Abstract
Among the cardinal features of malignancy is abrogation of cell death mechanisms, thus endowing cancer and leukemia cells with a selective survival advantage relative to normal cells. Genetic and epigenetic lesions that result in defects in cell death regulation represent an essential characteristic of acute myeloid leukemia (AML), promoting accumulation of leukemia cells by conferring tolerance to oncogene activation, cell cycle checkpoint defects, and genetic instability. Defects in cell death mechanisms also greatly contribute to resistance to cytotoxic anticancer drugs. Bcl-2 family proteins are central regulators of cell life and death, impacting both apoptotic and non-apoptotic cell death. The Bcl-2 family includes both cell survival- and death-promoting members, with the relative levels and activities of these proteins becoming imbalanced in favor of cell survival in AML and most other malignancies. The fundamental mechanisms of Bcl-2 family proteins and some of their roles in AML are reviewed in this chapter.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Defects in the normal apoptosis mechanisms that keep blood cell numbers in check commonly occur during the pathogenesis and progression of hematopoietic malignancies. Most physiological cell death occurs via apoptosis, a type of programmed cell death essential for normal development and adult tissue homeostasis. In addition to promoting clonal cell expansion by extending cell life span, apoptosis defects also contribute to myriad aspects of tumor biology, including (1) factor-independent growth, allowing hematopoietic cells to survive in absence of trophic support from lymphokines or colony-stimulating factors (CSFs); (2) oncogene activation, negating the pro-apoptotic activity of oncoproteins such as c-Myc and Cyclin-D1 that drive cell division and cell death unless complemented by anti-apoptotic mechanisms; (3) tissue infiltration, where invasive properties of leukemias and lymphomas are supported by promoting cell survival in extra-vascular and extra-nodal locations; (4) resistance of immune surveillance mechanisms, especially blunting the pathways that cytolytic T-cells (CTL) and natural killer (NK) cells rely upon for killing tumor target cells; and (5) chemoresistance , where defects in cell death mechanisms raise the threshold for cytotoxicity resulting from macromolecule-damaging drugs that attack DNA, microtubules, and other cellular structures. Thus, restoring sensitivity to apoptosis is an attractive strategy for eliminating malignant cells, which takes advantage in part of the intrinsic abnormalities in neoplastic cells to selectively trigger their death.
From an understanding of the core components of the apoptosis machinery at the molecular and structural levels, and from an emerging knowledge of the signal transduction pathways that link to this core machinery, many potential new therapies for leukemia are beginning to emerge, and new insights into the mechanisms by which currently available therapies work (and why they fail) are accumulating. This knowledge base provides the foundation upon which more effective therapies for hematopoietic malignancies may become a near-term reality.
1.1 Apoptosis Inducers and Effectors
Apoptosis is caused by the activation of intracellular proteases, known as caspases. These cysteine proteases cleave their cellular targets at aspartic acid residues residing in the context of tetrapeptide motifs within polypeptide substrates (Boatright and Salvesen 2003). The human genome encodes ten caspases (Reed et al. 2004; Saleh et al. 2004). Numerous cellular substrates of caspases have been identified, which in aggregate produce the characteristic morphology we call “apoptosis” when cleaved. Several pathways for triggering caspase activation exist, though two have been elucidated in great detail and have been the center of much attention in recent years. These two pathways for apoptosis are commonly referred to as the intrinsic and the extrinsic pathways (Salvesen 2002).
The intrinsic pathway centers on mitochondria as initiators of cell death . Multiple signals converge on mitochondria, including DNA damage, hypoxia, and oxidative stress, causing these organelles to release cytochrome c (cyt c) and other apoptogenic proteins into cytosol. In the cytosol, cyt c binds caspase-activating protein Apaf1, triggering its oligomerization into a heptameric complex that binds pro-caspase-9, forming a multi-protein structure known as the “apoptosome” (Salvesen and Renatus 2002). Physical binding of Apaf1 to pro-caspase-9 is mediated by their caspase recruitment domains (CARDs), through homotypic CARD–CARD binding. Activation of apoptosome-associated cell death protease caspase-9 then initiates a proteolytic cascade, where activated caspase-9 cleaves and activates downstream effector proteases, such as pro-caspase-3.
In contrast, the extrinsic apoptotic pathway relies on tumor necrosis factor (TNF) family death receptors for triggering apoptosis. A subgroup of the TNF family receptors contains a cytosolic death domain (DD) that enables their intracellular interaction with downstream adapter proteins, which link these receptors to specific caspases. Upon ligand binding, TNF family receptors containing cytosolic DDs (e.g., Fas, TNFR, TRAIL-R1, and TRAIL-R2) cluster in membranes, recruiting caspase-binding adaptor proteins, including the bipartite adapter Fas-associated protein with death domain (FADD) that contains both a DD and a death effector domain (DED) (Wallach et al. 1999). The DED of FADD binds DED-containing pro-caspases (e.g., caspases-8 and -10), forming a “death-inducing signaling complex” (DICS) and resulting in caspase activation by an “induced proximity” mechanism (Boatright and Salvesen 2003) .
Aside from the intrinsic and extrinsic pathways, multiple additional routes to caspase activation are possible, though for some the pathophysiological relevance is less well established (reviewed in (Reed 2005; Xu et al. 2005)). Also it is important to note that while these and the aforementioned can all lead to caspase activation and apoptosis, some of them also trigger parallel caspase-independent cell death mechanisms, which nevertheless kill cells via non-apoptotic mechanisms. For example, mitochondria not only release caspase-activating proteins such as cyt c, but also release endonuclease G (Endo G) and a chromatin-modifying protein apoptosis-inducing factor (AIF) that promote genome digestion and cell death independent of caspases (Penninger and Kroemer 2003). Thus, some types of cell death stimuli can induce parallel paths to apoptotic (caspase-dependent) and non-apoptotic (caspase-independent) cell demise .
1.2 Apoptosis Blockers
Given the critical importance of making the correct choices about cell life–death decisions in complex multicellular organisms, it is not surprising that the pathways governing caspase activation are under exquisite control by networks of proteins that directly or indirectly communicate with these proteases . A delicate balance between pro-apoptotic and anti-apoptotic regulators of apoptosis pathways is at play on a continual basis, ensuring the survival of long-lived cells and the proper turnover of short-lived cells in a variety of tissues, including the bone marrow, thymus, and peripheral lymphoid tissues. However, imbalances in this delicate dance of pro- and anti-apoptotic proteins occur in disease scenarios, including cancer where the scales tip in favor of anti-apoptotic proteins and endow cells with a selective survival advantage that promotes neoplasia and malignancy.
The anti-apoptotic proteins responsible for creating roadblocks to apoptosis have been mapped to specific pathways, providing insights into the defective cell death mechanisms that contribute to malignancy. Among these apoptosis blockers are members of the Bcl-2 family , a large group of proteins (n ≥ 25 in humans) that control mitochondria-dependent steps in cell death pathways (Reed et al. 2004), including dictating whether cyt c is or is not released from these organelles. These proteins control the intrinsic pathway (Kroemer and Reed 2000). Bcl-2 family proteins however are also capable of modulating other cell death and cell survival pathways and mechanisms, including the endoplasmic reticulum (ER) pathway for cell death (Demaurex and Distelhorst 2003), the extrinsic (death receptor) pathway, and autophagy (see below).
The Bcl-2 family proteins can be contrasted with other types of anti-apoptotic proteins known to create apoptosis roadblocks in cancer cells, which are discussed in other chapters in this book. Examples of alternative blockers of apoptosis include (a) c-FLIP, a protein that competes with pro-caspase-8 and -10 for interactions with TNF/Fas family death receptors complexes (Tschopp et al. 1998), and (b) IAP family proteins that thwart cell death by directly binding to and suppressing the activity of certain caspases (Deveraux and Reed 1999; Deveraux et al. 1999; Salvesen and Duckett 2002), in addition to other mechanisms .
