Abstract
Semen analysis is the most important and most widely used test of male fertility potential. In 2010, the World Health Organization (WHO) released new reference values based on the semen analysis results from prospective studies of recent fathers and healthy men from the general population. Although these new cutoff or threshold levels are now evidence-based, a great number of unanswered questions remain regarding the validity of these new reference values in the evaluation of male factor infertility.
In this chapter, we will review the latest WHO semen analysis reference values and the process by which these values were derived. We will also discuss the strengths and limitations of these new reference values in the evaluation and management of male factor infertility and in the context of assisted reproductive technologies (ARTs).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
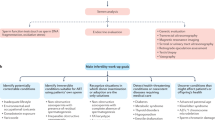
Infertility is defined as the inability to achieve a natural pregnancy after 1 year of unprotected intercourse and a male component is a contributing factor in roughly 50 % of couple infertility [1]. A cross-sectional study in the United States estimated that approximately 3.3–4.3 million men sought medical advice for infertility evaluation [2]. The evaluation of male factor infertility includes a detailed history, physical examination, and two or three semen analyses performed at 3 months interval.
The semen analysis is one of the most important investigations in the assessment of male fertility potential. The semen analysis provides a global measure of testicular and epididymal function (for sperm production and maturation, respectively), vasal patency (for sperm transport), and accessory sexual gland function (for production and delivery of seminal plasma). The semen parameters that are measured on a basic semen analysis include (1) semen volume, (2) sperm concentration and total count, (3) sperm motility, (4) sperm morphology, (5) sperm viability, (6) semen leukocyte concentration, and (7) semen pH. However, the measurement of all of these parameters on the semen analysis does not allow us to clearly differentiate fertile from infertile men because there is significant overlap in semen parameters between these two groups of men.
The history of the modern semen analysis dates back to the 1920s, when Macomber and Sanders assessed human semen and reported a median sperm concentration of 100 million spermatozoa per milliliter, using blood pipettes and a counting chamber [3]. In the 1950s, Macleod et al. compared the semen analyses of 1,000 fertile and 1,000 infertile couples to assess the differences in semen parameters between the two groups [4–7]. Given the increased demand to standardize the semen analysis worldwide, the World Health Organization (WHO) sets forth to standardize the evaluation and interpretation of the semen analysis and published a first manual on the examination of human semen in 1980. The semen analysis guidelines (and reference values) reported in the first WHO manual (1980) and in the subsequent versions (1987, 1992, and 1999) were largely based on the consensus of a panel of experts. The 1980–1999 WHO manuals were based on very little data on semen parameters of fertile men (recent fathers) and this has led some centers to view the reference values as either too high or too low [8–12]. Moreover, the authors (expert panel) of the first four editions of the WHO manuals acknowledged that the semen analysis reference values lacked validity because they were not evidence-based [13–16].
WHO 5th Edition Manual for Examining Semen Analysis
The most recent WHO semen analysis manual was published in 2010. Unlike prior WHO semen analysis manuals, the authors of the recent WHO manual (2010) reported evidence-based reference values for semen parameters [17]. The data used to generate the new semen parameter reference values were obtained from multinational studies of recent fathers with a known time to pregnancy (all had a time to pregnancy of 12 months or less). The total dataset was derived from five studies (conducted in seven countries) and included a total of 1,953 semen analyses (Table 1.1) [11, 12, 17–23]. Using the entire dataset of 1,953 semen analyses, the authors of the new WHO semen analysis guidelines set the semen parameter reference values at the lower 5th percentile. As such, according to the new WHO semen analysis guidelines, men who have one or more semen parameters below the lower 5th percentile are deemed to have an abnormal semen analysis. Nonetheless, it is important to remember that all of the 1,953 men from whom the semen parameter reference values were derived had fathered a child, including those men with an abnormal semen analysis.
