Abstract
This chapter is focused on the discussion and review of cytomorphological features of benign and malignant lymph node lesions in lymph node FNA. The lymph node may harbor a variety of reactive, infectious, and tumorous lesions. The tumors in the lymph node can be primary, such as lymphoma, or metastatic diseases. Accurate on-site diagnosis is important for a better triaging of the specimen. Ancillary testing in lymph node FNA is often needed for more specific diagnoses that can be reached in the majority of cases.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
5.1 Image-Based Questions 1–34 (Some Images Have More Than One Question)

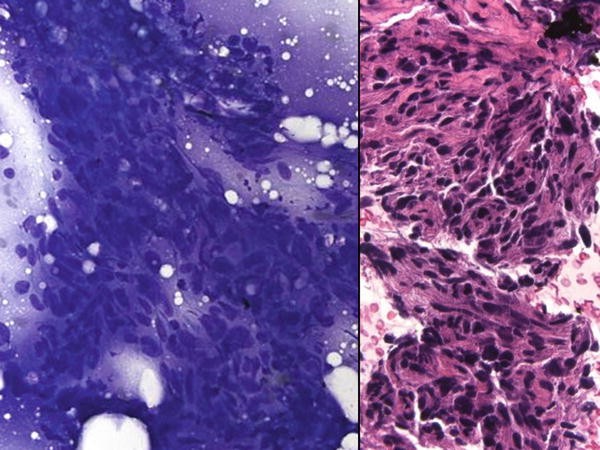
Fig. 5.1
-
Q-1. A 26-year-old nonsmoker female undergoes FNA of an enlarged cervical lymph node. The following are reprehensive images from ThinPrep preparation (Pap stain). Given the age of the patient and the cytomorphology, what are the most likely diagnosis and the appropriate stain to confirm the diagnosis?
-
(a)
Reactive lymphocytes and histiocytes (LCA and CD68)
-
(b)
Metastatic lung adenocarcinoma (TTF1)
-
(c)
Metastatic carcinoma (Pan CK, AE1/AE3)
-
(d)
Lymphoma (CD20 and CD3)
-
(e)
Metastatic papillary thyroid carcinoma (TTF1 and thyroglobulin)

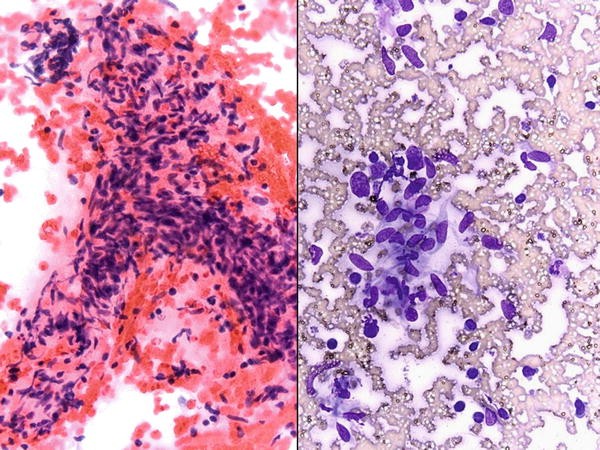
Fig. 5.2
-
(a)
-
Q-2. A 47-year-old female with a history of a colonic mass found to have cervical lymphadenopathy. She underwent FNA of one of the enlarged lymph node. Representative images from DQ-stained smear are below. The most likely diagnosis is:
-
(a)
Reactive hyperplasia
-
(b)
Metastatic melanoma
-
(c)
Metastatic mucinous adenocarcinoma
-
(d)
Posttransplant lymphoproliferative disorder
-
(e)
Diffuse large B-cell lymphoma

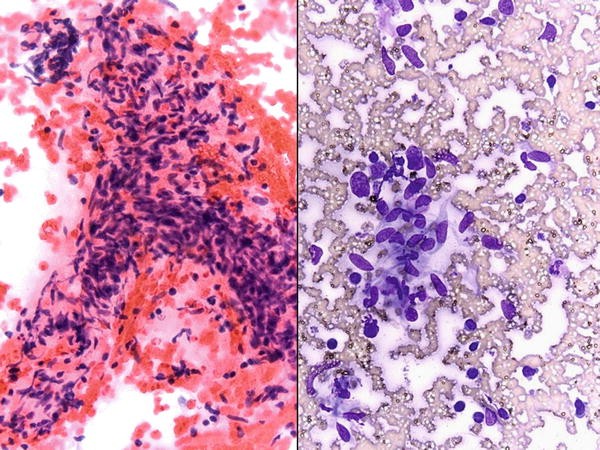
Fig. 5.3
-
(a)
-
Q-3. A 55-year-old male presents with an enlarged lymph node. A FNA of the lymph node demonstrates atypical lymphocytes seen in these images (DQ stain). The cells are positive for CD20 and CD10, while negative for CD5 and CD23. These cells are most likely to demonstrate which of the following translocation?
-
(a)
t(11;14)
-
(b)
t(14;18)
-
(c)
t(8:14)
-
(d)
t(8;22)
-
(e)
t(2;5)

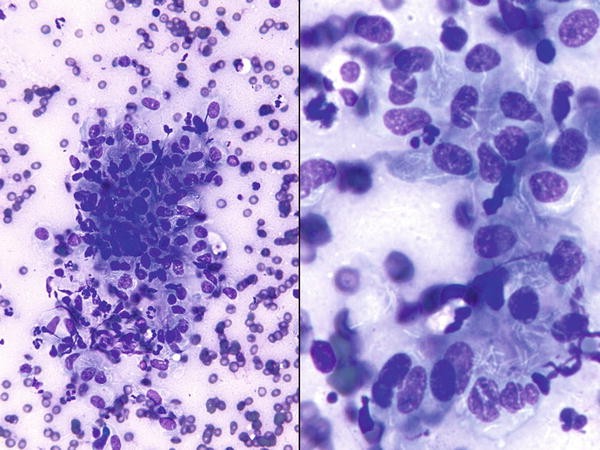
Fig. 5.4
-
(a)
-
Q-4. FNA of lymph node shows cells seen in these images (Pap stain). The patient is a 24-year-old male with previous diagnosis of malignancy. The best immunostain to confirm the diagnosis in this case is:
-
(a)
CD138
-
(b)
CK 5
-
(c)
Melan-A
-
(d)
CD3
-
(e)
OCT 3/4
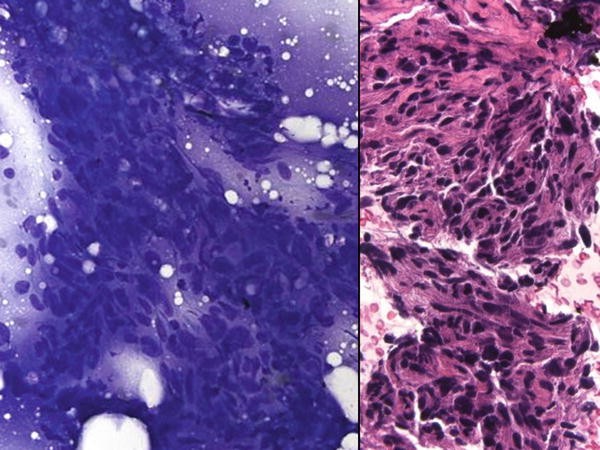
Fig. 5.5
-
(a)
-
Q-5. A 57-year-old female with a history of a previously treated retroperitoneal mass presents new-onset lymphadenopathy. A FNA is performed and demonstrates the cell pictured. The most likely diagnosis is:
-
(a)
Sarcoma
-
(b)
Melanoma
-
(c)
Lymphoma
-
(d)
Carcinoma
-
(e)
Infection

Fig. 5.6
-
(a)
-
Q-6. The neoplasm that is presented in these images most likely be positive for:
-
(a)
CD138
-
(b)
CK 5
-
(c)
Melan-A
-
(d)
CD3
-
(e)
OCT 3/4

Fig. 5.7
-
(a)
-
Q-7. This patient presented with pleural thickening and cervical lymphadenopathy. The pictured proliferation will most likely demonstrate positivity for:
-
(a)
WT1 and calretinin
-
(b)
Caldesmon and HMB45
-
(c)
CK 7 and mucicarmine
-
(d)
CD10 and PAX8
-
(e)
CD68 and CD168

Fig. 5.8
-
(a)
-
Q-8. The above findings are demonstrated during an on-site evaluation of a lymph node. The most appropriate next step is:
-
(a)
Request additional material for cell blocks
-
(b)
Request additional material for flow cytometry
-
(c)
Request additional material for molecular studies
-
(d)
Request additional material for culture
-
(e)
Request additional material for research

Fig. 5.9
-
(a)
-
Q-9. A 57-year-old female presents with an enlarged paraesophageal lymph node demonstrating the above findings. The most likely diagnosis is:
-
(a)
Adenocarcinoma
-
(b)
Squamous cell carcinoma
-
(c)
Glomus cell tumor
-
(d)
Small cell carcinoma
-
(e)
Adenosquamous carcinoma
Figs. 5.10 and 5.11
-
(a)
-
Q-10. A 27-year-old male with history of HIV/AIDS presents with an enlarged right supraclavicular lymph node. A FNA of the lymph node is pictured. What is the best confirmatory stain?
-
(a)
HTLV-1
-
(b)
HCV
-
(c)
CMV
-
(d)
EBV
-
(e)
HHV-8
-
(a)
-
Q-11. In the previously described case, the differential diagnosis includes all of the following except:
-
(a)
Angiosarcoma
-
(b)
Reactive lymphadenopathy
-
(c)
Melanoma
-
(d)
Hemangioma
-
(e)
Intranodal myofibroblastoma

Figs. 5.12 and 5.13
-
(a)
-
Q-12. A 22-year-old male with a history of malaise, mild fevers, and occasional headaches presents with several enlarged lymph nodes. Based on the image, the most likely diagnosis is:
-
(a)
Reactive viral lymphadenopathy
-
(b)
Toxoplasmosis
-
(c)
Castleman disease
-
(d)
Tuberculosis lymphadenitis
-
(e)
Cat scratch disease
-
(a)
-
Q-13. The most useful finding to substantiate the diagnosis in the previous image is:
-
(a)
Necrosis
-
(b)
Granuloma
-
(c)
Plasma cell proliferation
-
(d)
Infiltrating neutrophils
-
(e)
Mixed inflammatory response

Figs. 5.14 and 5.15
-
(a)
-
Q-14. A 53-year-old male presents with an enlarged axillary lymph node. Based on the above image, the stain most likely to confirm the diagnosis is:
-
(a)
CD138
-
(b)
LCA
-
(c)
Cytokeratin 7
-
(d)
Melan-A
-
(e)
Cytokeratin 20
-
(a)
-
Q-15. The previous image demonstrates a proliferation of large, atypical cells with scattered melanin pigment. The cell demonstrates a plasmacytoid morphology and occasional binucleation. The differential diagnosis includes all of the following except:
-
(a)
Multiple myeloma
-
(b)
Hodgkin lymphoma
-
(c)
Metastatic melanoma
-
(d)
Diffuse large B-cell lymphoma
-
(e)
Small cell carcinoma

Fig. 5.16
-
(a)
-
Q-16. An immunocompromised patient presents with lymphadenopathy and the pictured findings. The most likely diagnosis is:
-
(a)
Reactive lymphadenopathy
-
(b)
Cryptococcus neoformans
-
(c)
Trypanosoma cruzi
-
(d)
Leishmaniasis
-
(e)
Fat emboli

Fig. 5.17
-
(a)
-
Q-17. This is the lymph node FNA from a 7-year-old girl with an enlarged neck lymph node. What is the best preliminary diagnosis and triage of the specimen?
-
(a)
Suspicious for lymphoma; collect material for flow cytometry.
-
(b)
Suspicious for leukemia; collect material for flow cytometry.
-
(c)
Small round blue cell tumor; collect material for cell block and immunostains.
-
(d)
Acute suppurative lymphadenitis; collect material for microbial cultures.
-
(e)
Process additional material for cell block.

