Abstract
Retinopathy of prematurity (ROP) is a proliferative disorder involving the developing vasculature of premature infants that can result in retinal detachment and blindness. Timely screening for ROP and prompt treatment of severe ROP can decrease the prevalence of unfavorable retinal structural and poor visual outcome. The criteria for treatment of ROP has evolved from classic threshold ROP, as defined in the Multicenter Trial of Cryotherapy for ROP, to type 1 prethreshold ROP, as defined in the Early Treatment of ROP randomized trial, with incremental improvement in the overall treatment outcome. The mode of treatment has also transitioned from the use of cryotherapy to laser photocoagulation. The mouse model of oxygen-induced retinopathy has elucidated the pathogenesis of ROP and led to new interventions and screening approaches. Pharmacotherapy using the intravitreal injection of bevacizumab, an antibody to vascular endothelial growth factor, appears to be superior to laser photocoagulation for type 1 ROP in zone I but equivalent to laser therapy for type 1 ROP in zone II. However, the systemic risks associated with bevacizumab are uncertain. New screening algorithms based on the rate of postnatal growth of at risk infants are being developed in order to reduce the percentage of infants screened while maintaining efficacy. Digital fundus photography has a high degree of accuracy for the detection of treatment warranting ROP. Validation studies for the reliability and accuracy of telemedicine for ROP are under way.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Background
Retinopathy of prematurity (ROP) is a proliferative disorder involving the retinal vasculature of premature infants that can result in retinal detachment and blindness . Retinal vessels develop from the optic nerve beginning at 14–15 weeks of gestation and proceed peripherally to fully vascularize the retina to the ora serrata nasally and temporally by 32 weeks and approximately 40 weeks postmenstrual age (PMA), respectively [1].
In the currently accepted model of ROP pathogenesis (Table 29.1), the vascularization of the retina is dependent upon both insulin-like growth factor 1 (IGF-1) and vascular endothelial growth factor (VEGF) and may be divided into two phases [2, 3]. In phase I, premature birth disrupts the normal retinal vascularization process by depriving the premature infant of IGF-1, which is normally derived from the placenta and amniotic fluid in utero. VEGF, in the absence of IGF-1, is not sufficient to promote maximum retinal angiogenesis. In addition, VEGF expression is downregulated by the relatively higher oxygen environment outside the womb. Consequently, normal retinal vascularization during phase I is diminished.
Several weeks after birth, during phase II of ROP, the metabolic demand of the maturing retina increases. Relative hypoxia of the avascular retina develops and results in an up-regulation of VEGF. However, the higher levels of VEGF alone are not effective in promoting vascularization of the retina unless sufficient IGF-1 is also present. In the premature infant, low IGF-1 levels are associated with poor nutritional intake and poor weight gain [4]. As the infant gains weight postnatally over several weeks, IGF-1 levels also rise to a threshold level which then has a permissive effect on VEGF-stimulated retinal angiogenesis. If retinal vascular development up to this point has been sufficiently blunted by the previously low expression of VEGF and IGF-1, extraretinal neovascular proliferation may occur. This abnormal proliferative process may regress if retina vascularization continues such that hypoxia is diminished and VEGF expression reduced. But the persistence of hypoxia can result in continued fibrovascular proliferation and ultimately lead to a retinal detachment.
Clinical Appearance and Classification of ROP
Timely screening for and prompt treatment of severe ROP can prevent the development of unfavorable retinal structural outcome and visual loss. The International Classification for ROP (ICROP) , first developed in 1984 and revised in 2005 [5, 6], enabled clinicians and researchers to describe ROP using a common scheme, which also facilitated the conduct of clinical trials. ROP is classified on the basis of location (zones I–III), severity (stages 1–5), and the extent or number of clock hours of involvement. In general, the more posterior the location, the greater the extent of involvement, and the higher the stage, the more severe the ROP.
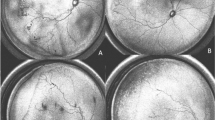
As shown in Fig. 29.1, the zones defined by ICROP are as follows :
-
Zone I is a circle centered upon the optic nerve with a radius that is twice the disc to macula distance.
-
Zone II is the region outside of zone I and inside a circle centered upon the optic nerve with a radius defined by the distance from the optic disc to the nasal ora serrata.