2 The Bcl-2 Family—Diversity of Players
The human genome encodes at least 25 Bcl-2 family proteins. Only six of these are anti-apoptotic and thus represent logical targets for cancer therapy. The six anti-apoptotic members of the family are Bcl-2, Bcl-XL, Mcl-1, Bcl-W, Bfl-1, and Bcl-B. Overexpression of several of these anti-apoptotic Bcl-2-family proteins has been documented in various hematopoietic malignancies (reviewed in Kitada et al. 2002). The anti-apoptotic members of the Bcl-2 are comprised of alpha-helical bundles with structural similarity to the pore-forming proteins of bacteria (e.g., colicins, diphtheria toxin, etc.). Sequence homology motifs called Bcl-2 homology (BH) domains are recognizable in these proteins, with anti-apoptotic members possessing BH1, BH2, BH3, and BH4 domains. These family members typically also have a C-terminal hydrophobic transmembrane domain that anchors them into intracellular membranes—primarily mitochondria and ER membranes.
Pro-apoptotic Bcl-2 family members can be subgrouped into different categories based on sequence, structure, and function properties, making this type of Bcl-2 family member much more diverse than the anti-apoptotic branch of the family. By definition, all pro-apoptotic family members possess the BH3 domain, an amphipathic alpha-helix that mediates their interactions with anti-apoptotic family members. One subset, characterized by Bax, Bak, and probably Bok, appears to have evolved directly from the same ancestor gene as the anti-apoptotic branch of the family, giving these proteins a similar 3D structure (namely alpha-helical bundled with similar to pore-forming bacterial proteins) and possessing several BH domains (typically BH1, BH2, and BH3, but not BH4). This pro-apoptotic group of the family is sometimes called the “multidomain” branch (reviewed in Reed 2006). The other subset of pro-apoptotic Bcl-2 family proteins typically has little overall structural similarity, with the BH3 domain representing the only commonality. This branch of the family has thus been dubbed the “BH3-only” proteins (reviewed in Bouillet and Strasser 2002). Among the BH3-only proteins are those that (a) bind to the anti-apoptotic family members to neutralize them and (b) those that bind to both anti-apoptotic and the multidomain pro-apoptotic family members, antagonizing the anti-apoptotic and activating the pro-apoptotic proteins.
3 Dimerization of Bcl-2 Family Proteins
Bcl-2 family proteins participate in hand-to-hand combat to control cell life-and-death decisions . The surface of the anti-apoptotic members of the family forms a crevice that serves as a receptor-like structure for binding the ligand-like BH3 domains of the pro-apoptotic proteins. The BH3 domain consists of an amphipathic alpha-helix that binds this hydrophobic crevice on anti-apoptotic Bcl-2-family members, negating their cytoprotective activity (Fesik 2000). Proof-of-concept experiments using BH3 peptides have suggested that compounds docking at this regulatory site on Bcl-2 and its related anti-apoptotic proteins could provide a route to effective suppression of these proteins, thereby promoting apoptosis of malignant cells (Holinger et al. 1999). Indeed, several chemicals have been identified that bind this pocket on anti-apoptotic Bcl-2-family proteins and that promote apoptosis (reviewed in Reed 2005; Pellecchia and Reed 2004; Reed 2008). Small-molecule inhibitors that directly interact with Bcl-2 or related anti-apoptotic proteins via the BH3-binding pocket have entered clinical trials for cancer and leukemia, a topic reviewed elsewhere in this book.
Additionally, some pro-apoptotic BH3-only members of the family use their BH3 domains to activate multidomain pro-apoptotic proteins Bax and Bak (Reed 2006). The structural basis for this protein interaction has been elucidated (Gavathiotis et al. 2010), thus suggesting a possible path to production of agonists of Bax and Bak for oncology therapeutics development .
Various BH3-mimicking compounds have been reported as a strategy for therapeutics development (Vogler et al. 2009; Kang and Reynolds 2009). A critical but unanswered question about the various chemical antagonists of Bcl-2 is to what extent they inhibit various anti-apoptotic members of the Bcl-2-family (n = 6), and whether broad-spectrum versus selective inhibitors would provide the optimal path forward for clinical applications, where efficacy is balanced against toxicity. Moreover, the structure activity relation (SAR) characteristics of the optimal compound may vary depending on the type of cancer or leukemia one wishes to attack, given that the repertoire of Bcl-2 family proteins differs among different types of malignancies. For instance, for optimal treatment of acute myeloid leukemia (AML), one might anticipate that the best compounds will have SAR characteristics that consistently promote apoptosis of AML cells (especially chemorefractory AML cells) but that do not kill normal hematopoietic stem cells .
4 Phenotype Conversion by Bcl-2 Family Proteins
Conditions have been identified where anti-apoptotic Bcl-2 family members can seemingly switch their phenotype, converting into pro-apoptotic proteins . The mechanism underlying this phenomenon involves exposure of the BH3 domain, which in proteins such as Bcl-2 and Bcl-XL is normally buried in the protein, with the interaction surface of the BH3 domain oriented towards the hydrophobic core of the protein. Mechanisms for phenotypic conversion include proteolytic cleavage and interactions with other proteins that promote conformational changes in anti-apoptotic Bcl-2 family proteins. Cleavage of Bcl-2 and Bcl-XL, for example, by caspases removes the N-terminal region containing the BH4 domain, presumably causing an opening of the protein structures that exposes the BH3 domain. Interaction of Bcl-2 with the orphan nuclear receptor, Nur77 (also known as TR3 and NR4A1), has also been identified as a mechanism for phenotype conversion. Stimuli that cause Nur77 to leave the nucleus and traffic to mitochondria cause apoptosis in a Bcl-2-dependent manner (Li et al. 2000). In the cytosol, Nur77 binds the Bcl-2 protein, thus accounting for accumulation of this nuclear receptor on the surface of mitochondria. Nur77 induces a profound conformational change of Bcl-2, causing exposure of this BH3 domain, and converting Bcl-2 from a protector to a killer (Lin et al. 2004). The Nur77-mediated mechanism of phenotypic conversion of Bcl-2 may be particularly relevant to AML, given that Nur77 is frequently epigenetically silenced in AML and considering that double knockout of Nur77 and its close relative Nor1 in mice causes AML (Mullican et al. 2007).
The revelation that the Bcl-2 protein can have two opposing phenotypes, depending upon its interactions with other proteins such as Nur77, suggests a possible explanation for the paradoxical association of higher Bcl-2 levels with favorable (not worse) clinical outcome in some types of cancer (Reed 1996), including some subtypes of AML (Kornblau et al. 1999). Examination of Bcl-2 and Nur77 expression in clinical specimens may help to select patients most likely to benefit from therapeutic strategies designed to stimulate the Nur77 pathway for Bcl-2 conversion, since cells with higher Bcl-2 are more sensitive to Nur77 activators (Lin et al. 2004) .
5 Mitochondrial Mechanisms at the Core of Bcl-2 Family Function
Though Bcl-2 family proteins possess diverse mechanisms by which they can impact cell life-and-death decisions (see below), their central mechanism is believed to relate to regulation of permeability of the outer mitochondrial membrane, thus controlling the release (or sequestration) of apoptogenic proteins stored in the inner membrane space between the inner and outer mitochondria membranes (reviewed in (Chipuk and Green 2008)). When activated, multidomain pro-apoptotic Bcl-2 family members Bax and Bak insert in the outer membrane, oligomerize, evidently forming lipid pores directly or indirectly, cause release of proteins from mitochondria, thus constituting the phenomenon of mitochondrial outer membrane permeabilization (MOMP) (reviewed in Reed 1997; Jurgensmeier et al. 1998; Qian et al. 2008).