Fig. 5.18
-
(a)
-
Q-18. A 42-year-old female with a retroperitoneal mass undergoes an FNA. The mass demonstrates adipocytes with bone marrow hematopoietic elements including erythrocytes and megakaryocytes. Which of the following is true regarding myelolipomas?
-
(a)
HMB45 positive
-
(b)
HMB45 negative
-
(c)
Are small in size
-
(d)
Are not incidental findings
-
(e)
Are common

Fig. 5.19
-
(a)
-
Q-19. A 39-year-old male undergoes a biopsy of a persistently enlarged cervical lymph node. The FNA demonstrates mixed inflammation with rare large, irregular cells with binucleation and prominent nuclei. Which of the following is true regarding classical Hodgkin lymphoma?
-
(a)
It is usually CD30−, CD15−.
-
(b)
CD45 is usually positive.
-
(c)
Sclerosis is uncommon.
-
(d)
EBV stains LMP-1 in Reed-Sternberg cells.
-
(e)
It typically presents in young children.

Fig. 5.20
-
(a)
-
Q-20. An FNA of an enlarged lymph node is performed. The neoplasm consists of small lymphocytes with mature chromatin and minimal cytoplasm. Immunohistochemical stains demonstrate CD5 and CD23 positivity. Which of the following morphological features would not be consistent with the diagnosis?
-
(a)
Clumped chromatin
-
(b)
Plasmacytoid appearance
-
(c)
Increased prolymphocytes
-
(d)
Prominent nucleoli
-
(e)
Minimal cytoplasm

Fig. 5.21
-
(a)
-
Q-21. The above FNA demonstrates a proliferation of small to medium-sized lymphoid cells with mature chromatin with a suggestion of clustering. Immunohistochemical stains in the suspicious cells are positive for CD10, Bcl-2, and Bcl-6. They are negative for CD5. Which of the following is true regarding follicular lymphoma?
-
(a)
The translocation pattern genes are Bcl-6 and Bcl-2.
-
(b)
Grading is based on the number of centroblasts.
-
(c)
It is the second most common small cell lymphoma.
-
(d)
Ki-67 proliferation index does not help in grading.
-
(e)
Nuclear irregularities are uncommon.

Fig. 5.22
-
(a)
-
Q-22. A 7-year-old male presents with a rapidly enlarging mandibular lesion demonstrated in the following image composed of medium to large cells with smooth chromatin and multiple conspicuous nucleoli. There are occasional cytoplasmic vacuoles. The cells demonstrate a t(8;14) translocation. The most likely diagnosis is:
-
(a)
Follicular lymphoma
-
(b)
Anaplastic large cell lymphoma
-
(c)
Burkitt lymphoma
-
(d)
Blastic plasmacytoid dendritic cell neoplasm
-
(e)
Multiple myeloma

Fig. 5.23
-
(a)
-
Q-23. An FNA of an axillary neoplasm demonstrates the following image consisting of large cells with large atypical nuclei occasionally in hallmark or donut shapes. The neoplastic cells are positive for CD30 and ALK and negative for CD15. Which of the following is true regarding the proliferation?
-
(a)
ALK positivity confers a better prognosis.
-
(b)
It is associated with EBV.
-
(c)
Characteristic cells have prominent red nucleoli with binucleation.
-
(d)
The t(2:5) translocation partners are ALK and Bcl-2.
-
(e)
It typically presents in elderly.

Figs. 5.24 and 5.25
-
(a)
-
Q-24. A 56-year-old man presents with a localized rash with skin thickening and generalized lymphadenopathy. A fine-needle aspiration of an inguinal lymph node demonstrates a discohesive population of intermediate size cells with prominent pleomorphism including nuclear contour irregularities, prominent nucleoli, and variable chromatin patterns. The cells of interest are positive for CD2 and CD7 and negative for CD20. A biopsy of the skin lesion will most likely demonstrate:
-
(a)
Lichen sclerosis
-
(b)
Mycosis fungoides
-
(c)
Actinic keratosis
-
(d)
Folliculitis
-
(e)
Dermatofibrosarcoma protuberans
-
(a)
-
Q-25. Based on the previous image and findings, the cells of interest are mostly likely:
-
(a)
CD4+/CD8+/CD34−
-
(b)
CD4+/CD8−/CD34−
-
(c)
CD4−/CD8−/CD34−
-
(d)
CD4+/CD8+/CD34+
-
(e)
CD4+/CD8−/CD34+

Fig. 5.26
-
(a)
-
Q-26. An FNA of an enlarged lymph node demonstrates the pictured findings including a proliferation of small to medium cells, with mild nuclear pleomorphism and irregularity, inconspicuous nucleoli, and minimal cytoplasm. The cells are positive for CD20, CD5, and Bcl-2 and negative for CD10 and CD23. Which is true regarding Mantle cell lymphoma?
-
(a)
It rarely demonstrates a t(11;14) translocation.
-
(b)
The blastoid variant is usually cyclin D1 negative.
-
(c)
Cyclin D1 is specific to mantle cell lymphoma.
-
(d)
The cells are usually intermediate to large.
-
(e)
Bcl-1 is usually positive.

Figs. 5.27 and 5.28
-
(a)
-
Q-27. An FNA of an enlarged lymph node is pictured above and demonstrates a proliferation of large cells with extremely irregular nuclear contours and increased nuclear to cytoplasmic ratios. The cells are discohesive but focally clustered. There are prominent nucleoli and scattered lymphoglandular bodies are present. Which is true regarding diffuse large B-cell lymphoma?
-
(a)
Germinal center phenotype has a worse prognosis.
-
(b)
Germinal center phenotype has a better prognosis.
-
(c)
CD10 negativity is considered specific for non-germinal center type.
-
(d)
Non-germinal center phenotype has a better prognosis.
-
(e)
FOXP1 is not useful for determining germinal center type.
-
(a)
-
Q-28. If the cells in the previous FNA demonstrated CD5 positivity, what would be the most appropriate subsequent immunohistochemical stain to order?
-
(a)
CD20
-
(b)
CD138
-
(c)
TdT
-
(d)
Cyclin D1
-
(e)
Ki-67
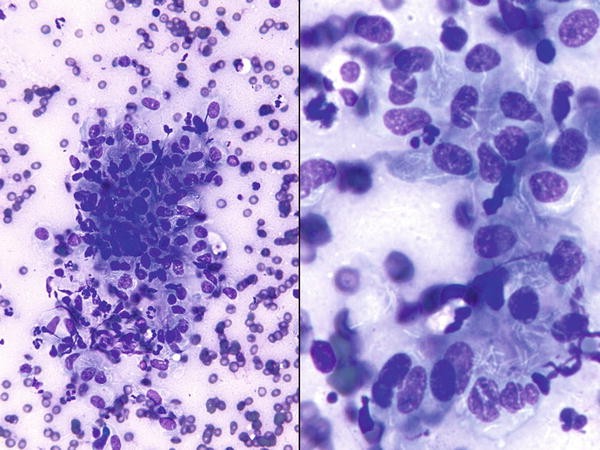
Fig. 5.29
-
(a)
-
Q-29. What is the most appropriate additional ancillary test after flow cytometry for the above sample?
-
(a)
Culture
-
(b)
Acid-fast stain
-
(c)
Cytochemical stains
-
(d)
Cut levels on the cell block
-
(e)
Viral PCR on the specimen

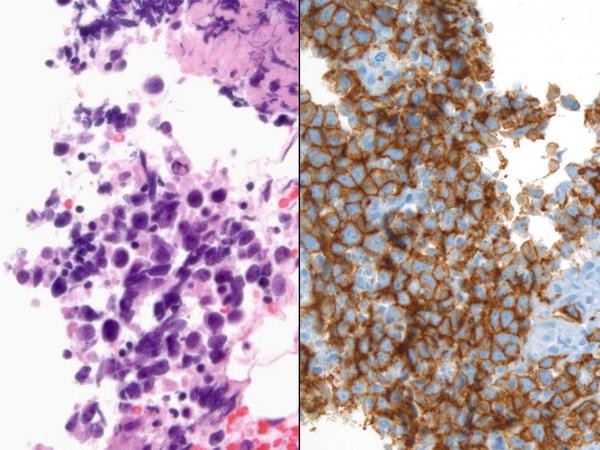
Figs. 5.30 and 5.31
-
(a)
-
Q-30. The pictured findings are most consistent with which diagnosis?
-
(a)
Diffuse large B-cell lymphoma
-
(b)
Seminoma
-
(c)
Reactive lymphadenopathy
-
(d)
Sarcoidosis
-
(e)
Metastatic melanoma
-
(a)
-
Q-31. The differential diagnosis of the above lesion includes all of the following except:
-
(a)
Metastatic melanoma
-
(b)
Metastatic squamous cell carcinoma
-
(c)
Poorly differentiated small cell carcinoma
-
(d)
Anaplastic large cell lymphoma
-
(e)
Metastatic prostate carcinoma
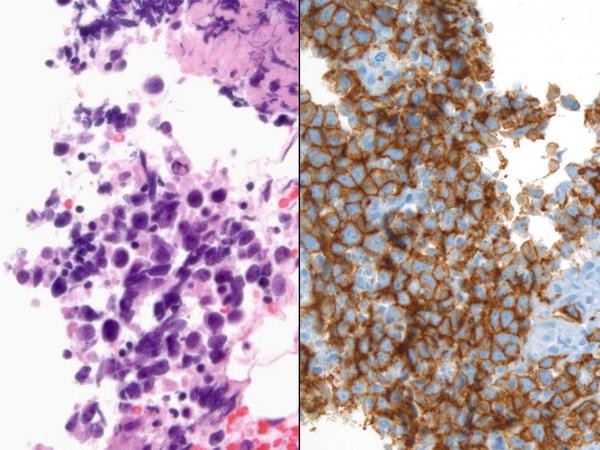
Fig. 5.32
-
(a)
-
Q-32. These images of cell block and immunostain of c-Kit corresponding to case seen in Q-30. Which of the following stains is most likely to confirm the above diagnosis?
-
(a)
PLAP
-
(b)
Melan-A
-
(c)
Congo red
-
(d)
Grocott
-
(e)
CK 20

Fig. 5.33
-
(a)
-
Q-33. A 65-year-old female with a history of a renal mass undergoes an FNA of an axillary lymph node. Which of the following is the most likely diagnosis?
-
(a)
Metastatic renal cell carcinoma
-
(b)
Metastatic thyroid carcinoma
-
(c)
Metastatic ovarian carcinoma
-
(d)
Plasma cell neoplasm
-
(e)
Metastatic liposarcoma

