Abstract
This chapter is focused on the discussion and review of cytomorphological features of benign and malignant lesions in thyroid FNA. Thyroid FNA is commonly utilized in the follow-up of thyroid nodules. Thyroid FNA is very useful to distinguish between patients with malignant, or possibly malignant, thyroid nodules requiring surgical treatment and those with benign nodules that can be followed up clinically or treated medically. Other indications are evaluation of diffuse goiter, follow-up of individuals exposed to irradiation of the head and neck, and therapeutic drainage of cystic lesions.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Papillary Thyroid Carcinoma
- Thyroid Nodule
- Papillary Carcinoma
- Medullary Thyroid Carcinoma
- Follicular Cell
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
4.1 Image-Based Questions 1–44

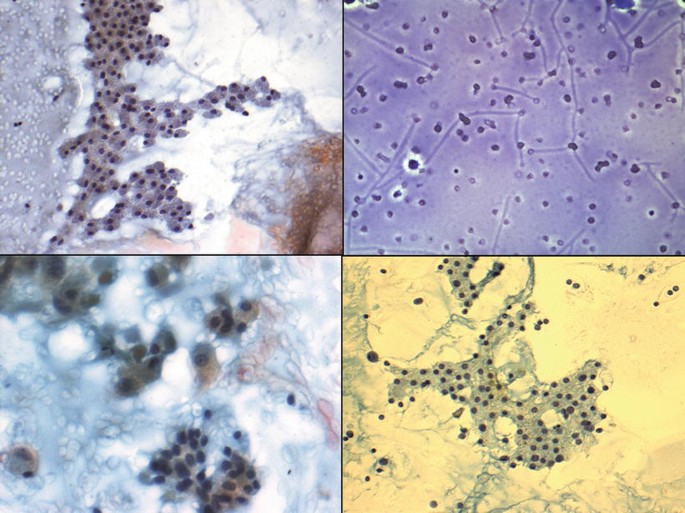
Fig. 4.1
-
Q-1. This aspirate is from a 49-year-old woman who complains of neck fullness. She has noticed gradual painless enlargement of her thyroid gland for more than 1 year. Laboratory studies of thyroid function shows normal free T4 and TSH levels. Ultrasound examination shows a multiple thyroid nodules with a prominent nodule measuring 4.0 cm and showing complexity of architecture. US-guided FNA of the nodule is performed. Which of the following is the most likely diagnosis?
-
(a)
Benign, colloid nodule
-
(b)
Follicular neoplasm
-
(c)
Benign, lymphocytic (Hashimoto) thyroiditis
-
(d)
Unsatisfactory specimen
-
(e)
Malignant, medullary carcinoma with amyloid

Fig. 4.2
-
(a)
-
Q-2. This aspirate is from a 56-year-old woman who complains of neck fullness. Physical examination shows multiple painless thyroid nodules. Laboratory studies of thyroid function show normal free T4 and TSH levels. Ultrasound examination shows a large prominent nodule measuring 3.5 cm. US-guided FNA of the thyroid nodule is done. Which of the following is the most likely diagnosis?
-
(a)
Benign, colloid nodule
-
(b)
Benign; adenomatous goiter
-
(c)
Nondiagnostic, cyst fluid only
-
(d)
Lymphocytic thyroiditis
-
(e)
Negative for malignancy

Fig. 4.3
-
(a)
-
Q-3. This aspirate is from a 35-year-old man who complains of lateral neck nodule. Physical examination shows a painless lateral right neck nodule, but not moving with swallowing. Laboratory studies of thyroid function shows normal free T4 and TSH levels. Ultrasound examination shows a cystic lesion measuring 2.8 cm. US-guided FNA is performed. Which of the following is the most likely diagnosis?
-
(a)
Benign, colloid nodule
-
(b)
Branchial cleft cyst
-
(c)
Benign, thyroid colloid cyst
-
(d)
Benign, lymphocytic thyroiditis
-
(e)
Nondiagnostic, unsatisfactory specimen

Fig. 4.4
-
(a)
-
Q-4. This aspirate is from a 37-year-old woman who presents with difficulty swallowing and a feeling of fullness in her neck for the past 2 weeks. She is recovering from a mild upper respiratory tract infection 1 month ago. Palpation of her diffusely enlarged thyroid elicits pain. Laboratory studies show an increased serum free T4 level and a decreased TSH level. US-guided FNA is performed. Which of the following is the most likely diagnosis?
-
(a)
Medullary carcinoma
-
(b)
Benign, subacute granulomatous (de Quervain) thyroiditis
-
(c)
Benign, multinodular goiter
-
(d)
Benign, Hashimoto thyroiditis
-
(e)
Benign, toxic thyrotoxicosis (Grave’s disease)

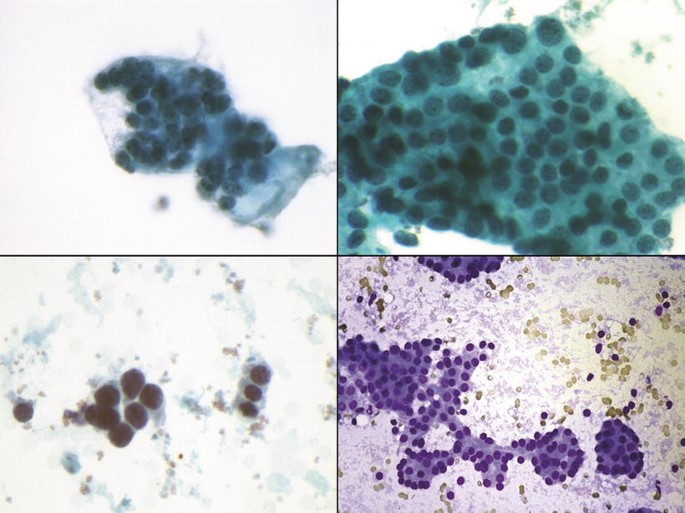
Fig. 4.5
-
(a)
-
Q-5. This aspirate is from a 61-year-old woman who has experienced a feeling of fullness in her neck for the past year. She complains of loss of energy, easy fatigue, and difficulty concentrating at work. On physical examination, the thyroid gland is diffusely large with a feeling of one thyroid nodule. The gland is not tender on palpation. She has dry, coarse skin and alopecia. US-guided FNA of the thyroid nodule is performed. Which of the following is the most likely the diagnosis?
-
(a)
Hurthle cell neoplasm
-
(b)
Subacute granulomatous (de Quervain) thyroiditis
-
(c)
Benign, acute thyroiditis
-
(d)
Atypical (FLUS/AUS), radiation atypia
-
(e)
Benign, chronic lymphocytic (Hashimoto) thyroiditis

Fig. 4.6
-
(a)
-
Q-6. This aspirate is from a 76-year-old woman who complains of neck fullness. Physical examination shows diffusely enlarged thyroid gland with a thyroid nodule. Laboratory studies of thyroid function show normal free T4 with low TSH levels. Ultrasound examination shows a large prominent nodule measuring 3.0 cm. US-guided FNA of the thyroid nodule is performed. Which of the following is the most likely diagnosis?
-
(a)
Benign colloid nodule
-
(b)
Benign, multinodular goiter
-
(c)
Benign, Hurthle cell metaplasia in background of lymphocytic thyroiditis
-
(d)
Hurthle cell neoplasm
-
(e)
Malignant, papillary thyroid carcinoma

Fig. 4.7
-
(a)
-
Q-7. This aspirate is from a 22-year-old woman who has experienced increasing fatigue and weight loss in spite of increasing her appetite over the past 4 months. She complains of increasing anxiety and nervousness with no apparent changes in her job or lifestyle. She now has diarrhea. Physical examination shows a diffusely enlarged thyroid gland with vague nodularity. The clinician decides to do US-guided FNA of the thyroid gland to confirm the benign diagnosis. Later, a radionuclide scan of the thyroid shows a diffuse increase in radioactive iodine uptake. Which of the following is the most likely diagnosis?
-
(a)
Irradiation effect
-
(b)
Toxic diffuse hyperplasia (Graves’ disease)
-
(c)
Colloid nodule
-
(d)
Multinodular goiter
-
(e)
Papillary carcinoma

Fig. 4.8
-
(a)
-
Q-8. This aspirate is from an 80-year-old man who has history of tongue squamous cell carcinoma. The patient has past history of receiving radiotherapy for his neck lymph nodes. Now he comes with sense of neck fullness. Physical examination shows diffusely enlarged thyroid gland with thyroid nodule. Ultrasound examination shows a prominent thyroid nodule measuring 2.5 cm. US-guided FNA of the thyroid nodule is performed to exclude the presence of malignancy. Which of the following is the most likely diagnosis?
-
(a)
Metastatic renal cell carcinoma
-
(b)
Metastatic squamous cell carcinoma
-
(c)
Benign, radiation changes
-
(d)
Hurthle cell neoplasm.
-
(e)
Malignant, papillary carcinoma
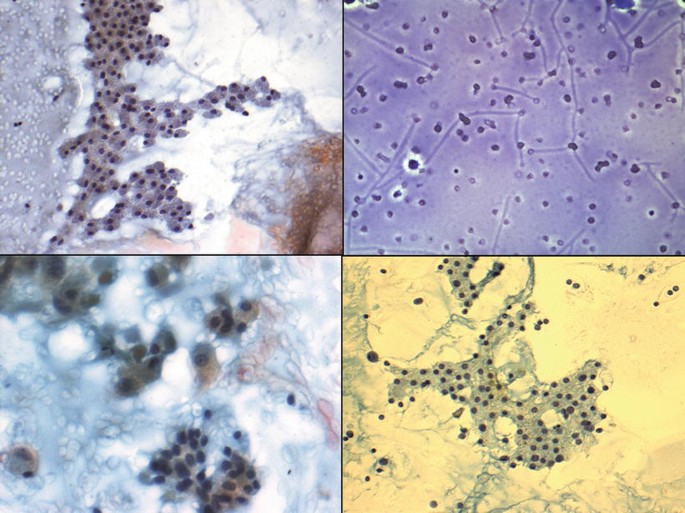
Fig. 4.9
-
(a)
-
Q-9. This aspirate is from a 47-year-old woman who complains of neck fullness. Physical examination shows multiple painless thyroid nodules. Laboratory studies of thyroid function show normal free T4 and TSH levels. Ultrasound examination shows a large prominent nodule measuring 3.5 cm. US-guided FNA is performed. Which of the following is the most likely diagnosis?
-
(a)
Hurthle cell neoplasm
-
(b)
Nondiagnostic, cyst fluid only
-
(c)
Benign, lymphocytic thyroiditis
-
(d)
Benign colloid nodule
-
(e)
Benign, hyperplastic thyroid nodule

Fig. 4.10
-
(a)
-
Q-10. This aspirate is from a 56-year-old woman who complains of neck fullness. Physical examination shows multiple painless thyroid nodules. Laboratory studies of thyroid function show normal free T4 and TSH levels. Ultrasound examination shows a large prominent nodule measuring 3.5 cm. US-guided FNA of the thyroid nodule is performed. Which of the following is the most likely diagnosis?
-
(a)
Hurthle cell neoplasm
-
(b)
Benign colloid nodule
-
(c)
Nondiagnostic, cyst fluid only
-
(d)
Benign, lymphocytic thyroiditis
-
(e)
Benign, hyperplastic thyroid nodule

Fig. 4.11
-
(a)
-
Q-11. This aspirate is from a 45-year-old woman who complains of neck fullness. Physical examination shows multiple painless thyroid nodules. Laboratory studies of thyroid function show normal free T4 and TSH levels. Ultrasound examination shows a large prominent nodule measuring 3.5 cm. US-guided FNA of the thyroid nodule is performed. Which of the following is the most likely diagnosis?
-
(a)
Hurthle cell neoplasm
-
(b)
Benign colloid nodule
-
(c)
Nondiagnostic, cyst fluid only
-
(d)
Benign, lymphocytic thyroiditis
-
(e)
Benign, hyperplastic (adenomatoid) nodule

Fig. 4.12
-
(a)
-
Q-12. This aspirate is from a 55-year-old woman who complains of neck fullness. Physical examination shows multiple painless thyroid nodules with some showing cystic changes. Laboratory studies of thyroid function shows normal free T4 and TSH levels. Ultrasound examination shows a large prominent nodule measuring 4.0 cm. US-guided FNA of the thyroid nodule is performed. Which of the following is the most likely diagnosis?
-
(a)
Benign, reactive atypia/cyst-lining
-
(b)
Malignant, papillary thyroid carcinoma
-
(c)
Malignant, anaplastic carcinoma
-
(d)
Benign, lymphocytic thyroiditis
-
(e)
Benign, hyperplastic nodule

Fig. 4.13
-
(a)
-
Q-13. This aspirate is from a 55-year-old man who noticed a nodule in his neck. Physical examination shows a painless thyroid nodule, 2.0 cm in greatest dimension. Laboratory studies of thyroid function shows normal free T4 and TSH levels. Ultrasound examination shows a large prominent nodule with complex architecture, suspicious for thyroid cancer. US-guided FNA of the thyroid nodule is performed. Which of the following is the most likely diagnosis?
-
(a)
Hurthle cell neoplasm
-
(b)
Benign, colloid nodule
-
(c)
Nondiagnostic, cyst fluid only
-
(d)
Atypical cells of undetermined significance (AUS/FLUS)
-
(e)
Benign, hyperplastic (adenomatoid) nodule

