Abstract
Mental health disorders, which are among the most prevalent chronic diseases affecting reproductive-aged women worldwide, can have adverse reproductive health consequences, including increased risk of unintended pregnancy. Contraception can play an important role in the health and well-being of women with depression, anxiety, and other serious mental illness. In this chapter, we describe contraceptive considerations for women with mental health conditions. We emphasize the most common mental health conditions, including depression and anxiety (Part I), but also discuss other serious mental illnesses (Part II). We address the potential effects of contraception on mental health and vice versa, contraceptive method effectiveness and adherence concerns, mental health-specific contraceptive method safety and drug considerations, clinically relevant counseling and management strategies, and ethical issues for reproductive autonomy and contraceptive decision-making for women with mental health conditions. Throughout, we note important gaps in scientific knowledge and areas for future research on mental health and contraception. Our goal is to offer a reference for health providers who care for women with mental health conditions wishing to avoid an unintended pregnancy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Intimate Partner Violence
- Mental Health Condition
- Contraceptive Method
- Unintended Pregnancy
- Mental Health Disorder
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Part I: Contraception and Common Mental Health Conditions
Scope of Common Mental Health Conditions Among Reproductive-Aged Women
Depressive and anxiety disorders are among the leading causes of disability in the USA and worldwide [1–8]. In the USA, women are 55 % more likely to experience a depressive disorder during their lifetime compared to men [8]. Approximately 20 % of women ages 18 years and older will experience a depressive disorder in their lifetime; 8.6 % will experience one each year [8]. Anxiety disorders are also common, with lifetime and 12-month prevalence rates estimated at 36 % and 23 %, respectively [8]. Depression and anxiety are frequently comorbid with one another and with other mental health disorders, including substance abuse and eating disorders. US nationally representative data show that of people with a depressive disorder in the past year, approximately 60 % also had an anxiety disorder and nearly 9 % had a substance use disorder [9]. Prevalence rates of depressive and anxiety disorders among new generations of adolescent and young women appear to be increasing in recent years [10–12].
Despite a clear need for women’s mental health care, mental health service utilization in the USA is low [13, 14]. Depression and anxiety disorders often go undetected and untreated among reproductive-aged women [15–21]. Sixty-three percent of adults who have depression do not talk to a professional in the first year of having the disorder [22]. In recent years, less than half of pregnant and nonpregnant US women with a major depressive episode received a mental health diagnosis or treatment [17, 19, 21]. A population-based study of over 70,000 nonpregnant women found that half of women meeting criteria for depression did not receive a diagnosis or treatment, even though more than 70 % had contact with a health provider in the last year [17]. Black and Hispanic women are even less likely to receive a mental health diagnosis and treatment than White women [17, 23, 24]. These same groups of women disproportionately experience high unintended pregnancy rates [25].
Certain social circumstances such as poverty, unemployment, and having less education are associated with experiencing common mental health conditions [10, 26–28]. Other risk factors for depression and anxiety include having a personal or family history of a mental health disorder, having other chronic medical illnesses such as cancer, stroke, or HIV/AIDs, and having adverse life experiences, including physical and sexual violence or trauma [1–4]. Some of these same characteristics, such as having less education or experiencing physical and sexual violence, also increase women’s risk of contraceptive non- or misuse [29–31], suggesting similar groups of women are vulnerable to mental health disorders and unintended pregnancy. In the pages that follow, we discuss more direct evidence that connects mental health disorders, contraception, and unintended pregnancy.
Relationships Between Reproductive Health and Depression and Anxiety
Research has examined the interplay between depressive or anxiety disorders and reproductive health [32–49]. Some studies have found depression and anxiety are precursors to a variety of negative reproductive outcomes, including maternal and infant morbidity, obstetrical complications, preterm labor, stillbirth, and low birth weight [32, 34, 35]. In addition, women with depression and anxiety appear to be at greater risk of experiencing an unintended pregnancy, and those pregnancies may be more likely to end in induced abortion, compared to women without depression and anxiety [38–40, 42, 43]. Depression and anxiety before pregnancy also consistently predict depression and anxiety after pregnancy [41, 42, 44, 45]. On the other hand, studies have also found that reproductive health influences subsequent mental health outcomes. For instance, women who carry their unintended pregnancies to term are at risk for antepartum and postpartum depression [44–50]. Some groups of women, including poor, underinsured, undereducated, and minority women, disproportionately experience adverse mental and reproductive health outcomes due to common risk factors, including limited health knowledge, access to medical resources, and social support [10–12, 17, 23, 25–28, 44, 48, 50, 51].
Effects of Contraception on Mental Health
While the causes of depression and anxiety are not fully understood, deficiencies in neurotransmitters (serotonin, norepinephrine, dopamine, GABA, and peptides) that impact mood have been implicated in clinical studies of depression and anxiety [1–4]. Genetic predisposition and psychosocial stressors appear to be important precursors to neurotransmitter deficiencies and contribute to these disorders [4]. Soon after the combined oral contraceptive pill (COC) was made available in 1960, researchers hypothesized that synthetic estrogens and progestins in COCs could potentially interact with mood-related neurotransmitters [52–55]. Articles published in the 1970s and 1980s suggested that the large steroid dosages in COCs (e.g., Enovid: 5 mg norethynodrel, 75 mcg mestranol) could interfere with serotonin, noradrenaline, tryptophan (an amino acid precursor to serotonin), and vitamin and endocrine metabolism [52–55]. Estrogen was thought to reduce noradrenaline and serotonin in the hypothalamus, resulting in pyridoxine deficiency [52, 53, 55]; progestins were thought to cause cerebral monoamine oxidase activity, triggering enzymatic breakdown of neurotransmitters [54].
However, given the significantly lower steroid dosages in modern hormonal contraceptives, these mechanistic theories appear to no longer be relevant. While few (if any) recent clinical trials have used brain imaging and hormonal bioassays to clarify these relationships, a notable newer body of scientific evidence suggests that the steroidal activity of modern methods does not have a clinically relevant physiological impact on women’s mood or mood-related neuroendocrine functioning [56–73]. In a comprehensive review, Robinson et al. analyzed seven studies examining COC pharmacological properties and mood-related side effects [56]. The researchers found no evidence for an association between the intrinsic biochemical mechanisms of COCs and mood effects reported by COC users. In the Medical Eligibility Criteria for Contraceptive Use report published in 2010, the US Centers for Disease Control and Prevention concluded there are no contraindications to hormonal contraception for women with depression, basing their recommendation on evidence that does not support a causal relationship [57]. Prospective clinical placebo-controlled and population-based cohort studies have reported similar or even lower rates of depression or mood symptoms between women who use COCs and those who do not [58–65]. The best scientific evidence to date suggests that modern COC formulations do not cause depression or mood symptoms among the women that use them, and in fact, COCs may improve depression and mood symptoms for some women.
Clinical research studies have examined whether mental health symptoms increase among women initiating other hormonal contraceptive methods, including the depot medroxyprogesterone acetate (DMPA) contraceptive injectable (e.g., Depo-Provera, Pfizer Inc., New York NY, USA), transdermal patch (e.g., Ortho-Evra patch, Ortho-McNeil Pharmaceutical Inc., Raritan, NJ, USA), vaginal ring (e.g., NuvaRing, Merck, Whitehouse Station, NJ, USA), and long-acting reversible contraceptive methods (LARC) such as the subdermal implant (e.g., Implanon, Nexplanon), levonorgestrel-releasing intrauterine device (IUD, e.g., Mirena, Bayer Healthcare Pharmaceuticals, Wayne, NJ, USA), and copper-containing IUD (e.g., ParaGard, Teva, Israel) [56–73]. Collectively, these studies have found no adverse effects of these methods on depression, anxiety, or mood [56–73].
Effects of Mental Health on Contraceptive Use
Compared to the large literature investigating the mental health effects of contraception, less research has focused on the extent to which mental health influences contraceptive behaviors. Even though, as detailed above, the literature does not support a causal relationship between contraception and negative mental health outcomes, perceived mood symptoms continue to be a primary reason why women report not using, misusing, or discontinuing hormonal contraceptives [74–77]. COC discontinuation rates from perceived mood symptoms have ranged from 14 to 21 % [74–77]. Some research has suggested that women with depression, anxiety, and related stress symptoms are more likely to perceive negative mood symptoms than those without those symptoms [77]. Yet, how depression and anxiety may influence perceived contraceptive side effects and use has not been well studied. It may be that neuroendocrine pathology amplifies physical symptomatology attributed to COCs. However, this hypothesis has not been studied.
