Abstract
Radiation is one of the few accepted risk factors for thyroid cancer. The majority of radiation-induced thyroid carcinomas are well-differentiated papillary carcinomas. Children treated with X-rays for various benign conditions were found to be at increased risk of developing thyroid cancer. Likewise, survivors of the atomic bomb exposures in Hiroshima and Nagasaki, Japan, who were under age 20 at the moment of exposure, were at increased risk of developing thyroid cancer. Latency periods are typically ten or more years, and it appears that excess risk persists for decades after exposure. A pooled analysis of seven major studies over a wide range of doses demonstrated an excess relative risk (ERR) of 7.7 per Gy. In individuals exposed before age 15, linear models best describe the dose–response relationship. Without question, the Chernobyl accident was the worst technological disaster in the history of nuclear power generation. Analysis of post-Chernobyl thyroid carcinomas has demonstrated conclusively that 131I is a thyroid carcinogen in children and adolescents. A linear dose–response relationship has also been documented in children exposed to Chernobyl fallout, with an ERR of 5.25 per Gy after one decade. Molecular analyses have revealed that the mechanism of Chernobyl radiation-induced papillary thyroid cancer pathogenesis is primarily related to double-stranded DNA breaks leading to chromosomal translocations and/or inversions and gene rearrangements. The ret/PTC3 rearrangement was most common in early (prior to 10 years) post-Chernobyl papillary thyroid carcinomas, whereas ret/PTC1 was more common after a 10-year latency period.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Radioactive iodine
- X-rays
- Atomic bomb exposures
- Radioactive fallout
- Excess relative risk
- Dose–response relationship
- Nuclear power plant
- Chernobyl accident
- Gomel oblast
- Republic of Belarus
- ret oncogene
- ret/PTC1
- ret/ PTC3
Radiation is one of the few accepted risk factors for thyroid cancer. Numerous studies have confirmed that the thyroid gland is one of the most radiation-sensitive human organs and that thyroid cancer is one of the most common radiogenic malignancies. Analysis of these studies is problematic, however, owing to difficulties in dose assessment, long-term follow-up of thousands of exposed subjects, definition and confirmation of pathological diagnoses, and differences in exposure modalities.
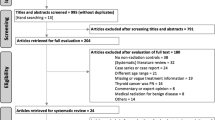
The first part of this chapter briefly outlines the nature and methods of the most significant studies to date and analyzes the data available to define the characteristics of the risks of radiation to the thyroid on subsequent development of thyroid cancer. The second part of the chapter presents an update on thyroid cancer in children exposed to fallout from the Chernobyl accident. Terminology used throughout the chapter is defined in Table 7.1.
Pathology
Knowledge of the pathology of radiation injury to the thyroid is essential to understanding the data from previous long-term follow-up studies. Thyroid glands exposed to external beam or 131I radiation show a variety of histological abnormalities, most often multinodularity, distorting fibrosis, oncocytic change, and chronic inflammation [1–3]. At higher (>1.5 Gy) doses, hyperplastic nodules may show cytologic atypia, which requires careful scrutiny to distinguish from malignancy [4]. The incidence of benign adenomas in patients who received thyroid irradiation is also greatly increased over nonirradiated individuals, as demonstrated by virtually every study of such populations. Many studies failed to distinguish between benign nodules and carcinoma and are therefore excluded from this discussion.
As early as 1949, Quimby and Werner [5] suggested the possibility of a relationship between radiation and the subsequent development of thyroid carcinoma. Winship and Rosvoll [6] began collecting data on children with thyroid cancer in 1948, and their final report on 878 cases worldwide represents the largest to date. They found a history of radiation in 76 % of 476 children with available records. Most received radiation for enlarged thymus or tonsils and adenoids, with an average thyroid dose of 0.512 Gy and an average interval to diagnosis of 8.5 year; 72 % of the cancers were of papillary type, and 18 % were follicular. Cervical lymph node metastases were present in 74 % of cases, with bilateral neck disease in 32 %. Nearly 20 % had pulmonary involvement, generally at presentation. The authors noted a sharp rise in thyroid cancer incidence in 1945, with the greatest number of cases presenting between 1946 and 1959. They attributed the subsequent decline to the curtailment of the practice of head and neck irradiation in children.
A number of additional studies [7, 8] have confirmed that the majority of radiation-induced thyroid carcinomas are well-differentiated papillary adenocarcinomas that more frequently present with extrathyroidal spread and bilateral thyroid lobe involvement but with similar recurrence and mortality rates to tumors in nonirradiated patients. The patients are also younger at diagnosis, usually less than 35 years of age, with an average interval to clinical presentation of 25–30 year. The incidence of radiation-induced thyroid carcinoma appeared to increase from 1940 to at least 1970, but since the discontinuation of widespread use of X-ray therapy in infancy, this trend has decreased [9, 10].
Clinically occult papillary microcarcinomas are generally not included in analysis of these data, but they are often detected by pathologists examining thyroids removed for larger benign nodules. Autopsy studies have demonstrated prevalence rates of papillary microcarcinoma (≤1 cm diameter) of up to 33.7 % in general populations, and ethnic and/or geographic differences exist [11, 12] (see Chap. 2). The prevalence of carcinoma is also dependent on the extent of surgery, the amount of resected thyroid tissue processed for histological assessment, and the absolute number of sections examined by the pathologist [13]. Care is required in evaluating studies with regard to these issues.
Although radiation exposure has a role in the development of clinical papillary carcinoma, the extent of such risk in a given population cannot always be ascertained, as the number of people at risk may be unknown. Currently, it is estimated that 9 % of thyroid cancers may be attributable to radiation [14]. Because radiation-induced thyroid carcinomas rarely include the more aggressive anaplastic and medullary types, its fatality rate is between 3 and 9 % [15].
A small but significant number of patients with anaplastic thyroid carcinoma have had a history of prior exposure to external irradiation or 131I. Such therapy for differentiated thyroid cancer might theoretically induce transformation to an anaplastic carcinoma, but because most cases of anaplastic carcinoma show areas of differentiated tumor, this phenomenon may be an aspect of the natural history of these tumors and may therefore not be a consequence of radiation [16].
Prior Studies
External Radiation
Introduction
From 1920 to 1960, radiation was commonly used to treat a variety of benign conditions, including several head, neck, and upper thoracic sites, which resulted in thyroid gland exposure. In 1950, Duffy and Fitzgerald [17] found that 9 of 28 children with thyroid cancer had received prior irradiation of the thymus as infants. Subsequent reports [18, 19] confirmed the risk of thyroid cancer in children exposed to high-dose radiation and the use of radiation to treat benign disease slowly diminished. Also, the risk of radiation has been analyzed in patients treated for malignant disease, in occupational settings, and in situations of inadvertent exposure.
Atomic Bomb Survivors
A fixed cohort of nearly 80,000 survivors of the atomic bomb exposures in Hiroshima and Nagasaki, Japan, has been followed since 1958 by the Atomic Bomb Casualty Commission and its successor, the Radiation Effects Research Foundation. In a comprehensive report [20] on the incidence and risk estimates for solid tumors diagnosed between 1958 and 1987, the thyroid had one of the highest solid tumor risk estimates in the Life Span Study cohort, with occult tumors excluded. The mean estimated thyroid dose was 0.264 Sv, and a strong linear dose–response was demonstrated. Persons exposed when younger than age 10 year had an excess relative risk (ERR) of 9.46, over three times greater than those in their second decade (see Table 7.2). Although earlier studies [21] suggested otherwise, this report [20] showed that those individuals over the age of 20 year at the time of the blast had no excess of thyroid cancer. Mortality data from the Life Span Study contributed little support for an increased risk of thyroid cancer, because the disease causes so few deaths [22].
Cervical Tuberculous Adenitis
Tisell and colleagues [23] evaluated 444 patients treated with X-rays for cervical tuberculous lymphadenitis between 1913 and 1951 in Göteborg, Sweden. The mean age at irradiation was 19 years, with almost 50 % of patients between 15 and 24 years of age. The calculated absorbed dose to the thyroid ranged from 0.40 to 50.90 Gy (median: 5.2 Gy; mean: 7.2 Gy); 25 thyroid cancers were found, all but one palpable, with a mean observation time of 43 years. The mean and median latency periods were 40 year to diagnosis. A positive correlation was shown between absorbed dose and the probability of developing carcinoma, even after doses of more than 20 Gy. No significant correlation between age at irradiation and the risk of developing cancer was detected.
Cutaneous Hemangioma
Furst and coworkers [24] conducted follow-up with 18,030 patients with skin hemangioma who were treated with external beam radiation between 1920 and 1959 at the Karolinska Hospital. At the time of therapy, 82 % were less than 1 year of age (median age: 6 months). Treatment methods varied, but the relative risk (RR) of thyroid cancer was only slightly increased (1.18) in the group treated with radium-226 or orthovoltage X-rays. In patients receiving contact X-rays or no radiation, no increased risk was noted. An estimation of absorbed thyroid doses was not made.
A similar analysis [25] of a cohort of 14,351 infants less than 18 months of age (mean: 6 months) irradiated for hemangioma during the period of 1920–1959 in Stockholm covered 406,355 person-years at risk, with a mean follow-up of 39 years. The mean absorbed thyroid dose was 0.26 Gy. The Swedish Cancer Registry documented 17 thyroid cancers. Excess cancers began 19 years after radiation and persisted for at least 40 year following radiation therapy (see Table 7.2).
Another study [26] involved 11,807 infants treated with radium-226 between 1930 and 1965 in Göteborg, Sweden, at a median age of 5 months. The mean absorbed thyroid dose was 0.12 Gy. Follow-up through the Swedish Cancer Registry yielded 15 thyroid cancers (ERR = 7.5/Gy; see Table 7.2).
Tonsils/Adenoids
Extensive data has been reported by Schneider and colleagues [27–30] from long-term follow-up studies of more than 5300 subjects who received external radiation for various benign head and neck abnormalities, principally for enlarged tonsils and adenoids, during 1939–1962. In analyzing 4296 of these individuals with an average age at first exposure of 4.4 years and an average thyroid dose of 0.59 Gy, they found that ERR was 3/Gy for thyroid cancer (see Table 7.2). With a mean follow-up of 33 years, the majority of cases occurred in the interval between 20 and 40 year after radiation therapy, peaking at 25–29 years, with a significant decline in risk with increasing age at exposure [27]. Additional data from this source includes information on the effect of screening, as well as characteristics of the secondary thyroid cancers. The authors documented recurrent malignancy in 13.5 % of the 296 patients with thyroid cancer, nearly all within 10 year after primary tumor resection. Significant risk factors for recurrence were the size of the primary lesion, number of lobes involved, histological type, vessel invasion, and lymph node metastasis [28]. Longer-term follow-up of 118 cases occurring before intensive screening showed recurrences in 23.7 % of this total; 39 % of cancers in children recurred vs 15.6 % in adults. This established an inverse relationship between the frequency of recurrence and the patient’s age at surgery (also between the frequency of recurrence and latency period between radiation and surgery). Age at radiation and treatment dose were not related to recurrences [29]. Another aspect explored in this group was the possibility of a radiation sensitivity within the population at risk. Patients with secondary salivary gland and/or neural tumors of the head and neck region had a significantly increased frequency of thyroid cancer compared to patients with neither of these tumors, suggesting that additional factors, such as radiation sensitivity, may account for this increased risk [30].
Acne
Paloyan and Lawrence [31] found that 20 of 224 patients referred for thyroidectomy for solitary nodules had received antecedent radiation for the treatment of acne vulgaris. Of the 20 patients, 12 had thyroid cancer 9–41 years after radiation therapy. Complete records were unavailable, and no statistical analysis was reported.
Thymus
Analysis of radiotherapy’s effect for thymic enlargement in infancy on subsequent neoplastic disease was initiated by Hempelmann and colleagues in Rochester, New York, in the 1950s. They established that the risk of cancer was proportional to the thyroid dose and raised concern that persons of Jewish ancestry might be at greater risk [32]. Extended 37-years average follow-up [33] of 2657 of these exposed infants and 4833 of their siblings via mail surveys through 1986 confirmed a linear dose–response relationship, with an ERR of 9/Gy (see Table 7.2). The median age at radiation therapy was 5 weeks, and 95 % were under 34 weeks of age. Estimated thyroid doses ranged from 0.03 to over 10 Gy, with a mean of 1.36 and median of only 0.3 Gy. None of the dose fractionation variables examined (dose per fraction, number of fractions, and interval between fractions) was significant in modifying risk.
Tinea Capitis
A major long-term study [34] of 10,834 subjects who received X-ray therapy for tinea capitis between 1948 and 1960 in Israel was compared with the effects with a similar number of nonirradiated individuals and 5392 nonirradiated siblings. All irradiated subjects were under 16 years old at the time of treatment, with a mean age of 7.4 years. The mean thyroid dose was 0.093 Gy, with the dose highly inversely correlated with age at exposure owing to the proximity of the thyroid to the X-ray fields in smaller children. The Israel Cancer Registry documented 98 thyroid cancers, showing a mean interval of 17.1 years from radiation therapy to diagnosis. A much higher excess risk of thyroid cancer was found than in other studies (Table 7.2), possibly relating to the underestimation of thyroid doses as a result of patient movement. An increased risk in Jewish patients may also have been a factor.
A similar study of 2215 children irradiated for tinea capitis in New York found no thyroid cancers through a mailed questionnaire after an average 20.5-year follow-up [35]. However, there were less than 300 females, and the expected number of thyroid cancers would have been only 2.9 [36]. The mean age at treatment was 7.9 years; the estimated thyroid dose was 0.06 Gy [35].
