Abstract
Chemotherapy has been used as a single-modality treatment or as part of combined-modality therapy in metastatic or locally advanced thyroid cancer when other conventional treatments (e.g., surgery and radiation therapy) have failed. Recent developments in the understanding of the molecular pathogenesis of thyroid cancer have allowed for more targeted investigations, but cytotoxic chemotherapy remains an important part of the armamentarium, particularly for anaplastic and relatively undifferentiated thyroid cancers. Numerous reports on the use of chemotherapy in a variety of thyroid cancers have been published, but only a few controlled clinical trials compare the efficacy of different drug regimens. We outline both conventional cytotoxic chemotherapeutic agents and novel targeted agents below.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Chemotherapy has been used as a single-modality treatment or as part of combined-modality therapy in metastatic or locally advanced thyroid cancer when other conventional treatments (e.g., surgery and radiation therapy) have failed. Recent developments in the understanding of the molecular pathogenesis of thyroid cancer have allowed for more targeted investigations, but cytotoxic chemotherapy remains an important part of the armamentarium, particularly for anaplastic and relatively undifferentiated thyroid cancers. Numerous reports on the use of chemotherapy in a variety of thyroid cancers have been published, but only a few controlled clinical trials compare the efficacy of different drug regimens. We outline both conventional cytotoxic chemotherapeutic agents and novel targeted agents below.
Cytotoxic Chemotherapy
Prior to the early 1970s, experience with individual chemotherapeutic agents in thyroid cancer was largely limited to case reports without systematic evaluation of efficacy in clinical trials [1]. Individual cytotoxic chemotherapeutic agents with known (or proposed) antitumor activity against thyroid cancer are listed in Table 64.1. Patient nutritional status and performance statuses have been noted as important predictors of response to these agents [2, 3]. Selected agents are discussed below.
Bleomycin
Bleomycin is an antineoplastic antibiotic that impairs DNA synthesis by generating superoxide and hydroxyl radicals that cause single- and double-stranded DNA breaks. It was the first chemotherapeutic agent reported effective in thyroid cancer [4, 5]. However, due to limited activity as monotherapy with associated risk of pulmonary toxicity, subsequent study focused primarily on combination regimens. A retrospective study of doxorubicin, bleomycin, and vincristine (ABC) in thyroid cancer reported responses in 5 of 13 patients (38 %) [6], and a phase II study of ABC-melphalan reported short-term responses in 4 of 11 patients (37 %) [7]. A retrospective study of bleomycin, doxorubicin, and cis-platinum (BAP) in 21 patients noted responses in 9 patients (42 %); the best responses were seen in individuals with medullary thyroid cancer (MTC) or anaplastic thyroid cancer (ATC) [8].
Doxorubicin
Doxorubicin is an anthracycline derivative that has been the most widely used and studied cytotoxic chemotherapeutic agent in thyroid cancer. On the basis of observational experience and initial results from phase I and II studies [1, 9], further investigation of doxorubicin monotherapy was pursued. Gottlieb and Hill enrolled patients with all histologic subtypes of thyroid cancer and reported that 11 of 30 patients treated with 45–75 mg/m2 doxorubicin every 3 weeks had greater than 50 % reductions in the size of their metastases [10]. Responses appeared to be best in patients with pulmonary metastases followed by bone metastases, and several patients with bone metastases reported subjective improvements in bone pain with treatment. Subsequent studies of doxorubicin monotherapy were undertaken, and a summary of these early studies suggested a response rate of 38.5 % in patients with differentiated thyroid cancer (DTC) (n = 109) and 41 % in patients with Hürthle cell carcinoma (n = 41) [11]. However, these studies were not placebo controlled and had varying inclusion criteria and definitions of response, which limited extrapolation. A more recent retrospective study of 22 patients with progressive, metastatic, unresectable DTC or medullary thyroid cancer (MTC) treated with either doxorubicin 60 mg/m2 every 3 weeks for 3–6 cycles or 15 mg/m2 weekly for 8–16 cycles documented WHO partial responses (PR) in 5 % of patients and stable disease in 42 % (median 7 months) [12]. A comparison of the two dosing regimens in DTC suggested better responses with 60 mg/m2 every 3 weeks compared to 15 mg/m2 weekly (PR: 11 % vs. 0 %, SD: 67 % vs. 20 %, PD: 22 % vs. 80 %). Common side effects are neutropenia, nausea, emesis, and alopecia. The recommended dose is 60–75 mg/m2 every 3 weeks, with cumulative dosing not recommended to exceed 450 mg/m2 due to the risk of anthracycline-associated cardiomyopathy.