Alternatively, cognitive processes related to “perceptions” of physical symptoms, rather than pathophysiological processes themselves, may be altered in COC users with mental health conditions. A study by Rubino-Watkins et al. found that COC users with psychological stress had higher self-reported negative cognitive patterns and emotions over time than stressed OC nonusers, and greater negative affect was attributed to more daily stressors among OC users versus nonusers [78]. Other researchers have found that higher levels of somatization (recurrent and frequently changing physical symptoms which cannot be explained by any known medical condition) and hypochondriasis (excessive worry about illness and the belief that one has an undiagnosed physical disease) are associated with higher rates of reported side effects among those using both active and placebo medications [79, 80]. Because depressed individuals are attuned to negative cues in their environment [81, 82], depressed women may internalize negative information about hormonal contraceptives (e.g., side effects and risks), which could preclude initiation or continuation. With anxiety, excessive worry could potentially contribute to irrational concerns about contraceptive safety or side effects, leading to misuse and discontinuation, though this has not been examined.
Depression and anxiety may also affect cognitive and behavioral processes related to use of contraception, including risk assessment, planning, and social learning, as well as perceptions of benefits and threats of contraception and perceived susceptibility to pregnancy [83–87]. Decreased motivation and desire for self-care, which may accompany depression [88, 89], could impact women’s abilities to use certain methods, like daily COCs. Anxiety symptoms also have the potential to interfere with contraceptive decision-making processes [90], leading women to make suboptimal contraceptive choices.
To our knowledge, no research studies have investigated these hypotheses directly, but scientific evidence indirectly supports a link between mental health and family planning. Some recent studies have shown that women with elevated depressive, anxiety, and stress symptoms have higher rates of risky sexual behaviors (e.g., increased numbers of sexual partners, earlier sexual debut) and contraceptive nonuse, misuse, discontinuation, and use of less effective methods, compared to women without elevated mental health symptoms [18, 66, 73, 91–99]. These findings have been most widely noted for condoms and COCs but have also been demonstrated for the DMPA injectable, IUDs, and implants [66, 69, 73].
Some emerging research also suggests that depression and anxiety may affect contraceptive method selection and use differently depending upon the health setting or social context of the woman. Garbers et al. found that among 2,476 urban women presenting to a health department clinic, those who screened positive for depression had 45 % higher odds of selecting condoms (compared to more effective methods) and 39 % lower odds of selecting hormonal methods (compared to less effective methods) at their routine clinic visit compared to women without depressive symptoms [94]. Similar findings have been noted among clinical and population-based samples of nonpregnant women [18, 95–97]. On the other hand, a study of abortion patients initiating contraception immediately following their abortion found that those with higher mental distress symptoms before their abortion had increased odds of leaving their visit with more effective methods including IUDs and implants compared to women without distress [99]. While reasons for these differences in associations between mental health and contraceptive method selection are not fully clear and may be partially attributed to different measurement approaches, it is possible that women with depression who have already experienced an unintended pregnancy are motivated to avoid a subsequent pregnancy due to their mental health concerns and stressful life circumstances. Research is warranted to clarify the role of mental health in women’s contraceptive decision-making and behavior across different life circumstances and health care contexts.
Clinical Assessment: Mental Health and Contraception
Common mental health disorders frequently go undiagnosed among reproductive-aged women, and yet underlying symptoms and the disorders themselves can impact women’s perceived and actual family planning needs [17, 18, 21, 94–97, 99]. A lack of detection and diagnosis of depression and anxiety among women points to the potential role that depression and anxiety screening and management may play in reproductive health contexts. In obstetrical settings, health providers may see women with postpartum depression who need assistance choosing a contraceptive method that is effective in preventing rapid repeat pregnancy and also safe for breastfeeding. Women presenting for abortion care may need education on contraceptive methods that will effectively prevent another unintended pregnancy, in addition to counseling on strategies and resources to cope with their stressful life experience. Women presenting for sexually transmitted infection (STI) treatment require counseling on dual method use and safe sex and may also need an evaluation of mental distress related to the STI diagnosis. These are just a few examples of clinical encounters in which family planning and mental health issues may interact. Symptoms of depression and anxiety can take many different forms, and signs may not be obvious to the provider or patient [100–105]. The following discussion highlights aspects of the clinical encounter relevant to mental health and contraception.
First, depression and anxiety may impact patient-provider communication and interaction in important ways [100–105]. A careful review of the past medical history will identify any personal or family risk factors for new, recurring, or chronic mental health conditions. For undiagnosed conditions, disclosure of mental health symptoms may be difficult for patients due to perceived stigma, as well as women’s lack of awareness and insight into their own mental health status [100–105]. Health providers should routinely engage their patients in a discussion about overall health, including psychological well-being, and its impact on sexual and reproductive health. Employing patience, empathy, and a nonjudgmental tone can help patients feel more comfortable discussing their mental health issues [100–105]. Directive, confrontational questions should be avoided. Mental health concerns can be introduced with a simple educational statement such as, “Did you know that a fifth of women will experience depression in their lifetimes? Because depression is so common, I like to check in with all my patients about their own mental health.” This approach can alert patients to the provider’s concern but also normalize the experience. Reflective listening, use of open-ended questions, and careful patient observation can help providers pick up subtle cues of an underlying mental health condition [100–105]. A clinical presentation of a sad voice, anxious expressions, or lethargic posture would raise suspicions of a mental health issue. Providers should also reflect on their own feelings, emotions, and mood during and after the clinical encounter and be attuned to transference (i.e., feeling down, sad, or upset after seeing a patient with depression or anxiety) [100, 101]. Finally, women with diagnosed or undiagnosed mental health conditions commonly present with multiple, vague complaints, nonspecific symptoms or pain-related syndromes. In women’s health contexts, complaints may include nonspecific vulva, pelvic, vaginal, coital, or menstrual-related pain, headaches, or gastrointestinal disturbances [105]. Cues such as these should alert the provider to an underlying mental health condition requiring further evaluation.
Second, use of standardized mental health screening instruments may be an effective, efficient method to screen patients for common mental health conditions and identify those who may need follow-up psychiatric care [106–113]. Commonly used, evidence-based depression and anxiety screens are presented in Tables 5.1 and 5.2. In busy clinical settings, use of an abbreviated tool, such as the Patient Health Questionnaire (PHQ), is ideal. Such screening instruments can be seamlessly included in electronic medical record charting and should be used routinely and systematically, for instance with all well-woman exams or new patients.
Third, clinical diagnosis of a mental health disorder is ideally made by a trained mental health care professional, such as a psychiatrist or clinical psychologist [4, 100–104, 106]. However, when standardized diagnostic criteria are followed, common mental health disorders like depression and anxiety may be diagnosed in non-specialty health care settings including family practice and reproductive health. While a structured psychiatric interview, such as the Composite International Diagnostic Interview or the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders (DSM), is the gold standard [4, 10–104, 106, 121], use of self-report instruments may be more feasible in settings where large volumes of patients are seen and time per patient is limited.
Differential diagnoses of reproductive-aged women presenting with new onset mental health symptoms should be evaluated [100, 102–105]. Chronic diseases such as hypothyroidism, diabetes mellitus, anemia, cancer, and multiple sclerosis, which are not uncommon among reproductive-aged women, can cause mood-related symptoms that may mimic depression or anxiety [100, 102–105]. Women with acute stress or grief may exhibit transient or chronic mood symptoms, as well as reproductive symptoms like irregular menses. Women with anorexia nervosa or bulimia nervosa may similarly experience co-occurring depression or anxiety and amenorrhea or irregular menses. Finally, medications such as beta blockers or calcium channel blockers, glucocorticoids, and GnRH analogues (e.g., Lupron) can cause mood changes [100, 102–105]. Therefore, reproductive health providers should be able to screen for depression and anxiety, differentiate subclinical symptomatology from a diagnosable disorder, rule out differential diagnoses, and provide or refer for further mental health evaluation and treatment when indicated.
