Abstract
Obesity is defined as an unhealthy excess of body fat, which increases the risk of morbidity and premature mortality. Obesity is a growing concern among adults. It has not only increased in prevalence, but it has also been associated with significant morbidity and mortality. Some of its medical risks include hypertension, diabetes, hyperlipidemia, coronary artery disease, and osteoarthritis. More so in older adults, obesity exacerbates the age-related decline in physical function, impairs quality of life, and leads to frailty. The current therapeutic and management tools designed for weight management in older persons include lifestyle intervention (diet, physical activity, and behavior modification), pharmacotherapy, and surgery. Current evidence suggests that weight-management strategies in obese older adults improves physical function, quality of life, and reduces medical complications. The treatment must consider the potential adverse effects of weight loss on bone and muscle mass
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Key Points
-
The increasing prevalence of obese older adults is a major public health issue.
-
Obesity causes frailty in older adults by exacerbating the age-related decline in physical function.
-
Treatment plans for obese older adults should include lifestyle interventions such as weight loss, behavior modification, and exercise therapy to improve physical function and quality of life and reduce medical complications associated with obesity.
-
While treatment of obesity may improve a number of health parameters, the potential for adverse effects of weight loss on bone and muscle mass must also be taken into consideration.
Introduction
Obesity is defined as an unhealthy excess of body fat, which increases the risk of morbidity and premature mortality. Obesity is a growing concern among adults. It has not only increased in prevalence, but it has also been associated with significant morbidity and mortality. Some of its medical risks include hypertension, diabetes, hyperlipidemia, coronary artery disease, and osteoarthritis. More so in older adults, obesity exacerbates the age-related decline in physical function, impairs quality of life, and leads to frailty. The current therapeutic and management tools designed for weight management in older persons include lifestyle intervention (diet, physical activity, and behavior modification), pharmacotherapy, and surgery. Current evidence suggests that weight-management strategies in obese older adults improves physical function, quality of life, and reduces medical complications. The treatment must consider the potential adverse effects of weight loss on bone and muscle mass.
This chapter will review the clinical issues related to obesity in older adults and provide health professionals with the appropriate weight-management guidelines on the basis of current evidence.
Obesity: An Epidemic
Obesity among older adults continues to grow in prevalence in the United States. Data from the National Health and Nutrition Examination Survey (NHANES) indicate that approximately one-third of United States adults are obese [1]. Likewise, in developed countries, the prevalence of obesity is increasing among older adults. The underlying reasons for the increased prevalence are an increase in the older person population, and an increase in the percentage of obesity in that population. Past studies have compared point-in-time statistics of the American older adult population and highlighted the increase in prevalence of obesity. For example, in a 10-year period between 1991 and 2000, obesity was found to grow from 14.7 to 22.9 % in the 60–69-year age group, while obesity grew from 11.4 to 15.5 % in the >70-year age group. This represents an increase of 56 and 36 % in the respective age groups [2]. More recent estimates suggest that 37 % of adults 65 years of age or older are obese (Body Mass Index, BMI ≥ 30 kg/m2), and such prevalence is expected to become even more evident with the aging of “baby boomers” [3]. The prevalence of obesity in older adults will continue to challenge our health care systems [4]. Furthermore, obesity poses an increasing problem for long-term care facilities [5]. On a positive note, obesity is less likely to develop in the very old population (>80-year-olds). In this age group, the prevalence rate of obesity is considerably lower than for younger cohorts. The relatively low prevalence of obesity after 80 years of age could be due to the survival advantage of being lean [6]. Nonetheless, overall, more than 15 % of the older American population is obese, and obesity is more common in older women than in men [2]. Moreover, concern about the prevalence of geriatric obesity is not contained to the United States. It is an increasing problem of older populations throughout the world [7].
Pathophysiology of Obesity
Aging is associated with marked changes in body composition. After 30 years of age, fat-free mass (FFM), which is comprised predominantly of muscle, progressively decreases, whereas fat mass increases. FFM reaches its peak during the third decade of life, while fat mass (FM) reaches its peak during the seventh decade [8]. Subsequently, after about age 70, both indices (FFM and fat mass) decrease. Aside from quantitative changes of FFM and fat mass, aging is also associated with a redistribution of body fat and FFM. The intra-abdominal fat increases, while the subcutaneous fat and total body fat decrease [9].
Body fat is accumulated when energy input exceeds energy expenditure. The intake of energy does not change or may even decline with aging. Energy output comprises the resting metabolic rate (accounts for ~70 %), the thermal effect of food (~10 %), and physical activity (20 %). Aging is associated with a decrease in all major components of energy output. Resting metabolic rate decreases by 3 % every decade after 20 years of age. About three-fourths of this decline can be accounted for by a loss in FFM [10]. The thermal effect of food is 20 % lower in older men than in younger men [11]. Physical activity decreases with increasing age, and it accounts for about one-half of the decrease in energy output that occurs with aging [12].
As one ages, the growth hormone and testosterone production decreases, which results in a reduction in FFM and increased accumulation of fat mass [13]. Thyroid hormone-induced oxidative bursts are decreased with aging. Changes in neurohumoral modulators of appetite and body composition such as leptin and ghrelin have also been implicated as causes of obesity in later life. Resistance to leptin could result in a diminished ability to downregulate appetite [14]. These changes in hormone levels with aging could play an important role in the pathogenesis of obesity.
Measuring Overweight and Obesity
It is difficult to accurately measure body fat mass in most clinical settings because such assessments require the use of sophisticated technologies that are not readily available. Two measures for assessing overweight and total body fat content are widely used and accepted as simple methods to classify medical risk with regards to body fat; they are the body mass index (BMI) and waist circumference.