Fig. 4.14
-
(a)
-
Q-14. A 49-year-old woman complains of neck fullness. She has noticed gradual painless enlargement of her thyroid gland for more than 1 year. Physical examination demonstrates diffuse enlargement of the thyroid gland. Laboratory studies of thyroid function show normal free T4 and TSH levels. Ultrasound examination shows a prominent nodule measuring 4.0 cm with complexity of architecture. There is background of multinodular goiter. US-guided FNA of the thyroid nodule is performed. Which of the following is the most likely diagnosis?
-
(a)
Papillary carcinoma
-
(b)
Follicular neoplasm
-
(c)
Benign, hyperplastic/adenomatoid nodule
-
(d)
Medullary carcinoma
-
(e)
Lymphocytic thyroiditis
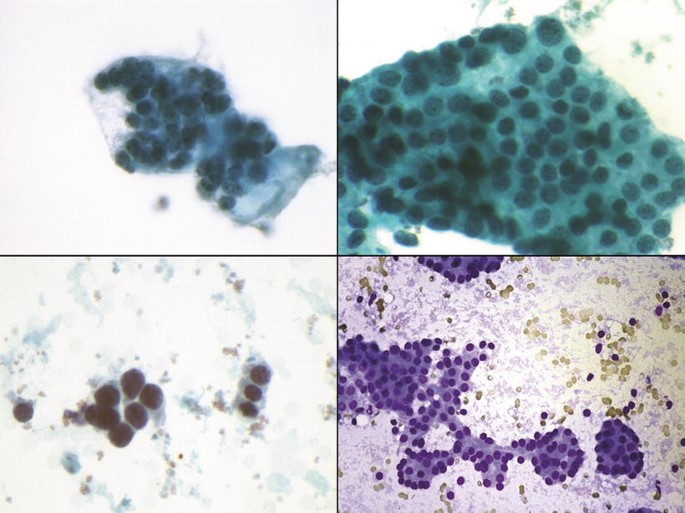
Fig. 4.15
-
(a)
-
Q-15. A 47-year-old man visits his physician because he noticed a “lump” in his neck 3 weeks ago. His past history is unremarkable. On physical examination, there is a 3-cm nodule in the right lobe of the thyroid gland. Laboratory studies of thyroid function shows normal free T4 and TSH levels. US-guided FNA of the thyroid nodule is performed. What is the most appropriate diagnosis of this lesion?
-
(a)
Papillary carcinoma
-
(b)
Follicular neoplasm
-
(c)
Medullary carcinoma
-
(d)
Benign, lymphocytic thyroiditis
-
(e)
Benign, hyperplastic (adenomatoid) nodule

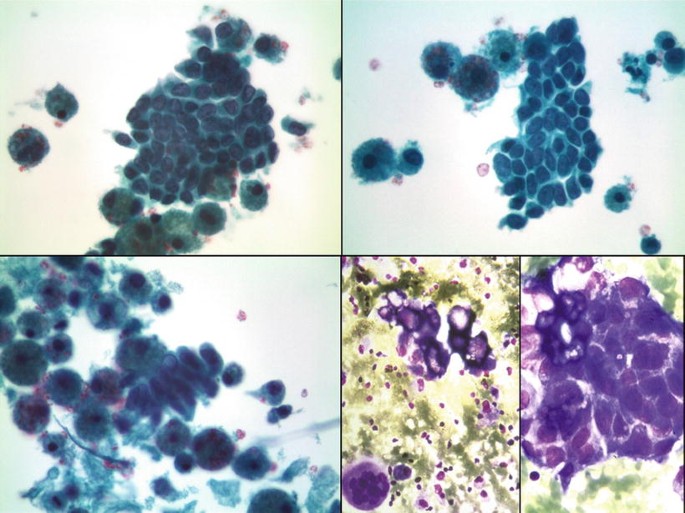
Fig. 4.16
-
(a)
-
Q-16. This aspirate is from a 65-year-old woman who noticed a nodule in her neck. Physical examination shows a painless thyroid nodule, measuring 2.0 cm. Laboratory studies of thyroid function show normal free T4 and TSH levels. The nodule is cold on scan. Ultrasound examination shows a large prominent nodule. US-guided FNA of the thyroid nodule is performed. Which of the following is the most likely diagnosis?
-
(a)
Hürthle cell neoplasm
-
(b)
Benign colloid nodule
-
(c)
Benign, hyperplastic/adenomatoid nodule
-
(d)
Follicular neoplasm
-
(e)
Papillary carcinoma

Fig. 4.17
-
(a)
-
Q-17. A 60-year-old woman has felt a lump on the right side of her neck for several months. On physical examination, she has a firm 3-cm mass in the right lobe of the thyroid gland. There is no palpable lymphadenopathy. Laboratory studies show normal TSH and T4 levels. A fine-needle aspiration biopsy is performed. Which of the following is the most likely diagnosis?
-
(a)
Anaplastic carcinoma
-
(b)
Medullary carcinoma
-
(c)
Granulomatous thyroiditis
-
(d)
Benign, Hashimoto thyroiditis
-
(e)
Follicular neoplasm

Fig. 4.18
-
(a)
-
Q-18. This aspirate is from a 60-year-old woman who has felt a “lump” on the right side of her neck for several months. On physical examination, she has a firm 3-cm mass in the right lobe of the thyroid gland. There is no palpable lymphadenopathy. Laboratory studies show normal TSH and T4 levels. Seven months later, she visits her physician again because of pain in the right hip. A radiograph shows a fracture of the right femur with an area of lytic bone destruction. FNA for both thyroid nodule and femur lesion is performed. Which of the following is the most likely diagnosis?
-
(a)
Anaplastic carcinoma
-
(b)
Follicular neoplasm, favoring follicular carcinoma
-
(c)
Granulomatous thyroiditis
-
(d)
Follicular neoplasm
-
(e)
Medullary carcinoma

Fig. 4.19
-
(a)
-
Q-19. A 62-year-old woman presents with a “lump” on right side of her neck for several months. On physical examination, she has a firm 2.5-cm mass in the isthmus lobe of the thyroid gland. There is no palpable lymphadenopathy. Laboratory studies show normal TSH and T4 levels. US-guided FNA of the thyroid nodule is performed. Which of the following is the most likely diagnosis?
-
(a)
Anaplastic carcinoma
-
(b)
Follicular neoplasm
-
(c)
Benign, granulomatous thyroiditis
-
(d)
Benign, Hashimoto thyroiditis
-
(e)
Hurthle cell neoplasm

Fig. 4.20
-
(a)
-
Q-20. This aspirate is from a 62-year-old man who has felt a “lump” on the left side of his neck. Physical examination reveals a firm 3-cm nodule in the left lobe of the thyroid gland. There is no palpable lymphadenopathy. Laboratory studies show normal TSH and T4 levels. Five months later, he presents with pain in his right hip. A radiograph shows a fracture of the right femur with an area of lytic bone destruction. A radioiodine scan shows uptake localized to the region of the fracture. FNA for both thyroid nodule and femur lesion is performed. Which of the following is the most likely diagnosis?
-
(a)
Anaplastic carcinoma
-
(b)
Hurthle cell metaplasia
-
(c)
Granulomatous thyroiditis
-
(d)
Medullary carcinoma
-
(e)
Hürthle cell neoplasm favoring Hurthle cell carcinoma

Fig. 4.21
-
(a)
-
Q-21. This aspirate is from a 53-year-old woman who has felt a “lump” on the left side of his neck. Physical examination reveals a firm 3.0-cm nodule in the left lobe of the thyroid gland. There is no palpable lymphadenopathy. Laboratory studies show normal TSH and T4 levels. FNA of the thyroid is performed. Which of the following is the most likely diagnosis?
-
(a)
Anaplastic carcinoma
-
(b)
Hürthle cell Carcinoma
-
(c)
Benign, Hurthle cell metaplasia
-
(d)
Benign, granulomatous thyroiditis
-
(e)
Medullary carcinoma

Fig. 4.22
-
(a)
-
Q-22. A 45-year-old man presents to his physician because of “lump” on the left side of his neck. Physical examination shows a nontender nodule on the left lobe of the thyroid gland. A cervical lymph node is enlarged and nontender. Laboratory thyroid studies show no thyroid autoantibodies in his serum, and the T4 and TSH levels are normal. US-guided FNA of thyroid nodule is performed. Which of the following is the most likely diagnosis?
-
(a)
Malignant, anaplastic carcinoma
-
(b)
Benign, Hurthle cell metaplasia
-
(c)
Malignant, papillary thyroid carcinoma
-
(d)
Malignant, medullary carcinoma
-
(e)
Malignant, Hurthle cell carcinoma

Fig. 4.23
-
(a)
-
Q-23. A 45-year-old female presents with a nodule on the right lobe of her thyroid. Physical examination shows a nontender nodule on the right lobe of the thyroid gland. Laboratory thyroid studies show no thyroid autoantibodies in his serum, and the T4 and TSH levels are normal. US-guided FNA of the thyroid nodule is performed. Which of the following is the most likely diagnosis?
-
(a)
Malignant, anaplastic carcinoma
-
(b)
Hurthle cell metaplasia
-
(c)
Malignant, papillary thyroid carcinoma
-
(d)
Malignant, medullary carcinoma
-
(e)
Malignant, Hurthle cell carcinoma

Fig. 4.24
-
(a)
-
Q-24. A 50-year-old man presents with neck mass on the left side. Physical examination shows a nontender nodule on the left lobe of the thyroid gland, 2.5 cm. A cervical lymph node is enlarged and nontender. Laboratory thyroid studies show no thyroid autoantibodies in his serum, and the T4 and TSH levels are normal. US-guided FNA of the thyroid nodule is performed. Which of the following is the most likely diagnosis?
-
(a)
Anaplastic carcinoma
-
(b)
Benign, Hurthle cell metaplasia
-
(c)
Medullary carcinoma
-
(d)
Hurthle cell neoplasm
-
(e)
Papillary carcinoma

Fig. 4.25
-
(a)
-
Q-25. A 55-year-old man presents with large mass on right side of his thyroid. Physical examination shows a nontender nodule on the right lobe of the thyroid gland. A cervical lymph node is enlarged and nontender. Laboratory thyroid studies show no thyroid autoantibodies in his serum, and the T4 and TSH levels are normal. US-guided FNA of the thyroid nodule is performed. ThinPrep smear was prepared. Which of the following is the most likely diagnosis?
-
(a)
Malignant, anaplastic carcinoma
-
(b)
Malignant, papillary thyroid carcinoma
-
(c)
Hurthle cell metaplasia
-
(d)
Malignant, medullary carcinoma
-
(e)
Hurthle cell neoplasm
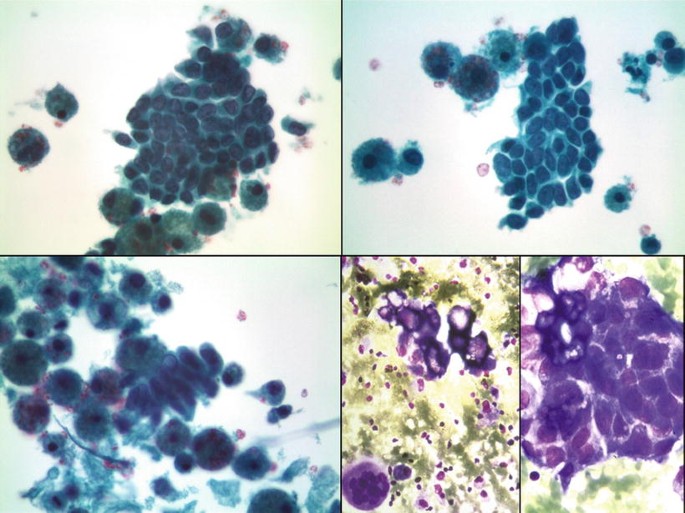
Fig. 4.26
-
(a)
-
Q-26. This aspirate is from a 65-year-old woman who presents to his physician because of “lump” on the left side of her neck. Physical examination shows a nontender nodule on the left lobe of the thyroid gland. Laboratory thyroid studies show normal free T4 and TSH levels. Ultrasound examination shows a cystic lesion with complex architecture. US-guided FNA of the thyroid nodule is performed. Which of the following is the most likely diagnosis?
-
(a)
Malignant, anaplastic carcinoma
-
(b)
Benign, Hashimoto thyroiditis with Hurthle cell metaplasia
-
(c)
Cystic papillary carcinoma
-
(d)
Nondiagnostic, cyst fluid content
-
(e)
Hurthle cell neoplasm