Contraceptive Management for Women with Common Mental Health Conditions
Eligibility and Drug Interaction Considerations
Women with depression and anxiety are generally good candidates for all contraceptive methods. In most cases, contraceptive method selection should not be limited by the mental health diagnosis or treatment but rather should occur through shared decision-making between patient and provider based upon individual health circumstances, contraceptive preferences, and family planning needs. The CDC Medical Eligibility Criteria for Contraceptive Use lists depression as Category 1 for eligibility, stating that there are no restrictions for use of hormonal contraception for women with depression and related disorders [57]. Drug interactions between modern pharmacologic antidepressant agents and hormonal contraception are relatively rare. The most widely used antidepressants include selective serotonin reuptake inhibitors (SSRIs, such as fluoxetine, citalopram, escitalopram, and sertraline) and more recently serotonin norepinephrine reuptake inhibitors (SNRIs, such as venlafaxine and duloxetine) [100, 102–105]. The best available scientific evidence suggests SSRIs and SNRIs do not interact with hepatic metabolism of synthetic steroids in COCs [122–125]. Women on SSRIs and SNRIs should be offered the full range of contraceptive methods.
Older generation antidepressant agents such as tricyclics (TCAs, such as amitriptyline or nortriptyline) and monoamine oxidase inhibitors (MAOIs, such as phenelzine and tranylcypromine), which are still used in treatment-refractive chronic depression, are highly interactive with other foods and drugs [100–105]. TCAs and MAOIs may interact with contraceptive steroid metabolism in the liver, potentially leading to decreased contraceptive efficacy; reduced hepatic metabolism can also lead to antidepressant side effects or toxicity [125]. In addition, while the scientific evidence is inconsistent, St. John’s wort (hypericum perforatum), an alternative over-the-counter antidepressant therapy, may also induce the cytochrome P450 system and subsequently reduce contraceptive steroid availability, by 13–15 % one study found [126, 127]. Thus, women who require more intensive psychiatric treatment with TCAs, MAOIs, or those using St. John’s wort are not ideal candidates for COCs or other systemic hormonal contraceptives. Other locally acting hormonal contraceptive methods, such as the levonorgestrel-releasing IUD, as well as nonhormonal methods like the copper-containing IUD, appear to be safe for women on TCAs, MAOIs, and St. John’s wort [128] (see Chap. 20 for more details).
Many women with depression and anxiety are treated with non-pharmacologic therapies including cognitive behavioral therapy, interpersonal psychotherapy, and adjunct therapies like exercise, sleep, and healthy diet [100–105, 129–131]. These treatments should not interfere with contraception or preclude use of any methods. Providers can encourage women to participate in these treatment modalities since the principles and self-care techniques learned (e.g., problem-solving and coping skills) may also benefit women’s reproductive health decision-making and behaviors.
Contraceptive Method Considerations
We present an overview of contraceptive method options and considerations for women with specific mental health issues in Table 5.3. In most cases, the full range of contraceptive methods is safe and suitable for women with depression and anxiety. Potential contraceptive adherence issues, however, may be an important factor for selection of the most appropriate method [132–138]. As mentioned earlier, women with depression and anxiety have more perceived contraceptive side effects and may misuse and discontinue methods at higher rates than women without these mental health conditions, with the greatest body of evidence available for user-dependent methods including condoms and COCs [18, 66, 73, 93–99]. Women with depression or anxiety may find it difficult to remember or find the energy to take a COC every day or may be too distracted, worried, or emotional to encourage their partner to apply a condom at every intercourse. LARC methods, including IUDs and the subdermal implant, require little user burden, have less worry and hassle, and offer the greatest contraceptive efficacy, making them ideal options for women with mental health conditions who wish to avoid an unintended pregnancy [128, 135, 136]. These “fit and forget” methods are also cost effective, which may be beneficial to women who have long-term financial concerns. On the other hand, not all women prefer long-acting methods. Women with depression or anxiety may prefer to be in regular control of using their method or may worry about menstrual irregularity. In this case, the vaginal ring, transdermal patch, or COCs are alternative options.
For providers who are initiating COCs or managing women with mental health conditions who have difficulty finding a satisfactory COC, several considerations may be useful. First, research has suggested that women’s experiences with perceived side effects are similar across different types of COCs [139], even though more than 90 different formulations are used by women in the USA alone [128, 136, 137, 140]. Thus, health providers can counsel their patients that most women do well with any COC. Second, a dose–response relationship with COCs and side effects was noted in the 1970s and 1980s, when contraceptive steroid dosages were significantly higher [128]. While modern formulations generally have low steroid dosages, providers may choose formulations with lower dosages (i.e., 20 mcg versus >20 mcg) in an attempt to minimize their patients’ risk of mood side effects [141]. On the other hand, lower dosage COCs are associated with other side effects like irregular bleeding, as well as vulnerable efficacy levels with missed pills [128, 141]. Providers should help women balance concerns about side effects and adherence. Second, in regard to the type of progestin, second-generation levonorgestrel- and norgestrel-containing COCs are the most widely used and are not known to contribute to mental health symptoms [140, 142, 143]. Newer fourth-generation drospirenone-containing COCs (e.g., Yaz, 3 mg drospirenone and 20 mcg ethinyl estradiol) are approved by the Food and Drug Administration (FDA) for treatment of mood symptoms occurring with premenstrual dysphoric disorder (PMDD) and may also be an option for women with depression and anxiety disorders [128]. Third, women’s experiences with mood symptoms can be worse during certain periods of the menstrual cycle, for instance during ovulation or menses, due to variable circulating estrogen levels. Theoretically, monophasic formulations, which offer a steady dose (versus multiphasic formulations), could better stabilize hormone levels to minimize the risk of mood symptoms [144]. Women who report mood symptoms during their placebo weeks (i.e., estrogen withdrawal) may benefit from COCs with extended cycle regimens (e.g., 24/4) or continuous dosing (i.e., skipping inactive pills), which would reduce or eliminate the estrogen withdrawal period [128, 145]. While a dearth of scientific evidence exists to support these strategies, they may be clinically useful for COC management of women with mood concerns.
Additional contraceptive method considerations may be specific to the mental health disorder itself. For instance, postpartum and perimenopausal depression, which affect approximately 10–20 % of women, have similar diagnostic criteria to major depressive disorder except onset occurs following pregnancy or during perimenopause, respectively [4, 45–48]. Explicit conversations about contraception are needed during these periods since postpartum and perimenopausal women may not be aware of their risks for unintended pregnancy. Mental health treatment options for postpartum depression (psychotherapy and SSRIs are the first lines of defense) should not interfere with modern contraceptive methods [33–39]. Postpartum women who are breastfeeding generally should not be initiated on estrogen-containing contraceptives due to possible reduction in breast milk production and VTE risk, and progestin-only methods including the levonorgestrel-releasing IUD, subdermal implant, DMPA injectable, or progestin-only pills can be used instead [57, 128]. Perimenopausal women may be ideal candidates for COCs, the patch, or ring, which can help stabilize hormonal fluctuations and control mood, menstrual, and hot flash symptoms while also preventing pregnancy [146–152]. Perimenopausal women should be evaluated for cardiovascular risks, tobacco use, and other contraindications to estrogen use prior to initiation and throughout treatment [57].
Education and Counseling
Education and counseling is a critical component of contraceptive initiation and management for women with mental health conditions [105, 125]. The scope of counseling needs among women with depression and anxiety may be broad and counseling should ultimately be tailored to individual patient’s specific needs and circumstances. Several key education and counseling considerations may be universally applicable: (1) accurate contraceptive information emphasizing method effectiveness, (2) mental health assessment, and (3) ongoing discussions about intimate partner violence.
Research has shown that women’s knowledge of contraception, including use, effectiveness, benefits, risks, and side effects of different contraceptive methods, is consistently low [153–160]. Women with mental health conditions may benefit from repeated and specific information on user-related method effectiveness rates. If a patient presenting for contraceptive initiation understands that her likelihood of becoming pregnant depends upon her ability to remember to take her pill every day and she is motivated to initiate or switch methods, then she may be more inclined to choose a highly effective method like an IUD that does not require daily diligence. Providers should encourage and support depressed women in taking action to select the most appropriate contraceptive method. Providers should also assess for and counsel on concurrent treatment adherence issues among patients who are taking antidepressants and contraception [133, 134]. If a patient reports that she is missing dosages or has stopped taking her antidepressant, this may alert the provider to contraceptive misuse or discontinuation. Counseling should focus on ways to improve accuracy and consistency of medication use in the context of her daily life, such as setting a cell phone reminder or taking pills when she brushes her teeth before bedtime [128]. Contraceptive counseling should also dispel myths and misperceptions of side effects and reinforce the benefits of modern methods for pregnancy prevention and non-contraceptive effects (e.g., improved mood and acne, protection from ovarian and uterine cancer) [154, 160]. Finally, women with depression and anxiety should be counseled on sexual risk behaviors and condom use given an increased risk for sexually transmitted infections [89–93].