Body Mass Index
BMI is calculated as weight (kg)/height squared (m2). The BMI is used to assess overweight and obesity and to monitor changes in body weight status. It allows meaningful comparisons of weight status within and between populations. However, in older adults, age-related changes in body composition and loss of height caused by compression of vertebral bodies and kyphosis alter the relationship between BMI and percentage body fat. Therefore, at any given BMI value, changes in body composition tend to underestimate fatness, whereas the loss of height would tend to overestimate fatness.
Waist Circumference
The presence of excess fat in the abdomen out of proportion to total body fat is an independent predictor of comorbidities such as cardiovascular disease, diabetes, and hypertension [15]. Men with a waist circumference of >40 in. and women with a waist circumference of >35 in. are considered to have increased disease risk.
Table 10.1 incorporates both BMI and waist circumference in the classification of overweight and obesity and provides an indication of relative disease risk [16].
Health Implications of Obesity
Adverse Effects of Obesity
Obesity is associated with a number of health hazards. Some adverse effects include increased mortality, health complications, poor quality of life, and disability. These hazards are discussed in detail below.
Mortality
Obesity was associated with significantly higher all-cause mortality relative to the normal weight BMI in both younger and older adults [17]. Although the relative risk of death associated with obesity is greater for younger adults than for older ones [18, 19], a high BMI increases absolute mortality and health risks linearly up to 75 years of age [20]. That is, from a clinical standpoint, the health complications associated with obesity increase linearly with increasing BMI until the age of 75. The relationship of obesity in >75 years of age with total mortality is unclear. Some previous epidemiological studies do not show that excess body weight is detrimental to mortality in advancing age [21, 22]. However, underlying diseases that can themselves increase the risk of early mortality may cause the underestimation of the relation between obesity and mortality in older adults. Since those who are susceptible to the effects of obesity die at a younger age, the surviving group of obese older adults are said to be the “resistant” survivors. Furthermore, waist circumference, an indicator of central adiposity, is identified as a potentially good risk factor for mortality in obese elderly adults [23].
Comorbid Disease
Obesity and increased visceral fat are associated with increased morbidity and poor quality of life. Most studies evaluating obesity-related complications focus on middle-aged and younger adults. The prevalence of the medical complications associated with obesity, such as hypertension, diabetes, cardiovascular disease, and osteoarthritis, increases with age. Therefore, obesity and weight gain during middle age may contribute to medical complications and development of obesity-associated chronic disease, and subsequent increased health care expenditures that occur during old age [24].
Metabolic Abnormalities
There is an age-related increase in the prevalence of all of the components of the metabolic syndrome. Relative to those who are 20–34 years of age, the odds of having metabolic syndrome for those who are over 65 years of age were reported to be 5.8 in men and 4.9 in women [25]. Additionally, increased abdominal fat is independently associated with metabolic syndrome in adults aged 70–79 years [26]. Fasting plasma glucose increases by 1–2 mg/dL and postprandial glucose by 10–20 mg/dL for each decade of age after 30 years. Accordingly, the prevalence of type 2 diabetes mellitus based on standard criteria is highest in older persons [27]. The age-related increase in fat and, more importantly, visceral fat, could be the main causative factor for the increased prevalence of diabetes mellitus and insulin resistance in the elderly. At the age of 65, there is a strong influence of BMI on the remaining lifetime risk of diabetes, with the increased risk ranging from ~3 % with BMI < 18.5 kg/m2, 10 % with BMI 18.5–25 kg/m2, 14 % with BMI 25–30 kg/m2, 29 % with BMI 30–35 kg/m2 and 35 % with BMI ≥ 35 kg/m2 [28].
Hypertension is extremely prevalent in the older population, affecting 65 % of all persons aged >60 years [29]. Obesity and high blood pressure continue to be correlated, even in old age [30]. Obesity-related dyslipidemia (i.e., low HDL cholesterol and high serum triglyceride concentrations) is seen in both younger and older adults. In the United States, 35–42 % of white men and women who are over 65 years of age with metabolic syndrome have low HDL cholesterol (<40 mg/dL in men and <50 mg/dL in women) and high triglyceride (>150 mg/dL) concentrations [25]. Data from longitudinal studies suggest that obesity increases the risk of cardiovascular disease in older men. Elevated BMI in older 70-year-old men and women was associated with an increase in new cases of coronary artery disease, fatal and nonfatal myocardial infarction, and cardiovascular disease mortality during 12–15 years of observation [31] in older men but not in older women.
Arthritis
Osteoarthritis (OA) is the most common type of arthritis and its prevalence increases progressively with age in both sexes in parallel with the increase in body weight and fat observed with aging. The age-related increase in prevalence of OA presumably reflects bodily changes as a result of a lifetime of being overweight, which results in chronic mechanical strain on weight-bearing joints [32, 33]. In a population-based study of older adults, with a mean age of 73, the relative risk of developing knee OA increased from 0.1 for a BMI lower than 20 kg/m2 to 13.6 for a BMI of 36 kg/m2 or higher [34].
Pulmonary Abnormalities
Obesity is associated with obstructive sleep apnea (OSA), obesity-hypoventilation syndrome, and pulmonary function abnormalities [35]. Increased fat on the chest wall decreases lung compliance, increases the work of breathing, and reduces ventilation [36]. The prevalence of OSA increases with age. Both waist circumference and waist changes were the most powerful predictors of OSA in older obese and normal-weight men in a 30-year follow-up study [37].
Urinary Incontinence
The prevalence of urinary incontinence increases after the age of 65 and affects 15–30 % of that population. Obesity further exacerbates the high prevalence of urinary incontinence in older adults, which has been shown to be directly associated with elevated BMI [38, 39].
