Abstract
Digital ischemia is the reduction in digital perfusion with impaired tissue viability and can frequently result in digital ulcers (DU). DU are denuded areas with a defined border, loss of epithelialization and loss of epidermis and dermis. DU from digital ischemia typically occurs at the distal aspects of the digits. Because the management of digital ischemia varies depending on the etiology, it is important to be familiar with the differential diagnosis. Digital ischemia may manifest due to connective tissue diseases, vasculitis, diffuse arteriopathy, occupational diseases, paraneoplastic syndromes, steal phenomenon, radial artery cannulation, septic shock, and anatomic variants. Although DU usually heal on their own over time, non-pharmacologic and pharmacologic therapies show some efficacy in DU management. A variety of agents can serve as treatments such as those typically used for the management of Raynaud’s phenomenon (RP), and more novel vasodilators including endothelin-1 receptor antagonists, phosphodiesterase inhibitors and prostanoids. However, if digital ischemia persists or progresses despite medical therapies, more aggressive management with procedures such as chemical and surgical sympathectomy, the local administration of botulinum toxin, vascular reconstruction, and/or amputation should be considered. In its more severe form, digital ischemia may present critically. This situation is a medical emergency and patients should be hospitalized and treated aggressively with medical and potentially surgical therapies to prevent digital loss.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Pulmonary Arterial Hypertension
- Mixed Connective Tissue Disease
- Ulnar Artery
- Digital Ulcer
- Digital Artery
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Key Points
-
1.
Digital ulcers are denuded areas with a defined border, loss of epithelialization, and loss of epidermis and dermis that typically occur at the distal aspects of the digits.
-
2.
Digital Ulcers are the consequence of tissue ischemia secondary to a variety of diseases that cause injury to peripheral arteries
-
3.
Ischemic digital ulcers are a consequence of multiple factors including ischemia–reperfusion injury with oxidative stress from recurrent vasospasm, thrombosis, and loss of vascular integrity from arterial disease.
-
4.
Both non-drug and drug therapy need to specifically address the underlying cause of the vascular disease whenever possible.
-
5.
Hydrocolloid membranes used as a dressing after cleansing can provide protection from repeated trauma and also accelerate DU healing and reduce pain
-
6.
Pharmacologic agents used to treat RP either alone or in combination can prevent DU since ischemia–reperfusion injury contributes to the development of ischemic DU [also see Chap. 20]
-
7.
Vasoactive drugs including endothelin receptor antagonists, phosphodiesterase inhibitors, prostaglandins, and statins may prevent the development of new DU in patients with scleroderma.
-
8.
Digital sympathectomy is favored over proximal upper limb sympathectomy in treating distal circulatory problems.
-
9.
Critical digital ischemia is a digit-threatening event requiring emergency care to immediately define the underlying cause and to begin appropriate vascular therapy.
Introduction
Digital ischemia is the reduction in digital perfusion associated with impaired tissue viability that can frequently result in digital pitting scars, digital ulcers (DU), loss of digital pulp, and if severe, gangrene requiring amputation. Ulceration from digital ischemia typically occurs at the distal aspects of the digits, at or distal to the proximal interphalangeal joints [1]. Because the management of digital ischemia varies depending on the etiology, it is important to be familiar with the differential diagnosis (see Table 21.1).
Connective Tissue Diseases
Connective tissue diseases are chronic autoimmune diseases that can result in inflammation and vascular pathology. In one study of 50 patients with digital ischemia, connective tissue disease was the predominant underlying disease, associated with 38 % of cases [2]. Forms of connective tissue disease that can present with digital ulcers include systemic sclerosis (SSc), systemic lupus erythematosus (SLE), and mixed connective tissue disease (MCTD) [2]. Digital ulcers and ischemia can occur in up to 50 % of SSc patients over the course of their disease [3]. Although clearly less common than in SSc, the exact incidence and prevalence of digital ischemia are currently unknown in SLE and MCTD patients [4, 5]. SSc is characterized by cutaneous and visceral fibrosis, in addition to vascular disease that involves the arterioles and arteries of the peripheral circulation [1]. Histologically, the digital arteries in patients with SSc are characterized by intimal hyperplastic or fibrotic proliferation, resulting in extensive luminal narrowing (Fig. 21.1) [6, 7]. Digital artery thrombosis can also occur, further compromising the peripheral circulation, leading to both chronic and acute episodes of digital ischemia [8]. The majority of studies on the management of digital ulcers and ischemia summarized below have included patients with SSc.
Digital artery from a patient who has SSc (amputation specimen) showing marked intimal hyperplasia and almost complete occlusion of the lumen (Reproduced with permission from: Herrick, A. (2008). “Diagnosis and management of scleroderma peripheral vascular disease.” Rheumatic Disease Clinics of North America 34(1): 89–114)
Vasculitis
Vasculitis occurs when there is inflammation and fibrinoid necrosis of blood vessel walls [9, 10]. This leads to vessel destruction and subsequent hemorrhagic and ischemic damage [11]. In addition to affecting the larger blood vessels, inflammation can occur in arterioles, venules, and capillaries. However, digital ischemia typically occurs in association with large or medium vessel vasculitis. Primary vasculitides that can be associated with digital ischemia include giant cell arteritis or Takayasu’s arteritis which affect large vessels; polyarteritis nodosa which affects medium vessels; and anti-neutrophilic cytoplasmic antibody (ANCA)-associated vasculitis, cryoglobulinemic vasculitis, and connective tissue disease-associated vasculitis which can affect small and medium sized blood vessels [12].
Arteriopathies
The most common cause of peripheral vascular disease is obstructive atherosclerosis of the extremities. Atherosclerosis is considered to involve an inflammatory component which may be in part immune-mediated [13]. Traditional risk factors are well known including age, gender, family history, diabetes mellitus, hypertension, hyperlipidemia, cigarette smoking, and obesity with metabolic syndrome [14, 15]. Atherosclerotic plaque can cause stenosis or occlude peripheral vessels causing claudication with physical activity or it can cause cutaneous ulceration. Thrombosis, embolism, and vascular dissection are complications that can cause digital ulcers or peripheral skin ulcerations. In patients with other vascular diseases, underlying larger vessel atherosclerosis is a common complicating factor that must be appreciated and addressed. The prevalence of atherosclerotic cardiovascular disease has been found to be higher in patients with SSc than in the general population [15, 16]. Although the exact mechanisms are unknown, this increased rate may be secondary to the chronic inflammation, altered lipid profiles and function, development of autoantibodies, and vascular dysfunction found in SSc [15].
Fibromuscular dysplasia (FMD) is a systemic arterial disease that is noninflammatory and nonatherosclerotic [17]. FMD has an unknown etiology but has been suggested to be due to hormonal, mechanical or genetic causes [17, 18]. It typically affects the renal and carotid arteries, but can also affect the small arterial beds where it manifests as lesions in the middle or distal arterial segments. Although uncommon, case studies have reported digital ischemia in patients with brachial artery FMD [19–21]. FMD predominantly presents in young female adults who are suffering from renal hypertension [18].
Degos disease (also called malignant atrophic papulosis) is a rare condition that can be purely cutaneous (small, white, and firm papules), or that can present as a systemic variant with cutaneous manifestations [22]. The pathogenesis is unknown [22–25]. The systemic variant has a high morbidity and can affect the nervous, ophthalmological, gastrointestinal, cardiothoracic, and hepatorenal systems. It has been suggested that the skin lesions of Degos disease are secondary to the slow occlusion of deeper arterioles [25], which can ultimately cause digital ischemia. Histologic findings in one small study noted that all patients with Degos syndrome had varying degrees of lymphocyte-mediated necrotizing vasculitis [24].
Occupational Diseases [See Chap. 9]
Blunt or penetrating injury can lead to vascular trauma and complications of digital ulcerations. Hypothenar hammer syndrome (HHS) is a condition resulting from constant pressure or vibrational force to the ulnar artery. Embolization to digital arteries from the injured ulnar artery can cause unilateral finger ischemia [26]. Occupations that require repetitive movement in which the palm is used as a hammer, such as carpenters, machinists, and mechanics, are most susceptible to digital ischemia related to injury of the ulnar artery [26–28]. The incidence of HHS in these occupations is estimated to be 14 % [29]. Symptoms associated with HHS range from mild pain or cold sensitivity to digital gangrene. It has been suggested that individuals who develop HHS may have a preexisting abnormality of their ulnar artery, making it more susceptible to digital artery embolization from traumatic injury [26]. Identifying HHS can be difficult, and it is believed to be underdiagnosed [30]. A thorough patient history for occupation, hobbies, and previous hand trauma is important to properly diagnose the disease [31].
Paraneoplastic Syndrome
Malignant disease can be associated with digital ischemia, and has been reported with a variety of cancers including those of the kidney, ovary, colon, and pancreas [32–34]. Although digital ischemia as a paraneoplastic syndrome has been reported in a number of case studies, the prevalence is unknown [32, 35–37]. Factors that may contribute to cancer-related ischemia include tumor cell infiltration, impaired blood flow due to hyperviscosity, an increase in circulating coagulant factors, and impaired anticoagulant and fibrinolytic pathways. Tumor antigen–antibody immune complexes can also cause arterial microvascular thrombosis [38]. Generally, onset is sudden and can be rapidly progressive [32]. In some cases, symptoms reduce after therapy for the primary tumor [39–41].
Steal Phenomenon After Vascular Access Shunts
If a patient has recently received shunt placement, steal phenomenon should be considered as a possible mechanism for digital ischemia. Placement of upper limb arteriovenous accesses for hemodialysis has been reported to induce hand ischemia in 1.6–8 % of hemodialysis patients [42–44]. With vascular steal, extremity ischemia can occur when significant arterial blood flow is shunted directly into the venous outflow of an arteriovenous fistula or graft but a portion of the collateral flow to the distal extremity is taken by the access [43]. Vascular steal can range in intensity. In mild cases, onset is insidious and can be delayed by a few days to a few months. Symptoms include numbness and paresthesia of one or more fingers. Pain, stiffness, and swelling of the fingers may also occur [42]. In severe cases, there is progressive numbness and pain, accompanied by reduced sensation, ischemic ulcers, and dry gangrene of the fingers [42, 44]. Confirmation of the diagnosis is made with digital plethysmography/pulse volume recordings that document digital pressures less than 50 mmHg and augmentation of the pulse wave with fistula compression [42].