Fig. 5.34
-
(a)
-
Q-34. The images depict a predominant of single large markedly pleomorphic plasmacytoid cells with giant nucleoli. Which is the most likely diagnosis of this case?
-
(a)
Plasmacytoma
-
(b)
Kimura disease
-
(c)
Non-Hodgkin lymphoma (NHL)
-
(d)
Metastatic melanoma
-
(e)
Giant cell tumor of bone
-
(a)
5.2 Text-Based Questions 35–101
-
Q-35. Which of the following is true regarding sarcoidosis?
-
(a)
It typically presents in a single organ system.
-
(b)
Asteroid bodies are more common than Schaumann bodies.
-
(c)
Hamazaki-Wesenberg bodies may mimic fungi.
-
(d)
Granulomas are typically necrotizing.
-
(e)
Infectious etiologies do not need to be ruled out.
-
(a)
-
Q-36. Which of the following is true regarding Mycobacterium avium infections?
-
(a)
It is the second most common infections in patient with AIDS.
-
(b)
It rarely presents with granulomas.
-
(c)
Negative images of rod-shaped organisms are not seen.
-
(d)
Using auramine O does highlight the organism.
-
(e)
Positive acid-fast staining is specific to mycobacterium.
-
(a)
-
Q-37. Which of the following is false regarding the t(2;5) translocation in lymphoma cases?
-
(a)
It is present in many anaplastic large cell lymphomas.
-
(b)
The translocation partner genes are ALK and PMN.
-
(c)
It is seen in other neoplasms.
-
(d)
It is present in primary cutaneous ALCL.
-
(e)
It is the most frequent, but not the sole translocation seen in ALCL.
-
(a)
-
Q-38. Which of the following is true regarding Burkitt lymphoma?
-
(a)
The most common translocation is t(2;8).
-
(b)
The cells are positive for CD20, CD23, and Bcl-2.
-
(c)
The Ki-67 proliferation index is low.
-
(d)
It affects immunocompromised patients.
-
(e)
It most commonly involves the orbit.
-
(a)
-
Q-39. Hematolymphoid malignancies are the #1 cause of malignant effusions in which patient population?
-
(a)
Older men (age 60+)
-
(b)
Older women (age 60+)
-
(c)
Middle-age women
-
(d)
Middle-age men
-
(e)
Children/adolescents
-
(a)
-
Q-40. The most helpful morphologic feature to support reactive lymphoid hyperplasia (and exclude lymphoma) is which of the following?
-
(a)
Germinal center cells
-
(b)
Lymphoglandular bodies
-
(c)
Plasma cells
-
(d)
Histiocytes
-
(e)
Heterogeneity of the lymphoid population
-
(a)
-
Q-41. Which of the following cannot be reliably distinguished from reactive lymphoid hyperplasia by FNA?
-
(a)
Castleman disease
-
(b)
Dermatopathic lymphadenopathy
-
(c)
HIV-associated lymphadenopathy
-
(d)
Toxoplasma lymphadenitis
-
(e)
All of the above
-
(a)
-
Q-42. Lymphomas in patients receiving rituximab-containing chemotherapy are most likely to lose which marker?
-
(a)
CD19
-
(b)
CD20
-
(c)
CD38
-
(d)
CD10
-
(e)
CD23
-
(a)
-
Q-43. A 28-year-old man with a history of AIDS presents for FNA with new-onset cervical lymphadenopathy. The most likely diagnosis is:
-
(a)
Reactive lymphoid hyperplasia
-
(b)
Kaposi sarcoma
-
(c)
Tuberculosis
-
(d)
Cryptococcus neoformans
-
(e)
Non-Hodgkin lymphoma
-
(a)
-
Q-44. An FNA specimen demonstrates multiple acid-fast bacilli staining positive for the Ziehl-Neelsen technique intermixed with a mixed population of lymphocytes and histiocytes including foamy multinucleated cells with perinuclear vesicles. The most likely etiologic agent is;
-
(a)
Tuberculosis
-
(b)
Lepra bacilli
-
(c)
Cat scratch disease
-
(d)
Suppurative lymphadenitis
-
(e)
Actinomyces
-
(a)
-
Q-45. An FNA of a lymph node from a 7-year-old male who was scratched by a cat demonstrates suppurative lymphadenitis including stellate microabscesses. The best method to confirm the diagnosis is:
-
(a)
Special silver stains
-
(b)
Immunohistochemistry on the cell block
-
(c)
Cultures
-
(d)
Papanicolaou stain alone
-
(e)
Molecular testing
-
(a)
-
Q-46. A 25-year-old, Asian, male with an enlarged right cervical lymph node undergoes an FNA which demonstrates abundant karyorrhexis, small to medium histiocytes with irregular, angulated nuclear contours, abundant cytoplasmic debris, and plasmacytoid monocytes. The most appropriate therapeutic intervention is:
-
(a)
Lymph node biopsy
-
(b)
Lymph node excision
-
(c)
Neck dissection
-
(d)
Watch and wait
-
(e)
Antibiotics
-
(a)
-
Q-47. Flow cytometry performed on a lymph node FNA demonstrates an atypical population of CD19+, CD5+, CD23+, kappa-restricted lymphocytes. Which chromosomal abnormality portends a more aggressive phenotype?
-
(a)
13q14 deletion
-
(b)
17p deletion
-
(c)
17q addition
-
(d)
Trisomy 12
-
(e)
11p deletion
-
(a)
-
Q-48. A 42-year-old male recently returned from Brazil and presented with lymphadenopathy. A FNA demonstrates lymphocytes with admixed histiocytes containing cytoplasm expanded by small round cells with large nuclei, thin membranes, and small rod-shaped structures. The most likely diagnosis is:
-
(a)
Histoplasmosis
-
(b)
Leishmaniasis
-
(c)
Toxoplasmosis
-
(d)
Acute promyelocytic leukemia
-
(e)
Plasmodium vivax malaria
-
(a)
-
Q-49. A 12-year-old male presents with fevers, night sweats, and malaise. An FNA of a lymph node is performed which demonstrates abundant small lymphocytes and large histiocytes with abundant cytoplasm containing occasional lymphocytes. The most likely diagnosis is:
-
(a)
Leishmaniasis
-
(b)
Acute myelocytic leukemia
-
(c)
Reactive lymphoid hyperplasia
-
(d)
Rosai-Dorfman disease
-
(e)
Kikuchi lymphadenitis
-
(a)
-
Q-50. A FNA of a cervical lymph node demonstrates a mixed population of lymphocytes admixed with a minority population of large cell with irregular multilobated nuclei. Immunohistochemical stains are positive for CD20, EMA, and CD45 and negative for CD30 and CD15. The most likely diagnosis is:
-
(a)
Nodular-sclerosing Hodgkin lymphoma
-
(b)
Lymphocyte-depleted Hodgkin lymphoma
-
(c)
Nodular lymphocyte-predominant Hodgkin lymphoma
-
(d)
Lymphocyte-rich Hodgkin lymphoma
-
(e)
Mixed-cellularity Hodgkin lymphoma
-
(a)
-
Q-51. The most common variant of Hodgkin lymphoma in developing countries is:
-
(a)
Nodular sclerosing
-
(b)
Lymphocyte depleted
-
(c)
Nodular lymphocyte predominant
-
(d)
Lymphocyte predominant
-
(e)
Mixed cellularity
-
(a)
-
Q-52. A lymph node FNA demonstrates a proliferation of mixed sized lymphocytes positive for CD19, CD20, CD10, Bcl-6, and Bcl-2. The atypical cells are negative for CD5. The most likely molecular finding is:
-
(a)
t(14;18)
-
(b)
t(11;14)
-
(c)
t(8;22)
-
(d)
t(2;5)
-
(e)
t(x;18)
-
(a)
-
Q-53. Which small cell lymphoma generally lacks transformed lymphocytes?
-
(a)
Mantle cell lymphoma
-
(b)
CLL/SLL
-
(c)
Follicular lymphoma
-
(d)
Hodgkin lymphoma
-
(e)
Anaplastic large cell lymphoma
-
(a)
-
Q-54. A lymph node FNA demonstrates a predominant population of small lymphocytes including a dominant population of centrocytes and few centroblasts. Immunohistochemical stains demonstrate a population of CD5 negative and CD20 and 10 positive cells. FISH studies are most likely to demonstrate which finding?
-
(a)
t(14;18)(q32;q31)
-
(b)
t(14;18)(p32;p31)
-
(c)
t(14;18)(q32;p31)
-
(d)
t(11;14)
-
(e)
t(8;14)
-
(a)
-
Q-55. Mucosa-associated lymphoid tissue lymphoma is associated with which of the following:?
-
(a)
Rheumatoid arthritis
-
(b)
Pseudogout
-
(c)
Helicobacter pylori chronic gastritis
-
(d)
Ocular melanoma
-
(e)
Chronic bronchiolitis
-
(a)
-
Q-56. Which type of Burkitt lymphoma is most likely to demonstrate Epstein-Barr virus positivity?
-
(a)
None, EBV is not associated with Burkitt lymphoma.
-
(b)
Endemic type.
-
(c)
Immunodeficiency related.
-
(d)
Sporadic.
-
(e)
Diffuse T-cell predominant.
-
(a)
-
Q-57. A 43-year-old man with a history of AIDS presents with a rapidly enlarging inguinal lymph node. FNA of the lymph node demonstrated a proliferation of CD5−, CD10+, Bcl-6+, c-Myc positive, large B cells with extensive apoptosis and tingible body macrophages. The expected Ki-67 proliferation index is:
-
(a)
0 %
-
(b)
10 %
-
(c)
45 %
-
(d)
70 %
-
(e)
95 %
-
(a)
-
Q-58. Which of the following T-cell lymphomas is most likely to demonstrate a characteristic translocation?
-
(a)
Precursor T-cell lymphoblastic lymphoma
-
(b)
Anaplastic large cell lymphoma
-
(c)
Angioimmunoblastic T-cell lymphoma
-
(d)
Mycosis fungoides
-
(e)
Extranodal NK/T-cell lymphoma, nasal type
-
(a)
-
Q-59. A child is diagnosed with precursor T-cell lymphoblastic lymphoma. Which of the following is true of the disease?
-
(a)
Usually presents above the diaphragm.
-
(b)
Is associated with superior vena cava thrombosis.
-
(c)
Is easily distinguished immunophenotypically from thymoma.
-
(d)
Smears rarely demonstrate lymphoblasts.
-
(e)
TdT positivity is rarely demonstrated.
-
(a)
-
Q-60. Which virus is commonly associated with the development of post-transplant lymphoproliferative disorders (PTLD)?
-
(a)
CMV
-
(b)
HPV
-
(c)
HTLV-1
-
(d)
EBV
-
(e)
HIV
-
(a)
-
Q-61. A useful finding that helps distinguish between recurrent lymphoma and PTLD is:
-
(a)
Large, atypical cells
-
(b)
Positive EBV immunohistochemical stains in a minority of cells
-
(c)
High mitotic rate
-
(d)
Lymphoglandular bodies
-
(e)
Positive EBV immunohistochemical stains in a majority of cells
-
(a)
-
Q-62. Which neoplasm may demonstrate lymphoglandular bodies?
-
(a)
Nasopharyngeal carcinoma
-
(b)
Granular cell tumor
-
(c)
Melanoma
-
(d)
Ovarian papillary serous carcinoma
-
(e)
Medullary carcinoma
-
(a)
-
Q-63. Anaplastic large cell lymphoma may be confused with carcinoma because of which of the following features?
-
(a)
Many lymphoglandular bodies
-
(b)
Discohesiveness
-
(c)
EMA positivity
-
(d)
Monomorphism
-
(e)
Paucity of spindled cells
-
(a)
-
Q-64. Cluster designation 163 positivity is characteristic of which histiocytic neoplasm?
-
(a)
Langerhans cell histiocytosis
-
(b)
Langerhans cell sarcoma
-
(c)
Histiocytic sarcoma
-
(d)
Interdigitating dendritic cell sarcoma
-
(e)
Follicular dendritic cell sarcoma
-
(a)
-
Q-65. A 43-year-old male presents with an enlarging axillary mass and recent allergic dermatitis. A fine-needle aspiration of the axillary mass demonstrates many CD1a positive grooved cells and scattered pigment laden macrophages. The most likely diagnosis is:
-
(a)
Langerhans cell histiocytosis
-
(b)
Dermatopathic lymphadenopathy
-
(c)
Langerhans cell sarcoma
-
(d)
Myeloid sarcoma
-
(e)
Interdigitating dendritic cell sarcoma
-
(a)
-
Q-66. A FNA is performed on a perihilar lymph node and demonstrates a population of small to medium-sized cells with salt and pepper chromatin, nuclear molding, and some degeneration. The immunohistochemical stain most likely to be positive is:
-
(a)
CD3
-
(b)
CD20
-
(c)
CD56
-
(d)
Melanin
-
(e)
Oct4
-
(a)
-
Q-67. A FNA of a left axillary lymph node demonstrates a proliferation of large cells with prominent nucleoli and occasional binucleated forms mixed with scattered small lymphocytes. There are scatted pigmented cells and necrotic debris. Immunohistochemical stains demonstrate S100, HMB45, and Melan-A positivity. The most appropriate molecular test is:
-
(a)
KRAS
-
(b)
BRAF
-
(c)
BRD4-NUT
-
(d)
t(2:5)
-
(e)
t(14;18)
-
(a)
-
Q-68. A useful technique to improve adequacy in lymph node FNA is:
-
(a)
A single pass at the periphery of the lesion
-
(b)
Using a smaller gauge needle
-
(c)
Applying anesthetic creams prior to the procedure
-
(d)
Performing multiple passes in different locations
-
(e)
Not stabilizing the lymph node prior to aspiration
-
(a)
-
Q-69. A monocytoid proliferation in a lymph node FNA suspicious for infectious mononucleosis is best confirmed by which method?
-
(a)
Monospot test
-
(b)
Clinical history
-
(c)
Urine screen
-
(d)
Breath test
-
(e)
Molecular testing
-
(a)
-
Q-70. Which of the following morphologic features is most useful in identifying metastatic colorectal carcinoma?
-
(a)
Intranuclear inclusions
-
(b)
Signet ring cells
-
(c)
Columnar cells and necrosis.
-
(d)
Brown pigment
-
(e)
Nuclear molding
-
(a)
-
Q-71. A 31-year-old female with a history of fevers underwent a FNA of an enlarged lymph node. A sample is sent for flow cytometric analysis. The generally accepted minimum number of events to ensure diagnostic accuracy is:
-
(a)
500 events
-
(b)
5,000 events
-
(c)
10,000 events
-
(d)
30,000 events
-
(e)
50,000 events
-
(a)
-
Q-72. Which of the following does not suffer from loss of important architectural changes for diagnosis on an FNA specimen?
-
(a)
Progressively transformed germinal centers
-
(b)
Castleman disease
-
(c)
CLL/SLL
-
(d)
Nodular lymphocyte-predominant Hodgkin lymphoma
-
(e)
Vascular transformation of lymph node sinuses
-
(a)
-
Q-73. Which of the following is not part of the differential diagnosis for sarcoidosis?
-
(a)
Melanoma
-
(b)
Infection
-
(c)
Foreign body reactions
-
(d)
Dendritic lymphocyte aggregates
-
(e)
Spindle-cell neoplasm
-
(a)
-
Q-74. Which of the following is not a feature of Kikuchi lymphadenitis?
-
(a)
Necrotic debris
-
(b)
Small phagocytic histiocytes
-
(c)
Cytoplasmic tingible body macrophages
-
(d)
Extensive neutrophilic infiltrate
-
(e)
Absence of neutrophilic infiltrate
-
(a)
-
Q-75. Which of the following diagnoses are not in the differential diagnosis of infectious mononucleosis?
-
(a)
Mantle cell lymphoma
-
(b)
Reactive lymphoid hyperplasia
-
(c)
Large cell lymphoma
-
(d)
Hodgkin lymphoma
-
(e)
Immunoblastic lymphoma
-
(a)
-
Q-76. Which of the following is not useful for differentiating anaplastic large cell lymphoma from classical Hodgkin lymphoma?
-
(a)
Number of malignant cells relative to lymphocytes
-
(b)
Morphology of the malignant cells
-
(c)
Staining pattern of epithelial membrane antigens
-
(d)
Molecular studies
-
(e)
Staining pattern of ALK
-
(a)
-
Q-77. Which of the following small lymphomas is generally considered the most aggressive?
-
(a)
CLL/SLL
-
(b)
Lymphoplasmacytic
-
(c)
Mantle cell lymphoma
-
(d)
Marginal zone/mucosal-associated lymphoid tissue lymphoma
-
(e)
Follicular lymphoma
-
(a)
-
Q-78. An 18-year-old male presents with a rapidly enlarging mandibular mass. A fine-needle aspiration demonstrates a starry-sky pattern of with extensive necrosis and composed of medium-sized lymphocytes with occasional vacuoles. The cells are positive for c-Myc. The most common translocation in these lymphomas is:
-
(a)
t(8;14)
-
(b)
t(2;5)
-
(c)
t(2;8)
-
(d)
t(8;22)
-
(e)
t(9;22)
-
(a)
-
Q-79. The c-Myc proto-oncogene is located on which chromosome?
-
(a)
14
-
(b)
22
-
(c)
8
-
(d)
2
-
(e)
9
-
(a)
-
Q-80. In addition to Burkitt lymphoma, c-Myc rearrangement may also be seen in which neoplasm?
-
(a)
Multiple myeloma
-
(b)
CLL/SLL
-
(c)
Mantle cell lymphoma
-
(d)
Hodgkin lymphoma
-
(e)
Castleman disease
-
(a)
-
Q-81. All of the following may mimic Bartonella lymphadenitis except:
-
(a)
Chlamydia trachomatis
-
(b)
Yersinia enterocolitica
-
(c)
Francisella tularensis
-
(d)
Pyogenic cocci
-
(e)
Epstein-Barr virus
-
(a)
-
Q-82. Which of the following is true regarding T-cell lymphoblastic lymphoma?
-
(a)
Most frequent in elderly males
-
(b)
Usually present with low leukocyte count
-
(c)
Comprise the majority of lymphoblastic lymphomas
-
(d)
Never present in mediastinum
-
(e)
Generally grow slowly
-
(a)
-
Q-83. A 47-year-old female presents with an enlarged axillary lymph node and a history of malaise and fevers. A fine-needle aspiration demonstrates small lymphocytes and numerous, irregular, cleaved lymphocytes with few tingible body macrophages. Immunohistochemical stains highlight the lymphocytes with CD10 and Bcl-6 and negative for CD5, CD23, and cyclin D1. Molecular studies for translocation 14;18 are positive. Which of the following diagnoses is most likely?
-
(a)
Follicular lymphoma
-
(b)
CLL/SLL
-
(c)
MCL
-
(d)
MZL
-
(e)
DLBCL
-
(a)
-
Q-84. An enlarged neck mass in a patient with a history of a thigh mass undergoes a FNA. The FNA demonstrates large cells with eosinophilic cytoplasm, eccentric nuclei, and scattered mitoses in a background of unremarkable small lymphocytes. The stains most likely to confirm the diagnosis are:
-
(a)
Desmin, myogenin, CD138, and SMA
-
(b)
CD138, wide-spectrum cytokeratin, CD5, CD45
-
(c)
HMB45, SMA, Melan-A, wide-spectrum cytokeratin
-
(d)
CD99, vimentin, wide-spectrum cytokeratin
-
(e)
PLAP, CA-125, WT-1
-
(a)
-
Q-85. Which molecular abnormality is most common in CLL/SLL?
-
(a)
Trisomy 12
-
(b)
del 11q22-23
-
(c)
del 13q14.3
-
(d)
del 17p13
-
(e)
del 6q21
-
(a)
-
Q-86. A FNA of an enlarged pelvic lymph node demonstrates dispersed large cleaved and non-cleaved cells. There are irregular nuclear profiles with occasional nuclear protrusions. There are occasional cytoplasmic vacuoles and the cells are discohesive. The differential diagnosis includes all the following except:
-
(a)
DLBCL
-
(b)
Metastatic melanoma
-
(c)
Small cell carcinoma
-
(d)
Seminoma
-
(e)
Pulmonary adenocarcinoma
-
(a)
-
Q-87. A specimen submitted for flow cytometric analysis suspicious for plasmacytoma is most likely to demonstrate which of the following immunophenotypic findings?
-
(a)
Surface kappa restriction, normal lambda
-
(b)
Surface lambda restriction, normal kappa
-
(c)
Cytoplasmic kappa restriction, normal lambda
-
(d)
Equal cytoplasmic kappa and lambda
-
(e)
Negativity for surface and cytoplasmic kappa and lambda
-
(a)
-
Q-88. Which cell population is most fragile and least likely to be accurately characterized on a flow cytometry sample that has been excessively delayed?
-
(a)
CD20-positive cells
-
(b)
CD138-positive cells
-
(c)
CD3-positive cells
-
(d)
CD13-positive cells
-
(e)
CD56 positive cells
-
(a)
-
Q-89. A patient presents with a gastric mass composed of a proliferation of lymphocytes consistent with a gastric mucosal-associated lymphoid tissue lymphoma. Special chemical stains highlight corkscrew-shaped organisms in the epithelium. What is the best next step in therapy?
-
(a)
Start triple therapy.
-
(b)
Gastric resection.
-
(c)
Perform a breath urease test.
-
(d)
Watch and wait.
-
(e)
Perform an endoscopic mucosal resection.
-
(a)
-
Q-90. A patient with an enlarged spleen undergoes a perisplenic lymph node FNA. This demonstrates multiple medium lymphocytes with asymmetric cytoplasmic buds but lacking cytoplasmic clearing. Imaging of the spleen revealed diffuse enlargement. Which immunophenotype is consistent with splenic marginal zone lymphoma?
-
(a)
CD103+, CD25+, CD23−
-
(b)
CD20+, CD79+, CD38+
-
(c)
CD20−, CD79+, CD138+
-
(d)
CD5+, CD23+, CD43+
-
(e)
CD5+, CD23−, CD10−
-
(a)
-
Q-91. Which immunophenotype is consistent with hairy cell leukemia?
-
(a)
CD103+, CD25+, CD23−
-
(b)
CD20+, CD79+, CD38+
-
(c)
CD20−, CD79+, CD138+
-
(d)
CD5+, CD23+, CD43+
-
(e)
CD5+, CD23−, CD10−
-
(a)
-
Q-92. Fine-needle aspiration of lymphoma and metastases is least sensitive for which of the following?
-
(a)
Non-Hodgkin lymphoma
-
(b)
Hodgkin lymphoma
-
(c)
Metastatic melanoma
-
(d)
Infections
-
(e)
Metastatic carcinoma
-
(a)
-
Q-93. Which of the following lymphomas is least likely in adults?
-
(a)
Diffuse large B cell
-
(b)
Small lymphocytic leukemia/chronic lymphocytic lymphoma
-
(c)
Follicular lymphoma
-
(d)
Endemic Burkitt lymphoma
-
(e)
Anaplastic large cell lymphoma
-
(a)
-
Q-94. A FNA of an enlarge lymph node demonstrates grape bunch-like clusters of cells with minimal cytoplasm and composed of cells ranging in size from 25 to 150 um in diameter consistent with Warthin-Finkeldey cells. These are associated with all of the following except:
-
(a)
Measles
-
(b)
Systemic lupus erythematosus
-
(c)
Kimura disease
-
(d)
Hodgkin lymphoma
-
(e)
Metastatic melanoma
-
(a)
-
Q-95. Which of the following is not associated with sinus histiocytosis?
-
(a)
Exogenous lipids
-
(b)
Rosai-Dorfman disease
-
(c)
Kikuchi disease
-
(d)
Whipple disease
-
(e)
Hodgkin lymphoma
-
(a)
-
Q-96. A patient with a history of systemic lupus erythematosus undergoes a FNA that demonstrates medium-sized cells with bright pink eosinophilic, hyaline-appearing bodies along with intermixed plasma cells. The eosinophilic material is composed of which of the following?
-
(a)
Denatured RNA and immunoglobulin
-
(b)
Denatured DNA and immunoglobulin
-
(c)
Immunoglobulin only
-
(d)
Amyloid
-
(e)
Calcium
-
(a)
-
Q-97. A 61-year-old man presents with an enlarged lymph node, bone pain, hypercalcemia, and a monoclonal gammopathy. A FNA of the lymph node demonstrates many plasma cells including occasional cells with strong metachromatic staining in the peripheral cytoplasm. The cells are referred to as which of the following?
-
(a)
Dutcher bodies
-
(b)
Flame cells
-
(c)
Russell bodies
-
(d)
Lymphoglandular bodies
-
(e)
Mott cells
-
(a)
-
Q-98. Which of the following is true regarding pediatric nodal marginal zone lymphoma?
-
(a)
It has a poor prognosis.
-
(b)
It most commonly presents in the groin.
-
(c)
It is predominantly in females.
-
(d)
It has the same immunophenotype as in adults.
-
(e)
It is easy to differentiate from reactive conditions.
-
(a)
-
Q-99. The most common mutation associated with ALK-positive large B-cell lymphoma is:
-
(a)
t(2;5)(p23;35)
-
(b)
t(2;17)(p23;q23)
-
(c)
Cryptic insertion of 3’ALK into 4q22-24
-
(d)
t(5;17)
-
(e)
t(9;22)(q34;p11.2)
-
(a)
-
Q-100. Which of the following is the most common B-cell lymphoma in adults?
-
(a)
Diffuse large B-cell lymphoma (DLBCL)
-
(b)
Follicular lymphoma
-
(c)
CLL/SLL
-
(d)
Mantle cell lymphoma
-
(e)
MALT lymphoma
-
(a)
-
Q-101. The most common mature T-cell lymphoma in adults is:
-
(a)
Peripheral T-cell lymphoma NOS
-
(b)
Angioimmunoblastic lymphoma
-
(c)
Extranodal natural killer/T-cell lymphoma
-
(d)
Hepatosplenic T-cell lymphoma
-
(e)
ALK+ anaplastic large cell lymphoma
-
(a)
5.3 Answers and Discussion of Image-Based Questions 1–34
-
A-1. (e) Metastatic papillary thyroid carcinoma (TTF1 and thyroglobulin)
The FNA demonstrates cohesive clusters of cells with increased nuclear to cytoplasmic ratios and nuclear irregularities suggestive of a metastatic carcinoma. Psammoma bodies are also present. Given the age of the patient, the location of the lymph node, and the cytomorphology features, this is most suggestive of metastatic papillary thyroid carcinoma. To confirm thyroid carcinoma, a positive thyroglobulin and TTF1 would be most useful. TTF-1, while positive in papillary thyroid carcinoma, like AE1/AE3, may be positive in a variety of other carcinomas. Calretinin is primarily used to identify mesothelial cells and LCA “common leukocyte antigen” is used to highlight lymphocytes.
-
A-2. (c) Metastatic mucinous adenocarcinoma
The history of a colon mass combined with the FNA findings of abundant mucin with scattered clusters of large, atypical cells with prominent nucleoli and increased nuclear to cytoplasmic ratios is most likely metastatic mucinous adenocarcinoma. A reactive hyperplastic lymph node should not demonstrate any mucin. Metastatic melanoma, PTLD, and DLBCL typically do not have abundant mucin production.
-
A-3. (b) t(14;18)
The t(14;18) translocation is seen in follicular lymphoma. The FNA demonstrates a proliferation of small to medium lymphocytes, primarily small cleaved centrocytes with occasional larger centroblasts. Many cells demonstrate characteristic extensive nuclear contour irregularities. The chromatin is coarse and nucleoli are inconspicuous. Follicular cell lymphoma usually is CD20+, CD10+, CD5−, and CD23−.
-
A-4. (c) Melan-A
The above FNA demonstrates a moderately cellular smear with dusty cytoplasm. These cells are dispersed as single cells with occasional aggregates. They are epithelioid with occasional binucleation. The cells have finely dispersed chromatin and prominent nucleoli. These features are most compatible with metastatic melanoma. Melan-A, along with S100 and HMB45, is positive in melanoma. Melanoma is notorious for presenting in a variety of forms and mimicking many neoplasms. CD138 is positive in plasma cells, CK 5 in squamous cell carcinoma and other carcinomas, CD3 in T lymphocytes, and OCT3/4 in intratubular germ cell neoplasia.
-
A-5. (a) Sarcoma
