Abstract
The hereditary spastic paraplegia (HSP) are inherited disorders in which the primary neurological syndrome is bilateral, approximately symmetrical, lower-extremity spastic weakness, often accompanied by urinary urgency (Fink 2003; Figs. 1 and 2)
Access provided by CONRICYT-eBooks. Download reference work entry PDF
Similar content being viewed by others
The hereditary spastic paraplegia (HSP) are inherited disorders in which the primary neurological syndrome is bilateral, approximately symmetrical, lower-extremity spastic weakness, often accompanied by urinary urgency (Fink 2003; Figs. 1 and 2)
Synonyms and Related Disorders
Allan–Herndon–Dudley syndrome; Cerebral palsy; Crash syndrome; Familial spastic paraplegia; Gareis–Mason syndrome; Kjellin syndrome; Mast syndrome; MASA syndrome; Pelizeaus–Merzbacher disease; Silver syndrome; Spastic quadriplegia/tetraplegia; Strumpell disease; Troyer syndrome; X-linked hydrocephalus
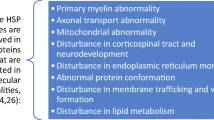
Genetics/Basic Defects
-
1.
Genetic types of HSP (Fink 1997, 2002, 2003, 2013; Online Mendelian Inheritance in Man (OMIM))
-
1.
Autosomal dominant, autosomal recessive, and X-linked HSP are each genetically heterogeneous
-
2.
Twenty genetic types of HSP defined by genetic linkage analysis
-
3.
HSP loci are designated SPG (“spastic paraplegia”) 1–21 in order of their discovery
-
1.
-
2.
Autosomal dominant HSP
-
1.
SPG3A (OMIM 182600) (14q22.1)
-
1.
Caused by mutation in the atlastin gene
-
2.
Symptoms usually begin in early childhood, often nonprogressive (Strumpell disease)
-
1.
-
2.
SPG4 (OMIM 182601) (2p22.3)
-
1.
Caused by mutation in the spastin gene
-
2.
Most common type of dominantly inherited HSP (45%)
-
3.
May be associated with dementia
-
1.
-
3.
SPG6 (OMIM 600363) (15q11.2)
-
1.
Caused by mutation in the nonimprinted gene in Prader–Willi syndrome/Angelman syndrome chromosome region-1 gene (NIPA1)
-
2.
Prototypical late-adolescent, early-adult onset, slowly progressive uncomplicated HSP. Rarely complicated by epilepsy or variable peripheral neuropathy
-
1.
-
4.
SPG8 (OMIM 603563) (8q24.13)
-
1.
Caused by mutation in the KIAA0196 gene
-
2.
Symptoms begin in adulthood, often severe
-
3.
Progressive lower-limb spasticity and hyperreflexia resulting in difficulty walking
-
4.
Other features: upper limb spasticity, impaired vibration sense in the distal lower limbs, and urinary urgency or incontinence (de Bot et al. 2013)
-
1.
-
5.
SPG10 (OMIM 604187) (12q13.3)
-
1.
Caused by mutation in the kinesin-5A gene
-
2.
Associated with distal muscle wasting
-
1.
-
6.
SPG12 (OMIM 604805) (19q13.32)
-
1.
Caused by mutation in the reticulon 2 gene (RTN2)
-
2.
Lower-limb spasticity and hyperreflexia, resulting in walking difficulties, with some patients having urinary symptoms and distal sensory impairment (Montenegro et al. 2012)
-
1.
-
7.
SPG13 (OMIM 605280) (2q33.1)
-
1.
Caused by mutation in the mitochondrial chaperonin HSP60 gene
-
2.
Lower-limb spasticity/weakness, hyperreflexia, extensor plantar responses, pyramidal signs, decreased vibratory sense in the lower limbs, and urinary urgency/incontinence
-
1.
-
8.
SPG17 (OMIM 270985) (11q12.3)
-
1.
Caused by mutation in the BSCL gene
-
2.
Spastic paraplegia with amyotrophy of hands and feet (Silver syndrome) (Silver 1966)
-
1.
-
9.
SPG31 (OMIM 610250) (2p11.2)
-
1.
Caused by mutation in the receptor expression–enhancing protein-1 gene (REEP1)
-
2.
Onset: most in first or second decade
-
1.
-
10.
SPG33 (OMIM 610244) (10q24.2)
-
1.
Caused by mutation in the zinc finger FYVE domain–containing protein-27 gene (ZFYVE27)
-
2.
Lower-limb spasticity/weakness, spastic gait, hyperreflexia, extensor plantar responses, ankle clonus
-
1.
-
11.
SPG42 (OMIM 612539) (3q25.31)
-
1.
Caused by mutation in the solute carrier family 33 (acetyl-CoA transporter), member 1 gene (SLC33A1)
-
2.
Varied age of onset with increased lower-limb tone, hyperreflexia, lower-limb muscle weakness/atrophy, extensor plantar responses, and pes cavus in Chinese (Lin et al. 2008)
-
1.
-
12.
SPG61 (OMIM 615685) (16p12.3)
-
1.
Caused by mutation in the ARL6IP1 gene
-
2.
Spastic paraplegia with polysensory and motor neuropathy and loss of terminal digits due to acropathy (Novarino et al. 2014)
-
1.