Iatrogenic After Radial Artery Cannulation
Although an uncommon complication, ischemic damage from radial artery cannulation may occur [45, 46]. Radial artery cannulation is a procedure that allows precise measurement of blood pressure, blood gases, arterial pulse contour, and cardiac output, and is particularly useful when managing critically ill patients and individuals who will be undergoing major surgery. However, indwelling catheters have been reported to create partial or complete vascular occlusion that results in ischemia and at times gangrene of a digit or hand. Autoimmune diseases, vasospastic conditions such as Raynaud’s phenomenon (RP), severe arteriosclerosis or ischemic disease, and thrombotic tendency have all been identified as risk factors for cannulation complications [46].
Septic Shock
Septic shock occurs when the systemic response to infection leads to hypotension and organ dysfunction [47]. Septic shock is characterized by decreased peripheral tissue perfusion, abnormal cellular metabolism, and misdistribution of blood flow due to vessel constriction, all of which can lead to digital ischemia [48].
Anatomic Variants
Abnormal anatomic structures may influence the occurrence of digital ischemia. Variations in the arterial anatomy of the upper extremities are found in as many as 24 % of patients and are most common in the radial or ulnar artery [49, 50]. Anatomic variation can be observed by arteriogram. Anatomic arterial contribution to abnormal blood flow should be assessed prior to determining the best therapy for digital ulceration [50].
Digital Ulcers
Definition
Digital ulcers (DU) are denuded areas with a defined border, loss of epithelialization, and loss of epidermis and dermis [51]. DU do not include fissures (Fig. 21.2) or paronychia (Fig. 21.3). DU can be related to ischemic causes, from severe recurrent vasospasm related to RP and underlying vascular pathology. Other contributing factors include trauma or underlying calcinosis (Fig. 21.4). They typically present as painful sores on the fingers or toes (Fig. 21.5), but can also occur over the interphalangeal joints of the hands, or other extensor surfaces (Fig. 21.6) [52]. DU can also be partially or completely covered with crust, hyperkeratosis, or fibrin. Chronic ulcers can progress to gangrene, loss of distal tissue, or become infected and lead to osteomyelitis [52].
Pathophysiology
Ischemic DU are a consequence of multiple factors. Although the vasospasm associated with RP is reversible, recurrent and prolonged episodes may contribute to ischemic damage to distal tissues. In addition, vascular injury can result in endothelial dysfunction and abnormal vascular reactivity. For example, increased levels of vasoconstrictors (endothelin-1) and decreased levels of vasodilators (nitric oxide and prostaglandin) are thought to lead to decreased perfusion of the digits in patients with SSc. Finally, the lumen of digital arteries in patients with SSc is compromised due to thrombosis [51] and fibrosis of the intimal layer [53]. Progressive occlusion of arteries from thrombosis can occur in other diseases associated with DU.
Prevention and Treatment of DU
Although treatment with a variety of vasodilators has been shown to be effective in managing RP, DU remain a serious complication for many patients, and a uniform effective therapy is lacking [53]. Below, we will address non-pharmacologic and pharmacologic therapies targeted to treat DU, as well as surgical options. It is important to note that most of the clinical trials investigating agents used to prevent or heal DU have been done in patients with SSc. Therefore, the benefit or not of a given agent in other vascular diseases causing DU is unclear. It is also important to address the underlying cause of the vascular disease with specific therapy if possible. For example, active vasculitis may need corticosteroids or immunosuppressive therapy to control the inflammatory component of the vascular insult.
Non-pharmacologic Therapy
The management of DU includes non pharmacological modalities, including the avoidance of all inciting factors such as cold exposure, emotional distress, smoking, repeated trauma of hands, and some drugs [54], specifically pharmacologic vasoconstrictors such as smoking, cocaine, and sympathomimetics [55]. In patients with scleroderma (SSc), physical therapy is important in improving joint contractures of the digits where abnormal skin stretched over an immobile joint often leads to a trauma-induced DU [1] (Fig. 21.7).
Keeping the affected area clean is of utmost importance to promote healing and prevent infection. Also, patients should minimize trauma to their digits as much as possible. Hydrocolloid membranes such as Duoderm can provide protection from repeated trauma and also accelerate DU healing and reduce pain [56]. These dressings decrease oxygen tension and preserve moisture over the damaged area, promoting growth of granulation tissue and the epidermal and dermal layers of the skin [1]. Duoderm is a polyurethane film coated with a strong adhesive that protects skin from bacteria and serves as a barrier against further injury. We use the following approach for the application of Duoderm. First, we recommend cleaning the area over the ulcer with hydrogen peroxide 3 % or an antibacterial soap, drying, and covering with antibacterial ointment, being careful not to get the greasy ointment where the adhesive will be placed. Duoderm should be cut approximately 1/2–1 in. beyond the wound’s margin and applied to the wound after peeling off the adhesive. Tape may be used around the edges of the dressing to aid keeping it in place. The Duoderm dressing should be changed and cleaned every third day, or sooner if the dressing is oozing a lot of fluid.
The removal of damaged tissue can be helpful in improving the healing potential of remaining tissue [57]. Debridement can be performed if the DU appears to be superficial and there is no deep infection or exposed bone [58]. Surgical debridement may be indicated for deeper lesions [see Chap. 22].
Pharmacologic Therapies
Optimization of Raynaud’s Phenomenon (RP) Therapy
We often use pharmacologic agents to treat RP either alone or in combination for the treatment and prevention of DU since RP contributes to the development of ischemic DU, and the majority of validated outcome measures used in DU clinical trials are borrowed from studies of RP [1, 59]. We will focus on treatments that have shown some efficacy specifically for DU. Please refer to Chap. 15 for details on RP management.
Calcium channel blockers (CCBs): CCBs are moderately effective in the treatment of RP, reducing the severity of attacks by 35 % in secondary RP [60] and by 33 % in primary RP [61]. In addition, one study demonstrated a significant reduction in the number of DU compared to baseline after 16 weeks of nifedipine, as compared to intravenous infusions of iloprost, but without change in hand temperature or digital microcirculatory blood flow [62]. Another study compared nifedipine to placebo in the treatment of RP [63] and found no statistically significant difference in the prevention of new DU; however, the trial was underpowered since few new ulcers developed [64]. CCBs may potentially be useful as “background” therapy in patients with DU, and most randomized controlled trials (RCT) for DU permit CCB use at stable doses throughout the studies [52].
Alpha-adrenergic inhibitors: Two RCT showed that prazosin is more effective than placebo in the treatment of RP secondary to SSc [65] and one observational study found that terazosin reduced the number, intensity and duration of vasospastic attacks to the hands in patients with idiopathic and secondary RP [66]. However, although they may reduce RP, alpha-adrenergic blockers have not been directly studied for DU treatment [59].
Angiotensin converting enzyme (ACE)-inhibitors and angiotensin receptor blockers (ARBs): Similarly, ACE-inhibitors and ARBs have limited benefit in the treatment of RP secondary to SSc, but studies evaluating their effects on DU are lacking [1]. One multicenter, randomized, double blind, placebo controlled study included 210 patients with limited scleroderma or with RP and the presence of SSc-specific antinuclear antibodies. This study found that quinapril 80 mg/day, or the maximum tolerated dosage, did not affect the occurrence of new DU or the frequency or severity of RP episodes over a 3-year follow-up period [67].
Nitroglycerin ointment or patches: Nitrates are used in topical, sublingual, or oral formulations, as adjunctive therapy in the treatment of RP and DU in SSc [1], but there is no evidence supporting their role in DU healing [54]. One double blind, placebo-controlled, randomized trial showed that a short-acting topical nitroglycerin gel was more effective than placebo for the treatment of RP but did not prevent new DU [68].
Selective serotonin reuptake inhibitors (SSRI): A small study of 26 patients with primary and 27 patients with secondary RP suggested that SSRI are more effective than nifedipine in reducing the frequency and severity of RP, particularly in female patients and those with primary RP [69]. However, no studies have evaluated the effect of SSRI on the treatment and prevention of DU [59].
Other Vasoactive Drugs
Endothelin-1 receptor antagonists Endothelin receptor antagonists (ETRA) are a class of pulmonary arterial hypertension (PAH)-specific drugs that block the interaction of Endothelin-1 (ET-1) with its receptors (ETA and ETB) interfering with its vasoconstrictive effects [70]. ETA receptors are located on vascular smooth muscle cells and primarily mediate vasoconstriction while ETB receptors are located on endothelial cells mediating vasodilatation by release of nitric oxide and prostanoids, and also on smooth muscle cells mediating vasoconstriction [71]. ET-1 is also noted to promote cell growth and proliferation and thus can also mediate vascular and tissue fibrosis and remodeling.
Bosentan The dual endothelin-1 receptor antagonist bosentan has been shown to prevent the development of new SSc-related DU in two randomized, double-blind controlled clinical trials [53, 72]. In the RAPIDS-1 trial, which included 122 patients with SSc, bosentan 62.5 mg twice daily for 4 weeks and thereafter 125 mg twice daily reduced the occurrence of new ulcers by 48 % after 16 weeks of treatment, particularly in patients with diffuse skin involvement, non-smokers, and patients with a high burden of DU. A slight trend toward slower healing was observed in patients treated with bosentan, but this did not reach statistical significance. RAPIDS-2, which enrolled 188 patients with SSc, confirmed the results of the previous RAPIDS-1 trial: 24 weeks of bosentan therapy was associated with a reduction in the number of new DU compared to placebo, but did not lead to more rapid ulcer healing. The most common side effect among patients treated with bosentan was elevation of liver enzymes, which was reported in 11.4–12.5 % of patients treated in clinical trials [64]; thus its use requires monthly liver function test monitoring. The FDA approved bosentan in the USA in November 2001 for the treatment of WHO functional class III/IV PAH, and in 2009 for the treatment of WHO functional class II PAH, while the EU approved it for PAH in May 2002. In June 2007, the EU extended the indication for bosentan as a therapy to reduce the number of new DU in patients with SSc and ongoing DU disease [70].
