Abstract
Ethanol is metabolized to acetaldehyde by catalase in the peroxisome, by the microsomal ethanol oxidation system (MEOS) containing cytochrome P-450, which is located in the endoplasmic reticulum, and by the alcohol dehydrogenase (ADH) pathway of cytosol or the soluble fraction of the cell [1, 2]. Among these metabolic processes, ADH is a key enzyme for metabolizing ethanol, and the role of non-ADH enzymes in systemic alcohol metabolism is unclear [3]. Ethanol absorption is primarily controlled by gastric emptying because the primary region of ethanol absorption is the small intestine, and ethanol is absorbed via simple diffusion [4]; for example, slow gastric emptying leads to increases in the first-pass metabolism of ingested ethanol. Ingested ethanol is primarily metabolized in the stomach and liver. In the stomach, ADH, including the isoenzymes ADH I, III, and IV, oxidizes the ingested ethanol, but most of the ethanol (approximately 90 %) is absorbed in the small intestine. Absorptive ethanol is metabolized by ADH, including the isoenzymes ADH I, II, and III, and primarily oxidizes in the liver. In comparison, the MEOS shares many properties with other microsomal drug-metabolizing enzymes, such as P-450; therefore, MEOS pathway activity increases under high ethanol concentrations and/or after chronic ethanol consumption. Ethanol and acetaldehyde are toxic and damage cells. Catalase can oxidize ethanol in vitro with H2O2, but it may not be a major system for ethanol oxidation [2]. ADH and/or catalase, MEOS enzyme pathways metabolize ethanol to produce acetaldehyde. Acetaldehyde is a harmful compound that causes hangovers and flush. It is detoxified by aldehyde dehydrogenase (ALDH), which is primarily composed of mitochondrial low Km ALDH, including the isoenzymes ALDH I, II, III, and IV, in the liver. The acetaldehyde metabolized by ALDH is converted to acetic acid and water, resulting in detoxification. The enzymatic activities of both of ADH and ALDH are regulated by the availability of the coenzyme nicotinamide adenine dinucleotide (NAD). NAD is reduced to NADH when ethanol and acetaldehyde are oxidized by ADH and ALDH, and NADH oxidation is the limiting factor of ethanol metabolism [2]. In addition to metabolizing ethanol, NAD and NADH regulate several metabolisms as coenzymes. However, ethanol metabolism is preferable to other metabolic pathways in terms of the resulting toxicity of ethanol and its metabolite, acetaldehyde; therefore, ethanol and acetaldehyde intake affect some metabolic pathways, such as lipid, hormone, protein, and amino acid metabolism, and induce disorders such as liver failure and muscle wasting.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Key Points
-
Leucine accelerates ethanol clearance.
-
Leucine enhances alcohol-metabolizing enzyme activities, such as ADH and low Km ALDH.
-
In contrast, valine has no effect on ethanol oxidation.
-
The effect of leucine on ethanol oxidation is not exerted directly in the liver.
-
Leucine treatment before alcohol intake may be important for enhancing ethanol oxidation.