-
1.
-
3.
Autosomal recessive HSP
-
1.
SPG5A (OMIM 270800) (8q12.3)
-
1.
Caused by mutation in the cytochrome P450, family 7, subfamily b, polypeptide 1 gene (CYP7B1)
-
2.
Some patients with pure spastic paraplegia affecting gait, whereas others with complicated phenotype with additional manifestations including optic atrophy or cerebellar ataxia (Arnoldi et al. 2012)
-
1.
-
2.
SPG7 (OMIM 607259) (16q24.3)
-
1.
Caused by mutation in the paraplegin gene (PGN)
-
2.
Variably associated with mitochondrial abnormalities on skeletal muscle biopsy and dysarthria, dysphagia, optic disc pallor, axonal neuropathy, and evidence of “vascular lesions,” cerebellar or cerebral atrophy on cranial MRI
-
1.
-
3.
SPG11 (OMIM 604360) (15q21.1)
-
1.
Caused by mutation in the spatacsin gene
-
2.
Perhaps the most common autosomal recessive form of HSP (50%)
-
3.
Variably associated with thin corpus callosum, mental retardation, upper extremity weakness, dysarthria, and nystagmus
-
4.
Symptoms begin in the first or second decades
-
1.
-
4.
SPG15 (OMIM 270700) (14q24.1)
-
1.
Caused by mutation in the gene encoding spastizin (ZFYVE26)
-
2.
Progressive spasticity affecting the lower limbs associated with retinal degeneration, pigmental maculopathy, distal amyotrophy, dysarthria, mental retardation, and further intellectual deterioration (Kjellin syndrome) (Goizet et al. 2009)
-
1.
-
5.
SPG18 (OMIM 611225) (8p11.3)
-
1.
Caused by mutation in the endoplasmic reticulum lipid raft–associated protein 2 gene (ERLIN2)
-
2.
Spastic paraplegia complicated by mental retardation and thin corpus callosum. Also juvenile primary lateral sclerosis
-
1.
-
6.
SPG20 (OMIM 275900) (13q13.3)
-
1.
Caused by mutation in the gene encoding spartin (SPG20)
-
2.
Spastic paraplegia associated with distal muscle wasting (Troyer syndrome)
-
1.
-
7.
SPG21 (OMIM 248900) (15q22.31)
-
1.
Caused by mutation in the gene encoding the 33-kD acidic cluster protein (ACP33)
-
2.
Progressive spastic paraparesis associated in more advanced cases with cognitive decline, dementia, other neurological abnormalities, and brain imaging showing thinning of the corpus callosum (Simpson et al. 2003)
-
3.
Also called Mast syndrome
-
1.
-
8.
SPG26 (OMIM 609195) (12p11.1-q14)
-
1.
Caused by mutation in the beta-1,4-N-acetylgalactosaminyltransferase 1 gene (B4GALNT1)
-
2.
Onset in the first two decades of life of gait abnormalities due to lower-limb spasticity and muscle weakness with upper limb involvement in some patients
-
3.
Additional features: intellectual disability, peripheral neuropathy, dysarthria, cerebellar signs, extrapyramidal signs, and cortical atrophy (Boukhris et al. 2013)
-
1.
-
9.
SPG 28 (OMIM 609340) (14q22.1)
-
1.
Caused by mutation in the DDHD1 gene
-
2.
Early-onset, slowly progressive lower-limb spasticity resulting in walking difficulties, with some patients having distal sensory impairment (Tesson et al. 2012)
-
1.
-
10.
SPG 30 (OMIM 610357) (2q37.3)
-
1.
Caused by mutation in the kinesin family member 1A gene (KIF1A)
-
2.
Onset in the first and second decades of unsteady spastic gait and hyperreflexia of the lower limbs (Erlich et al. 2011)
-
1.
-
11.
SPG35 (OMIM 612319) (16q23.1)
-
1.
Caused by mutation in the gene encoding fatty acid 2-hydroxylase (FA2H)
-
2.
Childhood onset of gait difficulties due to progressive spastic paraparesis, dysarthria, and mild cognitive decline associated with leukodystrophy on brain imaging
-
3.
Other variable neurological features: dystonia, optic atrophy, and seizures (Dick et al. 2010)
-
4.
Phenotypic spectrum of disorders referred as fatty acid hydrolase–associated neurodegeneration (Kruer et al. 2010)
-
1.
-
12.
SPG39 (OMIM 612020) (19p13.2)
-
1.
Uncomplicated HSP
-
2.
Caused by mutation in the patatin-like phospholipase domain–containing protein 6 gene (PNPLA6)
-
3.
Progressive spastic paraplegia associated with distal upper- and lower-extremity wasting (Rainier et al. 2008)
-
1.
-
13.
SPG43 (OMIM 615043) (19q12)
-
1.
Caused by mutation in the chromosome 19 open reading frame 12 gene (C19ORF12)
-
2.
Progressive spastic paraplegia with atrophy of intrinsic hand muscles and dysarthria
-
1.
-
14.
SPG44 (OMIM 613206) (1q42.13)
-
1.
Caused by mutation in the gap junction protein, gamma-2 gene (GJC2)
-
2.
