Abstract
Given the increasing detection rate of renal mass with the widespread utilization of cross-sectional imaging and the rising incidence rate of renal cell carcinoma (RCC), it is imperative that the nephrologist understands the behavior of this cancer, the treatment options available, and the impact of treatment on renal functional outcomes. Here, we present a review of various histologic subtypes of RCC, up-to-date surgical and medical treatment options, and their respective outcomes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
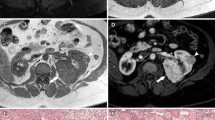
FormalPara Case #1AA is a 47-year-old male presented to the emergency department with a 1-day history of gross hematuria. Upon presentation, his vital signs were stable and the remainder of his exam was unremarkable. In the emergency department, a complete blood count revealed normal hematocrit and serum creatinine of 1.04 mg/dL. He underwent an MRI of the abdomen with and without IV contrast. Imaging revealed an 8 cm heterogeneous mass in the mid pole of the right kidney with mixed signal intensity but definite areas of enhancement (Fig. 9.1). Metastatic workup revealed no evidence of distant metastasis. His past medical history was significant for hypertension, hyperlipidemia, and non-insulin dependent diabetes mellitus (currently on metformin). Given his medical comorbidities and risk of future renal insufficiency, nephron-sparing surgery was recommended. He underwent a robotic-assisted laparoscopic partial nephrectomy. The surgery was uncomplicated, and the warm ischemia time during resection (minutes that the clamp was occluding arterial inflow) was 23 min. Upon resection, pathology revealed a clear cell renal cell carcinoma (RCC), Fuhrman grade 3, confined to the kidney (T2aNxMx). Postoperatively, creatinine at 4 weeks after surgery remained stable at 1.05 mg/dL.
Which are the known risk factors for development of RCC?
-
a.
Smoking
-
b.
ESKD
-
c.
Hypertension
-
d.
Obesity
-
e.
All of the above
Basic Epidemiology and Risk Factors of Kidney Cancer
Kidney cancer or RCC is the eighth most common cancer in men and the tenth leading cause of cancer-related death in men in the USA [1]. It accounts for 2–3 % of all adult malignancies. Of the estimated 1,660,290 new cancer cases in the USA in 2013, kidney and renal pelvis cancer combined will account for 40,430 (5 %) and 24,720 (3 %) new cancer cases in males and females, respectively. Similarly, of the anticipated 580,350 cancer deaths in 2013, kidney and renal pelvis cancer will account for 8780 (3 %) and 4900 (2 %) deaths in males and females, respectively [2].
Tobacco use has been shown to increase the risk of RCC up to twofold when compared with nonsmokers. This association demonstrates a dose–response relationship, with the number of packs per day or longer duration (pack-years) associated with an increased risk [3, 4] Compared with nonsmokers, smokers with RCC have poorer overall survival (6.6 years versus 4.2 years, respectively) [5]. Although increased body mass index has similarly been linked with a higher risk of developing RCC, [6, 7] obese individuals had better disease-free survival (DFS) when compared with those who were non-obese (5-year DFS of 80 % versus 72 %, respectively) [5, 8]. Obesity and hypertension have been shown to be modifiable risk factors among tobacco users [3]. The association of smoking with an increased risk of RCC was found in non-obese individuals (and not those with BMI ≥ 30 Kg/m2) and in those who reported no prior history of hypertension .
Hypertension is associated with RCC in two distinct ways: as a risk factor predisposing to the development of RCC; and as a paraneoplastic syndrome associated with RCC. Patients with hypertension have up to a twofold increase in risk of developing RCC as compared to their age-matched controls [9, 10]. This risk is hypothesized to result from chronic inflammation or hypertension-induced renal injury, especially to the renal tubules, rather than from the use of antihypertensive medications [10, 11]. Hypertension may also develop in patients with RCC in the setting of a tumor involving the juxtaglomerular apparatus cells resulting in abnormally increased renin production. The activation of the renin–angiotensin–aldosterone pathway leads to increased aldosterone and angiotensin synthesis with subsequent fluid retention and vasoconstriction. The downstream effect is an elevated blood pressure.
End-stage kidney disease (ESKD) has been identified as a risk factor for RCC, with up to a 100 % increase in incidence when compared with the general population. Although this increased risk was observed in both transplanted and dialysis-only patients, RCC was found to have more favorable clinical and pathological outcome features in individuals who have undergone renal transplantation [12, 13]. The difference in clinical outcomes in these settings, however, may be related in part to early detection bias. The patient with a transplanted kidney, followed by the urologist or the transplant surgeon or nephrologist, is more likely to have a tumor detected earlier than a dialysis-only patient, given the enhanced attention to the patients’ native kidneys between the surgeon and the nephrologist. Hemodialysis for more than 10 years is associated with poorer outcomes and adverse histopathological features, e.g., acquired cystic disease-associated RCC and sarcomatoid differentiation. Hence, patients on long-term hemodialysis should have annual screening of their native kidneys after more than 10 years of dialysis [14, 15].
A high-fat or high-protein diet, occupational exposures to lead, aromatic hydrocarbons, rubber, asbestos, and radiation are also presumed to be associated with an increased risk of development of RCC but the available data are inconclusive [6, 11].
Case #1 Follow-Up and Discussion
As stated above, ESKD, smoking, and obesity have been linked with the development of RCC. In addition, hypertension can be seen as a risk factor and a paraneoplastic syndrome associated with RCC. Hence, the correct answer is e.
Histological Subtypes and Genetic Changes Associated with RCC
RCC occurs sporadically in the majority of patients, accounting for more than 95 % of the cases, with only about 2–3 % of the cases resulting from hereditary predisposition [11]. Genetic alterations or abnormalities predisposing to inherited forms of RCC have been described, with tumors often occurring in multiple sites in the same or in both kidneys at the same time (synchronous) or at different times (metachronous). The efforts of Linehan et al. at the US National Cancer Institute have led to the discovery and understanding of the close molecular link between histopathology, i.e., clear cell, papillary type 1, papillary type 2, chromophobe, and oncocytoma, and specific genetic abnormalities (Fig. 9.2).
Histologic types of renal cell carcinoma (RCC) and associated genetic alteration in hereditary RCC. (From Linehan et al. [16])
Clear Cell RCC
Clear cell RCC is the most common and well-studied histological variant of RCC, accounting for about 75 % of all the cases of RCC . Clear cell RCC may be sporadic or may occur in inherited forms in association with von Hippel–Lindau (VHL) syndrome, in which individuals are also at risk of developing tumors in the cerebellum, spine, retina, inner ear, pancreas, adrenal glands, and the epididymis [17]. In patients with VHL syndrome, tumors in the kidney may increase to 600 [18], hence nephron sparing surgery is generally preferred. Given that the risk of metastasis is very low in small tumors, surgical exploration and resection are recommended once the lesions have reached the size of ≥ 3 cm. Although it was discovered in the setting of hereditary clear cell RCC, the VHL gene is an early driver of sporadic RCC as well. The loss of VHL function by mutation or promoter DNA methylation can be identified in most cases of sporadic clear cell RCC [17, 19, 20].
The VHL gene is a tumor suppressor gene located on the short arm of chromosome 3 (3p). The downstream effect of either VHL mutation or methylation is the accumulation of hypoxia inducible factor (HIF) and the subsequent increased downstream transcription of vascular endothelial growth factor (VEGF), platelet-derived growth factor (PDGF), and transforming growth factor-α (TGF-α) [21]. This ultimately leads to the increased angiogenesis and tumor cell proliferation. This mechanism or pathway is targeted by the newer systemic therapies for kidney cancer as discussed later in this chapter (Fig. 9.3) .