Ambrisentan Although evaluated in only a small number of patients, this ETA selective ETRA showed a reduction in the total number of DU in two open-label studies [73, 74]. In the first one, six patients with SSc with DU unresponsive to bosentan were treated with 5 mg daily of ambrisentan for 24 weeks. The recruited patients continued to receive intravenous therapy with prostanoids. Ambrisentan led to a reduction in baseline number of DU per patient with no appearance of new lesions [73]. In the second study, up to 10 mg daily as tolerated of ambrisentan significantly decreased DU burden and mean maximum diameter of lesions after 24 weeks of therapy in 20 patients with SSc. Ambrisentan did not prevent the incidence of new DU and no patients developed elevated transaminases, but 75 % experienced peripheral edema [74]. Ambrisentan does not require monthly liver function test monitoring, is given once daily, and two doses are available (5 and 10 mg). It is approved for the therapy of SSc-associated PAH in the USA, but has not been evaluated in RCT for the prevention and treatment of DU.
Macitentan Macitentan is a dual endothelin-receptor antagonist, developed by modifying the structure of bosentan to increase efficacy and safety. Macitentan was FDA-approved for the treatment of WHO functional class II-IV PAH in October 2013 at a dose of 10 mg once daily. Liver enzyme abnormalities occurred in a similar percentage of patients receiving placebo and macitentan in the PAH trial, but higher percentages of patients in the two macitentan groups had nasopharyngitis, headache, and anemia [75]. There are two ongoing multicenter randomized double-blind placebo controlled parallel group studies aimed to evaluate the effectiveness of macitentan in the prevention of new DU at 16 weeks. Although preliminary data analysis led to the early termination of these trials due to a lack of efficacy over placebo, results of final analyses are pending.
Phosphodiesterase inhibitors By inhibiting the hydrolysis of cyclic guanosine monophosphate (cGMP), agents in this class increase cGMP levels, with consequent vasodilatory, antiproliferative, and pro-apoptotic effects that may reverse pulmonary artery remodeling. Studies have suggested these agents may have a role in the treatment and prevention of DU, but solid evidence is lacking. Common side effects of these medications include headaches, dizziness, dyspepsia, and nasal congestion.
Sildenafil One open uncontrolled study of 16 patients with SSc treated with maximally tolerated doses of sildenafil (mean 114 mg daily for mean 5.2 months), and concomitant vasodilators and platelet inhibitors showed a significant decrease in the total number of DU. However, nine patients developed 12 new DU despite sildenafil therapy [76]. One double-blind placebo-controlled study, which did not measure DU outcomes, included 57 patients with limited cutaneous SSc and showed that 100 mg once daily for 3 days followed by 200 mg once daily for 25 days of modified-release sildenafil reduced RP frequency and was well tolerated [77].
Tadalafil One study concluded that tadalafil as add-on therapy may contribute to DU prevention and healing. 24 patients with SSc or mixed connective tissue disease were treated with 20 mg of tadalafil every other day or placebo for 6 weeks and then crossed over, with concomitant vasodilators (CCBs, ACE-inhibitors, and ARBs) and platelet inhibitors. All 24-fingertip ulcers healed during tadalafil compared to 3 of 13 during placebo treatment. Tadalafil also significantly prevented the appearance of new DU (1 during tadalafil treatment versus 13 during placebo) [78]. However, another randomized, double-blind, placebo-controlled, crossover study of 39 women with RP secondary to SSc receiving 20 mg of tadalafil daily or placebo for a period of 4 weeks showed that tadalafil lacked efficacy as a treatment for RP. There were too few DU in this study population to analyze the role of tadalafil in DU healing or prevention [79].
Prostacyclins
Prostacyclins are potent pulmonary and systemic vasodilators that also inhibit platelet adhesion and aggregation, and smooth muscle cell proliferation in the blood vessels [59, 80]. Common side effects of these medications include hypotension, dizziness, headache, flushing, jaw pain, and gastrointestinal symptoms [81].
Oral Prostanoids Overall, oral forms of prostanoids have not shown benefit in the treatment of DU. In one meta-analysis [64], none of the following studies showed a statistically significant difference in DU healing individually or in pooled analyses, and side effects were more common in subjects who received oral prostanoids compared to the placebo subjects.
Iloprost Although no studies have evaluated the effects of oral iloprost on DU, one study showed that oral iloprost at a dose of 50 mcg twice daily did not significantly improve RP compared to placebo [82]. Higher doses of oral iloprost may be more effective for the treatment of RP and potentially DU, but with increased side effects that may limit tolerability [59].
Beraprost In a study of 107 patients with SSc, the oral prostacyclin analog beraprost sodium at a dose of 60 μg three times daily, showed a trend towards fewer new DU compared to placebo [83]: 48 % of patients had new ulcers in the beraprost group versus 59 % in the placebo group (p = 0.325), but this has not been confirmed in further studies.
Cisaprost Cisaprost, another oral prostacyclin analog showed a trend for minimal improvement in efficacy when given orally at a dose of 2.5 or 5 μg three times daily for the treatment of RP secondary to SSc. This 4-month randomized, double-blind, placebo-controlled study involving 49 patients found that there were not statistically significant differences in the median change from baseline in the total number and duration of attacks, the number of painful attacks and the average severity of attacks between the three groups. However, cisaprost given at 5 μg three times daily produced a greater decrease in severity of RP at week 2 (p = 0.02). There were no significant changes in the number of active DU throughout the study between the three groups, but only five patients had DU at the time of enrollment [84].
Treprostinil A study of 148 subjects with DU showed that the administration of the oral prostacyclin analog treprostinil as a sustained-release osmotic tablet up to 16 mg twice daily for 20 weeks did not result in a statistically significant reduction in net ulcer burden when compared to placebo [85].
Systemic prostanoids Prostanoids delivered systemically, either by intravenous or subcutaneous administration, appear to be more effective for the treatment of DU than oral formulations likely related to better absorption. Intravenous prostanoids, in particular iloprost, are approved in the EU and recommended for the treatment of DU in patients with SSc [86].
Intravenous iloprost Intravenous iloprost (0.5–2 ng/kg per minute for 3–5 consecutive days) significantly improved DU healing, particularly for ischemic digital tip ulcers, in comparison with placebo in two RCT including 35 and 131 SSc patients, respectively [87, 88]. A third small RCT including 17 patients treated over the course of 4 months with monthly 3-h intravenous infusion of 0.5–2.0 ng/kg/min of iloprost or placebo did not find statistically significant differences [89]. In addition, two RCT comparing intravenous iloprost to oral nifedipine for the treatment of RP showed a beneficial effect on DU healing in both groups, but the number of patients with DU was small [62, 90]. The first one included 23 patients with SSc-related RP and the mean number of digital lesions was reduced with iloprost from 3.5 to 0.6 and with nifedipine from 4.3 to 1.4 after 16 weeks. The second study included 46 patients with SSc-related RP, 17 patients had DU at entry into the study. Among these, all the patients treated with nifedipine (3/3) and 12 out of 14 of those treated with iloprost decreased the number of DU after 12 months. In contrast, one meta-analysis showed that intravenous iloprost was beneficial for the prevention of new DU, but did not affect DU healing [64]. Long-term low-dose iloprost (0.5 ng/kg per minute) has been shown to be equally effective and less harmful than high-dose (2 ng/kg per minute) when given for 21 days, with both regimes reducing DU in 70 % of treated patients [91]. There is currently no generally accepted dosage scheme for the administration of iloprost [92]. We recommend the use of 0.5–2 ng/kg per minute for 3–5 consecutive days, then reassessing response for additional infusions.
Intravenous epoprostenol In one study that did not report effects on healing of existing ulcers, intravenous epoprostenol administered continuously for severe SSc-related pulmonary arterial hypertension tended to reduce the number of new DU when compare to conventional therapy [93]. Although not FDA approved for the treatment and prevention of DU, epoprostenol could potentially be used in a similar fashion to intravenous iloprost for the management of DU and digital ischemia.
Subcutaneous Treprostinil Treprostinil is a prostacyclin analog that is currently approved for the treatment of PAH in subcutaneous, intravenous, and oral formulations. In one small study, subcutaneous treprostinil was effective in both the healing and prevention of DU in patients with SSc [94]. However, only 5 of 12 patients were able to tolerate the medication due to severe injection site pain. Intravenous treprostinil has not been evaluated for the treatment of DU.
Anti-platelet Agents: Although a double blind controlled study of aspirin in combination with dipyridamole showed no benefit on RP or DU compared to placebo [95], 81 mg of aspirin daily is often prescribed for patients who do not have a contraindication, keeping in mind that patients with SSc often have gastrointestinal involvement and are at increased risk of side effects [96]. Cilostazol and its metabolites are inhibitors of phosphodiesterase III that increase cyclic adenosine monophosphate (cAMP) levels leading to reversible inhibition of platelet aggregation, vasodilation, and inhibition of vascular smooth muscle cell proliferation [97]. Pentoxifylline reduces blood viscosity and improves peripheral tissue oxygenation presumably through enhanced blood flow increasing leukocyte and erythrocyte deformability and decreasing neutrophil adhesion/activation [98]. A systematic review and network meta-analysis of 26 RCTs evaluated the efficacy and tolerability of cilostazol and pentoxifylline in patients with intermittent claudication due to peripheral arterial disease and found that cilostazol increased maximum and pain-free walking distance with minimal serious adverse events [99]. Although there is biologic rationale to use these agents for the treatment of DU, there is currently no strong evidence supporting their use for this indication. One small study of 11 females with primary RP treated with pentoxifylline 400 mg tid for 2 months showed photoplethysmographic improvement of peripheral blood flow and decrease in duration and frequency of attacks [100].