Lower-/upper-limb spasticity, spastic gait, hyperreflexia, extensor plantar responses, dysarthria, intentional tremor, dysmetria, cerebellar ataxia, hypomeyelinating leukoencephalopathy, and thin corpus callosum (Orthmann-Murphy et al. 2009)
-
1.
-
15.
SPG45 (OMIM 613162) (10q24.3-25.1)
-
1.
Caused by mutation in the 5-prime nucleotidase cytosolic II gene (NT5C2)
-
2.
Onset in the first 2 years of life with lower-limb spasticity, spastic gait, hyperreflexia, mental retardation, and brain MRI features of dysplastic/thin corpus callosum and white-matter changes (Novarino et al. 2014)
-
1.
-
16.
SPG46 (OMIM 614409) (9p13.3)
-
1.
Caused by mutation in the beta acid glucosidase 2 gene (GBA2)
-
2.
Onset: childhood with slowly progressive spastic paraplegia and cerebellar signs
-
3.
Some patients with cognitive impairment, cataracts, and cerebral, cerebellar, and corpus callosum atrophy (Boukhris et al. 2010; Martin et al. 2013)
-
1.
-
17.
SPG47 (OMIM 614066) (1p13.2)
-
1.
Caused by mutation in the adapter-related protein complex 4, beta-1 subunit gene (AP4B1)
-
2.
Neonatal hypotonia progressing to hypertonia and spasticity and severe mental retardation with poor or absent speech development (Abou Jamra et al. 2011)
-
1.
-
18.
SPG48 (OMIM 613647) (7p22.1)
-
1.
Caused by mutation in the KIAA0415 gene
-
2.
Progressive spastic paraplegia associated with urinary incontinence in two adult French sibs (Slabicki et al. 2010)
-
1.
-
19.
SPG49 (OMIM 615031) (14q32.31)
-
1.
Caused by mutation in the tectonin beta-propeller repeat-containing protein 2 gene (TECPR2)
-
2.
Onset of spastic paraplegia in the first decade associated with delayed psychomotor development, mental retardation, dysmorphic features, thin corpus callosum on MRI, and episodes of central apnea, which may be fatal (Oz-Levi et al. 2012)
-
1.
-
20.
SPG50 (OMIM 612936) (7q22.1)
-
1.
Caused by mutation in the adapter-related protein complex 4, MU-1 subunit gene (AP4M1)
-
2.
Neonatal hypotonia progressing to hypertonia, spastic quadriplegia, severe mental retardation with poor or absent speech development, dysmorphic features, and abnormal brain MRI (ventriculomegaly, white-matter abnormalities and variable cerebral atrophy) (Verkerk et al. 2009)
-
1.
-
21.
SPG51 (OMIM 613744) (15q21.2)
-
1.
Caused by mutation in the adapter-related protein complex 4, epsilon-1 subunit gene (AP4E1)
-
2.
Neonatal hypotonia progressing to hypertonia and spastic quadriplegia/tetraplegia and severe mental retardation, poor or absent speech development, dysmorphic features, and abnormal brain MRI (enlarged ventricles, cortical and cerebellar atrophy, and diffuse white-matter loss) (Moreno-De-Luca et al. 2011)
-
1.
-
22.
SPG52 (OMIM 614067) (14q12)
-
1.
Caused by mutation in the adapter-related protein complex 4, sigma-1 subunit (AP4S1)
-
2.
Neonatal hypotonia progressing to hypertonia, spastic quadriplegia, severe mental retardation with poor or absent speech development, dysmorphic features, shy character, and short stature (Abou Jamra et al. 2011)
-
1.
-
23.
SPG53 (OMIM 614898) (8p22)
-
1.
Caused by mutation in the homologue of the yeast vacuolar protein sorting 37 gene (VPS37A)
-
2.
Onset in infancy of delayed motor development progressing to upper- and lower-limb spasticity with impaired walking and mild-to-moderate cognitive impairment (Zivony-Elboum et al. 2012)
-
1.
-
24.
SPG54 (OMIM 615033) (8p11.23)
-
1.
Caused by mutation in the DDHD domain-containing protein 2 gene (DDHD2)
-
2.
Psychomotor delay, cognitive impairment, progressive spasticity (onset before age 2 years), thin corpus callosum, periventricular white-matter abnormalities.
-
3.
Additional clinical features: foot contractures, dysarthria, dysphagia, strabismus, optic hypoplasia
-
1.
-
25.
SPG55 (OMIM 615035) (12q24.31)
-
1.
Caused by mutation in the chromosome 12 open reading frame 65 gene (C12ORF65)
-
2.
Spastic paraplegia associated with distal muscle atrophy/weakness, predominantly affecting the lower limbs, optic atrophy, hyperreflexia, steppage gait, difficulty walking, extensor plantar responses, axonal neuropathy, distal sensory impairment, and hypoplastic corpus callosum in some patients (Shimazaki et al. 2012; Spiegel et al. 2014)
-
1.
-
26.
SPG56 (OMIM 615030) (4q25)
-
1.
Caused by mutation in the cytochrome P450, family 2, subfamily U, polypeptide 1 gene (CYP2U1)
-
2.