The VHL gene complex—hypoxia-inducible factors (HIF) molecular pathway in pathogenesis of RCC and sites of therapeutic targets. (From Rosner et al. [22])
Papillary Type 1 RCC
Papillary type 1 RCC accounts for approximately 5 % of all kidney cancers . The genetic abnormality associated with this histologic variant of RCC is activation of c-MET, an oncogene located on chromosome 7. Papillary renal tumors often demonstrate gains of chromosomes 3, 7, and 17, resulting in the increased activity of c-MET. Individuals with hereditary papillary RCC (very rare) tend to develop multiple, and often bilateral, multifocal tumors. With the goal of renal preservation and excellent oncological outcome, these tumors are managed surgically by partial nephrectomy [21−24].
Papillary Type 2 RCC
Papillary type 2 RCC is an aggressive form of kidney cancer accounting for about 10 % of all RCCs . It can be found in both sporadic cases as well as in the context of hereditary leiomyomatosis RCC (HLRCC) syndrome. Along with kidney cancer, HLRCC is characterized by the associated findings of cutaneous leiomyomas and uterine fibroids. The syndrome results from an inactivating mutation in fumarate hydratase, a Krebs cycle enzyme. Given the aggressive nature of this variant of RCC, total/radical nephrectomy is generally recommended [21, 22, 25].
Chromophobe RCC and Oncocytoma
Chromophobe RCC and oncocytoma , each accounting about 5 % of RCC, are associated with Birt–Hogg–Dube (BHD) syndrome, either as a single entity or in combination (hybrid forms). In addition to developing renal tumors, which are often multifocal and bilateral, individuals with BHD syndrome are prone to developing fibrofolliculomas and pulmonary cysts. The genetic defect in BHD syndrome is a loss of function of the BHD gene on chromosome 17 (17p11.2), which functions as a tumor suppressor gene [21, 26]. Chromophobe RCC has been shown to have equivalent or even better cancer-specific survival outcomes when compared with clear cell or papillary RCC [27, 28].
Diagnosis and Staging
The majority of cases of RCC are now found incidentally during abdominal imaging for unrelated reasons . However, patients with renal tumors may present with flank/abdominal pain, hematuria, or symptoms of metastasis and/or a paraneoplastic syndrome. The gold standard diagnostic imaging technique is a computerized tomogram (CT) scan of the abdomen without and with intravenous (IV) contrast to determine enhancement characteristics of the mass. In patients who have an allergy to iodinated contrast or have renal insufficiency, magnetic resonance imaging (MRI) without and with gadolinium is recommended. In patients with chronic kidney disease (CKD) stage 4 (estimated glomerular filtration rate (eGFR) ≤ 30 mL/min), gadolinium contrast is contraindicated. If an MRI with contrast is absolutely necessary for a proper evaluation, a nephrology consultation should be sought, and two sessions of dialysis separated by 2 days apart should be planned [29, 30]. Alternatively, in these patients, diffusion-weighted MRI (without gadolinium contrast) can be used to differentiate complex cystic and solid masses from benign lesions in the kidney [31].
Basic laboratory studies should be obtained including a complete blood count, comprehensive metabolic panel, urinalysis, and a chest radiograph . In individuals with an elevated corrected calcium level or alkaline phosphatase level, a nuclear medicine bone scan should be performed to evaluate for bone metastasis. With the presence of neurological symptoms or headaches, a CT or preferably an MRI of the brain should be obtained to evaluate the presence of central nervous system metastases. Other laboratory evaluations or imaging studies may be obtained as clinically indicated [32].
The TNM classification of RCC according to the AJCC 2010 staging is shown in Table 9.1.
Surgical excision of tumor or removal of the entire kidney, depending on the size and other criteria is a diagnostic approach of choice for kidney cancer . In certain clinical scenarios, such as a high-risk surgical candidate, the existence of a solitary kidney, the suspicion of secondary metastasis to the kidney, or patients considered for active surveillance or observation of their kidney tumor (in the case of small tumors), image-guided biopsy of the kidney tumor should be considered. With current CT, MRI, and biopsy techniques available, renal biopsy can accurately predict the histology of renal masses , thus helping to stratify patients into risk categories and determine those that may qualify for active surveillance . Halverson et al. [33] evaluated the utility of a kidney biopsy in stratifying patients into various risk groups by analyzing 151 patients with small renal masses who underwent kidney biopsy prior to extirpative surgery. They reported an agreement between kidney biopsy and final pathology in 97 % of the cases, with a negative predictive value of 0.86 and a positive predictive value of 1.0 [33]. Furthermore, a review of the published evidence regarding the use of kidney biopsies reported in the American Urological Association (AUA) guidelines revealed a sensitivity and specificity of up to 99.5 and 99.9 % respectively [34].
Active Surveillance (AS) for Renal Masses
Although the preferred choice of treatment for operable renal tumors is surgical extirpation, a clinical decision may be made to actively observe a renal mass (usually in the case of small renal masses) , especially in the elderly patient with multiple comorbidities rendering them as high-risk for general anesthesia. Mason et al. [35] actively followed 84 patients with renal masses ranging from 0.8 to 5.4 cm at diagnosis for a median duration of 36 months (range: 6–96 months). They reported that only one patient (1.2 %) developed metastases during follow-up. The mean growth rate of renal masses was reported to be 0.25 cm/year, with tumors ≥ 2.45 cm in its largest diameter at the time of diagnosis exhibiting a faster growth rate during follow-up [35]. Hence, in a carefully selected group of patients, AS may be a valuable option and kidney biopsy may be an adjunct in the management, as mentioned above [33, 34].
Surgical Management of Renal Masses
The mainstay of treatment of clinically localized RCC is excision based on the recommendations of the National Comprehensive Cancer Network (NCCN) [32], with the option of radical or nephron-sparing surgery (NSS), the latter commonly referred to as partial nephrectomy.
Radical Nephrectomy
The NCCN guidelines recommend radical nephrectomy (RN; surgical removal of the entire kidney and Gerota’s fascia +/− removal of the ipsilateral adrenal gland) in patients with kidney tumor measuring > 10 cm in its largest diameter or in patients with multiple kidney tumors in the same kidney but without genetic predispositions as described above . This treatment option is based on evidence that suggests a high risk of recurrence following surgery. However, as described below, the evidence is inconclusive as to the superiority of radical nephrectomy over partial nephrectomy in terms of renal functional or oncological outcomes [36−38].
Partial Nephrectomy
Partial nephrectomy (PN) (also termed nephron sparing surgery (NSS)) is the goldstandard for the treatment of patients with small renal masses (SRMs) (≤ 4 cm or T1a), although it is increasingly utilized for T1b tumors (4–7 cm, confined to the kidneys) [32]. This can be done via a traditional open incision, a laparoscopic approach with or without the assistance of a robotic system, and has been shown to be safely performed, even in old patients [39]. Variations in technique that include clamping the hilar vessels during tumor extirpation (goal clamp time ≤ 30 min), selective clamping of renal vessels (zero ischemia) [40, 41], and without clamping of hilar vessels (off-clamp) [42] even for complex or hilar [43] renal tumors have been described. Reducing or eliminating warm ischemia (time in which a tissue or an organ remains at body temperature after its blood supply has been cut off before it is perfused or cooled) is thought to reduce damage to nephrons from ischemia and the release of damage-inducing free radicals.