Anti-apoptotic Bcl-2 family proteins bind Bax and Bak, preventing their oligomerization in mitochondrial membranes (Fig. 3.1). The BH3-only proteins bind anti-apoptotic proteins, thus neutralizing them and preventing them from binding to and negating the pore-forming proteins Bax and Bak. In addition, a few of the BH3-only proteins (e.g., Bid, Bim, and Puma) not only antagonize the anti-apoptotic members of the family (e.g., Bcl-2 and Bcl-XL), but also bind to and activate the multidomain pro-apoptotic Bax and Bak proteins, stimulating their oligomerization in mitochondrial membranes.
Some studies have also suggested a role for Bcl-2 family proteins in regulating aspects of inner mitochondrial membrane function, particularly as pertains to perturbations in the electrochemical gradient (Chen et al. 2011). This aspect of Bcl-2 protein function is still poorly understood. Roles for interactions of Bcl-2 family proteins with resident mitochondrial proteins such as the voltage-dependent anion channels (VDACs) have also been implicated in mitochondrial control of apoptosis, but their overall importance is unclear (Cheng et al. 2003; Shimizu et al. 1999). Bcl-2 family proteins such as pro-apoptotic Bax have also been reported to impact mitochondrial ultrastructure by regulating membrane fission/fusion proteins such as Opa1 and Dynamin, a feature that has been correlated with remodeling of cristae of mitochondria to affect accessibility of cyt c for release (Yamaguchi et al. 2008; Cassidy-Stone et al. 2008).
6 Bcl-2 Family Proteins at the ER
The ER also plays an important role in regulating cell life-and-death decisions in the context of various cell stress scenarios . At least two aspects of ER biology are relevant. First, the ER is the major storage site for intracellular Ca2 +. Control of release of Ca2 + from the ER has a number of important implications for cell death regulation (reviewed in Demaurex and Distelhorst 2003; Kim et al. 2008a). Second, conditions that cause accumulation of unfolded proteins in the lumen of the ER invoke an evolutionarily conserved signaling program, called the unfolded protein response (UPR). Signaling proteins involved in the UPR are connected to the Bcl-2 family. These mechanisms are described below.
Conversely, the ER appears to be capable of regulating the functions of Bcl-2 family proteins. For example, sphingolipids derived from the ER and delivered into mitochondrial membranes (at sites of direct contact of ER with mitochondria) have been implicated in creating conditions in mitochondrial membranes that are permissive for pore formation by Bax and Bak (Chipuk et al. 2012; Lee et al. 2011) .
6.1 Ca2 + Regulation
Disturbances in intracellular Ca2 + regulation contribute to cell life and death. For example, acute release of Ca2 + from the ER can trigger a variety of signaling mechanisms that promote cell death (Kim et al. 2008b). Conversely, pulses of Ca2 + delivered via inositol triphosphate receptors (IP3Rs) at contact sites of ER with mitochondria promote mitochondrial bioenergetics, sustaining adenosine triphosphate (ATP) and cell survival (Cardenas et al. 2010). Several Bcl-2 family members, particularly the anti-apoptotic members of the family, reside within ER membranes. At least some Bcl-2 family proteins regulate ER Ca2 + homeostasis, with anti-apoptotic proteins Bcl-2 and Bcl-XL reducing the steady-state levels of luminal [Ca2 + ] (Chae et al. 2004; Xu et al. 2008; Kim et al. 2008a; Hunsberger et al. 2011). Various studies have shown that Bcl-2 and Bcl-XL increase passive leak of Ca2 + ions from the ER via a mechanisms that is dependent upon IP3Rs. A picture has emerged that envisions anti-apoptotic Bcl-2 proteins associating with IP3Rs, causing passive leak of Ca2 + to achieve a lower resting (free) Ca2 + concentration in the ER (Rong et al. 2008). In contrast, Bax and Bak increase ER Ca2 + levels (Oakes et al. 2005).
Bcl-2 and Bcl-XL interact in ER membranes with BI-1 (Bax inhibitor-1), a multimembrane ER protein that also regulates ER Ca2 + homeostasis, in a manner that largely phenocopies Bcl-2 (Chae et al. 2004; Xu et al. 2008). Interestingly, gene ablation studies suggest that BI-1 is required for ER Ca2 + regulation by Bcl-XL (Xu et al. 2008). BI-1 also reportedly binds IP3Rs (Kiviluoto et al. 2012) and controls Ca2 + transport from ER to mitochondria via IP3Rs (Sano et al. 2012). Thus, BI-1 appears to collaborate with Bcl-2/Bcl-XL to regulate ER Ca2 +. The impact of ER Ca2 + on tumor cell survival during ER and metabolic stress requires further investigation.
6.2 UPR Regulation
Accumulation of unfolded proteins in the ER stimulates the UPR, also called the ER stress response. ER stress can be induced by myriad stimuli that perturb protein folding, including hypoxia and oxidative stress (via effects on protein disulfide bonding), nutrient perturbations (hypoglycemia/hyperglycemia), and disturbances to cellular protein homeostasis that overwhelm proteasome function and molecular chaperones (Kim et al. 2008b; Ma and Hendershot 2004). (Dong et al. 2005; Shuda et al. 2003; Fernandez et al. 2000). While UPR signaling events clearly help cells (malignant and normal) to adapt to inhospitable microenvironments (Jamora et al. 1996; Li and Lee 2006; Lee 2007; Romero-Ramirez et al. 2004), when sustained or excessive, ER stress triggers cell death, usually by apoptosis but also by non-apoptotic mechanisms (Xu et al. 2005; Kim et al. 2008). Therefore, malignant cells often develop barriers to ER stress-induced apoptosis, providing novel targets for therapeutic intervention. For example, ER stress is causally involved in the cytotoxic activity of proteasome inhibitors used for cancer treatment (Lee et al. 2003). Also, some experimental agents now in clinical testing induce ER stress as their primary mechanism of action (Zou et al. 2008).
While three major signal transduction nodes have been identified as components of the UPR (initiated by IRE1, PERK, ATF6), it is the IRE1 that has been most clearly linked to the mechanism of Bcl-2 family proteins IRE1a is a transmembrane protein that contains both a Ser/Thr-kinase domain and an endoribonuclease domain, the latter of which processes an intron from X box-binding protein-1 (XBP-1) mRNA to produce the 41 kDa XBP-1 protein (a bZIP family transcription factor). XBP-1 binds to promoters of several genes involved in UPR and ERAD (ER-assisted degradation) (Rao and Bredesen 2004), and thus seems to be generally protective. In contrast, the protein kinase activity of IRE1a has been linked to cell death induction, initiated by apoptotic signaling kinase-1 (Ask1), which causes Jun-N-terminal kinase (JNK) activation (Nishitoh et al. 2002).
Bax and Bak reportedly bind IRE1 and activate it, thus inducing a cascade of stress kinase activation (Hetz et al. 2006) (Fig. 3.2). Within these kinase cascades, among the apoptosis-relevant substrates of JNK are Bcl-2 and Bim, which are inhibited and activated, respectively, by JNK phosphorylation (Lei and Davis 2003; Putcha et al. 2003; Srivastava et al. 1998; Wei et al. 2008). Substrates of p38 mitogen-activated protein kinase (MAPK) include transcription factor C/EBP homologous protein (CHOP), which represses expression of the gene encoding Bcl-2 and induces expression of genes encoding Bim and DR5 (TRAIL-R2) (Zou et al. 2008; Lei and Davis 2003; Putcha et al. 2003; McCullough et al. 2001; Puthalakath et al. 2007; Wang and Ron 1996). Prolonged CHOP activity can also promote non-apoptotic cell death via induction of ER oxidase-1a (ERO1a) (Li et al. 2009; Ozcan and Tabas 2012; Marciniak et al. 2004). Thus, IRE1 is a focal point for the ER-relevant activities of Bcl-2-family proteins, with pro-apoptotic Bax and Bak proteins interacting with and activating IRE1 (Hetz et al. 2006). Conversely, cytoprotective Bcl-2-interacting ER membrane protein, BI-1 (Tmbim6) (Xu and Reed 1998; Reimers et al. 2008) binds to and suppresses IRE1 signaling in cultured cells and in mice (Bailly-Maitre et al. 2006; Lisbona et al. 2009; Bailly-Maitre et al. 2010).