Fig. 4.27
-
(a)
-
Q-27. A 50-year-old man presents to his physician because of “lump” on the left side of his neck. Physical examination shows a nontender enlarged cervical lymph node. Laboratory thyroid studies show normal free T4 and TSH levels. A fine-needle aspiration biopsy of the cervical lymph node is performed. Which of the following is the most likely diagnosis?
-
(a)
Metastatic anaplastic carcinoma
-
(b)
Reactive lymphoid hyperplasia
-
(c)
Metastatic medullary carcinoma
-
(d)
Metastatic papillary thyroid carcinoma
-
(e)
Metastatic Hurthle cell carcinoma

Fig. 4.28
-
(a)
-
Q-28. This aspirate is from a 42-year-old man who presents to his physician because of “lump” on the left side of his neck. Physical examination shows a nontender nodule on the left lobe of the thyroid gland. Laboratory thyroid studies show normal free T4 and TSH levels. Ultrasound examination shows a cystic lesion with complex architecture. US-guided FNA of the thyroid nodule is performed. Which of the following is the most likely diagnosis?
-
(a)
Malignant, anaplastic carcinoma
-
(b)
Suspicious for papillary carcinoma
-
(c)
Malignant, medullary carcinoma
-
(d)
Follicular carcinoma
-
(e)
Hurthle cell neoplasm

Fig. 4.29
-
(a)
-
Q-29. A 38-year-old man feels a small thyroid nodule on the left side of his neck. Physical examination reveals a firm, painless, 2.5- cm cervical lymph node. The thyroid gland is not enlarged. A chest radiograph is unremarkable with normal laboratory studies. Fine-needle aspiration biopsy of the cervical lymph node is performed. Which of the following is the most likely diagnosis?
-
(a)
Papillary carcinoma (Follicular variant)
-
(b)
Medullar carcinoma
-
(c)
Follicular carcinoma
-
(d)
Hurthle cell neoplasm
-
(e)
Anaplastic carcinoma

Fig. 4.30
-
(a)
-
Q-30. A 63-year-old man feels a thyroid nodule on the left side of his neck. Physical examination reveals a firm, painless, 2.5- cm thyroid nodule. The thyroid gland is not enlarged. A chest radiograph is unremarkable with normal laboratory studies. US-guided FNA of the thyroid nodule is performed. Which of the following is the most likely diagnosis?
-
(a)
Papillary thyroid carcinoma, oncocytic variant
-
(b)
Medullar carcinoma
-
(c)
Follicular carcinoma
-
(d)
Hurthle cell carcinoma
-
(e)
Anaplastic carcinoma

Fig. 4.31
-
(a)
-
Q-31. This aspirate is from a 37-year-old man who presents with a single, firm mass within the thyroid gland. Patient has a family history of thyroid tumor affecting his father when he was 32 years of age. Ultrasound examination reveals a solid thyroid mass, suspicious for malignancy. FNA is performed. Which of the following is the most likely diagnosis?
-
(a)
Follicular neoplasm
-
(b)
Papillary thyroid carcinoma
-
(c)
Squamous cell carcinoma
-
(d)
Medullary carcinoma
-
(e)
Benign, nodular goiter

Fig. 4.32
-
(a)
-
Q-32. A 65-year-old man presents to his physician because of “lump” on the left side of his neck. Physical examination shows vague thyroid enlargement but no nodule can be identified. A cervical lymph node is enlarged and nontender. Laboratory thyroid studies show no thyroid autoantibodies in his serum, and the T4 and TSH levels are normal. A fine-needle aspiration biopsy of the cervical lymph node was performed. Which of the following is the most likely diagnosis?
-
(a)
Metastatic anaplastic carcinoma
-
(b)
Benign, reactive lymphoid hyperplasia
-
(c)
Metastatic medullary carcinoma
-
(d)
Metastatic papillary carcinoma
-
(e)
Metastatic Hurthle cell Carcinoma

Fig. 4.33
-
(a)
-
Q-33. This aspirate is from a 30-year-old woman who presents with a single left thyroid nodule. Patient has a family history of thyroid tumor. Ultrasound examination reveals a solid thyroid mass, suspicious for malignancy. FNA is performed. Which of the following is the most likely diagnosis?
-
(a)
Follicular neoplasm
-
(b)
Papillary thyroid carcinoma
-
(c)
Suspicious for medullary carcinoma
-
(d)
Squamous cell carcinoma
-
(e)
Anaplastic carcinoma

Fig. 4.34
-
(a)
-
Q-34. A 76-year-old man with no previous illnesses sees his physician because he has had progressive hoarseness, shortness of breath, and stridor for the past 3 weeks. On physical examination, he has a firm, large, tender mass involving the entire right thyroid lobe. CT scan shows that this mass extends posterior to the trachea and into the upper mediastinum. Cervical lymph nodes were enlarged and X-ray shows multiple pulmonary metastases on chest radiograph. A fine-needle aspiration biopsy of the thyroid mass is performed. Which of the following neoplasms is the most likely diagnosis?
-
(a)
Non-Hodgkin lymphoma
-
(b)
Follicular carcinoma
-
(c)
Medullary carcinoma
-
(d)
Papillary carcinoma
-
(e)
Anaplastic carcinoma

Fig. 4.35
-
(a)
-
Q-35. A 63-year-old man presents with thyroid mass and progressive hoarseness. On physical examination, he has a firm, large, painless mass involving the left thyroid lobe. CT scan shows that this mass extends posterior to the trachea. A fine-needle aspiration biopsy of the mass is performed. Which of the following neoplasms is most likely to be present in this patient?
-
(a)
Large cell lymphoma
-
(b)
Hurthle cell carcinoma
-
(c)
Anaplastic carcinoma
-
(d)
Papillary carcinoma
-
(e)
Medullary carcinoma

Fig. 4.36
-
(a)
-
Q-36. A 70-year-old woman feels a diffuse enlargement of his thyroid gland with sense of fullness and compression. Physical examination reveals a diffuse painless thyroid enlargement. A chest radiograph is unremarkable with normal laboratory studies. A fine-needle aspiration biopsy of the thyroid is performed. Which of the following is the most likely diagnosis?
-
(a)
Papillary carcinoma (follicular variant)
-
(b)
Medullary carcinoma
-
(c)
Follicular carcinoma
-
(d)
Large cell lymphoma
-
(e)
Anaplastic carcinoma

Fig. 4.37
-
(a)
-
Q-37. A 55-year-old man feels a thyroid nodule on the left side of his neck. Physical examination reveals a firm, painless, 2.5- cm thyroid nodule. Patient has past history of renal carcinoma which was treated by nephrectomy. A chest radiograph is unremarkable with normal laboratory studies. US-guided FNA of the thyroid nodule is performed. Which of the following is the most likely diagnosis?
-
(a)
Papillary carcinoma
-
(b)
Medullary carcinoma
-
(c)
Metastatic renal cell carcinoma
-
(d)
Metastatic squamous cell carcinoma
-
(e)
Hurthle cell neoplasm

Fig. 4.38
-
(a)
-
Q-38. A 55-year-old man feels a thyroid nodule on the left side of his neck. Physical examination reveals a firm, painless, 2.5- cm thyroid nodule. Patient has past history of heavy smoking for many years. A fine-needle aspiration biopsy of the thyroid nodule is performed. Which of the following is the most likely diagnosis?
-
(a)
Papillary carcinoma
-
(b)
Medullary carcinoma
-
(c)
Metastatic renal cell carcinoma
-
(d)
Metastatic squamous cell carcinoma
-
(e)
Hurthle cell neoplasm

Fig. 4.39
-
(a)
-
Q-39. A 55-year-old man feels a thyroid nodule on the left side of his neck. Physical examination reveals a firm, painless, 3.0- cm thyroid nodule. Patient has past history of skin melanoma 8 months ago. US-guided FNA of the thyroid nodule is performed. Which of the following is the most likely diagnosis?
-
(a)
Papillary carcinoma
-
(b)
Metastatic melanoma
-
(c)
Metastatic renal cell carcinoma
-
(d)
Metastatic squamous cell carcinoma
-
(e)
Hurthle cell neoplasm

Fig. 4.40
-
(a)
-
Q-40. A 45-year-old woman feels a thyroid nodule on the left side of her neck. Physical examination reveals a firm, painless, 1.5- cm thyroid nodule. Laboratory thyroid studies show normal free T4 and TSH levels. Patient has a history of kidney stones. US-guided FNA of the nodule is performed. Which of the following is the most likely diagnosis?
-
(a)
Colloid nodule
-
(b)
Hyperplastic thyroid nodule
-
(c)
Papillary carcinoma
-
(d)
Follicular neoplasm
-
(e)
Parathyroid adenoma

Fig. 4.41
-
(a)
-
Q-41. This aspirate is from a 27-year-old man who complains of a 3-cm right cystic thyroid nodule. Laboratory studies of thyroid function show normal free T4 and TSH levels. Ultrasound examination shows a 3-cm cystic/solid lesion. US-guided FNA is performed. Which of the following is the most likely diagnosis?
-
(a)
Benign, colloid nodule
-
(b)
Benign, thyroid colloid cyst
-
(c)
Benign, lymphocytic thyroiditis
-
(d)
Nondiagnostic, unsatisfactory specimen
-
(e)
Benign, intrathyroidal branchial cleft cyst

Fig. 4.42
-
(a)
-
Q-42. A 21-year-old young woman presents with a nontender left thyroid nodule. A cervical lymph node is enlarged and nontender. Laboratory thyroid studies show normal free T4 and TSH levels. US-guided FNA of thyroid nodule is performed. Which of the following is the most likely diagnosis?
-
(a)
Malignant, papillary thyroid carcinoma
-
(b)
Malignant, anaplastic carcinoma
-
(c)
Benign, Hurthle cell metaplasia
-
(d)
Malignant, medullary carcinoma
-
(e)
Malignant, Hurthle cell carcinoma

Fig. 4.43
-
(a)
-
Q-43. A 38-year-old woman presented with a thyroid nodule on the left side of her neck. Physical examination reveals a firm, painless 2- cm thyroid nodule. Laboratory thyroid studies show normal free T4 and TSH levels. US-guided FNA of the nodule is performed. Which of the following is the most likely diagnosis?
-
(a)
Benign, colloid nodule
-
(b)
Benign, hyperplastic thyroid nodule
-
(c)
Papillary carcinoma
-
(d)
Follicular carcinoma
-
(e)
Parathyroid adenoma/hyperplasia