Previous Malignancy
Tucker and colleagues [37] reported on the experience of the Late Effects Study Group, which followed a roster of 9170 patients surviving any type of malignancy in childhood for over 2 years. The period of risk extended to death, the last follow-up, or the date of developing any form of second malignancy, whether of the thyroid or not. The mean age at initial tumor diagnosis was 7 years, and 45 % of all patients were less than 5 years old. The duration of follow-up beginning 2 years after initial diagnosis was 2–48 years (mean: 5.5 years), with an aggregate follow-up of 50,609 person-years. The radiation dose to the thyroid ranged from 0 to 76 Gy (mean: 12.5; median: 3.6 Gy). The authors documented 23 secondary thyroid cancers through their 13 centers, yielding a 53-fold increased risk over matched controls, and a significantly increased RR was shown among those with early age at initial cancer diagnosis. All the thyroid cancer patients had received at least 1 Gy to the thyroid.
A study of 1787 patients treated for Hodgkin’s disease [38] at Stanford University between 1961 and 1989 included 1677 patients who had thyroid radiation, most receiving 44 Gy. The mean age at time of treatment was 28 years (range: 2–82 years). After an average follow-up of 9.9 years, they found six thyroid cancers 9–19 (median: 13) years after therapy began for a RR of 15.6 times expected. The age of these six patients ranged from 5 to 32 years at the time of exposure.
Additional studies [39–43] have assessed the risk of radiation therapy for malignancies on the subsequent occurrence of thyroid and other second cancers. These include investigations of large populations of women treated for uterine cervical cancer and males with testicular malignancy; no increased risk of secondary thyroid cancer has been demonstrated, but one such study in women found a slight insignificant excess (RR =1.1; [39]). In this study, as well as the others, the thyroid gland was outside the field of direct radiation, and the estimated average thyroid dose was 0.15 Gy.
Occupational Exposure
Occupational exposure to low-dose radiation has been analyzed in large studies of workers in the nuclear industry. In a report on mortality among radiation workers in the United Kingdom, thyroid cancer was the only malignancy for which the standardized mortality ratio was raised, but the ERR was low (1.05/Sv; [44]). A similar study of employees of the UK Atomic Energy Authority demonstrated a slight, nonsignificant increase in mortality from thyroid cancer [45]. Additional mortality studies in the United States [46–48] failed to demonstrate excess thyroid cancer deaths among nuclear materials workers.
A study of cancer incidence among medical diagnostic X-ray workers in China [49] found seven thyroid cancers in 27,011 individuals employed between 1950 and 1980, with nearly 700,000 person-years of observation. Thyroid cancers were increased among workers employed for 10 year or more and among those who began such work before 1960. No dosimetry measurements were obtained. A study of more than 143,000 members of the American Registry of Radiologic Technologists [50] from 1926 to 1982, who were evaluated through questionnaires, revealed a total of 220 self-reported thyroid cancers vs an expected number of approx 100 cases. However, these data do not include confirmation of the diagnoses, nor are thyroid dose estimates available.
Mortality analysis by review of death certificates of British radiologists who died between 1897 and 1976 failed to demonstrate an excess of thyroid cancers [51]. Similar mortality data from North American radiologists did not demonstrate any excess deaths from thyroid cancer compared to other specialty physicians during 1920–1969 [52].
Prenatal Exposure
The cancer risk of prenatal irradiation has been analyzed in atomic bomb survivors and from diagnostic imaging. Although some studies have found evidence of an increased incidence of childhood cancer following prenatal abdominal X-ray exposure, thyroid cancer rates have never been shown to increase. Many of these reports have been based on mortality data [53, 54], which would not be expected to show an increase for thyroid cancer, but several have utilized incidence data as well [55–57]. Yet, these studies are confounded by a number of factors, including difficulties in dose estimation and maternal issues that may affect the risk of subsequent malignancy, such as prenatal care, maternal age, sibship position, and prior miscarriage. Follow-up by death records and tumor registries of 1630 of the 2802 individuals surviving in utero exposure from the Japanese atomic bombs disclosed only one thyroid cancer until 1984 [58].
Internal Irradiation
Introduction
Human exposure to 131I has been analyzed in patients treated for hyperthyroidism and at smaller doses (<1 mCi) for diagnostic thyroid scans. Radioactive fallout containing 131I and short-lived radioiodines has also resulted in human thyroid irradiation. Although it is believed that 131I is considerably less effective in producing thyroid abnormalities than X-radiation, one of the best controlled animal studies suggests that the carcinogenic effects are similar [59]. Shorter-lived radioisotopes of iodine are more destructive because of the greater penetration of their beta rays and faster dose rate, but their ability to produce thyroid cancer relative to X-rays is uncertain.
Populations Near Nuclear Facilities
Research from the United States and United Kingdom [60, 61] have investigated the mortality from cancer among people residing near nuclear power plants. Although such analyses are problematic owing to relocation of potentially exposed people, case ascertainment in different areas, information on individual radiation exposures, and various social issues, an increase in thyroid cancer deaths has not yet been reported. The Chernobyl accident is considered separately below.
Hanford Nuclear Site
In 1986, it was revealed that the Hanford Atomic Products Operations in Richland, Washington, had released 131I into the environment over a period of years, the greatest during 1944–1947. The Hanford Thyroid Disease Study [62] reported that the thyroid glands of 3441 people born in the vicinity of the Hanford plant between 1940 and 1946 had been thoroughly examined and thyroid dose reconstruction calculations had been performed. The final Hanford report [62], released in 2002, failed to demonstrate an increased risk of thyroid cancer from exposure to Hanford’s 131I atmospheric releases. A review of the study by the National Research Council of the National Academy of Sciences [63] concluded that the imprecision of dose estimates weakened the statistical power of the study. Therefore, although the study did not detect a dose–response relationship, the data are not strong enough to determine whether there is a small incremental risk associated with 131I exposure.
Diagnostic 131I
In a multicenter cohort [64] study of 35,074 patients, 50 thyroid cancers were observed through the Swedish Cancer Registry vs an expected number of 39.4 in the general population. This incidence was not significantly greater than expected and may have been influenced by the prevalence of underlying thyroid disease in this selected population. The mean age at first 131I examination was about 44 years, with a mean total dose of 52 μCi and absorbed dose of 0.5 Gy. The mean follow-up was 20 year, with 527,056 person-years at risk, excluding the first 5 years after examination.
Therapeutic 131I
Several studies of the effect of 131I therapy for hyperthyroidism on subsequent malignancy have been performed. The largest of these [65] from the Cooperative Thyrotoxicosis Therapy Follow-up Study evaluated 35,593 patients, including 23,020 treated with 131I. An elevated risk of thyroid cancer mortality following 131I treatment was documented [65]; however, in absolute terms, the excess number of thyroid cancer deaths was small.
In a group of 4557 patients who received 131I therapy for hyperthyroidism between 1951 and 1975 in Sweden, Holm [66] found no increased risk of thyroid cancer at doses estimated at 60–100 Gy. The mean age at treatment in this study was 56 years and an average follow-up time of only 9.5 years. An excess of thyroid cancer was found by Hoffman and associates [67] in a study of 1005 women treated with 131I at the Mayo Clinic, but this excess was not statistically significant. In the study with the longest follow-up period (mean of 15 years for 85 % of recipient patients surviving), Holm and coworkers [68] found no increased risk of thyroid cancer in 3000 subjects treated for hyperthyroidism or cardiac disease, based on Swedish Cancer Registry data. Further mortality studies [69, 70] in women receiving 131I therapy for hyperthyroidism have shown no excess thyroid cancer deaths.
At the Cleveland Clinic [71], 87 children and adolescents less than 18 years of age when they received 131I treatment for hyperthyroidism were evaluated. The mean 131I dose was 9.75 mCi. No thyroid cancers were detected in these patients or their offspring; the mean follow-up period was 12.3 years. Although 131I in therapeutic doses may affect substantial cell killing and thereby mitigate any tumorigenic impact on the thyroid, long-term follow-up of exposed populations is needed to establish the effect of 131I on subsequent thyroid cancer risk.
Fallout
Southwestern United States
People living in Nevada and Utah near the nuclear test site were exposed to radioactive fallout in the 1950s. At least 87 of the atmospheric tests between 1951 and 1958 resulted in offsite contamination [72]. Thyroid dose estimates range from 0.46 [73] to 25 Gy or more [72] with added uncertainty regarding the amount of consumption of contaminated milk. It is not known whether short-lived isotopes of iodine were involved. Thyroid examination 12–18 years later of 5179 children from the area of greatest exposure failed to disclose any increase in abnormalities [73]. However, an interview survey of a 1951 cohort of 4125 Mormons in this area disclosed an excess incidence of thyroid cancers from 1958 to 1980 [72]. This report was challenged by a subsequent mortality study of this region, which found no excess thyroid cancer deaths [74]. Owing to the lack of accurate dose information in this setting, no definite conclusions regarding the risk of fallout exposure are possible.
Continental United States
The National Cancer Institute published estimates of 131I thyroid doses in the Continental United States from fallout exposure related to the Nevada tests of the 1950s [75]. An ecologic study of thyroid cancer death rates across the continental United States suggested an association with the thyroid dose received by children under 1 year of age but failed to demonstrate increased risk from doses received at ages 1–15 years [76]. This result may relate to biases inherent in an ecologic study design, especially limitations introduced by studying a mobile population. Based on the National Cancer Institute data, a committee of the US National Academy of Sciences Institute of Medicine and National Research Council [77] estimated that an excess of 11,300 thyroid cancer cases could be attributed to exposure from the Nevada atomic bomb testing. It was further calculated that 45 % of these cases had already occurred at the time of the report (1999).
Marshall Islands
In 1954, after detonation of a 15-megaton nuclear device at Bikini, an unanticipated wind shift caused exposure to fallout of at least 300 people on at least three of the atolls of the Marshall Islands [78–80]. Late effects of this exposure have been predominantly thyroid abnormalities from absorbed radioiodines (131I, 132I, 133I, and 135I), as well as penetrating whole-body γ radiation. Significant uncertainty exists regarding thyroid doses; rough estimates average 3.12 Gy in all exposed children. Although a significant increase in nodular thyroid disease and hypothyroidism has been shown throughout the northern atolls, few cancers have been documented, and the estimated risk only 1.9 times greater than unexposed Marshallese. The risk of thyroid cancer was lower in children under 10 year old at irradiation than in older populations, suggesting that dose estimates might be too low and that significant cell killing occurred in the younger group, which is reflected by their higher incidence of hypothyroidism. No thyroid cancer has been detected in the ten individuals exposed in utero, but two developed benign nodules.
Other Incidences
Wiklund and colleagues [81] studied a cohort of 2034 reindeer-breeding Lapps who had ingested large amounts of radioactive fallout products from nuclear weapons tests in the USSR. Exposure was through the lichen–reindeer–man food chain. From 1961 to 1984, an abundance in thyroid cancer incidence was not detected through the Swedish Cancer Registry.
131I Risk in Children and Adolescents
Prior to the Chernobyl accident, data in the literature regarding 131I exposures in individuals under age 20 are sparse [82]. Exposed populations were small, and only small numbers of thyroid cancer (23 cases) have been reported. Because of these factors, and the fact that some subjects were being investigated for thyroid diseases and others were administered 131I doses in the cell-sterilization range, there is insufficient scientific information from earlier studies to make conclusions about the risk posed by 131I in children and adolescents. However, analysis of post-Chernobyl thyroid cancer data has demonstrated conclusively that 131I is a thyroid carcinogen in children and adolescents (see section on “The Chernobyl accident and thyroid cancer” below).
Analysis of Risk Assessment
Introduction
The association between radiation exposure and subsequent thyroid cancer has been conclusively demonstrated in epidemiological studies of children receiving head and neck irradiation and in survivors of the atomic bomb exposures in Japan. These studies indicate that radiation to the thyroid at high doses (>1 Gy) is highly linked with the subsequent development of cancer; the effect at lower doses is difficult to assess. Previous studies to assess doses of less than 0.10 Gy have produced no conclusive evidence of significant risk, but the requisite sample of greater than 100,000 exposed individuals and a similar control population have not been identified and analyzed.
Modifying Factors
Type and Duration of Exposure
External radiation is roughly four to five times as effective in causing thyroid cancer as is 131I for each unit of absorbed dose [83], with other isotopes of iodine probably having an effect between that of 131I and external radiation. Fractionation appears to provide an approx 30 % reduction in the tumorigenic effect on the thyroid [84]. However, X-ray technicians may have an increased risk over the general population [49, 50].
Age at Irradiation
The thyroid is more radiosensitive in children than in adolescents and similarly more so in adolescents than in adults. Tucker and colleagues [37] found that individuals treated at an early age and also after lower doses of radiation appeared to have a higher RR of thyroid cancer, suggesting some increased sensitivity to radiation. Shore [83] estimated that the geometric mean ERR of thyroid cancer following irradiation in adulthood was about 10 % of that in children. In the atomic bomb survivors, thyroid cancer in children had one of the highest ERR estimates among solid malignancies, whereas there was virtually no ERR for thyroid cancer in adults [20]. Large studies of women treated with radiation therapy for cervical cancer [39, 40] are among the few in adults that have demonstrated an excess risk for thyroid cancer, but the confidence intervals were very wide in each study.