Statins: Extensive research suggests that the clinical benefits of statins are related to an improvement in vascular function and inhibition of smooth muscle proliferation [101], a reduction in blood thrombogenicity, anti-inflammatory properties, and immunomodulatory actions [102]. One single study involving 84 SSc patients showed that 12 weeks of atorvastatin therapy reduced RP and prevented new DU in comparison to placebo, without statistically significant differences in DU healing [102].
Botulinum toxin: The local administration of botulinum neurotoxin type A is thought to increase blood flow as a result of arteriolar vasodilation through sympathetic blockade [103]. One study of 26 patients found that the use of botulinum toxin type A (BTX-A) injection in patients with recalcitrant ischemia resolved pain in 75 % of patients; improved color in 57 % of patients, and improved transcutaneous oxygen saturation in 56 % of patients. A single treatment with BTX-A resulted in improvement 89 % of the time [104]. A recent review article [105] summarized the findings from four published studies [104, 106–108] of patients treated with botulinum neurotoxin A. All patients had overall improvement in pain as well as decrease in frequency and severity of vasospastic attacks and healing of DU. Current problems are the lack of a standardized injection site and dose, in addition to complications that include pain at the site of injection and transient intrinsic hand muscle weakness [104]. Further and longer-term evaluation is necessary to better define the role of botulinum toxin in DU treatment [96].
Topical Vitamin E: Vitamin E is believed to be the most important naturally occurring non-enzymatic, lipid-soluble antioxidative agent in human tissue, with also antiaggregant and mild vasodilating capabilities. It may both reduce the ischemic damage of reperfusion and stimulate the growth and stabilization of granulation tissue, as well as reepithelialization. In one single study, the application of topical vitamin E reduced time of healing of DU and was associated with a faster resolution of pain, with a significant reduction of costs [109].
More aggressive treatment may be necessary if conservative medical treatment is ineffective in treating digital ischemia. These include sympathectomy, surgery, and amputation.
Sympathectomy: [Also see Chap. 22]
Chemical sympathectomy: While more commonly performed for lower limb complications, upper limb chemical sympathectomy can provide relief and healing. Lidocaine or bupivacaine digital blocks have also been reported as effective in immediately decreasing pain [110, 111]. However, chemical sympathectomy can be complicated by neuritis and surgical sympathectomy may be favored [112, 113].
Surgical sympathectomy: Because of the relationship between blood flow and vessel radius, a small change in the vessel radius can impart a large effect on blood flow. Surgical sympathectomy is a procedure in which at least one sympathetic ganglion is removed. Eliminating sympathetic innervation creates a corresponding dilatation of blood vessels [114]. Sympathectomy may prevent the need for digital amputation if performed early enough [114]. Both cervical and digital sympathectomy can be useful in managing digital ischemia; however, cervical sympathectomy has been found to have limited results [115, 116]. Cervical sympathectomy involves blocking the sympathetic chain/ganglia in the lower cervical and upper thoracic region [117]. Patients with connective tissue disease, such as SSc, may only temporarily respond to sympathetic ablation, while digital sympathectomy to treat RP associated with occupational diseases typically results in longer lasting effects [28, 114]. It has been suggested that the success of cervical sympathectomy in digital ischemia is limited due to the fact that the brachial plexus does not receive its communicating rami exclusively from the cervicothoracic sympathetic trunk [57]. In a study of eight patients with SSc receiving cervical sympathectomy, four (50 %) patients experienced reduction of pain for 1–2 years, one patient had relief of symptoms for 10 years, while three (38 %) patients received no symptomatic relief [57].
Digital sympathectomy including the ulnar artery and the radial artery with its dorsal branch at the wrist level has been found to more successful than cervical sympathectomy in interrupting sympathetic supply to the digital arteries [118]. Distal sympathectomy has been favored over proximal upper limb sympathectomy in treating distal circulatory problems [115]. Distal digital sympathectomy entails stripping the adventitia from the superficial palmar arch, the radial digital artery to the index finger, the common digital artery, and the ulnar and radial digital arteries to the second, third, and fourth web spaces and the ulnar digital artery to the little finger at the level of the web spaces [2, 119].
The efficacy of digital sympathectomy is determined by assessing hand pain relief and DU healing, and more objectively by assessing postoperative pulse volume recordings in comparison to preoperative values [2]. At our center, digital sympathectomy was performed on 26 hands in 17 patients with SSc, resulting in improved pain in 92 % and healed DU in 88 % of patients (unpublished data). However, the results of surgical sympathectomy for the treatment of RP and DU are not always prolonged [118, 120]. Relapse has been attributed to incomplete denervation, regeneration of autonomic nerve fibers, and reorganization and activation of alternative pathways [118]. A study of sympathectomy outcomes in 22 patients with SSc reported fewer ulcers, faster ulcer healing, and decreased pain in 18 (82 %) of patients that persisted for a mean of 46 months [121].
Surgery: [See Also Chap. MMM]
Vascular reconstruction: Patients with persistent pain and multiple DU may be good candidates for vascular reconstruction. This option may be considered if chemical or surgical sympathectomy is unable to control symptoms [122]. Suboptimal fingertip perfusion and digital arterial occlusive disease may be signs for patients to undergo vascular reconstruction [123]. The best candidates for this procedure are those who show satisfactory distal runoff by visualization of the common digital arteries on angiography and if there is satisfactory backflow from the common digital arteries [2]. The reconstruction procedure creates a new palmar arch in which an interposition vein graft is anastomosed end to end to the distal radial or ulnar artery, and the common digital arteries are anastomosed end to side to the graft [2]. Vascular reconstruction has been able to significantly improve digital temperatures and microvascular perfusion, in addition to upper extremity function [124, 125].
Amputation: In cases where digital infection and necrosis is recurrent, conservative amputations can be useful in preserving fingertip length [28]. Moreover, fingertip amputation can sometimes be the only definitive solution for relieving the excruciating pain experienced by patients [57]. Wet gangrene or osteomyelitis of a phalanx can serve as indications for amputation. In the case of dry gangrene, auto-amputation is preferred in order to preserve the maximal amount of tissue [40, 126].
Supporting Therapy
Antibiotics for infections: An antibiotic should be prescribed if there is any suspicion of superinfection of DU, as indicated by spreading erythema around the lesion or evidence of purulent drainage [96]. We recommend oral antibiotics with good coverage for streptococci and methicillin sensitive staphylococci, such as cephalexin, dicloxacillin, or clindamycin. If there is purulent drainage, we recommend empirically covering for methicillin resistant staphylococcus with trimethoprim–sulfamethoxazole or clindamycin, after obtaining cultures. Antibiotics can then be changed based on the sensitivity results. Persistent infections can spread to underlying bone and cause osteomyelitis, requiring prolonged courses of intravenous antibiotics [1]. In such cases, we recommend consultation with Infectious Disease specialists for comanagement in determining the best antibiotic coverage and length of therapy.
Pain medications: DU are exquisitely painful. Acetaminophen and nonsteroidal anti-inflammatory agents can help, however narcotics may be necessary for adequate pain control. Tramadol is an effective oral analgesic that is not a controlled substance and can be used at doses of up to 100 mg every 6 h. Topical lidocaine can relieve pain, but its local effect on cutaneous blood flow is complex with evidence for both vasoconstriction and vasodilation [127]. In our opinion its overall benefit outweighs the risk. Referral to a Pain Clinic for management of narcotic medications is often helpful.
Critical Digital Ischemia
Definition
Critical digital ischemia is the sustained reduction in digital perfusion with resultant impaired tissue viability [128]. It is a digit-threatening event [55], may cause severe pain and well-demarcated persistent cyanosis or pallor with surrounding hyperemia [129]. Although it occurs much less frequently than DU [96], it is always a medical emergency since it may progress to digital loss [7]. One single-center, retrospective, longitudinal study of 103 patients with SSc (of whom 46 had history of DU) found that 68 % of patients had critical finger ischemia at least once over a 12-year period of follow-up [130]. However, in a cohort of 1,168 patients with SSc followed for an 18-month period, only 19 patients (1.6 %) developed critical ischemia [128].
Diagnosis
Clinical evaluation: It is crucial to assess for persistent cyanosis or pallor, increased pain, loss of epithelium, or gangrene, to examine peripheral pulses, and in patients with SSc, to look for capillary dilatation, hemorrhage, and dropout since progression of these nailfold capillaroscopic changes predicts the development of digital ischemia [131]. If pulses are weak or nonpalpable, an arterial Doppler should be performed. All patients should undergo laboratory analysis for the presence of antiphospholipid antibodies (lupus anticoagulant, anti-cardiolipin, and anti-beta2-glycoprotein I antibodies) and consider evaluation for other prothrombotic states.
Imaging: [See Chaps. 13 and 14] Imaging is especially indicated to identify lesions amenable to angioplasty or surgery. Conventional angiography is still considered the gold standard to visualize compromised arteries [51] but is invasive, and involves high radiation and contrast load. Advances in magnetic resonance angiography (MRA) and computed tomography (CT) angiography may replace the need of invasive diagnostic tools [132], but these are still investigational techniques [133, 134].
Treatment: Digital critical ischemia requires an aggressive approach to control symptoms and prevent digital loss.
Hospitalization: As this is considered a medical emergency, hospitalization and bed rest is useful to expedite interventions, provide warm environmental temperature and appropriate pain control, and decrease trauma and activity of the involved limb [51].