The goal of a partial nephrectomy is to spare residual normal nephrons, thus preserving renal function, particularly in patients who at the time of diagnosis have some form of CKD. However, studies evaluating renal functional outcomes following partial nephrectomy have reported conflicting results. van Poppel et al. [37], in a randomized trial comparing partial versus radical nephrectomy for low-stage renal tumors, reported a 10-year overall survival rates of 81.1 % for radical nephrectomy and 75.7 % for nephron-sparing surgery (superiority p-value = 0.03). On the other hand, Tan et al. [38], in a retrospective analysis of Medicare beneficiaries with T1a tumors, reported a significantly improved overall survival with partial nephrectomy when compared with radical nephrectomy, albeit with the caveat of unknown confounders regarding other risk factors .
With respect to renal functional outcomes, the European Organization for Research and Treatment of Cancer (EORTC) conducted a randomized trial by comparing nephron-sparing surgery versus radical nephrectomy. After a median follow-up of 6.7 years, Scosyrev et al. [44] reported a significant reduction in the incidence of moderate renal dysfunction (eGFR < 60 mL/min; 64.7 % for NSS versus 85.7 % for RN, respectively). Although not statistically significant, NSS was associated with a reduced incidence of advanced kidney disease (eGFR < 30 mL/min; 6.3 % and 10.0 %, respectively). However, the incidence of kidney failure (eGFR < 15 mL/min) was essentially identical between NSS and RN (1.6 % versus 1.5 %, respectively), and the impact of NSS on renal functional outcomes did not translate into an improved overall survival in this trial [44].
On the other hand, a study of a community-based population evaluating the impact of medical renal disease, demonstrated the risk of death to increase as GFR decreases below 60 mL/min, with hazard ratios ranging from 1.2 (with an eGFR of 45–59 mL/min) to 5.9 (with an eGFR of < 15 mL/min per 1.7 m2 of body-surface area). An inverse relationship was also observed between eGFR and the risk of cardiovascular events and hospitalization [45]. While NSS has not been shown to improve the overall survival outcome, this study indicates the importance of prevention of chronic renal insufficiency and the need to perform nephron-sparing surgery for renal masses when possible without compromising on oncologic outcomes .
Percutaneous Ablation
Although extirpative surgery is the mainstay of treatment of kidney tumors, percutaneous ablation is a safe and effective option and can be successfully employed in patients with multiple comorbidities who are not surgical candidates . Two modalities that have been popularized are cryoablation and radiofrequency ablation (RFA). Cryoablation involves the delivery of freezing temperatures (up to—50 °C) via probes (in a freeze-thaw cycles) to cause tissue destruction by an immediate direct cellular damaging effect and by a delayed vascular mechanism, with hypoxia-ischemia resulting from microvascular stasis during cooling [46, 47]. Alternatively, RFA involves the use of high-frequency alternating current, causing frictional heating from electrons flowing near the site of energy delivery. At temperatures 49 °C and above, cell death results from enzyme inactivation, denaturation of proteins, and irreparable damage to cellular membranes [48, 49].
In a meta-analysis comparing cryoablation and RFA, El Dib et al. [50] reported a clinical efficacy of 89 % and 90 %, respectively, for these two modalities in the management of patients with small renal masses ( ≤ 4 cm). This analysis showed no statistically significant difference in complication rates between cryoablation and RFA. While these ablation techniques may be a reasonable approach, they are limited by the paucity of long-term follow-up data and difficulty in evaluating patients for either recurrence or the presence of residual tumor following treatment [50].
Cytoreductive Nephrectomy
Unlike some other solid organ tumors, surgical removal of the kidney in the setting of metastatic kidney cancer (cytoreductive nephrectomy) has been shown to be associated with an improved overall survival . Motzer et al. [51] identified the absence of a prior nephrectomy as one of the five prognostic factors predicting shorter overall survival in patients with advanced RCC. Cytoreductive nephrectomy was evaluated in two prospective randomized controlled trials, both demonstrating an increase in overall survival favoring surgical intervention along with interferon versus interferon alone [52, 53]. The combined analysis of these two trials demonstrated a median survival of 13.6 months for the cytoreductive nephrectomy plus interferon cohort as compared with 7.8 months for interferon alone, corresponding to a 31 % decrease in the risk of death (p = 0.002) [54].
Several mechanisms have been proposed to explain the observed survival improvement following cytoreductive nephrectomy. Although all theoretical, the proposed mechanisms include reduced tumor burden, reversal of the associated immunosuppressive milieu within the primary tumor, and reduction in the amount of circulating angiogenic factors, such as VEGF [55].
Case #2
AA had surgery. Six months following surgery, he underwent surveillance imaging including CT scan of the chest, abdomen, and pelvis (Fig. 9.4). The imaging revealed no evidence of local recurrence within the kidney, but did reveal several enhancing retroperitoneal lymph nodes in the paracaval and interaortocaval regions. The lymph nodes were worrisome for metastatic recurrence. At the current time, he is weighing his options of surgical resection versus immunotherapy with high-dose interleukin 2 versus molecular-targeted therapy with sunitinib maleate.
What major side effect of Interleukin 2 leads to significant hypotension and acute kidney injury?
-
a.
Thrombotic microangiopathy
-
b.
Capillary Leak Syndrome
-
c.
Minimal Change Disease
-
d.
None of the above
-
e.
All of the above
Medical Treatment of Metastatic Renal Carcinoma
The natural history of RCC is quite variable and may be marked by prolonged stability of metastatic disease in some instances . Late relapses after nephrectomy, some decades later, may occur. In addition, there are reports of spontaneous regression of metastases after cytoreductive nephrectomy [56]. Treatments from the remote past have included hormonal agents and multiple small trials of various chemotherapy drugs. Medroxyprogesterone (MPA) was first utilized many years ago; it was associated with a small percentage of responses and, given the lack of response with cytotoxic chemotherapy, was prescribed in the metastatic setting. Since then, as described below, there have been several advances in immunotherapeutic and molecular-targeted therapeutic agents in metastatic kidney cancer .
Prognostic Stratification
Prognostic factors have become important stratification variables in clinical trials of agents for the treatment of metastatic RCC . The behavior of metastatic RCC is quite variable and some patients with low-disease burden and favorable prognostic features after nephrectomy may be followed for evidence of progression prior to the initiation of treatment [57]. There are a few patients that may not require treatment at all in the setting of asymptomatic indolent disease in the face of competing comorbidities. Others may have rapid progression of disease. With this disease heterogeneity in mind, a review of patients treated on prior chemotherapy and immunotherapy clinical trials at Memorial Sloan-Kettering Cancer Center (MSKCC) identified five prognostic factors that could be used to stratify patients into one of three prognostic groups. The five factors identified are: a Karnofsky performance status (KPS) of less than 80 %, low hemoglobin value (less than lower limit of normal), high corrected calcium level ( > 10 mg/dL), high LDH level ( > 1.5 times the upper limit of normal), and less than 1 year from the time of nephrectomy to metastases. The presence of three or more risk factors results in the shortest overall survival and comprises the poor-risk group. Patients with one or two factors are considered intermediate-risk and the absence of any of these factors, the favorable-risk group. In the initial study, the 3-year survival rate among patients treated with cytokines was 31, 7, and 0 % for the favorable-risk, intermediate-risk, and poor-risk groups, respectively [51].