Sex
The absolute risk in females is two to four times that of males, but the ERR/Gy is about the same in both sexes. In a study by Lundell and associates [25], most thyroid cancers occurred in females, but because of their higher background incidence rate, the sex-specific RR estimates were similar. Ron and associates [34] and Shore and coworkers [85] reported a greater excess number of cancers among females compared to males but no significant difference in the RR estimates. According to the report of the BEIR V Committee [86], females are about three times as susceptible to radiogenic and nonradiogenic thyroid cancer as males.
Race
The risk appears to be greater in individuals of Jewish ancestry. Thyroid cancer risks varied among different Jewish subgroups in the Israeli tinea study, with those born in Israel having one third the risk of those born in the Middle East or North Africa. Because the fathers of those born in Israel were themselves born in the Middle East or North Africa, environmental, rather than genetic, issues seem to be operative [86].
Iodine Deficiency
Iodine deficiency is a possible promoting factor, as decreased thyroid hormone results in increased stimulation of the thyroid epithelium by thyrotropin (TSH) . However, at least two human studies indicate the opposite effect, and thyroid cancer is associated with a high dietary iodine intake [83]. Prior to the Chernobyl experience, only a few reports exist on iodine deficiency’s influence on the risk of radiation-induced thyroid cancer [87, 88]. Analysis of post-Chernobyl data in one case–control study has demonstrated that iodine deficiency is a promoting factor in individuals exposed to 131I, although this was not confirmed in a large cohort study (see section on “The Chernobyl accident and thyroid cancer” below).
Parity
The observation that thyroid cancer among the exposed Marshall Island population occurred exclusively in multiparous women implied that parity might increase the chance of radiation-induced thyroid cancer. Shore and colleagues [33] demonstrated that older age at first childbirth significantly increased the risk of radiation-induced thyroid cancer in patients irradiated for thymic enlargement in infancy. A similar effect was found with older age at menarche. Other studies reveal that a history of miscarriage increased this risk, especially for younger women [83].
Latency Period
The interval between initial exposure to radiation and detection of thyroid cancer varies widely among human clinical studies, from 5 to 50 year after irradiation, largely reflecting the study’s follow-up interval. The latency period may also increase with the individual’s age at irradiation.
Effect of Screening
Based on an intensive screening program that started in 1974 in Chicago, Ron and colleagues [89] reported that adjusted incidence rates of secondary thyroid cancer were seven times greater during the screening period (1974–1979) than before.
Temporal Pattern
The temporal pattern of risk remains uncertain owing to the limited long-term follow-up data available. Schneider and colleagues [27] estimated that the increased risk of radiation-induced thyroid cancer probably lasts throughout life. Similarly, Thompson and colleagues [20] found no evidence for decreased risk with time after exposure. Ron and coworkers [34] reported a continued increase in risk over their entire study period of up to 38 years. Shore and collaborators [33] indicated that the risk ratio declined over time but remained highly elevated at least 45 years after irradiation. Excess risk began 5 years after exposure.
Shore and coworkers [33] found that the ERR decreased during the entire study period but that there was no significant change over time in excess absolute risk (EAR). Conversely, Ron and coworkers [34] demonstrated no significant change in ERR but a continuing increase in EAR during the entire study period (mean follow-up: 30 year). These somewhat contradictory results highlight the need for even longer follow-up periods to clarify the temporal pattern.
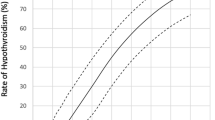
Dose–Response Relationship
A strong dose–response relationship between radiation and incidence of thyroid cancer has been documented in Japanese atomic bomb survivors [20] and in studies of children and adolescents [25, 27, 34, 85]. A pooled analysis [84] of seven major studies over a wide range of doses demonstrated an ERR of 7.7 per Gy (95 % confidence limits: 2.1–28.7). For those exposed to radiation before age 15 years, linearity best described the dose–response relationship, even at 0.10 Gy. Although risk estimates are generally those of the linear no-threshold model, at very high doses, these estimates might not be valid because of cell killing [15]. Regardless of possible threshold effects at high doses owing to cell killing, the greatest need is for an understanding of carcinogenic effects of low-dose radiation.
The Chernobyl Accident and Thyroid Cancer
Radioactivity Release
Without question, the Chernobyl accident was the worst technological disaster in the history of nuclear power generation. On April 26, 1986 at 1:23 AM, two explosions occurred (from steam and hydrogen) in reactor 4 of the Chernobyl nuclear power station, ejecting large amounts of radioactive material into the atmosphere. Subsequently, the graphite within the reactor ignited, and fuel elements in the core of the reactor melted, resulting in the release of volatile radioactive products over a 10-day period. The immediate cause of the accident was operator error, but the reactor design (which lacked a concrete containment vessel) has been implicated in the serious consequences of the accident. Initial estimates from officials in Moscow [90] indicated that approx 4 % of the total activity of the core escaped into the atmosphere, resulting in the release of some 50 million Ci (2 × 1018 Bq). However, other researchers concluded that the release was much greater [91, 92]. After 18 months of study at the reactor site, Sich [93, 94] estimated that the total release was actually in the range of 120–150 million Ci. Over 80 different isotopes were released [95]; the most abundant volatile isotopes were those of iodine (131I, 132I, 133I, and 135I), tellurium (132Te), and cesium (134Cs and 137Cs). Some radioactive isotopes released during the accident naturally decayed to isotopes of iodine, e.g., 132Te has a 3-day half-life and decays to 132I.
Geographic Distribution of Volatile Radioactive Isotopes
The distribution of volatile radioactive isotopes to different geographic regions was governed by the prevailing meteorologic conditions [96–99]. The initial plume of volatile isotopes drifted over northern Ukraine and the Gomel oblast (region) of southern Belarus (Fig. 7.1). Contaminated air masses moved west and then northwest, sweeping across the Brest and Grodno oblasts of Belarus, causing the deposition of isotopes in Sweden on April 27. The wind direction changed to the northeast and to the east on April 29, and a large cloud of radioactivity drifted over southern Belarus and the southwestern corner of the Russian Federation. A substantial deposit of radioactivity in the Gomel and Mogilev oblasts of Belarus and the Bryansk oblast of Russia resulted from rainfall during April 28–30, which washed fallout from the cloud onto the ground. Another substantial deposit about 500 km from Chernobyl was formed when the same cloud drifted over the Kaluga-Tula-Orel oblasts of Russia. Rain during April 28–30 washed fallout to the ground in these regions. Winds changed to the south and then shifted to the southwest during the last few days of the accident, contaminating the Balkans and Alps. The World Health Organization (WHO) estimated that 4.9 million people lived in areas where ground surface contamination exceeded 1 Ci/km2 [100]. About 2.3 million children lived in locations that were significantly contaminated at the time of the accident [101].
Map showing the distribution of 137Cs in Belarus, Ukraine, and Russia (From Ref. [100], courtesy of the World Health Organization)
Cesium-137 Release
Approximately 2 million Ci (8 × 1016 Bq) of 137Cs was released, causing widespread soil contamination [96, 102]. The distribution of 137Cs, which has a half-life of approx 30 years, has been carefully mapped [89] and was deposited in the following manner: Belarus, 33.5 %; Russia, 24 %; Ukraine, 20 %; Sweden, 4.4 %; and Finland, 4.3 %. The areas with the highest 137Cs contamination are shown in Fig. 7.1.
Radioiodine Release
The heaviest initial exposure to the population resulted from isotopes of iodine. According to recent studies, the release of 131I (half-life: 8.05 days) was 40–50 million Ci (approx 1.7 × 1018 Bq), representing about 50–60 % of the core inventory [102–105]. By comparison, the Three Mile Island accident released only 15–20 Ci of 131I in the United States in 1979. During the first month following the Chernobyl accident, the major source of internal radiation exposure was 131I, which was acquired by inhalation and ingestion of contaminated food. Deposits of 131I on pasture lands and gardens in the rural agricultural areas surrounding the reactor introduced this radioisotope into the food chain. Ingestion of contaminated milk was the most important source of internal 131I exposure in children [97]. Consumption of contaminated leafy vegetables was a secondary source of internal 131I exposure.
Short-lived isotopes of iodine, such as 132I (half-life: 2.3 h) and 133I (half-life: 21 h), were also released from Chernobyl-4. Very few direct measurements of radioiodines were made in the initial days following the explosion. Therefore, data regarding 132I and 133I, which were important primarily in the first days after the accident, are scarce. Measurements made on April 28, 1986, in Warsaw, Poland, revealed that 28 % of the radioactivity in the air was from short-lived iodine isotopes [106]. Thus, populations near the reactor location were exposed to 132I and 133I via inhalation for at least 1 or 2 days.
Following the accident, a limited number of measurements of the ground deposition density of 131I were conducted in Belarus by the Belarus Institute of Nuclear Physics (Minsk; [107]). A map (Fig. 7.2) of the 131I deposition in Belarus [103] shows some obvious differences in the distribution of 131I compared with the pattern of 137Cs ground contamination (Fig. 7.1). Particularly, the Gomel and Mogilev oblasts were both heavily contaminated with 137Cs, with relatively less contamination in the Brest oblast. In contrast, the 131I contamination was highest in the Gomel oblast and lower but significant levels of deposition were seen in both the Mogilev and Brest oblasts. The contamination in the Brest oblast arose from the initial plume of radioactivity that passed over this area during the first day of the accident.
Map showing the distribution of 131I ground contamination in Belarus. Annual incidence rates of thyroid cancer in children in different geographic districts are shown per 100,000 children (Based on data in Ref. [135]. From Ref. [103] with permission of the American Association for the Advancement of Science. Color illustration is printed in insert following p. 198)
Reconstruction of Thyroid Doses
Ideally, to support careful epidemiological studies, accurate thyroid dose reconstructions are needed that separate out the contribution of (1) external radiation, (2) internal radiation owing to 131I (from both inhalation and ingestion), and (3) internal radiation from the short-lived iodine isotopes (132I and 133I), because these three components may have differing potential to cause thyroid cancer. For example, 132I and 133I, which decay more rapidly than 131I, deliver their radiation dose over a shorter time interval and could theoretically have a carcinogenic effect on thyroid tissue similar to that of X-rays [108]. It has been suggested [101] that the majority of thyroid exposure (85 %) was from internally concentrated 131I derived from ingestion. Approximately 15 % was estimated to have been derived from inhalation of short-lived iodine isotopes.
Following the accident, direct measurements of thyroid radioactive iodine content were made in Belarus, Russia, and Ukraine. From these, the exposure to 131I can be extrapolated, but the measurements were made too late to provide useful information on 132I and 133I. Furthermore, the direct measurements were made on only a small proportion of the affected population. Thyroid dose reconstruction is required to determine the exposure for the rest of the population. Many factors may account for the variability in thyroid doses received by different individuals in the same geographic area. For example, many families grew their own vegetables and obtained milk from their own cows. Many individuals were outdoors most of the day at the time of the accident and slept with the windows open at night, thereby maximizing their exposure to 131I by inhalation. The thyroid dose is known to be inversely related to thyroid mass. Thus, for a given uptake of 131I, children achieve a higher thyroid dose than adults. The iodine level in the diet also influences the efficiency of uptake of 131I. Southern Belarus suffers from mild iodine deficiency, with some relatively isolated pockets of severe iodine deficiency [109, 110]. Iodine supplementation measures had lapsed by 1985. The subsequent implications are that individuals living in iodine-deficient areas would have a greater thyroid uptake of radioiodine than those living in iodine-replete areas. An effective prophylaxis program utilizing potassium iodide, as was administered in Poland [99], could have limited radioiodine exposure. As exposed inhabitants were not immediately informed of the accident, and there was no immediate effort to systematically prophylax the population, potassium iodide was not administered early enough (if at all) in Belarus, Ukraine, and Russia to be effective.
Belarus
Direct measurements of thyroid 131I content were made during May and June of 1986 in approx 300,000 individuals living in the contaminated areas of Belarus. About 200,000 records were verified and form the basis of a database for the calculation of individual thyroid doses of Belarussian residents [111–117]. Roughly 150,000 individuals in the database were interviewed regarding lifestyle and diet. Thyroid dose estimates have been completed for 130,000 residents of the Gomel and Mogilev oblasts and Minsk City who had direct thyroid measurements completed before June 6. Estimates were based on the direct measurements and information on lifestyle and diet (e.g., level of milk consumption). Calculations assumed 131I intake by inhalation and ingestion of fresh milk after a single deposition of fallout on pasture grass [111]. Average thyroid doses have also been estimated for individuals living in 800 rural settlements without direct thyroid measurements. These reconstructions are calculated using the aforementioned database, considering the level of consumption of fresh cows’ milk. A dose reconstruction study involving two cities and 2122 settlements in Belarus, as well as one city and 607 settlements in the Bryansk district of the Russian Federation, estimated an ERR of 23 per Gy [112].
Reported average thyroid doses of 131I in Belarussian children living in different contaminated raions (administrative districts) of the Gomel and Mogilev oblasts ranged from 0.15 to 4.7 Gy [111–117]. Young children (age ≤7) in these districts generally received thyroid doses that were three- to fivefold higher than those recorded in adults living in the same district. Several hundred children in Belarus received doses of 10 Gy or more to the thyroid; the highest thyroid dose did not exceed 60 Gy.
Russian Federation
In addition to the 130,000 direct measurements in Belarus, 28,000 measurements were made in the Kaluga oblast, and 2000 measurements were made in the Bryansk oblast of Russia [118–120]. These oblasts also suffered from mild-to-moderate iodine deficiency [110]. The mean thyroid dose owing to iodine radionuclides in children in Bryansk was 0.5 Gy, but it was 2.2 Gy in the more heavily contaminated zones. In the Kaluga oblast, the mean dose in children was 0.25 Gy. In the more heavily contaminated areas, the mean dose was 0.5 Gy, and individual doses were as high as 10 Gy.