Analgesics: As pain due to critical digital ischemia is extremely intense, appropriate pain control is essential. Opioids are often needed. Local anesthetic blocks with lidocaine or bupivacaine without epinephrine and temporary chemical sympathetic block in patients that will undergo sympathectomy may also be helpful [55].
Optimizing Vasodilator Treatment
Short-acting CCBs: Oral calcium channel blockers should be titrated to the maximum tolerated dose [51], and maintained once the acute episode has passed [96].
Intravenous prostanoids: Intravenous iloprost or epoprostenol at doses of 0.5–2 ng/kg/min, administered daily during 6 h through a peripheral line for 1–3 days should be considered [55]. Intravenous iloprost has been shown to reduce both the frequency and severity of ischemic attacks and to improve DU healing; epoprostenol has been shown to prevent the development of new DU [87, 88, 93]. Further studies are necessary to define the optimal dose and length of treatment with intravenous prostanoids for critical digital ischemia.
Treating Procoagulant Tendency
In some patients with SSc arterial thromboses have been found in digital arteries from amputation specimens [135]. Although there are no studies supporting this approach, low-dose aspirin and short-term anticoagulation with unfractionated or low molecular weight heparin are recommended for patients with rapidly advancing ischemic tissue who do not have contraindications. Of note, gastric antral vascular ectasia (GAVE) can affect up to one fourth of SSc patients and therefore anticoagulation might not be appropriate for all patients [136]. Chronic anticoagulation is not recommended unless a hypercoagulable state is defined. However, the exact duration of anticoagulation for digital ischemia also has not been studied. One study has demonstrated the benefit of low-molecular-weight heparin for symptomatic improvement in primary and secondary RP [137]. Thrombolytic therapy (e.g., with tissue plasminogen activator) may be helpful in selected patients with a new thrombotic or embolic event [138–140] In one randomized, placebo-controlled study urokinase improved capillaroscopic findings and promoted DU healing in patients with SSc [141]. New antithrombin agents such as direct thrombin inhibitors (argatroban, inogatran, efegatran, hirudin, and bivalirudin) have not been studied and controlled clinical trials would be necessary to determine if there is a role for these agents in the treatment of critical digital ischemia.
Sympathectomy: Similar to chronic digital ischemia, sympathectomy is a reasonable option for patients suffering from acute critical digital ischemia.
Hand Vascular Surgery
Debridement of necrotic tissue: An embolectomy may be performed to remove lodged emboli that are blocking blood flow [2, 142, 143]. Microvascular hand surgery should be done as soon as possible after the onset of symptoms to optimize results [142, 143].
Amputation: Because of the accelerated progression of critical digital ischemia, the digits may be unable to be saved and amputation may be required [143].
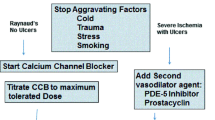
Author Recommendations (Fig. 21.8)
Algorithm for the treatment and prevention of digital ulcers in systemic sclerosis. (Modified with permission forms from: Chung L. Therapeutic options for digital ulcers in patients with systemic sclerosis. JDDG. 2007 Jun; 5(6):460–5). * All patients should be educated to avoid cold, stress, trauma, and nicotine. Aspirin 81 mg daily should be considered for all patients who do not have a contraindication. ACE-inhibitors and ARBs should be used as adjunctive therapy. DU = digital ulcers; RP = Raynaud’s phenomenon; CCB = calcium channel blockers; ACE = angiotensin converting enzyme; ARB = angiotensin II receptor blocker; SSRI = selective serotonin reuptake inhibitor; ASA = aspirin; PDE5 = phosphodiesterase-5; ET = endothelin; OTC = over the counter; IV = intravenous; SQ = subcutaneous
DU are associated with substantial pain, disability, and complications. We recommend preventative measures such as smoking cessation, avoidance of cold, stress, and trauma in all patients.
If a patient does not have existing ulcers, we consider aspirin 81 mg daily (for all patients who do not have a contraindication) and aggressive treatment of RP primarily with CCB (nifedipine 10–30 mg tid-qid, amlodipine 2.5–10 mg qd). Adjunctive therapy for RP might include ARB (losartan 50 mg bid), or SSRI (usually Lexapro 10–20 mg daily). In patients with history of DU in addition we recommend considering the adjunctive use of statins, PDE5-inhibitors, or ET-receptor blockers for the prevention of DU.
In patients with 1–2 active ulcers, we use hydrocolloid occlusion if the locations are amenable to such treatment; pain medications; wound care; and medical therapy typically with PDE5-inhibitors and ET-receptor blockers. In case of infection we add antibiotics as described above. For patients with refractory, progressive ulcers or multiple severe DU, our approach may include the use of prostacyclins, anticoagulants, cilostazol or pentoxifylline, and narcotics. We refer a significant proportion of patients with problematic DU for digital sympathectomy or revascularization.
In patients with acute critical ischemia we recommend hospitalization, anticoagulation and high dose vasodilator therapy with intravenous prostacyclins. We typically initiate therapy at 0.5–2 ng/kg per minute for 3–5 consecutive days then consider additional days of infusion or higher dosing if necessary. We also refer for consideration of surgical sympathectomy or vascular reconstruction while the patients are in the hospital. Surgical debridement or amputation may be necessary in some cases.
Conclusion
Digital ischemia is associated with substantial pain, disability, and complications. Clinicians should have a proactive approach to management including non-pharmacologic therapies, pharmacologic therapies and collaboration with surgeons, as debridement and sympathectomy may help to preserve a digit. Presumably, optimization of RP therapy should be helpful in the prevention and healing of DU by improving blood flow to the digits, although many of these medications have not been specifically evaluated for the treatment of DU. Oral forms of prostanoids have not shown benefit in the treatment of DU while prostanoids delivered systemically appear to be more effective. Other key recent advances include the promising use of endothelin-1 receptor antagonists. Early intervention will likely lead to better outcomes in patients suffering from digital ischemia. In severe cases, hand surgery is an appropriate and effective intervention that can provide rapid pain relief and improve vascular perfusion.
Abbreviations
- ACE:
-
Angiotensin converting enzyme
- ARBs:
-
Angiotensin receptor blockers
- cAMP:
-
Adenosine monophosphate
- CCBs:
-
Calcium channel blockers
- cGMP:
-
cyclic guanosine monophosphate
- DU:
-
Digital ulcers
- ET-1:
-
Endothelin-1
- ETA :
-
Endothelin-1 A receptor
- ETB :
-
Endothelin-1 B receptor
- ETRA:
-
Endothelin receptor antagonists
- FDA:
-
Food drug administration
- HHS:
-
Hypothenar hammer syndrome
- MCTD:
-
Mixed connective tissue disease
- PAH:
-
Pulmonary artery hypertension
- RCT:
-
Randomized controlled trials
- RP:
-
Raynaud’s phenomenon
- SLE:
-
Systemic lupus erythematosus
- SSc:
-
Systemic sclerosis
- SSRI:
-
Selective serotonin reuptake inhibitors
- WHO:
-
World Health Organization
References
Chung L, Fiorentino D. Digital ulcers in patients with systemic sclerosis. Autoimmun Rev. 2006;5(2):125–8. PubMed PMID: 16431342.
Jones NF. Acute and chronic ischemia of the hand: pathophysiology, treatment, and prognosis. J Hand Surg. 1991;16(6):1074–83.
Ferri C, Valentini G, Cozzi F, Sebastiani M, Michelassi C, La Montagna G, et al. Systemic sclerosis: demographic, clinical, and serologic features and survival in 1,012 Italian patients. Medicine. 2002;81(2):139–53.
Suzuki E, Kyozuka H, Nishida T, Kanno T, Ohira H. Systemic lupus erythematosus, complicated with refractory skin ulcers, treated successfully with bosentan. Mod Rheumatol. 2009;19(4):447–51.
Dabiri G, Falanga V. Connective tissue ulcers. J Tissue Viability. 2013;22(4):92–102.
RODNAN GP, MYEROWITZ RL, JUSTH GO. Morphologic changes in the digital arteries of patients with progressive systemic sclerosis (scleroderma) and Raynaud phenomenon. Medicine. 1980;59(6):393–408.
Herrick A. Diagnosis and management of scleroderma peripheral vascular disease. Rheum Dis Clin North Am. 2008;34(1):89–114.
Guiducci S, Giacomelli R, Cerinic MM. Vascular complications of scleroderma. Autoimmun Rev. 2007;6(8):520–3.
Jennette JC, Falk RJ. Small-vessel vasculitis. N Engl J Med. 1997;337(21):1512–23.
Guillevin L, Dorner T. Vasculitis: mechanisms involved and clinical manifestations. Arthritis Res Ther. 2007;9(2):S9.
Chen K-R, Carlson JA. Clinical approach to cutaneous vasculitis. Am J Clin Dermatol. 2008;9(2):71–92.
McCluskey RT, Fienberg R. Vasculitis in primary vasculitides, granulomatoses, and connective tissue diseases. Hum Pathol. 1983;14(4):305–15.
Shoenfeld Y, Gerli R, Doria A, Matsuura E, Cerinic MM, Ronda N, et al. Accelerated atherosclerosis in autoimmune rheumatic diseases. Circulation. 2005;112(21):3337–47.
Ngian G-S, Sahhar J, Proudman SM, Stevens W, Wicks IP, Van Doornum S. Prevalence of coronary heart disease and cardiovascular risk factors in a national cross-sectional cohort study of systemic sclerosis. Ann Rheum Dis. 2012;71(12):1980–3.
Au K, Singh MK, Bodukam V, Bae S, Maranian P, Ogawa R, et al. Atherosclerosis in systemic sclerosis: a systematic review and meta-analysis. Arthritis Rheum. 2011;63(7):2078–90.
Dave AJ, Fiorentino D, Lingala B, Krishnan E, Chung L. Atherosclerotic cardiovascular disease in hospitalized patients with systemic sclerosis: higher mortality than patients with lupus and rheumatoid arthritis. Arthritis Care Res. 2014;66(2):323–7.