Fig. 4.44
-
(a)
-
Q-44. The most likely immunostain in this case (insert) is:
-
(a)
TTF-1
-
(b)
Calcitonin.
-
(c)
PTH
-
(d)
Thyroglobulin
-
(e)
CD138
-
(a)
4.2 Text-Based Questions 45–50
-
Q-45. All of the following are correct about insular/poorly differentiated carcinoma of the thyroid except:
-
(a)
The smears are usually highly cellular and composed of monomorphic appearing small follicular cells, occurring singly and in clusters.
-
(b)
The neoplastic cells show scant delicate cytoplasm with round hyperchromatic nuclei, coarsely granular chromatin, and mild to moderate nuclear irregularities.
-
(c)
Many naked nuclei are often present in the background. Microfollicles as well as infrequent grooves and inclusions can be seen, mimicking follicular neoplasm and PTC. Colloid is scant.
-
(d)
Although foci of necrosis are common in histologic sections, necrosis is generally not appreciated on cytologic preparations.
-
(e)
It is a rare aggressive malignancy and accounts for 4–7 % of thyroid carcinoma and the disease is slightly more frequent in men and young adult. Metastases to regional lymph nodes are uncommon.
-
(a)
-
Q-46. Which is true about malignant lymphoma of the thyroid?
-
(a)
The smears usually show a monomorphic cell with eccentric nuclei.
-
(b)
The differential diagnosis includes lymphoid hyperplasia, lymphocytic thyroiditis, and papillary thyroid carcinoma.
-
(c)
Primary thyroid lymphoma represents approximately 15 % of all thyroid tumors.
-
(d)
Diffuse large B-cell lymphoma and extranodal marginal zone B-cell lymphoma are the most common types.
-
(e)
The tumor presents as a firm cervical mass of rapid growth that in a third of the cases is accompanied by compressive symptoms (hoarseness, dyspnea, dysphagia, and obstruction of the vena cava).
-
(a)
-
Q-47. Which is true about anaplastic thyroid carcinoma?
-
(a)
The cells can be arranged as large clusters.
-
(b)
Tumor cells can be monotonous or columnar.
-
(c)
The nuclei are large, pleomorphic with irregular nuclear membranes, coarse and irregular chromatin clumping, and macronucleoli.
-
(d)
Intranuclear inclusions are rarely seen.
-
(e)
Anaplastic carcinoma/undifferentiated carcinoma (UC) represents more than 5 % of all thyroid carcinomas.
-
(a)
-
Q-48. Which is true about psammoma bodies in thyroid FNA?
-
(a)
Psammoma bodies are basophilic calcified material.
-
(b)
It is seen in 80 % of papillary thyroid carcinoma.
-
(c)
Psammoma bodies are specific for papillary thyroid carcinoma.
-
(d)
Psammoma bodies can be seen in benign conditions and in Hürthle cell neoplasms.
-
(e)
Psammoma bodies and dystrophic calcification are the same.
-
(a)
-
Q-49. All of the following thyroid FNA are considered satisfactory except:
-
(a)
A thyroid FNA with abundant of colloid with no follicular or Hurthle cells seen
-
(b)
A thyroid FNA with lymphoid tissue and no follicular or Hurthle cells seen
-
(c)
Hypocellular smears with few atypical cells showing large, pleomorphic nuclei with irregular nuclear membranes, coarse and irregular chromatin clumping, and macronucleoli
-
(d)
Predominance of histiocytes, cholesterol clefts, and cellular debris
-
(e)
Smears with colloid and only six sheet of Hurthle cells and no follicular cells
-
(a)
-
Q-50. The management of thyroid FNA with an initial diagnosis of nondiagnostic/unsatisfactory should be repeated within:
-
(a)
One year
-
(b)
One week
-
(c)
Two week
-
(d)
Three weeks
-
(e)
Two to three months
-
(a)
4.3 Answers and Discussion of Image-Based Questions 1–44
-
A-1. (a) Benign thyroid nodule.
The images represent thyroid FNA with abundance of colloid with rare clusters of follicular cells (less than six clusters). Aspirates with large amounts of colloid are considered adequate for interpretation even when they contain less the six groups of follicular cells. Thyroid FNA is considered adequate for evaluation if it contains a minimum of six groups of well-visualized follicular cells, with at least ten cells per group, preferably on a single slide. However, exceptions to this requirement apply to three special circumstances: (1) Solid nodules with cytologic atypia. A sample that contains significant cytologic atypia is never considered nondiagnostic. It is mandatory to report any significant atypia as atypical (FLUS or AUS) or other abnormal category. A minimum number of follicular cells in these circumstances is not required. (2) Solid nodules with inflammation (lymphocytic/Hashimoto thyroiditis, thyroid abscess, or granulomatous thyroiditis) may contain only numerous inflammatory cells with no follicular cells. Such cases are interpreted as benign and not as nondiagnostic and a minimum number of follicular cells is not required. (3) Colloid nodules. Specimens that consist of abundant thick colloid are considered benign and a minimum number of follicular cells is not required if easily identifiable colloid is seen.
-
A-2. (c) Nondiagnostic, cyst fluid only (cystic nodules)
The images show the findings of thyroid cyst. Thyroid cyst fluid may be clear yellow, hemorrhagic, or dark brown. Specimens that consist of cyst contents (macrophages and inflammatory cells) without follicular cells are problematic, as up to 20 % of papillary carcinomas may show only cystic change. At the 2007 Bethesda Conference, it was decided that cyst fluid cases should be considered nondiagnostic, but that they create a separate subcategory called “Cyst Fluid Only” (CFO). Cystic nodules represent from 15 to 25 % of all thyroid nodules, and most are seen as a consequence of ischemia in a nodular goiter or in follicular cell neoplasms. The highest proportion of nondiagnostic specimens occurred in cystic lesions. The incidence of malignancy varies widely from 5 to 51 % of nondiagnostic specimens, depending on the selection criteria for surgical treatment, with papillary carcinoma being most common. In a study that analyzed them separately from other insufficient specimens, the risk of malignancy for a CFO sample was 4 %. Taking into account the incidence of malignancy among these nodules, follow-up evaluation is mandatory and a second or third aspiration, preferably using US guidance, should be done.
Occasional follicular cells with degenerative nuclear (smudging or hyperchromasia) or cytoplasmic (vacuolization) changes can be seen. In some aspirates, nuclei can demonstrate fine pale chromatin and grooves, mimicking papillary carcinoma, and may lead to false-positive diagnosis. The origin of these cells is still debated. Nassar et al. have reported that these cells stained for macrophages marker (CD-68 positive), while Faquin et al. demonstrated that these are reactive follicular cells (cytokeratin and thyroglobulin positive). In addition, lining cells from benign cysts often show reparative features, with dense cytoplasm, distinct cell borders, and prominent nucleoli. The mixture of these atypical reparative cells with benign-looking follicular cells is a clue favoring benignancy rather than malignancy. In addition, cystic papillary thyroid carcinoma often lacks the repair-like spindle morphology and shows other cytologic and nuclear features of papillary carcinoma.
Features associated with benign cysts include complete drainage of the cyst with no residual mass, no recurrence, and absence of cytologic atypia. If the nodule is almost entirely cystic, with no worrisome sonographic features, an endocrinologist might proceed as if this were a benign result. After evacuating any thyroid cyst, a new evaluation must be made, and any residual mass must be reaspirated under ultrasound guidance to rule out thyroid cancer.
-
A-3. (b) Branchial cleft cyst
The images represent the cytologic features of branchial cleft cyst. Branchial cyst usually presents in the lateral neck and can be confused with salivary/thyroid neoplasms. Aspiration of these squamous-lined cyst yields proteinaceous debris with nucleated and anucleated squamous cells, occasional columnar cells, lymphocytes, and germinal center fragments. If the cyst fluid is scant, aspirates may mimic epidermal inclusion cyst. When atypia is prominent, well-differentiated squamous cell carcinoma should be excluded. The presence of numerous anucleated squamous supports a branchial cleft cyst; however, excision should be recommended.
Other cystic lesions of the neck should be considered in the differential diagnosis such as thyroglossal, parathyroid cysts, and cystic lymph node metastases of papillary carcinoma. Clear-colorless fluid, however, should suggest a parathyroid cyst and trigger submitting cyst fluid for parathyroid hormone measurements.
-
A-4. (b) Benign, subacute granulomatous (de Quervain) thyroiditis
The images represent the cytologic findings of subacute thyroiditis. FNA is often painful, preventing adequate sampling. The key cytologic features of thyroiditis of de Quervain are presence of multinucleated giant cells; epithelioid histiocytes admixed with lymphocytes; and neutrophils, frequent degenerated follicular cells and dirty background with cellular debris, naked distorted nuclei, and colloid. Multinucleated giant cells are usually numerous with bizarre, angular shapes and more than 100 nuclei. Cytoplasm is densely granular with occasional colloid droplets, in contrast to the frothy cytoplasm typical of the multinucleated cells in multinodular goiter nodules with cystic degeneration. The degenerated follicular cells contain frequent intracytoplasmic dark-blue granules that correspond to lysosomal debris. In advanced stages, the aspirates contain scant inflammatory cells and reactive fibroblasts.
Subacute (de Quervain) thyroiditis is a rare disease and affects frequently middle-aged patients after a respiratory infection. It is characterized by painful enlargement of the thyroid gland with early, transient hypothyroidism and usually resolves spontaneously in the course of 2 or 3 months.
-
A-5. (e) Chronic lymphocytic (Hashimoto) thyroiditis:
The images show the cytomorphologic features of lymphocytic (Hashimoto) thyroiditis (HT). The aspirate is usually cellular, with numerous dispersed, polymorphic lymphoid populations, often intimately admixed with the follicular cells. Follicular cells occasionally demonstrate reactive changes and atypia, including nuclear grooves and nuclear enlargement. In our experience, HT is one of the most common causes of false-positive diagnosis for papillary carcinoma. Therefore, the diagnostic threshold for papillary thyroid carcinoma should be raised in the presence of lymphocytic thyroiditis and only considered when nuclear features of papillary carcinoma are diffusely present in a population of cells devoid of infiltrating lymphocytes.
HT is an autoimmune disease that usually affects middle-aged women. It is the most common form of noniatrogenic hypothyroidism. The disease usually results in a diffuse, painless goiter with or without nodularity. The diagnosis of HT is usually confirmed clinically by serologic tests for one or more of a variety of circulating autoantibodies; the most common are anti-thyroglobulin and antithyroid peroxidase. Clinically, HT may present as a thyroid nodule. This nodule can be originated by a nonneoplastic proliferation of follicular/Hurthle cells, extensive fibrosis, heavy focal lymphoid infiltrate, or true neoplasm in 17–22 % of the patients. The most common malignancy is papillary carcinoma.
Although the presence of a lymphoid infiltrate is an important clue for the diagnosis of HT, it can be seen in other entities, such as inflammation (tuberculosis), Graves’ disease, lymphoepithelial lesions, papillary carcinoma, and lymphoma. FNA of benign lymphoepithelial lesion is characterized by scant cellularity of the epithelial component and predominance of the lymphoid component. The squamous and mucinous epithelial component may show degenerative changes, but without significant atypia.
-
A-6. (c) Benign, Hurthle cell metaplasia in background of lymphocytic thyroiditis
The images represent the cytologic findings of Hurthle cell nodule associated with HT. Aspirates from HT with a predominance of the epithelial component may be confused with Hürthle cell tumors or with papillary carcinoma. However, in Hürthle cell neoplasms, the oncocytic cells show a uniform appearance, more prominent nucleoli, and a more dyshesive pattern and usually lack the lymphocytic component. Papillary thyroid carcinoma (PTC) variants, such as Warthin-like, tall cell, and oncocytic types, arising in a background of lymphocytic thyroiditis should also be considered in the differential diagnosis. The absence of nuclear and other cytologic features of papillary carcinoma and the presence of inflammatory infiltrate may aid in resolving the problem. In a patient with a history of HT, a nodule is more likely to represent Hürthle cell hyperplasia rather than neoplasm. If the inflammatory infiltrate is the main feature, the cytologic picture may simulate a malignant lymphoma. In these circumstances, flow cytometry, immunohistochemistry, or molecular analysis are necessary to confirm clonality.
-
A-7. (b) Toxic diffuse hyperplasia (Graves’ disease)
The images represent the cytologic findings of toxic diffuse hyperplasia (Graves’ disease). The key cytologic features of Graves’ disease are bloodstained smear with little or no colloid, numerous pale follicular cells dispersed or arrayed in cluster, and discrete to moderate anisonucleosis with marginal cytoplasmic vacuoles. The follicular cells are commonly arranged in flat sheets and have foamy delicate cytoplasm with distinctive flame (flare) cells, because of their irregular and radiating appearance. Flame cells are best appreciated on Diff-Quick stain and represent marginal cytoplasmic vacuoles with red to pink frayed edges, due to expansion of endoplasmic reticulum caused by the low pressure in the syringe during FNA. Flame cells, however, are not specific and may be encountered in other thyroid conditions. Prominent microfollicular architecture, significant nuclear overlapping and crowding, and considerable cell pleomorphism are occasionally seen. Hurthle cells (oncocytes) and lymphocytes may be found in the background. Sometimes the follicular cells display focal nuclear chromatin clearing, but other diagnostic nuclear features of papillary carcinoma are absent. The reported incidence of carcinoma in Graves’ disease is 5 % of cases, of which papillary carcinoma is the most common.
The usefulness of FNA in Graves’ disease is limited because the diagnosis is generally made on the basis of clinical features and laboratory data. Occasionally, however, thyroid nodules develop and prompt FNA. The cytologic features of Graves’ disease are nonspecific, and clinical correlation is needed for a definitive diagnosis.
Graves’ disease is an autoimmune disorder, typically characterized by diffuse goiter, hyperthyroidism, and exophthalmos. It is the most common cause of thyroid hyperfunction and usually affects middle-aged women. Glandular enlargement and hyperfunction are initiated by at least two immunoglobulin G (IgG) antibodies: thyroid-stimulating immunoglobulin (TSI) and thyrotropin-binding inhibitor immunoglobulin (TBII).