7 Autophagy
Autophagy is a catabolic cellular process for lysosome-mediated degradation of senescent proteins and organelles (Bernales et al. 2006; Kruse et al. 2006). Autophagy is implicated in cancer primarily as a survival mechanism , where it provides substrates for maintaining ATP levels during times of nutrient deprivation and hypoxia. However, autophagy that is excessive in nature may also contribute or induce to cell death in some contexts (Levine and Yuan 2005; Kroemer et al. 2010). Among the Bcl-2-interacting proteins is beclin (ATG6), an essential component of the autophagy machinery. The beclin protein has a BH3-like domain that mediates interactions with Bcl-2. Bcl-2 inhibits beclin’s participation in protein complexes that generate autophagic vesicles. Phosphorylation of Bcl-2 by JNK provides a means of freeing beclin to allow autophagy to proceed (Wei et al. 2008), in addition to displacement of beclin from Bcl-2 by various pro-apoptotic BH3-containing proteins.
Interestingly, ER stress also induces autophagy (Bernales et al. 2006; Momoi 2006; Yorimitsu et al. 2006; Ogata et al. 2006), potentially involving a diversity of mechanisms, including (a) changes in ER Ca2+, perhaps mediated by IP3Rs (Hoyer-Hansen and Jaattela 2007; Criollo et al. 2007; Lam et al. 2008; Vicencio et al. 2009); (b) activation of Ca2+ -dependent kinases, including CamKK and DAPK1 (Gozuacik et al. 2008; Zalckvar et al. 2009; Sakaki et al. 2008); and (c) JNK-mediated phosphorylation of Bcl-2 (which causes its release of Beclin-1) occurring downstream of IRE1 signaling (Pattingre et al. 2005; He et al. 2012). Thus, the ability of Bcl-2 family proteins to regulate ER Ca2+ via interactions with IP3Rs and to modulate UPR signaling via interactions with IRE1 appears to establish a complex network of regulatory mechanisms that link the Bcl-2 family to autophagy and cellular resilience.
8 Interacting Proteins and Posttranslational Modifications
A plethora of proteins have been reported to interact with Bcl-2 family members, suggesting that the Bcl-2 family connects to a variety of protein networks and cellular processes as a mechanism for sensing the cellular status. Bcl-2-interacting proteins range from nuclear receptors that exit the nucleus to bind Bcl-2 and promote apoptosis (Nur77, SHP), to molecular chaperones and co-chaperones (FK506-binding proteins, FKBPs; BAG family Hsp70/Hsc70 co-chaperone) that collaborate with Bcl-2 to promote cell survival, to NLR family innate immunity proteins involved in activation of pro-inflammatory caspases, to kinases and phosphatases (reviewed in Chipuk et al. 2010). Pro-apoptotic family members such as Bax have been reported to interact with Hsp27 family chaperone clusterin, innate immunity adapter protein ASC, the cytoprotective peptide humanin, cathepsin family proteases, and more (reviewed in Reed 2006). Much remains unknown about the cellular contexts in both health and disease where these various protein interactions play fundamentally important roles in cell life-and-death decisions.
Post-translational modifications of Bcl-2 family proteins have not been systemically studied, but multiple examples are found in the literature. For example, phosphorylation of Bcl-2 has been shown to modulate its activity (Konopleva et al. 2002), with MEK1 inhibitors suppressing Bcl-2 phosphorylation and displaying robust synergy with chemical inhibitors of Bcl-2 in AML cells (Milella et al. 2002). Akt (PKB) and several other kinases phosphorylate pro-apoptotic protein BAD (a BH3-only protein), causing its sequestration in a complex with 14-3-3 proteins (Khwaja 1999). Dephosphorylation of pro-apoptotic Bak protein on specific tyrosines has been reported to be required for its activation (Fox et al. 2010).
Proteolytic cleavage of Bcl-2 family proteins is another functionally important post-translational modification, with cleavage of pro-apoptotic BH3-only protein Bid serving as a prime example. Bid becomes activated by caspase-8-mediated cleavage in the context of signaling by TNF family death receptors (extrinsic pathway), resulting in its translocation from cytosol to mitochondrial membranes and exposure of its BH3 domain to enable interaction with other Bcl-2 family members (reviewed in Korsmeyer et al. 2000). Bid is also cleaved and activated by other classes of intracellular cysteine proteases in various pathological contexts (Droga-Mazovec et al. 2008; Upton et al. 2008; Stoka et al. 2001; Chen et al. 2001).
Deamidation of Bcl-XL, converting asparagine to isoaspartic acid residues, has been associated with DNA damage responses (Deverman et al. 2002). Deamidation of Bcl-XL impairs its ability to bind various BH3-containing proteins and to reduce its anti-apoptotic activity. Interestingly, defects in Bcl-XL deamidation have been associated with myeloproliferative disorders (Zhao et al. 2008).
Ubiquitination is an important post-translational modification for regulating the stability of Bcl-2 family proteins. For example, anti-apoptotic protein Mcl-1 is the substrate of an E3 ligase (MULE/ARF-BP1) that contains a BH3-like domain, mediating Mcl-1 degradation in the context of DNA damage (Zhong et al. 2005). Phosphorylation impacts Mcl-1 protein stability, with phosphorylation by Erk1 slowing and GSK3β accelerating degradation (Domina et al. 2004; Maurer et al. 2006). In contrast, ubiquitination of Bfl-1 occurs constitutively, keeping levels of Bfl-1 protein low—a mechanism that becomes defective in lymphomas (Fan et al. 2010).
9 Deregulated Expression of Bcl-2 Family Genes in AML
Many examples exist of alterations in the expression of either apoptosis-suppressing or apoptosis-inducing members of the Bcl-2 family in human cancers (reviewed in Reed et al. 2004; Levine and Yuan 2005; Kroemer et al. 2010; Momoi 2006) . The explanations for overexpression of anti-apoptotic proteins of the Bcl-2 family in cancer and leukemia cells vary, but documented mechanisms include chromosomal translocations, gene amplification, loss of microRNAs that target Bcl-2 family genes, gene hypomethylation, transcriptional upregulation, and perhaps altered protein stability (reviewed in (Kitada et al. 2002)).
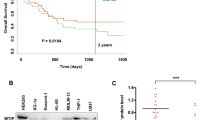
Bcl-2, Bcl-XL, Mcl-1, and, occasionally, other anti-apoptotic members of the Bcl-2 family are commonly overexpressed in AML (Kornblau et al. 1999; Andreeff et al. 1999; Campos et al. 1993;Konopleva and Andreeff 2002; Kasimirbauer et al. 1998; Deng et al. 1998; Lauria et al. 1997; Schaich et al. 2001). In AML, higher levels of Bcl-2 protein or mRNA have been associated with poor responses to chemotherapy and/or shorter overall survival (Campos et al. 1993; Kasimirbauer et al. 1998; Deng et al. 1998; Lauria et al. 1997; Bincoletto et al. 1999; Campos et al. 1997; Rochitz et al. 1999; Maung et al. 1994; Karakas et al. 1998).
Conversely, pro-apoptotic genes that oppose these cytoprotective proteins can become inactivated in malignant cells, through gene deletion, somatic mutation, gene hypermethylation, and transcriptional downregulation and probably other mechanisms. For example, inactivating mutations in the pro-apoptotic Bcl-2 family gene Bax occur in some hematological malignancies including AML (Meiijerink et al. 1995; Brimmell et al. 1998; Meijerink et al. 1998).