Women who present for contraception with underlying mental health conditions (newly detected or previously diagnosed) may benefit from education on the prevalence, signs, and symptoms, and treatment options for depression, anxiety, and related disorders [105, 147, 149]. Helping a patient to understand that her mental health is as important as her reproductive health and that the two are interrelated may facilitate honesty, trust, and communication. Evidence-based counseling techniques like motivational interviewing can be used to focus attention on specific behaviors that may need to change (e.g., frequent missed pills, condom nonuse), to evoke motivation for change by increasing confidence and readiness, and to plan practical steps to improve contraceptive behaviors [105, 147, 149, 155]. Providers should also assess for other dimensions of patients’ lives that impact their mental and reproductive health, for example, financial considerations, social support, and coping resources. Having readily available education and resource materials for local social work counselors, psychology or psychiatric services, and insurance or medication assistance programs can help patients address their mental health needs and potential life stressors which may be implicated in their mental health. Promoting mental health may ultimately promote positive family planning outcomes.
Contraceptive counseling should also include a discussion of intimate partner violence, which may be a contributing factor to depression and anxiety and which has serious implications for women’s reproductive autonomy and health. More than one in three women are estimated to experience some form of intimate partner violence—either rape, physical violence, or stalking by a sexual partner—in their lifetime [161–164]. Rates of mood and anxiety disorders are higher among women who have experienced violence compared to those who have not [42]. Women in violent relationships may experience reproductive coercion, birth control sabotage, intentional exposure to sexually transmitted infections, unintended pregnancy, and lack of control over their pregnancy outcomes, access to health services, and use of contraception [31, 161]. While most research has focused on the mental health effects of intimate partner violence, women with mental health disorders may be particularly susceptible to being victims of intimate partner violence or reproductive coercion [163]. Routine screening for intimate partner violence with simple questions such as “Has your partner ever hit, slapped, kicked, bitten, pushed, choked, shoved or physically hurt you?” can identify patients who may have special contraceptive considerations [161, 162]. Providers can assist patients in selecting methods that maximize contraceptive control and minimize the likelihood of exacerbating partner resistance or violence. The DMPA injectable is an effective, inconspicuous contraceptive method that is controlled by the woman. IUDs or the subdermal implant may offer other subtle, highly effective options that require less frequent health service visits. Overall, the individual situation and specific mental health and intimate partner violence concerns should be taken into account during contraceptive decision-making and management.
Part II: Contraception and Other Serious Mental Illnesses
While psychotic disorders like schizophrenia, bipolar disorder, and borderline personality disorder are less common than depression and anxiety disorders [164, 165], these other serious mental illnesses (SMI) have important implications for women’s reproductive health [165–170]. Women with other SMI may experience cognitive impairments, impulsivity, self-destructive behaviors, poor judgment, and co-occurring substance use that can affect family planning decision-making and contraceptive behaviors [125, 165–174]. Women with severe depression and anxiety may also exhibit similar symptoms. Women with SMI experience higher rates of non-adherence to contraceptives, unintended pregnancy, sexually transmitted infections, and nonconsensual and transactional sex than the general population of women [125, 166–181]. Unintended pregnancy for women with SMI, especially those taking teratogenic mood stabilizers, can have adverse physical, psychological, and social consequences for women and their offspring [166, 167, 169]. Thus, helping women with SMI prevent unintended pregnancy is a clinical priority. Health providers who care for with women with SMI may avoid contraceptive care due to insufficient knowledge and training, negative countertransference with regard to patients’ sexuality, incorrect assumptions about sexual activity, perceptions of contraception as secondary to psychiatric care, and concerns about ethical issues [125, 170–173, 182–185]. In this section, we offer strategies for contraceptive counseling and management for women with SMI.
Contraceptive Counseling Considerations for Other Serious Mental Illnesses
Some research on schizophrenia and bipolar disorder has found that some women with psychotic disorders lack basic knowledge of sexuality and reproduction, have misperceptions about contraception, and are concerned about access to contraceptive methods [125, 166–171, 175]. Thus, reproductive health education for women with SMI may need to be extensive. Contraceptive counseling should occur within a larger discussion of sexuality, reproductive health promotion, risk reduction and disease prevention, pregnancy intentions and readiness for pregnancy (emphasizing the value of stable social conditions and interpersonal relationships), and individual contraceptive expectations and preferences [125, 169]. Contraceptive information presented should be accurate, simple, clear, and provided at a time when patients are most receptive [125]. For instance, acutely psychotic patients are unlikely to have adequate attention and organization to assimilate contraceptive information [125, 171]. Counseling should be supplemented with simple written educational materials. Information on contraceptive methods should emphasize method-specific effectiveness rates, many of which are highly dependent upon correct use [128, 135, 154]. Effective use of some methods, like condoms, rely upon partner cooperation and support, and because women with SMI may have difficulties negotiating contraceptive use before or during sex, it is important for providers to engage partners in contraceptive counseling and education sessions when possible [170].
Contraceptive Method Considerations for Serious Mental Illness
The majority of women with SMI are eligible for the wide range of available contraceptive methods. In most cases, LARC methods, including the levonorgestrel-releasing and copper-containing IUDs and subdermal implant, should be considered as first line methods for women with SMI who wish to avoid an unintended pregnancy. LARC methods are highly effective, have few adherence issues, and do not contain estrogen, which eliminates cardiovascular risk concerns for women with chronic medical morbidities like diabetes, obesity, breast cancer, or hypertension, and women over 35 years of age who smoke. These are all health conditions which may co-occur with SMI and are CDC MEC contraindications to combined hormonal method use [57, 128, 135, 136, 171, 176]. Other progestin-only methods, including the DMPA injectable and progestin-only pills (POPs), are alterative options for women who do not wish to use LARC methods but have contraindications to estrogen. Monitoring for weight gain, truncal fat deposit, and peripheral glucose intolerance in the case of DMPA, especially among women using neuroleptics, may be useful since these potential side effects are of concern in the context of other medical morbidities [186–188]. Additionally, POPs require a relatively strict daily regimen for effectiveness (must be taken within a 3 h time frame daily) and are associated with irregular bleeding profiles, especially with missed or late dosages [128]. Barrier methods like condoms and diaphragms should be considered lower priority options for primary contraception for women with SMI given the amount of user involvement that is necessary [128, 135, 136].
For women with SMI who are eligible for estrogen-containing contraceptives and who do not want or have access to LARC, combined hormonal methods, including the vaginal ring, transdermal patch, and COCs, are reasonable options [128, 135, 136]. The effectiveness of these methods relies heavily on correct use. Health providers should work with women with SMI to optimize contraceptive choice based on co-occurring medical conditions, individual preferences, and the likelihood of method success. In all cases, dual method use (i.e., condoms plus another effective contraceptive) should be encouraged for HIV/STI prevention and unintended pregnancy protection [166, 167, 171, 175, 177–182]. Finally, because sexual intercourse is often unplanned (among all women but especially among those with SMI), emergency contraception is a necessary back up and is safe [171].
Contraceptive and Drug Interaction Considerations for Serious Mental Illness
Hyperprolactinemia and suppression of the hypothalamic–pituitary–gonadal axis is commonly experienced among women with schizophrenia on atypical antipsychotics (risperidone > aripiprazole > ziprasidone), which can lead to menstrual irregularities, amenorrhoea, sexual dysfunction, infertility issues, and galactorrhoea [189, 190]. Women taking atypical antipsychotics may believe they are not at risk for pregnancy because of menstrual irregularities or they may believe that their antipsychotic medication offers contraceptive protection, both of which are not accurate [189, 190]. Women who continue taking atypical antipsychotics with hyperprolactinemia should receive estradiol supplementation for neuroendocrine regulation, and some research has shown that estrogen may modulate and improve the expression of psychotic symptoms [189–194]. Thus, COCs may offer therapeutic effects for women on older atypical antipsychotics. However, frequent assessment of COC adherence and counseling on condom use would be essential. Women taking newer antipsychotics are less likely to experience elevated prolactin, so use of COCs for therapeutic purposes is less of a concern [189, 190, 194].