-
A-8. (c) Benign, radiation changes
The images show the cytologic features of radiation changes such as enlarged follicular cells with normal nuclear-to-cytoplasmic ratio, cytoplasmic vacuolization, marked nuclear atypia, hyperchromasia, and smudged nuclei with pseudoinclusions. Nuclei vary greatly in size, with dark, coarsely granular chromatin and eosinophilic prominent nucleoli. Cytoplasm is abundant and eosinophilic, suggestive of Hürthle cell change.
The differential diagnosis includes follicular carcinoma, papillary carcinoma, and undifferentiated (anaplastic) carcinoma. Both external radiation to the neck and systemic administration of radioactive iodine (131I) can cause long-term morphologic changes in the thyroid gland. In addition, external radiation has been associated with an increased risk of thyroid cancer. External radiation is used in low doses to treat a variety of benign conditions and in high doses for malignancies like Hodgkin lymphoma. Radioactive iodine is administered to treat hyperthyroidism.
-
A-9. (d) Benign colloid
The images show abundant colloid material and low number of follicular cells. Watery colloid often forms a “thin membrane/cellophane” coating or film and is difficult to recognize in Papanicolaou and Diff-Quik-stained specimens. It can also be confused with serum in bloody specimens. Colloid may also disappear completely in thin-layer liquid-based preparations. Helpful clues are the recognition of cracking and folding in colloid, as well as its tendency to surround follicular cells, whereas serum accumulates at the edges of the slide and around platelets, fibrin, and blood clots. Dense colloid is easy to recognize and has a hyaline quality, with folds imparting a “crazy pavement” appearance and/or cracks.
Colloid nodule aspiration usually shows few follicular cells and may result in a cytologically unsatisfactory specimen. We do not restrict ourselves to the number of follicular cells mentioned in the adequacy section when aspirates are predominately cystic or contain abundant colloid, as the presence of few benign follicular cells (3–4 groups) is sufficient to issue a diagnosis of benign/colloid nodule in these situations. However, we usually add to our diagnosis that colloid nodule is suggested if clinically benign and recommend repeat ultrasound and FNA in 6 months.
Benign colloid nodules are usually encountered in patients with multinodular goiter (MNG). MNG affects over 500 million people, especially in people with low dietary iodine. In the United States, despite iodine supplementation, the prevalence of MNG is roughly 4–7 %. MNG have 2 types of nodules (aspirates): hypocellular (colloid) nodules and hypercellular (hyperplastic) nodules. Hypocellular (colloid) nodules are the most common nodules.
-
A-10. (b) Benign colloid nodule
The aspirate demonstrates the cytologic findings of benign colloid nodule. The smears are hypocellular and consist of abundant colloid material and low number of follicular cells. Follicular cells are predominantly arranged in honeycomb configuration of the evenly spaced thyroid cells with rare follicle formation. During the FNA, most large macrofollicles break into fragments, forming flat sheets arranged in honeycomb sheets. The nuclei are more or less homogeneous, about the size of a red blood cell (7–9 μ), oval or round, centrally located with finely granular chromatin, and small or inconspicuous nucleoli. The cytoplasm is pale and poorly delimited and may have small blue-black granules that are of no diagnostic significance. Isolated cells have marked cytoplasmic fragility and often appear as bare, hyperchromatic nuclei that may simulate lymphocytes. Tissue fragments (microbiopsies) may be sparse or absent. Oncocytic (Hurthle) cells admixed with the usual follicular cells may be observed. The number of macrophages present in the background usually coincides with the extent of cystic degeneration. Focal reparative changes such as the presence of spindle cells and cells with tissue culture medium appearance can be seen. Microfollicles are usually absent or rare finding.
-
A-11. (e) Benign, hyperplastic (adenomatoid) nodule
The images represent the cytologic features of hyperplastic (adenomatoid) nodule. The aspirates are hypercellular with less colloid than seen in colloid nodules. Smears show abundant benign follicular cells arranged in honeycomb appearance and admixed with Hürthle cells in up to 50 % of cases. Macrophages with foamy or hemosiderin-laden cytoplasm, including multinucleated giant cells, are often present and are a nonspecific finding indicating cystic degeneration.
The distinction between a benign hypercellular nodule and papillary carcinoma depends primarily on careful examination of nuclear features. The large, pale nuclei of cyst-lining cells may bear a resemblance to the cells of papillary carcinoma, but missing other nuclear features characteristic of papillary carcinoma. Hürthle cells can be seen but admixed with ordinary follicular cells arranged in macrofollicles, which is a benign finding. By contrast, Hürthle cell neoplasms yield an exclusive population of oncocytic cells. Occasionally FNA is comprised predominantly of microfollicles which can be misinterpreted as follicular neoplasm. Hyperplastic nodule and follicular adenoma can be indistinguishable by FNA. However, both receive the same treatment. Early reports on the application of immunohistochemistry for galectin-3 and MIB-1 appeared promising, but subsequent studies showed overlapping results and were not conclusive.
-
A-12. (a) Benign, reactive atypia/cyst-lining cyst
Focal reparative changes are observed, especially in cystic lesions, including cyst-lining cells with enlarged nuclei, finely granular chromatin, and a squamoid- or spindle-shaped (“tissue-culture cell”) appearance. However, if the cyst-lining cells show marked atypia due to the presence of nuclear grooves, prominent nucleoli, elongated nuclei and cytoplasm, and/or intranuclear cytoplasmic inclusions in an otherwise predominantly benign-appearing sample, then, it may better be categorized as atypical (AUS or FLUS).
-
A-13. (d) Atypical cells of undetermined significance (AUS/FLUS)
The images represent the cytologic findings of atypical cells of undetermined significance. Some thyroid FNAs are not easily classified into the benign, suspicious, or malignant categories. Such cases represent the “indetermined” category and in the Bethesda System are reported as atypical cells of undetermined significance (AUS/FLUS). An AUS/FLUS diagnosis represents 3–7 % of thyroid FNAs. The recommended management is clinical correlation and a repeat FNA at an appropriate interval (6 months). Examples include a sparsely cellular specimen but one that shows a predominance of microfollicles or a case with rare but atypical cells that might represent cyst-lining cells but whose atypia extends beyond the usual.
Resection reveals malignancy in population of patients with repeatedly AUS results or patients with worrisome clinical or sonographic findings. In this selected population, 20–25 % of patients with AUS prove to have cancer after surgery.
-
A-14. (c) Benign, hyperplastic/adenomatoid nodule
The images represent the cytologic findings of hyperplastic adenomatoid nodule. Smears are usually cellular with colloid present. If the amount of colloid is small/scanty or no colloid present and nuclear overlapping is present, then, it should be categorized as follicular neoplasm. Follicular lesions of the thyroid represent the most problematic area in thyroid FNA cytology. Clearly, one of the most difficult problems in thyroid cytology is distinguishing hyperplastic nodule with little colloid from follicular neoplasm with some colloid. On surgical resection, they can be hyperplastic nodules, follicular adenoma, follicular carcinoma, or follicular variant of papillary carcinoma. Aspirates from hyperplastic thyroid nodule are cellular and contain colloid. Microfollicular structures can be seen. However, follicular cells are arranged mainly in flat sheets with a honeycomb configuration. The nuclei are uniform in appearance with smooth contour and approximate the size of RBCs. There is minimal nuclear overlapping and crowding. Although presence of colloidal material is indicative of a benign lesion, some papillary and follicular carcinomas may contain abundant colloid. Nodules with papillary hyperplasia yield follicular cells arranged in papillary structures. Special attention is required to avoid mistaking papillary hyperplasia for papillary carcinoma because nuclear features of papillary carcinoma are not present.
-
A-15. (b) Follicular neoplasm
Synonymous: Suspicious for follicular neoplasm = follicular neoplasm
The images represent the cytologic findings of follicular neoplasm. The purpose of this diagnostic category is to identify a nodule that might be a follicular carcinoma and triage it for surgical excision. The majority of cases in this suspicious category turn out to be follicular adenoma or hyperplastic nodules of multinodular goiter, both of which are more common than follicular carcinoma. About 15–30 % of cases turn to be malignant. As previously mentioned, the mere presence of microfollicles is not diagnostic of follicular neoplasm (FN), as microfollicles may be focally seen in 5–10 % of hyperplastic nodules. Although degenerative changes are often associated with hyperplastic nodule, they may be found in up to 30 % of FN. Low cellularity may be encountered in aspirates of FN due to poor biopsy technique or due to a macrofollicular architecture yielding abundant colloid and scant follicular cells. Some of them are highly vascular, yielding abundant blood and rare follicular groups.
Several studies have evaluated the variability in reporting and diagnosing FN and cellular hyperplastic nodules. Some pathologists apply the terms “follicular lesion” and FN interchangeably, while others require more stringent criteria for the diagnosis of FN. For example, the proportion of microfollicles needed to establish a FN diagnosis has ranged in the literature from none to predominant. A wide range of interobserver variability (fair to substantial) has been reported, even within the same institution. Carpi et al. have shown that the preoperative use of large-needle biopsy may show a mixed pattern of micro- and macrofollicles in 50 % of cases, with very low probability to be neoplastic.
Marked cellularity alone does not qualify the nodule for this category. If the sample is cellular but mostly macrofollicular (intact spheres and flat fragments), a benign interpretation is appropriate. A suspicious interpretation is rendered when the majority of the follicular cells are arranged in (microfollicles or crowded trabeculae/synchial pattern). If nuclear features of papillary carcinoma (nuclear grooves, pseudoinclusions, etc.) are present, the case should be reported as suspicious for papillary carcinoma.
-
A-16. (a) Hürthle cell neoplasm
Synonymous: Suspicious for Hurthle cell neoplasm = Hurthle cell neoplasm
The images represent the cytologic features of Hurthle cell neoplasm. The aspirate is composed exclusively of Hürthle cells. Smears demonstrate often isolated cells with abundant granular eosinophilic cytoplasm, resulting from accumulation of mitochondria. Groups, with crowded and syncytium-like pattern, can be seen. A large nucleolus is more typical of neoplastic than hyperplastic Hürthle cells. Colloid can be present, but abundant lymphocytes and normal follicular cells are absent. Basophilic structures with concentric lamellae, indistinguishable from psammoma bodies, are seen in some cases. The purpose of this diagnostic category is to identify a nodule that might be a Hürthle cell carcinoma (HC) and triage it for surgical excision.
Hürthle cells can be a component of HT when they are admixed with numerous lymphoid cells. Similarly, they can be seen admixed with macrofollicles and colloid, a heterogeneous mixture in MNG. Macronucleoli are usually absent. Macrophages can sometimes be confused with Hürthle cells, and vice versa, particularly with liquid-based preparations, in which the usually granular cytoplasm of Hürthle cells appears microvacuolated. But the pseudovacuolization of Hürthle cells in liquid-based preparations is fine and does not have the coarsely vacuolated appearance of macrophage cytoplasm. In addition, Hürthle cells generally lack hemosiderin and are more polygonal, rather than rounded like macrophages.
Variants of papillary carcinoma (tall cell and oncocytic) can be excluded by the absence of nuclear features diagnostic of papillary carcinoma. Because Hürthle cell tumors can have clear cell features, mimicking metastatic renal cell carcinoma, a clinical history of renal cell carcinoma can alert the cytopathologist to this possibility and should be provided on the requisition. Immunohistochemistry for thyroglobulin and TTF-1 is helpful because renal cell carcinoma is negative for these markers.
-
A-17. (e) Follicular neoplasm
The images represent the cytologic features of follicular neoplasm category. FNAs of follicular neoplasm (FN) are typically highly cellular with little or no colloid. Follicular cells are arranged in microfollicles and/or syncytial fragments, involving greater than 50–75 % of the cellular groups. Microfollicles are defined as groups of cells (6–12 cells) arranged in a ring or rosette-like configuration and often display a repetitive pattern. The syncytial groups exhibit a three-dimensional appearance with loss of cell borders.
The amount of colloid in the background is a very important feature of neoplastic lesions since large pools of colloid are usually seen in benign hyperplastic/adenomatoid nodules or in normo- and macrofollicular adenomas. The presence of abundant blood in the smears rather than being related to poor technique may be of help in the cytodiagnosis because follicular neoplasms are highly vascularized. The nuclei are uniform, slightly enlarged, round with smooth contour, but usually demonstrate prominent overlapping and crowding. The chromatin is finely to coarsely granular, and nucleoli are infrequent. The cytoplasm is pale with poorly defined border and no paravacuolar granules or oxyphilic changes. Significant nuclear atypia may or may not be present and characterized by nuclear enlargement that is greater than twice the size of red blood cells, coarse and clumped chromatin, and prominent enlarged nucleoli. Although large nuclei are more likely to be seen in carcinomas, small nuclei do not rule out malignancy. Nuclei of different sizes are more common in hyperplastic goiter and adenomas than in carcinomas.
-
A-18. (b) Follicular neoplasm, favoring follicular carcinoma
The images represent the cytologic findings of follicular carcinoma. There is no morphometric, cytometric data or even immunocytochemistry permit differentiation of adenomas and well-differentiated (minimally invasive) follicular carcinomas. Distinction of follicular carcinoma from adenoma on cytologic features (even histology) is difficult if not impossible, since histologic confirmation is needed to demonstrate the presence of capsular and/or vascular space invasion. The diagnosis of carcinoma is rendered in this case because of the presence of metastatic disease.