The FNA demonstrates a proliferation of spindled cells with many bizarre forms and intermixed necrosis. The history of a previous retroperitoneal mass and the morphologic findings support the diagnosis of a metastatic sarcoma. Melanoma may present with spindled cells and can be difficult to differentiate from sarcoma; however, the clinical history is supportive of a sarcoma. A lymphoma will be predominantly lymphocytes. Carcinomas tend to form clusters and also demonstrate epithelioid morphology. Soft tissue infections may cause reactive changes in the mesenchymal cells, but, generally, not proliferations to the degree demonstrated in the FNA.
-
A-6. (a) CD138 is positive in plasma cells.
The image demonstrates a proliferation of plasma cells with eccentric nuclei, clockface chromatin, and perinuclear hoffs suggesting a diagnosis of multiple myeloma/plasmacytoma. CK 5 is a basic, high-molecular-weight cytokeratin typically positive in squamous cell carcinoma. Melan-A is positive in melanoma. CD3 is positive in T lymphocytes. OCT3/4 is positive in germ cell neoplasia.
-
A-7. (a) WT-1 and calretinin
The image demonstrates a proliferation of mesothelial cells with large nuclei and nuclear contour irregularities. The cells have areas of clearing between cytoplasmic borders known as windows and are characteristic of mesothelial cells. The distinction between reactive mesothelial cells and a malignant mesothelioma can be difficult. In addition, differentiating between an adenocarcinoma and mesothelioma is challenging. Immunohistochemical stains may be useful. Mesothelial cells are positive for WT-1 and calponin. Caldesmon is seen in soft tissue neoplasm. HMB45 is a marker for melanoma and angiomyolipomas. CD7 and mucicarmine positivity would be seen in an adenocarcinoma. CD10 and PAX8 positivity is seen in clear cell renal cell carcinoma. CD68 and CD168 highlight macrophages/histiocytes.
-
A-8. (d) Request additional material for culture.
The FNA demonstrates multinucleated giant cells with a background of mixed lymphoplasmacytic inflammation. The differential diagnosis would include infection, sarcoidosis, foreign body reaction, and certain malignancies such as Hodgkin lymphoma and seminoma. Flow cytometry would not be particularly helpful for the possible malignancies in the differential diagnosis. Tissue for cell blocks may or may not be useful and is not as sensitive as culture for infectious etiologies. Tissue for molecular studies will not likely be helpful. Acquiring tissue for research purpose should be performed after adequate material for diagnosis is acquired.
-
A-9. (e) Adenosquamous carcinoma
The fine-needle aspiration demonstrates two populations of malignant cells in clusters. There are keratinized cells with dense cytoplasm, large nuclei, single cells with pleomorphism, and irregularly dispersed chromatin. In addition, there are clusters of large cells with cytoplasmic mucin, prominent nucleoli, round enlarged nuclei, and occasional cytoplasmic vacuoles. The findings of both features of adenocarcinoma and squamous cell carcinoma support a diagnosis of adenosquamous carcinoma. Glomus cell tumors usually behave in a benign manner and are found in the extremities and skin. Small cell carcinomas are usually less cohesive and composed of smaller cells frequently demonstrating molding.
-
A-10. (e) HHV-8
The FNA specimen demonstrates abundant atypical spindle cells and erythrocytes in a patient with a history of HIV/AIDS. These findings are most suggestive of Kaposi sarcoma. Kaposi sarcoma is related to infection with HHV-8 in patients with HIV/AIDS. HHV-8 immunohistochemical stains would confirm the diagnosis. HTLV-1 is the causative agent of adult T-cell lymphoma/leukemia, HCV is associated with hepatocellular carcinoma, and CMV is not associated with neoplasms but demonstrates characteristic nuclear and cytoplasmic inclusions. Finally, EBV is associated in varying degrees with the three types of Burkitt lymphoma, associated with many B-cell lymphomas in immunosuppressed individuals, extranodal NK/T-cell lymphoma, and two pediatric lymphomas but not Kaposi sarcoma.
-
A-11. (b) Reactive lymphadenopathy
The differential diagnosis for Kaposi sarcoma includes angiosarcoma, melanoma (spindle-cell type), hemangioma, and intranodal myofibroblastoma. All of these possible diagnoses may demonstrate proliferations of spindled cells or vessels that may mimic Kaposi sarcoma. Reactive lymphadenopathy presents with a mixed lymphocytic inflammatory pattern and spindled cell are uncommon.
-
A-12. (a) Viral lymphadenopathy
The image depicts a mixed inflammatory infiltrate including small lymphocytes, centrocytes, and a mixture of other mature lymphoid cells. A large collection of neutrophils or granulomas is lacking. The lack of neutrophils makes a diagnosis of toxoplasmosis or cat scratch disease unlikely. The lack of granulomas makes tuberculosis lymphadenitis unlikely. A diagnosis of Castleman disease on FNA typically cannot be made reliably.
-
A-13. (e) Mixed inflammatory response
The findings of necrosis, granulomas, predominantly plasma cell proliferation, or infiltrating neutrophils would suggest a diagnosis other than viral lymphadenopathy.
-
A-14. (d) Melan-A
The image depicts classic findings of metastatic melanoma including prominent nucleoli, binucleation, enlarged size and nuclear to cytoplasmic ratio, and black pigment. Melanoma will be positive for Melan-A. CD138 highlights plasma cells and LCA are positive in lymphoid cells, CK 7 in certain epithelial cells, and cytokeratin in certain epithelial cells.
-
A-15. (c) Small cell carcinoma
Small cell carcinoma typically presents as small cells, with minimal cytoplasm and occasional to abundant nuclear molding with characteristic chromatin. While melanoma is considered a frequent mimicker of a variety of neoplasms, when melanoma is the primary consideration for a neoplasm, it is important to consider other lesions that may demonstrate similar appearances and remember that the melanin pigment is not always present. The differential diagnosis for melanoma includes multiple myeloma (due to the plasmacytoid nature of some of the cells), Hodgkin lymphoma, and diffuse large B-cell lymphoma among others.
-
A-16. (b) Cryptococcus neoformans
The FNA demonstrates a diffuse infiltrate of round yeast-like forms, which are variable in size with occasional indentations and demonstrate narrow-based budding. There is mild inflammation. These findings, in conjunction with the patient’s immunocompromised status, support a diagnosis of Cryptococcus lymphadenitis. Reactive lymphadenopathy typically does not demonstrate a specific organism, otherwise it would be further classified. Trypanosoma and Leishmania have different morphologies and presentations. Fat emboli may resemble the circular nature of Cryptococcus; however, it is typically seen within vessels and is associated with trauma to the bone marrow.
-
A-17. (d) Acute suppurative lymphadenitis; collect material for microbial cultures.
The inflammatory infiltrate is primarily composed of neutrophils consistent with acute suppurative lymphadenitis. In such cases, it is helpful to collect/submit material for cultures, as this may help identify the etiologic organism. Immunohistochemical stains, flow cytometry, and the cell block would be of minimal value.
-
A-18. (b) HMB45 negative
Myelolipomas are uncommon neoplasms occurring in and around the adrenal gland. They may grow very large and are often incidental findings. In contrast to angiomyolipomas, they are HMB45 negative but do include adipocytes.
-
A-19. (d) EBV stains LMP-1 in Reed-Sternberg cells
Classical Hodgkin lymphoma (CHL) usually demonstrates CD30 and frequently CD15 positivity with CD45 negativity. Sclerosis is common and it typically presents in a bimodal distribution, the first 15–35 years old and the second peak later in life. When EBV in situ staining is performed, it stains LMP-1 in Reed-Sternberg cells, which is a protein involved in antiapoptotic activity.
-
A-20. (d) Prominent nucleoli
CLL/SLL is characterized as a mature B-cell lymphoma/leukemia composed of small cells, clumped mature chromatin, variable plasmacytoid appearance (eccentric nuclei and plasmacytoid rim demonstrates in image), and minimal cytoplasm occasionally demonstrating increased numbers of prolymphocytes and paraimmunoblasts. Prominent nucleoli are not typically seen in the CLL/SLL cells and are usually identified in other lymphoid malignancies, often higher grade or more immature types.
-
A-21. (b) Grading is based on the number of centroblasts
The grading system for follicular lymphoma is based on the number of centroblasts per high-power field: grade I, 0–5 centroblasts per hpf; grade II, 6–15 centroblasts per hpf; and grade III, >15 centroblasts per hpf. Grade 3 is split into 3A and 3B with 3A demonstrating centrocytes while 3B is solid sheets of centroblasts. Cases are usually reported as either low grade (grades 1–2) or high grade (grade 3). It is important to grade follicular lymphomas as cases with higher grades have demonstrated worse clinical outcomes and higher rates of progression to diffuse large cell lymphoma. The Ki-67 proliferation index can be used as supportive evidence of the grade, as it usually correlates with the grade. The t(14;18) translocation involves Bcl2, but not Bcl6. Nuclear irregularities are common and follicular lymphoma is generally the most common small cell lymphoma.
-
A-22. (c) Burkitt lymphoma
The clinical description in combination with the morphology and translocation is most supportive of a Burkitt lymphoma diagnosis. While the other answer choices may demonstrate similar findings, they less frequently present in children, do not demonstrate the translocations, or have different cytologic morphology.
-
A-23. (a) ALK positivity confers a better prognosis.
The findings of the large atypical cells with hallmark and donut-shaped nuclei that are CD30 and ALK positive are suggestive of anaplastic large cell lymphoma (ALCL). ALCLs have better outcomes when ALK positive. They are not associated with EBV and typically do not show prominent red nucleoli with binucleation (like melanoma); the t(2;5) translocation partner genes are ALK and NPM. It typically presents in the first three decades of life.
-
A-24. (b) Mycosis fungoides
The descriptions of a discohesive population of intermediates size cells that are positive for CD2 and CD7 while negative for CD20 suggest a T-cell lymphoproliferative disorder. Combined with the dermatologic presentation, it is most suspicious for mycosis fungoides. Lichen sclerosis, actinic keratosis, folliculitis, and DFSP may demonstrate varying degrees of inflammation, but disseminated proliferation of lymphoid cells is not seen.
-
A-25. (a) CD4+/CD8−/CD34−
Mycosis fungoides is the most likely diagnosis. These typically present with an increased CD4 population. CD8 positivity is rare. CD34 should highlight epithelial and lymphoblast cells, which would be unlikely to be part of this proliferation. Dual-positive or dual-negative CD4/CD8 is uncommon in mycosis fungoides and is more often seen in immature proliferations such as angioimmunoblastic lymphoma.
-
A-26. (e) Bcl-1 is usually positive.
Bcl-1 is the alternate name for cyclin D1 and typically positive in mantle cell lymphoma. Mantle cell lymphomas are positive for the t(11;14) translocation, the blastoid variant is usually cyclin D1 positive, the cells are usually small to medium in size, and cyclin D1 is not specific to mantle cell lymphoma and may also be seen in carcinomas, parathyroid neoplasms, multiple myeloma, and hairy cell leukemia.
-
A-27. (b) Germinal center phenotype has a better prognosis.
The germinal center phenotype (CD10+ or Bcl6+ and MUM1−) has a better prognosis than non-germinal center phenotype (CD10−, Bcl6−, MUM+). CD10 negativity alone is not considered specific for non-germinal center phenotype. If CD10 is negative, then additional stains for Bcl6 and MUM1 should be performed. A newer marker, FOXP1, has been recommended as an addition to the three-stain algorithm for determining germinal center type and has shown improved accuracy.