Ukraine
Direct measurements of thyroid 131I content were made in 150,000 people in Ukraine in May to June of 1986, including 108,000 children and adolescents ages 0–18 years [121–125]. The measurements were conducted in four of the northern oblasts: Chernigov, Kiev, Zhitomir, and Vinnytsia. Large-scale thyroid dose reconstructions were carried out using the direct measurements in combination with environmental data and information on personal behavior and intake of milk and leafy vegetables. Empirical relations were developed between parameters of 131I intake and the level of 137Cs soil contamination and the distance and direction from the nuclear plant. These relations allowed estimation of thyroid 131I content in territories without direct measurements, such as the Cherkassy and Rovno oblasts. In different administrative regions of northern Ukraine, average thyroid doses from 131I in children and adolescents ranged from 0.03 to 1.6 Gy.
Thyroid Cancer Incidence in Children
Following the Chernobyl accident, Prisyazhiuk and colleagues [126] reported a small increase in thyroid cancer cases in children from three districts in the northern Ukraine within 80 km of the nuclear plant. Another report from Ukraine followed [127]. Local physicians had simultaneously detected a marked increase in the rate of childhood thyroid cancer in Belarus, starting in 1990 and primarily affecting the Gomel oblast [99, 128–131]. Whereas only 1 or 2 cases of thyroid cancer were seen annually in the Gomel oblast during 1986–1989, there were 14 cases in 1990 and 38 cases in 1991. Most cases from Belarus (128/131) were diagnosed as papillary carcinomas. The initial reports were met with some skepticism by the international scientific community. Therefore, a team of international scientists under the auspices of the WHO and Swiss government visited Belarus in July of 1992 to verify the accuracy of the histologic diagnoses of thyroid cancer. The international team studied the histologic specimens from 104 children diagnosed with thyroid cancer since 1989 and agreed with the diagnosis in 102 cases [132]. The team also reported a marked increase in the incidence of childhood cancer (age ≤14) in Gomel from 1990 onward, with 80 cancers per million children each year by 1992, compared with the usual background rate of around one case of cancer per million children each year.
Subsequent data [101] have shown a continued increase in thyroid cancer incidence in children from Belarus, northern Ukraine (Kiev, Chernigov, Cherkassy, Rovno, and Zhitomir oblasts), and southwestern Russia (Bryansk and Kaluga oblasts) since the accident (Table 7.3). As shown, rates are expressed as cases of pediatric (age ≤14) thyroid cancer per million children each year.
Belarus
The annual pediatric (age ≤14) thyroid cancer incidence rate in Belarus increased from 0.3 per million in 1981–1985 to 30.6 per million in 1991–1994, a 100-fold increase. A total of 333 cases of pediatric thyroid cancer were diagnosed in Belarus from 1986 to 1994 [101, 133, 134]. During 1995, 91 additional cases were diagnosed (57 in the first 7 months of the year). Yet, there were only seven pediatric cases in Belarus for 9 years preceding the accident (1977–1985). In the Gomel oblast, the incidence rate increased nearly 200-fold up to 96.4 per million.
Of the 390 pediatric cases reported in Belarus through mid-1995, 54.3 % were from the Gomel oblast, and 21.8 % were from the Brest oblast. Only 1.8 % of cases were from the Vitebsk oblast, which was not contaminated following the Chernobyl accident. Annual childhood thyroid cancer incidence rates for different geographic zones in Belarus are shown in Fig. 7.2 (in cases per 100,000 children/year for 1990–1991). There is a strong correlation between these incidence rates and soil 131I contamination levels (Fig. 7.2), as documented by the study of Abelin and colleagues [135–137]. As noted by those authors, the higher incidence rates occurred along the two paths taken by the initial clouds of volatile radioisotopes: one pathway to the west and the other to the northeast. The highest annual incidence rate (130.8/million) was found in the southern part of the Gomel oblast, adjacent to Chernobyl, where the 131I contamination level was highest. The association between childhood thyroid cancer incidence and 131I deposition suggests that radioactive isotopes of iodine had an etiological role in the pathogenesis of the thyroid cancers.
The ratio of affected girls to boys in Belarus was 1.5: 1.0. Most affected children (386/390) were born either before the accident or near the time of the accident; only four of the children were born after 1986. The rate of thyroid cancer in children born after 1986 is low and approximates baseline levels before the accident. Figure 7.3 shows data from 298 children diagnosed with thyroid cancer at the Pathology Institute in Minsk from 1990 to 1994 [138]. Note that there is a sharp cutoff age (Fig. 7.3, bold line) below which few young children have presented with thyroid cancer, and the cutoff age increases with time. The bold line in Fig. 7.3 represents children who were born on November 26, 1986. Children born on this date would have been approx 10-weeks gestational age at the time of the Chernobyl accident. Because the fetal thyroid gland can concentrate iodine by 12 weeks, these children could have theoretically sustained significant thyroid exposure to 131I in utero during the first month following the accident. These data strongly suggest that intrathyroidal accumulation of radioactive iodine isotopes—either in utero or after birth—was an important factor in the pathogenesis of the pediatric thyroid cancers in Belarus.
Graph showing the age of Belarussian children at the time of thyroid surgery vs the date of surgery. The bold line corresponds to the age of a child born on November 26, 1986. Note that very few cases fall below the bold line (From Ref. [138], courtesy of the European Commission)
An analysis of thyroid cancer cases in Belarus by cohorts, defined according to the patient’s date of birth, is shown in Fig. 7.4 [136, 139]. Clearly, increasing numbers of cases have occurred in each cohort at least until 1993. The largest number of new thyroid cancer cases has occurred in individuals who were age 4 and younger at the time of the accident (birth date: 1982–1986), followed by those who were ages 5–9 (birth date: 1977–1981); however, individuals as old as 19 at the time of the accident were still at risk. These data suggest that younger children are most susceptible to the carcinogenic effects of radioactive iodine isotopes.
Graph showing the number of new thyroid cancer cases during each year from 1986 to 1994 in cohorts of Belarussian children defined by year of birth (From Ref. [139], courtesy of the European Commission)
The peak incidence of childhood papillary thyroid carcinoma (in patients up to age 14) occurred in Belarus in 1995 at 40 cases per million. Subsequently, a gradually decreasing frequency of papillary carcinoma has been observed in this age group. There were 84 cases observed in 1996, 66 cases in 1997, 54 cases in 1998, 49 cases in 1999, and 31 cases in 2000 [140]. This represents a total of 708 childhood cases presenting in Belarus from 1986 to 2000. After the latter half of 2001, only sporadic thyroid cancers were found in Belarussian children. The decrease is readily explained because over time, exposed individuals will reach age 15 or older and will no longer be reported in the data for children (up to age 14). In keeping with this analysis, since 1997, the incidence of thyroid cancer has increased in Belarussian adolescents ages 15–18 years old at the time of diagnosis or surgery. In 2001, the incidence was 112 per million in this patient cohort [141].
Russian Federation
In the contaminated oblasts of the Russian Federation, an increased incidence of thyroid cancer in children and adolescents has been registered [101, 119, 142, 143]. The annual prevalence in children (age ≤14) in the Bryansk and Kaluga oblasts has increased from background to ten per million. The major increase occurred in the Bryansk oblast, with 21 cases reported between 1986 and 1994.
Ukraine
Between 1986 and 1994, 211 children (age ≤14) underwent surgery for thyroid cancer in Ukraine [101, 121, 122, 144, 145]. The incidence in children increased from 0.4 to 0.6 per million pre-Chernobyl to 4 per million by 1992–1994. The ratio of girls to boys was 1.4: 1.0. In the five most northern oblasts (Kiev, Chernigov, Zhitomir, Cherkassy, and Rovno) that were heavily contaminated by the Chernobyl accident, the incidence was much higher: 11.5 per million children. About 60 % of the cases in Ukraine originated from these 5 oblasts out of 25 oblasts in the country. Only two children presenting with thyroid cancer were born after 1986, equivalent to an incidence of less than one per million each year in children born after 1986. In Pripyat, located 3.5 km from the Chernobyl plant, the incidence in children and adolescents who were ages 0–18 years old at the time of the accident was 137 per million by 1990–1992. Throughout Ukraine, there was a 30-fold gradient in thyroid cancer incidence rates in individuals ages 0–18 at the time of the accident, directly corresponding to the gradient in thyroid doses from 131I exposure [122]. This relationship between cancer incidence and thyroid 131I dose strongly supports a role for radioactive iodine isotopes in the pathogenesis of the cancers.
Pathological and Biologic Features of the Pediatric Thyroid Cancers
The pathological features of the thyroid cancers presenting after the Chernobyl accident in children from Belarus, Ukraine, and Russia have been well characterized [146–155]. With few exceptions, all the cases have been papillary carcinomas. Several histological subtypes have been noted [146–149]: classical papillary architecture, often with mixed papillary/follicular elements (approx 11 %); a mixture of solid and follicular structures (73 %); and the diffuse sclerosing type (8 %). Primary tumors were 1 cm or larger in diameter in the vast majority of cases (79–88.5 % in three series; [133, 150, 151]).
Thyroid tumors that arise in children are typically more aggressive than those that arise in adults [156–161]. This phenomenon was also true in the Chernobyl-related cases. The tumors were often widely invasive within the thyroid gland (33 % in one series [151]; 59 % of cases in another series [146]). There was direct invasion of extrathyroidal tissue (T4 stage) in a high proportion of cases (48–63 %; [133, 134, 144, 146, 150, 154]). Lymphatic invasion was present in 77 % of cases and blood vessel invasion in 15–32 % [146, 150, 151]. Regional lymph node metastases (N1 stage) were present in 59–88 % of cases [133, 144, 150, 151, 154]. Distant metastases (M1 stage, usually to lung) were present in 5–9 % of cases [133, 150, 154].
Only a few cases showed features of “occult” or microcarcinoma. Taken together, these pathological and biological features argue strongly against the cancers being incidental findings [162–164]. In nearly all cases, the cancers represented clinically significant disease; only 9 % of the children in one series from Belarus were staged at T1 N0 M0 [150].
Molecular Characterization of Chernobyl-Associated Papillary Thyroid Carcinomas
Ret Oncogene
Activation of the ret oncogene by chromosomal rearrangement was initially reported in four of seven Chernobyl-associated pediatric cases by Ito and coworkers [165] and is the most characteristic type of molecular alteration in post-Chernobyl papillary thyroid carcinomas [165–186]. An analysis of pooled data regarding ret rearrangements from eight published studies [166–168, 177–182] is presented in Table 7.4. For purposes of this analysis, those cases diagnosed or undergoing surgery on or before April 26, 1996, are reported in part A; those presenting after April 26, 1996, are reported in part B. The original published case series have been segregated into two groups according to this criterion. For example, the first 37 cases of Smida et al. [182] underwent surgery from April 21, 1993, to April 16, 1996, and are recorded in part A. The remaining 14 from this series underwent surgery from May 3, 1996, to February 14, 1997, and are recorded in part B. The 191 cases of Rabes et al. [177, 178] were divided into groups of 61 and 130 by the original authors using the same criterion. Case numbers 3, 4, 5, and 6 as published by Pisarchik et al. [179, 180] underwent surgery in February 1996 and are included in part A. Cases numbered 7–39 underwent surgery from October 2, 1996, to December 27, 1996, and are reported in part B. All individuals reported in this analysis were under age 20 at the moment of the accident (April 26, 1986).
As demonstrated in Table 7.4, part A, ret/PTC3 is the most prevalent form of ret rearrangement in post-Chernobyl papillary carcinomas diagnosed during the first decade following the accident (until April 26, 1996). The overall prevalence of ret/PTC3 in these cases is 43 %, whereas the prevalence of ret/PTC1 is 16 % and that of ret/PTC2 is only 1.3 %.
In contrast with the earlier case series, Pisarchik and colleagues [179] found a higher prevalence of ret/PTC1 rearrangements (29 %) in 31 post-Chernobyl papillary thyroid carcinomas presenting in 1996. However, the prevalence of ret/PTC3 was found to be quite low (7 %) in a subset of these cases [180]. Pisarchik and colleagues [180] suggested that there was a switch in the ratio of ret/PTC3 to ret/PTC1 rearrangements in late (1996) vs early (1991–1992) post-Chernobyl papillary thyroid cancers. Smida and colleagues [182] independently arrived at a similar conclusion after studying 51 Chernobyl-related cases. These authors [182] suggested that ret/PTC3 may be typical for radiation-associated childhood papillary thyroid carcinomas with a short latency period, whereas ret/PTC1 may be a marker for carcinomas appearing after a longer latency period. These observations are confirmed by the pooled analysis in Table 7.4, part B. The overall prevalence of ret/PTC3 in these later cases is significantly lower at 11 %, whereas the prevalence of ret/PTC1 is higher at 28 %.
In addition to influencing the latency period, the type of ret rearrangement correlates strongly with morphological variants of papillary thyroid carcinoma. Nikiforov and colleagues [167] first reported that post-Chernobyl papillary thyroid carcinomas with a solid differentiation pattern are associated with ret/PTC3, and the classic papillary differentiation pattern is related to the ret/PTC1 rearrangement. This finding has been confirmed by Rabes and colleagues [177, 178], as well as Thomas and colleagues [183–185], and similar results have been obtained in transgenic mice [187–189].