-
Zone III is the remaining temporal crescent provided that the nasal retina is fully vascularized to the ora serrata for at least 2 clock hours.
The stages of ROP are defined as follows :
-
Stage 0—immature vascularization
-
Stage 1—demarcation line
-
Stage 2—ridge (demarcation line with height and width)
-
Stage 3—extraretinal fibrovascular proliferation
-
Stage 4—partial retinal detachment
-
4A—not macula involving
-
4B—macula involving
-
-
Stage 5—total retinal detachment , which is funnel shaped and described based on the anterior and posterior configurations as open-open, open-closed, closed-open, or closed-closed.
In addition, plus disease, which usually develops with stage 3 ROP but may occur with other stages of ROP, is defined as venous dilation and arteriolar tortuosity in the posterior pole. Currently, the diagnosis of plus disease requires at least two quadrants of vessel dilation and tortuosity consistent with a standard reference photograph [6]. However, there is a subjective element in the examiner’s perception of vessel dilatation and tortuosity and, consequently, in the diagnosis of plus disease [7]. Care should be taken to differentiate plus disease from pre-plus disease in which the posterior vessel abnormalities are insufficient to warrant the diagnosis of plus disease [6].
Besides the standard zone-stage-plus disease combinations, subgroups of ROP have been defined in various clinical trials [6, 8, 9]. As shown in Table 29.2, these include classic threshold ROP and prethreshold ROP (types 1 and 2). In addition, aggressive posterior ROP (AP-ROP) describes a severe, rapidly progressing form of ROP that occurs mostly in zone I but may also appear in posterior zone II. It is characterized by a severity of plus disease out of proportion to the observed peripheral retinopathy. The typical progression from stage 1 to 3 ROP does not occur. Instead, a “deceptively featureless” flat neovascularization may occur at the junction of vascularized and nonvascularized retina, where a circumferential vessel often appears. If not treated promptly, AP-ROP usually progresses to a total retinal detachment [6].
ROP examination pearls are detailed in Appendix J.
Screening for ROP
The details of the currently recommended screening guidelines for ROP in the USA are provided in Appendix K [10]. Premature infants ≤1500 g birth weight (BW) or ≤30 weeks of estimated gestational age (EGA) are identified for screening. The recommended timing of initial screening for ROP and the subsequent intervals of screening are also described in Appendix K. Recent studies suggest, however, that postnatal weight gain, which is associated with postnatal IGF-1 levels, is an important predictor of infants developing severe ROP [2–4]. Different screening algorithms based on postnatal weight gain have been developed in an attempt to reduce the percentage of infants screened while maintaining efficacy. The Weight, Insulin-like growth factor I, Neonatal ROP algorithm (WINROP®) , developed in Sweden and Boston, has a sensitivity of 98.6 % in detecting type 1 prethreshold ROP when assessed in a multicenter cohort of premature infants [11]. The Children’s Hospital of Philadelphia (CHOP) ROP algorithm [12] is being evaluated in the postnatal growth in ROP studies (G-ROP) to determine if a sensitivity >99 % can be achieved for the detection of type 1 prethreshold ROP and whether the approach is cost effective. Remote screening for ROP using wide-angle digital fundus photography, i.e., telemedicine, has a high degree of accuracy and already complements standard ROP examinations in many institutions [13]. The multicenter Telemedicine Approaches to Evaluating Acute Phase ROP study (e-ROP) will provide important data regarding the validity, reliability, feasibility, and cost-effectiveness of digital retinal imaging by comparing it with diagnostic examinations by ophthalmologists performed on the same eyes.
Major Clinical Trials
The CRYO-ROP Study
The Multicenter Trial of Cryotherapy for Retinopathy of Prematurity (CRYO-ROP, 1986–1987) evaluated cryotherapy of the peripheral avascular retina for the treatment of classic threshold ROP as defined in Table 29.2 [8]. Cryotherapy, performed within 72 h of diagnosis, resulted in a 39.5 % reduction in the incidence of unfavorable retinal structural outcome at 3 months as compared with observation. During the 15 years of follow-up of the CRYO-ROP study, the beneficial effects of cryotherapy in reducing the proportion of eyes with unfavorable structural and visual outcome, as compared with observation, have remained consistent [14]. Subsequently, in the 1990s, cryotherapy was gradually replaced by laser therapy, which seemed to yield better structural and functional outcomes [15]. Ablation of the avascular retina has been found to reduce the expression of retinal VEGF mRNA, which has a critical role in the abnormal proliferative process in ROP [16].