Some studies have reported several cytologic features to predict high cancer risk (40–60 % cancer risk) such as an enlarged nuclei (at least twice the size of RBC), marked nuclear atypia including significant nuclear pleomorphism and irregularity, significant nuclear overlapping, and predominance of microfollicular structures (involving > 75 % of thyroid clusters). Most follicular carcinomas (>90 %) have prominent microfollicular architecture. However, the mere presence of microfollicles is not equated with neoplasia, since they can be seen in hyperplastic nodule. Microfollicles lacking nuclear overlap and mixed with abundant colloid had a 0 % chance of harboring cancer. The issue of nuclear atypia and its relationship to malignancy has been the subject of debate. The presence of microfollicles without cytologic atypia has a low cancer risk (6 %), while the presence of atypia increases the cancer risk to 44 %, most of which represented follicular variant of papillary carcinoma.
-
A-19. (e) Oncocytic (Hürthle cell) neoplasm
The images represent the cytologic features of Hürthle cell neoplasm category. FNA usually render highly cellular aspirates with scant colloid and rare to absent lymphocytes. The oncocytes are arranged mainly in large and small clusters and isolated single cells. Occasional microfollicles may be seen. The cells show uniform appearance and have abundant granular cytoplasm with well-defined border, round to oval nuclei, and granular chromatin. The nuclei show prominent cherry-red nucleoli. Cytologic atypia may be observed in oncocytic lesions, including nuclear enlargement and pleomorphism.
The main differential diagnosis includes oncocytic nodule in association with a nodular goiter or lymphocytic thyroiditis. A mixture of Hürthle cells with benign thyroid follicular cells and colloid favors nodular goiter, while a prominent lymphoid cell component favors lymphocytic thyroiditis. In medullary carcinoma, the nuclei typically have a “salt and pepper” chromatin, but may show pleomorphism with prominent nucleoli and scattered stripped atypical nuclei. Silver and Busseniers called attention to the presence of prominent vascularity and intracytoplasmic lumina as characteristic features of Hürthle cell neoplasms. In contrast, Elliot et al. have confirmed the lack of significance of intracytoplasmic lumina as a differentiating feature between neoplastic and nonneoplastic Hürthle cell lesions. Hürthle cells may occasionally contain nuclear cytoplasmic inclusions and should not be considered a papillary carcinoma in absence of other nuclear features. Hürthle cells arranged in papillary clusters may occasionally be found; however, nuclear features of papillary carcinoma are absent.
-
A-20. (e) Hürthle cell neoplasm favoring Hürthle cell carcinoma
The images represent the cytologic features of the Hürthle cell carcinoma. Similar to FN, there is no morphometric, cytometric data, cytological or even immunocytochemistry permit differentiation of adenomas and well-differentiated (minimally invasive) Hürthle cell carcinomas, since histologic confirmation is needed to demonstrate the presence of capsular and/or vascular space invasion. The diagnosis of Hürthle cell carcinoma was rendered in this case because of the presence of metastatic carcinoma to the bone of right hip.
Some cytologic features may help in establishing the diagnosis of Hurthle cell carcinoma. Nuclear membrane irregularities, nuclear cytoplasmic inclusions, and multiple nucleoli or a cherry-red macronucleolus have been suggested. Nonetheless, using several of these criteria, the diagnostic precision reaches only 60 %, since 67 % of the adenomas and 25 % of nonneoplastic Hürthle cell metaplasias were found to fulfill the cytologic criteria for malignancy. Ordinary follicular cells are usually fairly scarce or absent; their presence in large numbers is a favoring feature of nodular goiter. Hürthle cell tumors constitute 5 % of thyroid tumors and are associated with nodal metastases in 30 % of cases.
-
A-21. (b) Hürthle cell carcinoma
The images represent the cytologic features of the Hürthle cell carcinoma in ThinPrep smear. Nuclear membrane irregularities, nuclear cytoplasmic inclusions, and multiple nucleoli or a cherry-red macronucleolus have been suggested as cytologic criteria to diagnose Hurthle cell carcinoma. However, similar to FN, there is no morphometric, cytometric data, cytological or even immunocytochemistry permit differentiation of adenomas and Hürthle cell carcinomas, since histologic confirmation is needed to demonstrate the presence of capsular and/or vascular space invasion. Using several of these criteria, the diagnostic precision reaches only 60 %, since 67 % of the adenomas and 25 % of nonneoplastic Hürthle cell metaplasias were found to fulfill the cytologic criteria for malignancy. Ordinary follicular cells are usually fairly scarce or absent; their presence in large numbers is a favoring feature of nodular goiter.
-
A-22. (c) Malignant, papillary thyroid carcinoma
The images represent the cytologic features of classic papillary carcinoma (PTC) category. Smears show distinctive architectural and cytologic features. Architectural features include the presence of papillary and tightly cohesive three-dimensional syncytial clusters of neoplastic cells. In other cases, there are large tissue fragments with prominent vascular networks and frequent digitiform projections (complex papilla). The tips of the papillae may appear as spherical cellular fragments (CAPS) with palisaded and overlapping nuclei. Many of the neoplastic groups demonstrate prominent nuclear crowding and overlapping. In most cases, the cytoplasm has a thick “metaplastic” consistency, with well-defined borders.
Nuclear features are the most important diagnostic clues for PTC. The diffuse presence of nuclear grooves, nuclear enlargement, and finely granular (powdery) chromatin must be present, before a definitive diagnosis is rendered. Nuclei are oval and large in size mimicking “bag of potato.” The ground glass appearance of the nuclei seen in histologic sections is an artifact of formalin fixation and is not recognized in cytologic preparations. Nucleoli are often small and peripherally situated against a thickened nuclear membrane. Nuclear grooves may traverse the entire longitudinal axis of the nucleus or may appear as invaginations of the nuclear membrane. Intranuclear pseudoinclusions, which are also distinctive of PTC, are not present in all cases. However, they can be seen in more than 5 % of the cells in 90 % of cases. The inclusions usually have sharp margins and should reflect the color of the cytoplasm of that cell (not just a clear hole in the nucleus). Cell block can be helpful in definitive diagnosis of papillary carcinoma.
Papillary thyroid carcinoma (PTC) is the most common thyroid malignancy, accounting for 80 % of all thyroid cancers in the United States. It can occur at any age, but most patients are between 20 and 50 years old with a female-to-male ratio of 4:1. It is the most common pediatric thyroid malignancy. PTC presents as a solitary nodule or a distinct nodule within a nodular goiter. PTC can be partially or entirely cystic in up to 10 % of cases. In more than 50 % of the patients, regional cervical lymph nodes are affected at the time of surgery. Cervical lymphadenopathy resulting from a metastatic tumor can be the initial presentation in some cases.
-
A-23. (c) Malignant, papillary thyroid carcinoma
The images represent the other cytologic features of classic papillary carcinoma (PTC) category. In addition to the previous distinctive architectural and cytologic features, other features can be seen.
Psammoma bodies are a useful diagnostic feature, identified in only about 50 % of PTC and less frequent on cytologic preparations. Psammoma bodies are not specific and can also be seen in MNG and Hürthle cell neoplasms. However, the presence of psammoma bodies should raise the suspicion of PTC, especially in a cystic background. Psammoma bodies should not be confused with the nonlaminated dystrophic calcification that sometimes is observed in benign thyroid lesions.
A proportion of cases may show multinucleated giant cells, the presence of which should increase awareness about the possibility of PTC and invoke a more thorough search for diagnostic nuclear features. The colloid in papillary carcinoma is scant but fairly characteristic; it is thick (chewing gum colloid) and appears as threads of irregular thickness or dense blobs. Sometimes follicular cells may show degenerative changes, such as cytoplasmic microvacuolization (resembling macrophages).
-
A-24. (e) Papillary thyroid carcinoma
The images represent the cytologic features of classic papillary carcinoma (PTC) category in air-dried preparation (Diff-Quick stain). Although distinctive architectural features of papillary carcinoma can be seen, nuclear details are usually not appreciated. However, nuclei are usually large and oval. Intranuclear inclusion can be identified. Cytoplasm is dense and thick (squamoid in nature).
The colloid in papillary carcinoma is fairly characteristic, particularly in air-dried preparation; it is thick (chewing gum colloid) and appears as threads of irregular thickness or dense blobs. Psammoma bodies are a useful diagnostic feature. Although they are not specific and can also be seen in other conditions, their presence should raise the suspicion of PTC, especially in a cystic background. Psammoma bodies should not be confused with the nonlaminated dystrophic calcification that sometimes is observed in benign thyroid lesions.
-
A-25. (b) Malignant, papillary thyroid carcinoma
The images represent the cytologic features of classic papillary carcinoma (PTC) category in ThinPrep smears. Smears show distinctive architectural and cytologic features. Architectural features include the presence of papillary and tightly cohesive three-dimensional syncytial clusters of neoplastic cells. Large tissue fragments with prominent vascular networks and frequent digitiform projections (complex papilla) were seen. The tips of the papillae may appear as spherical cellular fragments (CAPS) with palisaded and overlapping nuclei. Powdery chromatin nature of nuclei with inconspicuous nucleoli, irregular nuclear membranes, and abundant nuclear grooves are seen in the cells. Intranuclear pseudoinclusions can be seen. The inclusions usually have sharp margins and should reflect the color of the cytoplasm of that cell (not just a clear hole in the nucleus). Cytologic classification is accurate in over 90 % of classic PTC, but is much less reproducible in other PTC variants.
-
A-26. (c) Cystic papillary thyroid carcinoma
The images represent the cytologic findings of papillary carcinoma associated with cystic changes. In cystic PTC or lymph node metastases of papillary carcinoma, aspiration yields abundant brown or bloody fluid with numerous hemosiderin-laden macrophages and occasional follicular neoplastic cells with characteristic nuclear findings and sometimes psammoma bodies.
PTC accounts for the most common cystic neoplasm of the thyroid. FNA is unable to establish a diagnosis of malignancy in 50 % of entirely cystic PTC. This is mainly due to scant cellularity and presence of abundant foamy macrophages, blood, and reparative changes. The hallmark for diagnosing PTC, however, is based on its distinctive nuclear features.
Few cases of papillary carcinoma arising in a thyroglossal cyst have been diagnosed by FNA. Previously described cytologic features are useful in the diagnosis of papillary carcinoma, except squamous metaplasia, because squamous cells are a common component of the nonneoplastic thyroglossal cyst.
-
A-27. (d) Metastatic papillary thyroid carcinoma
The images represent the cytologic findings of metastatic papillary carcinoma. Smears shows the characteristic features of papillary carcinoma, admixed with lymphocytic background. PCs are immunoreactive for keratins, thyroglobulin, and TTF-1.
-
A-28. (b) Suspicious for papillary thyroid carcinoma
The images represent the cytologic features of “suspicious for papillary carcinoma” category. The majority of PTCs are straightforward to diagnose, because most or all of the nuclear and architectural features previously described are clearly identifiable and widespread. It is important to note that there is no single feature that is diagnostic of PTC and that a definitive diagnosis should be based on a constellation of cytologic features. If only one or two characteristic features of PTC are present, or present only focal, or if the sample is sparsely cellular, a malignant diagnosis cannot be made with certainty. Such cases are best classified as “suspicious for papillary carcinoma.” It is important to recognize “suspicious for PTC” as a distinct and separate category, and not to lump it with other “indeterminate” or “follicular neoplasm” diagnoses, due to its substantially greater association with malignancy on surgical follow-up. “Suspicious for PTC” has been reported to show PTC on histologic resection in approximately 75 %, while it is 10–30 % with indeterminate or FN diagnoses. With such a high risk of malignancy, clinicians and patients may consider total thyroidectomy as an alternative management option to lobectomy.
Several studies have attempted to determine the most sensitive cytologic criteria for diagnosing PTC and found nuclear inclusions, nuclear grooves, papillary structures, and metaplastic cytoplasm, when present in combination, to be the most reliable cytologic features. The coexistence of longitudinal folds and nuclear inclusions in the same nucleus is very improbable. Some authors showed that the presence of more than three enlarged nuclei with intranuclear cytoplasmic inclusion in a single aspirate is almost pathognomonic for PTC.
Care must be taken not to overinterpret nonspecific findings as malignant or suspicious for PTC. None of the features mentioned before is diagnostic of PTC by itself, and therefore a diagnosis (or even suspicion) of PTC cannot be made on the basis of a single finding. If a well-sampled nodule has the characteristics of a benign follicular nodule, but a few grooves are present, they have little significance and can be ignored. The same applies to psammoma bodies, which can be also seen in MNG. Nuclear pallor not accompanied by other nuclear changes can result from a technical staining problem. Mimickers of intranuclear pseudoinclusions as a result of a fixation artifact or overlying red blood cells can be seen.
-
A-29. (a) Papillary thyroid carcinoma (Follicular variant)