The results regarding ret rearrangements are particularly interesting in view of the recent demonstration that X-irradiation (50–100 Gy) in vitro can induce ret oncogene rearrangements in undifferentiated human thyroid carcinoma cells [190]. Furthermore, Bounacer and colleagues [191] reported a high frequency of ret rearrangements (primarily ret/PTC1) in papillary thyroid carcinomas originating from patients with a history of external radiation. Similar results using immunohistochemistry were reported by Collins and colleagues [192]. Taken together, they suggest that ret rearrangements are important in the pathogenesis of radiation-induced papillary thyroid carcinomas, and the specific type of molecular rearrangement (ret/PTC1 vs ret/PTC3) may influence the biology of the cancer (e.g., the latency period and morphological variant).
Following the Chernobyl accident, rare types of ret/PTC rearrangements were also described (Fig. 7.5). These include a variant of ret/PTC1 [193], ret/PTC4 [172], and other variants of ret/PTC3 [170, 171], ret/PTC5 [173], ret/PTC6 [174], ret/PTC7 [174], ret/PTC8 [175], and ret/PTC9 [176]. Three other rearrangements—ret/PCM1 [194], ELKS/RET [195], and ret/PTC1L (another variant of ret/PTC1) [196]—were recently described.
Other Genetic Loci
Other genetic loci have been investigated [138, 146, 197–205] including NTRK1, TP53, the TSH receptor, the three ras genes (H-RAS, K-RAS, and N-RAS), and BRAF. Chromosomal rearrangements associated with the NTRK1 gene [197] have been identified infrequently in post-Chernobyl papillary thyroid carcinomas [177, 178, 198]. Missense, silent, and nonsense mutations involving the TP53 gene have been identified in a small number of Chernobyl-associated papillary thyroid carcinomas [199–204]. Alterations of the TSH receptor and RAS genes are very rare, suggesting that point mutations in these genes do not have a significant role in the pathogenesis of Chernobyl-associated thyroid cancers. A novel AKAP9-BRAF fusion resulting from an internal rearrangement of chromosome 7 has been described in a subset of post-Chernobyl papillary thyroid carcinomas [205]. In contrast, activating point mutations of BRAF are absent [205].
Summary Molecular Model
The available molecular data, taken together, suggest that the mechanism of Chernobyl radiation-induced papillary thyroid cancer pathogenesis is primarily related to double-stranded DNA breaks leading to chromosomal translocations and/or inversions and gene rearrangements (e.g., involving ret, NTRK1, and BRAF genes). The resulting hybrid gene products are expressed within thyroid follicular cells and exhibit ligand-independent activation. These hybrid proteins then constitutively activate the MAPK pathway. This is in contrast to sporadic papillary thyroid cancers where activating point mutations within elements of the MAPK pathway are more common.
Epidemiological Considerations
Following the initial reports of thyroid cancer cases in the regions surrounding Chernobyl, there were many questions about whether the cases were related to the accident or simply represented increased ascertainment [89, 206, 207]. The data reviewed in this chapter support the contention that nearly all the cancer cases were correctly diagnosed, and the majority represented clinically important disease, not incidental cases found by screening. Some oblasts that received little radiation (Vitebsk) were subjected to intensive screening but yielded very few cases. Thus, increased ascertainment cannot explain the dramatic and sustained increase in incidence that has been documented. The large number of cases and latency period support an association with the accident [108]. In addition, data reviewed previously suggest that radioiodine isotopes are implicated in the pathogenesis of the cancers. A small case–control epidemiological study has provided some further evidence for this point by demonstrating a dose–response relationship at the level of the individual thyroid dose [208, 209]. A study by Jacob et al. [210] showed a linear dose–response relationship between the thyroid dose, resulting from internal 131I exposure and the risk of thyroid cancer. A recent analysis by Shibata et al. [211] further supports the concept that direct external or internal exposure to 131I and short-lived radioiodine isotopes was a causative factor in the pediatric thyroid cancers. An analysis of children who lived within a 150-km radius from Chernobyl revealed that cancer frequently developed in children born in 1983–1986; however, no cases were seen in children born in 1987–1989 [211]. This is most likely explained by natural degradation of 131I and short-lived radioiodine isotopes, as well as erosion of these isotopes from the contaminated territory by wind and rain. A large case–control study has definitively established a relationship between childhood radioiodine dose following the Chernobyl accident and the subsequent risk of thyroid cancer [212]. Risk is modified by iodine status; children living in iodine-deficient areas have greater risk of developing thyroid cancer following 131I exposure [212]. Another case–control study by Davis and colleagues [213] demonstrated a dose-dependent relationship of thyroid cancer risk in the Bryansk oblast of the Russian Federation. Finally, a large-scale prospective cohort study involving 32,385 individuals under age 18 living in contaminated areas of Ukraine demonstrated an ERR of 5.25 per Gy during the first screening in 1998–2000 [214]. A linear dose–response relationship between individual 131I dose and thyroid cancer risk persisted in this cohort for two decades following the Chernobyl accident, although at a somewhat lower ERR of 1.91 per Gy [215] based on screenings in 2001 through 2007. A major strength of this study was availability of individual 131I dose estimates derived from radioactivity measurements taken within 2 months after the accident [214, 215]. This cohort study did not confirm a modifying effect of iodine status on 131I- related risk of thyroid cancer [215].
References
Hanson GA, Komorowski RA, Cerletty JM, Wilson SD. Thyroid gland morphology in young adults: normal subjects versus those with prior low-dose neck irradiation in childhood. Surgery. 1983;94:984–8.
Spitalnik PF, Straus FH. Patterns of human thyroid parenchymal reaction following low-dose childhood irradiation. Cancer. 1978;41:1098–105.
Freedberg AS, Kurland GS, Blumgart HL. The pathologic effects of I-131 on the normal thyroid gland of man. J Clin Endocrinol. 1952;12:1315–48.
Carr RF, LiVolsi VA. Morphologic changes in the thyroid after irradiation for Hodgkin’s and non-Hodgkin’s lymphoma. Cancer. 1989;64:825–9.
Quimby EH, Werner SC. Late radiation effects in roentgen therapy for hyperthyroidism. JAMA. 1949;140:1046–7.
Winship T, Rosvoll RV. Thyroid carcinoma in childhood: final report on a 20 year study. Clin Proc Child Hosp Washington DC. 1970;26:327–49.
Roudebush CP, Asteris GT, DeGroot LJ. Natural history of radiation-associated thyroid cancer. Arch Intern Med. 1978;138:1631–4.
Samaan NA, Schultz PN, Ordonez NG, Hickey RC, Johnston DA. A comparison of thyroid carcinoma in those who have and have not had head and neck irradiation in childhood. J Clin Endocrinol Metab. 1987;64:219–23.
Mehta MP, Goetowski PG, Kinsella TJ. Radiation induced thyroid neoplasms 1920 to 1987: a vanishing problem? Int J Radial Oncol Biol Phys. 1989;16:1471–5.
Akslen LA, Haldorsen T, Thoresen SO, Glattre E. Incidence pattern of thyroid cancer in Norway: influence of birth cohort and time period. Int J Cancer. 1993;53:183–7.
Harach HR, Franssila KO, Wasenius V-M. Occult papillary carcinoma of the thyroid: a “normal” finding in Finland—a systematic autopsy study. Cancer. 1985;56:531–8.
Sampson RJ, Woolner LB, Bahn RC, Kurland LT. Occult thyroid carcinoma in Olmsted County, Minnesota: prevalence at autopsy compared with that in Hiroshima and Nagasaki, Japan. Cancer. 1974;34:2072–6.
Wilson SD, Komorowski R, Cerletty J, Majewski JT, Hooper M. Radiation-associated thyroid tumors: extent of operation and pathology technique influence the apparent incidence of carcinoma. Surgery. 1983;94:663–7.
Robbins J. Thyroid cancer: a lethal endocrine neoplasm—NIH conference. Ann Intern Med. 1991;115:133–47.
Mettler FA, Upton AC. Carcinogenesis at specific sites. In: Medical effects of ionizing radiation. Philadelphia: WB Saunders; 1995. p. 130–9.
Aldinger KA, Samaan NA, Ibanez M, Hill CS. Anaplastic carcinoma of the thyroid: a review of 84 cases of spindle and giant cell carcinoma of the thyroid. Cancer. 1978;41:2267–75.
Duffy BJ, Fitzgerald PJ. Cancer of the thyroid in children: a report of 28 cases. J Clin Endocrinol Metab. 1950;10:1296–308.
Simpson CL, Hempelmann LH. The association of tumors and roentgen-ray treatment of the thorax in infancy. Cancer. 1957;10:42–56.
Saenger EL, Silverman FN, Sterling TD, Turner ME. Neoplasia following therapeutic irradiation for benign conditions in childhood. Radiology. 1960;74:889–904.
Thompson DE, Mabuchi K, Ron E, Soda M, Tokunaga M, Ochikubo S, et al. Cancer incidence in atomic bomb survivors. Part II: solid tumors, 1958–1987. Radiat Res. 1994;137:817–67.
Parker LN, Belsky JL, Yamamoto T, Kawamoto S, Keehn RJ. Thyroid carcinoma after exposure to atomic radiation: a continuing survey of a fixed population, Hiroshima and Nagasaki, 1958–1971. Ann Intern Med. 1974;80:600–4.
Schull WJ. Atomic bomb survivors: patterns of cancer risk. Prog Cancer Res Ther. 1984;26:21–36.
Fjalling M, Tisell L-E, Carlsson S, Hansson G, Lundberg L-M, Oden A. Benign and malignant thyroid nodules after neck irradiation. Cancer. 1986;58:1219–24.
Furst CJ, Lundell M, Holm LE, Silfversward C. Cancer incidence after radiotherapy for skin hemangioma: a retrospective cohort study in Sweden. J Natl Cancer Inst. 1988;80:1387–92.
Lundell M, Hakulinen T, Holm L-E. Thyroid cancer after radiotherapy for skin hemangioma in infancy. Radiat Res. 1994;140:334–9.
Lindberg S, Karlsson P, Arvidsson B, Holmberg E, Lundberg LM, Wallgren A. Cancer incidence after radiotherapy for skin haemangioma during infancy. Acta Oncol. 1995;34:735–40.
Schneider AB, Ron E, Lubin J, Slovall M, Gierlowski TC. Dose-response relationships for radiation-induced thyroid cancer and nodules: evidence for the prolonged effects of radiation on the thyroid. J Clin Endocrinol Metab. 1993;77:362–9.
Schneider AB, Recant W, Pinsky SM, Ryo UY, Bekerman C, Shore-Freedman E. Radiation-induced thyroid carcinoma: clinical course and results of therapy in 296 patients. Ann Intern Med. 1986;105:405–12.
Viswanathan K, Gierlowski TC, Schneider AB. Childhood thyroid cancer: characteristics and long-term outcome in children irradiated for benign conditions of the head and neck. Arch Pediatr Adolesc Med. 1994;148:260–5.
Schneider AB, Shore-Freedman E, Weinstein RA. Radiation-induced thyroid and other head and neck tumors: occurrence of multiple tumors and analysis of risk factors. J Clin Endocrinol Metab. 1986;63:107–12.
Paloyan E, Lawrence AM. Thyroid neoplasms after radiation therapy for adolescent acne vulgaris. Arch Dermatol. 1978;114:53–5.
Hempelmann LH, Hall WJ, Phillips M, Cooper RA, Ames WR. Neoplasms in persons treated with x-rays in infancy: fourth survey in 20 years. J Natl Cancer Inst. 1975;55:519–30.
Shore RE, Hildreth N, Dvoretsky P, Andresen E, Moseson M, Pasternack B. Thyroid cancer among persons given x-ray treatment in infancy for an enlarged thymus gland. Am J Epidemiol. 1993;137:1068–80.
Ron E, Modan B, Preston D, Alfandary E, Stovall M, Boice JD. Thyroid neoplasia following low-dose radiation in childhood. Radiat Res. 1989;120:516–31.
Shore RE, Albert RE, Pasternack BS. Follow-up study of patients treated by x-ray epilation for tinea capitis: resurvey of post-treatment illness and mortality experience. Arch Environ Health. 1976;31:17–24.
Ron E, Modan B. Thyroid and other neoplasms following childhood scalp irradiation. Prog Cancer Res Ther. 1984;26:139–51.
Tucker MA, Morris Jones PH, Boice JD, Robison LL, Stone BJ, Stovall M, et al. Therapeutic radiation at a young age is linked to secondary thyroid cancer. Cancer Res. 1991;51:2885–8.
Hancock SL, Cox RS, McDougall IR. Thyroid diseases after treatment of Hodgkin’s disease. N Engl J Med. 1991;325:599–605.
Boice JD, Day NE, Andersen A, Brinton LA, Brown R, Choi NW, et al. Second cancers following radiation treatment for cervical cancer: an international collaboration among cancer registries. J Natl Cancer Inst. 1985;74:955–75.
Boice JD, Engholm G, Klienerman RA, Blettner M, Stovall M, Lisco H, et al. Radiation dose and second cancer risk in patients treated for cancer of the cervix. Radiat Res. 1988;116:3–55.
Arai T, Nakano T, Fukuhisa K, Kasamatsu T, Tsunematsu R, Masubuchi K, et al. Second cancer after radiation therapy for cancer of the uterine cervix. Cancer. 1991;67:398–405.
Hay JH, Duncan W, Kerr GR. Subsequent malignancies in patients irradiated for testicular tumours. Br J Radiol. 1984;57:597–602.
Fossa SD, Langmark F, Aass N, Andersen A, Lothe R, Borrasen AL. Second non-germ cell malignancies after radiotherapy of testicular cancer with or without chemotherapy. Br J Cancer. 1990;61:639–43.