Lüscher TF, Lie J, Stanson AW, Houser OW, Hollier LH, Sheps SG, editors. Arterial fibromuscular dysplasia, Mayo Clinic proceedings. Amsterdam: Elsevier; 1987.
Slovut DP, Olin JW. Fibromuscular dysplasia. N Engl J Med. 2004;350(18):1862–71.
Dorman Jr RL, Kaufman JA, LaMuraglia GM. Digital emboli from brachial artery fibromuscular dysplasia. Cardiovasc Intervent Radiol. 1994;17(2):95–8.
Edwards JM, Antonius JI, Porter JM. Critical hand ischemia caused by forearm fibromuscular dysplasia. J Vasc Surg. 1985;2(3):459–63.
Reilly JM, McGraw DJ, Sicard GA. Bilateral brachial artery fibromuscular dysplasia. Ann Vasc Surg. 1993;7(5):483–7.
Scheinfeld N. Malignant atrophic papulosis. Clin Exp Dermatol. 2007;32(5):483–7.
Güven FÖ, Bozdağg KE, Ermete M, Karaman A. Degos’ disease. Int J Dermatol. 2000;39(5):361–2.
Clarke JT, Werth VP. Rheumatic manifestations of skin disease. Curr Opin Rheumatol. 2010;22(1):78–84. PubMed PMID: 19851110, Pubmed Central PMCID: PMC3081507.
BLACK MM, NISHIOKA K, LEVENE GM. The role of dermal blood vessels in the pathogenesis of malignant atrophic papulosis (Degos’ disease). Br J Dermatol. 1973;88(3):213–9.
Ferris BL, Taylor Jr LM, Oyama K, McLafferty RB, Edwards JM, Moneta GL, et al. Hypothenar hammer syndrome: proposed etiology. J Vasc Surg. 2000;31(1):104–13.
Duncan WC. Hypothenar hammer syndrome: an uncommon cause of digital ischemia. J Am Acad Dermatol. 1996;34(5):881–3.
Bergan JJ, Conn Jr J, Trippel O. Severe ischemia of the hand. Ann Surg. 1971;173(2):301.
Little JM, Ferguson DA. The incidence of the hypothenar hammer syndrome. Arch Surg. 1972;105(5):684.
Abudakka M, Pillai A, Al-Khaffaf H. Hypothenar hammer syndrome: rare or underdiagnosed? Eur J Vasc Endovasc Surg. 2006;32(3):257–60.
Gaylis H, Kushlick A. The hypothenar hammer syndrome. S Afr Med J. 1976;50(5):125–7.
Hawley P, Johnston A, Rankin J. Association between digital ischaemia and malignant disease. Br Med J. 1967;3(5559):208.
Mills JL, Friedman EI, Taylor Jr L, Porter JM. Upper extremity ischemia caused by small artery disease. Ann Surg. 1987;206(4):521.
Ohtsuka T, Yamakage A, Yamazaki S. Digital ulcers and necroses: novel manifestations of angiocentric lymphoma. Br J Dermatol. 2000;142(5):1013–6.
Garioch J, Todd P, Soukop M, Thomson J. T-Cell lymphoma presenting with severe digital ischaemia. Clin Exp Dermatol. 1991;16(3):202–3.
Maurice P. Ovarian carcinoma and digital ischaemia. Clin Exp Dermatol. 1996;21(5):381–2.
Wright JR, Gudelis S. Digital necrosis associated with squamous cell carcinoma of the tonsil. Head Neck. 2002;24(11):1019–21.
Woei-A-Jin FSH, Tamsma JT, Khoe LV, den Hartog WC, Gerritsen JJ, Brand A. Lymphoma-associated paraneoplastic digital ischemia. Ann Hematol. 2013;93:355.
Halpern S, Todd P, Kirby J. Hodgkin’s disease presenting with digital ischaemia. Clin Exp Dermatol. 1994;19(4):330–1.
Jones NF, Imbriglia JE, Steen VD, Medsger TA. Surgery for scleroderma of the hand. J Hand Surg. 1987;12(3):391–400.
Eisendrath SJ. Psychiatric aspects of chronic pain. Neurology. 1995;45(12 Suppl 9):S26–34.
Miles AM. Upper limb ischemia after vascular access surgery: differential diagnosis and management. Semin Dial. 2000;13(5):312–5. Wiley Online Library.
Knox RC, Berman SS, Hughes JD, Gentile AT, Mills JL. Distal revascularization-interval ligation: a durable and effective treatment for ischemic steal syndrome after hemodialysis access. J Vasc Surg. 2002;36(2):250–6.
Wixon CL, Hughes JD, Mills JL. Understanding strategies for the treatment of ischemic steal syndrome after hemodialysis access. J Am Coll Surg. 2000;191(3):301–10.
Oh T, Davis N. Radial artery cannulation. Anaesth Intensive Care. 1975;3(1):12.
Mandel M, Dauchot P. Radial artery cannulation in 1,000 patients: precautions and complications. J Hand Surg. 1977;2(6):482–5.
Annane D, Bellissant E, Cavaillon J-M. Septic shock. Lancet. 2005;365(9453):63–78.
Epstein FH, Parrillo JE. Pathogenetic mechanisms of septic shock. N Engl J Med. 1993;328(20):1471–7.
Ciervo A, Kahn M, Pangilinan AJ, Dardik H. Absence of the brachial artery: report of a rare human variation and review of upper extremity arterial anomalies. J Vasc Surg. 2001;33(1):191–4.
Uglietta JP, Kadir S. Arteriographic study of variant arterial anatomy of the upper extremities. Cardiovasc Intervent Radiol. 1989;12(3):145–8.
Marvi U, Chung L. Digital ischemic loss in systemic sclerosis. Int J Rheumatol. 2010;2010:1. PubMed PMID: 20871838, Pubmed Central PMCID: PMC2943156.
Steen V, Denton CP, Pope JE, Matucci-Cerinic M. Digital ulcers: overt vascular disease in systemic sclerosis. Rheumatology (Oxford). 2009;48 Suppl 3:iii19–24. PubMed PMID: 19487218.
Korn JH, Mayes M, Matucci Cerinic M, Rainisio M, Pope J, Hachulla E, et al. Digital ulcers in systemic sclerosis: prevention by treatment with bosentan, an oral endothelin receptor antagonist. Arthritis Rheum. 2004;50(12):3985–93. PubMed PMID: 15593188.
Galluccio F, Matucci-Cerinic M. Two faces of the same coin: Raynaud phenomenon and digital ulcers in systemic sclerosis. Autoimmun Rev. 2011;10(5):241–3. PubMed PMID: 20863907.
Hummers LK, Wigley FM. Management of Raynaud’s phenomenon and digital ischemic lesions in scleroderma. Rheum Dis Clin North Am. 2003;29(2):293–313. PubMed PMID: 12841296.
Milburn PB, Singer JZ, Milburn MA. Treatment of scleroderma skin ulcers with a hydrocolloid membrane. J Am Acad Dermatol. 1989;21(2 Pt 1):200–4. PubMed PMID: 2768569.
Gahhos F, Ariyan S, Frazier WH, Cuono CB. Management of sclerodermal finger ulcers. J Hand Surg. 1984;9(3):320–7. PubMed PMID: 6725888.
Tomaino MM, Goitz RJ, Medsger TA. Surgery for ischemic pain and Raynaud’s’ phenomenon in scleroderma: a description of treatment protocol and evaluation of results. Microsurgery. 2001;21(3):75–9.
Chung L. Therapeutic options for digital ulcers in patients with systemic sclerosis. J Ger Soc Dermatol. 2007;5(6):460–5.
Thompson AE, Shea B, Welch V, Fenlon D, Pope JE. Calcium-channel blockers for Raynaud’s phenomenon in systemic sclerosis. Arthritis Rheum. 2001;44(8):1841–7. PubMed PMID: 11508437.
Thompson AE, Pope JE. Calcium channel blockers for primary Raynaud’s phenomenon: a meta-analysis. Rheumatology (Oxford). 2005;44(2):145–50. PubMed PMID: 15546967.
Rademaker M, Cooke ED, Almond NE, Beacham JA, Smith RE, Mant TG, et al. Comparison of intravenous infusions of iloprost and oral nifedipine in treatment of Raynaud’s phenomenon in patients with systemic sclerosis: a double blind randomised study. BMJ. 1989;298(6673):561–4. PubMed PMID: 2467711, Pubmed Central PMCID: PMC1835951.
Meyrick Thomas RH, Rademaker M, Grimes SM, MacKay A, Kovacs IB, Cook ED, et al. Nifedipine in the treatment of Raynaud’s phenomenon in patients with systemic sclerosis. Br J Dermatol. 1987;117(2):237–41. PubMed PMID: 3307894.
Tingey T, Shu J, Smuczek J, Pope J. A meta-analysis of healing and prevention of digital ulcers (DU) in systemic sclerosis (SSc). Arthritis Care Res. 2013;65:1460. PubMed PMID: 23554239.
Pope J, Fenlon D, Thompson A, Shea B, Furst D, Wells G, et al. Prazosin for Raynaud’s phenomenon in progressive systemic sclerosis. Cochrane Database Syst Rev. 2000 (2):CD000956. PubMed PMID: 10796398.
Paterna S, Pinto A, Arrostuto A, Cannavo MG, Di Pasquale P, Cottone C, et al. Raynaud’s phenomenon: effects of terazosin. Minerva Cardioangiol. 1997;45(5):215–21. PubMed PMID: 9273472, Il fenomeno di Raynaud: effetti della terazosina. ita.
Gliddon AE, Dore CJ, Black CM, McHugh N, Moots R, Denton CP, et al. Prevention of vascular damage in scleroderma and autoimmune Raynaud’s phenomenon: a multicenter, randomized, double-blind, placebo-controlled trial of the angiotensin-converting enzyme inhibitor quinapril. Arthritis Rheum. 2007;56(11):3837–46. PubMed PMID: 17968938.