Cancer
Obesity is a risk factor for several types of cancer, including breast, colon, gallbladder, pancreas, and bladder amongst both men and women, more so in older than younger adults [40]. A study in older women has shown that breast cancer occurs more frequently in obese older women than all older women [40]. Obese postmenopausal women are also at higher risk of developing malignant melanoma and endometrial cancer than their nonobese counterparts [41].
Functional Impairment and Quality of Life
Aging causes a progressive decline in physical function because of a continued decline in muscle mass, strength, and power, and an increase in joint instability and arthritis [42]. These functional impairments affect activities of daily living, decrease quality of life, and lead to an increased utilization of health care services. Obesity has important functional implications in older adults because it worsens their age-related decline in physical function. Data from both cross-sectional [43–45] and longitudinal studies [46–48] have consistently demonstrated a strong link between increasing BMI and worsening physical function in older persons. High BMI is associated with self-reported impairment in ADLs, limitations in mobility, decreased physical performance, and increased risk for functional decline [45–50]. Moreover, obesity is associated with increasing nursing home admissions [51, 52].
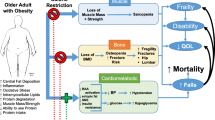
Although obesity is associated with increases in FM, aging is associated with a decline in FFM (primarily skeletal muscle) and function, referred to as sarcopenia [53] and obesity does not appear to protect against sarcopenia. In one study [54], the prevalence of sarcopenia in obese persons increased with age, suggesting that many obese persons maintain a constant fat mass while losing muscle mass. In another study [55], obese older adults were found to have sarcopenia based on lower relative muscle mass and low muscle strength per muscle area (low muscle quality, Fig. 10.1), despite having more than adequate body weight, which is opposite of the stereotypical frail older adult. Their functional performance, aerobic capacity, strength, balance, and walking speed were as severely reduced as the frail nonobese adults [55]. Thus, obesity in older adults acts synergistically with sarcopenia (sarcopenic obesity; see also Chap. 6) to augment disability. Accordingly, the “sarcopenic-obese” individual has two problems that lead to frailty: (1) decreased muscle mass and strength, which occur with aging, and (2) a need to carry greater weight due to excess body fat [55, 56]. Figure 10.2 is a cross-sectional MRI image from the mid-thigh in a frail obese older adult. This figure demonstrates the excessive adipose tissue infiltration of skeletal muscle mass with obesity.
Muscle quality (strength per muscle mass) in nonobese nonfrail, nonobese frail, and obese elderly subjects. Reprinted by permission from Macmillan Publishers Ltd: Obesity. Villareal DT, Banks M, Siener C, Sinacore DR, Klein S. Physical frailty and body composition in obese elderly men and women, 12(6), copyright 2004
In one study [55], 96 % of community-living older adults with BMIs >30 were frail, as determined by physical performance test scores [57], peak oxygen consumption [58], and self-reported ability to perform activities of daily living [59]. Data from another study [60] also demonstrated that obesity was associated with a marked increased risk of frailty (odds ratio = 3.5), determined by weakness, slowness, weight loss, low physical activity, and exhaustion. In another study [61] obesity was identified as one of the five modifiable risk factors that predict functional decline in both vigorous and basic activities among older women. Recently in a study of community dwelling older adults, frailty was related to BMI in a U-shaped manner (i.e., increased frailty in people with extremes of low or high BMI). However, in people with large WC (≥35 in. in women and ≥40 in. in men), frailty was shown to exist in all BMI categories [62].
Beneficial Effects of Obesity
Increased body weight is associated with increased bone mineral density (BMD) and decreased osteoporosis and hip fracture in older men and women, whereas the converse is true for being of low body weight. Both body fat mass and FFM are directly correlated with BMD. Although the increase in BMD has been attributed to mechanical stress on the weight-bearing skeleton, the protective effects have also been observed in non-weight-bearing bones [63]. Therefore, hormonal factors that are increased in obese persons, such as circulating estrogens, insulin, and leptin, might contribute to the osteoprotective effects of obesity, by stimulating bone formation and inhibiting bone resorption. The increase in both BMD and the extra cushioning effect of the fat surrounding crucial areas such as the hip might provide protection against hip fracture during a fall in obese older adults [64]. On the other hand, recent studies also suggest that excess adiposity could be detrimental to bone and also increases fall risk [65, 66].
Effects of Intentional Weight Loss in Older Adults
Body Composition
Loss of body weight is accompanied by a decrease in both FM and FFM. Therefore, it is possible that weight loss in obese older persons could increase sarcopenia by worsening the age-related loss of muscle mass. In younger adults, ~75 % of diet-induced weight loss is composed of fat tissue and ~25 % is composed of FFM [67]. The relative amount of diet-induced weight loss as FFM and fat mass in older men and women is similar to that observed in younger adults [68]. Therefore, diet-induced weight loss does not produce a disproportionate loss of lean tissue in old persons. Despite much evidence linking high body fat to functional disability [45, 47, 48], weight loss has not been typically instituted in obese older persons because of the fear that it will exacerbate sarcopenia. Additionally, it is a general belief among many geriatricians that some “reserve” of body fat is advantageous in the older people particularly if they are hospitalized [69].
In a randomized controlled trial conducted in obese older subjects, there was no significant difference in loss of FFM after a diet-induced weight loss plus regular exercise compared with the control group who did not lose weight. These encouraging findings suggest that regular exercise can attenuate a diet-induced loss of FFM in older persons [70].
Medical Complications
Data from young and middle-aged adults show that weight loss improves or normalizes metabolic abnormalities associated with obesity. Similarly, it has been shown that moderate weight loss in obese older adults simultaneously decreases an array of metabolic coronary heart disease risk factors [71].