Given that the MSKCC schema was developed in the cytokine era, additional risk-stratification systems have been proposed more recently. Prior radiotherapy and the number of metastatic sites were added to the MSKCC scoring system in a model from the Cleveland Clinic [58]. Heng et al. proposed a new model for patients treated in the current era of targeted therapy from a cohort of consecutive patients that were treatment naive and had received sunitinib, sorafenib, or bevacizumab on clinical trial. Using overall survival as the endpoint, 16 potential predictive covariates were assessed in univariate and multivariate analyses. In the final analysis, four of the five predictive factors from the original MSKCC criteria remained significant. Additionally, an elevated absolute neutrophil count and an elevated platelet count (both above the upper limit of normal) were predictive of worse outcome. The authors reported 2-year overall survival probability of 75, 53, and 7 % for the favorable-risk, intermediate-risk, and poor-risk groups, respectively [59].
Progression-free survival (PFS) is the most utilized trial endpoint as the use of multiple agents in succession as well as crossover in many trials have made the assessment of overall survival (OS) problematic [60]. A large retrospective analysis from consecutive patients treated with targeted agents at 12 cancer centers in North America revealed that lack of disease progression at 3 and 6 months intervals independently predicted improved overall survival. The conclusion from the authors was that there is a dependent relationship between PFS and OS in metastatic RCC patients treated with current targeted agents [61]. This has led to the use of the endpoint of PFS as an acceptable determinant of benefit in clinical trials in RCC .
Immunotherapy
Interferon-Alpha
Interferon-alpha was shown to improve overall survival of patients in a randomized controlled trial against medroxyprogesterone acetate, an agent that had been utilized for metastatic RCC based on occasional tumor responses . The primary endpoint of the trial was OS and the interferon group had a superior outcome, with a 2.5-month improvement in survival (median OS 8.5 months versus 6 months for MPA) [62]. Interferon-alpha did not receive regulatory approval for the treatment of metastatic RCC in the USA but became the standard of care for many years. This was evident in the two trials conducted in the USA and Europe that established cytoreductive nephrectomy as the standard of care. Patients deemed eligible for a cytoreductive nephrectomy were randomized to surgery with interferon treatment versus interferon alone. Patients who underwent cytoreductive nephrectomy were found to have a 5.8-month median survival advantage [54]. However, the trial also established that the response to interferon was modest, underscored by a recently published negative trial by the French Immunotherapy Group. In 2005, a Cochrane review by Coppin et al. concluded that interferon-alpha provided modest survival benefit and (in the pre-targeted therapy era) cytoreductive nephrectomy followed by interferon-alpha provided the best outcomes in surgically fit patients [63].
Interleukin-2
Interleukin-2 received regulatory approval in 1992 based on uncontrolled experience demonstrating objective responses, including several complete responses. More importantly, a proportion of those complete responders proved to be durable in long-term follow-up. In a retrospective review of the experience at the US National Institutes of Health (n = 259 patients), perhaps the largest national experience, the overall objective response rate was 20 %, with 23 patients experiencing a complete response (CR) and 30 patients achieving a partial response (PR). Only four of those complete responders remained without evidence of disease at the time of last assessment [64].
Given the potential toxicity, high-dose IL-2 (preferred over low dose IL-2) is administered in limited centers in the USA. The usual dose planned is 720,000 IU/kg administered IV over 15 min every 8 h for a total of 15 doses. Since many patients do not tolerate the total number of doses, the investigators at the NCI proposed to reduce the number of doses to 12 per cycle. Two cycles constitute one course of treatment, with usual plan of administering two courses. Profound hypotension and oliguria are common significant adverse events resulting from capillary leak syndrome and often require an intensive care unit admission during treatment. Additionally, patients can experience confusion and a depressed level of consciousness . Given the high incidence of grades 3–4 toxicity, patient selection is very important in this potentially curative treatment where durable remissions have been noted to occur [62]. The ideal patient is generally younger with an excellent performance status, pulmonary only metastasis, previous nephrectomy, and no significant cardiovascular comorbidities. Given the potential for complete and durable response, high-dose IL2 has become the standard of care immunotherapy for metastatic kidney cancer in well-selected patients.
Tyrosine Kinase Inhibitors (TKIs)
The addiction of clear cell carcinoma to the VEGF pathway led to the development of several agents targeting this pathway for use in metastatic RCC . Four agents are currently approved for use in the USA, and each targets the VEGF receptor. Sorafenib and sunitinib were approved in 2006. Subsequently, pazopanib and axitinib achieved regulatory approval based on benefits demonstrated in randomized Phase 3 trials.
Sorafenib was compared to placebo in patients who previously received cytokine therapy (defined as IL-2 or interferon-alpha), demonstrating a PFS benefit in comparison to placebo of 5.5 months versus 2.8 months, respectively (p < 0.00001, hazard ratio 0.44). Sorafenib blocks the kinase domain of the VEGF receptor (VEGFR)-2, VEGFR-3, platelet derived growth factor receptor (PDGFR)-β, as well as RAF-1, Flt-3, and c-KIT. The original primary end-point of the trial was OS, yet 48 % of the patients on placebo crossed over to receive sorafenib [65]. A post-hoc analysis of the trial, with censoring of those patients that crossed over from placebo to sorafenib, suggested an OS benefit. In the intention-to-treat analysis, OS was 17.8 versus 15.2 months for sorafenib versus placebo, respectively. After censoring the crossover patients, OS was 17.8 versus 14.3 months, (HR 0.78, p = 0.029). This result is suggestive of an improved overall survival, with caveat that higher proportion of good-risk patients crossed over to receive sorafenib. Sorafenib did not have a PFS benefit over interferon-alpha in the first-line treatment of metastatic RCC in a randomized Phase 2 trial [66]. Sorafenib has modest efficacy in the second-line treatment of metastatic RCC after sunitinib or bevacizumab, with an objective response rate of less than 10 % and a median PFS of 4.4 months [66]. Sorafenib has been used as the control arm for trials in the development of subsequent agents .
Sunitinib maleate inhibits multiple receptor tyrosine kinases including PDGFR-α and -β, VEGFR-1, -2 and -3, c-KIT, Fms-like tyrosine kinase-3 (FLT-3), CSF receptor-1 and neurotrophic factor receptor (RET) [67]. The sunitinib registration trial compared this agent in treatment-naive patients to interferon-alpha, revealing a PFS benefit of 11 months versus 5 months, favoring sunitinib. OS improvement was not reported as the median survival had not been reached in the pre-planned early analysis for PFS [68]. There was limited crossover to sunitinib on this trial (7 % of interferon-treated patients received sunitinib). In the intention-to-treat analysis, OS was 26.4 months versus 21.8 months, respectively, for sunitinib compared with the interferon-treated group (p = 0.51). In an exploratory analysis of OS with censoring of those who crossed over, the median OS was 26.4 versus 20 months, respectively, for sunitinib versus interferon (p = 0.036) [69].
Pazopanib targets VEGF-R-1, -2 and -3, PDGFR-α and -β, fibroblast growth factor receptor (FGF-R)-1 and -3 and c-Kit. It was approved in the USA in 2010 based on a randomized controlled trial versus placebo in treatment-naive individuals and cytokine pretreated individuals, revealing a PFS of 9.2 months for the pazopanib arm versus 4.2 months for the placebo-treated individuals. This trial was conducted in countries where other agents were generally not available and thus placebo was utilized as the control arm [70]. The PFS for the treatment-naive population was 11.1 months for pazopanib versus 2.8 months for placebo. Pazopanib-treated patients were noted to have total objective response rate of 30 %, and disease stability in an additional 38 % [70].