There are several important changes in the current WHO semen analysis guidelines when compared to previous guidelines [17]. One of the notable aspects of the current WHO semen parameter cutoffs is that they are lower than reported in the previous WHO manuals (Table 1.2). These lower reference values in no way indicate a decline in semen quality but, rather, are simply a reflection of the new methods of establishing the cutoff values. Also, the assessment of motility has been simplified to include two motility categories (progressive and nonprogressive) rather than the three categories previously reported: rapid progressive (grade a), slow progressive (grade b), and nonprogressive (grade c) motility. This modification in motility evaluation was meant to allow the technician to assess sperm motility in a more objective manner. However, combining rapid (grade a) and slow progressive motility (grade b) into a single reading is a less accurate means of reporting sperm motility and it is unclear how this will affect management of the infertile male. In the current manual, sperm morphology is reported using strict methods (Tygerberg and David) [24].
WHO 2010: Limitations
Although the new WHO manual semen parameter reference values are evidence-based (derived from controlled studies of recent fathers), these reference values have several limitations. One of the notable limitations is that the sample size (n = 1953) from which these reference values were derived is relatively small. Also, the mean age of the fathers was 31 years with only ten men above the age of 45 years, thereby limiting the relevance of these reference values to older men [17]. Another limitation is that the men who were tested came from seven countries and three continents, with 55 % of the population originating from western European cities. This means that in the development of the new reference values, there was clear overrepresentation from some continents (Europe) and no representation from others (e.g., Africa, Asia). This is an important limitation because regional differences in semen parameters between different European cities have been reported [20]. Moreover, Swan et al. [21] have also observed differences in semen parameters between different cities in the United States.
The reference values are based on studies that included men who had submitted only one semen analysis [12]. It is well known that the results of the semen analysis can vary markedly both between different men as well as between different ejaculates from the same man [25, 26]. Also, a fair number of men included in these studies had conditions or prior exposure that might have affected their reproductive health (e.g., prior chemotherapy, radiotherapy, and cryptorchidism) [12, 20] with an indirect effect on their semen analysis. Lastly, the studies included in the new WHO manual used two different sperm morphology evaluation criteria. Auger et al. [19], Bonde et al. [11], Jorgensen et al. [20], Jensen et al. [23], and Slama et al. [12] all used David sperm morphology criteria method which differs from the strict or Tygerberg sperm morphology used by the other studies. Thus, the latest WHO reference value for sperm morphology do not accurately represent either the strict (Tygerberg) or David methods.
Impact of the New WHO Reference Values on Clinical Practice
Establishing a Correct Diagnosis of Male Factor Infertility
The male partner evaluation of an infertile couple includes a detailed history, physical examination, and two or more semen analyses. Although the semen analysis represents a key component of the male evaluation, it is important to recognize that this test does not discriminate infertile from fertile men [27]. The semen parameter reference values reported in the new WHO semen analysis manual provide a more objective framework with which a clinician can gauge a man’s fertility potential because these reference values are evidence-based. However, as with the reference values reported in the previous editions of the WHO manuals, the new WHO reference values also fail to discriminate infertile from fertile men. Therefore, using the lower 5th percentile (of semen parameters) as a threshold to assign or not to assign a diagnosis of male infertility is too simplistic and probably incorrect. Using the 50th percentile, which represents the median value of the reference population, together with the 5th percentile may be a better way to gauge the relative fertility potential of the infertile man as suggested by Esteves et al. [28]. As such, it is important that clinicians integrate clinical parameters (e.g., history, physical examination, other laboratory evaluation) as well as a general sense of the distribution of semen parameter values (e.g., 5th and 50th percentiles) before establishing a diagnosis of male factor infertility (Table 1.3).
If clinicians (e.g., urologists, gynecologists, reproductive endocrinologists) misinterpret the new semen parameter reference values and solely rely on the lower 5th percentile as a threshold to assign a diagnosis of male infertility, it is likely that a large number of couples with male factor infertility will be incorrectly classified as having unexplained infertility because the new (5th edition) WHO semen parameter reference values are lower than the previous WHO reference values. As a result of misinterpreting the new semen parameter reference values, many of these infertile couples will not proceed to a male partner evaluation. For some of these couples, the male evaluation may be postponed until subsequent semen analyses demonstrate abnormal sperm parameters or until other therapies have failed (e.g., assisted reproduction). It is unclear whether this re-classification will be more or less cost-effective but it is likely that assisted reproductive technologies utilization will increase as a result of an increased number of couples now being classified as having unexplained infertility [29].