Physical Function and Quality of Life
Moderate weight loss in conjunction with physical activity improves physical function and health-related quality of life in obese older persons. Data from studies conducted in overweight and obese older persons with or without joint disease have shown that the combination of moderate diet-induced weight loss and exercise therapy improved both subjective and objective measures of physical function and health-related quality of life and had a greater beneficial effect than did either diet or exercise interventions alone [70, 72–74]. These findings suggest that obesity is a reversible cause of frailty and impaired quality of life in older adults.
Recently, in a 1-year randomized controlled clinical trial, 107 obese adults aged 65 years and older were recruited to investigate the independent and combined effects of weight loss and exercise on physical function, body composition, and quality of life [75]. Participants were randomized into a weight management program, exercise training program, weight management plus exercise training program, and a control group. The weight management program consisted of a balanced diet producing an energy deficit of 500–750 kcal/day in participants’ daily requirements. The exercise intervention included both aerobic and resistance training components. Results demonstrated that while physical function improved in all of the intervention groups compared to the control group, the group simultaneously adopting the weight management and exercise training programs demonstrated a significantly higher physical function compared to the other interventions. Moreover, the group that received the combined intervention also tended to demonstrate more benefits in terms of reduced loss of lean body mass and bone mineral density, as well as improved aerobic capacity, strength, balance, and gait speed. These findings suggest that the combination of weight loss and exercise programs is more effective at preventing frailty and preserving quality of life for obese older adults compared to interventions focused on one single modality.
In this context, it is important to underline that the combination of weight loss and exercise programs is safe, and the exercise benefits may effectively compensate the reduction of lean mass due to the weight loss program [76] (see also Chap. 22). Further studies are needed to determine whether weight loss can be maintained beyond 1 year and may be able to prevent major health-related outcomes (including mortality and nursing home admissions) in obese older adults. These studies should focus on evaluating whether long-term weight maintenance is likely to produce the most meaningful changes in health outcomes in obese older adults.
Mortality
It has been observed in several population-based studies that community-dwelling older adults who lost weight, or who experienced weight variability, had an increased relative mortality risk compared with those who were weight stable [37].
However, most studies have inherent weaknesses, such as not reporting whether the observed weight changes were intentional or unintentional, relying upon self-reported weight change, or not distinguishing between weight loss in obese and lean subjects. Moreover, a recent randomized controlled clinical trial demonstrated that intentional dietary weight loss was not significantly associated with increased all-cause mortality over 12-year of follow-up in older overweight or obese adults [77].
Bone Mineral Density
Weight loss can have adverse effects on bone mass. Previous interventional studies conducted in young and middle-aged adults reported that weight loss causes bone loss that may be proportional to the amount of weight loss [78–80]. However, it is not known whether the bone loss associated with intentional weight loss increases the risk of osteoporotic fractures in obese persons. One study showed that diet-induced weight loss, but not exercise-induced weight loss, is associated with reductions in BMD at weight-bearing sites, suggesting that exercise should be an important component of a weight-loss program to offset adverse effects of diet-induced weight loss on bone [81]. In a more recent study, regular exercise was able to attenuate weight-loss-induced bone loss [76]. It is thought that this beneficial effect may be specific for sites involved in weight-bearing exercise [82], mediated by prevention of weight-loss-induced increase in sclerostin (Sclerostin is a secreted Wnt antagonist that inhibits osteoblastic proliferation and differentiation, thus reducing bone formation, an inhibitor of bone formation secreted by osteocytes) [83]. Therefore, including exercise as part of a weight-loss program is particularly important in older persons to reduce bone loss.
Interventions and Treatment
Weight loss in obese persons of any age can improve obesity-related medical complications, physical function, and quality of life. In older adults, improving physical function and quality of life may be the most important goals of therapy. The current therapeutic tools and recommendations available for weight management in older persons are (1) lifestyle intervention involving diet, physical activity, and behavior modification; (2) pharmacotherapy; and (3) surgery.
Weight Management Intervention
Weight management intervention is just as effective in older as in younger subjects [70, 72–74]. The combination of an energy-deficit producing diet, increased physical activity, and behavior therapy causes moderate weight loss and is associated with a lower risk of treatment-induced complications. Weight-management therapy that minimizes muscle and bone losses is recommended for older adults who are obese and who have functional impairments or metabolic complications that can benefit from weight loss.
Diet Therapy
In order for weight loss to be successful, an energy deficit must be achieved. A low-calorie diet that reduces energy intake by 500–750 kcal/day results in a weight loss of 0.4–0.9 kg (about 1–2 lb)/week and a weight loss of 8–10 % by 6 months. The diet should contain 1.0 g/kg high-quality protein/day [70], and multivitamin, and mineral supplements to ensure that all daily recommended requirements are met, including daily intakes of 1,500 mg calcium and 1,000 IU vitamin D to prevent bone loss. Very low-calorie diets (<800 kcal/day) should be avoided because of an increased risk of medical complications. Also, depending on the patient’s cardiovascular risk status, the diet therapy should be consistent with the National Cholesterol Education Program Expert Panel (Adult Treatment Panel III)’s Therapeutic Lifestyle Changes Diet and or possibly the Dietary Approaches to Stop Hypertension (DASH diet) [84].
Referral to a registered dietitian, who has weight-management experience, is often necessary to ensure that appropriate nutritional counseling is provided. Patients should be educated on food composition, preparation, and portion control and their food preferences should be supported to improve compliance.
Successful weight loss and maintenance program should be based on a sound scientific rationale. The program should be safe and nutritionally adequate, as well as practical and applicable to patient’s social and ethnic background.
