Abstract
The increased recognition of anatomic factors associated with the tear trough deformity in the lower eyelids and an increased sensitivity of patients and surgeons to the secondary deformities associated with purely subtractive blepharoplasty surgery have led to a variety of conservative lower blepharoplasty techniques focused on the translocation or repositioning of fat to camouflage the anatomic tear trough. We have found that intra-SOOF fat repositioning generally yields excellent results for correction of the tear trough deformity.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
The increased recognition of anatomic factors associated with the tear trough deformity in the lower eyelids (Muzaffar et al. 2002) and an increased sensitivity of patients and surgeons to the secondary deformities associated with purely subtractive blepharoplasty surgery have led to a variety of conservative lower blepharoplasty techniques focused on the translocation or repositioning of fat to camouflage the anatomic tear trough (Goldberg 2000).
The authors have used two variations on a pre-periosteal fat repositioning over the past 12 years. Generally excellent results have been obtained with correction of the tear trough deformity and in achieving an aesthetic lower eyelid (Mohadjer and Holds 2006).
Key Elements of Procedure
Patient Selection
The authors have found these fat repositioning techniques to be applicable to the vast majority of their lower blepharoplasty patients. Preoperative examination should focus on the relevant anatomy including the configuration of the tear trough as well as lid tone and laxity, midface configuration including globe prominence, and condition of the skin. Preoperative counseling should include discussion of surgical expectations. If laser skin resurfacing is to be performed as an adjunct procedure, a full discussion of the expectations and preoperative and postoperative care must be undertaken. More generalized facial volume depletion may mandate the recommendation for additional fat transfer technique or synthetic filler to achieve optimal results.
Procedure
Except for special patient needs or requests, this technique of lower lid blepharoplasty may be carried out in the office-based procedure room with light oral sedation. The prominence of the fat pads and the edge of the tear trough and the exit site of repositioning sutures and skin resurfacing zones if indicated are marked. Pledgets of topical proparacaine are placed in the inferior fornix. Local anesthetic consisting initially of 0.25 % lidocaine with epinephrine buffered with sodium bicarbonate is injected through the inferior fornix. An infraorbital nerve block is important to achieve adequate anesthesia.
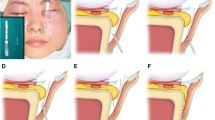
Metallic eye shields are placed. Lidocaine 2 % with epinephrine is infiltrated to reinforce the anesthesia. A standard transconjunctival incision is made with a Luxar LX-20 CO2 laser using a 0.4 mm tip. Dissection is carried anterior to the orbital septum down to the orbital rim exposing the periosteum at the arcus marginalis (Fig. 68.1). Careful blunt dissection is completed in the plane of the SOOF from the orbital rim just anterior to the arcus marginalis to a level 8–12 mm below the orbital rim. Medially, the SOOF thins with the muscle lying directly on the periosteum.
Each orbital fat pad is opened, and the fat is allowed to prolapse across the lid. A pedicle is developed in any pad to be repositioned, circumferentially releasing the fat to allow advancement. Gentle sculpting is done as necessary, most commonly only in the temporal fat pad (Fig. 68.2). One to three mattress sutures (one for each fat pad) of 5-0 polypropylene are passed from the cheek into the dissected supraperiosteal pocket. Generally, only the medial and central pads are repositioned using a single suture. A robust bite is taken weaving through the fat pedicle, and the fat pads are each repositioned into the supraperiosteal plane (Fig. 68.3). The polypropylene suture is passed through a foam bolster and tied on the skin.
Appropriate patients undergo light or medium depth laser skin resurfacing at the end of the procedure. Lateral canthopexy and direct excision of excess skin via a subciliary incision are performed as indicated.
Patients are treated with antibiotic ointment and a skin dressing postoperatively. Mild analgesics are prescribed. We normally do not prescribe oral antibiotics or antivirals unless there is a specific indication. Sutures and bolsters are removed in 7 days.
The authors have found it to be difficult to perform this procedure in the crowded Asian eyelid. An anterior approach utilizing a subciliary incision and skin muscle flap to expose the arcus marginalis and then perform the surgery as described is performed. The fat can be directly sutured in place using 5-0 polyglactin 910 (Vicryl) sutures on a P-2 needle. This variation allows a comprehensive treatment of the tear trough in most patients and avoids the externalized bolsters and sutures. In some patients with significant lower eyelid laxity, it is possible to suture the fat pads internally with this needle via the transconjunctival incision.
Postoperative
Ophthalmic ointment is instilled and cold compresses placed. Skin resurfacing may indicate follow-up at 1-day postoperative; otherwise, any external sutures are removed at 6 days. The repositioned fat often hardens and is palpable from 10 to 20 days postoperatively, later softening with a natural correction of the tear trough.
Conclusion
This technique of fat repositioning blepharoplasty has yielded a pleasing improvement in the tear trough deformity with a revision rate comparable to other blepharoplasty techniques. The authors have noted that this technique is particularly effective in patients with a prominent eye, such as thyroid eye disease patients, or negative vector eyelids. The authors have reported (Couch et al. 2011) that the muscle edge close to the arcus marginalis rises almost 9 mm superiorly during the procedure (Fig. 68.4). It is believed that this muscle repositioning accounts for much of the improvement seen in the tear trough and eyelid contour with this technique. Short- and long-term results are generally excellent. We recommend this approach for the surgical treatment of the tear trough deformity.
Lower eyelid after blepharoplasty with supraperiosteal fat repositioning and an externalized bolster. Note the elevated orbicularis muscle edge (arrow) that was previously below the orbital rim, after release from the orbital rim (Reprinted from Couch et al. (2011). With permission from American Medical Association)
References
Couch SM, Buchanan AG, Holds JB. Orbicularis muscle position during fat repositioning lower blepharoplasty. Arch Facial Plast Surg. 2011;13(6):387–91. Epub 2011 Jun 20.
Goldberg RA. Transconjunctival orbital fat repositioning: transposition of orbital fat pedicles into a subperiosteal pocket. Plast Reconstr Surg. 2000;105:743–51.
Mohadjer Y, Holds JB. Cosmetic lower eyelid blepharoplasty with fat repositioning via intra-SOOF dissection: Surgical technique and initial outcomes. Ophthal Plast Reconstr Surg. 2006;22:409–13.
Muzaffar AR, Mendelson BC, Adams WP. Surgical anatomy of the ligamentous attachments of the lower lid and lateral canthus. Plast Reconstr Surg. 2002;110:873–84.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Holds, J.B., Mohadjer, Y. (2015). Transconjunctival Pre-periosteal Fat Repositioning Blepharoplasty. In: Hartstein, MD, FACS, M., Massry, MD, FACS, G., Holds, MD, FACS, J. (eds) Pearls and Pitfalls in Cosmetic Oculoplastic Surgery. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-1544-6_68
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1544-6_68
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-1543-9
Online ISBN: 978-1-4939-1544-6
eBook Packages: MedicineMedicine (R0)