The tumor microenvironment undoubtedly contributes to the regulation of Bcl-2 family proteins in AML. Several cytokines, including granulocyte colony-stimulating factor (G-CSF) and Flt3, have been reported to upregulate expression of Bcl-2 and promote apoptosis resistance in freshly isolated AML cells in vitro, implying that the Bcl-2 gene is subject to regulation by inputs from cytokine/lymphokine receptor pathways of the tumor microenvironment (Lisovsky et al. 1996; Bradbury et al. 1994). Lymphokines that activate STAT3 stimulate expression of Bcl-XL. Retinoids also can modulate the expression of Bcl-2 family proteins, including downregulating Bcl-2 and Bcl-XL in AML (Andreeff et al. 1999; Ahmed et al. 1999; Elstner et al. 1996; Dipietrantonio et al. 1996; Delia et al. 1995). Thus, numerous signal transduction and transcriptional pathways may be capable of modulating the expression of Bcl-2 family genes in AML .
10 Cytotoxic Chemotherapy and Bcl-2 Family Proteins
In many instances, cell death induced by anticancer drugs appears to occur via the mitochondrial pathway that involves release of cytochrome c . It remains unclear how damage induced to DNA or other macromolecules by anticancer drug triggers mitochondrial release of cyt c. However, some specific mechanisms have been revealed in recent years. For example, in some types of cells, DNA-damaging agents can induce activation of p53, which in turn binds to cis-acting elements located within the Bax gene and transcriptionally upregulates Bax expression (Miyashita and Reed 1995) and the Bax–activity gene Puma and Bim. The p53 protein has also been reported to modulate the activity of Bcl-2 family proteins in the cytosol and on the surface of mitochondria. Another example of how anticancer drugs activate the mitochondrial (intrinsic) pathway is found in the pro-apoptotic Bcl-2 family protein Bim, which can be activated by anti-microtubule drugs. The Bim protein is normally sequestered at microtubules but can be released into the cytosol when it translocates to the surface of mitochondria, heterodimerizing with Bcl-2 or Bcl-XL and triggering cytochrome c release .
References
Ahmed N, Sammons J, Hassan H (1999) Bcl-2 protein in human myeloid leukemia cells and its down-regulation during chemotherapy-induced apoptosis. Oncol Rep 6(2):403–407
Andreeff M, Jiang SW, Zhang X, Konopleva M, Estrov Z, Snell VE et al (1999) Expression of Bcl-2-related genes in normal and AML progenitors: changes induced by chemotherapy and retinoic acid. Leukemia 13:1881–1892
Bailly-Maitre B, Fondevila C, Kaldas F, Droin N, Luciano F, Ricci JE et al (2006) Cytoprotective gene bi-1 is required for intrinsic protection from endoplasmic reticulum stress and ischemia-reperfusion injury. Proc Natl Acad Sci U S A 103:2809–2814
Bailly-Maitre B, Belgardt BF, Jordan SD, Coornaert B, von Freyend MJ, Kleinridders A et al (2010) Hepatic Bax inhibitor-1 inhibits IRE1alpha and protects from obesity-associated insulin resistance and glucose intolerance. J Biol Chem 285(9):6198–6207
Bernales S, McDonald KL, Walter P (2006) Autophagy counterbalances endoplasmic reticulum expansion during the unfolded protein response. PLoS Biol 4(12):e423
Bincoletto C, Saad STO, Soares de Silva E, Queiroz MLS (1999) Haematopoietic response and bcl-2 expression in patients with acute myeloid leukaemia. Eur J Haematol 62:38–42
Boatright KM, Salvesen GS (2003) Mechanisms of caspase activation. Curr Opin Cell Biol 15:725–731
Bouillet P, Strasser A (2002) BH3-only proteins—evolutionarily conserved proapoptotic Bcl-2 family members essential for initiating programmed cell death. J Cell Sci 115(Pt 8):1567–1574
Bradbury D, Zhu Y-M, Russell N (1994) Regulation of Bcl-2 expression and apoptosis in acute myeloblastic leukemia cells by granulocyte-macrophage colony-stimulating factor. Leukemia 8:786–791
Brimmell M, Mendiola R, Mangion J, Packham G (1998) Bax frameshift mutations in cell lines derived from human haemopoietic malignacies are associated with resistance to apoptosis and microsatellite instability. Oncogene 16:1803–1812
Campos L, Roualult J-P, Sabido O, Roubi N, Vasselon C, Archimbaud E et al (1993) High expression of Bcl-2 protein in acute myeloid leukemia cells is associated with poor response to chemotherapy. Blood 81:3091–3096
Campos L, Oriol P, Sabido O, Guyotat D (1997) Simultaneous expression of P-glycoprotein and bcl-2 in acute. Leuk Lymphoma 27(1–2):119–125
Cardenas C, Miller RA, Smith I, Bui T, Molgo J, Muller M et al (2010) Essential regulation of cell bioenergetics by constitutive InsP3 receptor Ca2+ transfer to mitochondria. Cell 142(2):270–283
Cassidy-Stone A, Chipuk JE, Ingerman E, Song C, Yoo C, Kuwana T et al (2008) Chemical inhibition of the mitochondrial division dynamin reveals its role in Bax/Bak-dependent mitochondrial outer membrane permeabilization. Dev Cell 14(2):193–204
Chae HJ, Kim HR, Xu C, Bailly-Maitre B, Krajewska M, Krajewski S et al (2004) BI-1 regulates an apoptosis pathway linked to endoplasmic reticulum stress. Mol Cell 15(3):355–356
Chen M, He H, Zhan S, Krajewski S, Reed JC, Gottlieb RA (2001) Bid is cleaved by calpain to an active fragment in vitro and during myocardial ischemia/ reperfusion. J Biol Chem 276:30724–30728
Chen YB, Aon MA, Hsu YT, Soane L, Teng X, McCaffery JM et al (2011) Bcl-xL regulates mitochondrial energetics by stabilizing the inner membrane potential. J Cell Biol 195(2):263–276
Cheng EH, Sheiko TV, Fisher JK, Craigen WJ, Korsmeyer SJ (2003) VDAC2 inhibits BAK activation and mitochondrial apoptosis. Science 301:513–517
Chipuk JE, Green DR (2008) How do BCL-2 proteins induce mitochondrial outer membrane permeabilization? Trends Cell Biol 18(4):157–164
Chipuk JE, Moldoveanu T, Llambi F, Parsons MJ, Green DR (2010) The BCL-2 family reunion. Mol Cell 37(3):299–310
Chipuk J, McStay G, Bharti A, Kuwana T, Clarke C, Siskind L et al (2012) Sphingolipid metabolism cooperates with BAK and BAX to promote the mitochondrial pathway of apoptosis. Cell 148(5):845–848
Criollo A, Maiuri MC, Tasdemir E, Vitale I, Fiebig AA, Andrews D et al (2007) Regulation of autophagy by the inositol trisphosphate receptor. Cell Death Differ 14(5):1029–1039
Delia D, Aiello A, Formelli F, Fontanella E, Costa A, Miyashita T et al (1995) Regulation of apoptosis induced by N-(4-hydroxyphenyl) retinamide and effect of Bcl-2. Blood 85:359–367
Demaurex N, Distelhorst C (2003) Apoptosis—the calcium connection. Science 300(5616):65–67
Deng GL ane C, Kornblau S, Goodacre A, Snell V, Andreeff M et al (1998) Ratio of bcl-xshort to bcl-xlong is different in good- and poor-prognosis subsets of acute myeloid leukemia. Mol Med 4(3):158–164