Physical Activity
Introducing an exercise component early in the treatment course can improve physical function and can ameliorate frailty in the older adult [70]. The exercise program should be individualized according to a person’s medical conditions and disability (again, see Chap. 22). The program should start at a low-to-moderate intensity, duration, and frequency to promote adherence and avoid musculoskeletal injuries. If possible, the program should be gradually progressed over a period of several weeks or months to a longer, more frequent, and more vigorous effort. The goals of regular exercise in obese older persons are to increase flexibility, endurance, and strength; therefore, a multicomponent exercise program that includes stretching, aerobic activity, and strength exercises is recommended. Even very old or frail persons can participate in these types of physical activities.
Behavior Modification
Clinicians should help obese older adults set personal goals, monitor progress, and use motivational strategies to improve adherence to the weight-loss program (see also Chap. 1). The cognitive behavioral therapy strategies that should be considered include goal setting, self-monitoring, social support, stimulus control techniques, and problem-solving skills. Lifestyle and behavior modification can be facilitated by counseling from a behavioral therapist, exercise specialist, or dietitian who has weight-management experience.
Implementation of changes in the diet and activity habits of older adults may be challenging. An increased burden of disease, adverse quality of life, depression, hearing and visual difficulties, and cognitive dysfunction may make it difficult to change one’s lifestyle. This increase in chronic disabilities with aging reduces physical activity and exercise capacity. Common geriatric situations, such as depression, cognitive impairment, dependency on others, institutionalization, widowhood, loneliness, and isolation should be addressed, because these factors can make it more difficult to adopt or adhere to lifestyle changes designed to lose weight. Lifestyle-change programs should also encourage participation by family members and care providers for better compliance.
Pharmacotherapy
Since most clinical trials that evaluate the use of pharmacotherapy excluded older adults or included only a small number of older adults, the available data are insufficient to determine the efficacy and safety of pharmacotherapy in this population.
The use of pharmacological agents to treat obesity can add an additional burden on older persons. Many obese older patients are already taking multiple medications for other diseases, which can increase the chances of nonadherence, drug–drug interactions, and errors with obesity pharmacotherapy.
Moreover, potential side effects can have more serious consequences in older adults. Some examples of weight loss drugs that are FDA approved include phenteramine, orlistat, and a recently approved drug Qysmia (combination of phentermine and topiramate extended-release). These drugs are seldom covered by health insurance or Medicare, which can add an additional financial burden in older patients who have a fixed income. A thorough review of all the medications should be conducted for older adults who are obese, because some medications may cause weight gain (e.g., antipsychotic, antidepressants, anticonvulsants, or steroids). Furthermore, weight- loss-induced clinical improvements might require changes in medications to avoid iatrogenic complications.
Weight-Loss Surgery
A few studies have provided information on the effectiveness and safety of bariatric surgery among older adults. Data from case series that evaluate the effect of bariatric surgery in patients who are over 60 years of age suggest that the relative weight loss and improvement in obesity-related medical complications are lower, whereas the perioperative morbidity and mortality are greater, in older compared to younger patients [85]. However, bariatric surgery can result in considerable weight loss and marked improvements in obesity-related physical impairment and medical complications in the older patients such as reversal of diabetes. The laparoscopic-adjustable gastric band is associated with fewer serious complications and a lower mortality rate; therefore the gastric band may be a better choice than the Roux-en-Y gastric bypass for older patients. However, it should be emphasized that the efficacy and safety of these procedures have not been compared in randomized trials in older adults. Therefore, careful patient selection, intensive preoperative education, and expert operative and perioperative management are advised. Surgery should be considered in selected older adults who have disabling obesity that can be ameliorated with weight loss and who meet the criteria for surgery. The preoperative evaluation should include an assessment for depression, which is common amongst older adults and could influence outcome. Postoperative management should include monitoring for nutritional and metabolic problems; particularly, vitamin B12 deficiency, iron deficiency, and osteoporosis.
Conclusion
The increasing prevalence of obese older adults is a major public health issue. Decreased muscle mass with aging and the burden of extra body mass due to obesity make it particularly difficult for obese older adults to function independently and may lead to the secondary complication of frailty. Treatment plans for obese older adults should include comprehensive lifestyle interventions such as dietary changes that promote weight loss, behavior modification, and exercise therapy to improve physical function, quality of life, and the medical complications associated with obesity. Finally, the treatment must consider the potential adverse effects of weight loss on bone and muscle mass, as well as physical function and quality of life. Randomized controlled trials to determine health benefits and risks from long-term weight management in obese older adults are necessary.
Clinical Recommendations for Older Adult Weight-loss Therapy
-
1.
Initial assessment
-
A thorough medical history, physical examination, appropriate laboratory tests, and review of medications should be conducted to assess the patient’s current health and comorbidity risks.
-
Additional information such as the patient’s readiness to lose weight, previous attempts at weight loss, and current lifestyle habits should be collected before initiating weight-loss therapy.
-
Clinicians should help obese older adults set their personal goals and welcome participation by family members and care providers.
-
Clinicians should individualize the weight-loss plan after taking into account the special needs of this population.
-
-
2.
Diet therapy
-
Advocate a modest reduction in energy intake (500–750 kcal/day) containing 1.0 g/kg high-quality protein/day, multivitamin, and mineral supplements (including 1,500 mg calcium and 1,000 IU vitamin D/day).
-
Consider referrals to a registered dietitian for appropriate nutritional counseling and education.
-
-
3.
Behavior therapy
-
Behavior therapy should highlight both diet and exercise—the integral parts of weight loss therapy and weight maintenance. The self-monitoring of nutrient intake and better understanding of physical activity accomplishes this task.
-
Consider referring to a behavioral therapist for counseling.