Abbreviations
- MEOS:
-
Microsomal ethanol oxidation system
- ADH:
-
Alcohol dehydrogenase
- ALDH:
-
Aldehyde dehydrogenase
- NAD:
-
Nicotinamide adenine dinucleotide
- PPARα:
-
Peroxisome proliferator-activated receptor-α
- AMPK:
-
AMP-activated protein kinase
- IGF-1:
-
Insulin like growth factor-1
- 4E-BP1:
-
Eukaryotic initiation factor-binding protein 1
- S6K:
-
Ribosomal protein S6 kinase
- mTOR:
-
Mammalian target of rapamycin
- BCAAs:
-
Branched chain amino acids
- KIC:
-
α-Keto-isocaproic acid
- KMV:
-
β-Methyl isovalerianic acid
- AST:
-
Aspartate aminotransferase
- TBARS:
-
Thiobarbituric acid reactive substances
- eIF:
-
Eukaryotic initiation factor
- IL-6:
-
Interleukin-6
- TNF-α:
-
Tumor necrosis factor-α
Introduction
Ethanol Metabolism
Ethanol is metabolized to acetaldehyde by catalase in the peroxisome, by the microsomal ethanol oxidation system (MEOS) containing cytochrome P-450, which is located in the endoplasmic reticulum, and by the alcohol dehydrogenase (ADH) pathway of cytosol or the soluble fraction of the cell [1, 2]. Among these metabolic processes, ADH is a key enzyme for metabolizing ethanol, and the role of non-ADH enzymes in systemic alcohol metabolism is unclear [3]. Ethanol absorption is primarily controlled by gastric emptying because the primary region of ethanol absorption is the small intestine, and ethanol is absorbed via simple diffusion [4]; for example, slow gastric emptying leads to increases in the first-pass metabolism of ingested ethanol. Ingested ethanol is primarily metabolized in the stomach and liver. In the stomach, ADH, including the isoenzymes ADH I, III, and IV, oxidizes the ingested ethanol, but most of the ethanol (approximately 90 %) is absorbed in the small intestine. Absorptive ethanol is metabolized by ADH, including the isoenzymes ADH I, II, and III, and primarily oxidizes in the liver. In comparison, the MEOS shares many properties with other microsomal drug-metabolizing enzymes, such as P-450; therefore, MEOS pathway activity increases under high ethanol concentrations and/or after chronic ethanol consumption. Ethanol and acetaldehyde are toxic and damage cells. Catalase can oxidize ethanol in vitro with H2O2, but it may not be a major system for ethanol oxidation [2]. ADH and/or catalase, MEOS enzyme pathways metabolize ethanol to produce acetaldehyde. Acetaldehyde is a harmful compound that causes hangovers and flush. It is detoxified by aldehyde dehydrogenase (ALDH), which is primarily composed of mitochondrial low Km ALDH, including the isoenzymes ALDH I, II, III, and IV, in the liver. The acetaldehyde metabolized by ALDH is converted to acetic acid and water, resulting in detoxification. The enzymatic activities of both of ADH and ALDH are regulated by the availability of the coenzyme nicotinamide adenine dinucleotide (NAD). NAD is reduced to NADH when ethanol and acetaldehyde are oxidized by ADH and ALDH, and NADH oxidation is the limiting factor of ethanol metabolism [2]. In addition to metabolizing ethanol, NAD and NADH regulate several metabolisms as coenzymes. However, ethanol metabolism is preferable to other metabolic pathways in terms of the resulting toxicity of ethanol and its metabolite, acetaldehyde; therefore, ethanol and acetaldehyde intake affect some metabolic pathways, such as lipid, hormone, protein, and amino acid metabolism, and induce disorders such as liver failure and muscle wasting.
Metabolic Changes Resulting from Ethanol Consumption
Ethanol metabolism causes changes in redox homeostasis and induces metabolic disorders, such as hepatitis and liver cirrhosis. Lieber reviewed the adverse effects of ethanol intake [2, 5]. The change in redox state is associated with hyperlactacidemia, which contributes to acidosis. Hyperlactacidemia reduces the kidney’s capacity to excrete uric acid, thus inducing hyperuricemia. Furthermore, ethanol induces ketosis and purine breakdown, which are associated with hyperuricemia. In addition, enhanced purine breakdown increases the oxygen species resulting from xanthine oxidase. The CYP2E1 form of cytochrome P450 enzymes generates several reactive oxygen species [5]. Chronic ethanol intake induces cytokine formation in the liver and promotes oxidative stress via both the increased formation of ROS and the depletion of oxidative defenses in the cell. Liver cells from ethanol-treated animals are more susceptible to the cytotoxic effects of TNF-α and other cytokines than cells from control animals [6, 7]. These ethanol-induced changes in redox state, oxidative stress, and cytokines are associated with the metabolic disturbances described below.
Ethanol and Lipid Metabolism
The change in the redox state (i.e., the increase in the NADH/NAD ratio) generates the mobilization of peripheral triglyceride from the adipose tissue. The NADH accumulation inhibits β-oxidation by inhibiting the mitochondrial fatty acid-oxidizing dehydrogenase. Additionally, the ethanol intake decreases the fatty acid oxidation by decreasing the expression of peroxisome proliferator-activated receptor-α (PPARα)-regulated genes. PPARα knockout mice develop worse hepatomegaly and hepatocyte damage with ethanol consumption as a result of increased exposure to oxidative stress via the decrease in glutathione peroxidase, superoxide dismutase, and catalase [8]. In addition, ethanol consumption decreases the activity of AMP-activated protein kinase (AMPK), which is a key regulator of lipid metabolism, resulting in the decrease of fatty acid oxidation and increase of fatty acid synthesis through the activation of sterol regulatory element-binding protein 1 and acetyl-CoA carboxylase. These lipid metabolism impairments caused by ethanol consumption induce alcoholic fatty liver [8].