Early-onset progressive lower-limb spasticity resulting in walking difficulties and often affected upper limbs (Tesson et al. 2012)
-
1.
-
27.
SPG57 (OMIM 615658) (3q12.2)
-
1.
Caused by mutation in the TRK-fused gene (TFG)
-
2.
Severe spasticity affecting lower limbs with inability to walk, hyperreflexia, extensor plantar responses, muscle weakness/atrophy affecting upper and lower limbs due to an axonal demyelinating sensorimotor neuropathy, and optic atrophy (Beetz et al. 2013)
-
1.
-
28.
SPG63 (OMIM 615686) (1p13.3)
-
1.
Caused by mutation in the AMPD2 gene
-
2.
Delayed walking and a scissors gait, followed by hypertonia, hyperreflexia, and MRI showing periventricular deep white-matter changes in the corpus callosum (Novarino et al. 2014)
-
1.
-
29.
SPG64 (OMIM 615683) (10q24.1)
-
1.
Caused by mutation in the ENTPD1 gene
-
2.
Childhood onset with unsteady gait with areflexia/hyperreflexia, dysarthria, and spasticity (Novarino et al. 2014)
-
1.
-
30.
SPG72 (OMIM 615625) (5q31.2)
-
1.
Caused by mutation in the receptor expression–enhancing protein 2 gene (REEP2)
-
2.
Spastic paraplegia with difficulty walking and stiff legs associated with hyperreflexia and extensor plantar responses in early childhood (Esteves et al. 2014)
-
3.
Autosomal recessive form has been described
-
1.
-
1.
-
4.
X-linked HSP
-
1.
SPG1 (OMIM 303350) (Xq28)
-
1.
Caused by mutation in the gene encoding the L1 cell adhesion molecule (LICAM)
-
2.
Mutations in this gene also cause MASA syndrome and X-linked recessive hydrocephalus (Crash syndrome) (OMIM 303350)
-
3.
Some forms of HSP with progressive spasticity occurs in isolation
-
4.
Others with progressive spasticity with other neurologic features including mental retardation, and variably, hydrocephalus, aphasia, and adducted/clapsed thumbs
-
5.
Also called Gareis-Mason syndrome
-
1.
-
2.
SPG2 (OMIM 312920) (Xq22.2)
-
1.
Caused by mutation in the myelin proteolipid protein gene (PLP1)
-
2.
X-linked recessive inheritance
-
3.
Allelic to Pelizaeus-Merzbacher disease
-
4.
Progressive spasticity occurs in isolation or occurs with other neurologic features, variably associated with MRI evidence of CNS white matter abnormality
-
5.
Mutations in this gene also cause Pelizeaus-Merzbacher disease (OMIM 312080)
-
1.
-
3.
SPG22 (OMIM
-
1.
Caused by mutation in the monocarboxylate transporter 8 gene (MCT8)
-
2.
Also called Allan-Herndon-Dudley syndrome (X-linked dominant)
-
3.
Congenital onset with neck muscle hypotonia in infancy, mental retardation, dysarthria, ataxia, spastic paraplegia, abnormal facies
-
1.
-
1.
Clinical Features
-
1.
Variable onset of symptoms, rate of progression and degree of disability between genetic types of HSP (Fink and Hedera 1999; Fink 2003), as well as within individual families in which all subjects have precisely the same HSP gene mutation
-
1.
Initial symptoms: tumbling and tripping due to lower-extremity stiffness and weakness with age of onset at any age from infancy to senescence
-
2.
Later symptoms
-
1.
Marked lower-extremity spastic weakness
-
2.
Requiring cane, walker, or wheelchair
-
1.
-
1.
-
2.
Correlation of age of onset and progression of the disease
-
1.
In general, HSP symptoms beginning in early childhood may not show significant worsening even over many years.
-
2.
In contrast, HSP symptoms beginning after adolescence typically worsen insidiously
-
3.
Urinary urgency is very common, and although usually occurring after many years, it may occasionally be the presenting symptom of HSP
-
4.
In uncomplicated HSP
-
1.
Spastic weakness: confined to the lower extremities
-
2.
Normal strength and dexterity of the upper extremities, speech, and swallowing remain normal
-
1.
-
1.
-
3.
Classification of HSP (Harding 1983)
-
1.
Uncomplicated HSP
-
1.
Neurological findings confined to the lower extremities
-
1.
Spastic weakness
-
2.
Hyperreflexia
-
3.
Extensor plantar responses
-
4.
Mildly impaired vibratory sensation in the distal lower extremities
-
1.
-
2.
Normal strength and dexterity of the upper extremities, speech, and swallowing remain normal
-
1.
-
2.
Complicated HSP
-
1.
Signs of uncomplicated HSP plus
-
2.
Other neurological or systemic impairments not attributed to coexisting disorders
-
1.
Cataracts
-
2.
Motor neuropathy
-
3.
Mental retardation
-
4.
Muscle wasting
-
1.
-
1.
-
1.
-
4.
Diagnosis of HSP
-
1.
Typical symptoms of gait disturbance often associated with urinary urgency
-
1.
Childhood onset, essentially nonprogressive spastic diplegia
-
2.
Childhood-through-adulthood onset of insidiously progressive spastic weakness in the legs
-
1.