In a comparison trial of pazopanib and sunitinib designed as a non-inferiority comparison for treatment-naive patients, median PFS was similar in both arms, at 10.5 months for pazopanib and 10.2 months for sunitinib. The results met the pretrial assessment for non-inferiority. Health-related quality of life parameters were assessed with significant differences favoring pazopanib in 11 of 14 comparisons [71]. Pazopanib and sunitinib are both considered first-line receptor TKI-targeted treatments for treatment-naive patients.
Axitinib is the most recent TKI to receive approval in the USA for the treatment of metastatic RCC. It is a potent and selective second-generation inhibitor of VEGFR-1, -2, and -3 with a relative potency of 50–450-fold greater than first generation VEGFR inhibitors. This agent was compared to sorafenib in second-line treatment after the failure of one TKI. The trial demonstrated improved PFS: 6.7 months for axitinib treated patients versus 4.7 months for sorafenib treated patients (OS, 11.9 versus 9.1 months, respectively) [72]. Axitinib is currently approved as second line or later treatment in patients who have previously received a TKI .
mTOR Inhibitors
Mammalian target of rapamycin (mTOR) signaling is prominent in many tumor types including kidney cancer , and two agents are currently approved in the USA as treatment for metastatic RCC. Temsirolimus is an intravenously administered mTOR inhibitor, given on a weekly basis, and approved for poor-risk metastatic RCC patients. This agent was evaluated among poor-risk metastatic RCC in a threearm trial including temsirolimus monotherapy, interferon-alpha monotherapy, and combination temsirolimus/interferon alpha. Patients enrolled in this trial had to have three or more MSKCC risk criteria, thus comprising a poor-risk group. In addition to the MSKCC criteria, metastasis in multiple organ sites was included as a sixth risk factor. The temsirolimus arm demonstrated an improved overall survival as well as an improved PFS. Of note, temsirolimus is the only targeted therapy with statistically significant OS benefit in a randomized control trial. The PFS for temsirolimus was 5.5 months versus 3.1 months for the interferon group. The OS was 10.9 months for temsirolimus compared to 7.3 months for the interferon alone arm. The combination arm had similar outcomes to the interferon alone arm, albeit with greater toxicity [73]. This trial also permitted the enrollment of patients with non-clear cell histology comprising approximately 20 % of the study population.
Everolimus is an orally available mTOR inhibitor, which was studied in patients that were previously treated with either sunitinib or sorafenib. At the time of the trial, there was no approved second line agent. Therefore, in this trial, the comparator group was administered placebo. The results showed PFS of 4.9 months for everolimus versus 1.9 months for placebo. These findings led to regulatory approval of everolimus as second-line treatment after failure of one TKI treatment [74].
Bevacizumab and Interferon Combination
The AVOREN trial compared bevacizumab plus interferon-alpha versus interferon alone. Bevacizumab is a monoclonal antibody directed against VEGF . The trial demonstrated PFS of 8.2 months versus 5.2 months favoring the treatment arm. All patients had either cytoreductive or previous nephrectomy and the majority of subjects consisted of intermediate-risk individuals. Objective response rates were also higher in the bevacizumab treated patients, 31 % versus 13 % in the interferon only arm. In a similar trial design, Rini et al. also demonstrated a superior PFS with the addition of bevacizumab, at 8.5 months for the combination arm and 5.7 months for the interferon alone arm. Similar to the AVOREN trial, prior nephrectomy occurred in 85 % of the trial population [75]. In the final analysis of this trial, OS favored the bevacizumab arm, but did not meet the predefined criteria for significance. The hazard ratio was 0.86 (95 % confidence interval: 0.73–1.01) [76]. Overall response rates were 25.5 % for the combination arm versus 13 % for the interferon alone arm .
Bevacizumab Monotherapy
As a result of the toxicity associated with interferon-alpha treatment of RCC, many physicians utilize monotherapy with bevacizumab . A randomized trial of bevacizumab (at 2 dose levels) versus placebo in cytokine pretreated patients was conducted and published in 2003. PFS was superior to placebo at the second interim analysis in the higher dose level and the trial was halted for further accrual. The PFS was 4.8 months versus 2.5 months for bevacizumab versus interferon, respectively. The objective response rate was 10 %. Overall survival was not significantly improved [77].
Non-Clear Cell RCC
Management of patients with non-clear cell histology is beyond the scope of this chapter . Collecting duct carcinomas have been shown to possibly benefit from cisplatin-based combination chemotherapy with some responses noted in a prospective Phase 2 trial (objective responses rate 26 %) [78]. Sarcomatoid histology is often seen in high-grade clear cell RCC and is considered an aggressive variant. In a small trial of 18 patients with predominant sarcomatoid histology, two complete responses and four partial responses were noted in patients treated with a combination of gemcitabine and doxorubicin [79]. The relatively small number of cases and the limited clinical trial opportunities have resulted in a void as to the optimal management of these patients in the era of targeted therapy.
In an analysis of the expanded access cohort for sunitinib, the non-clear cell histology group revealed an overall response rate of 11 %. PFS was 7.8 months with an OS of 13.4 months, significantly less than the clear cell patients treated on the Phase 3 trial. The total cohort consisted of greater than 4000 patients with all histologic types, with a PFS of 10.9 months and an OS of 18.4 months [80].
Toxicity Management of Targeted Agents
The targeted agents discussed above and outlined in Table 9.2 require skilled professionals in the management of the significant toxicity associated with these agents . These “off-target” adverse events are capable of producing significant issues in terms of quality of life for individual patients, and patient education is critical in order to maintain safe administration and dose intensity.
Uncontrolled hypertension, decreased cardiac function, hypothyroidism, hand–foot syndrome, and many other adverse events require vigilance and prompt management interventions. Renal abnormalities may also be caused by many of the agents, including proteinuria (occasionally in the nephrotic range), thrombotic microangiopathy, and interstitial nephritis among other described entities. The inability to perform a kidney biopsy limits the interpretation of causation in these individuals as most patients usually have a solitary kidney after excision of their malignancy [81]. Treatment with TKIs for 6 months or greater in an expanded access program revealed a higher cumulative incidence of National Cancer Institute-Common Terminology Criteria for Adverse Events grade 3 or 4 events compared to patients treated less than 6 months, underscoring the vigilance required on the part of the prescriber. An overview of toxicity and management recommendations can be accessed in the citation by Eisen et al. [82]. In addition, an entire chapter is dedicated in this book on renal toxicities of biological agents as the ones used in RCC treatment.
Case #2 Follow-Up and Discussion
Based on above discussion, capillary leak syndrome (b) is the correct answer. Thrombotic microangiopathy is usually seen in TKIs and anti-VEGF agents. Minimal-change disease has been reported in TKIs.
Summary
Active surveillance may be considered in the management of small renal masses, especially in individuals who are not surgical candidates. Surgical treatment for renal masses includes partial or radical nephrectomy via an open approach or laparoscopy with or without the use of robot assistance. Although image-guided percutaneous ablative therapies are utilized, data regarding long-term oncologic and renal functional outcomes are not yet available. The era of targeted therapy for RCC has seen the development of several agents that have improved upon the prior treatment paradigm of the cytokine era. Sequencing of the use of these medications is becoming clearer with experience and new data. Combinations of therapy have generally resulted in increased toxicity without concomitant improvements in efficacy. Management of the treatment-related adverse effects requires in depth understanding of the “off target” effects in order to maintain patients on therapy with the best possible outcomes for survival and for quality of life.