Women with schizophrenia and bipolar disorder may be treated with mood stabilizers, including antiepileptic medications including lamotrigine, carbamazepine, and topiramate. Many of these medications can induce cytochrome P450 3A4 causing enhanced hepatic metabolism of contraceptive steroids and potentially decreased contraceptive efficacy [125, 171, 176, 187, 188, 195–201]. Contraceptive steroids can also decrease levels of antiepileptics, such as valproate and lamotrigine, rendering them less effective [201–204]. Antipsychotic medications, including clozapine and chlorpromazine, are also metabolized by the liver, and contraceptive steroids can cause a significant increase in antipsychotic medication levels resulting in severe side effects such as hypotension, sedation, and tremor [202–204]. Providers should monitor psychiatric drug levels and adjust dosages as needed for hormonal contraceptive users [200–204] (see Chap. 8 for more information).
For women with SMI and drug interaction concerns, the local action of the IUDs, or the high dose of the DMPA injectable, offers effective alternative contraceptive options [128]. The injectable requires more effort on the part of the user (i.e., injections required every 3 months) compared to IUDs [128, 135]. Research that has compared these methods among women with SMI has found higher continuation rates for IUDs than for DMPA, with no differences in psychiatric complication and hospitalization rates between methods [176–185].
Ethical Considerations for Contraception in Serious Mental Illness
One of the most important and controversial but understudied topics in regard to contraception for women with SMI is how to best assess, promote, and protect women’s reproductive autonomy. SMIs are often accompanied by deficits in reality testing that can negatively impact their decision-making capabilities. This may present an ethical dilemma for health providers who wish to help protect their patients from unintended pregnancy and avoid contraceptive coercion [172, 173]. Routine mental status exams of women with acute or chronic SMI symptoms are required during all phases of contraceptive care. Women should be able to consent to contraception—specifically, attend to, absorb, retain, and recall information disclosed in contraceptive counseling sessions, appreciate the information and its significance for their lives, evaluate the consequences, express both cognitive and evaluative understanding, and communicate a decision based upon that understanding [172, 173]. Thus, the first goal of contraceptive management among patients with chronic and variable impaired autonomy and reality testing is to restore decision-making capacities. In most cases, treatment of the underlying SMI can improve functioning, which will enhance understanding of contraceptive information and the ability to apply it to family planning decision-making and behavior [172, 173]. Providers have an ethical responsibility to help patients with SMI understand the implications of unintended pregnancy and should assist in weighing the risks of pregnancy with individual reproductive values (which may be dynamic). As opposed to sterilization, LARC methods are highly effective and reversible [128]. However, these methods require provider-controlled insertion and removal procedures, which may present a dilemma for informed consent. Other long-acting methods like the DMPA injectable are less invasive but also effective and reversible [128]. When possible, spouses, partners, or family members should be engaged in contraceptive counseling and management for patients with SMI since they can provide insight into reproductive values and treatment preferences [170, 172, 173]. Providers should be aware of any undue pressure from family or signs of intimate partner violence, and patients should always be provided with ample opportunities to discuss contraception in private [172, 173].
Conclusion
Depression, anxiety, and related disorders are common among reproductive-aged women and have significant implications for women’s risk of unintended pregnancy. While other serious mental illnesses like schizophrenia and bipolar disorders are less common, these conditions can have especially adverse consequences for the health and well-being of women and their offspring. There has been a lack of attention to mental health in family planning settings, and significant research gaps prevent an in-depth understanding of the most effective approaches for contraceptive management among women with mental health conditions. From the best available scientific evidence, however, we have offered several take-home messages.
First, modern contraceptives do not appear to cause clinically significant mood symptoms or mental health conditions. The impact of hormonal contraceptives on perceived mood symptoms among women with preexisting mental health disorders warrants additional scientific investigation. Second, potential neuroendocrine, cognitive, and behavioral pathways may link mental health conditions with contraceptive decision-making and behaviors and place women at risk of unintended pregnancy. Additional research is needed to better understand these mechanisms. Third, contraceptive education and counseling is essential for women with mental health conditions who wish to avoid an unintended pregnancy. Special attention should be given to method effectiveness and adherence issues. Fourth, modern contraceptive methods are generally safe for women with mental health conditions and should be made available. Selection of an appropriate method should occur through shared decision-making. LARC methods offer strong options for women with mental health conditions since they are highly effective, are reversible, and have little user-burden. Fifth, while drug interactions with modern antidepressant and contraceptive therapies are rare, hormonal contraceptives and older antidepressant agents and some antipsychotics and mood stabilizers can interact. Similarly, chronic comorbid diseases, which commonly co-occur with mental health conditions and that may preclude estrogen use, should be taken into account. Finally, attention to ethical issues around reproductive autonomy and contraceptive decision-making, especially for women with SMI who have significant cognitive impairments, is essential. Treatment of the underlying mental health condition can restore cognitive functioning to improve contraceptive decision-making capacities.
Overall, while additional scientific research can improve our understanding of the role of mental health in contraception (and vice versa), health providers should prioritize contraceptive counseling and management for women with mental health conditions who wish to avoid unintended pregnancy. An integrated approach is needed to address interrelated mental and reproductive health issues, ultimately to improve the health and well-being of women, their families, and society [205].
References
U.S. Department of Health and Human Services’ Office on Women’s Health; Substance Abuse and Mental Health Services Administration. Action Steps for Improving Women’s Mental Health. 2009. Author.
U.S. Department of Health and Human Services. Mental Health. Healthy People 2020. http://www.healthypeople.gov/2020/LHI/mentalHealth.aspx. Accessed 27 Sept 2013.
World Health Organization. The World Health Report 2001, Mental Health: New Understanding, New Hope. 2001. Geneva, Switzerland: World Health Organization; 2001.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 4th edition, text revised. Washington, DC: American Psychiatric Association; 2000.
Gore FM, Bloem PJN, Patton GC, Ferguson J, Joseph V, Coffey C, et al. Global burden of disease in young people aged 10–24 years: a systematic analysis. Lancet. 2011;377:2093–102.
WHO. The global burden of disease: 2004 update 2008. Geneva, Switzerland: WHO; 2008.
Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74(1):5–13.
Harvard Medical School. National Comorbidity Survey. 2009. http://www.hcp.med.harvard.edu/ncs/index.php. Accessed 27 Sept 2013.
Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003;289(23):3095–105.
Twenge JM, Gentile B, DeWall N, Ma D, Lacefield K, Schurtz DR. Birth cohort increases in psychopathology among young Americans, 1938–2007: a cross-temporal meta-analysis of the MMPI. Clin Psychol Rev. 2010;30(2):145–54.
Cross-National Collaborative Group. The changing rate of major depression. Cross-national comparisons. JAMA. 1992;268(21):3098–105.
Compton WM, Conway KP, Stinson FS, Grant BF. Changes in the prevalence of major depression and substance use disorders in the United States between 1991–1992 and 2001–2002. Am J Psychiatry. 2006;163(12):2141–7.
National Institute of Mental Health [internet]. Use of mental health services and treatment among adults. http://www.nimh.nih.gov/statistics/3USE_MT_ADULT.shtml. Accessed 24 Oct 2012.
National Institute of Mental Health [internet]. Use of mental health services and treatment among children. http://www.nimh.nih.gov/statistics/1NHANES.shtml. Accessed 24 Oct 2012.
Barrio L, Burt V. Depression in pregnancy: strategies for primary care management. Dealing with under-diagnosed and undertreated problem. Wom Health Prim Care. 2000;3:490.
Miranda J, Chung JY, Green BL, Krupnick J, Siddique J, Revicki DA, Belin T. Treating depression in predominantly low-income young minority women: a randomized controlled trial. JAMA. 2003;290:57–65.
Farr SL, Dietz PM, Williams JR, Gibbs FA, Tregear S. Depression screening and treatment among non-pregnant women of reproductive age in the United States, 1990–2010. Prev Chron Dis. 2011;8:A122.
Li-Ching L, Casanueva CE, Martin SL. Depression among female family planning patients: prevalence, risk factors and use of mental health services. J Womens Health. 2005;14:225–32.
Ko JY, Farr SL, Dietz PM, Robbins CL. Depression and treatment among US pregnant and non-pregnant women of reproductive age, 2005–2009. J Womens Health. 2012;21:830–6.
Dennis CL, Ross LE, Grigoriadis S. Psychosocial and psychological interventions for treating antenatal depression. Cochrane Database Syst Rev. 2007;3. Art. No.: CD006309. DOI: 10.1002/14651858.CD006309.pub2.
Farr SL, Bitsko RH, Hayes DK, Dietz PM. Mental health and access to services among US women of reproductive aged. Am J Obstet Gynecol. 2010;203:e1–9.
Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve month use of mental health services in the United States. Arch Gen Psychiatry. 2005;62:629–40.
Carrington CH. Clinical depression in African American women: diagnosis, treatment and research. J Clin Psychol. 2006;62:779–91.
