accompanying electrophysiological changes. Reduced numbers of synaptic terminals have been reported in aged dentate gyrus. The hippocampal CA1 region is the most-studied brain area with regard to age-related changes in synapses. Notably perforated synapses (synapses with multiple contact zones) are selectively reduced in size in aged rats with impaired spatial learning (Fig. 3).
Aging neurons are characterized by a reduced dendritic tree and reduced numbers of dendritic spines (inset (a) and (c) for the young and aged neuron, respectively). Few morphological changes are found at the synaptic level, although in some cases the active zone is reduced with less synaptic vesicles and a reduced postsynaptic density. Aged synapses can be relatively large, which is considered to be a compensation for the loss in number of synaptic contacts (inset (b) and (d) show a synaptic contact of a young and aged neuron, respectively; the altered morphology in (d) is an exaggerated example) (The synaptic contact is modified from Geinisman et al. (2001). New figure adapted from own work Fig. 2 in J Neurosci. 2001, 21:103–116)
The number of perforated synapses correlates positively with spatial memory capacity in aged animals. If the entire hippocampus is considered, only minor loss of synapses is found. If the dorsal hippocampus is taken apart, a loss of synapses in the dentate gyrus as a function of normal aging is found and even more so in rats with age-related decline in spatial memory. It should be noted that synapse number by itself does not predict cognitive status. It is more likely that Ca2+-dependent cellular processes responsible for maintaining or altering synaptic strength are pivotal to AMI (see below). Pre- and postsynaptic parameters remain relatively constant throughout the lifespan of rats. However, NMDA-receptor-mediated synaptic transmission is enhanced in very old rats, contributing to dysregulation of Ca2+-dependent cellular processes. This age-related dysregulation of NMDA receptors affects place cell function negatively, influencing spatial memory performance in aged individuals.
Synaptic plasticity , notably long-term potentiation (LTP), is hampered in the aged brain, and learning and memory deficits found in aged rodents parallel deficits in LTP (Fig. 4). LTP is considered the cellular basis of learning and memory processes as information is stored via activity-dependent changes at the synapse. LTP is characterized by at least two different phases: induction (early-phase LTP) and maintenance (late-phase LTP). There are no age-related deficits in LTP induction if the stimulus parameters are strong enough. However, if the stimulus parameters are close to the threshold of LTP induction, the aged hippocampus reveals an LTP-induction deficit. The decay rates of LTP do not differ much between young and old rats in the first hours after LTP induction. At longer time intervals, however, significant maintenance deficits do appear. At these time points, LTP decays twice as fast in aged rats than in young rats. Spatial memory deficits in aged rats correlate with LTP (both within and between age groups). The rate of acquisition of spatial memory correlates significantly with LTP induction, and rate of forgetting of spatial memory correlates significantly (but negatively) with LTP maintenance.
Schematic representation of the abolishment of LTP in the aging hippocampus. At time point 0 (indicated by the arrow), a train of 100-Hz stimuli is given to the hippocampus. LTP is rapidly induced, irrespective of age. While LTP is maintained in a stable fashion for a long period in the young hippocampus, it is not maintained in such a way in the aged hippocampus. Here, the EPSPs drop back to baseline (and even slightly below) relatively quickly
Epigenetics refers to modification of DNA and posttranslational modulation of nuclear proteins by which patterns of gene expression are altered. Next to the age-related changes in gene transcription, it is very likely that age-associated disruption in DNA methylation and histone modification, two major processes in epigenetic mechanisms, leads to age-specific memory disruption.
In summary, to draw a clear distinction between normal and pathological neuronal aging is not yet possible, and the transition from aging cell to a pathological state can be very gradual and not always easy to define unless explicit neurotoxic mechanisms can be identified. The AMI-related changes include shrinkage in soma size, loss or regression of dendrites and dendritic spines, alterations in neurotransmitter receptors, and changes in electrophysiological properties. The integrative functional characteristics of dendrites are determined by several factors, including their morphology, the spatiotemporal patterning of synaptic inputs, and the balance of inhibition and excitation. Thus, dendrites play a vital role in the functional properties of neuronal circuits, and any structural changes can have profound and detrimental functional effects. Turnover of synapses, dendritic spines, and axonal nerve endings forms the basis of functional plasticity of neurons. The recent findings in neuronal morphology during normal and abnormal brain aging support the view that the suboptimal plastic renewal of neuritic structures plays a key role in cognitive aging among the brain aging processes. The structural and functional aberrations of axons, synapses, and synaptic signaling appear to be the primary events during aging which is enhanced in time and in magnitude in cognitive neurodegeneration processes as in Alzheimer’s disease and other dementias.
Neuronal Membrane Structure and Composition Changes at Older Ages and Influences Membrane Fluidity and Membrane Signaling. The Role of Cholesterol
Neuronal membranes support the larger part of cellular macromolecules (about 80 %) and form functionally connected morphological structures including nuclear membrane, endoplasmic reticulum, Golgi apparatus, synaptic vesicles, and synaptic terminal membrane. The basic structure is the lipid bilayer, which provides a matrix for proper membrane functioning. The major components of membranes are lipids, predominantly phospholipids and sterols (cholesterol), and proteins. The hydrophobic hydrocarbon chains of the polar lipids are located in the interior of the bilayer, whereas the hydrophilic head groups are exposed to the aqueous surroundings. The included proteins are membrane-spanning, anchored, and membrane-associated proteins, which can be receptors, ion channels, cytoskeletal proteins, and proteins of the signaling machinery conveying information between the extra- and intracellular compartments. Physicochemically the lipid-protein interaction is one of the primary determinants of the quality of membrane function and, from this aspect, membrane fluidity merits consideration.
The fluidity of neuronal membranes plays a pivotal role in brain aging and neurodegeneration. Membrane fluidity under normal conditions supports lipid-protein interactions leading to adequate neurotransmitter functioning and transmembrane signal transfer, for example, in relaying transmitter signals to their second messenger machinery. The structure of fatty acids influences membrane fluidity; the higher the number of double bonds, the higher the impact on fluidity. Aging is accompanied by a decrement in long-chained polyunsaturated fatty acids (PUFAs, mainly arachidonic acid (ARA) and docosahexaenoic acid (DHA)) in membrane phospholipids which results in decreased membrane fluidity, i.e., a more rigid membrane is formed. Dietary omega-3 fatty acid intake improves the membrane function in the hippocampus and, consequently, especially by DHA intake from fish oil, spatial learning ability in old rats can be enhanced. It has been widely accepted that optimal learning capability requires normal membrane fluidity.
PUFA’s are not only structural components of the membrane but also play a role in synapse formation which is diminishing during aging. Brain phosphatide synthesis requires three circulating compounds: DHA, uridine, and choline. Oral administration of these phosphatide precursors to experimental animals increases the level of phosphatides and synaptic proteins in the brain and the numbers of dendritic spines on hippocampal neurons.
As indicated above, LTP is considered as a reliable physiological biomarker of learning capability. Aged rats exhibit an impaired ability to sustain LTP in the dentate gyrus of the hippocampus which correlates with a decrease in ARA concentration. Dietary supplementation with arachidonic acid and its precursor, gamma-linolenic acid, reversed the impairment in LTP in aged rats.