-
A-28. (d) Cyclin D1
The above cell are suggestive of a diffuse large B-cell lymphoma and would be supported by an appropriate immunophenotype (CD20+, CD19+, CD10+/−, CD5−, increase Ki-67 and surface immunoglobulin positive). In the event of CD5 positivity, the possibility of a blastoid mantle cell lymphoma should be entertained. The most useful stain to investigate this possibility is cyclin D1. In addition, molecular testing for the t(11;14)(CCND1-IGH) rearrangement would be useful. CD20 may be lost in DLBCL treated with rituximab but are usually otherwise positive. CD138 would highlight a plasma cell neoplasm and marginal zone lymphoma. Tdt is a marker of cell immaturity and seen primarily in lymphoblastic neoplasms. Ki-67 proliferation index would not help further differentiate the type of malignancy.
-
A-29. (b) Acid-fast stain
The image demonstrates a proliferation of small lymphocytes concerning for lymphoma. In addition, close examination of the lymphocytes demonstrates rod-shaped negative images. Morphologically and based on the negative staining, these are concerning for mycobacterium and would best be evaluated with an acid-fast stain.
-
A-30. (b) The image depicts a loosely cohesive proliferation of medium-sized cells with a tigroid background. These findings are most consistent with metastatic seminoma.
-
A-31. (e) Metastatic prostate carcinoma
While the tigroid background is typical of seminomas, this is not the only diagnosis that may present with this background. In addition, the cytomorphology may also be present in melanoma, small cell carcinoma, and ALCL. Prostate carcinoma is cohesive and demonstrates glandular morphology.
-
A-32. (a) PLAP
Seminomas typically stain positive with PLAP, c-Kit, and OCT3/4. Melan-A is positive in melanoma, Congo red is used for amyloid, Grocott is a silver stain that highlights fungal walls, and CK 20 stains many carcinomas.
-
A-33. (a) Metastatic renal cell carcinoma
The proliferation demonstrated in the image represents a lymph node involved by metastatic renal cell carcinoma. When dealing with metastatic disease, clinical history and examination are often the most helpful clue. In cases lacking history or where the history is not concordant with the findings in the FNA specimen, immunohistochemical stains of a cell block are often the most useful ancillary tool.
-
A-34. (d) Metastatic melanoma
Metastatic melanoma is frequently discohesive or presents in loose clusters, epithelioid, often binucleated with prominent nuclei, plasmacytoid morphology, and dusty cytoplasm. Melanoma may demonstrate cytoplasmic pigment and intranuclear inclusions. Plasmacytoma or NHL are small- to medium-sized cells and rarely shows large cells with giant nucleoli. Giant cell tumor of bone is a low-grade malignancy and shows cytologically bland cells and very rare causes metastatic disease.
5.4 Answers and Discussion of Text-Based Questions 35–101
-
A-35. (c) Hamazaki-Wesenberg bodies may mimic fungi.
Hamazaki-Wesenberg bodies are highlighted by GMS and acid-fast stains and may be misinterpreted as fungi. Schaumann bodies are more common than asteroid bodies and sarcoidosis typically presents in multiple organ systems with non-necrotizing granulomas. Any granulomatous presentation needs to include investigation of an infectious etiology.
-
A-36. (d) Auramine O may highlight the organism.
Mycobacterium avium often presents with granulomas and may present as negative images of the organisms and they typically stain positive with acid-fast stains. Auramine O highlights mycobacterium and is now the most common infection in patients with AIDS. Acid-fast staining, while it does highlight mycobacterium, may also highlight nocardia, cryptosporidium, and Cyclospora.
-
A-37. (a) It is present in primary cutaneous ALCL.
Typical ALCLs presenting in lymph nodes and other sites frequently demonstrate the t(2;5) translocation. In contrast, cutaneous ALCL does not demonstrate the translocation. The t(2;5) does include the partner genes ALK and PMN is seen in other neoplasms (inflammatory myofibroblastic tumor) and is the most frequent translocation seen in ALCL.
-
A-38. (d) It affects immunocompromised patients.
There are three forms of Burkitt lymphoma, endemic, sporadic, and immunodeficiency associated. The most common translocation is the t(8;14); the cells are usually positive for CD20, CD19, CD10, and BCL-6, while the Ki-67 proliferation index approaches 100 %. It most commonly involves the abdomen, mandible, gonads, kidneys, salivary glands, breasts, and lymph nodes.
-
A-39. (e) Children and adolescents.
In adult men and women, the most likely source of a malignant effusion is an occult primary neoplasm such as lung, breast, or colorectal carcinoma.
-
A-40. (e) Heterogeneity of the lymphoid population.
The differentiation between lymphoid hyperplasia and lymphoma can be difficult. All of the features may help suggest a lymphoid population is benign. Several lymphoid malignancies consistently demonstrate heterogeneity, which makes classification difficult and includes: follicular lymphoma, MALT lymphoma, T-cell-rich large B-cell lymphoma, and Hodgkin lymphoma.
-
A-41. (e) All of the above
Each diagnosis listed demonstrates features similar to reactive lymphoid hyperplasia and cannot be reliably classified.
-
A-42. (b) CD20
Many patients are treated with Rituxan (rituximab) chemotherapy for CD20+ lymphoma. This chemotherapy targets CD20-positive B cells and the CD20 receptor. As a result, residual and recurrent B-cell lymphomas, status post therapy often lack this marker. The other markers may be modified after chemotherapy; however, this is not seen as frequently as the loss of CD20.
-
A-43. (a) Reactive lymphoid hyperplasia.
Patients with AIDS are prone to many opportunistic infections including tuberculosis and Cryptococcus neoformans. In addition, these patients may develop Kaposi sarcoma or non-Hodgkin lymphoma. However, the most frequent cause of lymphadenopathy in AIDS patients is reactive lymphoid hyperplasia.
-
A-44. (a) Lepra bacilli
The described foamy cells are the classic Virchow cells with vacuoles containing multiple bacilli. Cat scratch disease, actinomyces, and suppurative lymphadenitis contain primarily neutrophils. Tuberculosis contains acid-fast bacilli and histiocytes, but not with the Virchow cell morphology.
-
A-45. (e) Molecular testing
All of the other techniques may demonstrate the organism (Bartonella henselae); however, they are unreliable. Molecular techniques, serologic testing, or immunofluorescence are more reliable alternatives to confirming the suspicion of cat scratch disease.
-
A-46. (d ) Watch and wait
The findings and clinical history are typical of Kikuchi lymphadenitis. It is characterized by extensive karyorrhexis, histiocytes with sharply angulated nuclei, and plasmacytoid monocytes. Clinical intervention including antibiotics is unnecessary in these cases as the lymphadenopathy is self-limited and will resolve without intervention.
-
A-47. (b) 17p deletion
The 17p deletion in CLL/SLL is associated with a more aggressive course. An 11q deletion is also aggressive, not 11p. The 13q14 deletion phenotype has a better prognosis. The 17q addition is not a common known mutation. Trisomy 12 has an intermediate phenotype.
-
A-48. (b) Leishmaniasis
The description of the histiocytic intracytoplasmic amastigotes is consistent with leishmanial infection. The rod-shaped structure is the kinetoplast. Visceral leishmaniasis is caused by Leishmania donovani and is endemic to parts of Africa and South America. The amastigotes may be found within histiocytes or outside upon rupture of the cells.
-
A-49. (d) Rosai-Dorfman disease
Rosai-Dorfman disease, also known as sinus histiocytosis with massive lymphadenopathy, most frequently occurs in children and adolescents. Clinically it frequently presents with symptoms similar to lymphoma and leukemia including fevers, night sweats, malaise, and joint pain. Cytologically, the characteristic finding in addition to abundant lymphocytes is lymphocytes transgressing through histiocytes (emperipolesis). The histiocytes are S100 and CD68 positive. The alternate answer choices do not typically demonstrate emperipolesis.
-
A-50. (c) Nodular lymphocyte-predominant Hodgkin lymphoma usually presents in patients between 30 and 50 years of age and classically demonstrates CD20-, EMA-, and CD45-positive L&H (popcorn) cells, which are CD30 negative and often CD15 negative.
Compared to Reed-Sternberg cells in classical forms of Hodgkin lymphoma, L&H cells usually have a single irregular or multinucleated nucleolus with extreme irregularities, hence the popcorn cell description. The other choices are subcategories of classical-type Hodgkin lymphoma, which usually demonstrate CD30 and CD15 positivity and are characterized by the Reed-Sternberg cell.
-
A-51. (e) Mixed cellularity is the most common subtype of Hodgkin lymphoma in the developing world. In the developed world, nodular-sclerosing variant is the most common subtype. Overall, the classical subtypes comprise 95 % of cases worldwide.
-
A-52. (a) The t(14;18) translocation is classically found in follicular cell lymphoma and characteristically positive for B-cell markers and follicular center markers Bcl-6 and Bcl-2. The t(14;18) translocation represents a Bcl-2 gene rearrangement. Translocation t(11;14) is typically found in mantle cell lymphoma, t(8;22) Ewing sarcoma, t(2;5) anaplastic large cell lymphoma, and t(x;18) in synovial sarcoma.
-
A-53. (a) Unlike the other small cell lymphomas (follicular lymphoma, CLL/SLL) mantle cell typically lacks transformed lymphocytes. Hodgkin lymphoma and anaplastic large cell lymphomas typically are not considered small cell lymphomas.
-
A-54. (a) A. t(14;18)(q32;q31)
The cytologic and immunohistochemical findings suggest follicular lymphoma. The translocation partners for follicular lymphoma are both found on the long arms of chromosomes 14 and 18. This translocation results in rearrangement of the Bcl-2 gene. The t(11;14) is found in mantle cell lymphoma and t(8;18) in Burkitt lymphoma.
-
A-55. (c) MALT lymphomas are associated with several chronic autoimmune conditions including Sjögren disease, H. pylori chronic gastritis, and Hashimoto thyroiditis. The most frequent site is the gastric mucosa. MALT lymphomas frequently demonstrate the t(11;18) translocation.
-
A-56. (b) The endemic form of Burkitt lymphoma is most likely to demonstrate EBV positivity. The endemic form is found in patients from Africa and less frequently in the Middle East and Asia. The endemic form is rare in the United States. Burkitt lymphoma commonly presents in young children, frequently in the mandible or abdomen.
-
A-57. (e) 95 %
The cytomorphologic and immunohistochemical findings suggest a Burkitt lymphoma, immunodeficiency-related type. Burkitt lymphoma is known to demonstrate a very high proliferation index approaching 100 %, as such a value greater than 70 % is expected.
-
A-58. (b) Anaplastic large cell lymphoma frequently demonstrates a t (2;5)(p23;q35) translocation. The translocation results in expression of the ALK protein from the fusion of the ALK gene with the nucleophosmin gene. ALCL is among the more common T-cell lymphomas. ALCL usually demonstrates positivity for T-cell markers: however, occasionally they are negative for T-cell markers and are given the null designation. In the classic form, the neoplastic cells are large with extensive pleomorphism. Many cells may demonstrate a horseshoe-shaped nucleus, known as a “horseshoe” cell. The tumor cells are positive for CD30. Usually tingible body macrophages are absent and lymphoglandular bodies are rare.
-