Abbreviations
- AS:
-
Active Surveillance
- AUA:
-
American Urological Association
- BHD:
-
Birt–Hogg–Dube
- CKD:
-
Chronic kidney disease
- CR:
-
Complete response
- CT:
-
Computed tomography
- DFS:
-
Disease-free survival
- EORTC:
-
European Organization for Research and Treatment of Cancer
- ESKD:
-
End-stage kidney disease
- FGFR:
-
Fibroblast growth factor receptor
- GFR:
-
Glomerular filtration rate
- HLRCC:
-
Hereditary Leiomyomatosis Renal Cell Cancer
- HIF:
-
Hypoxia inducible factor
- IV:
-
Intravenous
- KPS:
-
Karnofsky performance score
- MRI:
-
Magnetic resonance imaging
- MPA:
-
Medroxyprogesterone
- MSKCC:
-
Memorial Sloan Kettering Cancer Center
- mTOR:
-
Mammalian target of rapamycin
- NCCN:
-
National Comprehensive Cancer Network
- NSS:
-
Nephron sparing surgery
- OS:
-
Overall survival
- PDGF:
-
Platelet-derived growth factor
- PDGFR:
-
Platelet-derived growth factor receptor
- PFS:
-
Progression-free survival
- PN:
-
Partial nephrectomy
- RCC:
-
Renal cell cancer
- RFA:
-
Radiofrequency ablation
- RN:
-
Radical Nephrectomy
- TGF:
-
Transforming growth factor
- TKI:
-
Tyrosine kinase inhibitors
- VEGF:
-
Vascular endothelial growth factor
- VEGFR:
-
Vascular endothelial growth factor receptor
- VHL:
-
von Hippel–Lindau
References
Cancer of the Kidney and Renal Pelvis – SEER Stat Fact Sheets [Internet]. seer.cancer.gov. [cited 2014 ]. http://seer.cancer.gov/statfacts/html/kidrp.html.
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63(1):11–30.
Cote ML, Colt JS, Schwartz KL, Wacholder S, Ruterbusch JJ, Davis F, et al. Cigarette smoking and renal cell carcinoma risk among black and white Americans: effect modification by hypertension and obesity. Cancer Epidemiol Biomarkers Prev. 2012;21(5):770–9.
Kroeger N, Klatte T, Birkhäuser FD, Rampersaud EN, Seligson DB, Zomorodian N, et al. Smoking negatively impacts renal cell carcinoma overall and cancer-specific survival. Cancer. 2012;118(7):1795–802.
Sunela KL, Kataja MJ, Kellokumpu-Lehtinen P-LI. Influence of body mass index and smoking on the long-term survival of patients with renal cell cancer. Clin Genitourin Cancer. 2013;11(4):458–64.
Ljungberg B, Campbell SC, Choi HY, Cho HY, Jacqmin D, Lee JE, et al. The epidemiology of renal cell carcinoma. Eur Urol. 2011;60(4):615–21.
Reeves GK, Pirie K, Beral V, Green J, Spencer E, Bull D, et al. Cancer incidence and mortality in relation to body mass index in the Million Women Study: cohort study. BMJ. 2007;335(7630):1134.
Schrader AJ, Rustemeier J, Rustemeier JC, Timmesfeld N, Varga Z, Hegele A, et al. Overweight is associated with improved cancer-specific survival in patients with organ-confined renal cell carcinoma. J Cancer Res Clin Oncol. 2009;135(12):1693–9.
Colt JS, Schwartz K, Graubard BI, Davis F, Ruterbusch J, DiGaetano R, et al. Hypertension and risk of renal cell carcinoma among white and black Americans. Epidemiology. 2011;22(6):797–804.
Fryzek JP, Poulsen AH, Johnsen SP, McLaughlin JK, Sørensen HT, Friis S. A cohort study of antihypertensive treatments and risk of renal cell cancer. Br J Cancer. 2005;92(7):1302–6.
Lipworth L, Tarone RE, McLaughlin JK. The epidemiology of renal cell carcinoma. J Urol. 2006;176(6 Pt 1):2353–8.
Gigante M, Neuzillet Y, Patard J-J, Tillou X, Thuret R, Branchereau J, et al. Renal cell carcinoma (RCC) arising in native kidneys of dialyzed and transplant patients: are they different entities? BJU Int. 2012 ;110(11 Pt B):E570–3.
Neuzillet Y, Tillou X, Mathieu R, Long J-A, Gigante M, Paparel P, et al. Renal cell carcinoma (RCC) in patients with end-stage renal disease exhibits many favourable clinical, pathologic, and outcome features compared with RCC in the general population. Eur Urol. 2011;60(2):366–73.
Sassa N, Hattori R, Tsuzuki T, Watarai Y, Fukatsu A, Katsuno S, et al. Renal cell carcinomas in haemodialysis patients: does haemodialysis duration influence pathological cell types and prognosis? Nephrol Dial Transplant. 2011;26(5):1677–82.
Nouh MAAM, Kuroda N, Yamashita M, Hayashida Y, Yano T, Minakuchi J, et al. Renal cell carcinoma in patients with end-stage renal disease: relationship between histological type and duration of dialysis. BJU Int. 2010;105(5):620–7.
Linehan WM, Walther MM, Zbar B. The genetic basis of cancer of the kidney. J Urol. 2003;170(6 Pt 1):2163–72.
Linehan WM, Lerman MI, Zbar B. Identification of the von Hippel-Lindau (VHL) gene. Its role in renal cancer. JAMA. 1995;273(7):564–70.
Walther MM, Lubensky IA, Venzon D, Zbar B, Linehan WM. Prevalence of microscopic lesions in grossly normal renal parenchyma from patients with von Hippel-Lindau disease, sporadic renal cell carcinoma and no renal disease: clinical implications. J Urol. 1995;154(6):2010–4; (discussion2014–5).
Gnarra JR, Tory K, Weng Y, Schmidt L, Wei MH, Li H, et al. Mutations of the VHL tumour suppressor gene in renal carcinoma. Nat Genet. 1994;7(1):85–90.
Herman JG, Latif F, Weng Y, Lerman MI, Zbar B, Liu S, et al. Silencing of the VHL tumor-suppressor gene by DNA methylation in renal carcinoma. Proc Natl Acad Sci U S A. 1994;91(21):9700–4.
Linehan WM, Vasselli J, Srinivasan R, Walther MM, Merino M, Choyke P, et al. Genetic basis of cancer of the kidney: disease-specific approaches to therapy. Clin Cancer Res. 2004;10(18 Pt 2):6282S–9S.
Rosner I, Bratslavsky G, Pinto PA, Linehan WM. The clinical implications of the genetics of renal cell carcinoma. Urol Oncol. 2009;27(2):131–6.
Hughson MD, Meloni A, Dougherty S, Silva FG, Sandberg AA. Analysis of 3p allelic loss in papillary and nonpapillary renal cell carcinomas. Correlation with tumor karyotypes. Cancer Genet Cytogenet. 1996;87(2):133–9.
Corless CL, Aburatani H, Fletcher JA, Housman DE, Amin MB, Weinberg DS. Papillary renal cell carcinoma: quantitation of chromosomes 7 and 17 by FISH, analysis of chromosome 3p for LOH, and DNA ploidy. Diagn Mol Pathol. 1996;5(1):53–64.