Another key membrane function which can become affected during aging is the processing of amyloid precursor protein (APP) especially with respect to AMI, and eventually to the development of Alzheimer’s disease (AD) neuropathology. Gradual changes in steady-state levels of beta amyloid peptides (Ab peptides) in the brain are considered as the initial step in the amyloid cascade hypothesis of AD. DHA supports normal, physiological APP processing by increasing α-secretase activity at the cell surface, since α-secretase leads to APP splicing products that are removed and broken down by natural and nontoxic fragment processing. The alternative splicing of the APP molecule in the neuronal plasma membrane by b-and g-secretases leads to the release of Ab peptides, of which the oligomeric forms are the most toxic for the brain which is partly explained by the propensity of Aβ to aggregate initially to soluble and finally to insoluble polymers and fibrils.
Cholesterol plays several structural and metabolic roles that are crucial to brain functioning. In membranes, it regulates fluidity and cell signaling events in cooperation with other lipids. Aβ-induced changes in membrane fluidity could be explained by physicochemical interactions of the peptide with membrane components such as cholesterol, phospholipids, and sphingolipids, while reversely cholesterol stimulates Aβ production. Beside cholesterol, other lipids strongly modulate APP processing, whereas the APP cleavage products themselves regulate lipid, including cholesterol homeostasis, resulting in complex regulatory feedback cycles.
High levels of cholesterol have been proposed as a risk factor for AD. Cholesterol inhibits α-secretase activity and facilitates β- and γ-secretases, and in this way increases Aβ production. Therefore, it has been argued that cholesterol lowering drugs such as statins could diminish the risk of AD. Indeed, there is evidence for a significantly reduced incidence of AD among people who have been using statins to curb hypercholesterolemia and its cardiovascular effects. There is now evidence for a diminished synthesis of cholesterol in the aging hippocampus, but without a noticeable change in its concentration. In rat, the cholesterol levels at the age of 24 months appear to be increased in striatum, cerebellum, and brain stem, but not in the cerebral cortex or hippocampus.
With respect to the cholesterol content in the nervous tissues in the various age phases, it became clear that regional differences and subcellular partitioning of the cholesterol concentrations are characteristic for aging. An interesting view on the role of cholesterol in the aged brain is the asymmetric distribution of cholesterol among different domains during aging and that the cholesterol content of the exofacial leaflet of synaptic plasma membranes doubles with age (Fig. 5). This figure shows that the transbilayer distribution of cholesterol is associated with Aβ accumulation in the external layer of the synaptic membrane of aged mice. This accumulation of Aβ may disrupt other membrane lipid domains such as lipid rafts, which are membrane microdomains particularly rich in ion channel and signaling proteins and actively involved in setting membrane potential and ionic signaling. This way cholesterol via amyloid may impinge on normal membrane function in general. Note that polyunsaturated fatty acids, especially the abovementioned DHA, and the main cholesterol transporting neuronal lipoprotein ApoE are potent regulators of transbilayer cholesterol distribution.
Distribution of cholesterol in the synaptic plasma membrane (SPM) outer (Exo.) and inner (Cyto.) layers of young and aged. The SPM outer, exofacial leaflet of aged mice contains twice the amount of cholesterol than the younger mice. Partitioning of amyloid beta-peptides (red structure) into or out of the exofacial layer may be hindered by the accumulation of cholesterol (yellow structure) in the exofacial leaflet of aged individuals. This accumulation of Aß may disrupt membrane lipid domains and affect membrane functions (Adapted with permission from Wood et al. (2002))
Neurotransmitter Systems Projecting to the Forebrain Appear Particularly Vulnerable to the Aging Process
Many neurotransmitter systems to the cerebral cortex that have their origin in brain stem structures show aging-related downregulation in activity (e.g., acetylcholine, dopamine, serotonin, and noradrenaline). Usually specific changes occur at the receptor level, contributing to a reduction in overall signal transduction. Several receptor types of these four ascending systems target on the same downstream intracellular pathways and molecular cascades. Nearly all signal transduction pathways involved in cognitive performance utilize the activation of kinases and phosphatases. Among the most robustly downregulated genes in aging humans are the “cognitive kinase” CAMKIV gene linked to the CREB-related pathway, and the eukaryotic translation initiation factors (eIFs) belonging to the translational machinery. Hence, protein synthesis needed for neuronal plasticity is hampered in the aged brain.
Protein modification through phosphorylation by kinases is a critical regulatory tool of enzyme activity levels (Fig. 6). One cognitive kinase required for memory acquisition is the Ca2+-dependent and brain-specific protein kinase Cγ (PKCγ). This kinase translocates from the cytosol to the membrane (or specific intracellular targets) during encoding of information, and remains attached to the membrane long after the initiating stimulus is gone. Here, it phosphorylates learning- and memory-specific substrates. Various forms of age-related dysregulations of PKCγ have been reported, depending on the species studied. For example, upregulations in kinase activity levels (demonstrated in rabbit and Sprague Dawley rat) or increased levels of membrane-bound PKCγ (demonstrated in Wistar rat) most likely reflect compensatory attempts. However, like with PFC overactivation, a negative effect of this type of compensation is loss of specificity in PKCγ activity. Many dysregulations of kinase activities are due to changes in the scaffolding and anchoring proteins, for these enzymes orchestrate their subcellular location and regulate activity levels. Notably proteins like RACK-1 and AKAP150 are dramatically reduced in the aged hippocampus (Fig. 6).
Dysregulations of intracellular phosphorylation events occur in aging neurons due to dramatic reductions in the expression of scaffolding and anchoring proteins, for example, RACK-1 and AKAP150. Due to the loss of these regulatory elements, the delicate balance between levels of phosphorylation and dephosphorylation of target proteins gets disturbed, as depicted schematically in the upper panels (a) (young neuron) versus (b) (aged neuron) for target protein 1 (normally heavily phosphorylated) and target protein 2 (normally non-phosphorylated). In the lower panels, examples are shown for the dramatic reduction in hippocampal AKAP150 expression in aged as compared to young mice (panels (e) and (b), respectively), and the increased activity of the calcium-dependent kinase PKCγ as detected by an antibody specifically recognizing the activated form of PKCγ (c) and (f) for the young and aged rabbit hippocampus, respectively). AKAP150 (Data taken from Ostroveanu et al. (2007)), PKCγ (Data taken from Van der Zee et al. (2004))
The structural and anatomical axonal and neuritic dystrophies described above are paralleled by reductions in the enzymes that synthesize the neurotransmitters dopamine, norepinephrine, serotonin, and acetylcholine. This is accompanied by partial shrinkage and functional decline of their subcortical cell bodies of origin in the midbrain substantia nigra, locus coeruleus, raphe, and nucleus basalis of Meynert. Therefore, not only neuronal loss in these subcortical nuclei but also the vitality of the remaining or surviving neurons is essential for maintaining normal or adequate mental functions.
Cognitive Dysfunction Parallels Degenerative Changes in Cortical Projection Transmitter Systems
Some of the cognitive dysfunctions in aging can well be linked to specific transmitter deficits. Converging evidence from patient studies, animal research, pharmacological intervention, and molecular genetics indicates that dopamine is critically implicated in higher-order cognitive functioning. Many cognitive functions and multiple markers of striatal and extrastriatal DA systems decline across adulthood and aging. Molecular imaging studies of dopaminergic neurotransmission measure biomarkers of dopamine, such as the dopamine transporter and dopamine receptor D1 and D2 indicate that individual differences in dopamine functions are linked to age-related decline in executive functioning, episodic memory, and perceptual speed.