-
2.
Neurological findings of corticospinal tract deficits
-
1.
Lower extremities
-
1.
Spasticity
-
2.
Weakness
-
3.
Hyperreflexia
-
4.
Extensor plantar responses
-
1.
-
2.
Upper extremities
-
1.
Brisk but not pathological reflexes
-
2.
Normal muscle tone
-
1.
-
1.
-
3.
Family history of similar disorder
-
4.
Exclusion of alternate disorders such as
-
1.
Multiple sclerosis
-
2.
Leukodystrophy
-
3.
Structural abnormalities involving the brain and spinal cord
-
4.
Dopa-responsive dystonia
-
1.
-
1.
-
5.
Differential diagnosis of spastic paraplegia with additional abnormalities on MRI of the brain (de Bot et al. 2010)
-
1.
Leukoencephalopathy
-
1.
Many neurometabolic and other hereditary white-matter disorders with characteristic MRI pattern like Krabbe disease, Alexander disease, X-linked adrenoleukodystrophy, vanishing white matter; inflammatory disorders like multiple sclerosis, acute disseminated encephalomyelitis, and neuromyelitis optica
-
2.
HSPs: SPG4 (some), SPG11, SPG15, SPG21
-
1.
-
2.
Thin corpus callosum
-
1.
Thin corpus callosum + epilepsy, Andermann syndrome (agenesis of the corpus callosum with peripheral neuropathy) (OMIM 218000)
-
2.
HSPs: SPG1, SPG4 (some), SPG11, SPG15, SPG21, SPG32
-
1.
-
3.
Cerebral atrophy
-
1.
Cerebellar ataxia
-
2.
HSPs: SPG7
-
1.
-
1.
-
6.
Differential diagnosis of spastic paraplegia with additional clinical features (de Bot et al. 2010)
-
1.
Mental retardation
-
1.
Many neurometabolic or neurogenetic disorders; sometimes recognizable based on MRI abnormalities or further additional features
-
2.
HSPs: SPG1, SPG2, SPG11, SPG14, SPG15, SPG16, SPG20, SPG21, SPG23, SPG27, SPG32, SPG35
-
1.
-
2.
Dysmorphisms
-
1.
Andermann syndrome, hydrocephalus due to congenital stenosis of aqueduct of Sylvius
-
2.
HSPs: SPG1, SPG23
-
1.
-
3.
Optic atrophy
-
1.
Cobalamin C disease, biotinidase deficiency, cerebral folate deficiency, SPOAN (spastic paraplegia, optic atrophy, and neuropathy), ARSACS (autosomal recessive spastic ataxia of Charlevoix-Saguenay), type III 3-methylglutaconic aciduria
-
2.
HSPs: SPG7
-
1.
-
4.
Retinopathy
-
1.
Cobalamin C disease, Sjögren–Larsson syndrome, homocarnosinosis, abetalipoproteinemia
-
2.
HSPs: SPG15
-
1.
-
5.
Cataract
-
1.
Cerebrotendinous xanthomatosis, α-methyl-CoA racemase deficiency
-
2.
HSPs: SPG9
-
1.
-
6.
Hearing loss/deafness
-
1.
Biotinidase deficiency, cerebral folate deficiency
-
2.
HSPs: SPG29
-
1.
-
7.
Neuropathy/amyotrophy
-
1.
dHMN (distal hereditary motor neuropathy), HMSN (hereditary motor and sensory neuropathy) V, cerebrotendinous xanthomatosis, cobalamin C disease, MTHFR (5,10-methylenetetrahydrofolate) deficiency, metachromatic leukodystrophy, Krabbe disease, adrenomyeloneuropathy, polyglucosan body disease, α-methyl-CoA racemase deficiency, biotinidase deficiency, abetalipoproteinemia (posterior column), homocysteine remethylation defects, SPOAN, ARSACS, Andermann syndrome
-
2.
HSPs: SPG7, SPG9, SPG10, SPG11, SPG14, SPG17, SPG20, SPG27, SPG38, SPG39
-
1.
-
8.
Cerebellar ataxia
-
1.
Atypical Friedreich ataxia, cerebrotendinous xanthomatosis, triple H (hyperornithinemia-hyperammonemia-homocitrullinuria) syndrome, cerebral folate deficiency, metachromatic leukodystrophy, SAX (spastic ataxia) 1, SAX2, ARSACS, ARSAL (autosomal recessive spastic ataxia with leukoencephalopathy), Type III 3-methylglutaconic aciduria, Alexander disease
-
2.
HSPs: SPG7, SPG15, SPG20, SPG21, SPG27
-
1.
-
9.
Extrapyramidal signs/diurnal fluctuations
-
1.
Dopamine synthesis defects and cerebral folate deficiency (dystonia), amyotrophic dystonic paraplegia (dystonia), polyglucosan body disease, phenylketonuria and cerebrotendinous xanthomatosis (parkinsonism), dopa-responsive dystonia (diurnal fluctuations)
-
2.
HSPs: SPG21, SPG23 (tremor)
-
1.
-
10.
Epilepsy
-
1.
Dopamine synthesis defects, α-methyl-CoA racemase deficiency, triple H syndrome, metachromatic leukodystrophy, cerebrotendinous xanthomatosis, arginase deficiency, cerebral folate deficiency, thin corpus callosum + epilepsy, Alexander disease
-
2.