A-59. (a) Precursor T-cell lymphoblastic lymphoma is a common lymphoma of childhood. Clinically, it most frequently presents as an anterior compartment mediastinal mass. Due to its location, the mass may place pressure on adjacent structures and induce symptoms that mimic other diagnoses including acute bronchitis and superior vena cava thrombosis. Smears are usually hypercellular and composed of large lymphoblasts with inconspicuous nucleoli, fine chromatin, and increased nuclear to cytoplasmic ratios. The cell may demonstrate molding. Immunophenotypically, the lymphoblasts are characteristically TdT positive. The distinction from thymoma is made by cytomorphology and clinical history, as both neoplasms demonstrate immature immunophenotypes.
-
A-60. (d) EBV.
A large percentage of PTLDs are associated with concomitant EBV infection. It is thought that Epstein-Barr virus induces the monoclonal or polyclonal proliferations. Human papilloma virus (HPV) is associated with squamous cell carcinomas. Human T-cell lymphoma virus 1 (HTLV-1) is associated with Kaposi sarcoma. Human immunodeficiency virus (HIV) has not been directly implicated in the development of a neoplasm.
-
A-61. (e) Positive EBV immunohistochemical stains in a majority of cells.
Recurrent lymphomas may take many forms and have a variety of characteristics. It is often useful to compare to the previous material or report to confirm morphological and immunohistochemical similarities. Findings such as large atypical cells, high mitotic rate, and lymphoglandular bodies do not specifically help distinguish between PTLD and recurrent lymphoma. A small number of EBV positive cells are not a reliable indicator of PTLD as this may be seen in a variety of settings. True EBV-related PTLD demonstrates EBV positivity in the majority of cells.
-
A-62. (a) Nasopharyngeal carcinoma and seminoma are two neoplasms that may mimic diffuse large B-cell lymphoma. Other neoplasms may mimic DLBCL, including melanoma, epithelioid carcinoma, and poorly differentiated carcinomas. Nasopharyngeal carcinoma occurring in a lymph node will frequently demonstrate lymphoglandular bodies. Lymphoglandular bodies are fragments of lymphocytes and are accepted as markers of lymphoid tissue and may be seen in the background in tumors involving lymph nodes or intermixed in malignant lymphoid populations.
-
A-63. (c) Anaplastic large cell lymphoma (ALCL) may be confused with carcinoma for several reasons. These neoplasms usually have a paucity of lymphoglandular bodies, are cohesive or frequently clustered, demonstrate EMA positivity (which is generally a marker of epithelial derivation), are pleomorphic, small lymphocytes, and may be rare and often ALCL contains spindled cells.
-
A-64. (c) Histiocytic sarcoma, formerly known as true histiocytic lymphoma, may be nodal or extranodal and is characterized by CD68 and CD163 positivity with CD1a, CD30, and keratin negativity. They are composed of sheets of large cells with abundant eosinophilic cytoplasm. Langerhans cell histiocytosis and Langerhans cell sarcoma demonstrate S100 and CD1a positivity. Interdigitating dendritic cell sarcoma shows S100 positivity and follicular dendritic cell sarcoma is positive for CD23, CD21, and CD35.
-
A-65. (b) Dermatopathic lymphadenopathy is a frequent mimic of Langerhans cell histiocytosis. Both may demonstrate CD1a grooved Langerhans cells. Dermatopathic lymphadenopathy is seen as a result of a recent dermatologic infection or reaction and results from Langerhans cell from the skin migrating to lymph nodes and includes surrounding pigment laden macrophages. Langerhans cell histiocytosis usually also has a population of eosinophils. On surgical excision, Langerhans cells in LCH are usually in the interfollicular zones, while in dermatopathic lymphadenopathy, they are usually located in the sinuses and peripheral node.
-
A-66. (c) The description is of a small cell carcinoma. Small cell carcinomas may demonstrate some similarities in their cell size to a lymphocytic proliferation. The characteristic features of nuclear molding and salt and pepper chromatin are seen in small cell carcinoma. In addition to being positive for neuroendocrine markers including CD56, chromogranin, and synaptophysin, it is also positive for cytokeratins. CD3 and CD20 are positive in lymphoid proliferations. Melanin is positive in melanoma and Oct4 is seen in germ cell tumors.
-
A-67. (b) BRAF testing in metastatic melanoma/stage IV melanoma is important to help aid in therapy. Currently, signal transduction therapeutics (vemurafenib) is available for patients with the BRAF V600E mutation. These have been shown to help prolong survival in patients with metastatic disease. KRAS may be mutated in melanoma but is rare and not currently an approved therapeutic target. The BRD4-NUT and BRD3-NUT translocations are seen in NUT midline carcinoma. The t(2;5) translocation is important in identifying anaplastic large cell lymphoma; however, the immunohistochemical studies in this case support a diagnosis of melanoma. The t(14;18) translocation is seen in follicular lymphoma.
-
A-68. (d) Performing multiple passes with the needle helps improve sampling by evaluating multiple areas of the lymph node and acquiring more material. Applying anesthetic creams may help decrease the pain associated with the technique for the patient, but will not directly improve adequacy. Lymph nodes should be stabilized while performing the aspiration; otherwise, they may move and inhibit proper sampling. Large gauge needles provide more tissue but are more painful for the patient and result in more bleeding. Gauges are counterintuitive in that the higher the number, the smaller the needle.
-
A-69. (a) The Monospot test is an agglutination test developed in 1968, using the principle that horse erythrocytes are more likely to react than sheep erythrocytes to the presence of heterophile antibodies produced in response to infection by Epstein-Barr virus. Clinical history is not highly specific for infectious mononucleosis; currently there is neither urine test for EBV antibodies nor a breath test. Molecular testing could be performed for the presence of EBV, but this does not determine whether an immune response has occurred, leading to the infectious mononucleosis manifestations.
-
A-70. (c) Tall columnar cells
Colorectal adenocarcinoma commonly includes tall columnar cells often with mucin production and gland formation. Signet ring cells are characteristic of gastric adenocarcinoma. Intranuclear pseudoinclusions are frequently seen in papillary thyroid carcinoma. Brown pigment may be either hemosiderin or melanin in metastatic melanoma. Nuclear molding is seen in small cell carcinoma and herpes simplex infections.
-
A-71. (c) 10,000 events.
The generally accepted minimum number of events to be confident in flow cytometric results is 10,000. This number is based on statistical calculations and the clinical implications of diagnoses requiring a low enough coefficient of variation for a subpopulation of cells comprising 5 % of the sample.
-
A-72. (c) CLL/SLL is a lymphoid proliferation of small mature B-lineage lymphocytes with mature clumped chromatin. The architectural findings in CLL/SLL are not necessary diagnostic and usually the most useful additional information is the immunophenotype of the proliferation (CD5 and CD23+ B cells). Progressively transformed germinal centers, Castleman disease, nodular lymphocyte-predominant Hodgkin lymphoma, and vascular transformation of the lymph node sinuses, either all rely on or are substantially supported by architectural findings.
-
A-73. (a) Melanoma
Sarcoidosis demonstrates granulomas usually composed of epithelioid histiocytes and variable nonspecific findings such as asteroid bodies (starlike eosinophilic shapes in histiocytes). Sarcoid is commonly a diagnosis of exclusion; once other etiologies with similar morphologic findings are excluded. Entities demonstrating similar granulomatous reactions includes: infections, foreign body reactions, dendritic lymphocytic aggregates, and spindle-cell neoplasms. All of these may have a proliferation of histiocytes. Melanoma typically does not demonstrate a granulomatous reaction unless presenting in the setting of another concurrent process. Immunohistochemical stains for Melan-A and HMB45 would help confirm the diagnosis of melanoma if there is a concern.
-
A-74. (d) Extensive neutrophilic infiltrate
Kikuchi lymphadenitis is a reactive process that typically demonstrates necrotic debris, small phagocytic histiocytes, tingible body macrophages, and minimal to no neutrophilic inflammation. A reactive lymph node with a neutrophilic infiltrate would not only make the diagnosis of Kikuchi lymphadenitis unlikely but would raise suspicion for alternate diagnoses including cat scratch disease, Francisella, Yersinia, and Chlamydia.
-
A-75. (a) Mantle cell lymphoma
Infectious mononucleosis can mimic many neoplasms. It is caused by EBV and seen frequently in adolescents. Lymph nodes may be tender and splenomegaly is a frequent finding. Aspirates usually demonstrate a mix of small lymphocytes, plasmacytoid lymphocytes, centroblasts, and immunoblasts. In addition, there is an increase in large cells, which may mimic large cell lymphoma, Hodgkin lymphoma, or immunoblastic lymphoma. The mixed inflammation is similar to reactive lymphoid hyperplasia. The proliferations can be differentiated from infectious mononucleosis by the polyclonality of IM.
-
A-76. (b) Morphology of malignant cells
Anaplastic large cell lymphoma (ALCL) and classical Hodgkin lymphoma may have very similar appearances. ALCL usually has a higher number of malignant cells compared to an alternate composition in classical Hodgkin lymphoma. EMA is typically negative in classical HL (positive in NLPHL) and positive in ALCL. Molecular studies may demonstrate t(2;5) seen in ALCL and not HL. Finally, ALK immunohistochemical stains are positive in most ALCLs and negative in HL.
-
A-77. (c) Mantle cell
When comparing the aggressiveness of small lymphomas, Mantle cell lymphoma is considered the most aggressive. In comparison, small lymphocytic, follicular, marginal zone/MALT, and lymphoplasmacytic are considered indolent. Of these lymphomas, marginal zone/MALT lymphoma is the only one considered regularly curable, while follicular lymphomas are rarely cured.
-
A-78. (a) t(8;14)
The c-Myc immunohistochemical stain is positive in Burkitt lymphoma, which has an associated t(8;14) translocation and has presentation both clinically and morphologically similar to the described patient. A subset of Burkitt lymphomas demonstrate the t(2:8) or t(8;22) translocations, but they occur much less frequently than the t(8;14) translocation. Rarely, diffuse large B-cell lymphomas may be positive for c-Myc. However, they typically demonstrate Bcl-2 gene rearrangement or abnormalities in 3q27. Translocation t(2;5) is typically seen in anaplastic large cell lymphoma and t(9;22) translocation is seen in chronic myelogenous leukemia and acute lymphoblastic leukemia.
-
A-79. (c) 8
C-Myc was first discovered in Burkitt lymphoma and is located on chromosome 8 and acts as a transcription factor involved in gene regulation. The c-Myc translocation occurs from band 8q24 to the IG heaving chain 14q32. Occasionally it occurs at the 22q11 lambda or 2p12 kappa light chain loci. C-Myc has also been identified in diffuse large B-cell lymphoma and multiple myeloma.
-
A-80. (a) Multiple myeloma
The c-Myc rearrangement may be seen in a variety of lymphoid neoplasms including Burkitt lymphoma, multiple myeloma, and diffuse large B-cell lymphoma. In Burkitt lymphoma, the c-Myc positivity is a common finding, while it is uncommon in diffuse large B-cell lymphoma and multiple myeloma.
-
A-81. (e) EBV
The differential diagnosis of a fine-needle aspiration with findings including neutrophilic infiltrate consistent with a suppurative lymphadenitis includes: Chlamydia trachomatis, Yersinia enterocolitica, Francisella tularensis, Bartonella henselae, and pyogenic cocci. Clinical history and cultures are frequently necessary to confirm a diagnosis or further classify the etiology of suppurative lymphadenitis. Bartonella frequently demonstrates palisading histiocytes and stellate abscesses, which may help lend weight to cat scratch diagnosis. Epstein-Barr-related lymphadenitis may present as infectious mononucleosis or in relation to a neoplastic process. These typically lack a prominent neutrophilic component.