The neurotransmitter serotonin (5-hydroxytryptamine) is paramount for regulation of mood, food intake, activity rhythms, and sexual behavior, which are all behavioral expressions prone to changes during aging. Moreover, the serotonergic system is significantly involved in learning and memory, in particular by interacting with the cholinergic, glutamatergic, dopaminergic, or GABAergic systems. Its action is mediated via specific receptors located in crucial brain structures involved in these functions, primarily the septo-hippocampal complex, the nucleus basalis magnocellularis, and the PFC. There is now ample evidence that the administration of a variety of serotonergic receptor targeting drugs can prevent memory impairment and facilitate learning in situations involving a high cognitive demand.
The human cholinergic basal forebrain system is comprised of magnocellular neurons within the septal/diagonal band complex and nucleus basalis of Meynert. During normal aging, the anatomical integrity of fiber pathways penetrating the various cortical layers is compromised, a phenomenon that is not limited to the cortical regions but affects structures like thalamus and brain stem as well. Cholinergic neuronal cell loss was found predominantly in pathological aging, such as Alzheimer’s disease or Parkinson’s disease, while normal aging is accompanied by a gradual loss of cholinergic function caused by dendritic, synaptic, and axonal degeneration as well as a decrease in trophic support by nerve growth factor (NGF). As a consequence, decrements in gene expression, impairments in intracellular signaling and cytoskeletal transport, and weakening of trophic support may mediate cholinergic cell atrophy finally leading to the known age-related functional decline in the brain including AMI.
As mentioned in section “During Aging, Neurons Rarely Die but Change at the Level of Cytoskeleton, Synapse, and Synthetic Activity Negatively Affecting Synaptic Plasticity,” during aging, neurons evidently undergo a reduction in the complexity of dendritic arborization and dendritic length. Dendritic spine numbers are also decreased, and since spines are the major sites for excitatory synapses, changes in their numbers reflect a change in excitatory neurotransmission. This theory has been supported by the demonstration of a decrease in glutamate-receptor-mediated excitatory responses, as well as a decrease in the levels of alpha-amino-3-hydroxy-5-methylisoxazole-4-propionic acid (AMPA) and N-methyl-d-aspartate (NMDA) receptor expression during aging. The latter findings are of major importance for understanding aging effects on cortical cognitive functioning since these glutamate-driven ion channel receptors are paramount in intercortical information processing and basic mechanisms such as LTP. Glutamate is also an important player in the aging brain because of its role in both neuroprotection as well as in facilitation of excitotoxic neuronal injury and death. Glutamate, the brain’s predominant excitatory neurotransmitter, facilitates release of brain-derived neurotrophic factor (BDNF) and other neurotrophins and in this way indirectly modulates synaptic plasticity and activity-dependent neuronal survival which implicates a neuroprotective function of this neurotransmitter system. Neurotrophins comprise neuromodulatory functions and closely interact with neurotransmitters. Among neurotrophins, BDNF is the best characterized modulator of normal brain aging. It is a considerable modulator of molecular aging, as it is a neuronal activity-dependent secreted growth factor that declines steadily with age in the brain. It is neuroprotective against a variety of insults emerging in the course of aging and is required for changes in spine density underlying learning and memory systems that decline with age.
The aging process has also clear effects on the most common inhibiting neurotransmitter of the brain gamma-aminobutyric acid (GABA). Its functional expressions such as GABA-A ion channel receptor-mediated inhibitory responses and action potential firing rates are both significantly increased with age. Considering the mechanisms responsible for age- and AD-related neuronal degeneration, little attention has been paid to the opposing relationships between the energy-rich phosphates, mainly the availability of the adenosine triphosphate (ATP), and the activity of the glutamic acid decarboxylase (GAD), the rate-limiting enzyme synthesizing the GABA. It has been postulated that in all neuronal phenotypes, the declining ATP-mediated negative control of GABA synthesis gradually declines and results in age-related increases of GABA synthesis.
Aging Has Serious Consequences for the Calcium Homeostasis of Neurons Which Has a Major Impact on Neuronal Physiology and Signaling
The regulation of intracellular free calcium levels is a crucial phenomenon for the cellular physiology of glial and neuronal cells of the nervous system and has attracted ample attention in aging research. Destruction or impairment of intracellular calcium maintenance is not only essential for understanding breakdown of brain tissue in essentially all neurodegenerative disease, but also for brain aging in general. The reason being that loss of control of free calcium levels has profound consequences for a multitude of cellular neuronal functions. In young nerve cells, free calcium homeostasis is very well maintained by balancing influx and intracellular release of calcium, temporary binding or storage of excess calcium, and transport of excess out of the cell. Calcium concentrations in young neurons show a very low basal level, a peak-like increase upon a variety of activations followed by orchestrated stimulation of calcium targets necessary to perform the required physiological functions, and finally a quick and efficient return to baseline levels (Fig. 7).
Intracellular free calcium concentration in aged versus young nerve cells, baseline levels, and the calcium response upon stimulation of the neuron by the neurotransmitter glutamate or by potassium. Characteristically the baseline levels of free calcium are considerably higher in the aged neuron. Stimulation of the young nerve cell results in a steep rise of calcium, which quickly returns to baseline level when the stimulus ends due to the homeostatic mechanisms. In the aged neuron, the rise of calcium during stimulation is much lower, and the return to baseline levels is very slow. Together this means probably an inadequate physiological response to a temporary stimulus and a constantly high level of free calcium and its damaging consequences on activation of calcium-sensitive enzymatic processes (Adapted with permission from Kirischuk and Verkhratsky (1996))
To appreciate the impact of aging, it is important to understand the basic mechanisms of intraneuronal calcium homeostasis (Fig. 8). Levels of intracellular calcium increase upon activation of ionotropic receptors. Well-known representatives of these receptors are the ion channels that can open by the binding of excitatory amino acids such as glutamate of which the NMDA (N-methyl-d-aspartate) receptor has been extensively studied. Interestingly, the opening of the ion channel of the NMDA receptor is voltage dependently blocked by Mg2+ ions. When glutamate binds to the AMPA receptor due to sodium influx, the membrane potential of the neuron decreases from −70 to −35 mV upon which the magnesium block is removed followed by opening of the glutamate bound NMDA channel and the influx of calcium. This influx of calcium is a strong ion flow which is potentiated by the very high concentration gradient over the neuronal cell membrane between insite and outside of the cell since the extracellular concentration is 104 times the intracellular concentration. A second major calcium rise comes from opening of voltage-dependent calcium channels (VDCC). These calcium channels vary in localization and function, and in the postsynaptic neuron in the brain, the L-type and T-type calcium channels play a role, but of these, the L-type channel is best characterized. L-type channels have a high activation threshold but after opening become slowly inactivated. Upon depolarization, for example, by excitatory amino acids like glutamate but also as a result of any source of depolarization, VDCCs open and allow a strong influx of calcium ions. During aging, the density of L-type calcium channels increases in areas involved in cognitive functions like the hippocampus leading to enhanced inflow of calcium. A third source of increase of intracellular calcium levels comes from activation of G-protein-coupled receptors which are linked to the phosphoinositol system that leads to mobilization of phospholipase C and the formation of inositol triphosphate (IP3) as a splicing product of the membrane phospholipid phosphatidylinositol-biphosphate (PIP2). The second messenger IP3 diffuses into the cytoplasm, binds to its receptors on the membranes of the endoplasmic reticulum, and allows an outflow of calcium from the endoplasmic stores into the cytoplasm. Next to the IP3 channels, the endoplasmic reticulum is endowed with ryanodine-sensitive channels that are gated by the calcium itself and amplify the release of intracellular calcium.