HSPs: SPG2, SPG35
-
1.
-
11.
Cutaneous signs
-
1.
Cerebrotendinous xanthomatosis (xanthomas), biotinidase deficiency (alopecia, dermatitis), Sjögren–Larsson (ichthyosis), adrenoleukodystrophy/adrenomyeloneuropathy (melanoderma)
-
2.
HSPs: SPG23 (pigmentary abnormalities)
-
1.
-
12.
Episodes of confusion, nausea/vomiting, or diarrhea
-
1.
Cobalamin C disease, MTHFR deficiency, triple H, arginase deficiency, cerebrotendinous xanthomatosis (chronic diarrhea), adrenal insufficiency (adrenomyeloneuropathy, adrenoleukodystrophy), abetalipoproteinemia (diarrhea), homocysteine remethylation defects (confusion)
-
2.
HSPs: SPG9 (gastroesophageal reflux), SPG29 (hiatus hernia, hyperbilirubinemia)
-
1.
-
1.
Diagnostic Investigations
-
1.
MRI (Fink 2006)
-
1.
Important to exclude alternative disorders including multiple sclerosis, leukodystrophies, and structural abnormalities affecting the brain or spinal cord
-
2.
Uncomplicated HSP: normal in conventional brain MRI
-
3.
Severe forms of complicated HSP: brain MRI may reveal syndrome-specific abnormalities such as thin corpus callosum in SPG11, cerebral or cerebellar abnormalities in SPG7, and hydrocephalus in SPG1
-
4.
MRI of the spinal cord: may be entirely normal or show atrophy, particularly involving the thoracic spinal cord
-
1.
-
2.
Electromyography (EMG)/nerve conduction studies (NCSs) (Fink 2006)
-
1.
Uncomplicated HSP: usually normal
-
2.
Complicated forms of HSP (e.g., SPG10, SPG14, SPG15, and SPG26): associated with peripheral neuropathy and evidence of lower motor neuron involvement
-
1.
-
3.
Muscle biopsy in some subjects with SPG7 (due to mutations in the mitochondrial metalloprotease paraplegin) shows ragged red fibers and cytochrome oxidase C negative fibers (DeMichele et al. 1998)
-
4.
Neuropathologic studies in uncomplicated HSP (Behan and Maia 1974)
-
1.
Axonal degeneration of selected motor (corticospinal tracts) and sensory (dorsal column fibers) within the spinal cord, particularly prominent in the distal aspects of these fibers
-
2.
Anterior horn cells are generally preserved
-
1.
-
5.
Molecular genetic analysis: uncomplicated, complicated, and full panel gene tests for HSP are clinically available at Invitae, San Francisco, CA (www.invitae.com)
Genetic Counseling
-
1.
Recurrence risk (Fink 2006; Finsterer et al. 2012)
-
1.
Patient’s sib
-
1.
Autosomal dominant inheritance
-
1.
Over 90% of the affected individuals have an affected parent, depending on the penetrance, proportion of de novo mutations, and germinal mosaicism
-
2.
Each child of an affected individual has a 50% chance of inheriting the mutation
-
1.
-
2.
Autosomal recessive inheritance: Each sibling of an affected patient has a 25% chance of being affected, a 50% risk of being an asymptomatic carrier, and a 25% chance of being unaffected and not a carrier
-
3.
X-linked recessive inheritance
-
1.
Mother is a carrier: 50% of brothers are affected and 50% of sisters are carriers
-
2.
Mother is not a carrier: low recurrence risk but still exists since the risk of germline mosaicism in mothers is not known
-
1.
-
4.
X-linked dominant inheritance
-
1.
A carrier mother: a 50% risk of transmitting the disease-causing mutation with each pregnancy. Sons who inherit the mutation will be affected. Daughters who inherit the mutation will be carriers and may or may not be affected
-
2.
A noncarrier mother: recurrence risk to sibs low but not zero since the risk of germline mosaicism in mothers is not known
-
1.
-
1.
-
2.
Patient’s offspring
-
1.
Autosomal dominant inheritance: 50%
-
2.
Autosomal recessive inheritance: not increased unless the spouse is a carrier
-
3.
X-linked recessive inheritance
-
1.
No sons will inherit the mutant allele and therefore will not be affected
-
2.
All daughters will be carriers
-
1.
-
4.
X-linked dominant inheritance
-
1.
All the daughters of an affected male inherit the mutation but may or may not have symptoms
-
2.
None of his sons will be affected
-
1.
-
1.
-
3.
Frequency of spontaneous mutations for dominantly inherited HSP: 12%
-
4.
Genetic penetrance
-
1.
Uncomplicated HSPs: age-dependent and high penetrance (70–85% for SPG4)
-
2.
Incomplete penetrance: reported in SPG4, SPG8, and SPG3A
-
3.
Extent of clinical variability
-
4.
Genetic anticipation (affected individuals in succeeding generations may be more severely affected and develop symptoms at an earlier age): reported in a minority of SPG3A
-
1.
-
1.
-
2.