-
Stress management, stimulus control, problem solving, contingency management, and social support should be addressed.
-
-
4.
Exercise therapy
-
Clinicians should assess the need for stress test before any physical activity.
-
Advocate an exercise program that is gradual, individualized, and monitored.
-
A multicomponent exercise program including stretching, aerobic activity, and strength exercises is recommended.
-
-
5.
Additional recommendations
-
Advocate a combination of energy deficit–producing diet, increased physical activity, and behavior therapy. Such combinations are associated with the low risk of treatment-induced complications.
-
Bariatric surgery may be an option for patients who have failed multiple weight-loss attempts.
-
Weight maintenance efforts should be implemented once weight-loss goals have been achieved.
-
References
Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999-2000. JAMA. 2002;288(14):1723–7.
Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. JAMA. 2001;286(10):1195–200.
Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010;303(3):235–41.
Arterburn DE, Crane PK, Sullivan SD. The coming epidemic of obesity in elderly Americans. J Am Geriatr Soc. 2004;52(11):1907–12.
Lapane KL, Resnik L. Obesity in nursing homes: an escalating problem. J Am Geriatr Soc. 2005;53(8):1386–91.
Wallace JI, Schwartz RS. Involuntary weight loss in elderly outpatients: recognition, etiologies, and treatment. Clin Geriatr Med. 1997;13(4):717–35.
Kopelman PG. Obesity as a medical problem. Nature. 2000;404(6778):635–43.
Gallagher D, Visser M, De Meersman RE, Sepulveda D, Baumgartner RN, Pierson RN, et al. Appendicular skeletal muscle mass: effects of age, gender, and ethnicity. J Appl Physiol. 1997;83(1):229–39.
Beaufrere B, Morio B. Fat and protein redistribution with aging: metabolic considerations. Eur J Clin Nutr. 2000;54 Suppl 3:S48–53.
Tzankoff SP, Norris AH. Effect of muscle mass decrease on age-related BMR changes. J Appl Physiol. 1977;43(6):1001–6.
Schwartz RS, Jaeger LF, Veith RC. The thermic effect of feeding in older men: the importance of the sympathetic nervous system. Metabolism. 1990;39(7):733–7.
Elia M, Ritz P, Stubbs RJ. Total energy expenditure in the elderly. Eur J Clin Nutr. 2000;54 Suppl 3:S92–103.
Schwartz RS. Trophic factor supplementation: effect on the age-associated changes in body composition. J Gerontol A Biol Sci Med Sci 1995;50 Spec No: 151–6.
Enriori PJ, Evans AE, Sinnayah P, Cowley MA. Leptin resistance and obesity. Obesity (Silver Spring). 2006;14 Suppl 5:254S–8.
Kissebah AH, Krakower GR. Regional adiposity and morbidity. Physiol Rev. 1994;74(4):761–811.
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 2000; 894: i-253.
Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309(1):71–82.
Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA. 2007;298(17):2028–37.
Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath Jr CW. Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341(15):1097–105.
Villareal DT, Apovian CM, Kushner RF, Klein S. Obesity in older adults: technical review and position statement of the American Society for Nutrition and NAASO, The Obesity Society. Am J Clin Nutr. 2005;82(5):923–34.
Troiano RP, Frongillo Jr EA, Sobal J, Levitsky DA. The relationship between body weight and mortality: a quantitative analysis of combined information from existing studies. Int J Obes Relat Metab Disord. 1996;20(1):63–75.
Allison DB, Gallagher D, Heo M, Pi-Sunyer FX, Heymsfield SB. Body mass index and all-cause mortality among people age 70 and over: the Longitudinal Study of Aging. Int J Obes Relat Metab Disord. 1997;21(6):424–31.
Donini LM, Savina C, Gennaro E, De Felice MR, Rosano A, Pandolfo MM, et al. A systematic review of the literature concerning the relationship between obesity and mortality in the elderly. J Nutr Health Aging. 2012;16(1):89–98.
Daviglus ML, Liu K, Yan LL, Pirzada A, Manheim L, Manning W, et al. Relation of body mass index in young adulthood and middle age to Medicare expenditures in older age. JAMA. 2004;292(22):2743–9.
Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB. The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988-1994. Arch Intern Med. 2003;163(4):427–36.
Goodpaster BH, Krishnaswami S, Harris TB, Katsiaras A, Kritchevsky SB, Simonsick EM, et al. Obesity, regional body fat distribution, and the metabolic syndrome in older men and women. Arch Intern Med. 2005;165(7):777–83.
Kahn SE, Schwartz RS, Porte Jr D, Abrass IB. The glucose intolerance of aging. Implications for intervention. Hosp Pract. 1991;26(4A):29–38.
Narayan KM, Boyle JP, Thompson TJ, Gregg EW, Williamson DF. Effect of BMI on lifetime risk for diabetes in the U.S. Diabetes Care. 2007;30(6):1562–6.
Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988-2000. JAMA. 2003;290(2):199–206.
Masaki KH, Curb JD, Chiu D, Petrovitch H, Rodriguez BL. Association of body mass index with blood pressure in elderly Japanese American men. The Honolulu Heart Program. Hypertension. 1997;29(2):673–7.
Dey DK, Lissner L. Obesity in 70-year-old subjects as a risk factor for 15-year coronary heart disease incidence. Obes Res. 2003;11(7):817–27.
Badley EM, Ansari H. Arthritis and arthritis-attributable activity limitations in the United States and Canada: a cross-border comparison. Arthritis Care Res (Hoboken). 2010;62(3):308–15.
Al SS, Graham JE, Kuo YF, Goodwin JS, Markides KS, Ottenbacher KJ. Obesity and disability: relation among older adults living in Latin America and the Caribbean. Am J Epidemiol. 2010;171(12):1282–8.