Homeostatic mechanisms of intracellular Ca2+ concentration. The various systems responsible for the maintenance of low Ca2+ levels include plasmalemmal Ca2+-ATPase (PMCA) and Na+/Ca2+ exchanger for calcium clearance out of the cell; Ca2+-binding proteins (Ca 2+ -BP); endoplasmic-reticulum (ER) Ca2+ ATPases; and mitochondria. Ca2+ enters the cell via voltage-dependent Ca2+ channels (VGCC) and ionotropic receptors. The glutamate-operated NMDA channel is the most potent receptor of this latter type. In addition, metabotropic receptors via inositol triphosphate IP3 generation that control the IP3 calcium channels on the ER and Ca2+ gated ryanodine channels can release calcium from intracellular (ER) stores (Adapted with permission from Verkhratsky and Toescu (1998))
In rest conditions, the levels of intracellular calcium are very low. Free calcium can be buffered and bound to calcium-binding proteins like parvalbumin, calmodulin, or calbindin. Excess of calcium will be transported into the endoplasmic reticulum and mitochondria, and in particular the latter storage in the mitochondria during aging will be a source of oxidative stress to the cell. In the normally functioning neuron, however, calcium levels will be quickly brought back to baseline by efflux out of the cell by ion exchange proteins (like Na+/Ca2+ exchange proteins) or ATP-dependent calcium pumps.
Aging has profound effects on neuronal (and glial) calcium homeostasis. The nerve cell loses the capacity to maintain an optimal calcium homeostasis, and baseline calcium levels rise. This creates a condition that will challenge an adequate cellular physiology. Some major contributions to our insight in the effects of aging on calcium homeostasis come from the Kostyuk group in Kiev and Landfield and coworkers in Lexington. Due to changes in calcium channel densities, concentrations in calcium-binding proteins, permeability of ionic glutamate receptor channels, and efflux pumping mechanisms, the intracellular calcium balance changes during aging although not in all brain regions in the same way. In general the typical peak-like rise in calcium upon synaptic stimulations levels off, and the return to baseline concentrations is highly prolonged. Together with the elevated baseline, this means a chronically higher free calcium presence in the aged neuron. Continuous higher calcium levels can have a plethora of effects on receptor proteins including ion channels, membrane lipids, kinases, proteases, and gene expression processes. Calcium-induced oxidative stress and a compromised mitochondrial energy production in the form of ATP as a consequence of the aging process will constitute major hazards to cellular physiology underlying neuronal signaling that is basic to cognitive functioning. As we will see below, chronic high calcium levels in the aged neuron has been associated with enlarged polarization of neurons at the end of the action potential.
Aged Neurons in the Hippocampus Show an Enlarged Afterhyperpolarization Which Parallels Impaired Learning and Conditioning
Cognitive functions of the brain like learning, memory, and attention rely for an important part on frontal and temporal lobes of the forebrain. Since these cortical regions in particular are subject to aging-related functional and structural decline, it appears that the neurons and glia of these brain areas are more than average sensitive to the aging process. The cognitive functions in the aged are subject to subtle changes. So the question remains which mechanisms may be responsible for the physiological decline of neuronal function. One of the answers to this question can be found in the electrophysiological properties of aging nerve cells. Basic to all brain activity is the generation of action potentials by the individual neuron. When the membrane potential decreases upon any source of excitatory activation beyond a critical threshold, an action potential occurs that results from massive opening of sodium channels and influx of sodium ions. After reaching the depolarization peak, sodium channels close, and potassium channels open that allow a fast outward K+ current. The potassium currents are activated by calcium, and since calcium is high during and shortly after the depolarization phase of the action potential, the K+ current leads to an overshoot of the membrane potential which is called the afterhyperpolarization (AHP). Since the baseline calcium concentrations are high in the aging nerve cell, and the K+ current is calcium dependent, the AHP is increased in the aged neuron. This phenomenon was first discovered by Landfield and Pitler in 1984 and was confirmed and extended by others. The calcium-dependent enlarged AHP has serious consequences for the excitability of neurons in the aging brain, in particular in those brain regions involved in cognitive processes.
Prolonged AHP is one of the mechanisms that make neurons more resistant to depolarization and recruitment for participation in neuronal network activity during performance of a cognitive task. Interesting experiments that reveal the impact of aging on AHP and a learning task were carried out by the group of John Disterhoft in Chicago. The learning task they used was trace eye blink conditioning in which animals (or humans) “learn” to associate a tone with an airpuff applied later in time and that leads to an eye blink. Learning is successful when the eye blinks after the tone but before the airpuff. Aged animals perform much worse than young which was directly related to the much larger calcium-dependent AHP. Interestingly when they blocked the calcium influx in the neurons by means of the L-type calcium antagonist nimodipine, the AHP was reduced, the excitability of the neuron increased, and the performance in the eye blink conditioning task greatly improved. Similar type of studies was reported more recently which described the relationship between the magnitude of the AHP in aged rats and the scores of these animals in the Morris water maze as a typical learning test. In these experiments, it could clearly be demonstrated that there is strong correlation between an enlarged AHP and poor memory performance in the water maze (see Fig. 9).
Relations between performance of aged rats in the Morris water maze (a) and the afterhyperpolarization after electrical stimulation of neurons in the CA1 area of the hippocampus (b). Dotted line in (b) is the rest membrane potential. The learning curve in (a) is indicated by the distance that rats swim to escape to a hidden platform in a large water tank. During 5 days of training, it can be appreciated that young and aged-unimpaired rats quickly learn to find the escape platform, whereas aged memory-impaired animals perform much worse. The waveforms in (b) show that the aged memory-impaired rats have a much larger AHP as compared to the young and aged-unimpaired rats, which suggests that an enlarged AHP is a causal factor for impaired memory functions (Adapted with permission from Tombaugh et al. (2005))
Sophisticated research on the consequences of these aging mechanisms was carried out by Carol Barnes and her team on hippocampal neuronal networks during spatial orientation in which place cell assemblies respond to changes in space according to dynamic activity patterns. Aging had profound effects on these pattern dynamics (as mentioned above) that were most likely the result of the deranged calcium homeostasis in the aged cell.
In summary, aging does not so much affect the number or form of the neuron, but it does exert its influence on neuronal plasticity at the level of action potential generation of the individual neuron and subsequently on the dynamics of neuronal activity as they participate in neuronal networks during behavioral and cognitive tasks.
In the Aged Mammalian Brain, Blood Supply Is Decreased and the Vascular Condition Is Subject to Degenerative Mechanisms
Nervous Tissue Is Highly Dependent on Optimal Blood Flow for Its Energy Generation
The central nervous system for performance of its many simultaneous functions is utterly dependent on an adequate and unhampered supply of nutrients for the generation of energy. In particular in an acute sense, the supply of glucose and oxygen is critical, and in a somewhat less acute way the availability of other feeding components such as amino acids for the synthesis of neurotransmitters for neuronal signaling and proteins for neuronal housekeeping. The importance of readily available glucose and oxygen can easily be observed when the blood supply to the central nervous system is obstructed when the larger arterial vessels to the brain become occluded as it occurs in ischemic stroke. Such an ischemic insult in general is the result of long-term narrowing of the arterial lumen as a consequence of atherosclerosis of the vascular wall combined with the presence of a blood clot or thrombus in the brain circulation which results in a vascular occlusion. Notably when larger brain arteries are obstructed, this condition within seconds can lead to loss of consciousness after onset of the occlusion and become the source of severe brain damage in the flow region of a particular vessel if this condition continues.