Prenatal diagnosis for pregnancies at risk is offered by specialized laboratories providing custom prenatal diagnosis to families in which the disease-causing mutation has been identified
-
3.
Management: presently limited to symptomatic reduction of muscle spasticity (Fink 2003)
-
1.
Exercise/daily physical therapy
-
1.
Maintain and improve muscle flexibility and range of motion (stretching exercises)
-
2.
Improve muscle strength (resistance exercise)
-
3.
Maintain walking reflexes (walking on a slowly moving treadmill with arm supports or walking in a swimming pool)
-
4.
Improve cardiovascular fitness
-
5.
Ankle-foot orthotic devices: often useful to reduce toe dragging
-
1.
-
2.
Medications
-
1.
Lioresal (oral or intrathecal)
-
2.
Tizanidine
-
3.
Dantrolene
-
4.
Oxybutynin (helpful in reducing urinary urgency)
-
1.
-
1.
This 8-year-old boy was noted to have unstable gait with frequent falls, and weakness on the upper extremities. On examination, he had ankle clonuses, brisk deep tendon reflexes (DTR), weak grasp, and occasional tip-toe walking. He was receiving special education. Chromosome analysis (46, XY), Fragile X analysis, and brain MRI were normal. The 7-year-old brother had similar but milder symptoms. The father is similarly affected
This 4-year-old girl was evaluated for spastic legs with onset since 3 month of age. On examination, she was noted to have brisk DTR, ankle clonuses, tight Achilles tendon, and tip toe walking. Her mother had spastic legs with brisk DTR, ankle clonuses, and some loss of sensation in her toes. The maternal grandmother had a history of leg weakness and bladder problems with onset in her 30s
References
Abou Jamra, R., Philippe, O., Raas-Rothschild, A., et al. (2011). Adaptor protein complex 4 deficiency causes severe autosomal-recessive intellectual disability, progressive spastic paraplegia, shy character, and short stature. American Journal of Human Genetics, 88, 788–795.
Arnoldi, A., Crimella, C., Tenderini, E., et al. (2012). Clinical phenotype variability in patients with hereditary spastic paraplegia type 5 associated with CYP7B1 mutations. Clinical Genetics, 81, 150–157.
Beetz, C., Johnson, A., Schuh, A. L., et al. (2013). Inhibition of TFG function causes hereditary axon degeneration by impairing endoplasmic reticulum structure. Proceedings of the National Academy of Sciences, 110, 5091–5096.
Behan, W., & Maia, M. (1974). Strumpell’s familial spastic paraplegia: genetics and neuropathology. Journal of Neurology, Neurosurgery, and Psychiatry, 37, 8–20.
Boukhris, A., Feki, I., Elleuch, N., et al. (2010). A new locus (SPG46) maps to 9p21.2-q21.12 in a Tunisian family with a complicated autosomal recessive hereditary spastic paraplegia with mental impairment and thin corpus callosum. Neurogenetics, 11, 441–448.
Boukhris, A., Schule, R., Loureiro, J. L., et al. (2013). Alteration of ganglioside biosynthesis responsible for complex hereditary spastic paraplegia. American Journal of Human Genetics, 93, 118–123.
De Bot, S. T., van de Warrenburg, B. P. C., Kremer, H. P. H., et al. (2010). Child neurology: hereditary spastic paraplegia in children. Neurology, 75, e75–e79.
de Bot, S. T., Vermeer, S., Buijsman, W., et al. (2013). Pure adult-onset spastic paraplegia caused by a novel mutation in the KIAA0196 (SPG8) gene. Journal of Neurology, 260, 1765–1769.
DeMichele, G., DeFusco, M., Cavalcant, I. F., et al. (1998). A new locus for autosomal recessive hereditary spastic paraplegia maps to chromosome 16q24.3. The American Journal of Human Genetics, 63, 135–139.
Dick, K. J., Eckhardt, M., Paisan-Ruiz, C., et al. (2010). Mutation of FA2H underlies a complicated form of hereditary spastic paraplegia (SPG35). Human Mutation, 31, E1251–E1260.
Erlich, Y., Edvardson, S., Hodges, E., et al. (2011). Exome sequencing and disease-network analysis of a single family implicate a mutation in KIF1A in hereditary spastic paraparesis. Genome Research, 21, 658–664.
Esteves, T., Durr, A., Mundwiller, E., et al. (2014). Loss of association of REEP2 with membranes leads to hereditary spastic paraplegia. American Journal of Human Genetics, 94, 268–277.
Fink, J. K. (1997). Advances in hereditary spastic paraplegia. Current Opinion in Neurology, 10, 313–318.
Fink, J. K. (2002). Hereditary spastic paraplegia. In D. Rimoin, R. Pyeritz, J. Connor, & B. Korf (Eds.), Emery & Rimoin’s principles and practice of medical genetics (4th ed., pp. 3124–3145). London: Harcourt Publishers.
Fink, J. K. (2003). Advances in the hereditary spastic paraplegias. Experimental Neurology, 184, S106–S110.
Fink, J. K. (2006). Hereditary spastic paraplegia. Current Neurology and Neuroscience Reports, 6, 65–76.
Fink, J. K. (2013). Hereditary spastic paraplegia: clinic-pathologic features and emerging molecular mechanisms. Acta Neuropathologica, 126, 304–328.