Kendall GM, Muirhead CR, MacGibbon BH, O’Hagan JA, Conquest AJ, Goodill AA, et al. Mortality and occupational exposure to radiation: first analysis of the National Registry for Radiation Workers. BMJ. 1992;304:220–5.
Beral V, Inskip H, Fraser P, Booth M, Coleman D, Rose G. Mortality of employees of the United Kingdom Atomic Energy Authority, 19461979. BMJ. 1985;291:440–7.
Wilkinson GS, Tietjen GL, Wiggs LD, Galke WA, Acquavella JF, Reyes M, et al. Mortality among plutonium and other radiation workers at a plutonium weapons facility. Am J Epidemiol. 1987;125:231–50.
Checkoway H, Pearce N, Crawford-Brown DJ, Cragle DL. Radiation doses and cause-specific mortality among workers at a nuclear materials fabrication plant. Am J Epidemiol. 1988;127:255–66.
Wing S, Shy CM, Wood JL, Wolf S, Cragle DL, Frame EL. Mortality among workers at Oak Ridge Nationaal Laboratory: evidence of radiation effects in follow-up through 1984. JAMA. 1991;265:1397–402.
Wang J-X, Boice JD, Li B-X, Zhang J-Y, Fraumeni JF. Cancer among medical diagnostic x-ray workers in China. J Natl Cancer Inst. 1988;80:344–50.
Boice JD, Mandel JS, Doody MM, Yoder RC, McGowan R. A health survey of radiologic technologists. Cancer. 1992;69:586–98.
Smith PG, Doll R. Mortality from cancer and all causes among British radiologists. Br J Radiol. 1981;54:187–94.
Mátanosla GM, Seltser R, Sartwell PE, Diamond EL, Elliott EA. The current mortality rates of radiologists and other physician specialists: specific causes of death. Am J Epidemiol. 1975;101:199–210.
Stewart A, Kneale GW. Radiation dose effects in relation to obstetric x-rays and childhood cancers. Lancet. 1970;1:1185–8.
Mole RH. Childhood cancer after prenatal exposure to diagnostic x-ray examinations in Britain. Br J Cancer. 1990;62:152–68.
Oppenheim BE, Griem ML, Meier P. Effects of low-dose prenatal irradiation in humans: analysis of Chicago Lying-in data and comparison with other studies. Radiat Res. 1974;57:508–44.
Harvey EB, Boice JD, Honeyman M, Flannery JT. Prenatal x-ray exposure and childhood cancer in twins. N Engl J Med. 1985;312:541–5.
Rodvall Y, Pershagen G, Hrubec Z, Ahlbom A, Pedersen NL, Boice JD. Prenatal x-ray exposure and childhood cancer in Swedish twins. Int J Cancer. 1990;46:362–5.
Yoshimoto Y, Kato H, Schull WJ. Risk of cancer among children exposed in útero to A-bomb radiations, 1950–1984. Lancet. 1988;2:665–9.
Lee W, Chiacchierini RP, Shleien B, Telles NC. Thyroid tumors following I-131 or localized X irradiation to the thyroid and pituitary glands in rats. Radiat Res. 1982;92:307–19.
Forman D, Cook-Mozaffari P, Darby S, Davey G, Sratton I, Doll R, Pike M. Cancer near nuclear installations. Nature. 1987;329:499–505.
Jablon S, Urubec Z, Boice JD. Cancer in populations living near nuclear facilities: a survey of mortality nationwide and incidence in two states. JAMA. 1991;265:1403–8.
Davis S, Kopecky KJ, Hamilton T. Hanford thyroid disease final report. Seattle: Fred Hutchinson Cancer Research Center; 2002.
Committee on an Assessment of Centers for Disease Control and Prevention Radiation Studies from DOE Contractor Sites: Subcommittee to Review the Hanford Thyroid Disease Study Final Results and Report, National Academy of Sciences. Review of the Hanford thyroid disease study draft final report. Washington, DC: National Academies Press; 2000.
Holm L-E, Wiklund KE, Lundell GE, Bergman NA, Bjelkengren G, Cederquist ES, et al. Thyroid cancer after diagnostic doses of iodine 131: a retrospective cohort study. J Natl Cancer Inst. 1988;80:1132–8.
Ron E, Doody MM, Becker DV, Brill AB, Curtis RE, Goldman MB, et al. Cancer mortality following treatment for adult hyperthyroidism. JAMA. 1998;280:347–55.
Holm L-E. Malignant disease following iodine-131 therapy in Sweden. Prog Cancer Res Ther. 1984;26:263–71.
Hoffman DA, McConahey WM, Fraumeni JF, Kurland LT. Cancer incidence following treatment of hyperthyroidism. Int J Epidemiol. 1982;11:218–24.
Holm L-E, Dahlqvist I, Israelsson A, Lundell G. Malignant thyroid tumors after iodine-131 therapy: a retrospective cohort study. N Engl J Med. 1980;303:188–91.
Hoffman DA, McConahey WM, Diamond EL, Kurland LT. Mortality in women treated for hyperthyroidism. Am J Epidemiol. 1982;115:243–54.
Goldman MB, Maloof F, Monson RR, Aschengrau A, Cooper DS, Ridgway EC. Radioactive iodine therapy and breast cancer: a follow-up study of hyperthyroid women. Am J Epidemiol. 1988;127:969–80.
Safa AM, Schumacher OP, Rodriguez-Antunez A. Long-term follow-up results in children and adolescents treated with radioactive iodine (I-131) for hyperthyroidism. N Engl J Med. 1975;292:167–71.
Johnson CJ. Cancer incidence in an area of radioactive fallout downwind from the Nevada test site. JAMA. 1984;251:230–6.
Rallison ML, Dobyns BM, Keating PR, Rail JE, Tyler FH. Thyroid disease in children: a survey of subjects potentially exposed to fallout radiation. Am J Med. 1974;56:457–63.
Machado SG, Land CE, McKay FW. Cancer mortality and radioactive fallout in southwestern Utah. Am J Epidemiol. 1987;125:44–61.
National Cancer Institute. Estimated exposures and thyroid doses received by the American People from Iodine-131 in fallout following Nevada atmospheric nuclear bomb tests: a report from the National Cancer Institute. Washington, DC: U.S. Department of Health and Human Services; 1997.
Gilbert ES, Tarone R, Bouville A, Ron E. Thyroid cancer rates and 131-I doses from Nevada atmospheric nuclear bomb tests. J Natl Cancer Inst. 1998;90:1654–60.
Committee on Thyroid Screening Related to I-131 Exposure, Institute of Medicine, and Committee on Exposure of the American People to I-131 from the Nevada Atomic Bomb Tests, National Research Council. Exposure of the American people to Iodine-131 from Nevada nuclear-bomb tests: review of the National Cancer Institute Report and Public Health Implications. Washington, DC: National Academies Press; 1999.
Conard RA, Paglia DE, Larsen PR, Sutow WW, Dobyns BM, Robbins J, et al. Review of medical findings in a Marshallese population twenty-six years after accidental exposure to radioactive fallout. Brookhaven National Laboratory Report 1980; BNL 51261.
Conard RA. Late radiation effects in Marshall Islanders exposed to fallout 28 years ago. Prog Cancer Res Ther. 1984;26:57–71.
Hamilton TE, van Belle G, LoGerfo JP. Thyroid neoplasia in Marshall Islanders exposed to nuclear fallout. JAMA. 1987;258:629–36.
Wiklund K, Holm L-E, Eklund G. Cancer risks in Swedish Lapps who breed reindeer. Am J Epidemiol. 1990;132:1078–82.
Shore RE. Human thyroid cancer induction by ionizing radiation: summary of studies based on external irradiation and radioactive iodines. In: Karaoglou A, Desmet G, Kelly GN, Menzel HG, editors. The radiological consequences of the Chernobyl Accident. Brussels: European Commission; 1996. p. 669–75.
Shore RE. Issues and epidemiological evidence regarding radiation-induced thyroid cancer. Radiat Res. 1992;131:98–111.
Ron E, Lubin JH, Shore RE, Mabuchi K, Modan B, Pottern LM, et al. Thyroid cancer after exposure to external radiation: a pooled analysis of seven studies. Radiat Res. 1995;141:259–77.
Shore RE, Woodard E, Hildreth N, Dvoretsky P, Hempelmann L, Pasternack B. Thyroid tumors following thymus irradiation. J Natl Cancer Inst. 1985;74:1177–84.
National Academy of Sciences. Committee on the biological effects of ionizing radiations: health effects of exposure to low level of ionizing radiation (BEIR V). Washington, DC: National Academy Press; 1990.
Shakhtarin VV, Tsyb AF, Stepanenko VF, Orlov MY, Kopecky KJ, Davis S. Iodine deficiency, radiation dose, and the risk of thyroid cancer among children and adolescents in the Bryansk region of Russia following the Chernobyl power station accident. Int J Epidemiol. 2003;32:584–91.
Niedziela M, Korman E, Breborowicz D, et al. A prospective study of thyroid nodular disease in children and adolescents in western Poland from 1996 to 2000 and the incidence of thyroid carcinoma relative to iodine deficiency and the Chernobyl disaster. Pediatr Blood Cancer. 2004;42:84–92.
Ron E, Lubin J, Schneider AB. Thyroid cancer incidence. Nature. 1992;360:113.
USSR State Committee on the Utilization of Atomic Energy. The accident at the Chernobyl nuclear power plant and its consequences. Information compiled for the International Atomic Energy Agency Experts Meeting, August 25–29, 1986, Vienna. Moscow: USSR State Committee on the Utilization of Atomic Energy; 1986.
Travis J. Chernobyl explosion. Inside look confirms more radiation. Science. 1994;263:750.
Warman EA. Paper presented at the New York Chapter Health Physics Society symposium on the effects of the nuclear reactor accident at Chernobyl. Upton: Brookhaven National Laboratory; 1987.
Sich AR. Chernobyl thesis. Science. 1994;266:1627–8.
Stone R. The explosions that shook the world. Science. 1996;272:352–4.
Sobotovich E, Bondarenko G, Petriaev E. Geochemistry of Chernobyl radionuclides. In: Karaoglou A, Desmet G, Kelly GN, Menzel HG, editors. The radiological consequences of the Chernobyl accident. Brussels: European Commission; 1996. p. 477–83.
Izrael YA, De Cort M, Jones AR, et al. The atlas of caesium-137 contamination of Europe after the Chernobyl accident. In: Karaoglou A, Desmet G, Kelly GN, Menzel HG, editors. The radiological consequences of the Chernobyl accident. Brussels: European Commission; 1996. p. 1–10.
Balonov M, Jacob P, Likhtarev I, Minenko V. Pathways, levels and trends of population exposure after the Chernobyl accident. In: Karaoglou A, Desmet G, Kelly GN, Menzel HG, editors. The radiological consequences of the Chernobyl accident. Brussels: European Commission; 1996. p. 235–49.
Tsaturov YS, De Cort M, Dubois G, Izrael YA, Stukin ED, Fridman SD, et al. The need for standardization in the analysis, sampling and measurement of deposited radionuclides. In: Karaoglou A, Desmet G, Kelly GN, Menzel HG, editors. The radiological consequences of the Chernobyl accident. Brussels: European Commission; 1996. p. 425–33.
Kazakov VS, Demidchik EP, Astakhova LN. Thyroid cancer after Chernobyl. Nature. 1992;359:21.
World Health Organization. International programme on the health effects of the Chernobyl accident. Geneva: World Health Organization; 1993.
Stsjazhko VA, Tsyb AF, Tronko ND, Souchkevitch G, Baverstock KF. Childhood thyroid cancer since accident at Chernobyl. BMJ. 1995;310:801.
Williams N, Balter M. Chernobyl research becomes international growth industry. Science. 1996;272:355–6.
Balter M. Children become the first victims of fallout. Science. 1996;272:357–60.
Goldman M, Catlin R, Anspaugh L. Health and environmental consequences of the Chernobyl nuclear power plant accident. Washington, DC: U.S. Department of Energy Report DOE/ER 0332; 1987.
Lange R, Dickerson MH, Gudiksen PH. Dose estimates from the Chernobyl accident. Nucl Technol. 1988;82:311–23.
Nauman J, Wolff J. Iodine prophylaxis in Poland after the Chernobyl reactor accident: benefits and risks. Am J Med. 1993;94:524–32.
Dubina YV, Schekin YK, Guskina LN. Systematisation and verification of the spectrometrical analysis data of soil, grass, milk and milk products samples with results of 131-iodine measurements. Minsk Belarus Institute of Nuclear Physics; 1990, In Russian.
Becker DV, Robbins J, Beebe GW, Bouville AC, Wachholz BW. Childhood thyroid cancer following the Chernobyl accident. Endocrinol Metab Clin North Am. 1996;25:197–211.
Mityukova T, Astakhova L, Asenchyk L, Orlov M, Van Middlesworth L. Urinary iodine excretion in Belarus children. Eur J Endocrinol. 1995;133:216–7.
Gerasimov G, Alexandrova G, Arbuzova M, Butrova S, Kenzhibaeva M, Kotova G, et al. Iodine deficiency disorders (IDD) in regions of Russia affected by Chernobyl. In: Karaoglou A, Desmet G, Kelly GN, Menzel HG, editors. The radiological consequences of the Chernobyl accident. Brussels: European Commission; 1996. p. 813–5.