Impact of the New WHO Reference Values on Treatment of Clinical Varicocele
A clinical varicocele is detected in approximately 35 % of men presenting for infertility evaluation [30] and many of these men have normal or low-normal semen parameters [31]. It has been shown that varicocele repair will result in improved semen parameters and sperm DNA integrity, and in lower seminal oxidative stress [32–36]. Moreover, repair of clinical varicocele may increase pregnancy rates although the number of high-quality studies supporting this premise is low [37, 38].
The current AUA guidelines suggest treating a varicocele if it is clinically palpable and associated with couple infertility and abnormal semen parameters (based on the 4th edition WHO guidelines) [39]. If clinicians adopt and misinterpret the new semen parameter reference values, and, solely rely on the lower 5th percentile as a threshold to assign a diagnosis of male infertility, there will be fewer candidates for varicocele repair because the new (5th edition) WHO semen parameter reference values are lower than the previous WHO reference values. This suggests that many infertile couples with clinical varicocele and normal or low-normal semen parameters (based on the previous, 4th edition, WHO guidelines) will potentially be denied a varicocele repair. Yet, several studies have demonstrated that adults can present with palpable varicocele and normal semen parameters but have abnormal sperm function tests, such as high levels of sperm DNA damage or seminal oxidative stress [33, 40]. Moreover, couples in whom men have clinical varicocele and mild oligozoospermia or normozoospermia will achieve greater spontaneous pregnancy rates after varicocele repair than similar couples with moderate or severe oligozoospermia. Therefore, denying these couples (with clinical varicocele and mild oligozoospermia or normozoospermia) a varicocele repair would be deemed poor clinical practice [41, 42]. Nonetheless, the exact semen parameter thresholds below which an infertile couple with a clinical varicocele is deemed to benefit from varicocele repair remain unknown. Additional prospective studies on the effect of varicocelectomy in infertile couples with clinical varicocele and low-normal semen parameters are needed to address this question, and in particular the relevance of the new WHO reference values in the management of clinical varicocele.
Impact of the New WHO Reference Values on Assisted Reproductive Technologies (ART)
The effect of applying the new reference values into clinical practice on ARTs has not been studied extensively. However, if clinicians use the lower 5th percentile as a threshold to assign a diagnosis of male infertility, it is likely that ART utilization will increase because the new (5th edition) WHO semen parameter reference values are lower than the previous WHO reference values and a greater number of couples will now be classified as having unexplained infertility. Using the 4th edition WHO guidelines, couples with borderline or subnormal semen parameters (e.g., sperm concentration between 15 and 20 million per ml) would have been classified as having male factor infertility, and in many cases would have been offered male-specific therapy. Using the new, 5th edition WHO guidelines, these same couples with borderline or subnormal semen parameters would now be offered ARTs rather than male-specific therapy, if the lower 5th percentile is used as a threshold to assign a diagnosis of male infertility. As such, it is likely that utilization of intrauterine insemination (IUI) and intracytoplasmic sperm injection (ICSI) will increase because there will be larger pool of couples with unexplained infertility. Although many of the couples with borderline or subnormal semen parameters will be offered IUI first, those couples who fail IUI will then likely proceed to ICSI [43–45].
Conclusion
The latest WHO manual is a valuable resource for laboratories analyzing semen samples and clinicians alike. However, it is important to recognize that the new reference values cannot differentiate between fertile and infertile men and the evaluation of the infertile man also needs to include a detailed history and physical examination. There is concern that many infertile men will be exempt from having timely and necessary male evaluation because the new WHO reference limits are lower (compared to prior WHO guidelines) and may be used incorrectly to establish or exclude a diagnosis of male factor infertility. As a result, clinicians will delay male-specific treatments or altogether fail to treat a potentially correctable cause of male factor infertility. The development of new markers of male factor infertility (e.g., sperm function tests or new biomarkers) may help clarify the clinical importance of the semen analysis in the evaluation of the infertile couple.