Deveraux QL, Reed JC (1999) IAP family proteins: suppressors of apoptosis. Genes Dev 13:239–252
Deveraux QL, Leo E, Stennicke HR, Welsh K, Salvesen GS, Reed JC (1999) Cleavage of human inhibitor of apoptosis protein XIAP results in fragments with distinct specificities for caspases. EMBO J 18:5242–5251
Deverman BE, Cook BL, Manson SR, Niederhoff RA, Langer EM, Rosova I et al (2002) Bcl-xL deamidation is a critical switch in the regulation of the response to DNA damage. Cell 111:51–62
Dipietrantonio A, Hsieh T-C, Wu JM (1996) Differential effects of retinoic acid (RA) and N –(4-hydroxyphenyl)retinamide (4-HPR) on cell growth, induction of differentiation, and changes in p34cdc2, bcl-2, and actin expression in the human promyelocytic hl-60 leukemic cells. Biochem Biophys Res Commun 224:837–842
Domina AM, Vrana JA, Gregory MA, Hann SR, Craig RW (2004) MCL1 is phosphorylated in the PEST region and stabilized upon ERK activation in viable cells, and at additional sites with cytotoxic okadaic acid or taxol. Oncogene 23(31):5301–5315
Dong D, Ko B, Baumeister P, Swenson S, Costa F, Markland F et al (2005) Vascular targeting and antiangiogenesis agents induce drug resistance effector GRP78 within the tumor microenvironment. Cancer Res 65(13):5785–5791
Droga-Mazovec G, Bojic L, Petelin A, Ivanova S, Romih R, Repnik U et al (2008) Cysteine cathepsins trigger caspase-dependent cell death through cleavage of bid and antiapoptotic Bcl-2 homologues. J Biol Chem 283(27):19140–19150
Elstner E, Linker-Israeli M, Umiel T, Le J, Grillier I, Said J et al (1996) Combination of a potent 20-epi-vitamin D3 analogue (KH 1060) with 9-cis-retinoic acid irreversibly inhibits clonal growth, decreases bcl-2 expression, and induces apoptosis in HL-60 leukemic cells. Cancer Res 56(15):3570–3576
Fan G, Simmons MJ, Ge S, Dutta-Simmons J, Kucharczak J, Ron Y et al (2010) Defective ubiquitin-mediated degradation of antiapoptotic Bfl-1 predisposes to lymphoma. Blood 115(17):3559–3569
Fernandez PM, Tabbara SO, Jacobs LK, Manning FC, Tsangaris TN, Schwartz AM et al (2000) Overexpression of the glucose-regulated stress gene GRP78 in malignant but not benign human breast lesions. Breast Cancer Res Treat 59(1):15–26
Fesik SW (2000) Insights into programmed cell death through structural biology. Cell 103:273–282
Fox JL, Ismail F, Azad A, Ternette N, Leverrier S, Edelmann MJ et al (2010) Tyrosine dephosphorylation is required for Bak activation in apoptosis. EMBO J 29(22):3853–3868
Gavathiotis E, Reyna DE, Davis ML, Bird GH, Walensky LD (2010) BH3-Triggered Structural Reorganization Drives the Activation of Proapoptotic BAX. Mol Cell 40(3):481–492
Gozuacik D, Bialik S, Raveh T, Mitou G, Shohat G, Sabanay H et al (2008) DAP-kinase is a mediator of endoplasmic reticulum stress-induced caspase activation and autophagic cell death. Cell Death Differ 15(12):1875–1886
He C, Bassik MC, Moresi V, Sun K, Wei Y, Zou Z et al (2012) Exercise-induced BCL2-regulated autophagy is required for muscle glucose homeostasis. Nature 481(7382):511–515
Hetz C, Bernasconi P, Fisher J, Lee AH, Bassik MC, Antonsson B et al (2006) Proapoptotic BAX and BAK modulate the unfolded protein response by a direct interaction with IRE1alpha. Science 312(5773):572–576
Holinger E, Chittenden T, Lutz R (1999) Bak BH3 Peptides antagonize Bcl-xL Function and induce apoptosis through cytochrome c-independent Activation of Caspases. J Biol Chem 274:13298–13304
Hoyer-Hansen M, Jaattela M (2007) Connecting endoplasmic reticulum stress to autophagy by unfolded protein response and calcium. Cell Death Differ 14(9):1576–1582
Hunsberger JG, Machado-Vieira R, Austin DR, Zarate C, Chuang DM, Chen G et al (2011) Bax inhibitor 1, a modulator of calcium homeostasis, confers affective resilience. Brain Res 1403:19–27
Jamora C, Dennert G, Lee AS (1996) Inhibition of tumor progression by suppression of stress protein GRP78/BiP induction in fibrosarcoma B/C10ME. Proc Natl Acad Sci U S A 93(15):7690–7694
Jurgensmeier JM, Xie Z, Deveraux Q, Ellerby L, Bredesen D, Reed JC (1998) Bax directly induces release of cytochrome c from isolated mitochondria. Proc Natl Acad Sci U S A 95:4997–5002
Kang MH, Reynolds CP (2009) Bcl-2 inhibitors: targeting mitochondrial apoptotic pathways in cancer therapy. Clin Cancer Res 15(4):1126–1132
Karakas T, Maurer U, Weidmann E, Miething C, Hoelzer D, Bergmann L (1998) High expression of bcl-2 mRNA as a determinant of poor prognosis in acute myeloid leukemia. Ann Oncol 9(2):159–165
Kasimirbauer S, Ottinger H, Meusers P, Beelen D, Brittinger G, Seeber S et al (1998) In acute myeloid leukemia, coexpression of at least two proteins, including P-glycoprotein, the multidrug resistance-related protien, bcl-2, mutant p53, and heat-shock protein 27, is predictive of the response to induction chemotherapy. Exp Hematol 26(12):1111–1117
Khwaja A (1999) Akt is more than just a bad kinase. Nature 401:33–34
Kim I, Xu W, Reed JC (2008) Cell death and endoplasmic reticulum stress: disease relevance and therapeutic opportunities. Nat Rev Drug Discov 7(12):1013–1030
Kim HR, Lee GH, Ha KC, Ahn T, Moon JY, Lee BJ et al (2008) Bax Inhibitor-1 Is a pH-dependent regulator of Ca2+ channel activity in the endoplasmic reticulum. J Biol Chem 283(23):15946–15955
Kitada S, Pedersen IM, Schimmer A, Reed JC (2002) Dysregulation of apoptosis genes in hematopeietic malignancies. Oncogene 21:3459–3474
Kiviluoto S, Schneider L, Luyten T, Vervliet T, Missiaen L, De Smedt H et al (2012) Bax Inhibitor-1 is a novel IP(3) receptor-interacting and -sensitizing protein. Cell Death Dis 3:e367
Konopleva M, Andreeff M (2002) Mechanisms in drug resistance in AML. In: Murray D, Andersson BS (eds) Clinically relevant resisitance in cancer chemotherapy, Kluwer Academic Publishers, Norwell, pp 237–262
Konopleva M, Tsao T, Ruvolo P, Stiouf I, Estrov Z, Leysath CE et al (2002) Novel triterpenoid CDDO-Me is a potent inducer of apoptosis and differentiation in acute myelogenous leukemia. Blood 99:326–335
Kornblau SM, Thall PF, Estrov Z, Walterscheid M, Patel S, Theriault A et al (1999) The prognostic impact of BCL2 protein expression in acute myelogenous leukemia varies with cytogenetics. Clin Cancer Res 5:1758–1766
Korsmeyer SJ, Wei MC, Saito M, Weiler S, Oh KJ, Schlesinger PH (2000) Pro-apoptotic cascade activates BID, which oligomerizes BAK or BAX into pores that result in the release of cytochrome c. Cell Death Differ 7:1166–1173
Kroemer G, Reed JC (2000) Mitochondrial control of cell death. Nat Med 6:513–519
Kroemer G, Marino G, Levine B (2010) Autophagy and the integrated stress response. Mol Cell 40(2):280–293