Ethanol and Protein Metabolism
Ingested ethanol is a potent inhibitor of hepatic regeneration [9]. Ethanol suppresses growth hormone-induced signal transduction, resulting in a decrease in insulin like growth factor-1 (IGF-1) gene expression [10]. In humans, acute ethanol ingestion impairs the postprandial protein synthesis of hepatic proteins, such as albumin and fibrinogen [11]. Albumin synthesis is impaired, even when alcohol intake is moderate [12]; this impairment is associated with limited ATP availability, which results from the change in redox state [13]. In addition, ethanol blunts protein synthesis in skeletal muscle by decreasing the phosphorylation of eukaryotic initiation factor-binding protein 1 (4E-BP1) and ribosomal protein S6 kinase (S6K) [14]. Generally, leucine stimulates protein synthesis by activating 4E-BP1 and S6K via the mTOR pathway; however, ethanol impairs leucine’s anabolic effect on protein metabolism, an impairment that is not attributable to differences in the plasma concentration of insulin, IGF-1, and leucine [15].
Ethanol and Amino acid Metabolism
Ethanol affects amino acid metabolism. Amino acids are well known as protein component and regulators of the signaling pathway of protein metabolism; therefore, ethanol-related changes in amino acid metabolism are also associated with impaired liver regeneration. Plasma amino acid concentration is affected by ethanol consumption. In rats, acute ethanol intake decreases alanine, arginine, aspartic acid, β-alanine, glycine, phenylalanine, and serine, but the plasma levels of other amino acids are not significantly changed [16]. Ethanol ingestion alters the metabolism of sulfur amino acids, such as cysteine and taurine, in the liver, resulting in a decrease in glutathione level via a decrease in glutathione synthesis [17]. Chronic ethanol consumption increases the concentration of branched chain amino acids (BCAAs) in plasma, the liver, skeletal muscle, and the jejunal mucosa in rats through a decrease in protein synthesis and increase in protein breakdown [18]. In addition, chronic ethanol intake reduces the flux of a substrate of leucine (α-ketoisocaproate; KIC) via a decrease in the basal and total activity of branched chain keto acid (BCKA) dehydrogenase and non-increase in the conversion of the enzyme to its inactive form [19]. Furthermore, it is well known that plasma BCAA concentrations are reduced in cases of liver cirrhosis [20]. It has been indicated that the predominant mechanism for the decreases in plasma leucine levels in cirrhosis is an increase in the oxidized leucine fraction associated with decreased leucine turnover [21].
Ethanol also has a direct and/or selective inhibitory effect on amino acid transport into the cells. Ethanol inhibits sodium-dependent alanine and cysteine uptake, but no effect has been observed on sodium-independent alanine and cysteine transport in basolateral rat liver plasma membranes [22]. In comparison, ethanol exposure stimulates leucine uptake in rat fetal hepatocytes via sodium independent-system L [23].
Therefore, ethanol exposure changes several metabolic pathways, resulting in liver failure via fatty liver and liver cirrhosis. Thus, the acceleration of ethanol oxidation is very important to prevent liver disease and the metabolic anabolism impairment induced by alcohol intake.