The images represent the cytologic features of follicular variant of papillary carcinoma category. The follicular variant of PTC (FVPC) is by far the most common of papillary carcinoma subtypes. The smears consist predominately of follicular structures, admixed with flat syncytial sheets. Cells demonstrate large nuclei and fine powdery chromatin and nuclear grooves, specific cytologic nuclear features for the diagnosis of FVPC. Fulciniti et al. emphasized the importance of nuclear grooves and nucleoli over intranuclear inclusions in the diagnosis of FVPC. The predominance of microfollicles in some cases can lead to misclassification as follicular neoplasm. However, careful high power examination of the nuclei and recognition of the nuclear features of PTC in these cases will usually establish the diagnosis of FVPC. FVPC is the second to sampling error as the most common cause of false negative diagnoses in thyroid FNA.
-
A-30. (a) Papillary thyroid carcinoma, oncocytic variant
The images represent the cytologic features of oncocytic variant of papillary carcinoma. Smears are characterized by large tumor cells with abundant dense granular cytoplasm, well-defined cytoplasmic borders, eccentric nuclei, and nuclear features of PTC.
Other PTC variants: The tall-cell variant of papillary carcinoma shows, elongated to tall cells with distinct cell borders, cyanophilic and eosinophilic cytoplasm, and a high nucleocytoplasmic ratio. The nuclear features of PTC, in tall cell variant, are often diffuse and extensive, compared to classic PTC. Often, the nuclei contain numerous inclusions, imparting a soap-bubble appearance. Columnar cell variant of PTC demonstrates columnar cells with ill-defined cell borders, delicate cytoplasm with focal vacuolization/clearing, nuclear pseudostratification, and oval to elongated hyperchromatic nuclei. Architecturally, it may resemble colonic adenocarcinoma.
Diffuse sclerosing papillary carcinoma is a relatively common lesion that affects one or both thyroid lobes and consists of multiple foci of papillary carcinoma immersed in a fibrous stroma with lymphoid infiltration. The smears show a dense lymphocytic inflammatory component together with a monolayer of squamous metaplastic cells and numerous psammoma bodies. Cases with marked stromal lymphocytic infiltrate are also called the Warthin-like variant.
-
A-31. (d) Medullary thyroid carcinoma
The images represent the cytologic features of medullary carcinoma (MTC). MTC is notorious for its variable cytologic appearances, ranging from a monomorphic to a pleomorphic cell population. Typically, medullary carcinoma presents mostly as dyscohesive cells. The neoplastic cells may have a plasmacytoid-, spindle-, epithelioid-, or carcinoid-like appearance, but often a mixture of different cell types is encountered in the same specimen. Binucleated or multinucleated cells are sometimes seen. The cytoplasm has a delicate lacy quality and may show pink cytoplasmic granules. The nuclei are round to oval, with fine to coarse chromatin (salt and pepper), and have small or inconspicuous nucleoli. Occasional intranuclear inclusions are appreciated in some cases. Variable amount of amyloid may be present in the background. Amyloid has an appearance similar to thick colloid, but is confirmed with Congo red stain, which shows apple-green dichroism with polarized light. Immunocytochemical stains for calcitonin and neuroendocrine markers such as chromogranin and Synaptophysin and antigen (CEA) are positive, but negative for thyroglobulin.
Medullary thyroid carcinoma (MTC) constitutes 5–10 % of all thyroid carcinomas. It does not show a sex or age association. About 80–90 % of MTC are sporadic and occur in adults with a mean age of 50 years. The rest occur in children in association with genetic syndromes like multiple endocrine neoplasia (MEN2) syndromes with a dominant autosomal inheritance. Serum calcitonin levels are elevated in most patients and help establish the diagnosis.
-
A-32. (c) Metastatic medullary carcinoma
The images represent the cytologic features of metastatic medullary carcinoma. Up to 50 % of patients with MTC present with regional node metastases, and therefore, MTC should be considered in the differential diagnosis of patients with a positive neck node and an unknown primary. MTC is notorious for its variable cytologic appearances, ranging from a monomorphic to a pleomorphic cell population.
The differential diagnosis of medullary carcinoma includes Hürthle cell tumor, hyalinizing trabecular tumor, papillary carcinoma, anaplastic carcinoma, and metastatic neoplasms, particularly malignant melanoma. However, oncocytic neoplasm usually has cells with well-defined borders, in contrast to ill-defined wispy cytoplasmic borders of medullary carcinoma. Oncocytic tumors show prominent nucleoli and lack the neuroendocrine chromatin pattern. MTC may display intranuclear inclusions, but other diagnostic nuclear features of PTC are absent. Spindle cell melanoma are included in the differential diagnosis of predominately spindle medullary carcinoma, while plasmacytoma and melanoma may be confused with plasmacytoid medullary carcinoma. The most characteristic findings to support the diagnosis of medullary carcinoma are abundant isolated cells with marked variations in size and form, plasmacytic-like cells, and presence of metachromatic cytoplasmic granules. Positive staining for calcitonin in cell blocks is helpful in confirming the cytologic diagnosis of MTC.
-
A-33. (c) Suspicious for medullary thyroid carcinoma
The images represent the cytologic features suspicious for medullary carcinoma (MTC) with amyloid deposit present. MTC is notorious for its variable cytologic appearances, ranging from a monomorphic to a pleomorphic cell population. Typically, medullary carcinoma presents mostly as dyscohesive cells. The neoplastic cells may have a plasmacytoid-, spindle-, epithelioid-, or carcinoid-like appearance, but often a mixture of different cell types is encountered in the same specimen. Binucleated or multinucleated cells are sometimes seen. The cytoplasm has a delicate lacy quality and may show pink cytoplasmic granules. The nuclei are round to oval, with fine to coarse chromatin (salt and pepper), and have small or inconspicuous nucleoli. Occasional intranuclear inclusions are appreciated in some cases. Variable amount of amyloid may be present in the background. Amyloid has an appearance similar to thick colloid, but is confirmed with Congo red stain, which shows apple-green dichroism with polarized light. Positive diagnosis of medullary carcinoma requires elevated serum calcitonin or positive immunocytochemical stains for calcitonin and neuroendocrine markers such as chromogranin and Synpatophysin and CEA are positive, but negative for thyroglobulin. Serum calcitonin levels are elevated in most patients and help establish the diagnosis.
-
A-34. (e) Anaplastic carcinoma/undifferentiated carcinoma
The images represent the cytologic features of anaplastic carcinoma. The cytologic appearance is variable, reflecting the diversity of histologic patterns. Three basic types of anaplastic cells (fusiform, giant, and squamous) can coexist in different proportions, but the predominance of any one lacks prognostic significance. The nuclear features are unmistakably malignant. The cells can be arranged as large loose fragments, small clusters, or isolated cells. Tumor cells can be spindle-shaped or epithelioid, with squamoid features. Nuclei are hyperchromatic and vary widely in size and shape. Extremely large, pleomorphic, and bizarrely shaped cells are seen. Some FNAs contain numerous osteoclast-type multinucleated giant cells. The nuclear features are unmistakably malignant. The nuclei are large, pleomorphic with irregular nuclear membranes, coarse and irregular chromatin clumping, and macronucleoli. Intranuclear inclusions are common, and mitotic figures may be numerous. Abundant necrosis may be present in the background.
Anaplastic carcinoma/undifferentiated carcinoma (UC) represents less than 5 % of all thyroid carcinomas. It is the most aggressive thyroid neoplasm: more than 90 % of patients die within a year of diagnosis.
-
A-35. (c) Anaplastic carcinoma
The images represent the cytologic features of anaplastic carcinoma. The cytologic smears are hypercellular and consist of anaplastic cells. The cells can be arranged as large loose fragments, small clusters, or isolated cells. Extremely large, pleomorphic, and bizarrely shaped cells are seen. Some FNAs contain numerous osteoclast-type multinucleated giant cells. Abundant necrosis may be present in the background.
The differential diagnosis of anaplastic carcinoma includes medullary carcinoma, sarcoma, and metastatic carcinoma to the thyroid. Sarcomas can be excluded with an immunohistochemical panel that includes cytokeratins, muscle markers (desmin, Myo-D1, myogenin), and vascular markers (CD31, CD34). Metastatic carcinoma and medullary carcinoma are probably the most important consideration. Anaplastic carcinomas are usually reactive for keratins, but are negative for thyroglobulin and TTF-1. The distinction rests heavily on clinical correlation, imaging studies, and immunohistochemistry; UC is ultimately a diagnosis of exclusion.
-
A-36. (d) Large cell lymphoma
The images represent the cytologic findings of large cell lymphoma. FNA cytology of thyroid lymphoma is similar to its lymph node counterpart. The smears have a monomorphic lymphoid appearance and show many lymphoglandular bodies in the background. Diffuse large B-cell lymphoma and extranodal marginal zone B-cell lymphoma are the most common types. Flow cytometry and/or immunocytochemistry are necessary for establishing a definitive diagnosis, particularly in patients with no previous history. Differential diagnosis includes lymphoid hyperplasia and lymphocytic thyroiditis, both of which are characterized by a polymorphic population of lymphoid cells.
Primary thyroid lymphoma represents approximately 5 % of all thyroid tumors and 2.5–7 % of all extrathyroid lymphomas. Non-Hodgkin lymphoma is by far the most common type, with Hodgkin disease representing a rarity in the thyroid. Because 15 % of patients with systemic malignant lymphomas present with thyroid involvement, systemic disease must be excluded before diagnosing primary thyroid lymphoma. The tumor presents as a firm cervical mass of rapid growth that in a third of the cases is accompanied by compressive symptoms (hoarseness, dyspnea, dysphagia, and obstruction of the vena cava).
-
A-37. (c) Metastatic renal cell carcinoma
The images represent the cytologic features of metastatic renal cell carcinoma. Smears show single cells and sheets with moderate to abundant finely vacuolated/clear cytoplasm and frayed cytoplasmic borders. Nuclear to cytoplasmic ratios may range from low to high, and nucleoli may or may not be prominent. Occasionally, vascularized epithelial fragments are seen. Metastatic renal cell carcinoma should first be excluded, when a neoplasm displays prominent clear cell change.
Cellular proliferations with clear cell features raise the possibility of primary and secondary thyroid neoplasms. Follicular neoplasm (adenoma or carcinoma) may show clear cell features; however, these changes are usually focal, and there is often an associated prominent microfollicular architecture and/or syncytial arrangement and pronounced nuclear overlap and crowding. Clustering of histiocytes and cyst-lining cells may at times raise the possibility of neoplasia; however, these aspirates are of scant cellularity and show spindling and degenerative changes. Granular renal cell carcinoma can cytologically mimic oncocytic neoplasm. Again, the utilization of immunohistochemical stains such as calcitonin, chromogranin, kappa, lambda, cytokeratin, thyroglobulin, and TTF-1 may be helpful in the work-up of renal cell carcinoma. Finally, other metastatic cancers from such sites as lung, head and neck, breast, and liver, as well as germ cell tumors, may show prominent clear cell features and should be considered in the differential diagnosis. Detailed clinical history is crucial. Clear cell carcinoma may appear as synchronic or metachronic disease, even after a long latency period.
In clinical practice, the incidence of metastatic carcinoma amounts to 5.7–7.5 % in preoperative FNA thyroid masses, but in postmortem examination, it ranges from 1.25 to 24.5 %. Metastasis to the thyroid can present as multiple small nodules or as a solitary tumor mass mimicking a primary neoplasm. The majority are produced by contiguous spread of primary neoplasms of the pharynx, larynx, and upper third of the esophagus. In addition, the thyroid is subject to hematogenously disseminated disease in the advanced stages of carcinoma of the breast, lung, and kidney; melanoma; leukemia; and lymphoma. In some cases, metastasis to the thyroid can present after long time from the detection of primary cancer, especially renal cell carcinoma. Breast and lung cancers are the most common primary tumors seen in autopsy studies, while the kidney is the most common site reported in surgical series. Melanoma and colon cancers do not infrequently metastasize to the thyroid. Metastasis should be suspected when the microscopic features appear alien to those neoplasms more commonly encountered in the thyroid. Michelow and Leiman reported 21 cases of metastases to the thyroid gland, in which only five patients had a known history of malignancy.
-
A-38. (d) Metastatic squamous cell carcinoma
The images represent the cytologic findings of metastatic squamous cell carcinoma. Although the appearance of a thyroid nodule in the case of disseminated tumoral disease usually is suggestive of metastatic disease, this is not always so. Approximately 71 % of the thyroid nodules in patients with extrathyroid cancer turn to be benign lesions, metastatic tumors in 17 %, and primary malignant tumors in 6 %.
-
A-39. (b) Metastatic melanoma
The images represent the cytologic findings of metastatic melanoma. Although the appearance of a thyroid nodule in the case of disseminated tumoral disease usually is suggestive of metastatic disease, this is not always so. Approximately 71 % of the thyroid nodules in patients with extrathyroid cancer turn to be benign lesions, metastatic tumors in 17 %, and primary malignant tumors in 6 %.
In recent years, the cytologic characteristics of unusual thyroid lesions have been described. Among the very unusual thyroid lesions, there have been cases of ectopic lingual thyroid, mucoepidermoid carcinoma, synovial sarcoma, neural tumors (schwannoma and malignant peripheral nerve sheath tumor), intrathyroid parathyroid adenoma, squamous cell carcinoma, thymoma, Langerhans histiocytosis, and liposarcoma. Among the extrathyroid lesions initially interpreted as cold nodules, cases of lipoma and thymoma have been reported.
-
A-40. (e) Parathyroid adenoma
Parathyroid adenomas and the rare parathyroid carcinoma can be mistaken clinically for thyroid nodules. Smears are cellular, composed of cohesive sheets, ribbon-like cords, and occasional microacini. Nuclei are round and have a coarsely granular chromatin pattern; nucleoli are small. Cytoplasm is moderately abundant and granular. Isolated cells and naked nuclei can be present. Focal nuclear pleomorphism is seen, but it is not prominent. Colloid is absent.