Gavrilin Y, Khrouch V, Shinkarev S, Drozdovitch V, Minenko V, Shemyakina E, et al. Estimation of thyroid doses received by the population of Belarus as a result of the Chernobyl accident. In: Karaoglou A, Desmet G, Kelly GN, Menzel HG, editors. The radiological consequences of the Chernobyl accident. Brussels: European Commission; 1996. p. 1011–20.
Jacob P, Kenigsberg Y, Zvonova I, Goulko G, Buglova E, Heidenreich WF, et al. Childhood exposure due to the Chernobyl accident and thyroid cancer risk in contaminated areas of Belarus and Russia. Br J Cancer. 1999;80:1461–9.
Gavrilin YI, Gordeev KI, Ivanov VK, Ilyin LA, Kondrusev AI, Margulis UY, et al. The process and results of the reconstruction of internal thyroid doses for the population of contaminated areas of the Republic of Belarus. Vestn Acad Med Sci. 1992;2:35–43. In Russian.
Ilyin LA, Balonov MI, Buldakov LA, et al. Radiocontamination patterns and possible health consequences of the accident at the Chernobyl nuclear power station. J Radiol Prot. 1990;10:13–29.
Gavrilin YI, Gordeev KI, Ilyin LA, et al. Results of thyroid dose assessment for contaminated territories of Belarussia. Bull Acad Med Sci USSR. 1991;8:35. In Russian.
Gavrilin YI, Khrouch VT, Shinkarev SM. Internal thyroid exposure of the residents in several contaminated areas of Belarus. J Med Radiol. 1993;6:15–20. In Russian.
Khrouch VT, Gavrilin YI, Shinkarev SM, et al. Generalization of results of individual thyroid dose reconstruction: determination of connections between parameters of contamination of people residences and levels of irradiation on thyroid glands. (In Russian) Minsk: Final Report of Institute of Biophysics, Moscow Contract N 7-17/93 with the Ministry of Public Health; 1994.
Stepanenko V, Gavrilin Y, Khrousch V, et al. The reconstruction of thyroid dose following Chernobyl. In: Karaoglou A, Desmet G, Kelly GN, Menzel HG, editors. The radiological consequences of the Chernobyl accident. Brussels: European Commission; 1996. p. 937–48.
Tsyb AF, Parshkov EM, Shakhtarin VV, Stepanenko VF, Skvortsov VF, Chebotareva IV. Thyroid cancer in children and adolescents of Bryansk and Kaluga regions. In: Karaoglou A, Desmet G, Kelly GN, Menzel HG, editors. The radiological consequences of the Chernobyl accident. Brussels: European Commission; 1996. p. 691–7.
Zvonova I, Balonov MI. Radioiodine dosimetry and prediction of thyroid effects on inhabitants of Russia following the Chernobyl accident. In: Merwin SE, Balonov MI, editors. The Chernobyl papers, vol. I: doses to the Soviet population and early health effects studies. Richland: Research Enterprises; 1993. p. 71–126.
Sobolev B, Likhtarev I, Kairo I, Tronko N, Oleynik V, Bogdanova T. Radiation risk assessment of the thyroid cancer in Ukrainian children exposed due to Chernobyl. In: Karaoglou A, Desmet G, Kelly GN, Menzel HG, editors. The radiological consequences of the Chernobyl accident. Brussels: European Commission; 1996. p. 741–8.
Likhtarev IA, Sobolev BG, Kairo IA, Tronko ND, Bogdanova TI, Oleinic VA, et al. Thyroid cancer in the Ukraine. Nature. 1995;375:365.
Likhtarev IA, Shandala NK, Gulko GM, Kairo IA, Chepurny NI. Ukrainian thyroid doses after the Chernobyl accident. Health Phys. 1993;64:594–9.
Likhtarev I, Sobolev B, Kairo I, et al. Results of large scale thyroid dose reconstruction in Ukraine. In: Karaoglou A, Desmet G, Kelly GN, Menzel HG, editors. The radiological consequences of the Chernobyl accident. Brussels: European Commission; 1996. p. 1021–34.
Likhtarev IA, Gulko GM, Sobolev BG, et al. Thyroid dose assessment for the Chernigov region (Ukraine): estimation based on 131I thyroid measurements and extrapolation of the results to districts without monitoring. Radiat Environ Biophys. 1994;33:149–66.
Prisyazhiuk A, Pjatak OA, Buzanov VA, Reeves GK, Beral V. Cancer in the Ukraine, post-Chernobyl. Lancet. 1991;338:1334–5.
Oleynic VA, Cheban AK. Thyroid cancer in children of Ukraine from 1981 to 1992. In: Robbins J, editor. Treatment of thyroid cancer in childhood. Proceedings of a workshop on September 10–11, 1992, at the National Institutes of Health. Publication No. DOE/EH-0406; 1992. p. 35.
Astakhova LN. Condition of the thyroid system and peculiarity of forming its pathology in the BSSR population under influence of the iodine-radionuclides in connection with Chernobyl nuclear accident. Zdravoohranenie Belorussi. 1990;6:11–5. In Russian.
Astakhova LN, Demidchuk EP, Davydova EV, et al. Health status of Byelorussian children and adolescents exposed to radiation as consequence of the Chernobyl atomic energy station accident. Vestn Akad Med Nauk USSR. 1991;11:25–7. In Russian.
Okeanov AE, Averkin YI. Analysis of malignant neoplasms in population of the Republic of Belarus before and after the Chernobyl accident. In: Matyukhin VA, Astakhova LN, Konigsberg YE, Nalivko SN, editors. Catastrophe at the Chernobyl atomic energy station and estimation of health state of population of the Republic of Belarus. Minsk: Research Institute of Radiation Medicine; 1991. p. 25–33.
Astakhova LN, Vorontsova TV, Drozd VM. Thyroid nodule pathology in children of Belarus following the Chernobyl accident. In: Robbins J, editor. Treatment of thyroid cancer in childhood. Proceedings of a workshop on September 10–11, 1992, at the National Institutes of Health. Publication No. DOE/EH-0406; 1992. p. 35.
Baverstock K, Egloff B, Finchera A, Ruchti C, Williams D. Thyroid cancer after Chernobyl. Nature. 1992;359:21–2.
Demidchik EP, Kazakov VS, Astakhova LN, et al. Thyroid cancer in children after the Chernobyl accident: clinical and epidemiological evaluation of 251 cases in the Republic of Belarus. In: Nagataki S, editor. Nagasaki symposium on Chernobyl: update and future. Amsterdam: Elsevier; 1994. p. 21.
Demidchik EP, Drobyshevskaya IM, Cherstvoy ED, et al. Thyroid cancer in children in Belarus. In: Karaoglou A, Desmet G, Kelly GN, Menzel HG, editors. The radiological consequences of the Chernobyl accident. Brussels: European Commission; 1996. p. 677–82.
Abelin T, Averkin JI, Egger M, et al. Thyroid cancer in Belarus post-Chernobyl: improved detection or increased incidence? Soz Praventivmed. 1994;39:189–97.
Averkin JI, Abelin T, Bleuer JP. Thyroid cancer in children in Belarus: ascertainment bias? Lancet. 1995;346:1223–4.
Abelin T, Egger M, Ruchti C. Belarus increase was probably caused by Chernobyl. BMJ. 1994;309:1298.
Williams ED, Cherstvoy E, Egloff B, et al. Interaction of pathology and molecular characterization of thyroid cancers. In: Karaoglou A, Desmet G, Kelly GN, Menzel HG, editors. The radiological consequences of the Chernobyl accident. Brussels: European Commission; 1996. p. 699–714.
Abelin T, Averkin JI, Okeanov AE, Bleuer JP. Thyroid cancer in Belarus: the epidemiologic situation. In: Karaoglou A, Desmet G, Kelly GN, Menzel HG, editors. The radiological consequences of the Chernobyl accident. Brussels: European Commission; 1996. p. 727–30.
Malko M. Chernobyl radiation induced thyroid cancers in Belarus. Joint Institute of Power and Nuclear Research, National Academy of Science of Belarus, pp. 240–55. Available on: http://www.rri.kyoto-u.ac.jp/NSRG/reports/kr79/kr79pdf/Malko2.pdf. Retrieved on 15 Jan 2012.
Demidchik YE, Demidchik EP. Thyroid carcinomas in Belarus 16 years after the Chernobyl disaster. In: Proceedings of symposium of Chernobyl-related health effects. Tokyo: Radiation Effects Association; 2002.
Tsyb AF, Parshkov EM, Ivanov VK, Stepanenko VF, Matveenko EG, Skoropad YD. Disease indices of thyroid and their dose dependence in children and adolescents affected as a result of the Chernobyl accident. In: Nagataki S, editor. Amsterdam: Elsevier Science; 1994. p. 9–19.
Remennik LV, Starinsky VV, Mokina VD, et al. Malignant neoplasms on the territories of Russia damaged owing to the Chernobyl accident. In: Karaoglou A, Desmet G, Kelly GN, Menzel HG, editors. The radiological consequences of the Chernobyl accident. Brussels: European Commission; 1996. p. 825–8.
Tronko N, Bogdanova T, Komissarenko I, et al. Thyroid cancer in children and adolescents in Ukraine after the Chernobyl accident. In: Karaoglou A, Desmet G, Kelly GN, Menzel HG, editors. The radiological consequences of the Chernobyl accident. Brussels: European Commission; 1996. p. 683–90.
Tronko N, Epstein Y, Oleinik V, et al. Thyroid gland in children after the Chernobyl accident (yesterday and today). In: Nagataki S, editor. Nagasaki symposium on Chernobyl: update and future. Amsterdam: Elsevier; 1994. p. 31–46.
Williams ED, Tronko ND. Molecular, cellular, biological characterization of childhood thyroid cancer. Brussels: European Commission; 1996.
Cherstvoy E, Pozcharskaya V, Harach HR, Thomas GA, Williams ED. The pathology of childhood thyroid carcinoma in Belarus. In: Karaoglou A, Desmet G, Kelly GN, Menzel HG, editors. The radiological consequences of the Chernobyl accident. Brussels: European Commission; 1996. p. 779–84.
Bogdanova T, Bragarnik M, Tronko ND, Harach HR, Thomas GA, William ED. The pathology of thyroid cancer in Ukraine post Chernobyl. In: Karaoglou A, Desmet G, Kelly GN, Menzel HG, editors. The radiological consequences of the Chernobyl accident. Brussels: European Commission; 1996. p. 785–9.
Abrosimov AY, Lushnikov EF, Tsyb AF, Harach HR, Thomas GA, Williams ED. The pathology of childhood thyroid tumours in the Russian Federation after Chernobyl. In: Karaoglou A, Desmet G, Kelly GN, Menzel HG, editors. The radiological consequences of the Chernobyl accident. Brussels: European Commission; 1996. p. 791–3.
Furmanchuk AW, Averkin JI, Egloff B, et al. Pathomorphological findings in thyroid cancers of children from the Republic of Belarus: a study of 86 cases occurring between 1986 (“post-Chernobyl”) and 1991. Histopathology. 1992;21:401–8.
Nikiforov Y, Gnepp DR. Pediatric thyroid cancer after the Chernobyl disaster. Cancer. 1994;74:748–66.
Williams ED. Thyroid cancer in United Kingdom children and in children exposed to fallout from Chernobyl. In: Nagataki S, editor. Nagasaki symposium on Chernobyl: update and future. Tokyo: Elsevier; 1994.
Nikiforov Y, Gnepp DR, Fagin JA. Thyroid lesions in children and adolescents after the Chernobyl disaster: implications for the study of radiation tumorigenesis. J Clin Endocrinol Metab. 1996;81:9–14.
Pacini F, Vorontsova T, Demidchik EP, et al. Diagnosis, surgical treatment and follow-up of thyroid cancers. In: Karaoglou A, Desmet G, Kelly GN, Menzel HG, editors. The radiological consequences of the Chernobyl accident. Brussels: European Commission; 1996. p. 755–63.
Nikiforov YE, Heffess CS, Korzenko AV, Fagin JA, Gnepp DR. Characteristics of follicular tumors and nonneoplastic thyroid lesions in children and adolescents exposed to radiation as a result of the Chernobyl disaster. Cancer. 1995;76:900–9.
Sierk AE, Askin FB, Reddick RL, Thomas CG. Pediatric thyroid cancer. Pediatr Pathol. 1990;10:877–93.
Harness JK, Thompson NW, Nishiyama RH. Childhood thyroid carcinoma. Arch Surg. 1971;102:278–84.
Richardson JE, Beaugie JM, Brown CL, Doniach I. Thyroid cancer in young patients in Great Britain. Br J Surg. 1974;61:85–9.
Tallroth E, Backdahl M, Einhorn J, Lundell G, Lowhagen T, Silfversward C. Thyroid carcinoma in children and adolescents. Cancer. 1986;58:2329–32.
Mizukami Y, Michigishi T, Nonomura A, et al. Carcinoma of the thyroid at young age: a review of 23 patients. Histopathology. 1992;20:63–6.
Robbins J. Characteristics of spontaneous and radiation induced thyroid cancers in children. In: Nagataki S, editor. Nagasaki symposium on Chernobyl: update and future. Amsterdam: Elsevier; 1994. p. 81.
Williams ED. Radiation-induced thyroid cancer. Histopathology. 1993;23:387–9.
Willams ED. Chernobyl, eight years on. Nature. 1994;371:556.
Williams D. Thyroid cancer and the Chernobyl accident. J Clin Endocrinol Metab. 1996;81:6–8.
Ito T, Seyama T, Iwamoto KS, Mizuno T, Tronko ND, Komissarenko IV, et al. Activated RET oncogene in thyroid cancers of children from areas contaminated by Chernobyl accident. Lancet. 1994;344:259.