Amino Acid Supplementation Improves the Metabolic Changes Caused by Ethanol Consumption
The development of ethanol-induced fatty liver, alcoholic hepatitis, and cirrhosis has been partially attributed to nutritional deficiencies in compounds such as amino acids, lipids, and vitamins [24]. Some studies have indicated that amino acids reduce the liver damage and oxidative stress caused by chronic ethanol consumption. Beauge et al. showed that only the amino acids that are precursors of pyruvate, alanine, aspartate or glutamate are able to activate ethanol oxidation in rat hepatocytes [25]. These compounds supply malate-aspartate shuttle components and stimulate the oxidation of NADH generation via ethanol consumption, resulting in enhanced ethanol clearance. Yang et al. demonstrated that a diet supplemented with amino acids (alanine, glutamine, glutamate, protein, and ten essential amino acids) reduced plasma aspartate aminotransferase (AST) levels in rats that chronically consume ethanol [26]. Glutamine pretreatment suppresses plasma inflammation in chronically ethanol-fed rats [27]. Treatment with histidine or carnosine after liver injury from chronic ethanol exposure increases the mRNA expression levels of catalase and glutathione peroxidase and downregulates the mRNA expression levels of IL-6 and TNF-α in mice livers [28]. Aspartate attenuates ethanol-induced oxidative stress, such as thiobarbituric acid reactive substances (TBARS), and reduces glutathione transferase activity in rats [29]. Torii et al. indicated that a preference for both alanine and glutamine was observed in preference tests when alcoholic rats developed hepatic disorder [30], and supplementation with these amino acids prevented the ethanol-induced inhibition of liver regeneration [31]. In addition, treatment with d/l-cysteine and alanine before ethanol loading accelerates ethanol and acetaldehyde clearance [32].
It is well known that BCAA supplementation improves liver failures, such as liver cirrhosis. A BCAA-enriched diet partly prevents the morphological ultrastructural changes in the liver caused by chronic ethanol consumption and improves positive body weight gain in rats [33]. Leucine administration improves myocardial protein synthesis, which is impaired by ethanol intoxication, by enhancing anabolic signaling pathways, such as eukaryotic initiation factor 4G (eIF4G) [34]. In addition, we recently reported the effect of each BCAA on ethanol clearance after acute ethanol loading in rats [35].
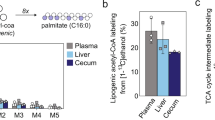
Leucine Accelerates Ethanol Oxidation
The effect of pretreatment with each BCAA via oral administration or tail-vein infusion on ethanol clearance was investigated after acute ethanol loading in rats. First-pass ethanol metabolism in the stomach and liver is important for alcohol metabolism [4]; therefore, to understand the effects of amino acids in the digestive tract on ethanol absorption and metabolism, each amino acid was administered either orally or via the tail vein. Leucine significantly decreased the blood ethanol levels after oral ethanol administration, and the individuals in the isoleucine group tended to have reduced ethanol levels (Fig. 20.1). In contrast, alanine treatment, which is known as amino acid-enhancing ethanol oxidation [31], slightly decreased the ethanol concentrations, but the reduction was not significant. Valine did not affect blood ethanol oxidation. The amount of orally administered alanine in this study was low compared with the levels reported in a previous study (0.084 g/kg body weigh in the present study [35] and 1 g/kg BW in the previous study [31]). Therefore, the effect of orally administered alanine on ethanol clearance in rats may be weak in this study [35]. Furthermore, leucine also significantly decreased the blood ethanol concentration after acute ethanol intake in rats who received infusions of each amino acid into the tail vein (Fig. 20.2). The infused alanine significantly decreased the blood ethanol levels after ethanol intake. However, isoleucine and valine did not decrease the blood ethanol concentrations. Leucine is the only amino acid that has been found to enhance ethanol clearance via both administration routes.
The effects of orally administered amino acids on blood ethanol clearance in rats. Leucine significantly decreased the blood ethanol concentration 1 h after ethanol administration, but the other amino acids did not significantly decrease the blood ethanol values. The values are presented as the mean ± SEM of four rats in each group. Comparisons with the control group at each time point were performed with Bonferroni’s post-test following a two-way ANOVA for multiple comparisons (*P < 0.05). With permission from Amino Acids, 2012, 43, 2545–51 [35]
The effects of amino acids infused into the tail vein on ethanol oxidation in rats. Leucine significantly decreased the blood ethanol concentration 1 h after ethanol administration, and the ethanol concentration in the leucine group was lower for 5 h after the ethanol administration. In addition, alanine significantly decreased the blood ethanol level 0.5 h after acute ethanol administration. However, isoleucine and valine did not decrease the blood ethanol concentrations. The values are presented as the mean ± SEM of six rats in each group. Comparisons with the control group at each time point were performed using Bonferroni’s post-test following a two-way ANOVA for multiple comparisons (*P < 0.05). With permission from Amino Acids, 2012, 43, 2545–51 [35]
Leucine induces an increase in ethanol clearance by enhancing ethanol enzyme activity. ADH activity tended to be increased by pretreatment with leucine and alanine before ethanol intake, and these amino acids also significantly increased ADH activity after ethanol intake. In contrast, ADH activity was lower in the valine group before and after ethanol administration (Table 20.1). The low Km ALDH activity was significantly increased in the leucine group (Table 20.2). Liver ADH is the primary enzyme responsible for ethanol oxidation, and low Km ALDH encodes the mitochondrial enzyme that is primarily responsible for oxidizing the ethanol-derived acetaldehyde [36–38]. Low Km ALDH impairment negatively affects the capacity for acetaldehyde metabolism, which is one of the primary causes of the alcohol-flush reactions that have been observed in Asian individuals [38]. Therefore, these results indicate that pretreatment with leucine accelerates ethanol clearance and enhances acetaldehyde oxidation by activating the alcoholic enzymes in the liver. In contrast, low Km ALDH was lower in individuals pretreated with valine (Table 20.2).