One of the reasons why brain functions are so quickly influenced by a reduction of cerebral blood flow and thus of glucose and oxygen is the extreme dependence of readily available energy in the form of ATP. Each nerve cell for performance of its signaling functions is dependent on maintaining the gradients of ions between the inside and the outside of its membranes: notably sodium, potassium, but also chloride and calcium. The control of the ionic concentration gradients over the neuronal membrane is paramount to the balance of positive and negative charges between inside and outside of the nerve cell that is basic to the characteristic membrane potential of 65–70 mV in rest conditions. Without a well-controlled membrane potential, the communication between nerve cells by way of action potentials is impossible and silence occurs. Nerve cells have only a very limited capacity to store glucose in the form of glycogen to provide sufficient glucose or the glucose metabolite pyruvate once the regular availability is hampered. If the regular supply route of glucose is entirely blocked as in stroke, the production of ATP within seconds drops from 36 ATP molecules per glucose molecule to 2 ATPs. The consequence of this rapid loss of ATP production will depend on the activity state of the affected neuron, but if blood reperfusion does not occur, the sustained ATP depletion will result in loss of the capacity of ATP-dependent pumping mechanisms to restore the ionic balances over the neuronal membrane necessary to maintain the membrane potential. Massive loss of membrane potential prohibits neuronal signaling which will lead to a variety of behavioral and cognitive dysfunctions dependent on the affected brain area. Loss of consciousness will occur when cortical structures are involved and the communication of the cortical mantle with the thalamic relay structures.
Cerebral Blood Flow Decreases with Climbing Age
Reduction of cerebral blood flow will not always be as dramatic and acute as is the case in pathological conditions like vascular occlusion in ischemic stroke or during the characteristic sudden but transient obstruction of arterial blood flow that are known as transient ischemic attacks (TIAs). Ischemic stroke and TIAs, however, are conditions that commonly (but not exclusively) take place in the aging individual, which already indicates that vascular condition and vascular integrity, combined with spontaneous blood clotting, are associated with the aging process. As already noted reduction of blood flow in the brain in most cases is not dramatic but rather has the nature of a slowly developing condition in the aging period of life. Interestingly the reduction of blood flow is not equally affecting all brain divisions and regions in a similar way. Recent progress of techniques for noninvasive measurement of cerebral blood flow by means of functional magnetic resonance imaging (fMRI) and blood-oxygen-level-dependent (BOLD) signaling measurement has provided detailed knowledge of the dynamics of general blood supply and neuronal activity assessment during the various phases in life (Fig. 10).
Blood-oxygen-level-dependent (BOLD) imaging of individuals during performance of a simple sensory-motor task, that is pressing a key when viewing a flickering checkerboard. BOLD imaging is taken as a measure of brain activation. It can be clearly seen that both motor and visual brain regions are activated, but the response in non-demented older adults (b) and demented older adults (c) is significantly less than in the young adults (a) (Reproduced with permission from Buckner et al. (2000))
There is now ample evidence that during normal aging, there is a significant reduction in cerebral blood flow and BOLD neuronal signaling MRI in those cortical brain regions associated with cognitive function. This reduction in blood supply to the brain and to the cortical mantle in particular has been established both for baseline resting state conditions, but also when individuals perform behavioral and cognitive activities such as a simple sensory-motor task that require activation of the respective brain regions necessary to carry out the task. However, the reduction of blood flow is not equal for all brain regions, and sensory areas appear to react more sensitive to the aging process than motor regions. From such experimental findings, it can be concluded that cerebral blood supply tends to decrease with climbing age which has been correlated to cognitive performance, but also that individual variation within the aged population can be high. Apparently some individuals appear to be much more sensitive to the aging process than others. Besides genetic disposition and development of high blood pressure, other risk factors like feeding pattern, socioeconomic background, and chronic stressful life circumstances are considered to play an important role.
Several causal factors have been identified that can be linked to the age-related reduction in blood flow. Common in especially human aging is the occurrence of atherosclerotic mechanisms that lead to narrowing of major arterial channels that provide the brain with blood. An often measured parameter in that respect is the intima-media thickness of the carotid arteries, and several investigations have indicated a direct association between carotid artery atherosclerosis and cognitive function. For that reason, laser Doppler flow measurement of carotid circulation is often considered to provide a reliable record for threats of adequate cerebral blood supply.
Apart from the changes in major arterial vessels to the brain, the entry of oxygen, glucose, and other nutrients to the neural tissues is for a very large part dependent on the functional integrity of the microvasculature and in particular of the capillary systems of the brain (Fig. 11). There is the general notion that the arteries and arterioles regulate blood pressure, for example, by modulating smooth muscle cell contractility but that the exchange of critical components such as glucose is dependent on the blood–brain barrier structure and its transporter functions. In other words, the larger vessels could be seen as the bulk suppliers of blood volumes, and the enormous number of brain capillaries as the domain of fine regulation for local nutrients and gas delivery and the seat of the blood–brain barrier. In that respect, it can be noted that there is clear difference between brain capillary densities in white matter and gray matter, the latter being the domain of the metabolically much more active nerve cell bodies. Along the same line there is a prominent correlation between capillary density, local blood flow, and glucose utilization in a given brain area.
Electron microscopic image from a brain capillary taken from the cingulate cortex of a young rat (a) and a drawn version of this capillary with the various components of the microvessel. Note the thin layer of cytoplasm of the endothelial cell (ep), the location of mitochondria (em), the characteristic tight junction (tj), the position of the pericytes (p) embedded in a thin and regular layer of the basement membrane (bm). Other abbreviations: a astrocytic endfeet, en endothelial nucleus, l microvascular lumen (Farkas and Luiten 2001)
Moreover brain microdomains that are metabolically very active, such as regions with a high synaptic density, also have the highest capillary densities. Obviously since the distance between vascular lumen and brain parenchyma is shortest between capillaries and neural tissue, and because of the transport systems over the vascular membrane structures, the access of nutrients to the metabolic active components of the brain is most direct in the capillary microdomain. Furthermore, new insights in blood flow regulation give a more prominent role to brain capillaries next to arteries and arterioles than previously considered. The classical concepts were based on the key importance of smooth muscle cells in the arterial wall, but novel research data point to an essential role of the capillary pericytes that are endowed with high levels of contractile proteins. The current concept is that blood circulation in the brain is for a large part oxygen dependent and subject to neuronal and glial regulation at the microvascular level .
Brain Microvessels Undergo a Progressive Structural Degenerative Decline During Aging
The blood–brain barrier consists of specific structural and functional components including the endothelial cells with their tight junctions where their membranes meet, an extracellular matrix of the basement membrane surrounding the endothelial cell, pericytes embedded in the basement membrane, and a layer of astrocytic endfeet. A major role in barrier function has been assigned to the endothelial cell with its characteristic continuous tight junction complexes, the lack or paucity of vesicular transport, high density of mitochondria, and a range of transmembranous transporter proteins. Together this structural complex constitutes the blood–brain barrier which acts as the gatekeeper of entry but also removal of compounds into or out of the brain parenchyma. Its functional and anatomical integrity is critical for the maintenance of the homeostatic stability of the neural tissue.