Epirubicin
Epirubicin is an anthracycline analog of doxorubicin, with dose-limiting myelosuppression and less cardiotoxicity than doxorubicin [13]. Santini and colleagues investigated the combination of the epirubicin with carboplatin in a small single-arm study of patients with progressive, metastatic poorly differentiated thyroid cancer [14]. A total of 14 patients were treated with carboplatin 300 mg/m2 and epirubicin 75 mg/m2 every 4–6 weeks. These patients also underwent TSH stimulation in an attempt to improve response to therapy. Responses were comparable to other historical regimens (CR: 6 %, PR: 31 %, SD: 44 %).
Cisplatin
Cisplatin is an inorganic platinum agent which forms intra- and interstrand DNA cross-links, leading to tumor cell death. Several early studies documented the activity of cisplatin as a single agent in advanced thyroid cancer. Hoskin and Harmer [6] reported objective responses in 5 out of 13 patients treated with cisplatin; responses were noted in all tumor histologies, including DTC, MTC, and ATC. Similar response rates were noted in subsequent studies [15], though response rates appeared lower in patients with DTC who had progressed following treatment with doxorubicin [16]. Toxicities include myelosuppression, nephrotoxicity, and ototoxicity.
Paclitaxel
Paclitaxel is a compound derived from the Pacific yew tree which stabilizes microtubules and inhibits cell division. Higashiyama and colleagues [17] reported objective responses in 4 out of 13 patients with anaplastic thyroid cancer treated with paclitaxel administered weekly as a 1-h infusion. A second study of paclitaxel administered as a continuous 96-h infusion in anaplastic thyroid cancer reported responses in 10 out of 20 patients [18]. Common toxicities include peripheral neuropathy and myelosuppression.
Targeted Agents
The last decade has witnessed an impressive expansion in our understanding of the disease pathobiology of advanced thyroid cancer and the advent of several novel targeted therapies. Several of these agents are summarized in Table 64.2. Selected agents are discussed below.
FDA-Approved Targeted Therapy
Vandetanib
Vandetanib (Zactima, Caprelsa) is an orally bioavailable tyrosine-kinase inhibitor of RET, VEGFR-2, and EGFR [19, 20]. The results of a randomized, double-blinded, multicenter placebo-controlled phase III trial of vandetanib in patients with locally advanced or metastatic MTC (ZETA trial) were reported in 2011 [21]. A total of 331 patients were enrolled in the trial. Progression-free survival at 6 months was 83 % in the vandetanib arm, compared to 63 % in the placebo arm (HR for progression 0.45, CI 0.30–0.69). Improvements were also noted in the overall response rate, disease control rate, and biochemical response rates. Overall survival was not significantly different between the two groups, but this was confounded in part by the crossover design of the study. Common side effects included diarrhea, rash, nausea, hypertension, and headache. It is currently one of two targeted therapies approved by the US Food and Drug Administration (FDA) for advanced, unresectable, or metastatic MTC.
Investigational Targeted Therapies
Cabozantinib
Cabozantinib (XL184) is a potent, orally bioavailable receptor tyrosine-kinase inhibitor of Met, VEGFR-2, KIT, RET, FLT3, and Tie-2. The results from a large, phase III, randomized, placebo-controlled study in patients with MTC were published in 2013 [22]. A total of 330 patients were enrolled in the trial; median PFS in patients treated with placebo was 4.0 months, compared to 11.2 months in patients receiving cabozantinib (HR 0.28, p < 0.001). Unlike the ZETA trial, patients on this trial were not allowed to cross over on progression. Overall survival data were analyzed in an interim analysis when 44 % of 217 required events had occurred and no difference was seen between the two arms (HR 0.98; 95 % CI 0.63–1.52). All patients were required to have evidence of disease progression within the last 14 months prior to enrollment. The most frequent grade 3 events included diarrhea (15.9 % vs. 1.8 %), hand-foot syndrome (12.6 % vs. 0 %), fatigue (9.3 % vs. 2.8 %), hypocalcemia (2.8 % vs. 0 %), and hypertension (7.9 % vs. 0 %) in the two groups, respectively. This agent was the second FDA-approved therapy for use in progressive, metastatic MTC.
Pazopanib
Pazopanib (Votrient) is an orally bioavailable inhibitor of VEGFR-1–3, PDGFR, and KIT [23] that is FDA-approved for the treatment of advanced renal cell carcinoma. Results of an NCI-sponsored multicenter, phase II trial of pazopanib in patients with locally advanced or metastatic, radioiodine-resistant DTC were reported in 2010 [24]. Despite the fact that all patients had evidence of progressive disease at enrollment, partial responses were seen in 18 of 37 patients, and there was a reported median progression-free survival of 11.7 months. Adverse events were common and similar to other VEGFR-targeted tyrosine-kinase inhibitors, including fatigue, skin and hair hypopigmentation, diarrhea, nausea, and hypertension. Two deaths occurred during treatment, including one fatal myocardial infarction and a bowel perforation following a complicated case of cholecystitis.