The ETROP Study
The CRYO-ROP study showed that eyes with threshold disease in zone I had a particularly high rate of progressing to an unfavorable retinal structural outcome despite treatment (78 % for cryotherapy versus 94 % for observation) [8]. This led investigators to consider whether treatment at a lower severity of disease, namely prethreshold ROP (Table 29.2), prior to the onset of threshold ROP would improve outcome. In the Early Treatment for ROP (ETROP) randomized trial, a multiple logistic regression formula was used to categorize the prethreshold ROP eyes of infants enrolled in the ETROP study as either high or low risk [9, 17]. The formula, also known as risk models for ROP version 2 (RM-ROP2) , was developed using information regarding untreated prethreshold ROP eyes from the CRYO-ROP study that developed an unfavorable retinal structural outcome at 3 months. It was comprised of prognostic variables that included “baby” characteristics, such as birth weight, gestational age, race, location of birth, and multiple birth status, as well as eye characteristics, such as the age at which the initial detection of ROP occurred or the interval of time between the onset of ROP and prethreshold ROP. Using this formula, high-risk prethreshold ROP eyes in ETROP were randomized to early treatment within 48 h of diagnosis or to conventional management in which treatment occurred only if the eyes progressed to classic threshold ROP [9]. By contrast, low-risk prethreshold ROP eyes were reexamined and reassessed for risk at the appropriate intervals and triaged accordingly. At 9 months after treatment, early treatment had reduced the proportion of eyes with unfavorable retinal structural outcome and with unfavorable visual acuity from 15.6 % to 9.1 % and from 19.5 % to 14.5 %, respectively, as compared with conventional management [9].
While the results for the early treatment of high-risk prethreshold ROP eyes were compelling, the ETROP investigators also performed a post hoc analysis in which they evaluated the eye outcome of early treatment versus conventional management for various zone-stage-plus disease combinations of high-risk prethreshold ROP. Based on these results, they recommended the early treatment of those zone-stage-plus disease combinations defined as type 1 prethreshold ROP and conventional management of those combinations defined as type 2 prethreshold ROP (Table 29.2) [9]. It should be emphasized that the ETROP was not designed to evaluate the benefits of early treatment versus conventional management of type 1 or type 2 prethreshold ROP but rather of high-risk prethreshold ROP as calculated by RM-ROP2. Even though the early treatment of type 1 prethreshold ROP may have become the de facto standard of care, there has been controversy with some clinicians advocating early treatment for only zone I type 1 prethreshold ROP [18–21]. To their credit, the ETROP authors acknowledged that the type 1 versus type 2 prethreshold ROP distinction was in part for the benefit of those clinicians who did not wish to use the RM-ROP2 formula to determine if a prethreshold ROP eye was at high risk. Moreover, rather than mandating treatment at the onset of type 1 prethreshold ROP, they saw the development of type 1 prethreshold ROP as opening a time window of opportunity until the onset of threshold ROP, during which early treatment should be seriously considered [21].
The BEAT-ROP Study
The mouse model for the pathogenesis of ROP had suggested that the injection of anti-VEGF antibodies into the vitreous could be used to reverse the manifestations of oxygen-induced retinopathy [22]. The Bevacizumab Eliminates the Angiogenic Threat of ROP (BEAT-ROP) randomized trial compared the intravitreal injection of 0.625 mg bevacizumab (IVB) with laser treatment for type 1 prethreshold ROP [23]. With respect to the proportion of eyes that developed a recurrence of neovascularization by 54-week PMA, IVB was superior to laser for the treatment of type 1 prethreshold ROP in zone I (6 % vs. 42 %, p = 0.003) but not different from laser for the treatment of type 1 prethreshold ROP in zone II (5 % vs. 12 %, p = 0.27). In addition, IVB-treated eyes showed progressive vascularization of the immature retina beyond the original vascular-avascular junction at the time of therapy, an area that would otherwise have been destroyed by laser photocoagulation. Since recurrence of neovascularization generally occurred later in eyes receiving IVB as compared with laser treatment (16.0 ± 4.6 vs. 6.2 ± 5.7 weeks), infants treated with IVB should be monitored for a longer period of time than those receiving laser therapy. However, there is currently no consensus on the intervals and duration of posttreatment follow-up examinations or on the use of laser as an adjunctive treatment in eyes previously treated with IVB, which have had regression of neovascularization, but nevertheless still possess persistent avascular areas in the peripheral retina.