BCAAs are primarily metabolized in skeletal muscles and the brain by branched chain amino acid aminotransferase. This process produces branched chain α-keto acids, such as α-keto isocaproic acid from leucine and β-methyl isovalerianic acid (KMV) from isoleucine. Branched chain α-keto acids are metabolized in the liver. Some studies have demonstrated that leucine directly affects hepatocytes. Leucine has been shown to inhibit proteolysis in isolated-rat hepatocytes [39] and stimulate hepatic growth factor production in hepatic stellate cells [40]. Therefore, leucine or its metabolite, α-keto isocaproic acid, may directly affect ethanol clearance in the liver. To understand the effect of leucine or its metabolite on ethanol oxidation in the hepatocytes, this study investigated changes in the media ethanol levels of isolated rat hepatocytes incubated with ethanol after preincubation with each amino acid or BCAA metabolites. Interestingly, leucine, other branched amino acids and α-keto acids did not accelerate ethanol oxidation (Fig. 20.3). In contrast, alanine significantly increased ethanol oxidation in the hepatocytes (Fig. 20.3). Each BCAA also accelerated ethanol clearance in the liver perfusion performed using a modification of the method described by Mortimore [41] (data not shown). NADH reoxidation is believed to be the primary rate-determining step in hepatic ethanol oxidation, and the malate-aspartate shuttle is an important rate determinant in hepatic ethanol oxidation [42]. Precursors of malate-aspartate shuttle components, such as alanine, increased ethanol metabolism in hepatocytes [25]. In addition, it has been suggested that alanine stimulates the glucose-alanine cycle, which improves the NADH redox state and results in increased ethanol elimination [43]. Therefore, the effect of leucine on ethanol clearance may not be attributable to changes in the redox state via leucine metabolism in the liver, and leucine and its metabolite will not directly affect ethanol oxidation in the liver.
The effects of amino acids on ethanol oxidation in isolated rat hepatocytes. Alanine significantly decreased the ethanol concentration in the medium 90 min after ethanol injection. However, the BCAAs and their metabolites did not decrease the ethanol concentrations in the isolated rat hepatocytes. The values are presented as the mean ± SEM of six set in each group. Comparisons of each group were performed with a Bonferroni’s post-test following a two-way ANOVA for multiple comparisons (*P < 0.05). With permission from Amino Acids, 2012, 43, 2545–51 [35]
Alcohol-metabolizing enzymes are activated by hormonal and nutritional factors. ADH has been shown to be increased by insulin in vivo and by IGF-1 and growth hormone via an increase in cyclic AMP in hepatocytes [44–46]. Insulin also enhanced the effect of IGF-1 on ADH activation [45]. In addition, insulin secretion has been shown to be stimulated by amino acids, such as leucine [47], but ethanol has been shown to inhibit insulin secretion [48]. As shown in Fig. 20.4, pretreatment with leucine significantly increased insulin secretion just prior to ethanol administration, but alanine did not confer this effect. This suggests that the stimulation of hormone secretion, such as insulin secretion, by leucine may contribute to enhanced alcohol-metabolizing enzyme activities. The mechanism of leucine’s effect on ethanol clearance may be associated with the change in liquid factors (e.g., insulin). However, leucine’s mechanism of action on the acceleration of ethanol clearance is unclear. Further studies are required to investigate this mechanism.