Kruse KB, Dear A, Kaltenbrun ER, Crum BE, George PM, Brennan SO et al (2006) Mutant fibrinogen cleared from the endoplasmic reticulum via endoplasmic reticulum-associated protein degradation and autophagy: an explanation for liver disease. Am J Pathol 168(4):1299–1308; quiz 1404–1295
Lam D, Kosta A, Luciani MF, Golstein P (2008) The Inositol 1,4,5-Trisphosphate receptor is required to signal autophagic cell death. Mol Biol Cell 19(2):691–700
Lauria F, Raspadori D, Rondelli D, Ventura M, Fiacchini M, Visani G et al (1997) High bcl-2 expression in acute myeloid leukemia cells correlates with CD34 positivity and complete remission rate. Leukemia 11(12):2075–2078
Lee AS (2007) GRP78 induction in cancer: therapeutic and prognostic implications. Cancer Res 67(8):3496–3499
Lee AH, Iwakoshi NN, Anderson KC, Glimcher LH (2003) Proteasome inhibitors disrupt the unfolded protein response in myeloma cells. Proc Natl Acad Sci U S A 100(17):9946–9951
Lee H, Rotolo JA, Mesicek J, Penate-Medina T, Rimner A, Liao WC et al (2011) Mitochondrial ceramide-rich macrodomains functionalize Bax upon irradiation. PLoS One 6(6):e19783
Lei K, Davis RJ (2003) JNK phosphorylation of Bim-related members of the Bcl2 family induces Bax-dependent apoptosis. Proc Natl Acad Sci U S A 100(5):2432–2437
Levine B, Yuan J (2005) Autophagy in cell death: an innocent convict? J Clin Invest 115(10):2679–2688
Li J, Lee AS (2006) Stress induction of GRP78/BiP and its role in cancer. Curr Mol Med 6(1):45–54
Li H, Kolluri SK, Gu J, Dawson MI, Cao X, Hobbs PD et al (2000) Cytochrome c release and apoptosis induced by mitochondrial targeting of nuclear orphan receptor TR3. Science 289:1159–1164
Li G, Mongillo M, Chin KT, Harding H, Ron D, Marks AR et al (2009) Role of ERO1-alpha-mediated stimulation of inositol 1,4,5-triphosphate receptor activity in endoplasmic reticulum stress-induced apoptosis. J Cell Biol 186(6):783–792
Lin B, Kolluri SK, Lin F, Liu W, Han Y-H, Cao X et al (2004) Conversion of Bcl-2 from protector to killer by interaction with nuclear orphan receptor TR3/NGFI-B/Nur Cell 116:527–540
Lisbona F, Rojas-Rivera D, Thielen P, Zamorano S, Todd D, Martinon F et al (2009) BAX inhibitor-1 is a negative regulator of the ER stress sensor IRE1alpha. Mol Cell 33(6):679–691
Lisovsky M, Extrov Z, Zhang X, Consoli U, Sanchez-Williams G, Snell V et al (1996) Flt3 ligand stimulates proliferation and inhibits apoptosis of acute myeloid leukemia cells: regulation of Bcl-2 and Bax. Blood 88(10):3987–3997
Ma Y, Hendershot LM (2004) The role of the unfolded protein response in tumour development: friend or foe? Nat Rev Cancer 4(12):966–977
Marciniak SJ, Yun CY, Oyadomari S, Novoa I, Zhang Y, Jungreis R et al (2004) CHOP induces death by promoting protein synthesis and oxidation in the stressed endoplasmic reticulum. Genes Dev 18(24):3066–3077
Maung ZT, MacLean FR, Reid MM, Pearson ADJ, Proctor SJ, Hamilton PJ et al (1994) The relationship between Bcl-2 expression and response to chemotherapy in acute leukemia. Br J Haematol 88:105–109
Maurer U, Charvet C, Wagman AS, Dejardin E, Green DR (2006) Glycogen synthase kinase-3 regulates mitochondrial outer membrane permeabilization and apoptosis by destabilization of MCL-1. Mol Cell 21:749–760
McCullough KD, Martindale JL, Klotz LO, Aw TY, Holbrook NJ (2001) Gadd153 sensitizes cells to endoplasmic reticulum stress by down-regulating Bcl2 and perturbing the cellular redox state. Mol Cell Biol 21(4):1249–1259
Meiijerink JPP, Smetsers TFCM, Slöetjes AW, Linders EHP, Mensink EJBM (1995) Bax mutations in cell lines derived from hematological malignancies. Leukemia 9:1828–1832
Meijerink JP, Mensink EJ, Wang K, Sedlak TW, Sloetjes AW, de Witte T et al (1998) Hematopoietic malignancies demonstrate loss-of-function mutations of BAX. Blood 91:2991–2997
Milella M, Estrov Z, Kornblau SM, Carter BZ, Konopleva M, Tari A et al (2002) Synergistic induction of apoptosis by simultaneous disruption of the Bcl-2 and MEK/MAPK pathways in acute myelogenous leukemia. Blood 99:3461–3464
Miyashita T, Reed JC (1995) Tumor suppressor p53 is a direct transcriptional activator of human Bax gene. Cell 80:293–299
Momoi T (2006) Conformational diseases and ER stress-mediated cell death: apoptotic cell death and autophagic cell death. Curr Mol Med 6(1):111–118
Mullican S, Zhang S, Konopleva M, Ruvolo V, Andreeff M, Milbrandt J et al (2007) Abrogation of nuclear receptors Nr4a3 and Nr4a1 leads to development of acute myeloid leukemia. Nat Med 13(6):730–735
Nishitoh H, Matsuzawa A, Tobiume K, Saegusa K, Takeda K, Inoue K et al (2002) ASK1 is essential for endoplasmic reticulum stress-induced neuronal cell death triggered by expanded polyglutamine repeats. Genes Dev 16(11):1345–1355
Oakes SA, Scorrano L, Opferman JT, Bassik MC, Nishino M, Pozzan T et al (2005) Proapoptotic BAX and BAK regulate the type 1 inositol trisphosphate receptor and calcium leak from the endoplasmic reticulum. Proc Natl Acad Sci U S A 102:105–110
Ogata M, Hino S, Saito A, Morikawa K, Kondo S, Kanemoto S et al (2006) Autophagy is activated for cell survival after endoplasmic reticulum stress. Mol Cell Biol 26(24):9220–9231
Ozcan L, Tabas I (2012) Role of endoplasmic reticulum stress in metabolic disease and other disorders. Annu Rev Med 63:317–328
Pattingre S, Tassa A, Qu X, Garuti R, Liang XH, Mizushima N et al (2005) Bcl-2 antiapoptotic proteins inhibit beclin 1-dependent autophagy. Cell 122:927–939
Pellecchia M, Reed JC (2004) Inhibition of anti-apoptotic Bcl-2 family proteins by natural polyphenols: new avenues for cancer chemoprevention and chemotherapy. Curr Pharm Des 10:1387–1398
Penninger JM, Kroemer G (2003) Mitochondria, AIF and caspases–rivaling for cell death execution. Nat Cell Biol 5:97–99
Putcha GV, Le S, Frank S, Besirli CG, Clark K, Chu B et al (2003) JNK-mediated BIM phosphorylation potentiates BAX-dependent apoptosis. Neuron 38(6):899–914
Puthalakath H, O’Reilly L, Gunn P, Lee L, Kelly P, Huntington N et al (2007) ER stress triggers apoptosis by activating BH3-only protein bim. Cell 129:1337–1349
Qian S, Wang W, Yang L, Huang HW (2008) Structure of transmembrane pore induced by Bax-derived peptide: evidence for lipidic pores. Proc Natl Acad Sci U S A 105(45):17379–17383
Rao RV, Bredesen DE (2004) Misfolded proteins, endoplasmic reticulum stress and neurodegeneration. Curr Opin Cell Biol 16:653–662
Reed JC (1996) Balancing cell life and death: bax, apoptosis, and breast cancer. J Clin Invest 97: 2403–2404
Reed JC (1997) Double identity for proteins of the Bcl-2 family. Nature 387:773–776
Reed JC (2005) Pellecchia M. apoptosis-based therapies for hematological malignancies. Blood 106:408–418
Reed JC (2006) Proapoptotic multidomain Bcl-2/Bax-family proteins: mechanisms, physiological roles, and therapeutic opportunities. Cell Death Differ 13(8):1378–1386