Coggon D, Reading I, Croft P, McLaren M, Barrett D, Cooper C. Knee osteoarthritis and obesity. Int J Obes Relat Metab Disord. 2001;25(5):622–7.
Lazarus R, Sparrow D, Weiss ST. Effects of obesity and fat distribution on ventilatory function: the normative aging study. Chest. 1997;111(4):891–8.
Franssen FM, O’Donnell DE, Goossens GH, Blaak EE, Schols AM. Obesity and the lung: 5. Obesity and COPD. Thorax. 2008;63(12):1110–7.
Carmelli D, Swan GE, Bliwise DL. Relationship of 30-year changes in obesity to sleep-disordered breathing in the Western Collaborative Group Study. Obes Res. 2000;8(9):632–7.
Brown JS, Seeley DG, Fong J, Black DM, Ensrud KE, Grady D. Urinary incontinence in older women: who is at risk? Study of Osteoporotic Fractures Research Group. Obstet Gynecol. 1996;87(5 Pt 1):715–21.
Hunskaar S. A systematic review of overweight and obesity as risk factors and targets for clinical intervention for urinary incontinence in women. Neurourol Urodyn. 2008;27(8):749–57.
Wolk A, Gridley G, Svensson M, Nyren O, McLaughlin JK, Fraumeni JF, et al. A prospective study of obesity and cancer risk (Sweden). Cancer Causes Control. 2001;12(1):13–21.
Reeves GK, Pirie K, Beral V, Green J, Spencer E, Bull D. Cancer incidence and mortality in relation to body mass index in the Million Women Study: cohort study. BMJ. 2007;335(7630):1134.
Jordan JM, Luta G, Renner JB, Linder GF, Dragomir A, Hochberg MC, et al. Self-reported functional status in osteoarthritis of the knee in a rural southern community: the role of sociodemographic factors, obesity, and knee pain. Arthritis Care Res. 1996;9(4):273–8.
Apovian CM, Frey CM, Rogers JZ, McDermott EA, Jensen GL. Body mass index and physical function in obese older women. J Am Geriatr Soc. 1996;44(12):1487–8.
Himes CL. Obesity, disease, and functional limitation in later life. Demography. 2000;37(1):73–82.
Davison KK, Ford ES, Cogswell ME, Dietz WH. Percentage of body fat and body mass index are associated with mobility limitations in people aged 70 and older from NHANES III. J Am Geriatr Soc. 2002;50(11):1802–9.
Jensen GL, Friedmann JM. Obesity is associated with functional decline in community-dwelling rural older persons. J Am Geriatr Soc. 2002;50(5):918–23.
Launer LJ, Harris T, Rumpel C, Madans J. Body mass index, weight change, and risk of mobility disability in middle-aged and older women. The epidemiologic follow-up study of NHANES I. JAMA. 1994;271(14):1093–8.
Galanos AN, Pieper CF, Cornoni-Huntley JC, Bales CW, Fillenbaum GG. Nutrition and function: is there a relationship between body mass index and the functional capabilities of community-dwelling elderly? J Am Geriatr Soc. 1994;42(4):368–73.
Jenkins KR. Obesity’s effects on the onset of functional impairment among older adults. Gerontologist. 2004;44(2):206–16.
Rolland Y, Lauwers-Cances V, Cristini C, van Abellan KG, Janssen I, Morley JE, et al. Difficulties with physical function associated with obesity, sarcopenia, and sarcopenic-obesity in community-dwelling elderly women: the EPIDOS (EPIDemiologie de l’OSteoporose) Study. Am J Clin Nutr. 2009;89(6):1895–900.
Zizza CA, Herring A, Stevens J, Popkin BM. Obesity affects nursing-care facility admission among whites but not blacks. Obes Res. 2002;10(8):816–23.
Yang Y, Brown CJ, Burgio KL, Kilgore ML, Ritchie CS, Roth DL, et al. Undernutrition at baseline and health services utilization and mortality over a 1-year period in older adults receiving Medicare home health services. J Am Med Dir Assoc. 2011;12(4):287–94.
Roubenoff R. Sarcopenia: effects on body composition and function. J Gerontol A Biol Sci Med Sci. 2003;58(11):1012–7.
Baumgartner RN. Body composition in healthy aging. Ann N Y Acad Sci. 2000;904:437–48.
Villareal DT, Banks M, Siener C, Sinacore DR, Klein S. Physical frailty and body composition in obese elderly men and women. Obes Res. 2004;12(6):913–20.
Roubenoff R. Sarcopenic obesity: the confluence of two epidemics. Obes Res. 2004;12(6):887–8.
Brown M, Sinacore DR, Binder EF, Kohrt WM. Physical and performance measures for the identification of mild to moderate frailty. J Gerontol A Biol Sci Med Sci. 2000;55(6):M350–5.
Holloszy JO, Kohrt WM. Handbook of physiology - aging. London: Oxford University Press; 1995.
Jette AM, Cleary PD. Functional disability assessment. Phys Ther. 1987;67(12):1854–9.
Blaum CS, Xue QL, Michelon E, Semba RD, Fried LP. The association between obesity and the frailty syndrome in older women: the women’s health and aging studies. J Am Geriatr Soc. 2005;53(6):927–34.
Sarkisian CA, Liu H, Gutierrez PR, Seeley DG, Cummings SR, Mangione CM. Modifiable risk factors predict functional decline among older women: a prospectively validated clinical prediction tool. The Study of Osteoporotic Fractures Research Group. J Am Geriatr Soc. 2000;48(2):170–8.