The effects of leucine or alanine on insulin secretion after the administration of each amino acid and ethanol. Leucine significantly increased the insulin concentrations 30 min after administration, but alanine did not confer this effect. The values are presented as the mean ± SEM of five rats in each group. Comparisons with the control group at each time point were performed with Bonferroni’s post-test following a two-way ANOVA for multiple comparisons (*P < 0.05). With permission from Amino Acids, 2012, 43, 2545–51 [35]
Estimation of Effective Amount of Leucine for Humans
The amount of leucine used in the study performed by Murakami et al. was 0.125 g/kg body weight in rats [35]. In addition, two-thirds of this amount (0.083 g/kg body weight) of leucine had the same effect on ethanol clearance in rats (data not shown). The increase of BCAAs in plasma depends on the BCAA intake [49]. In an animal study, the plasma leucine concentration after BCAA administration (the amounts of leucine, isoleucine, and valine were 0.5, 0.25, and 0.25 g/kg body weight, respectively) was 12.6-fold higher than that of the control group, which was administered water [50]. Thus, plasma leucine levels will increase approximately 2.1-fold when leucine is administered at 0.083 g/kg body weight in rats. Plasma leucine concentration increases 3.80-fold over the basal level with an intake of 5 g of BCAAs (the leucine content was 2.56 g) in young Japanese men (22–25 years old) [49]. Therefore, we estimate that 1.41 g of leucine is needed to accelerate ethanol oxidation in humans.
Conclusions
Leucine accelerates ethanol clearance after acute ethanol administration by enhancing alcohol-metabolizing enzyme activities, such as alcohol and aldehyde dehydrogenase. In contrast, valine has no effect on ethanol oxidation. Effect of leucine on ethanol oxidation is not exerted directly in the liver. The increase in alcohol dehydrogenase activity resulting from leucine treatment may be associated with the induction of insulin secretion. In addition, leucine treatment before alcohol intake may be important to enhance alcoholic enzyme activities and accelerate ethanol oxidation.
Chronic alcohol intake leads to liver failures, such as hepatic inflammation and fatty liver, and induces liver cirrhosis. Therefore, it is important to accelerate ethanol oxidation after alcohol intake to prevent these liver failures. Leucine may be a powerful solution for preventing liver failure resulting from acute and chronic alcohol intake.
References
Lieber CS. Metabolism of alcohol. Clin Liver Dis. 2005;9(1):1–35.
Lieber CS. Ethanol metabolism, cirrhosis and alcoholism. Clin Chim Acta. 1997;257(1):59–84.
Haseba T, Ohno Y. A new view of alcohol metabolism and alcoholism–role of the high-Km Class III alcohol dehydrogenase (ADH3). Int J Environ Res Public Health. 2010;7(3):1076–92.
Oneta CM, Simanowski UA, Martinez M, et al. First pass metabolism of ethanol is strikingly influenced by the speed of gastric emptying. Gut. 1998;43(5):612–9.
Lieber CS. ALCOHOL: its metabolism and interaction with nutrients. Annu Rev Nutr. 2000;20:395–430.
Hoek JB, Pastorino JG. Ethanol, oxidative stress, and cytokine-induced liver cell injury. Alcohol. 2002;27(1):63–8.
Koch OR, Pani G, Borrello S, et al. Oxidative stress and antioxidant defenses in ethanol-induced cell injury. Mol Asp Med. 2004;25(1–2):191–8.
Sozio M, Crabb DW. Alcohol and lipid metabolism. Am J Physiol. 2008;295(1):E10–6.
Wands JR, Carter EA, Bucher NL, Isselbacher KJ. Inhibition of hepatic regeneration in rats by acute and chronic ethanol intoxication. Gastroenterology. 1979;77(3):528–31.
Xu X, Ingram RL, Sonntag WE. Ethanol suppresses growth hormone-mediated cellular responses in liver slices. Alcohol Clin Exp Res. 1995;19(5):1246–51.
De Feo P, Volpi E, Lucidi P, et al. Ethanol impairs post-prandial hepatic protein metabolism. J Clin Invest. 1995;95(4):1472–9.