References
Practice Committee of American Society for Reproductive Medicine. Definitions of infertility and recurrent pregnancy loss: a committee opinion. Fertil Steril. 2013;99(1):63.
Anderson JE, et al. Infertility services reported by men in the United States: national survey data. Fertil Steril. 2009;91(6):2466–70.
Macomber D, Sanders MB. The spermatozoa count. N Engl J Med. 1929;200(19):981–4.
Macleod JF, Gold RZ. The male factor in fertility and infertility. III. An analysis of motile activity in the spermatozoa of 1000 fertile men and 1000 men in infertile marriage. Fertil Steril. 1951;2:187–204.
Macleod JF, Gold RZ. The male factor in fertility and infertility. II. Spermatozoon counts in 1000 men of known fertility and in 1000 cases of infertile marriage. J Urol. 1951;66:436–9.
Mac LJ. The male factor in fertility and infertility; an analysis of ejaculate volume in 800 fertile men and in 600 men in infertile marriage. Fertil Steril. 1950;1(4):347–61.
MacLeod JF, Gold RZ. The male factor in fertility and infertility. IV. Sperm morphology in fertile and infertile marriage. Fertil Steril. 1951;2(5):394–414.
Barratt CL, Dunphy BC, et al. Semen characteristics of 49 fertile males. Andrologia. 1988;20(3):264–9.
Chia SE, Tay SK, Lim ST. What constitutes a normal seminal analysis? Semen parameters of 243 fertile men. Hum Reprod. 1998;13(12):3394–8.
Nallella KP, Sharma RK, et al. Significance of sperm characteristics in the evaluation of male infertility. Fertil Steril. 2006;85(3):629–34.
Bonde JP, Ernst E, et al. Relation between semen quality and fertility: a population-based study of 430 first-pregnancy planners. Lancet. 1988;352(9135):1172–7.
Slama R, Eustache F, et al. Time to pregnancy and semen parameters: a cross-sectional study among fertile couples from four European cities. Hum Prod. 2002;17(2):503–15.
W.H. Organization. WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 2nd ed. Cambridge: Cambridge University Press; 1987.
W.H. Organization. WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 3rd ed. Cambridge: Cambridge University Press; 1992.
W.H. Organization. WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 4th ed. Cambridge: Cambridge University Press; 1999.
W.H. Organization. WHO laboratory manual for the examination of human semen and semen-cervical mucus interaction. 1st ed. Singapore: Press Concern; 1980.
Cooper TG, Noonan E, et al. World Health Organization reference values for human semen characteristics. Hum Reprod Update. 2010;16(3):231–45.
Stewart TM, Liu DY, et al. Associations between andrological measures, hormones and semen quality in fertile Australian men: inverse relationship between obesity and sperm output. Hum Reprod. 2009;24(7):1561–8.
Auger J, Eustache F, et al. Sperm morphological defects related to environment, lifestyle and medical history of 1001 male partners of pregnant women from four European cities. Hum Reprod. 2001;16(12):2710–7.
Jorgensen N, Andersen AG, et al. Regional differences in semen quality in Europe. Hum Reprod. 2001;16(5):1012–9.
Swan SH, Brazil C, et al. Geographic differences in semen quality of fertile U.S. males. Environ Health Perspect. 2003;114(4):414–20.
Haugen TB, Egeland T, Magnus T. Semen parameters in Norwegian fertile men. J Androl. 2006;27(1):66–71.
Jensen TK, Slama R, et al. Regional differences in waiting time to pregnancy among fertile couples from four European cities. Hum Reprod. 2002;16:2697–704.