Das AK, Ofson M, McCurtis HL, Weissman MM. Depression in African Americans: breaking barriers to detection and treatment. J Fam Pract. 2006;55:30–9.
Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38:90–6.
American Psychological Association [internet]. Women and depression. http://www.apa.org/about/gr/issues/women/depression.aspx. Accessed 24 Oct 2012.
Mcleod JD, Kessler RC. Socioeconomic status differences in vulnerability to undesired life events. J Health Soc Behav. 1990;31:162–72.
U.S. Department of Health and Human Services. Mental Health: Culture, Race, and Ethnicity: A Supplement to Mental Health: A Report of the Surgeon General. Rockville, MD: US Dept of Health and Human Services, Public Health Service, Office of the Surgeon General; 2001.
Frost JJ, Singh S, Finer LB. Factors associated with contraceptive use and nonuse, United States, 2004. Perspect Sex Reprod Health. 2007;39(1):48–55.
Gee RE, Mitra N, Wan F, Chavkin DE, Long JA. Power over parity: intimate partner violence and issues of fertility control. Am J Obstet Gynecol. 2009;201(148):e1–7.
Miller E, Decker MR, McCauley HL, Tancredi DJ, Levenson RR, Waldman J, et al. Pregnancy coercion, intimate partner violence and unintended pregnancy. Contraception. 2010;81(4):316–22.
Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of pre-term birth, low birth weight and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67:1012–24.
Flynn HA, Walton MA, Chermack ST, Cunningham RM, Marcus SM. Brief detection and co-occurrence of violence, depression and alcohol risk in prenatal care settings. Arch Womens Ment Health. 2007;10:155–61.
Alder J, Fink N, Bitzer J, Hosli I, Holzgreve W. Depression and anxiety during pregnancy: a risk factor the obstetric, fetal and neonatal outcome? A critical review of the literature. J Matern Fetal Neonatal Med. 2007;20:189–209.
Kelly RH, Russo J, Holt V, Danielsen BH, Zatzick DF, Walker E, et al. Psychiatric and substance use disorders as risk factors for low birth weight and preterm delivery. Obstet Gynecol. 2002;100:297–304.
Vesga-Lopez O, Blanco C, Keyes K, Olfson M, Grant BF, Hasin DS. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry. 2008;65:805–15.
Williams KE, Marsh WK, Rasgon NL. Mood disorders and fertility in women: a critical review of the literature and implications for future research. Hum Reprod Update. 2007;13:607–16.
Bennett IM, Culhane JF, McColuum KF, Elo IT. Unintended rapid repeat pregnancy and low education status: any role for depression and contraceptive use? Obstet Gynecol. 2006;194:749–54.
Steinberg JR, Trussell J, Hall KS, Guthrie K. Fatal flaws in a recent meta-analysis on abortion and mental health. Contraception. 2012;86(5):4307.
Takahashi S, Tsuchiya KJ, Matsumoto K, Suzuki K, Mori N, Takei N. Psychosocial determinants of mistimed and unwanted pregnancy: the Hamamatsu Birth Cohort Study. Matern Child Health J. 2012;16(5):947–55.
Steinberg JR, Becker D, Henderson JT. Does the outcome of a first pregnancy predict depression, suicidal ideation, or lower self-esteem? Data from the National Comorbidity Survey. Am J Orthopsychiatry. 2011;81(2):193–201.
Steinberg JR, Finer LB. Examining the association of abortion history and current mental health: a reanalysis of the National Comorbidity Survey using a common-risk-factors model. Soc Sci Med. 2011;72:72–82.
Kessler RC, Berglund PA, Foster CL, Saunders WB, Stang PE. Walters EE Social consequences of psychiatric disorders. II: Teenage parenthood. Am J Psychiatry. 1997;154(10):1405–11.
Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, Davis MM. Risk factors for depressive symptoms during pregnancy: a systematic review. Am J Obstet Gynecol. 2010;205(3):5–14.
Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005;106(5):1071–83.
Marcus S, Flynn H, Blow F, Barry K. Depressive symptoms among pregnant women screening in obstetrics settings. J Womens Health. 2003;12(4):373–80.
Milgrom J, Gemmill AW, Bilszta JL, Hayes B, Barnett B, Brooks J, et al. Antenatal risk factors for postnatal depression: a large prospective study. J Affect Disord. 2008;108(1–2):147–57.
Beck CT. Predictors of postpartum depression: an update. Nurs Res. 2001;50(5):278–85.
Marcus SM, Flynn HA, Young E, Ghaziuddin N, Mudd S. Recurrent depression in women through the lifespan. In: Riba M, Oldham J, editors. American psychiatric press review of psychiatry. Washington, DC: American Psychiatric Press, Inc.; 2001. p. 19–50.
Silverman JG, Raj A, Mucci LA, Hathaway JE. Dating violence against adolescent girls and associated substance use, unhealthy weight control, sexual risk behavior, pregnancy, and suicidality. JAMA. 2001;286:572–9.
Wittchen H, Zhao S, Kessler RC, Eaton WW. DSM-III-R generalized anxiety disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:355–64.
Moller SE. Effect of oral contraceptives on tryptophan and tyrosine availability: evidence for a possible contribution to mental depression. Neuropsychobiology. 1981;7:192–200.
Parry BL, Rush AJ. Oral contraceptives and depressive symptomatology: biologic mechanisms. Compr Psychiatry. 1979;20:347–58.
Sheenan DV, Sheenan KH. Psychiatric aspects of oral contraceptive use. Psychiatr Ann. 1976;6:500–8.
Winston F. Oral contraceptives, pyridoxine and depression. Am J Psychiatry. 1973;130:1217–21.
Robinson SA, Dowell M, Pedulla D, McCauley L. Do the emotional side-effects of hormonal contraceptives come from pharmacologic or psychological mechanisms? Med Hypotheses. 2004;63:268–73.
CDC. U.S. Medical eligibility criteria for contraceptive use, 2010. MMWR. 2010;59.
Vessey MP, McPherson K, Lawless M, Yeates D. Oral contraception and serious psychiatric illness: absence of an association. Br J Psychiatry. 1985;146:45–9.
Duke JM, Sibbritt DW, Young AF. Is there an association between the use of oral contraception and depressive symptoms in young Australian women? Contraception. 2007;75:27–31.
Walker A, Bancroft J. Relationship between premenstrual symptoms and oral contraceptive use: a controlled study. Psychosom Med. 1990;52:86–96.
O’Connell K, Davis AR, Kerns J. Oral contraceptives: side effects and depression in adolescent girls. Contraception. 2007;75:299–304.
Deijen JB, Duyn KJ, Jansen WA, Klittsie JW. Use of a monophasic low-dose oral contraceptive in relation to mental functioning. Contraception. 1992;46:359–67.
Almagor M, Ben-Porath MS. Mood changes during the menstrual cycle and their relation to the use of oral contraceptives. J Psychosom Res. 1991;35:721–8.
Sanders SA, Graham CA, Bass JL, Bancroft J. A prospective study of the effects of oral contraceptives on sexuality and wellbeing and their relationship to discontinuation. Contraception. 2001;64:51–8.
Segebladh B, Borgstrom A, Odlind V, Bixo M, Sundstrom-Poromaa I. Prevalence of psychiatric disorders and premenstrual dysphoric symptoms in patients with experience of adverse mood during treatment with combined oral contraceptives. Contraception. 2009;79:50–5.
Westhoff C, Truman C, Kalmuss D, Cushman L, Davidson A, Rulin M, et al. Depressive symptoms and depo-provera. Contraception. 1998;57:237–40.
Gupta N, O’Brien R, Jacobsen LJ, Davis A, Zuckerman A, Supran S, et al. Mood changes in adolescents using depo-medroxyprogesterone acetate for contraception. J Pediatr Adolesc Gynecol. 2001;14:71–6.
Tsai S. Effect of depot medroxyprogesterone acetate on postpartum depression. Contraception. 2010;82:174–7.
Westhoff C, Truman C, Kalmuss D, Cushman L, Rulin M, Heartwell S, et al. Depressive symptoms and Norplant contraceptive implants. Contraception. 1998;57(4):241–5.
Lopez LM, Grimes DA, Gallo MF, Schulz KF. Skin patch and vaginal ring versus combined oral contraceptives for contraception. Cochrane Database Syst Rev. 2010;17(3)pub3.
Sucato GS, Land SR, Murray PJ, Cecchini R, Gold MA. Adolescents experiences using the contraceptive patch versus pills. J Pediatr Adolesc Gynecol. 2011;24:197–203.