Sorafenib
Sorafenib (Nexavar) is a multi-kinase inhibitor with activity against VEGFR-2–3, PDGFR-β, FLT3, KIT, Raf-1, BRAF, and RET kinases and was approved by the FDA in November 2013 for use in metastatic differentiated thyroid cancer based on the results of the DECISION trial [25]. It is also approved for the treatment of hepatocellular carcinoma and renal cell carcinoma. The phase III randomized placebo-controlled DECISION trial enrolled 417 patients with radioactive iodine-refractory locally advanced or metastatic differentiated thyroid cancer that had progressed within the past 14 months and randomized them on a 1:1 basis. Median PFS was significantly longer in the sorafenib-treated group compared to the placebo-treated group (10.8 months vs. 5.8 months, HR 0.59, p < 0.0001). Seventy-one percent of placebo-treated patients crossed over to open-label sorafenib upon disease progression. Overall survival did not differ significantly between the groups (HR 0.80, p = 0.14), and the median survival had not been reached at the time of primary analysis data cutoff. The most frequent adverse events included hand-foot skin reaction (76.3 %), diarrhea (68.6 %), alopecia (67.1 %), and rash or desquamation (50.2 %) Five phase II clinical trials have evaluated sorafenib in patients with all histologies of thyroid cancer [26–30]. Objective response rates range from 11 to 25 % with clinical benefit rates (objective responses or stable disease of at least 6 months) of 59–74 %. Toxicities were similar in the four trials, with the most common adverse events being hand-foot syndrome, rash, fatigue, diarrhea, bloating, musculoskeletal pain, weight loss, and mucositis. Roughly one-third of patients also required adjustments in their thyroid replacement.
Sunitinib
Sunitinib (Sutent) is a multi-kinase inhibitor with activity against VEGFR-1, VEGFR-2, PDGFR, c-KIT, FLT3, and RET that is approved for treatment of renal cell carcinoma, gastrointestinal stromal tumors resistant to imatinib, and pancreatic neuroendocrine tumors. Four phase II studies have investigated sunitinib in advanced differentiated or medullary thyroid cancer [31–34]. Objective responses were seen in 13–33 % of patients. Common side effects include fatigue, lymphopenia, nausea, diarrhea, mucositis, and hand-foot syndrome.
Summary
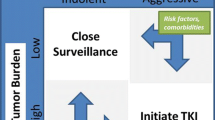
Cytotoxic chemotherapeutic agents have historically been the backbone for treatment of advanced, unresectable thyroid cancer. Cytotoxic agents remain important as a component of multimodality therapy for anaplastic thyroid cancer. However, targeted agents have emerged as frontline therapy for the majority of patients with advanced differentiated or medullary thyroid cancers [35]. See Chaps. 71, 83, and 94 for further discussion of chemotherapy in DTC, MTC, and ATC, respectively.
References
Gottlieb JA, et al. Chemotherapy of thyroid cancer. An evaluation of experience with 37 patients. Cancer. 1972;30(3):848–53.
O’Bryan RM, et al. Dose response evaluation of adriamycin in human neoplasia. Cancer. 1977;39(5):1940–8.
Shimaoka K, et al. A randomized trial of doxorubicin versus doxorubicin plus cisplatin in patients with advanced thyroid carcinoma. Cancer. 1985;56(9):2155–60.
Harada T, et al. Bleomycin treatment for cancer of the thyroid. Am J Surg. 1971;122(1):53–7.
Harada T, et al. Bleomycin beneficial for thyroid cancer. Aerosp Med. 1972;43(3):330.
Hoskin PJ, Harmer C. Chemotherapy for thyroid cancer. Radiother Oncol. 1987;10(3):187–94.
Bukowski RM, et al. Combination chemotherapy of metastatic thyroid cancer. Phase II study. Am J Clin Oncol. 1983;6(5):579–81.
De Besi P, et al. Combined chemotherapy with bleomycin, adriamycin, and platinum in advanced thyroid cancer. J Endocrinol Invest. 1991;14(6):475–80.
Bonadonna G, et al. Phase I and preliminary phase II evaluation of adriamycin (NSC 123127). Cancer Res. 1970;30(10):2572–82.
Gottlieb JA, Hill Jr CS. Chemotherapy of thyroid cancer with adriamycin. Experience with 30 patients. N Engl J Med. 1974;290(4):193–7.
Haugen BR. Management of the patient with progressive radioiodine non-responsive disease. Semin Surg Oncol. 1999;16(1):34–41.
Matuszczyk A, et al. Chemotherapy with doxorubicin in progressive medullary and thyroid carcinoma of the follicular epithelium. Horm Metab Res. 2008;40(3):210–3.
Smith LA, et al. Cardiotoxicity of anthracycline agents for the treatment of cancer: systematic review and meta-analysis of randomised controlled trials. BMC Cancer. 2010;10:337.