With respect to safety, BEAT-ROP was not sufficiently powered to evaluate the risk of mortality [23]. Thus, it was not possible to determine if the number of infant deaths in the group receiving IVB was significantly higher than the group receiving laser therapy (5 vs. 2). However, in animal and human studies, bevacizumab appears to escape from the eye as indicated by either an elevation in the serum concentration of bevacizumab or a reduction in the level of VEGF in the peripheral circulation after IVB [24, 25]. These findings are concerning as VEGF is important in the development of the brain, lungs, kidney, and bones. Since the current dose of IVB is theoretically capable of neutralizing all VEGF in the vitreous in excess of 5000-fold [24], it may be possible to reduce the dose of IVB without loss efficacy for the treatment of type 1 prethreshold ROP while lowering the infant’s systemic exposure to the drug. A forthcoming Phase 1 trial by the Pediatric Eye Disease Investigator Group is designed to answer this question.
Abbreviations
- AP-ROP:
-
Aggressive posterior ROP
- BEAT-ROP:
-
Bevacizumab eliminates the angiogenic threat of ROP randomized trial
- BW:
-
Birth weight
- CHOP:
-
Children’s Hospital of Philadelphia
- CRYO-ROP:
-
Multicenter trial of cryotherapy for ROP
- EGA:
-
Estimated gestational age
- e-ROP:
-
Telemedicine approaches to evaluating acute-phase ROP study
- ETROP:
-
Early treatment for ROP randomized trial
- G-ROP:
-
Postnatal growth in ROP studies
- ICROP:
-
International classification of ROP
- IGF-1:
-
Insulin-like growth factor 1
- IVB:
-
Intravitreal injection of bevacizumab
- PMA:
-
Postmenstrual age
- RM-ROP2:
-
Risk models for ROP version 2
- ROP:
-
Retinopathy of prematurity
- VEGF:
-
Vascular endothelial growth factor
- WINROP® :
-
Weight insulin-like growth factor I, neonatal ROP algorithm
References
Michaelson IC. The mode of development of the vascular system of the retina, with some observations on its significance for certain retinal diseases. Trans Ophthalmol Soc UK. 1948;68:137–80.
Smith LEH. Through the eyes of a child: understanding retinopathy of prematurity. The Friedenwald Lecture. Invest Ophthalmol Vis Sci. 2008;49:5177–82.
Hellstrom A, Perruzzi C, Ju M, Enstrom E, Hard AL, Liu JL, et al. Low IGF-1 suppresses VEGF-survival signaling in retinal endothelial cells: direct correlation with clinical retinopathy of prematurity. PNAS. 2001;98:5804–8.
Lofqvist C, Andersson E, Sigurdsson J, Enstrom E, Hard AL, Niklasson A, et al. Longitudinal postnatal weight and insulin-like growth factor I measurements in the prediction of retinopathy of prematurity. Arch Ophthalmol. 2006;124:1711–8.
The Committee for the Classification of Retinopathy of Prematurity. An international classification of retinopathy of prematurity. Arch Ophthalmol. 1984;102:1130–4.
International Committee for the Classification of Retinopathy of Prematurity. The international classification of retinopathy of prematurity revisited. Arch Ophthalmol. 2005;123:991–9.
Chiang MF, Gelman R, Jiang L, Martinez-Perez ME, Du YE, Flynn JT. Plus disease in retinopathy of prematurity: an analysis of diagnostic performance. Trans Am Ophthalmol Soc. 2007;105:73–84. discussion 84–5.
Cryotherapy for Retinopathy of Prematurity Cooperative Group. Multicenter trial of cryotherapy for retinopathy of prematurity: three-month outcome. Arch Ophthalmol. 1990;108:195–204.
Early Treatment for Retinopathy of Prematurity Cooperative Group. Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol. 2003;121:1684–96.