Fink, J. K., & Hedera, P. (1999). Hereditary spastic paraplegia: genetic heterogeneity and genotype-phenotype correlation. Seminars in Neurology, 19, 301–310.
Finsterer, J., Löscher, W., Quasthoff, S., et al. (2012). Hereditary spastic paraplegias with autosomal dominant, recessive, X-linked, or maternal trait of inheritance. Journal of Neurologic Science, 318, 1–18.
Goizet, C., Boukhris, A., Maltete, D., et al. (2009). SPG15 is the second most common cause of hereditary spastic paraplegia with thin corpus callosum. Neurology, 73, 1111–1119.
Harding, A. E. (1983). Classification of the hereditary ataxias and paraplegias. Lancet, 1, 1151–1155.
Kruer, M. C., Paisan-Ruiz, C., Boddaert, N., et al. (2010). Defective FA2H leads to a novel form of neurodegeneration with brain iron accumulation (NBIA). Annals of Neurology, 68, 611–618.
Lin, P., Li, J., Liu, Q., Mao, F., et al. (2008). A missense mutation in SLC33A1, which encodes the acetyl-CoA transporter, causes autosomal-dominant spastic paraplegia (SPG42). American Journal of Human Genetics, 83, 752–759.
Martin, E., Schule, R., Smets, K., et al. (2013). Loss of function of glucocerebrosidase GBA2 is responsible for motor neuron defects in hereditary spastic paraplegia. American Journal of Human Genetics, 92, 238–244.
Montenegro, G., Rebelo, A. P., Connell, J., et al. (2012). Mutations in the ER-shaping protein reticulon 2 cause the axon-degenerative disorder hereditary spastic paraplegia type 12. The Journal of Clinical Investigation, 122, 538–544.
Moreno-De-Luca, A., Helmers, S. L., Mao, H., et al. (2011). Adaptor protein complex-4 (AP-4) deficiency causes a novel autosomal recessive cerebral palsy syndrome with microcephaly and intellectual disability. Journal of Medical Genetics, 48, 141–144.
Novarino, G., Fenstermaker, A. G., Zaki, M. S., et al. (2014). Exome sequencing links corticospinal motor neuron disease to common neurodegenerative disorders. Science, 343, 506–511.
Orthmann-Murphy, J. L., Salsano, E., Abrams, C. K., et al. (2009). Hereditary spastic paraplegia is a novel phenotype for GJA12/GJC2 mutations. Brain, 132(pt 2), 426–438.
Oz-Levi, D., Ben-Zeev, B., Ruzzo, E. K., et al. (2012). Mutation in TECPR2 reveals a role for autophagy in hereditary spastic paraparesis. American Journal of Human Genetics, 91, 1065–1072.
Rainier, S., Bui, M., Mark, E., et al. (2008). Neuropathy target esterase gene mutations cause motor neuron disease. American Journal of Human Genetics, 82, 780–785.
Silver, J. R. (1966). Familial spastic paraplegia with amyotrophy of the hands. Journal of Neurology, Neurosurgery, and Psychiatry, 29, 135–144.
Simpson, M. A., Cross, H., Proukakis, C., et al. (2003). Maspardin is mutated in Mast syndrome, a complicated form of hereditary spastic paraplegia associated with dementia. American Journal of Human Genetics, 73, 1147–1156.
Slabicki, M., Theis, M., Krastev, D. B., et al. (2010). A genome-scale DNA repair RNAi screen identifies SPG48 as a novel gene associated with hereditary spastic paraplegia. PLoS Biology, 8, e1000408.
Shimazaki, H., Takiyama, Y., Ishiura, H., Japan Spastic Paraplegia Research Consortium (JASPAC), et al. (2012). A homozygous mutation of C12orf65 causes spastic paraplegia with optic atrophy and neuropathy (SPG55). Journal of Medical Genetics, 49, 777–784.
Spiegel, R., Mandel, H., Saada, A., et al. (2014). Delineation of C12orf65-related phenotypes: a genotype-phenotype relationship. European Journal of Human Genetics, 22, 1019–1025.
Tesson, C., Nawara, M., Salih, M. A. M., et al. (2012). Alteration of fatty-acid-metabolizing enzymes affects mitochondrial form and function in hereditary spastic paraplegia. American Journal of Human Genetics, 91, 1051–1064.
Verkerk, A. J. M. H., Schot, R., Dumee, B., et al. (2009). Mutation in the AP4M1 gene provides a model for neuroaxonal injury in cerebral palsy. American Journal of Human Genetics, 85, 40–52.
Zivony-Elboum, Y., Westbroek, W., Kfir, N., et al. (2012). A founder mutation in Vps37A causes autosomal recessive complex hereditary spastic paraparesis. Journal of Medical Genetics, 49, 462–472.
Author information
Authors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Science+Business Media LLC
About this entry
Cite this entry
Chen, H. (2017). Hereditary Spastic Paraplegia. In: Atlas of Genetic Diagnosis and Counseling. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-2401-1_272
Download citation
DOI: https://doi.org/10.1007/978-1-4939-2401-1_272
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-2400-4
Online ISBN: 978-1-4939-2401-1
eBook Packages: MedicineReference Module Medicine