Study of the capillary ultrastructure in various brain regions including the cerebral cortex in a number of mammalian species including man showed an almost linear decline of the cellular and subcellular condition of the microvascular components (Fig. 12). This decline can be summarized as the local increase of the thickness of the basement membrane, distortion of the endothelial cell structure and its luminal surface, massive pericytic degeneration, and swelling of the surrounding astrocytic terminal endfeet embracing the capillary. The basement membrane thickening is characterized by deposition of various collagen components including packages of collagen type IV with its characteristic periodicity and of which the fibers can run both longitudinal to and circular to the capillary. Degenerating features of microvascular pericytes consist of large amounts of intracellular membranous inclusions and swelling of the cytoplasm. Pericytic degeneration has serious consequences since these cells are key players in the blood–brain barrier, control capillary integrity, and have a major function in microvascular blood flow (Fig. 13).
Electron microscopic microphotographs of characteristic aging-dependent degenerative changes in the capillary wall of microvessels in the cingulate cortex of senescent rats (30 month of age). The endothelial lining can often display an irregular shape and surface (asterisks in (a)), accompanied by an increase of mitochondria indicative for enhanced demand of energy probably for blood–brain barrier transport of nutrients and other components. The basement membrane undergoes considerable thickening by the deposition of collagen of different compositions. The collagen in (b) is clearly stratified by molecular periodicity, while in (a) and (c), the collagen became amorphous. Membrane thickening is accompanied by swelling of perivascular astrocytic endfeet (arrowheads in (c)) (Farkas and Luiten 2001)
Diagrams of characteristic microvascular degenerative changes in the aging vertebrate and human brain. From left to right: an intact capillary; membrane thickening by irregular amorphous depositions (arrows); depositions of collagen packages in the basement membrane (arrows); and degeneration of pericytes (p) filled with intracellular debris. Abbreviations: e endothelial cell, l lumen, en endothelial nucleus (Own work, Fig. 7 in Farkas and Luiten (2001) Prog Neurobiol 64:575–611)
Experimental studies indicate that various conditions affect the microvascular breakdown process during aging, which include high systemic blood pressure, feeding pattern and fatty acid consumption, cerebral hypoperfusion, and blood-borne amyloid, but the most consistent factor is climbing age. Other factors of importance can be loss of cholinergic innervation of cerebral vasculature that finds its origin in the cholinergic basal forebrain nuclei. Such loss of cholinergic cortical innervation is a common feature of AD, but degeneration of distal cholinergic fibers in the cortical mantle is probably also a regular phenomenon in the aging mammalian brain as can be observed in the aging rodent forebrain. Loss of cholinergic vascular innervation has serious consequences for cerebral blood flow which was experimentally demonstrated by the flow reduction as a consequence of experimental lesions of cholinergic basal forebrain neurons.
Quantification of microvascular aberrations during aging shows some variation that depends on species, brain region, and risk conditions like hypertension, experimental reduction of blood flow, or diet composition. In rat cortex, microvascular aberrations affect 20 % of the capillaries but can increase to 50 % in spontaneously hypertensive strains. The hippocampal region appears to be more sensitive to the aging process with 30 % of the microvessels affected in aged normotensive animals. This percentage is even higher in hippocampus of highly aged rhesus monkey of 30 years adding up to 60 % of affected capillaries. In the aging human brain, the microvascular pathology is similar in nature as in aging mammals, but the number of degenerating capillaries appears to be lower in number. This may be related to treatment of hypertension which is almost a common feature in western nations. However, when comparing non-pathological aging to age-associated diseases like AD, Lewy body dementia, or Parkinson’s disease with dementia, cortical capillary degeneration is more than doubled and amounts to 35 % of cortical microvessels. It is not known whether this high frequency of capillary aberration is a consequence of the disease or a causal factor in the development of the pathological condition.
Cortical Microvascular Decline Correlates with Cognitive Decline
It is not precisely clear how age-related structural changes in the microvascular system exert their influence on cognitive performance during aging (Fig. 14). However, several human studies indicate that the reduction of cerebral blood flow correlates strongly with the cognitive decline in dementing disorders. It is also known from animal studies in which cerebral blood flow was experimentally reduced that the number of degenerating microvessels correlates significantly with the performance of these animals in cognitive tests like the Morris water maze. Such findings and other supportive data have led to the hypothesis that links microvascular breakdown processes to loss of microvascular flexibility and concomitant changes in the blood–brain barrier transport capacity of nutrient supply. Dysfunctioning microvasculature as a result of impaired capacity to respond to metabolic demands of the surrounding neural tissue, degeneration of its structural components, and changes in the transport functions of the blood–brain barrier pose a challenge to the metabolism of neurons and glia reminiscent of a state of mild but chronic ischemia. Such a complex of a gradually deranged physiological environment forms a challenge to neuronal energy dynamics, formation of oxygen radicals, and oxidative stress, which will affect the neuronal and glial calcium homeostasis. The loss of homeostatic mechanisms in neurons during aging appears to be one of the leading underlying principles of age-related impairment of neuronal physiology and efficiency of neuronal signal generation and transduction which eventually becomes expressed in AMI.
Diagram with hypothesis on interrelations between microvascular degenerative processes and cognitive dysfunctions. Conditions like high age, alone or in combination with hypertension, breakdown of the cholinergic innervation of forebrain vasculature, or blood-borne amyloid-β protein will lead to a gradual loss of vasoregulation processes of microvasculature accompanied by a variety of degenerative changes of the microvascular wall. These microvascular aberrations will have their consequences for the transport machinery of the blood–brain barrier of which the glucose transporter has a direct and immediate effect on supply of key nutrients. In a chronic condition, this will affect the activity level of the mitochondria that are highly dependent on unhampered availability of energy sources which has its consequences for ATP production and formation of reactive oxygen species. This, in turn, will exert its influence on neuronal and glial physiology and the physiological functions of the neuronal substrate underlying the cognitive brain ultimately ending up in cognitive failure (Own work, Fig.19 in Farkas and Luiten (2001) Prog Neurobiol 64:575–611)
The Innate Inflammatory System of the Brain Can Both Damage and Protect the Brain Against Breakdown Processes
Challenging Conditions in the Brain Lead to Activation of Microglia
Microglia cells are cells of mesodermal origin and thus a group of cells that do not belong to the neuroectodermal line of endogenous CNS cells like neurons, oligodendrocytes, and astrocytes. Microglia and their precursors invade the CNS during early embryonic development and serve as CNS-specific tissue macrophages. The primary function of microglia and astrocytes (macroglia) is the maintenance of tissue homeostasis including the active regulation and modulation of the neuronal circuit and the defense and repair upon cellular stress, infection, trauma, and other injuries. For these purposes, neurons, astrocytes, and microglia interact in a dynamic way. Resting microglia appears always in a ramified shape with fine cellular processes moving around and actively scanning their cellular environment. Upon sensing of any homeostatic disturbance, microglia change their shape and can induce tissue remodeling, inflammation, and neurogenesis. For this purpose, microglia are able to induce a broad spectrum of molecules such as cytokines and chemokines, and can serve as antigen presenting cells. These possibilities enable microglia to trigger a cascade of responses inducing the attraction of peripheral immune cells through the blood–brain barrier which can finally end in a massive inflammatory response including the induction of apoptosis, but they are also important in the finalizing of an inflammatory reaction, removing of cell debris, and cell survival.