W.H.Organization. WHO Laboratory Manual for the Examination and Processing of Human Semen. 5th ed. Geneva: WHO Press; 2010. p. 287.
Keel BA. Within- and between-subject variation in semen parameters in infertile men and normal semen donors. Fertil Steril. 2006;85(1):128–34.
Amann RP. Considerations in evaluating human spermatogenesis on the basis of total sperm per ejaculate. J Androl. 2009;30(6):626–41.
Guzick DS, Overstreet JW, et al. Sperm morphology, motility, and concentration in fertile and infertile men. N Engl J Med. 2001;345(19):1388–93.
Esteves SC, Zini A, et al. Critical appraisal of World Health Organization’s new reference values for human semen characteristics and effect on diagnosis and treatment of subfertile men. Urology. 2012;79(1):16–22.
Meacham RB, Joyce GF, et al. Male infertility. J Urol. 2007;177:2058–66.
Greenberg SH, Lipshultz LI, Wein AJ. Experience with 425 subfertile male patients. J Urol. 1978;119(4):507–10.
Bm A-A, Marszalek M, et al. Clinical parameters and semen analysis in 716 Austrian patients with varicocele. Urology. 2010;75(5):1069–73.
Zini A, Blumenfeld A, et al. Beneficial effect of microsurgical varicocelectomy on human sperm DNA integrity. Hum Reprod. 2005;20(4):1018–21.
Agarwal A, Deepinder F, et al. Efficacy of varicocelectomy in improving semen parameters: new meta-analytical approach. Urology. 2007;70(3):532–8.
Smit M, Romijn JC, et al. Decreased sperm DNA fragmentation after surgical varicocelectomy is associated with increased pregnancy rate. J Urol. 2010;183(1):270–4.
Esteves SC, Oliveira FV, Bertolla RP. Clinical outcome of intracytoplasmic sperm injection in infertile men with treated and untreated clinical varicocele. J Urol. 2010;184(4):1442–6.
Schlesinger MH, Wilets IF, Nagler HM. Treatment outcome after varicocelectomy. A critical analysis. Urol Clin North Am. 1994;21(3):517–29.
Baazeem A, Belzile E, et al. Varicocele and male factor infertility treatment: a new meta-analysis and review of the role of varicocele repair. Eur Urol. 2011;60(47):796–808.
Kroese AC, de Lange NM, et al. Varicocele surgery, new evidence. Hum Reprod Update. 2013;19(4):317.
Report on varicocele and infertility. Fertil Steril. 2008;90(5):247–9.
Bertolla RP, Cedenho AP, et al. Sperm nuclear DNA fragmentation in adolescents with varicocele. Fertil Steril. 2006;85(3):625–8.
Kamal KM, Jarvi K, Zini A. Microsurgical varicocelectomy in the era of assisted reproductive technology: influence of initial semen quality on pregnancy rates. Fertil Steril. 2001;75(5):1013–6.
Richardson I, Grotas M, Nagler HM. Outcomes of varicocelectomy treatment: an updated critical analysis. Urol Clin North Am. 2008;35(2):191–209.
Smith S, Pfeifer SM, Collins JA. Diagnosis and management of female infertility. JAMA. 2003;290(13):1767–70.
Nuojua-Huttunen S, Gissler M, et al. Obstetric and perinatal outcome of pregnancies after intrauterine insemination. Hum Reprod. 1999;14(8):2110–5.
Murray KS, James A, et al. The effect of the new 2010 World Health Organization criteria for semen analyses on male infertility. Fertil Steril. 2012;98(6):1428–31.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Alrabeeah, K., Zini, A. (2015). Male Infertility Laboratory Investigation: A Critical Analysis of the 2010 World Health Organization Semen Analysis Guidelines. In: Agarwal, A., Borges Jr., E., Setti, A. (eds) Non-Invasive Sperm Selection for In Vitro Fertilization. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-1411-1_1
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1411-1_1
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-1410-4
Online ISBN: 978-1-4939-1411-1
eBook Packages: MedicineMedicine (R0)