Grubb RL, Franks ME, Toro J, Middelton L, Choyke L, Fowler S, et al. Hereditary leiomyomatosis and renal cell cancer: a syndrome associated with an aggressive form of inherited renal cancer. J Urol. 2007;177(6):2074–9; (discussion2079–80).
Menko FH, van Steensel MAM, Giraud S, Friis-Hansen L, Richard S, Ungari S, et al. Birt-Hogg-Dubé syndrome: diagnosis and management. Lancet Oncol. 2009;10(12):1199–206.
Lee WK, Byun S-S, Kim HH, Rha KH, Hwang T-K, Sung GT, et al. Characteristics and prognosis of chromophobe non-metastatic renal cell carcinoma: a multicenter study. Int J Urol. 2010;17(11):898–904.
Przybycin CG, Cronin AM, Darvishian F, Gopalan A, Al-Ahmadie HA, Fine SW, et al. Chromophobe renal cell carcinoma: a clinicopathologic study of 203 tumors in 200 patients with primary resection at a single institution. Am J Surg Pathol. 2011;35(7):962–70.
Prince MR, Zhang H, Morris M, MacGregor JL, Grossman ME, Silberzweig J, et al. Incidence of nephrogenic systemic fibrosis at two large medical centers. Radiology. 2008;248(3):807–16.
Perez-Rodriguez J, Lai S, Ehst BD, Fine DM, Bluemke DA. Nephrogenic systemic fibrosis: incidence, associations, and effect of risk factor assessment-report of 33 cases. Radiology. 2009;250(2):371–7.
Mühlfeld AS, Lange C, Kroll G, Floege J, Krombach GA, Kuhl C, et al. Pilot study of noncontrast-enhanced MRI vs. ultrasound in renal transplant recipients with acquired cystic kidney disease: a prospective intra-individual comparison. Clin Transplant. 2013;27(6):E694–701.
Motzer RJ, Agarwal N, Beard C, Bolger GB, Boston B, Carducci MA, et al. NCCN clinical practice guidelines in oncology: kidney cancer. J Natl Compr Canc Netw. 2009;7(6):618–30.
Halverson SJ, Kunju LP, Bhalla R, Gadzinski AJ, Alderman M, Miller DC, et al. Accuracy of determining small renal mass management with risk stratified biopsies: confirmation by final pathology. J Urol. 2013;189(2):441–6.
Donat SM, Diaz M, Bishoff JT, Coleman JA, Dahm P, Derweesh IH, et al. Follow-up for clinically localized renal neoplasms: AUA guideline. J Urol. 2013;190(2):407–16.
Mason RJ, Abdolell M, Trottier G, Pringle C, Lawen JG, Bell DG, et al. Growth kinetics of renal masses: analysis of a prospective cohort of patients undergoing active surveillance. Eur Urol. 2011;59(5):863–7.
George AK, herati AS, Rais-Bahrami S, waingankar N, Kavoussi LR. Laparoscopic partial nephrectomy for hilar tumors: oncologic and renal functional outcomes. Urology. 2014;83(1):111–5.
van Poppel H, Da Pozzo L, Albrecht W, Matveev V, Bono A, Borkowski A, et al. A prospective, randomised EORTC intergroup phase 3 study comparing the oncologic outcome of elective nephron-sparing surgery and radical nephrectomy for low-stage renal cell carcinoma. Eur Urol. 2011;59(4):543–52.
Tan H-J, Norton EC, Ye Z, Hafez KS, Gore JL, Miller DC. Long-term survival following partial vs radical nephrectomy among older patients with early-stage kidney cancer. JAMA. 2012;307(15):1629–35.
Salami SS, George AK, Rais-Bahrami S. Outcomes of minimally invasive urologic surgery in the elderly patient population. Curr Transl Geriatr and Exp Gerontol Rep. Current Science Inc. 2013;2(2):84–90.
Gill IS, Patil MB, Abreu AL de C, Ng C, Cai J, Berger A, et al. Zero ischemia anatomical partial nephrectomy: a novel approach. J Urol. 2012;187(3):807–14.
Abreu ALC, Gill IS, Desai MM. Zero-ischaemia robotic partial nephrectomy (RPN) for hilar tumours. BJU Int. 2011;108(6 Pt 2):948–54.
George AK, herati AS, Srinivasan AK, Rais-Bahrami S, waingankar N, Sadek MA, et al. Perioperative outcomes of off-clamp vs complete hilar control laparoscopic partial nephrectomy. BJU Int. 2013;111(4 Pt B):E235–41.
Salami SS, George AK, Rais-Bahrami S, Okhunov Z, waingankar N, Kavoussi LR. Off-clamp laparoscopic partial nephrectomy for hilar tumors: oncologic and renal functional outcomes. J Endourol. 2014;28(2):191–5.
Scosyrev E, Messing EM, Sylvester R, Campbell S, Van Poppel H. Renal function after nephron-sparing surgery versus radical nephrectomy: results from eortc randomized trial 30904. Eur Urol. 2014;65(2):372–7.
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu C-Y. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351(13):1296–305.
Baust J, Gage AA, Ma H, Zhang CM. Minimally invasive cryosurgery-technological advances. Cryobiology. 1997;34(4):373–84.
Gage AA, Baust J. Mechanisms of tissue injury in cryosurgery. Cryobiology. 1998;37(3):171–86.
Goldberg SN, Gazelle GS, Mueller PR. Thermal ablation therapy for focal malignancy: a unified approach to underlying principles, techniques, and diagnostic imaging guidance. AJR Am J Roentgenol. 2000;174(2):323–31.
Lui K-W, Gervais DA, Arellano RA, Mueller PR. Radiofrequency ablation of renal cell carcinoma. Clin Radiol. 2003;58(12):905–13.
Dib El R, Touma NJ, Kapoor A. Cryoablation vs radiofrequency ablation for the treatment of renal cell carcinoma: a meta-analysis of case series studies. BJU Int. 2012;110(4):510–6.
Motzer RJ, Mazumdar M, Bacik J, Berg W, Amsterdam A, Ferrara J. Survival and prognostic stratification of 670 patients with advanced renal cell carcinoma. J Clin Oncol. 1999;17(8):2530–40.
Mickisch GH, Garin A, Van Poppel H, de Prijck L, Sylvester R. European Organisation for Research and Treatment of Cancer (EORTC) Genitourinary Group. Radical nephrectomy plus interferon-alfa-based immunotherapy compared with interferon alfa alone in metastatic renal-cell carcinoma: a randomised trial. The Lancet. 2001;358(9286):966–70.
Flanigan RC, Salmon SE, Blumenstein BA, Bearman SI, Roy V, McGrath PC, et al. Nephrectomy followed by interferon alfa-2b compared with interferon alfa-2b alone for metastatic renal-cell cancer. N Engl J Med. 2001;345(23):1655–9.
Flanigan RC, Mickisch G, Sylvester R, Tangen C, Van Poppel H, Crawford ED. Cytoreductive nephrectomy in patients with metastatic renal cancer: a combined analysis. J Urol. 2004;171(3):1071–6.
Rini BI. Metastatic renal cell carcinoma: many treatment options, one patient. J Clin Oncol. 2009;27(19):3225–34.
Gleave ME, Elhilali M, Fradet Y, Davis I, Venner P, Saad F, et al. Interferon gamma-1b compared with placebo in metastatic renal-cell carcinoma. Canadian Urologic Oncology Group. N Engl J Med. 1998;338(18):1265–71.