Neuroinflammatory Mechanisms and Release of Cytokines by Microglia Can Protect Against External Threats
The communication and interaction between microglia or the immune system and neurons – in close physical contact – is essential for the maintenance of brain function and homeostasis but also for the modulation of neurological functions and dysfunctions. The first line of defense is the innate immune response. Innate immune cells such as microglia in the CNS detect potential disturbances in their environment via pattern-recognition receptors that recognize infections as well as tissue damage. They respond by synthesizing and releasing cytokines such as interleukin-1β (IL-1β), IL-6, and tumor necrosis factor-α (TNF-α) which mediate the immune response. These cytokines, however, can also lead to the breakdown of the blood–brain barrier and the infiltration of peripheral immune cells.
Cytokines (also stemming from peripheral organs) can induce the so-called sickness behavior, a mixture of lethargy, decreased activity, and retraction from social interactions, which goes together with other responses to infections like increased sleep, higher body temperature, decreased food intake, and activation of the hypothalamic-pituitary axis. This general sickness response is thought to promote resistance to pathogens and to recovery from infection.
Besides the response to intruding pathogens, microglia and other immune cells also monitor the state of tissue damage and can induce a transformatory process called tissue repair. This can also include signals to induce apoptosis of badly damaged cells at the same time when other cells get trophic support.
Microglia can activate the neuroinflammatory response by expressing proinflammatory cytokines such as TNF-α, IL-1α, and ILβ or IL-6. Although the proinflammatory responses are often reported as part of a pathological process, most inflammatory processes are actually protective in nature (Fig. 15). TNF-α, for example, can induce apoptosis via its TNF receptor-1, whereas TNF receptor-2 counteracts this effect and triggers a neuroprotective signaling cascade via protein kinase B (PKB/Akt) and nuclear factor kappa B (NF-kB). Interestingly this neuroprotective signal is enhanced by the ionotropic NMDA glutamate receptor and therefore reveals a direct interaction of neuronal and immune signals at the molecular level.
TNF cell survival signaling in neurons. TNF-induced signaling via its two receptors. Tumor necrosis factor plays an important role in guiding the cell through stress situations. The two receptors for TNF can have therefore extremely opposite functions: with TNFR1-mediated apoptosis and TNFR2-mediated pro-survival pathways. Depending on the surrounding situation, the TNF system allows cells not only to respond by cellular restructuring, adaptation, and modulation of the surrounding immune response by activating either pro- or anti-inflammatory responses. One key signaling mechanism in achieving this is the activation of the transcription factor NF-kB (p50/p65). Both TNFRs are able to activate this transcription factor by separate signaling mechanisms and with different kinetics. Anti-apoptotic activation of NF-kB via TNFR2 in neurons is achieved by co-signaling with the ionotropic glutamate receptor NMDAR. Together they can activate protein kinase B/Akt which activates a long-lasting NF-kB activation which leads to neuronal survival. Abbreviations: DD death domain, cIAP cellular inhibitor of apoptosis, FADD Fas-associated death domain protein, IkBα inhibitor of kappa B, NFkB nuclear factor kappa B, PKB/Akt protein kinase B/serine-threonine kinase, PI3K phosphoinositide 3-kinases, RIP receptor-interacting protein, TRADD TNF receptor-associated death domain, TRAF TNF receptor-associated factor, TNF tumor necrosis factor, TNFR1 tumor necrosis factor receptor-1, TNFR2 tumor necrosis factor receptor-2
The Dynamic Activation of Microglia Changes in Later Life
During normal aging, microglia become more sensitized, which means they react faster and stronger upon activation. This effect, also known as priming, results in a more rapid induction of activation and increased cytokine release. Primed microglia seem to stay in an intermediate activation state. Microglia priming was first described in chronic neurodegenerative diseases but seems also to be a part of the aging process of the brain. Several indicators support this view: Microglial expression of MHCII, a marker for microglial activation, is increased in aged but healthy brains along with other cell surface markers and cell adhesion molecules. In addition, it was shown that aged microglia expresses higher amounts of IL-1β, IL-6, and TNF-α. As these cytokines are normally considered to be proinflammatory, it is of some importance that at the same time anti-inflammatory cytokines such as IL-10 and IL-4 are decreased. These findings are accompanied by findings that during aging, genes involved in oxidative stress, inflammation, and glial activation are upregulated whereas those associated with synaptic, transport, and restorative functions decrease. This leads to a rather pro-inflammatory and less flexible phenotype. Age-related priming of microglia leads to an exaggerated immune response following challenges. Prolonged and/or chronic increase of cytokines such as IL-1β, IL-6, and TNF-α leads to extended sickness response, impaired cognition, and depressive behaviors.
Neuroinflammatory Processes Affect Cognitive Functions During Aging
To estimate the grade of influence that the immune system has on brain functions, one should consider, for example, the mood changes at the onset of a common cold. So it is no wonder that a direct influence of components of the immune system on basic neuronal functions can be observed. Proinflammatory cytokines such as IL-1b, IL-6, and TNF-α directly influence LTP. Glia actively participates in the homeostatic activity-dependent regulation of synaptic activity by the release of TNF-α. TNF-α also increases the expression of AMPA receptors and influences synaptic scaling. In addition to the modulatory function in neuronal networks, cytokines and microglia are also considered to be involved in the development of depression. As depressive and sickness behavior have a lot in common, a new concept considers a neuroinflammatory response at the basis of major depression. In fact, peripheral as well as centrally applied lipopolysaccharides (LPS) can induce an inflammatory response in the brain and can induce in animal models depressive-like behavior. These effects can be mimicked by various proinflammatory cytokines. It has been argued that these mechanisms come into play during development of late-onset depression in the elderly. The modulatory function of cytokines is of great interest when we consider their constitutive upregulation during healthy aging but also in neurodegenerative diseases is considered. With primed microglia during aging in a more proinflammatory state, with more exaggerated responses to stimuli, the modulatory role of cytokines on cognitive functions and mood functions and depression, it is now becoming better understood which important role the immune response plays in AMI and why aged people are more prone to develop depressive symptoms.
Outlook
Aging of the brain is more relevant than ever given that life expectancy is nearly doubled in the twentieth century. As some say, “the aging boom is upon us.” Although the science of aging is developing rapidly, it still has to come of age. Many of the fundamental underpinnings of brain aging remain unclear and require continuous and extended research efforts of a multidisciplinary nature. Neurobiological, genetic, biochemical, and physiological processes need to be interconnected to fully appreciate and understand the maintenance machinery to keep the brain going at a high level of cognitive performance – even at an age of 85 and beyond as is anticipated to be the average life expectancy in the near future. We expect that many more secrets of how to age healthy will be unraveled in the near future, and this chapter provides some of key topics in which such discoveries may arise.