Santini F, et al. Cytotoxic effects of carboplatinum and epirubicin in the setting of an elevated serum thyrotropin for advanced poorly differentiated thyroid cancer. J Clin Endocrinol Metab. 2002;87(9):4160–5.
Droz JP, et al. Chemotherapy for medullary cancer of the thyroid. Phase II trials with adriamycin and cis-platinum administered as monochemotherapy. Bull Cancer. 1984;71(3):195–9.
Droz JP, et al. Phase II trials of chemotherapy with adriamycin, cisplatin, and their combination in thyroid cancers: a review of 44 cases. Int Congr Ser. 1985;684:203–8.
Higashiyama T, et al. Induction chemotherapy with weekly paclitaxel administration for anaplastic thyroid carcinoma. Thyroid. 2010;20(1):7–14.
Ain KB, Egorin MJ, DeSimone PA. Treatment of anaplastic thyroid carcinoma with paclitaxel: phase 2 trial using ninety-six-hour infusion. Collaborative Anaplastic Thyroid Cancer Health Intervention Trials (CATCHIT) Group. Thyroid. 2000;10(7):587–94.
Wedge SR, et al. ZD6474 inhibits vascular endothelial growth factor signaling, angiogenesis, and tumor growth following oral administration. Cancer Res. 2002;62(16):4645–55.
Carlomagno F, et al. ZD6474, an orally available inhibitor of KDR tyrosine kinase activity, efficiently blocks oncogenic RET kinases. Cancer Res. 2002;62(24):7284–90.
Wells Jr SA, et al. Vandetanib in patients with locally advanced or metastatic medullary thyroid cancer: a randomized, double-blind phase III trial. J Clin Oncol. 2012;30(2):134–41.
Elisei R, et al. Cabozantinib in progressive medullary thyroid cancer. J Clin Oncol. 2013;31(29):3639–46.
Kumar R, et al. Pharmacokinetic-pharmacodynamic correlation from mouse to human with pazopanib, a multikinase angiogenesis inhibitor with potent antitumor and antiangiogenic activity. Mol Cancer Ther. 2007;6(7):2012–21.
Bible KC, et al. Efficacy of pazopanib in progressive, radioiodine-refractory, metastatic differentiated thyroid cancers: results of a phase 2 consortium study. Lancet Oncol. 2010;11(10):962–72.
Brose MS, et al. Sorafenib in radioactive iodine-refractory, locally advanced or metastatic differentiated thyroid cancer: a randomised, double-blind, phase 3 trial. Lancet. 2014;384:319–28.
Gupta-Abramson V, et al. Phase II trial of sorafenib in advanced thyroid cancer. J Clin Oncol. 2008;26(29):4714–9.
Kloos RT, et al. Phase II trial of sorafenib in metastatic thyroid cancer. J Clin Oncol. 2009;27(10):1675–84.
Hoftijzer H, et al. Beneficial effects of sorafenib on tumor progression, but not on radioiodine uptake, in patients with differentiated thyroid carcinoma. Eur J Endocrinol. 2009;161(6):923–31.
Lam ET, et al. Phase II clinical trial of sorafenib in metastatic medullary thyroid cancer. J Clin Oncol. 2010;28(14):2323–30.
Ahmed M, et al. Analysis of the efficacy and toxicity of sorafenib in thyroid cancer: a phase II study in a UK based population. Eur J Endocrinol. 2011;165(2):315–22.
Carr LL, et al. Phase II study of daily sunitinib in FDG-PET-positive, iodine-refractory differentiated thyroid cancer and metastatic medullary carcinoma of the thyroid with functional imaging correlation. Clin Cancer Res. 2010;16(21):5260–8.
Cohen E, et al. Phase 2 study of sunitinib in refractory thyroid cancer. J Clin Oncol. 2008;26(20 suppl):abstr 6025.
De Souza J, et al. Phase II trial of sunitinib in medullary thyroid cancer (MTC). J Clin Oncol. 2010;28(15S):abstr 5504.
Ravaud A, et al. Efficacy of sunitinib in advanced medullary thyroid carcinoma: intermediate results of phase II THYSU. Oncologist. 2010;15(2):212–3; author reply 214.
Tuttle R, et al. NCCN clinical practice guidelines in oncology (NCCN guidelines): thyroid carcinoma. 2014. www.nccn.org.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this chapter
Cite this chapter
Liebner, D.A., Haraldsdottir, S., Shah, M.H. (2016). Chemotherapy of Thyroid Cancer: General Principles. In: Wartofsky, L., Van Nostrand, D. (eds) Thyroid Cancer. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-3314-3_64
Download citation
DOI: https://doi.org/10.1007/978-1-4939-3314-3_64
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-3312-9
Online ISBN: 978-1-4939-3314-3
eBook Packages: MedicineMedicine (R0)