Volpi E, Lucidi P, Cruciani G, et al. Moderate and large doses of ethanol differentially affect hepatic protein metabolism in humans. J Nutr. 1998;128(2):198–203.
Deaciuc IV, D’Souza NB, Lang CH, Spitzer JJ. Effects of acute alcohol intoxication on gluconeogenesis and its hormonal responsiveness in isolated, perfused rat liver. Biochem Pharmacol. 1992;44(8):1617–24.
Vary TC, Deiter G, Goodman SA. Acute alcohol intoxication enhances myocardial eIF4G phosphorylation despite reducing mTOR signaling. Am J Physiol. 2005;288(1):H121–8.
Lang CH, Frost RA, Deshpande N, et al. Alcohol impairs leucine-mediated phosphorylation of 4E-BP1, S6K1, eIF4G, and mTOR in skeletal muscle. Am J Physiol. 2003;285(6):E1205–15.
Abdel-Nabi R, Milakofsky L, Hofford JM, Hare TA, Vogel WH. Effect of ethanol on amino acids and related compounds in rat plasma, heart, aorta, bronchus, and pancreas. Alcohol. 1996;13(2):171–4.
Jung YS, Kwak HE, Choi KH, Kim YC. Effect of acute ethanol administration on S-amino acid metabolism: increased utilization of cysteine for synthesis of taurine rather than glutathione. Adv Exp Med Biol. 2003;526:245–52.
Bernal CA, Vazquez JA, Adibi SA. Leucine metabolism during chronic ethanol consumption. Metab Clin Exp. 1993;42(9):1084–6.
Bernal CA, Vazquez JA, Adibi SA. Chronic ethanol intake reduces the flux through liver branched-chain keto-acid dehydrogenase. Metab Clin Exp. 1995;44(10):1243–6.
Morgan MY, Marshall AW, Milsom JP, Sherlock S. Plasma amino-acid patterns in liver disease. Gut. 1982;23(5):362–70.
Holecek M, Tilser I, Skopec F, Sprongl L. Leucine metabolism in rats with cirrhosis. J Hepatol. 1996;24(2):209–16.
Moseley RH, Murphy SM. Effects of ethanol on amino acid transport in basolateral liver plasma membrane vesicles. Am J Physiol. 1989;256(3 Pt 1):G458–65.
Henderson GI, Frosto TA, Heitman DW, Schenker S. Ethanol stimulates leucine uptake by rat fetal hepatocytes via trans-stimulation. Am J Physiol. 1989;256(2 Pt 1):G384–9.
Leevy CM, Moroianu SA. Nutritional aspects of alcoholic liver disease. Clin Liver Dis. 2005;9(1):67–81.
Beauge F, Mangeney M, Nordmann J, Nordmann R. Comparative study of the effect of amino acids on ethanol oxidation in isolated hepatocytes from starved and fed rats. Adv Exp Med Biol. 1980;132:393–402.
Yang SC, Ito M, Morimatsu F, Furukawa Y, Kimura S. Effects of amino acids on alcohol intake in stroke-prone spontaneously hypertensive rats. J Nutr Sci Vitaminol. 1993;39(1):55–61.
Peng HC, Chen YL, Chen JR, et al. Effects of glutamine administration on inflammatory responses in chronic ethanol-fed rats. J Nutr Biochem. 2011;22(3):282–8.
Liu WH, Liu TC, Yin MC. Beneficial effects of histidine and carnosine on ethanol-induced chronic liver injury. Food Chem Toxicol. 2008;46(5):1503–9.
Oh SI, Lee MS, Kim CI, Song KY, Park SC. Aspartate modulates the ethanol-induced oxidative stress and glutathione utilizing enzymes in rat testes. Exp Mol Med. 2002;34(1):47–52.
Torii K. A new pharmacological and physiological aspects of L-amino acids. Nihon Yakurigaku Zasshi. 1997;110 Suppl 1:28P–32.
Tanaka T, Imano M, Yamashita T, et al. Effect of combined alanine and glutamine administration on the inhibition of liver regeneration caused by long-term administration of alcohol. Alcohol Alcohol. 1994;29(1):125–32.
Tsukamoto S, Kanegae T, Nagoya T, et al. Effects of amino acids on acute alcohol intoxication in mice–concentrations of ethanol, acetaldehyde, acetate and acetone in blood and tissues. Arukoru Kenkyuto Yakubutsu Izon. 1990;25(5):429–40.