There is no doubt that we will experience a burgeoning increase in scientific knowledge on the aging brain. Most, if not all, nations in the world are confronted with an aging population, and since most health problems and problems of well-being manifest themselves in the later phases of human life, this is becoming a matter of global dimensions. Aging is a phenomenon with a large number of interacting and interdependent variables. When we can more fully understand these factors that determine the functioning of the aged individual, we could make predictions on how to adapt to lifestyle and (preferably noninvasive) treatments in order to achieve a better health condition, guarantee independent living, and delay the onset of aging-associated disease. It is obvious from many scientific sources that the fate of the aged brain already starts with the beginning of life with the genetic capital we are endowed with. Furthermore, complex factors like food quality and food composition, education and upbringing, chronic stress levels, hygiene, available health care during the various life phases including pregnancy, exposure to disease in early life, and so on all exert their influence on the aging process. No doubt that the collective information on all these determining factors will be leading to a better insight in healthy aging conditions. For example, we know that perinatal stress makes the brain more sensitive to later life ischemic events, we know that lipid composition in the daily diet affects brain vessel condition and blood pressure, we know that calcium inhibiting drugs can improve learning performance in aging, we know that high levels of stress hormones enhance the formation of the neurotoxic amyloid proteins, and we know that regular motor activity promotes the formation of new neurons. These are just a few examples of how we could influence our aging brain in a positive way based on recent scientific insights.
Abbreviations
- AD:
-
Alzheimer’s disease
- AHP:
-
Afterhyperpolarization
- AKAP:
-
A-kinase-anchoring protein
- AMI:
-
Aging-related memory impairment
- AMPA:
-
Alpha-amino-3-hydroxy-5-methylisoxazole-4-propionic acid
- ApoE:
-
Apolipoprotein E
- APP:
-
Amyloid precursor protein
- ARA:
-
Arachidonic acid
- Arc:
-
Activity-regulated cytoskeletal gene
- ATP:
-
Adenosine triphosphate
- Aβ:
-
Amyloid beta
- BDNF:
-
Brain-derived neurotrophic factor
- BOLD:
-
Blood-oxygen level dependent (imaging)
- CA1:
-
Cornu ammonis1 (2,3)
- CAMK:
-
Calcium-calmodulin kinase
- CNS:
-
Central nervous system
- DA:
-
Dopamine
- DHA:
-
Docosahexaenoic acid
- fMRI:
-
Functional magnetic resonance imaging
- GABA:
-
Gamma-aminobutyric acid
- GAD:
-
Glutamic acid decarboxylase
- IEG:
-
Immediate early genes
- IL-1:
-
Interleukin-1 (4 6, 10)
- IP3:
-
Inositol triphosphate
- LPS:
-
Lipopolysaccharide
- LTP:
-
Long-term potentiation
- MWM:
-
Morris water maze
- NF-kB:
-
Nuclear factor kappa B
- NGF:
-
Nerve growth factor
- NMDA:
-
N-methyl d-aspartate
- PFC:
-
Prefrontal cortex
- PIP2:
-
Phosphatidylinositol-biphosphate
- PKB:
-
Protein kinase B (Akt)
- PKCγ:
-
Protein kinase C gamma
- PUFA:
-
Polyunsaturated fatty acid
- RACK:
-
Receptor for activated C-kinase
- TIA:
-
Transient ischemic attack
- TNF:
-
Tumor necrosis factor
- VDCC:
-
Voltage-dependent calcium channel
References
Barcelo-Coblijn G, Hogyes E, Kitajka K, Puskás LG, Zvara A, Hackler L Jr, Nyakas C, Penke Z, Farkas T (2003) Modification by docosahexaenoic acid of age-induced alterations in gene expression and molecular composition of rat brain phospholipids. Proc Natl Acad Sci U S A 100:11321–11326
Bishop NA, Lu T, Yankner BA (2010) Neural mechanisms of ageing and cognitive decline. Nature 464:529–535
Buckner RL, Snyder AZ, Sanders AL, Raichle ME, Morris JC (2000) Functional brain imaging of young, nondemented, and demented older adults. J Cogn Neurosci 12(Suppl 2):24–34
Burke SN, Barnes CA (2006) Neural plasticity in the aged brain. Nat Rev Neurosci 7:30–40
Dickstein DL, Kabaso D, Rocher AB, Luebke JI, Wearne SL, Hof PR (2007) Changes in the structural complexity of the aged brain. Aging Cell 6(3):275–284
Disterhoft JF, Oh MM (2006) Learning, aging and intrinsic neuronal plasticity. Trends Neurosci 29:587–599
Farkas E, Luiten PGM (2001) Cerebral microvascular pathology in aging and Alzheimer’s disease. Prog Neurobiol 64:575–611
Fontaine V, Mohand-Said S, Hanoteau N, Fuchs C, Pfizenmaier K, Eisel U (2002) Neurodegenerative and neuroprotective effects of tumor necrosis factor (TNF) in retinal ischemia: opposite roles of TNF receptor 1 and TNF receptor 2. J Neurosci 22:RC216 (1)–RC216 (7)
Gaykema RP, Nyakas C, Horvath E, Hersh LB, Majtenyi C, Luiten PG (1992) Cholinergic fiber aberrations in nucleus basalis lesioned rat and Alzheimer’s disease. Neurobiol Aging 13:441–448
Geinisman Y, Berry RW, Disterhoft JF, Power JM, Van der Zee EA (2001) Associative learning elicits the formation of multiple-synapse boutons. J Neurosci 21:5568–5573
Havekes R, Abel T, Van der Zee EA (2011) The cholinergic system and neostriatal memory functions. Behav Brain Res 221:412–423
Kirischuk S, Verkhratsky A (1996) Calcium homeostasis in aged neurons. Life Sci 59:451–459
Landfield PW, Pitler TA (1984) Prolonged Ca2+ -dependent afterhyperpolarization in hippocampal neurons of aged rats. Science 226:1089–1092
Mattson MP (2007) Calcium and neurodegeneration. Aging Cell 6:337–350
Nimmerjahn A, Kirchhoff F, Helmchen F (2005) Resting microglial cells are highly dynamic surveillants of brain parenchyma in vivo. Science 308:1314–1318
Ostroveanu A, Van der Zee EA, Dolga AM, Luiten PG, Eisel UL, Nijholt IM (2007) A-kinase anchoring protein 150 in the mouse brain is concentrated in areas involved in learning and memory. Brain Res 1145:97–107
Stellwagen D, Malenka RC (2006) Synaptic scaling mediated by glial TNF-a. Nature 440:1054–1059
Tombaugh GC, Rowe WB, Rose GM (2005) The slow afterhyperpolarization in hippocampal CA1 neurons covaries in aged Fisher 344 rats. J Neurosci 25:2609–2616
Van der Zee EA, Naber PA, Disterhoft JF (1997) Age-dependent changes in the immunoreactivity for neurofilaments in rabbit hippocampus. Neuroscience 79:103–116
Van der Zee EA, Palm IF, O’Connor M, Maizels ET, Hunzicker-Dunn M, Disterhoft JF (2004) Aging-related alterations in the distribution of Ca(2+)-dependent PKC isoforms in rabbit hippocampus. Hippocampus 14:849–860
Verkhratsky A, Toescu EC (1998) Calcium and neuronal aging. Trends Neurosci 21:2–7
Wood WG, Schroeder F, Igbavboa U, Avdulov NA, Chochina SV (2002) Brain membrane cholesterol domains, aging and amyloid beta-peptides. Neurobiol Aging 23:685–694
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this entry
Cite this entry
Luiten, P., Nyakas, C., Eisel, U., van der Zee, E. (2016). Aging of the Brain. In: Pfaff, D., Volkow, N. (eds) Neuroscience in the 21st Century. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-3474-4_84
Download citation
DOI: https://doi.org/10.1007/978-1-4939-3474-4_84
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-3473-7
Online ISBN: 978-1-4939-3474-4
eBook Packages: Biomedical and Life SciencesReference Module Biomedical and Life Sciences