Section on Ophthalmology, American Academy of Pediatrics, American Academy of Ophthalmology, and American Association for Pediatric Ophthalmology and Strabismus, and American Association of Certified Orthoptists. Screening examinations of premature infants for retinopathy of prematurity. Pediatrics. 2013;131:189–95.
Wu C, Lofqvist C, Smith LEH, Vanderveen DK, Hellstrom A, for the WINROP Consortium. Importance of early postnatal weight gain for normal retinal angiogenesis in very preterm infants: a multicenter study analyzing weight velocity deviations for the prediction of retinopathy of prematurity. Arch Ophthalmol. 2012;130:992–9.
Binebaum G, Ying GS, Quinn GE, Huang J, Dreiseiti S, Antiqua J, et al. The CHOP postnatal weight gain, birth weight, and gestational age retinopathy of prematurity risk model. Arch Ophthalmol. 2012;130:1560–5.
Chiang MF, Melia M, Buffenn AN, Lambert SR, Recchia FM, Simpson JL, et al. Detection of clinically significant retinopathy of prematurity using wide-angle digital retinal photography: a report by the American Academy of Ophthalmology. Ophthalmology. 2012;119:1272–80.
Cryotherapy for Retinopathy of Prematurity Cooperative Group. 15-year outcomes following threshold retinopathy of prematurity: final results from the multicenter trial of cryotherapy for retinopathy of prematurity. Arch Ophthalmol. 2005;123:311–8.
Simpson JL, Melia M, Yang MB, Buffenn AN, Chiang MF, Lambert SR. Current role of cryotherapy in retinopathy of prematurity: a report by the American Academy of Ophthalmology. Ophthalmology. 2012;119:873–7.
Young TL, Anthony DC, Pierce E, Foley E, Smith LEH. Histopathology and vascular endothelial growth factor in untreated and diode laser-treated retinopathy of prematurity. J AAPOS. 1997;1:105–10.
Hardy RJ, Palmer EA, Dobson V, Summers CG, Phelps DL, Quinn GE, et al for the Cryotherapy for Retinopathy of Prematurity Cooperative Group. Risk analysis of prethreshold retinopathy of prematurity. Arch Ophthalmolol. 2003;121:1697–701.
Averbukh E. The evidence supporting the early treatment for type 1 retinopathy of prematurity needs further evaluation. Arch Ophthalmol. 2005;123:406.
Coats D, Saunders R. The dilemma of exercising clinical judgment in the treatment of retinopathy of prematurity. Arch Ophthalmol. 2005;123:408–9.
Vander JF, MacNamara JA, Tasman W, Brown GC. Revised indications for early treatment of retinopathy of prematurity. Arch Ophthalmol. 2005;123:406–7.
Good WV, Hardy RJ. Reply to letters concerning ETROP. Arch Ophthalmol. 2005;123:409–10.
Aiello LP, Pierce EA, Foley ED, Takagi H, Chen H, Riddle L, et al. Suppression of retinal neovascularization in vivo by inhibition of vascular endothelial growth factor (VEGF) using soluble VEGF-receptor chimeric proteins. PNAS. 1995;92:10457–61.
Mintz-Hittner HA, Kennedy KA, Chuang AZ for the BEAT-ROP Cooperative Group. Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. NEJM. 2011;364:603–15.
Hard AL, Hellstrom A. On safety, pharmacokinetics and dosage of bevacizumab in ROP treatment–a review. Acta Paediatr. 2011;100:1523–7.
Sato T, Wada K, Arahori H, Kuno N, Imoto K, Iwahashi-Shima C, et al. Serum concentrations of bevacizumab (avastin) and vascular endothelial growth factor in infants with retinopathy of prematurity. Am J Ophthalmol. 2012;153:327–33.
Zepeda-Romero LC, Martinez-Perez ME, Ruiz-Velasco S, Ramirez-Ortiz MA, Gutierrez-Padilla JA. Temporary morphological changes in plus disease induced during contact digital imaging. Eye. 2013;27:589–96.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Yang, M.B. (2016). Retinopathy of Prematurity. In: Traboulsi, E., Utz, V. (eds) Practical Management of Pediatric Ocular Disorders and Strabismus. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-2745-6_29
Download citation
DOI: https://doi.org/10.1007/978-1-4939-2745-6_29
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-2744-9
Online ISBN: 978-1-4939-2745-6
eBook Packages: MedicineMedicine (R0)