-
A-82. (c) Comprise the majority of lymphoblastic lymphomas
T-cell lymphoblastic lymphoma most frequently occurs in children. B-cell lymphoblastic lymphomas are also frequent in children, however, more common than T-cell lymphoblastic lymphomas, in adults. The leukocyte count is typically elevated. The neoplastic process frequently presents in the mediastinum and may be included in the differential diagnosis with thymomas. They usually grow rapidly and comprise the majority of lymphoblastic lymphomas.
-
A-83. (a) Follicular lymphoma
The cytologic features of a small lymphocytic proliferation with irregular cleaved lymphocytes and few tingible body macrophages suggests a small lymphocyte lymphoma and provides nonspecific findings in favor of follicular lymphoma. The immunophenotype is characteristic of follicular lymphoma and confirmed by the t(14;18) translocation. CLL/SLL is typically positive for CD5 and CD23, mantle cell is CD5 positive and has the t(11;14) translocation, and marginal zone lymphoma is usually negative for CD5, CD23, Bcl-6, and CD10 and does not demonstrate (14;18). Finally, diffuse large B cell may demonstrate CD10 and Bcl-6 positivity and also may have the t(14;18) translocation, but morphologically is comprised of larger cells with a higher proliferation index.
-
A-84. (a) Desmin, myogenin, CD138, and SMA
The history of a thigh mass, coupled with the description of large eosinophilic cytoplasm and eccentric nuclei suggests rhabdoid morphology, likely rhabdomyosarcoma. Confirming a diagnosis of rhabdomyosarcoma is best done with positivity for desmin and myogenin. CD138 should be negative and rule out a plasma cell neoplasm and smooth muscle actin would be positive in a leiomyosarcoma. HMB45 and Melan-A would confirm a melanoma, cytokeratins are positive in epithelial neoplasms; CD99 can be seen in a variety of more immature and spindled neoplasms; vimentin highlights mesenchymal elements, but is not specific; PLAP is useful to confirm yolk sac tumors; CA-125 is positive in ovarian neoplasms; and WT-1 will highlight mesothelial cells and mullerian tumors in general.
-
A-85. (c) del 13q14.3
CLL/SLL may demonstrate several abnormalities molecular abnormalities. The most common abnormality is the deletion of 13q14.3 (approximately 50 % of cases), while approximately 20 % of cases demonstrate trisomy 12. Additional less frequent cytogenetic abnormalities are deletions of 11q22-23, 17p13, and 6q21.
-
A-86. (e) Pulmonary adenocarcinoma
The FNA description highlights the cell size (large) and shape (cleaved and non-cleaved) and cytoplasmic characteristics (vacuoles) with a lymphoid appearance. These findings suggest a lymphoid malignancy, but additional neoplasms may demonstrate similar morphology. Metastatic melanoma is frequently discohesive or presents in loose clusters, epithelioid, often binucleated with prominent nuclei and may demonstrate cytoplasmic black pigment. Small cell carcinoma is characterized by smaller cells that are often discohesive and have a lymphoid appearance but usually demonstrate molding. Testicular and mediastinal seminomas frequently metastasize to lymph nodes and typically have macronucleoli and abundant cytoplasm occurring in a tigroid background. The most likely process given the findings is diffuse large B-cell lymphoma. Pulmonary adenocarcinoma presents as medium to large cells clustered in three-dimensional sheets with prominent nucleoli and occasional cytoplasmic vacuoles.
-
A-87. (c) Cytoplasmic kappa restriction, normal lambda
Clonal proliferation of plasma cells is seen in mature neoplasms. Over the course of their maturity, plasma cells transition form surface to cytoplasmic expression of immunoglobulins. Normal plasma cell population will present with a kappa to lambda ratio of 2–4 kappa to 1 lambda. In malignant plasma cell proliferations, there is usually a predominance of either kappa or lambda and it is found cytoplasmically. This is important as a clonal plasma cell population may not be identified immunophenotypically if cell lysis procedures that can characterize cytoplasmic expression are not performed.
-
A-88. (b) CD138-positive cells
CD138-positive cells are primarily plasma cells. Plasma cells are more fragile than most other cell types. Due to their fragility, plasma cells may be hard to characterize in general, and when a sample is not rapidly processed, the cells will most likely degrade to a degree that prevents accurate evaluation.
-
A-89. (a) Start triple therapy
Triple therapy consists of a regimen of amoxicillin, clarithromycin, and omeprazole to eradicate Helicobacter pylori and/or Helmenii from the stomach. Both organisms are associated with gastric MALT lymphomas and have led to a complete response. If this therapy fails, the next step would include gastric resection. It would be inappropriate to watch and wait, perform the urease breath test, or perform an endoscopic mucosal resection.
-
A-90. (b) B. CD20+, CD79+, CD38+
Splenic marginal zone lymphoma has a typically nonspecific immunophenotype. In contrast, hairy cell leukemia is positive for CD103 and CD25, while negative for CD23. Plasma cell neoplasms are typically CD20− but CD79+ and CD138+ and have typical plasmacytoid morphology. CLL/SLL is positive for CD5 and CD23, while mantle cell lymphoma is positive for CD5, but negative for CD23 and CD10.
-
A-91. (a) CD103+, CD25+, CD23−
Hairy cell leukemia is positive for CD103 and CD23, while negative for CD23. Splenic marginal zone lymphoma has a typically nonspecific immunophenotype. Plasma cell neoplasms are typically CD20−, but CD79+ and CD138+ and have typical plasmacytoid morphology. CLL/SLL is positive for CD5 and CD23, while mantle cell lymphoma is positive for CD5, but negative for CD23 and CD10.
-
A-92. (b) Hodgkin lymphoma
Based on various studies there is a range of sensitivities and specificities for FNA of lymph nodes depending on the underlying character of a lesion. In general, the lowest sensitivities are seen in Hodgkin lymphoma, likely due to the mixed inflammatory infiltrate and frequently the paucity of malignant cells in addition to difficulties with flow cytometric analysis for characterizing Hodgkin lymphoma. The low ends of sensitivity ranges are higher for non-Hodgkin lymphoma and metastatic disease.
-
A-93. (a) Burkitt lymphoma
Endemic and sporadic Burkitt lymphoma typically present in younger patients. Immunodeficiency-associated Burkitt lymphoma may be more frequent in young adults depending on the HIV/AIDS demographics of a population. CLL/SLL, DLBCL, follicular lymphoma, and ALCL are more common in adults.
-
A-94. (a) Metastatic melanoma
Warthin-Finkeldey cells are described as grape bunch-like clusters of cells with minimal cytoplasm of variable size. These cells are classically associated with vaccination for measles. In addition, they have been demonstrated in systemic lupus erythematosus, Kimura disease, and Hodgkin lymphoma. They have not classically been associated with metastatic melanoma.
-
A-95. (e) Hodgkin lymphoma
Sinus histiocytosis on FNA or touch imprint is characterized by increased benign histiocytes in loose clusters or individually. They usually contain foamy cytoplasm. The intermixed cells are composed of mixed maturity lymphocytes and plasma cells. Of the listed diseases, Hodgkin lymphoma is classically not associated with sinus histiocytosis. All of the other entities may demonstrate increased sinus histiocytes.
-
A-96. (b) Denatured DNA and immunoglobulin
Systemic lupus erythematosus (SLE) lymphadenopathy on FNA typically demonstrate a mixed pattern with small lymphocytes, plasma cells, tingible body macrophages, and transformed cells. There may be background karyorrhexis. A characteristic feature of SLE material is lupus erythematosus (LE) cells. These are brightly eosinophilic cells with a hyalinized appearance hematoxylin bodies. The hematoxylin bodies contain denatured DNA and immunoglobulin.
-
A-97. (b) Flame cells
The description of plasma cell leukemia and cells with strong metachromatic staining in the peripheral cytoplasm is characteristic of flame cells. These cells have been associated with IgA secretion. Dutcher bodies are intranuclear and contain immunoglobulin, while Russell bodies are intracytoplasmic and also contain immunoglobulin. Lymphoglandular bodies are fragments of lymphocytes cytoplasm. Finally, Mott cells are plasma cell with abundant Russell bodies formed from immunoglobulin that cannot be eliminated.
-
A-98. (c) It has the same immunophenotype as in adults.
Pediatric nodal marginal zone lymphoma typically has the same immunophenotype as adult nodal marginal zone lymphomas, which is typically nonspecific and may mimic other neoplasms. They have an excellent prognosis, commonly present in the head and neck lymph nodes, predominantly in males (20:1), and may be difficult to distinguish from reactive conditions. In addition, they may require IGH clonal rearrangement studies.
-
A-99. (b) t(2;17)(p23;q23)
In contrast to anaplastic large cell lymphoma, which most frequently demonstrates the t (2:5) translocation, ALK-positive LBCL most commonly demonstrates the t(2;17) translocation. This is responsible for clathrin-ALK fusion protein. The cryptic insertion of 3′ ALK into 4q22–24 has been rarely reported. The t(5:17) translocation is not a common translocation and the t(9;22) translocation is seen in chronic myelogenous leukemia.
-
A-100. (a) DLBCL
Among adults, DLBCL is the most common B-cell lymphoma. The second most common is follicular lymphoma, followed by CLL/SLL, MALT lymphoma, and mantle cell lymphoma.
-
A-101. (a) Peripheral T-cell lymphoma NOS
The most common mature T-cell lymphoma subtype is peripheral T-cell lymphoma NOS followed by angioimmunoblastic lymphoma. Extranodal NK/T-cell lymphoma makes up about 10 % of case followed by much less frequent anaplastic large cell lymphoma, ALK+, and hepatosplenic T-cell lymphoma.
Reading List
Caraway NP, Katz RL. Chapter 31. Lymph nodes. In: Koss LG, Melamed MR, editors. Koss’ diagnostic cytology and its histopathologic bases. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2006. p. 1186–228.
DeMay RM. Chapter 13. Lymph nodes. In: DeMay RM, editor. The art & science of cytopathology. 2nd ed. Chicago: ASCP Press; 2012. p. 966–1031.
Khalbuss WE, Monaco SE, and Pantanowitz L. Chapter 13. Lymph nodes. In: The ASCP quick compendium of cytopathology. IL, USA: ASCP Press; 2013. p 259–91.
Monaco SE, Pantanowitz L, Khalbuss WE. Cytopathology of nonneoplastic and infectious lymphadenopathy. In: Cualing HD, Bhargava P, Sandin RL, editors. Nonneoplastic hematopathology and infections. NJ, USA: Wiley- Blackwell; 2012. p 481.
Pambuccian SE, Bardales RH. Lymph node cytopathology. New York: Springer; 2011.
Wakely PE, Cibas ES. Chapter 11. Lymph nodes. In: Cibas ES, Ducatman BS, editors. Cytology diagnostic principles & clinical correlates. 3rd ed. Philadelphia: Saunders Elsevier; 2009. p. 319–57.
Young NA, Al-Saleem T. Chapter 24. Lymph nodes: cytomorphology & flow cytometry. In: Bibbo M, Wilbur DC, editors. Comprehensive cytopathology. 3rd ed. Philadelphia: Saunders Elsevier; 2008. p. 671–711.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Smith, M.A., Khalbuss, W.E. (2015). Lymph Node Cytopathology. In: Khalbuss, W., Li, Q. (eds) Diagnostic Cytopathology Board Review and Self-Assessment. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-1477-7_5
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1477-7_5
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-1476-0
Online ISBN: 978-1-4939-1477-7
eBook Packages: MedicineMedicine (R0)