Mansour D, Korver T, Marintcheva-Petrova M, Fraser IS. The effects of Implanon on menstrual bleeding patterns. Eur J Contracept Reprod Health Care. 2008;13:13–28.
Elovainio M, Teperi J, Aalto AM, Grenman S, Kivelä A, Kujansuu E, et al. Depressive symptoms as a predictor of discontinuation of treatment of menorrhagia by levoenorgesterol releasing intrauterine system. Int J Behav Med. 2007;14:70–5.
Westhoff C, Heartwell S, Edwards S, Zieman M, Stuart G, Cwiak C, et al. Oral contraceptive discontinuation: do side effects matter? Am J Obstet Gynecol. 2007;196:412e1–7.
Rosenberg MJ, Waugh MS, Long S. Unintended pregnancies and use, misuse and discontinuation of oral contraceptives. J Reprod Med. 1995;40:355–60.
Stenchever MA, Herbst AL, Droegemueller W, Mishell D, editors. Comprehensive gynecology. St. Louis: Elsevier Health Sciences; 2001.
Hall K, Reame N, O’Connell K, Rickert V, Weshoff C. Influence of depressed mood and psychological stress symptoms on perceived oral contraceptive side effects and discontinuation in young minority women. Contraception. 2012;86:518–25.
Rubino-Watkins MF, Doster JA, Franks S, Kelly KS, Sonnier BL, Goven AJ, et al. Oral contraceptive use: implications for cognitive and emotional functioning. J Nerv Ment Dis. 1999;187:275–80.
Barsky AJ, Saintfort R, Rogers MP, Borus JF. Nonspecific medication side effects and the Nocebo phenomenon. JAMA. 2002;287:22–7.
Katon W, Lin E, Von Korff M, Russo J, Lipscomb P, Bush T. Somatization: a spectrum of severity. Am J Psychiatry. 1991;148:34–40.
Mathews A, MacLeod C. Cognitive vulnerability to emotional disorders. Annu Rev Clin Psychol. 2005;1:167–95.
Beck AT. Cognitive models of depression. J Cognit Psychother. 1987;1(1):5–37.
Maner JK, Schmidt NB. The role of risk avoidance in anxiety. Behav Ther. 2006;37(2):181–9.
Yuen KSL, Lee TMC. Could mood state affect risk-taking decisions? J Affect Disord. 2003;75(1):11–8.
Ruscher S, de Wit R, Mazimanian D. Psychiatric patients’ attitudes about medication and factors affecting noncompliance. Psychiatr Serv. 1997;48:82–5.
Patel MS, David AS. Medication adherence: predictive factors and enhancement strategies. Psychiatry. 2004;3:41–4.
Calev A. Assessment of neuropsychological functions in psychotic disorders. Washington, DC: American Psychiatric Press; 1999.
Alvy LM, McKirnan DJ, Mansergh G, Koblin B, Colfax GN, Flores SA, et al. Project MIX Study Group. Depression is associated with sexual risk among men who have sex with men, but is mediated by cognitive escape and self-efficacy. AIDS Behav. 2011;15(6):1171–9.
Clery-Melin ML, Schmidt L, Lafargue G, Baup N, Fossati P, Pessiglione M. Why don’t you try harder? An investigation of effort production in major depression. PLoS One. 2011;6(7):e23178. 1–8.
Hartley CA, Phelps EA. Anxiety and decision-making. Biol Psychiatr. 2012;72(2):113–8.
Lehrer JA, Shrier LA, Gortmaker S, Buka S. Depressive symptoms as longitudinal predictors of sexual risk behaviors among US middle and high school students. Pediatrics. 2006;118:189–200.
Shrier LA, Harris SK, Sternberg M, Beardslee WR. Associations of depression, self-esteem, and substance use with sexual risk among adolescents. Prev Med. 2001;33(3):179–89.
Chen YW, Stiffman AR, Cheng LC, Dore P. Mental health, social environment and sexual risk behaviors of adolescent service users: a gender comparison. J Child Fam Stud. 1997;6:9–25.
Garbers S, Correa N, Tobier N, Blust S, Chiasson MA. Associations between symptoms of depression and contraceptive method choices among low-income women at urban reproductive health centers. Matern Child Health J. 2010;14:102–9.
Hall K, Moreau C, Trussell J, Barber J. Role of young women’s depression and stress symptoms in their weekly use and nonuse of contraceptive methods. J Adolesc Health. 2013;53(2):241–8.
Hall K, Moreau C, Trussell J, Barber J. Young women’s consistency of contraceptive use—do depression and stress matter? Contraception. 2013;88(5):641–9.
Brooks TL, Harris SK, Thrall JS. Woods ER Association of adolescent risk behaviors with mental health symptoms in high school students. J Adolesc Health. 2002;31:240–6.
Zink TM, Shireman TI, Ho M, Buchanan T. High-risk teen compliance with prescription contraception: an analysis of Ohio medicaid claims. J Pediatr Adolesc Gynecol. 2002;15:15–21.
Steinberg JR, Tschann JM, Henderson JT, Drey EA, Steinauer JE, Harper CC. Psychological distress and post-abortion contraceptive choice at an urban clinic. Contraception. 2013;88:717–24.
Mann JJ. The medical management of depression. N Engl J Med. 2005;353:1819–34.
Roter DL, Frankel RM, Hall JA, Sluyter D. The expression of emotion through nonverbal behavior in medical visits. Mechanisms and outcomes. J Gen Intern Med. 2006;21:s28–34.
Hackley B, Sharma C, Kedzior A, Sreenivasan S. Managing mental health conditions in primary care settings. J Midwifery Womens Health. 2010;55(1):9–19.
National Institute for Health and Clinical Excellence Clinical guidelines CG90, TMAP Guidelines, The MacArthur Initiative on Depression and Primary Care. 2009.
University of Michigan Depression Center Toolkit [internet]. http://depressiontoolkit.org/treatmentoptions/Psychotherapy/dbt.asp. Accessed 20 Dec 2012.
ARHP’s Clinical Advisory Committee for The Reproductive Health Implications of Depression [internet]. 2011. http://www.arhp.org/core. Accessed 1 Feb 2013.
American Psychological Association [internet]. Assessment tools. http://www.apa.org/pi/about/publications/caregivers/practice-settings/assessment/tools/index.aspx. Accessed 1 Feb 2013.
Bohannon RW, Maljanian R, Goethe J. Screening for depression in clinical practice: reliability and validity of a five-item subset of the CES-depression. Percept Mot Skills. 2003;97:855–61.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1993;24:385–96.
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Ewing JA. Detecting alcoholism. The CAGE questionnaire. JAMA. 1984;12(14):1905–7.
Kroenke K, Spitzer RL, Williams JB. The patient health questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284–92.
Cotton MA, Ball C, Robinson P. Four simple questions can help screen for eating disorders. J Gen Intern Med. 2003;18:53–6.
McDowell AK, Lineberry TW, Bostwick JM. Practical suicide-risk management for the busy primary care physician. Mayo Clin Proc. 2011;86:792–800.
Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10(2):77–84.
Spitzer RL, Kroenke K, Williams JBW, Patient Health Questionnaire Primary Care Study Group. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA. 1999;282(18):1737–44.
Richter P, Werner J, Heerlein A, Kraus A, Sauer H. On the validity of the beck depression inventory: a review. Psychopathology. 1998;31(3):160–8.
Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the beck depression and anxiety inventories. Behav Res Ther. 1995;33(3):335–43.
Fydrich T, Dowdall D, Chambless DL. Reliability and validity of the beck anxiety inventory. J Anxiety Dis. 1992;6(1):55–61.
Beck AT, Steer RA. Manual for the beck anxiety inventory. San Antonio, TX: Psychological Corporation; 1990.
Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. State-trait anxiety inventory for adults: manual, test booklet and scoring key 1983. Palo Alto, CA: Consulting Psychologist Press, Inc.; 1983.
Higgins ES. A review of unrecognized mental illness in primary care prevalence, natural history and efforts to change the course. Arch Fam Med. 1994;3:908–17.
Koke SC, Brown EB, Miner CM. Safety and efficacy of fluoxetine in patients who receive oral contraceptive therapy. Am J Obstet Gynecol. 2002;187:551–5.
D’Arcy PF. Drug interactions with oral contraceptives. Drug Intell Clin Pharm. 1986;20:353–62.