Chung L, Shapiro L, Fiorentino D, Baron M, Shanahan J, Sule S, et al. MQX-503, a novel formulation of nitroglycerin, improves the severity of Raynaud’s phenomenon: a randomized, controlled trial. Arthritis Rheum. 2009;60(3):870–7. PubMed PMID: 19248104.
Coleiro B, Marshall SE, Denton CP, Howell K, Blann A, Welsh KI, et al. Treatment of Raynaud’s phenomenon with the selective serotonin reuptake inhibitor fluoxetine. Rheumatology (Oxford). 2001;40(9):1038–43. PubMed PMID: 11561116.
Arefiev K, Fiorentino DF, Chung L. Endothelin receptor antagonists for the treatment of Raynaud’s phenomenon and digital ulcers in systemic sclerosis. Int J Rheumatol. 2011;2011:201787. PubMed PMID: 22121371, Pubmed Central PMCID: PMC3205679.
Jain M, Varga J. Bosentan for the treatment of systemic sclerosis-associated pulmonary arterial hypertension, pulmonary fibrosis and digital ulcers. Expert Opin Pharmacother. 2006;7(11):1487–501. PubMed PMID: 16859432.
Matucci-Cerinic M, Denton CP, Furst DE, Mayes MD, Hsu VM, Carpentier P, et al. Bosentan treatment of digital ulcers related to systemic sclerosis: results from the RAPIDS-2 randomised, double-blind, placebo-controlled trial. Ann Rheum Dis. 2011;70(1):32–8. PubMed PMID: 20805294, Pubmed Central PMCID: PMC3002766.
Parisi S, Peroni CL, Lagana A, Scarati M, Ambrogio F, Bruzzone M, et al. Efficacy of ambrisentan in the treatment of digital ulcers in patients with systemic sclerosis: a preliminary study. Rheumatology (Oxford). 2013;52(6):1142–4. PubMed PMID: 23463806.
Chung L, Arefiev K, Yaqub A, Strahs D, Lingala B, Fiorentino D. Effect of the ETA selective endothelin receptor antagonist ambrisentan on digital ulcers in patients with systemic sclerosis: results of a prospective pilot study [Abstract]. Arthritis Rheum. 2011;63(Suppl):S259.
Pulido T, Adzerikho I, Channick RN, Delcroix M, Galie N, Ghofrani HA, et al. Macitentan and morbidity and mortality in pulmonary arterial hypertension. N Engl J Med. 2013;369(9):809–18. PubMed PMID: 23984728.
Brueckner CS, Becker MO, Kroencke T, Huscher D, Scherer HU, Worm M, et al. Effect of sildenafil on digital ulcers in systemic sclerosis: analysis from a single centre pilot study. Ann Rheum Dis. 2010;69(8):1475–8. PubMed PMID: 19900936, Pubmed Central PMCID: PMC2938897.
Herrick AL, van den Hoogen F, Gabrielli A, Tamimi N, Reid C, O’Connell D, et al. Modified-release sildenafil reduces Raynaud’s phenomenon attack frequency in limited cutaneous systemic sclerosis. Arthritis Rheum. 2011;63(3):775–82. PubMed PMID: 21360507.
Shenoy PD, Kumar S, Jha LK, Choudhary SK, Singh U, Misra R, et al. Efficacy of tadalafil in secondary Raynaud’s phenomenon resistant to vasodilator therapy: a double-blind randomized cross-over trial. Rheumatology (Oxford). 2010;49(12):2420–8. PubMed PMID: 20837499.
Schiopu E, Hsu VM, Impens AJ, Rothman JA, McCloskey DA, Wilson JE, et al. Randomized placebo-controlled crossover trial of tadalafil in Raynaud’s phenomenon secondary to systemic sclerosis. J Rheumatol. 2009;36(10):2264–8. PubMed PMID: 19755613.
Barreira RI, Garcia BB, Lopez MG, Legazpi IR, Diaz HA, Penin IR. Paradoxical reaction of Raynaud phenomenon following the repeated administration of iloprost in a patient with diffuse cutaneous systemic sclerosis. Ann Pharmacother. 2012;46(10):e28. PubMed PMID: 23032649.
Pope J, Fenlon D, Thompson A, Shea B, Furst D, Wells G, et al. Iloprost and cisaprost for Raynaud’s phenomenon in progressive systemic sclerosis. Cochrane Database Syst Rev. 2000 (2):CD000953. PubMed PMID: 10796395
Wigley FM, Korn JH, Csuka ME, Medsger Jr TA, Rothfield NF, Ellman M, et al. Oral iloprost treatment in patients with Raynaud’s phenomenon secondary to systemic sclerosis: a multicenter, placebo-controlled, double-blind study. Arthritis Rheum. 1998;41(4):670–7. PubMed PMID: 9550476.
Vayssairat M. Preventive effect of an oral prostacyclin analog, beraprost sodium, on digital necrosis in systemic sclerosis. French Microcirculation Society Multicenter Group for the Study of Vascular Acrosyndromes. J Rheumatol. 1999;26(10):2173–8. PubMed PMID: 10529135.
Lau CS, Belch JJ, Madhok R, Cappell H, Herrick A, Jayson M, et al. A randomised, double-blind study of cicaprost, an oral prostacyclin analogue, in the treatment of Raynaud’s phenomenon secondary to systemic sclerosis. Clin Exp Rheumatol. 1993;11(1):35–40. PubMed PMID: 8453795.
Seibold, Wigley JR, Schiopu F, Denton E, Silver CD, Steen RM, Medsger Jr VD, et al. Digital ischemic ulcers in scleroderma treated with oral treprostinil diethanolamine: a randomized, double- blind, placebo-controlled, multicenter study [abstract]. Arthritis Rheum. 2011;63(Suppl):S968.
Kowal-Bielecka O, Landewe R, Avouac J, Chwiesko S, Miniati I, Czirjak L, et al. EULAR recommendations for the treatment of systemic sclerosis: a report from the EULAR Scleroderma Trials and Research group (EUSTAR). Ann Rheum Dis. 2009;68(5):620–8. PubMed PMID: 19147617.
Wigley FM, Seibold JR, Wise RA, McCloskey DA, Dole WP. Intravenous iloprost treatment of Raynaud’s phenomenon and ischemic ulcers secondary to systemic sclerosis. J Rheumatol. 1992;19(9):1407–14. PubMed PMID: 1279170.
Wigley FM, Wise RA, Seibold JR, McCloskey DA, Kujala G, Medsger Jr TA, et al. Intravenous iloprost infusion in patients with Raynaud phenomenon secondary to systemic sclerosis. A multicenter, placebo-controlled, double-blind study. Ann Intern Med. 1994;120(3):199–206.
Bali G, Schwantzer G, Aberer F, Kraenke B, Aberer E. Discontinuing long-term Iloprost treatment for Raynaud’s Phenomenon and systemic sclerosis: a single-center, randomized, placebo-controlled, double-blind study. Acta Dermatovenerol Alp Panonica Adriat. 2011;20(1):13–21. PubMed PMID: 21879200.
Scorza R, Caronni M, Mascagni B, Berruti V, Bazzi S, Micallef E, et al. Effects of long-term cyclic iloprost therapy in systemic sclerosis with Raynaud’s phenomenon. A randomized, controlled study. Clin Exp Rheumatol. 2001;19(5):503–8. PubMed PMID: 11579708.
Kawald A, Burmester GR, Huscher D, Sunderkotter C, Riemekasten G. Low versus high-dose iloprost therapy over 21 days in patients with secondary Raynaud’s phenomenon and systemic sclerosis: a randomized, open, single-center study. J Rheumatol. 2008;35(9):1830–7. PubMed PMID: 18634152.
Opitz C, Klein-Weigel PF, Riemekasten G. Systemic sclerosis - a systematic overview: Part 2 - immunosuppression, treatment of SSc-associated vasculopathy, and treatment of pulmonary arterial hypertension. VASA Zeitschrift fur Gefasskrankheiten. 2011;40(1):20–30. PubMed PMID: 21283970.
Badesch DB, Tapson VF, McGoon MD, Brundage BH, Rubin LJ, Wigley FM, et al. Continuous intravenous epoprostenol for pulmonary hypertension due to the scleroderma spectrum of disease. A randomized, controlled trial. Ann Intern Med. 2000;132(6):425–34.
Chung L, Fiorentino D. A pilot trial of treprostinil for the treatment and prevention of digital ulcers in patients with systemic sclerosis. J Am Acad Dermatol. 2006;54(5):880–2. PubMed PMID: 16635673.
Beckett VL, Conn DL, Fuster V, Osmundson PJ, Strong CG, Chao EY, et al. Trial of platelet-inhibiting drug in scleroderma. Double-blind study with dipyridamole and aspirin. Arthritis Rheum. 1984;27(10):1137–43. PubMed PMID: 6386002.
Herrick AL. Management of Raynaud’s phenomenon and digital ischemia. Curr Rheumatol Rep. 2013;15(1):303. PubMed PMID: 23292819.
Rajagopalan S, Pfenninger D, Somers E, Kehrer C, Chakrabarti A, Mukherjee D, et al. Effects of cilostazol in patients with Raynaud’s syndrome. Am J Cardiol. 2003;92(11):1310–5. PubMed PMID: 14636909.
Neiko Ie M, Iatsyshyn RI. Use of pentoxifylline in the treatment of systemic scleroderma. Likars’ka sprava/Ministerstvo okhorony zdorov’ia Ukrainy. 2002;1:97–102. PubMed PMID: 11944397, Zastosuvannia pentoksyfilinu v likuvanni systemnoi sklerodermii. ukr.
Stevens JW, Simpson E, Harnan S, Squires H, Meng Y, Thomas S, et al. Systematic review of the efficacy of cilostazol, naftidrofuryl oxalate and pentoxifylline for the treatment of intermittent claudication. Br J Surg. 2012;99(12):1630–8. PubMed PMID: 23034699.