Reed JC (2008) Bcl-2-family proteins and hematologic malignancies: history and future prospects. Blood 111(7):3322–3330
Reed JC, Doctor KS, Godzik A (2004) The domains of apoptosis: a genomics perspective. Science STKE 239:RE9
Reimers K, Choi CY, Bucan V, Vogt PM (2008) The Bax Inhibitor-1 (BI-1) Family in Apoptosis and Tumorigenesis. Curr Mol Med 8(2):148–156
Rochitz C, Lohri A, Bacchi M, Schmidt M, Nagel S, Fopp M et al (1999) Axl expression is associated with adverse prognosis and with expression of Bcl-2 and CD34 in de novo acute myeloid leukemia (AML): results from a multicenter trial of the swiss group for clinical cancer research. Leukemia 13(9):1352–1358
Romero-Ramirez L, Cao H, Nelson D, Hammond E, Lee AH, Yoshida H et al (2004) XBP1 is essential for survival under hypoxic conditions and is required for tumor growth. Cancer Res 64(17):5943–5947
Rong YP, Aromolaran AS, Bultynck G, Zhong F, Li X, McColl K et al (2008) Targeting Bcl-2-IP3 Receptor Interaction to Reverse Bcl-2’s Inhibition of Apoptotic Calcium Signals. Mol Cell 31(2):255–265
Sakaki K, Wu J, Kaufman RJ (2008) Protein Kinase C{theta} is required for autophagy in response to stress in the endoplasmic reticulum. J Biol Chem 283(22):15370–15380
Saleh M, Vaillancourt JP, Graham RK, Huyck M, Srinivasula SM, Alnemri ES et al (2004) Differential modulation of endotoxin responsiveness by human caspase-12 polymorphisms. Nature 429:75–79
Salvesen GS (2002) Caspases: opening the boxes and interpreting the arrows. Cell Death Differ 9:3–5
Salvesen GS, Duckett CS (2002) IAP proteins: blocking the road to death’s door. Nat Rev Mol Cell Biol 3:401–410
Salvesen GS, Renatus M (2002) Apoptosome: the seven-spoked death machine. Develop Cell 2:256–257
Sano R, Hou Y-CC, Hedvat M, Correa RG, Shu CW, Krajewska M et al (2012) Endoplasmic Reticulum Protein BI-1 regulates Ca2+ -mediated bioenergetics to promote autophagy Genes Dev 26(10):1041–1054
Schaich M, Illmer T, Seitz G, Mohr B, Schakel U, Beck JF et al (2001) The prognostic value of Bcl-XL gene expression for remission induction is influenced by cytogenetics in adult acute myeloid leukemia. Haematologica 86:470–477
Shimizu S, Narita M, Tsujimoto Y (1999) Bcl-2 family proteins regulate the release of apoptogenic cytochrome c by the mitochondrial channel VDAC. Nature 399:483–487
Shuda M, Kondoh N, Imazeki N, Tanaka K, Okada T, Mori K et al (2003) Activation of the ATF6, XBP1 and grp78 genes in human hepatocellular carcinoma: a possible involvement of the ER stress pathway in hepatocarcinogenesis. J Hepatol 38(5):605–614
Srivastava RK, Srivastava AR, Korsmeyer SJ, Nesterova M, Cho-Chung YS, Longo D (1998) Involvement of microtubules in the regulation of Bcl-2 phosphorylation and apoptosis through cyclic AMP-dependent protein kinase. Mol Cell Biol 18:3509–3517
Stoka V, Turk B, Schendel SL, Kim TH, Cirman T, Snipas SJ et al (2001) Lysosomal protease pathways to apoptosis. Cleavage of bid, not pro-caspases, is the most likely route. J Biol Chem 276(5):3149–3157
Tschopp J, Irmler M, Thome M (1998) Inhibition of Fas death signals by FLIPs. Curr Opin Immunol 10:552–558
Upton JP, Austgen K, Nishino M, Coakley KM, Hagen A, Han D et al (2008) Caspase-2 cleavage of BID is a critical apoptotic signal downstream of endoplasmic reticulum stress. Mol Cell Biol 28(12):3943–3951
Vicencio JM, Ortiz C, Criollo A, Jones AW, Kepp O, Galluzzi L et al (2009) The inositol 1,4,5-trisphosphate receptor regulates autophagy through its interaction with Beclin 1. Cell Death Differ 16(7):1006–1017
Vogler M, Dinsdale D, Dyer MJ, Cohen GM (2009) Bcl-2 inhibitors: small molecules with a big impact on cancer therapy. Cell Death Differ 16(3):360–367
Wallach D, Varfolomeev EE, Malinin NL, Goltsev YV, Kovalenko AV, Boldin MP (1999) Tumor necrosis factor receptor and Fas signaling mechanisms. Ann Rev Immunol 17:331–367
Wang XZ, Ron D (1996) Stress-induced phosphorylation and activation of the transcription factor CHOP (GADD153) by p38 MAP Kinase. Science 272:1347–1349
Wei Y, Sinha S, Levine B (2008) Dual role of JNK1-mediated phosphorylation of Bcl-2 in autophagy and apoptosis regulation. Autophagy 4(7):949–951
Xu Q, Reed JC (1998) BAX inhibitor-1, a mammalian apoptosis suppressor identified by functional screening in yeast. Mol Cell 1:337–346
Xu C, Bailly-Maitre B, Reed JC (2005) Endoplamic reticulum stress: cell life and death decisions. J Clin Invest 115:2656–2664
Xu C, Xu W, Palmer AE, Reed JC (2008) BI-1 regulates endoplasmic reticulum Ca2 + homeostasis downstream of Bcl-2 family proteins. J Biol Chem 283(17):11477–11484
Yamaguchi R, Lartigue L, Perkins G, Scott RT, Dixit A, Kushnareva Y et al (2008) Opa1-mediated cristae opening is Bax/Bak and BH3 dependent, required for apoptosis, and independent of Bak oligomerization. Mol Cell 31(4):557–569
Yorimitsu T, Nair U, Yang Z, Klionsky DJ (2006) Endoplasmic reticulum stress triggers autophagy. J Biol Chem 281(40):30299–30304
Zalckvar E, Berissi H, Eisenstein M, Kimchi A (2009) Phosphorylation of Beclin 1 by DAP-kinase promotes autophagy by weakening its interactions with Bcl-2 and Bcl-XL. Autophagy 5(5):720–722
Zhao R, Follows GA, Beer PA, Scott LM, Huntly BJ, Green AR et al (2008) Inhibition of the Bcl-xL deamidation pathway in myeloproliferative disorders. N Engl J Med 359(26):2778–2789
Zhong Q, Gao W, Du F, Wang X (2005) Mule/ARF-BP1, a BH3-only E3 ubiquitin ligase, catalyzes the polyubiquitination of Mcl-1 and regulates apoptosis. Cell 121:1085–1095
Zou W, Yue P, Khuri FR, Sun SY (2008) Coupling of endoplasmic reticulum stress to CDDO-Me-induced up-regulation of death receptor 5 via a CHOP-dependent mechanism involving JNK activation. Cancer Res 68(18):7484–7492
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Conclusions
Conclusions
Bcl-2 family proteins are intricately involved in the biology of AML. From pathogenesis to progression and resistance to therapy, Bcl-2 family proteins are inextricably linked to AML. The advent of experimental therapeutics targeting anti-apoptotic Bcl-2 family proteins (small molecules) and mRNA (antisense) creates hope that are more effective strategies for treating AML may be near.
Rights and permissions
Copyright information
© 2015 Springer-Verlag New York
About this chapter
Cite this chapter
Reed, J. (2015). Roles of Apoptosis-Regulating Bcl-2 Family Genes in AML. In: Andreeff, M. (eds) Targeted Therapy of Acute Myeloid Leukemia. Current Cancer Research. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-1393-0_3
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1393-0_3
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-1392-3
Online ISBN: 978-1-4939-1393-0
eBook Packages: MedicineMedicine (R0)