Wong ASA, Chong K-TK, Heng C-TC, Consigliere DTD, Esuvaranathan KK, Toh K-LK, et al. Debulking nephrectomy followed by a “watch and wait” approach in metastatic renal cell carcinoma. Urol Oncol. 2009;27(2):149–54.
Mekhail TM, Abou-Jawde RM, Boumerhi G, Malhi S, Wood L, Elson P, et al. Validation and extension of the Memorial Sloan-Kettering prognostic factors model for survival in patients with previously untreated metastatic renal cell carcinoma. J Clin Oncol. 2005;23(4):832–41.
Heng DY, Xie W, Regan MM, Warren MA, Golshayan AR, Sahi C, et al. Prognostic factors for overall survival in patients with metastatic renal cell carcinoma treated with vascular endothelial growth factor-targeted agents: results from a large, multicenter study. J Clin Oncol. 2009;27(34):5794–9.
Coppin C, Kollmannsberger C, Le L, Porzsolt F, Wilt TJ. Targeted therapy for advanced renal cell cancer (RCC): a Cochrane systematic review of published randomised trials. BJU Int. 2011;108(10):1556–63.
Heng DYC, Xie W, Bjarnason GA, Vaishampayan U, Tan M-H, Knox J, et al. Progression-free survival as a predictor of overall survival in metastatic renal cell carcinoma treated with contemporary targeted therapy. Cancer. 2011;117(12):2637–42.
Medical Research Council Renal Cancer Collaborators. Interferon-alpha and survival in metastatic renal carcinoma: early results of a randomised controlled trial. The Lancet. 1999;353(9146):14–7.
Coppin C, Porzsolt F, Awa A, Kumpf J, Coldman A, Wilt T. Immunotherapy for advanced renal cell cancer. Cochrane Database Syst Rev. 2005 Jan 25;(1):CD001425.
Klapper JAJ, Downey SGS, Smith FOF, Yang JCJ, Hughes MSM, Kammula USU, et al. High-dose interleukin-2 for the treatment of metastatic renal cell carcinoma: a retrospective analysis of response and survival in patients treated in the surgery branch at the National Cancer Institute between 1986 and 2006. Cancer. 2008;113(2):293–301.
Escudier B, Eisen T, Stadler WM, Szczylik C, Oudard S, Siebels M, et al. Sorafenib in advanced clear-cell renal-cell carcinoma. N Engl J Med. 2007;356(2):125–34.
Escudier B, Szczylik C, Hutson TE, Demkow T, Staehler M, Rolland F, et al. Randomized phase ii trial of first-line treatment with sorafenib versus interferon Alfa-2a in patients with metastatic renal cell carcinoma. J Clin Oncol. 2009;27(8):1280–9.
Perry MC, Doll DC, Freter CE. Perry’s The Chemotherapy source book. Philadelphia: Lippincott Williams & Wilkins. 2012. (1 p).
Motzer RJ, Hutson TE, Tomczak P, Michaelson MD, Bukowski RM, Rixe O, et al. Sunitinib versus interferon alfa in metastatic renal-cell carcinoma. N Engl J Med. 2007;356(2):115–24.
Motzer RJ, Hutson TE, Tomczak P, Michaelson MD, Bukowski RM, Oudard S, et al. Overall survival and updated results for sunitinib compared with interferon alfa in patients with metastatic renal cell carcinoma. J Clin Oncol. 2009;27(22):3584–90.
Sternberg CNC, Davis IDI, Mardiak JJ, Szczylik CC, Lee EE, Wagstaff JJ, et al. Pazopanib in locally advanced or metastatic renal cell carcinoma: results of a randomized phase III trial. J Clin Oncol. 2010;28(6):1061–8.
Motzer RJ, Hutson TE, Cella D, Reeves J, Hawkins R, Guo J, et al. Pazopanib versus sunitinib in metastatic renal-cell carcinoma. N Engl J Med. 2013;369(8):722–31.
Rini BI, Escudier B, Tomczak P, Kaprin A, Szczylik C, Hutson TE, et al. Comparative effectiveness of axitinib versus sorafenib in advanced renal cell carcinoma (AXIS): a randomised phase 3 trial. The Lancet. 2011;378(9807):1931–9.
Hudes G, Carducci M, Tomczak P, Dutcher J, Figlin R, Kapoor A, et al. Temsirolimus, interferon alfa, or both for advanced renal-cell carcinoma. N Engl J Med. 2007;356(22):2271–81.
Motzer RJ, Escudier B, Oudard S, Hutson TE, Porta C, Bracarda S, et al. Efficacy of everolimus in advanced renal cell carcinoma: a double-blind, randomised, placebo-controlled phase III trial. The Lancet. 2008;372(9637):449–56.
Rini BI, Halabi S, Rosenberg JE, Stadler WM, Vaena DA, Ou S-S, et al. Bevacizumab plus interferon alfa compared with interferon alfa monotherapy in patients with metastatic renal cell carcinoma: CALGB 90206. J Clin Oncol. 2008;26(33):5422–8.
Rini BI, Halabi S, Rosenberg JE, Stadler WM, Vaena DA, Archer L, et al. Phase III trial of bevacizumab plus interferon alfa versus interferon alfa monotherapy in patients with metastatic renal cell carcinoma: final results of CALGB 90206. J Clin Oncol. 2010;28(13):2137–43.
Yang JC, Haworth L, Sherry RM, Hwu P, Schwartzentruber DJ, Topalian SL, et al. A randomized trial of bevacizumab, an anti-vascular endothelial growth factor antibody, for metastatic renal cancer. N Engl J Med. 2003;349(5):427–34.
Oudard SS, Banu EE, Vieillefond AA, Fournier LL, Priou FF, Medioni JJ, et al. Prospective multicenter phase II study of gemcitabine plus platinum salt for metastatic collecting duct carcinoma: results of a GETUG (Groupe d’Etudes des Tumeurs Uro-Génitales) study. J Urol. 2007;177(5):1698–702.
Nanus DMD, Garino AA, Milowsky MIM, Larkin MM, Dutcher JPJ. Active chemotherapy for sarcomatoid and rapidly progressing renal cell carcinoma. Cancer. 2004;101(7):1545–51.
Gore ME, Szczylik C, Porta C, Bracarda S, Bjarnason GA, Oudard S, et al. Safety and efficacy of sunitinib for metastatic renal-cell carcinoma: an expanded-access trial. Lancet Oncol. 2009;10(8):757–63.
Jhaveri KD, Flombaum CD, Kroog G, Glezerman IG. Nephrotoxicities associated with the use of tyrosine kinase inhibitors: a single-center experience and review of the literature. Nephron Clin Pract. 2011;117(4):c312–9.
Eisen TT, Sternberg CNC, Robert CC, Mulders PP, Pyle LL, Zbinden SS, et al. Targeted therapies for renal cell carcinoma: review of adverse event management strategies. J Natl Cancer Inst. 2012;104(2):93–113.
Acknowledgement
The authors thank Paras Shah, MD, for assisting with the development of Table 9.2.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Salami, S., Vira, M., Bradley, T. (2015). Surgical and Medical Options in the Management of Renal Cell Carcinoma. In: Jhaveri, K., Salahudeen, A. (eds) Onconephrology. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-2659-6_9
Download citation
DOI: https://doi.org/10.1007/978-1-4939-2659-6_9
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-2658-9
Online ISBN: 978-1-4939-2659-6
eBook Packages: MedicineMedicine (R0)