Parathyroid adenomas are frequently mistaken cytologically for a follicular lesion of the thyroid. Most patients with a parathyroid adenoma have hypercalcemia, which is a clue to the correct diagnosis. Immunohistochemistry for thyroglobulin and parathyroid hormone can be helpful if a nonthyroid origin is suspected.
-
A-41. (e) Benign, intrathyroidal branchial cleft cyst
The images represent the cytologic features of intrathyroidal branchial cleft cyst. Branchial cyst usually presents in the lateral neck and can be presented also as intrathyroid cyst. Aspiration of these cysts shows in addition to follicular cells or colloid, squamous cells and proteinaceous debris with nucleated and anucleated squamous cells, occasional columnar cells, lymphocytes, and germinal center fragments. If the cyst fluid is scant, aspirates may mimic epidermal inclusion cyst. When atypia is prominent, well-differentiated squamous cell carcinoma should be excluded. The presence of numerous anucleated squamous supports a branchial cleft cyst; however, excision should be recommended.
Other cystic lesions of the thyroid should be considered in the differential diagnosis such as thyroglossal, parathyroid cysts, and cystic metastases of papillary carcinoma. Clear-colorless fluid, however, should suggest a parathyroid cyst and trigger submitting cyst fluid for parathyroid hormone measurements.
-
A-42. (a) Malignant, papillary thyroid carcinoma
The images represent the cytologic features of papillary carcinoma (PTC) category with psammoma bodies. Smears show distinctive architectural and cytologic features. Architectural features include the presence of papillary and tightly cohesive three-dimensional syncytial clusters of neoplastic cells. In other cases, there are large tissue fragments with prominent vascular networks and frequent digitiform projections (complex papilla). The tips of the papillae may appear as spherical cellular fragments (CAPS) with palisaded and overlapping nuclei. Many of the neoplastic groups demonstrate prominent nuclear crowding and overlapping. In most cases, the cytoplasm has a thick “metaplastic” consistency, with well-defined borders. Basophilic structures with concentric lamellae, indistinguishable from psammoma bodies, are seen in some cases. Psammoma bodies are a useful diagnostic feature, identified in only about 50 % of PTC and less frequent on cytologic preparations. Psammoma bodies are not specific and can also be seen in MNG and Hürthle cell neoplasms. However, the presence of psammoma bodies should raise the suspicion of PTC, especially in a cystic background. Psammoma bodies should not be confused with the nonlaminated dystrophic calcification that sometimes is observed in benign thyroid lesions.
-
A-43. (e) Parathyroid adenoma/hyperplasia
Parathyroid adenomas and the rare parathyroid carcinoma can be mistaken clinically for thyroid nodules. Smears are cellular and composed of cohesive sheets, ribbon-like cords, and occasional microacini. Nuclei are round and have a coarsely granular chromatin pattern; nucleoli are small or prominent. Cytoplasm is moderately abundant and granular. Isolated cells and naked nuclei can be present. Focal nuclear pleomorphism is seen, but it is not prominent. Colloid is absent. Prominent vascular structures may be seen. Parathyroid adenomas are frequently mistaken cytologically for a follicular lesion of the thyroid. Most patients with a parathyroid adenoma have hypercalcemia, which is a clue to the correct diagnosis. Immunohistochemistry for thyroglobulin and parathyroid hormone can be helpful if a nonthyroid origin is suspected.
-
A-44. (b) Calcitonin
The images represent the cytologic features of medullary carcinoma. MTC has variable cytologic appearances, ranging from a monomorphic to a pleomorphic cell population. Typically, medullary carcinoma presents mostly as dyscohesive plasmacytoid cells. The neoplastic cells may have a plasmacytoid-, spindle-, epithelioid-, or carcinoid-like appearance, but often a mixture of different cell types is encountered in the same specimen. Binucleated or multinucleated cells are sometimes seen. The cytoplasm has a delicate lacy quality and may show pink cytoplasmic granules. The nuclei are round to oval, with fine to coarse chromatin (salt and pepper), and have small or inconspicuous nucleoli. Occasional intranuclear inclusions are appreciated in some cases. Variable amount of amyloid may be present in the background. Amyloid has an appearance similar to thick colloid, but is confirmed with Congo red stain, which shows apple-green dichroism with polarized light.
4.4 Answers and Discussion of Text-Based Questions 45–50
-
A-45. (e) It is a rare aggressive malignancy and accounts for 4–7 % of thyroid carcinoma and the disease is slightly more frequent in men and young adult. Metastases to regional lymph nodes are uncommon.
The images represent the cytologic features of insular (poorly differentiated carcinoma). FNA smears are usually highly cellular and composed of monomorphic appearing small follicular cells, occurring singly and in clusters. The neoplastic cells show scant delicate cytoplasm with round hyperchromatic nuclei, coarsely granular chromatin, and mild to moderate nuclear irregularities. Many naked nuclei are often present in the background. Microfollicles as well as infrequent grooves and inclusions can be seen, mimicking follicular neoplasm and PTC. Colloid is scant. Although foci of necrosis are common in histologic sections, necrosis is generally not appreciated on cytologic preparations. A helpful clue to the aggressive nature of this tumor is the presence of increased mitotic activity and individual cell necrosis. In our experience, a definitive diagnosis of insular carcinoma cannot be established by FNA.
The differential diagnosis is broad. The presence of intranuclear inclusions and grooves in many of these tumor cells suggests a PTC, but the prominence of isolated cells is unusual and might suggest PDC. Focal nuclear pleomorphism, if present, raises the possibility of an undifferentiated (anaplastic) carcinoma. Metastatic carcinoma is also in the differential diagnosis. Immunohistochemistry and clinical history may be definitive for solving the problem
.
-
A-46. (d) Diffuse large B-cell lymphoma and extranodal marginal zone B-cell lymphoma are the most common types
The images represent the cytologic findings of large cell lymphoma. FNA cytology of thyroid lymphoma is similar to its lymph node counterpart. The smears have a monomorphic lymphoid appearance and show many lymphoglandular bodies in the background. Diffuse large B-cell lymphoma and extranodal marginal zone B-cell lymphoma are the most common types. Flow cytometry and/or immunocytochemistry is necessary for establishing a definitive diagnosis, particularly in patients with no previous history. Differential diagnosis includes lymphoid hyperplasia and lymphocytic thyroiditis, both of which are characterized by a polymorphic population of lymphoid cells. Primary thyroid lymphoma represents approximately 5 % of all thyroid tumors and 2.5–7 % of all extrathyroid lymphomas. Non-Hodgkin lymphoma is by far the most common type, with Hodgkin disease representing a rarity in the thyroid. Because 15 % of patients with systemic malignant lymphomas present with thyroid involvement, systemic disease must be excluded before diagnosing primary thyroid lymphoma.
-
A-47. (c) The nuclei are large, pleomorphic with irregular nuclear membranes, coarse and irregular chromatin clumping, and macronucleoli.
The cytologic appearance of anaplastic thyroid carcinoma is variable, reflecting the diversity of histologic patterns. Three basic types of anaplastic cells (fusiform, giant, and squamous) can coexist in different proportions, but the predominance of any one lacks prognostic significance. The nuclear features are unmistakably malignant. The cells can be arranged as large loose fragments, small clusters, or isolated cells. Tumor cells can be spindle-shaped or epithelioid, with squamoid features. Nuclei are hyperchromatic and vary widely in size and shape. Extremely large, pleomorphic, and bizarrely shaped cells are seen. Some FNAs contain numerous osteoclast-type multinucleated giant cells. The nuclear features are unmistakably malignant. The nuclei are large, pleomorphic with irregular nuclear membranes, coarse and irregular chromatin clumping, and macronucleoli. Intranuclear inclusions are common, and mitotic figures may be numerous. Abundant necrosis may be present in the background. Therefore, the presence of rare pleomorphic cells associated with necrosis, in an elderly patient, should raise the possibility of anaplastic carcinoma and trigger additional studies. The cytoplasm can be densely granular or contain tiny vacuoles. Tumor cells may be accompanied by an inflammatory component rich in neutrophils and may show neutrophilic cannibalism.
Anaplastic carcinoma/undifferentiated carcinoma (UC) represents less than 5 % of all thyroid carcinomas. It is the most aggressive thyroid neoplasm: more than 90 % of patients die within a year of diagnosis.
-
A-48. (d) Psammoma bodies can be seen in benign conditions and in Hürthle cell neoplasms.
Psammoma bodies are basophilic structures with concentric lamellae, indistinguishable from psammoma bodies, seen in some cases. Psammoma bodies are a useful diagnostic feature, identified in only about 50 % of PTC and less frequent on cytologic preparations. Psammoma bodies are not specific and can also be seen in MNG and Hürthle cell neoplasms. However, the presence of psammoma bodies should raise the suspicion of PTC, especially in a cystic background. Psammoma bodies should not be confused with the nonlaminated dystrophic calcification that sometimes is observed in benign thyroid lesions.
-
A-49. (d) Predominance of histiocytes, cholesterol clefts, and cellular debris should be considered nondiagnostic cyst fluid only. Abundant of colloid with rare or no clusters of follicular cells should be adequate for benign (satisfactory thyroid FNA) diagnosis. Aspirates with large amounts of colloid are considered adequate for interpretation even when they contain less the six groups of follicular cells. Thyroid FNA is considered adequate for evaluation if it contains a minimum of six groups of well-visualized follicular cells, with at least ten cells per group, preferably on a single slide. However, exceptions to this requirement apply to three special circumstances: (1) Solid nodules with cytologic atypia. A sample that contains significant cytologic atypia is never considered nondiagnostic. It is mandatory to report any significant atypia as atypical (FLUS or AUS) or other abnormal category. (2) Solid nodules with inflammation (lymphocytic/Hashimoto thyroiditis, thyroid abscess, or granulomatous thyroiditis) may contain only numerous inflammatory cells with no follicular cells. Such cases are interpreted as benign and not as nondiagnostic (3) Colloid nodules. Specimens that consist of abundant thick colloid are considered benign and if easily identifiable colloid is seen.
-
A-50. (e) Two to three months
Indications for repeat FNA of thyroid nodules include follow-up of benign nodules, enlarging nodules, nodules larger than 4 cm, recurrent cyst, and an initial unsatisfactory/nondiagnostic FNA. Repeat thyroid FNA, without image-guided, in patients with initial unsatisfactory specimens results in an adequate sample in approximately 50 % of cases. However, repeat US-guided FNA of previously nondiagnostic biopsies can lead to a definitive diagnosis in up to 90 % of cases. This is especially helpful in small nodules less than 1.5 cm and complex cystic lesions, where needles can target the more solid component. On the other hand, repeated US-FNA has led to a more definitive diagnosis in 80 % of “indeterminate for follicular neoplasm” diagnoses with follow-up surgical resection. Repeat FNA in patients with initial benign cytologic diagnoses increases the sensitivity for detecting malignancy from 82 to 90 %. Two to three months interval is recommended to prevent false-positive interpretations due to reactive/reparative changes. US-guided FNA with immediate, onsite adequacy evaluation is preferred for repeat aspiration after an initial nondiagnostic diagnosis.
Reading List
Castro MR, Gharib H. Continuing controversies in the management of thyroid nodules. Ann Intern Med. 2005;142(11):926–31.
Cibas ES. Thyroid. In: Cibas ES, Ducatman BS, editors. Cytology: diagnostic principles and clinical correlates. 3rd ed. Edinburgh: Saunders/Elsevier; 2009.
Cichón S, Anielski R, Konturek A, et al. Metastases to the thyroid gland: seventeen cases operated on a single clinical center. Langenbecks Arch Surg. 2006;391:581–7.
Galera-Davidson H, González-Cámpora R. Thyroid. In: Bibbo M, Wilbur DC, editors. Comprehensive cytopathology. 3rd ed. NJ, USA: Saunders/Elsevier; 2009.
Gharib H, Papini E, Valcavi R, Baskin HJ, Crescenzi A, Dottorini ME, Duick DS, Guglielmi R, Hamilton CR Jr, Zeiger MA, Zini M; AACE/AME Task Force on Thyroid Nodules. American Association of Clinical Endocrinologists and Associazione Medici Endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules. Endocr Pract. 2006;12(1):63–102.
Guarda LA, Peterson CE, Hall W, et al. Anaplastic thyroid carcinoma. Cytomorphology and clinical implications of fine needle aspiration. Diagn Cytopathol. 1991;7:63–7.
Khalbuss WE, Monaco SE, Pantanowitz L. Chapter 15. Thyroid. In: In the ASCP quick compendium (QC) of cytopathology. Chicago: ASCP Press; 2013. p. 314–39.
Koss LG, Melamed MR. Thyroid cytology. In: Koss LG, Melamed MR, editors. Koss’ diagnostic cytology and its histopathologic bases, vol. 2, set (Hardcover). NY, USA: Lippincott Williams & Wilkins; 2005
Luze T, Totsch M, Banger LI, et al. Fine needle aspiration cytodiagnosis of anaplastic carcinoma and malignant haemangioendothelioma of the thyroid in an endemic goiter area. Cytopathology. 1990;1:305–10.
Michelow PM, Leiman G. Metastases to the thyroid gland: diagnosis by aspiration cytology. Diagn Cytopathol. 1995;13:209–13.
NCI thyroid fine needle aspiration state of the science conference. Review and conclusions document. In: http://thyroidfna.cancer.gov/pages/conclusions/, ed. http://thyroidfna.cancer.gov/pages/conclusions/. 2007.
Papanicolaou Society of Cytopathology recommendations for thyroid fine needle aspiration. Diagnostic terminology and criteria for the cytologic diagnosis of thyroid lesions. www.papsociety.org/guidelines.html. 2006.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Saad, R.S., Silverman, J.F., Khalbuss, W.E. (2015). Thyroid Fine-Needle Aspiration. In: Khalbuss, W., Li, Q. (eds) Diagnostic Cytopathology Board Review and Self-Assessment. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-1477-7_4
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1477-7_4
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-1476-0
Online ISBN: 978-1-4939-1477-7
eBook Packages: MedicineMedicine (R0)