Fugazzola L, Pilotti S, Pinchera A, et al. Oncogenic rearrangements of the RET proto-oncogene in papillary thyroid carcinomas from children exposed to the Chernobyl nuclear accident. Cancer Res. 1995;55:5617–20.
Nikiforov YE, Rowland JM, Bove KE, Monforte-Munoz H, Fagin JA. Distinct pattern of ret oncogene rearrangements in morphological variants of radiation-induced and sporadic thyroid papillary carcinomas in children. Cancer Res. 1997;57:1690–4.
Klugbauer S, Lengfelder E, Demidchik EP, Rabes HM. High prevalence of RET rearrangement in thyroid tumors of children from Belarus after the Chernobyl reactor accident. Oncogene. 1995;11:2459–67.
Rabes HM, Klugbauer S. Radiation-induced thyroid carcinomas in children: high prevalence of RET rearrangement. Verh Dtsch Ges Pathol. 1997;81:139–44. German.
Klugbauer S, Lengfelder E, Demidchik EP, Rabes HM. A new form of RET rearrangement in thyroid carcinomas of children after the Chernobyl reactor accident. Oncogene. 1996;13:1099–102.
Klugbauer S, Demidchik EP, Lengfelder E, Rabes HM. Molecular analysis of new subtypes of ELE/RET rearrangements, their reciprocal transcripts and breakpoints in papillary thyroid carcinomas of children after Chernobyl. Oncogene. 1998;16:671–5.
Fugazzola L, Pierotti M, Vigano E, Pacini F, Verontsova T, Bongarzone I. Molecular and biochemical analysis of RET/PTC4, a novel oncogeneic rearrangement between RET and ELE1 genes, in a post-Chernobyl papillary thyroid cancer. Oncogene. 1996;13:1093–7.
Klugbauer S, Demidchik EP, Lengfelder E, Rabes HM. Detection of a novel type of RET rearrangement (PTC5) in thyroid carcinomas after Chernobyl and analysis of the involved RET-fused gene RFG5. Cancer Res. 1998;58:198–203.
Klugbauer S, Rabes HM. The transcription coactivator HTIF1 and a related protein are fused to the RET receptor tyrosine kinase in childhood papillary thyroid carcinomas. Oncogene. 1999;18:4388–93.
Salassidis K, Bruch J, Zitzelsberger H, Lengfelder E, Kellerer AM, Bauchinger M. Translocation t(10;14)(q11.2:q22.1) fusing the kinectin to the RET gene creates a novel rearranged form (PTC8) of the RET proto-oncogene in radiation-induced childhood papillary thyroid carcinoma. Cancer Res. 2000;60:2786–9.
Klugbauer S, Jauch A, Lengfelder E, Demidchik E, Rabes HM. A novel type of RET rearrangement (PTC8) in childhood papillary thyroid carcinomas and characterization of the involved gene (RFG8). Cancer Res. 2000;60:7028–32.
Rabes HM, Demidchik EP, Sidorow JD, et al. Pattern of radiation-induced RET and NTRK1 rearrangements in 191 post-Chernobyl papillary thyroid carcinomas: biological, phenotypic, and clinical implications. Clin Cancer Res. 2000;6:1093–103.
Rabes HM. Gene rearrangements in radiation-induced thyroid carcinogenesis. Med Pediatr Oncol. 2001;36:574–82.
Pisarchik AV, Ermak G, Fomicheva V, Kartel NA, Figge J. The ret/PTC1 rearrangement is a common feature of Chernobyl-associated papillary thyroid carcinomas from Belarus. Thyroid. 1998;8:133–9.
Pisarchik AV, Ermak G, Demidchik EP, Mikhalevich LS, Kartel NA, Figge J. Low prevalence of the ret/PTC3r1 rearrangement in a series of papillary thyroid carcinomas presenting in Belarus ten year post-Chernobyl. Thyroid. 1998;8:1003–8.
Pisarchik AV, Yarmolinskii DG, Demidchik YE, Ermak GZ, Kartel NA, Figge J. ret/PTC1 and ret/PTC3r1 rearrangement in thyroid cancer cells, arising in residents of Belarus in the period after the accident at the Chernobyl nuclear power plant. Genetika. 2000;36:959–64. In Russian.
Smida J, Salassidis K, Hieber L, et al. Distinct frequency of ret rearrangements in papillary thyroid carcinomas of children and adults from Belarus. Int J Cancer. 1999;80:32–8.
Thomas GA, Bunnell H, Cook HA, et al. High prevalence of RET/PTC rearrangements in Ukrainian and Belarussian post-Chernobyl thyroid papillary carcinomas: a strong correlation between RET/PTC3 and the solid-follicular variant. J Clin Endocrinol Metab. 1999;84:4232–8.
Santoro M, Thomas GA, Vecchio G, et al. Gene rearrangement and Chernobyl related thyroid cancers. Br J Cancer. 2000;82:315–22.
Williams ED, Abrosimov A, Bogdanova T, et al. Thyroid carcinoma after Chernobyl latent period, morphology and aggressiveness. Br J Cancer. 2004;90:2219–24.
Elisei R, Romei C, Vorontsova T, et al. RET/PTC rearrangements in thyroid nodules: studies in irradiated and not irradiated, malignant and benign thyroid lesions in children and adults. J Clin Endocrinol Metab. 2001;86:3211–6.
Jhiang SM, Sagartz JE, Tong Q, et al. Targeted expression of the RET/PTC1 oncogene induces papillary thyroid carcinomas. Endocrinology. 1996;137:375–8.
Santoro M, Chiappetta G, Cerrato A, et al. Development of thyroid papillary carcinomas secondary to tissue-specific expression of the RET/PTC1 oncogene in transgenic mice. Oncogene. 1996;12:1821–6.
Powell Jr DJ, Russell J, Nibu K, et al. The RET/PTC3 oncogene: metastatic solid-type papillary carcinomas in murine thyroids. Cancer Res. 1998;58:5523–8.
Ito T, Seyama T, Iwamoto KS, et al. In vitro irradiation is able to cause RET oncogene rearrangement. Cancer Res. 1993;53:2940–3.
Bounacer A, Wicker R, Caillou B, et al. High prevalence of activating ret proto-oncogene rearrangements, in thyroid tumors from patients who had received external radiation. Oncogene. 1997;15:1263–73.
Collins BJ, Chiappetta G, Schneider AB, et al. RET expression in papillary thyroid cancer from patients irradiated in childhood for benign conditions. J Clin Endocrinol Metab. 2002;87:3941–6.
Elisei R, Romei C, Soldatenko PP, Cosci B, Vorontsova T, Vivaldi A, et al. New breakpoints in both the H4 and RET genes create a variant of PTC-1 in a post-Chernobyl papillary thyroid carcinoma. Clin Endocrinol. 2000;53:131–6.
Corvi R, Berger N, Balczon R, Romeo G. RET/PCM-1: a novel fusion gene in papillary thyroid carcinoma. Oncogene. 2000;19:4236–42.
Nakata T, Kitamura Y, Shimizu K, Tanaka S, Fujimori M, Yokoyama S, Ito K, Emi M. Fusion of a novel gene, ELKS, to RET due to translocation t(10;12)(q11;p13) in a papillary thyroid carcinoma. Genes Chromosomes Cancer. 1999;25:97–103.
Giannini R, Salvatore G, Monaco C, Sferratore F, Pollina L, Pacini F, et al. Identification of a novel subtype of H4-RET rearrangement in a thyroid papillary carcinoma and lymph node metastasis. Int J Oncol. 2000;16:485–9.
Butti MG, Bongarzone I, Ferraresi G, Mondellini P, Borrello MG, Pierotti MA. A sequence analysis of the genomic regions involved in the rearrangements between TPM3 and NTRK1 genes producing TRK oncogenes in papillary thyroid carcinomas. Genomics. 1995;28:15–24.
Beimfohr C, Klugbauer S, Demidchik EP, Lengfelder E, Rabes HM. NTRK1 re-arrangement in papillary thyroid carcinomas of children after the Chernobyl reactor accident. Int J Cancer. 1999;80:842–7.
Nikiforov YE, Nikiforova MN, Gnepp DR, Fagin JA. Prevalence of mutations of ras and p53 in benign and malignant thyroid tumors from children exposed to radiation after the Chernobyl nuclear accident. Oncogene. 1996;13:687–93.
Hillebrandt S, Streffer C, Reiners C, Demidchik E. Mutations in the p53 tumor suppressor gene in thyroid tumors of children from areas contaminated by the Chernobyl accident. Int J Radial Biol. 1996;69:39–45.
Hillebrandt S, Streffer C, Demidchik EP, Biko J, Reiners C. Polymorphisms in the p53 gene in thyroid tumors and blood samples of children from areas in Belarus. Mutat Res. 1997;381:201–7.
Smida J, Zitzelsberger H, Kellerer AM, et al. P53 mutations in childhood thyroid tumors from Belarus and in thyroid tumors without radiation history. Int J Cancer. 1997;73:802–7.
Suchy B, Waldmann V, Klugbauer S, Rabes HM. Absence of RAS and p53 mutations in thyroid carcinomas of children after Chernobyl in contrast to adult thyroid tumors. Br J Cancer. 1998;77:952–5.
Pisarchik AV, Ermak G, Kartel NA, Figge J. Molecular alterations involving p53 codons 167 and 183 in papillary thyroid carcinomas from Chernobyl-contaminated regions of Belarus. Thyroid. 2000;10:25–30.
Ciampi R, Knauf JA, Kerler R, Gandhi M, Zhu Z, Nikiforova MN, Rabes HM, Fagin JA, Nikiforov YE. Oncogenic AKAP9-BRAF fusion is a novel mechanism of MAPK pathway activation in thyroid cancer. J Clin Invest. 2005;115(1):94–101.
Beral V, Reeves G. Childhood thyroid cancer in Belarus. Nature. 1992;359:680–1.
Shigematsu I, Thiessen JW. Childhood thyroid cancer in Belarus. Nature. 1992;359:681.
Beebe GW. Epidemiologic studies of thyroid cancer in the CIS. In: Karaoglou A, Desmet G, Kelly GN, Menzel HG, editors. The radiological consequences of the Chernobyl accident. Brussels: European Commission; 1996. p. 731–40.
Astakhova LN, Anspaugh LR, Beebe GW, Bouville A, Drozdovitch VV, Garber V, et al. Chernobyl-related thyroid cancer in children of Belarus: a case-control study. Radiat Res. 1998;150:349–56.
Jacob P, Goulko G, Heidenreich WF, et al. Thyroid cancer risk to children calculated. Nature. 1998;392:31–2.
Shibata Y, Yamashita S, Masyakin VB, Panasyuk GD, Nagataki S. 15 years after Chernobyl: new evidence of thyroid cancer. Lancet. 2001;358:1965–6.
Cardis E, Kesminiene A, Ivanov V, Malakhova I, Shibata Y, Khrouch V, Drozdovitch V, Maceika E, Zvonova I, Vlassov O, Bouville A, Goulko G, Hoshi M, Abrosimov A, Anoshko J, Astakhova L, Chekin S, Demidchik E, Galanti R, Ito M, Korobova E, Lushnikov E, Maksioutov M, Masyakin V, Nerovnia A, Parshin V, Parshkov E, Piliptsevich N, Pinchera A, Polyakov S, Shabeka N, Suonio E, Tenet V, Tsyb A, Yamashita S, Williams D. Risk of thyroid cancer after exposure to 131I in childhood. J Natl Cancer Inst. 2005;97(10):724–32.
Davis S, Stepanenko V, Rivkind N, Kopecky KJ, Voillequé P, Shakhtarin V, Parshkov E, Kulikov S, Lushnikov E, Abrosimov A, Troshin V, Romanova G, Doroschenko V, Proshin A, Tsyb A. Risk of thyroid cancer in the Bryansk oblast of the Russian Federation after the Chernobyl power station accident. Radiat Res. 2004;162(3):241–8.
Tronko MD, Howe GR, Bogdanova TI, Bouville AC, Epstein OV, Brill AB, Likhtarev IA, Fink DJ, Markov VV, Greenebaum E, Olijnyk VA, Masnyk IJ, Shpak VM, McConnell RJ, Tereshchenko VP, Robbins J, Zvinchuk OV, Zablotska LB, Hatch M, Luckyanov NK, Ron E, Thomas TL, Voillequé PG, Beebe GW. A cohort study of thyroid cancer and other thyroid diseases after the Chornobyl accident: thyroid cancer in Ukraine detected during first screening. J Natl Cancer Inst. 2006;98:897–903.
Brenner AV, Tronko MD, Hatch M, Bogdanova TI, Oliynik VA, Lubin JH, Zablotska LB, Tereschenko VP, McConnell RJ, Zamotaeva GA, O’Kane P, Bouville AC, Chaykovskaya LV, Greenebaum E, Paster IP, Shpak VM, Ron E. I-131 dose response for incident thyroid cancers in Ukraine related to the Chornobyl accident. Environ Health Perspect. 2011;119(7):933–9. Epub 2011 Mar 14.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this chapter
Cite this chapter
Figge, J.J., Jennings, T.A., Gerasimov, G., Kartel, N.A., Ermak, G. (2016). Radiation-Induced Thyroid Cancer. In: Wartofsky, L., Van Nostrand, D. (eds) Thyroid Cancer. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-3314-3_7
Download citation
DOI: https://doi.org/10.1007/978-1-4939-3314-3_7
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-3312-9
Online ISBN: 978-1-4939-3314-3
eBook Packages: MedicineMedicine (R0)