Neirotti M, Longo F, Molaschi M, Macchione C, Pernigotti L. Functional vascular disorders: treatment with pentoxifylline. Angiology. 1987;38(8):575–80. PubMed PMID: 3631642.
Kuwana M, Kaburaki J, Okazaki Y, Yasuoka H, Kawakami Y, Ikeda Y. Increase in circulating endothelial precursors by atorvastatin in patients with systemic sclerosis. Arthritis Rheum. 2006;54(6):1946–51. PubMed PMID: 16729283.
Abou-Raya A, Abou-Raya S, Helmii M. Statins: potentially useful in therapy of systemic sclerosis-related Raynaud’s phenomenon and digital ulcers. J Rheumatol. 2008;35(9):1801–8. PubMed PMID: 18709692.
Stone AV, Koman LA, Callahan MF, Eckman DM, Smith BP, Plate JF, et al. The effect of botulinum neurotoxin-A on blood flow in rats: a potential mechanism for treatment of Raynaud phenomenon. J Hand Surg. 2012;37(4):795–802. PubMed PMID: 22386546.
Fregene A, Ditmars D, Siddiqui A. Botulinum toxin type A: a treatment option for digital ischemia in patients with Raynaud’s phenomenon. J Hand Surg. 2009;34(3):446–52. PubMed PMID: 19258141.
Iorio ML, Masden DL, Higgins JP. Botulinum toxin A treatment of Raynaud’s phenomenon: a review. Semin Arthritis Rheum. 2012;41(4):599–603. PubMed PMID: 21868066.
Van Beek AL, Lim PK, Gear AJ, Pritzker MR. Management of vasospastic disorders with botulinum toxin A. Plast Reconstr Surg. 2007;119(1):217–26. PubMed PMID: 17255677.
Neumeister MW. Botulinum toxin type A in the treatment of Raynaud’s phenomenon. J Hand Surg. 2010;35(12):2085–92. PubMed PMID: 21134617.
Neumeister MW, Chambers CB, Herron MS, Webb K, Wietfeldt J, Gillespie JN, et al. Botox therapy for ischemic digits. Plast Reconstr Surg. 2009;124(1):191–201. PubMed PMID: 19568080.
Fiori G, Galluccio F, Braschi F, Amanzi L, Miniati I, Conforti ML, et al. Vitamin E gel reduces time of healing of digital ulcers in systemic sclerosis. Clin Exp Rheumatol. 2009;3 Suppl 54:51–4. PubMed PMID: 19796562.
Nelson C. Scleroderma complicates Raynaud’s emergencies. Skin and Allergy News. 2005.
Wigley FM, Wung PK. Painful digital ulcers in a scleroderma patient with Raynaud’s phenomenon, Case studies in systemic sclerosis. New York, NY: Springer; 2011. p. 95–105.
Haxton HA. Chemical sympathectomy. Br Med J. 1949;1(4614):1026.
Royle JP. A history of sympathectomy. Aust N Z J Surg. 1999;69(4):302–7.
McCall TE, Petersen DP, Wong LB. The use of digital artery sympathectomy as a salvage procedure for severe ischemia of Raynaud’s disease and phenomenon. J Hand Surg. 1999;24(1):173–7.
Flatt AE. Digital artery sympathectomy. J Hand Surg. 1980;5(6):550–6.
GIFFORD RW, HINES EA, CRAIG WM. Sympathectomy for Raynaud’s phenomenon follow-up study of 70 women with Raynaud’s disease and 54 women with secondary Raynaud’s phenomenon. Circulation. 1958;17(1):5–13.
Elias M. Cervical sympathetic and stellate ganglion blocks. Pain Physician. 2000;3(3):294–304.
El-Gammal T, Blair W. Digital periarterial sympathectomy for ischaemic digital pain and ulcers. J Hand Surg Br. 1991;16(4):382–5.
Wilgis E. Evaluation and treatment of chronic digital ischemia. Ann Surg. 1981;193(6):693.
Gordon A, Zechmeister K, Collin J. The role of sympathectomy in current surgical practice. Eur J Vasc Surg. 1994;8(2):129–37.
Ruch DS, Holden M, Smith BP, Smith TL, Koman LA. Periarterial sympathectomy in scleroderma patients: intermediate-term follow-up. J Hand Surg. 2002;27(2):258–64.
Koman LA, Urbaniak JR. Ulnar artery insufficiency: a guide to treatment. J Hand Surg. 1981;6(1):16–24.
Tomaino M. Digital arterial occlusion in scleroderma: is there a role for digital arterial reconstruction? J Hand Surg Br. 2000;25(6):611–3.
Koman LA, Ruch DS, Aldridge M, Smith BP, Holden MB, Fulcher M. Arterial reconstruction in the ischemic hand and wrist: effects on microvascular physiology and health-related quality of life. J Hand Surg. 1998;23(5):773–82.
Jones NF, Raynor SC, Medsger TA. Microsurgical revascularisation of the hand in scleroderma. Br J Plast Surg. 1987;40(3):264–9.
Bogoch ER, Gross DK. Surgery of the hand in patients with systemic sclerosis: outcomes and considerations. J Rheumatol. 2005;32(4):642–8.
Ozgocmen S, Kaya A, Coskun BK. Topical lidocaine helps reduce pain of digital ulcers in systemic sclerosis (scleroderma). Clin Rheumatol. 2006;25(3):378–9. PubMed PMID: 16211339.
Nihtyanova SI, Brough GM, Black CM, Denton CP. Clinical burden of digital vasculopathy in limited and diffuse cutaneous systemic sclerosis. Ann Rheum Dis. 2008;67(1):120–3. PubMed PMID: 17660220.
McMahan ZH, Hummers LK. Systemic sclerosis – challenges for clinical practice. Nat Rev Rheumatol. 2013;9(2):90–100. PubMed PMID: 23147899.
Hachulla E, Clerson P, Launay D, Lambert M, Morell-Dubois S, Queyrel V, et al. Natural history of ischemic digital ulcers in systemic sclerosis: single-center retrospective longitudinal study. J Rheumatol. 2007;34(12):2423–30. PubMed PMID: 17985402.
Sebastiani M, Manfredi A, Colaci M, D’Amico R, Malagoli V, Giuggioli D, et al. Capillaroscopic skin ulcer risk index: a new prognostic tool for digital skin ulcer development in systemic sclerosis patients. Arthritis Rheum. 2009;61(5):688–94. PubMed PMID: 19405007.
Zhang W, Xu JR, Lu Q, Ye S, Liu XS. High-resolution magnetic resonance angiography of digital arteries in SSc patients on 3 Tesla: preliminary study. Rheumatology (Oxford). 2011;50(9):1712–9. PubMed PMID: 21693547.
Wang J, Yarnykh VL, Molitor JA, Nash RA, Chu B, Wilson GJ, et al. Micro magnetic resonance angiography of the finger in systemic sclerosis. Rheumatology (Oxford). 2008;47(8):1239–43. PubMed PMID: 18559373.
Allanore Y, Seror R, Chevrot A, Kahan A, Drape JL. Hand vascular involvement assessed by magnetic resonance angiography in systemic sclerosis. Arthritis Rheum. 2007;56(8):2747–54. PubMed PMID: 17665441.
Herrick AL, Oogarah PK, Freemont AJ, Marcuson R, Haeney M, Jayson MI. Vasculitis in patients with systemic sclerosis and severe digital ischaemia requiring amputation. Ann Rheum Dis. 1994;53(5):323–6. PubMed PMID: 8017986, Pubmed Central PMCID: PMC1005331.
Hung EW, Mayes MD, Sharif R, Assassi S, Machicao VI, Hosing C, et al. Gastric antral vascular ectasia and its clinical correlates in patients with early diffuse systemic sclerosis in the SCOT trial. J Rheumatol. 2013;40(4):455–60. PubMed PMID: 23418384, Pubmed Central PMCID: PMC3652008.
Denton CP, Howell K, Stratton RJ, Black CM. Long-term low molecular weight heparin therapy for severe Raynaud’s phenomenon: a pilot study. Clin Exp Rheumatol. 2000;18(4):499–502. PubMed PMID: 10949727.
Hart DA, Fritzler MJ. Regulation of plasminogen activators and their inhibitors in rheumatic diseases: new understanding and the potential for new directions. J Rheumatol. 1989;16(9):1184–91. PubMed PMID: 2681762.
Bridges AJ, Spadone DP. Tissue plasminogen activator treatment of digital thrombosis in severe Raynaud’s phenomenon – a case report. Angiology. 1993;44(7):566–9. PubMed PMID: 8328685.
Lakshminarayanan S, Vazquez-Abad D, Maestrello SJ, Waterman JR. Treatment of severe Raynaud’s phenomenon and ischemic ulcerations with tissue plasminogen activator. Clin Exp Rheumatol. 1999;17(2):260. PubMed PMID: 10342058.
Ciompi ML, Bazzichi L, Melchiorre D, De Giorgio F, Bondi F, Puccetti L. A placebo-controlled study on urokinase therapy in systemic sclerosis. Biomed Pharmacother. 1996;50(8):363–8. PubMed PMID: 8952856.
Leclère FM, Mordon S, Schoofs M. Acute digital ischemia: a neglected microsurgical emergency. Report of 17 patients and literature review. Microsurgery. 2010;30(3):207–13.
Eyers P, Earnshaw J. Acute non-traumatic arm ischaemia. Br J Surg. 1998;85(10):1340–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Valenzuela, A., Adeduntan, R., Chung, L. (2015). Management of Digital Ischemia. In: Wigley, F., Herrick, A., Flavahan, N. (eds) Raynaud’s Phenomenon. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-1526-2_21
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1526-2_21
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-1525-5
Online ISBN: 978-1-4939-1526-2
eBook Packages: MedicineMedicine (R0)