Hubbard RE, Lang IA, Llewellyn DJ, Rockwood K. Frailty, body mass index, and abdominal obesity in older people. J Gerontol A Biol Sci Med Sci. 2010;65(4):377–81.
Reid IR, Cornish J, Baldock PA. Nutrition-related peptides and bone homeostasis. J Bone Miner Res. 2006;21(4):495–500.
Schott AM, Cormier C, Hans D, Favier F, Hausherr E, Dargent-Molina P, et al. How hip and whole-body bone mineral density predict hip fracture in elderly women: the EPIDOS Prospective Study. Osteoporos Int. 1998;8(3):247–54.
Nielson CM, Marshall LM, Adams AL, LeBlanc ES, Cawthon PM, Ensrud K, et al. BMI and fracture risk in older men: the osteoporotic fractures in men study (MrOS). J Bone Miner Res. 2011;26(3):496–502.
Himes CL, Reynolds SL. Effect of obesity on falls, injury, and disability. J Am Geriatr Soc. 2012;60(1):124–9.
Garrow JS, Summerbell CD. Meta-analysis: effect of exercise, with or without dieting, on the body composition of overweight subjects. Eur J Clin Nutr. 1995;49(1):1–10.
Gallagher D, Kovera AJ, Clay-Williams G, Agin D, Leone P, Albu J, et al. Weight loss in postmenopausal obesity: no adverse alterations in body composition and protein metabolism. Am J Physiol Endocrinol Metab. 2000;279(1):E124–31.
Inelmen EM, Sergi G, Coin A, Miotto F, Peruzza S, Enzi G. Can obesity be a risk factor in elderly people? Obes Rev. 2003;4(3):147–55.
Villareal DT, Banks M, Sinacore DR, Siener C, Klein S. Effect of weight loss and exercise on frailty in obese older adults. Arch Intern Med. 2006;166(8):860–6.
Villareal DT, Miller III BV, Banks M, Fontana L, Sinacore DR, Klein S. Effect of lifestyle intervention on metabolic coronary heart disease risk factors in obese older adults. Am J Clin Nutr. 2006;84(6):1317–23.
Jensen GL, Roy MA, Buchanan AE, Berg MB. Weight loss intervention for obese older women: improvements in performance and function. Obes Res. 2004;12(11):1814–20.
Messier SP, Loeser RF, Miller GD, Morgan TM, Rejeski WJ, Sevick MA, et al. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the Arthritis, Diet, and Activity Promotion Trial. Arthritis Rheum. 2004;50(5):1501–10.
Miller GD, Nicklas BJ, Davis C, Loeser RF, Lenchik L, Messier SP. Intensive weight loss program improves physical function in older obese adults with knee osteoarthritis. Obesity (Silver Spring). 2006;14(7):1219–30.
Villareal DT, Chode S, Parimi N, Sinacore DR, Hilton T, Armamento-Villareal R, et al. Weight loss, exercise, or both and physical function in obese older adults. N Engl J Med. 2011;364(13):1218–29.
Shah K, Armamento-Villareal R, Parimi N, Chode S, Sinacore DR, Hilton TN, et al. Exercise training in obese older adults prevents increase in bone turnover and attenuates decrease in hip bone mineral density induced by weight loss despite decline in bone-active hormones. J Bone Miner Res. 2011;26(12):2851–9.
Shea MK, Nicklas BJ, Houston DK, Miller ME, Davis CC, Kitzman DW, et al. The effect of intentional weight loss on all-cause mortality in older adults: results of a randomized controlled weight-loss trial. Am J Clin Nutr. 2011;94(3):839–46.
Avenell A, Richmond PR, Lean ME, Reid DM. Bone loss associated with a high fibre weight reduction diet in postmenopausal women. Eur J Clin Nutr. 1994;48(8):561–6.
Riedt CS, Cifuentes M, Stahl T, Chowdhury HA, Schlussel Y, Shapses SA. Overweight postmenopausal women lose bone with moderate weight reduction and 1 g/day calcium intake. J Bone Miner Res. 2005;20(3):455–63.
Jensen LB, Kollerup G, Quaade F, Sorensen OH. Bone minerals changes in obese women during a moderate weight loss with and without calcium supplementation. J Bone Miner Res. 2001;16(1):141–7.
Villareal DT, Fontana L, Weiss EP, Racette SB, Steger-May K, Schechtman KB, et al. Bone mineral density response to caloric restriction-induced weight loss or exercise-induced weight loss: a randomized controlled trial. Arch Intern Med. 2006;166(22):2502–10.
Ryan AS, Nicklas BJ, Dennis KE. Aerobic exercise maintains regional bone mineral density during weight loss in postmenopausal women. J Appl Physiol. 1998;84(4):1305–10.
Armamento-Villareal R, Sadler C, Napoli N, Shah K, Chode S, Sinacore DR, et al. Weight loss in obese older adults increases serum sclerostin and impairs hip geometry but both are prevented by exercise training. J Bone Miner Res. 2012;27(5):1215–21.
Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults. Executive summary of the third report of The National Cholesterol Education Program (NCEP) (Adult Treatment Panel III). JAMA. 2001;285(19):2486–97.
Sugerman HJ, DeMaria EJ, Kellum JM, Sugerman EL, Meador JG, Wolfe LG. Effects of bariatric surgery in older patients. Ann Surg. 2004;240(2):243–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Villareal, D.T., Shah, K. (2015). Obesity in Older Adults and Strategies for Weight Management. In: Bales, C., Locher, J., Saltzman, E. (eds) Handbook of Clinical Nutrition and Aging. Nutrition and Health. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-1929-1_10
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1929-1_10
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-1928-4
Online ISBN: 978-1-4939-1929-1
eBook Packages: MedicineMedicine (R0)