Farbiszewski R, Chyczewski L, Holownia A, Pawlowska D, Chwiecko M. Branched-chain amino acid enriched diet given simultaneously with ethanol partially prevents morphological and biochemical changes in the liver. Patologia Polska. 1990;41(4):183–6.
Vary T. Oral leucine enhances myocardial protein synthesis in rats acutely administered ethanol. J Nutr. 2009;139(8):1439–44.
Murakami H, Ito M, Furukawa Y, Komai M. Leucine accelerates blood ethanol oxidation by enhancing the activity of ethanol metabolic enzymes in the livers of SHRSP rats. Amino Acids. 2012;43(6):2545–51.
Deitrich RA, Petersen D, Vasiliou V. Removal of acetaldehyde from the body. Novartis Found Symp. 2007;285:23–40. discussion 40-51, 198–199.
Yin SJ. Alcohol dehydrogenase: enzymology and metabolism. Alcohol Alcohol. 1994;2:113–9.
Ehrig T, Bosron WF, Li TK. Alcohol and aldehyde dehydrogenase. Alcohol Alcohol. 1990;25(2–3):105–16.
Venerando R, Miotto G, Kadowaki M, Siliprandi N, Mortimore GE. Multiphasic control of proteolysis by leucine and alanine in the isolated rat hepatocyte. Am J Physiol. 1994;266(2 Pt 1):C455–61.
Tomiya T, Nishikawa T, Inoue Y, et al. Leucine stimulates HGF production by hepatic stellate cells through mTOR pathway. Biochem Biophys Res Commun. 2007;358(1):176–80.
Mortimore GE, Khurana KK, Miotto G. Amino acid control of proteolysis in perfused livers of synchronously fed rats. Mechanism and specificity of alanine co-regulation. J Biol Chem. 1991;266(2):1021–8.
Sugano T, Handler JA, Yoshihara H, Kizaki Z, Thurman RG. Acute and chronic ethanol treatment in vivo increases malate-aspartate shuttle capacity in perfused rat liver. J Biol Chem. 1990;265(35):21549–53.
Cunningham CC, Preedy VR, Paice AG, et al. Ethanol and protein metabolism. Alcohol Clin Exp Res. 2001;25(5 (Suppl ISBRA)):262S–8.
Lakshman MR, Chambers LL, Chirtel SJ, Ekarohita N. Roles of hormonal and nutritional factors in the regulation of rat liver alcohol dehydrogenase activity and ethanol elimination rate in vivo. Alcohol Clin Exp Res. 1988;12(3):407–11.
Mezey E, Potter JJ, Mishra L, Sharma S, Janicot M. Effect of insulin-like growth factor I on rat alcohol dehydrogenase in primary hepatocyte culture. Arch Biochem Biophys. 1990;280(2):390–6.
Mezey E, Potter JJ, Rhodes DL. Effect of growth hormone on alcohol dehydrogenase activity in hepatocyte culture. Hepatology. 1986;6(6):1386–90.
Milner RD. Stimulation of insulin secretion in vitro by essential aminoacids. Lancet. 1969;1(7605):1075–6.
Singh SP, Patel DG, Snyder AK. Ethanol inhibition of insulin secretion by perifused rat islets. Acta Endocrinol (Copenh). 1980;93(1):61–6.
Zhang Y, Kobayashi H, Mawatari K, et al. Effects of branched-chain amino acid supplementation on plasma concentrations of free amino acids, insulin, and energy substrates in young men. J Nutr Sci Vitaminol. 2011;57(1):114–7.
Murakami H, Shimbo K, Inoue Y, Takino Y, Kobayashi H. Importance of amino acid composition to improve skin collagen protein synthesis rates in UV-irradiated mice. Amino Acids. 2012;42(6):2481–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Murakami, H., Komai, M. (2015). Leucine and Ethanol Oxidation. In: Rajendram, R., Preedy, V., Patel, V. (eds) Branched Chain Amino Acids in Clinical Nutrition. Nutrition and Health. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-1923-9_20
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1923-9_20
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-1922-2
Online ISBN: 978-1-4939-1923-9
eBook Packages: MedicineMedicine (R0)