Anderson IM, Edwards JG. Guidelines for choice of selective serotonin reuptake inhibitor in depressive illness. Adv Psychiatr Treat. 2001;7:170–80.
Buckley P, editor. Sexuality and serious mental illness. Netherlands: Harwood Academic Publishers; 2013.
Will-Shahab L, Bauer S, Kunter U, Roots I, Brattstrom A. St John’s wort extract (Ze 117) does not alter the pharmacokinetics of a low dose oral contraceptive. Eur J Clin Pharmacol. 2009;65:287–94.
Murphy PA, Kern SE, Stanczyk FZ, Westhoff CL. Interaction of St. John’s wort with oral contraceptives; effects on the pharmacokinetics of norethindrone and ethinyl estradiol, ovarian activity and breakthrough bleeding. Contraception. 2005;71:402–8.
Hatcher RA, Trussell J, Stewart F, et al. Contraceptive technology. 20 (Revised)th ed. New York, NY: Ardent Media; 2004.
Hunot VM, Caldwell D, Jones DP, Furukawa TA, Lewis G, Churchhill R. Cognitive behavioural therapies versus treatment as usual for depression. Cochrane Database Syst Rev. 2010; DOI: 10.1002/14651858.CD008699.
Hunot V, Churchill R, Teixeira V, Silva de Lima M. Psychological therapies for generalised anxiety disorder. Cochrane Data Syst Rev. 2007;1, Art. No.: CD001848. DOI:10.1002/14651858
Churchill R, Davies P, Caldwell D, Moore THM, Jones H, Lewis G, Hunot V. Interpersonal, cognitive analytic and other integrative therapies versus treatment as usual for depression. Cochrane Database Syst Rev. 2010;9, Art. No.: CD008703. DOI:10.1002/14651858.CD008703.
Hall KS, Reame N, O’Connell K, Westhoff C. Studying the use of oral contraception: a review of measurement approaches. J Womens Health. 2010;19:2203–10.
DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–7.
Osterberg L, Blascke T. Adherence to medication. N Engl J Med. 2005;353:487–97.
World Health Organization (WHO) Department of Reproductive Health and Research, Johns Hopkins Bloomberg School of Public Health/Center for Communication Programs (CCP). Knowledge for health project. Family planning: a global handbook for providers (2011 update). Baltimore, MD; Geneva, Switzerland: CCP and WHO; 2011.
Trussell J, Vaughn B. Contraceptive failure, method-related discontinuation and resumption of use: results from the 1995 NSFG. Fam Plann Perspect. 1999;31:64–72. 93.
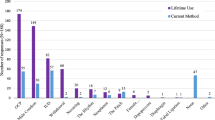
Mosher WD, Jones J. Use of contraception in the United States: 1982–2008. Vital Health Stat. 2010;23:1–43.
Kost K, Singh S, Vaughan B, Trussell J, Bankole A. Estimates of contraceptive failure from the 2002 National Survey of Family Growth. Contraception. 2008;77:10–21.
Moreau C, Trussell J, Gilbert F, Bajos N, Bouyer J. Oral contraceptive tolerance: does the type of pill matter? Obstet Gynecol. 2007;109:1277–85.
Hall KS, Trussell J. Types of combined oral contraceptives used by US women. Contraception. 2012;86(6):659–65.
Gallo MF, Grimes NK, Lopez LM, Schulz KF. 20ug versus >20ug estrogen combined oral contraceptives for contraception. Cochrane Collab Rev. 2011;1. http://www.thecochranelibrary.com.
Maitra NN, Kulier R, Bloemenkamp K, Helmerhorst FM, Gulmezogul AM. Progestogens in combined oral contraceptives for contraception. Cochrane Collab Rev. 2011;3. http://www.thecochranelibrary.com.
Lawrie TA, Helmerhorst FM, Maitra NN, Kulier R, Bloemenkamp K, Gulmezoglu AM. Types of progestogens in combined oral contraception: effectiveness and side-effects Cochrane Collab Rev. 2011;5. http://www.thecochranelibrary.com.
Van Vliet HAAM, Grimes DA, Lopez LM, Schulz KF, Helmerhorst FM. Triphasic versus monophasic oral contraceptives for contraception. Cochrane Collab Rev. 2011;12. http://www.thecochranelibrary.com.
Edelman A, Gallo MF, Jensen JT, Nichols MD, Grimes DA. Continuous or extended cycle vs. cyclic use of combined hormonal contraceptives for contraception. Cochrane Collab Rev. 2011;8. http://www.thecochranelibrary.com.
Ward RK, Zamorski MA. Benefits and risks of psychiatric medication during pregnancy. Am Fan Physician. 2002;66:629–36.
Flynn HA, O'Mahen HA, Massey L, Marcus S. The impact of a brief obstetrics clinic-based intervention on treatment use for perinatal depression. J Womens Health. 2006;15:1195–204.
Marcus SM, Barry KL, Flynn HA, Tandon R, Greden JF. Treatment guidelines for depression in pregnancy. Int J Gynecol Obstet. 2001;72:61–70.
O’Mahen HA, Himle JA, Fedock G, Henshaw E, Flynn HA. A pilot randomized controlled trial of cognitive behavioral therapy for perinatal depression adapted for women with low incomes. Depress Anxiety. 2013;30(7):679–87.
Freeman EW, Samuel MD, Lin H, Nelson DB. Associations of hormones and menopausal status with depressed mood in women with no history of depression. Arch Gen Psychiatry. 2006;63(4):375–82.
Parry BL. Optimal management of perimenopausal depression. Int J Womens Health. 2010;2:143–51.
Steinberg EM, Rubinow DR, Bartko JJ, Fortinsky PM, Haq N, Thompson K, et al. A cross-sectional evaluation of perimenopausal depression. J Clin Psychiatry. 2008;69(6):973–80.
Frost JJ, Lindberg LD, Finer LB. Young adults’ contraceptive knowledge, norms and attitudes: associations with risk of unintended pregnancy. Perspect Sex Reprod Health. 2012;44(2):107–16.
Hall KS, Castano P, Stone P, Westhoff C. Measuring oral contraceptive knowledge: a review of research findings and limitations. Patient Educ Couns. 2010;81:388–94.
Akers AY, Gold MA, Borrero S, Santucci A, Schwarz EB. Structured contraceptive counseling—a randomized controlled trial. J Womens Health. 2010;19:1163–70.
Hall K. The health belief model can guide modern contraceptive research. J Midwifery Womens Health. 2011;57:74–81.
Lopez LM, Tolley EE, Grimes DA, Mario CM. Theory-based strategies for improving contraceptive use: a systematic review. Contraception. 2009;79:411–7.
Tessler SL, Peipert JF. Perceptions of contraceptive effectiveness and health effects of oral contraception. Womens Health Issues. 1997;7:400–6.
Rickert VI, Berenson AB, Williamson AJ, Wiemann CM. Immediate recall of oral contraceptive instructions: implications for providers. Am J Obstet Gynecol. 1999;180:1399–406.
Grimes DA, Schulz KF. Nonspecific side effects of oral contraceptives: nocebo or noise? Contraception. 2011;83(1):5–9.
ACOG. Intimate partner violence. Committee Opinion No. 518. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2012;119:412–7.
Black MC, Basile KC, Breidig MJ, Smith SG, Walters ML, Merrick MT, et al. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 summary report. Atlanta (GA): National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2011.
Lehrer JA, Buka B, Gortmaker S, Shrier LA. Depressive symptomatology as a predictor of exposure to intimate partner violence among US female adolescents and young adults. Arch Pediatr Adolesc Med. 2006;160(3):270–6.
National Alliance on Mental Illness [internet]. About mental illness. http://www.nami.org/template.cfm?section=about_mental_illness. Accessed 2 June 2013
National Institute of Mental Health [internet]. Prevalence of serious mental illness among U.S. Adults by age, sex and race. http://www.nimh.nih.gov/statistics/SMI_AASR.shtml. Accessed 20 Aug 2013.
Matevosyan NR. Reproductive health in women with serious mental illnesses: a review. Sex Disabil. 2009;27:109–18.
Miller LJ. Sexuality, reproduction, and family planning in women with schizophrenia. Schizopr Bull. 1997;23(4):623–35.
Miller LJ, Finnerty M. Family planning knowledge, attitudes and practices in women with schizophrenic spectrum disorders. J Psychosom Obstet Gynaecol. 1998;19:210–7.
Krumm S, Killan R, Becker T. Mentally ill women’s subjective views on social context of desire for children. A qualitative approach. Psychiatr Prax. 2011;38(1):23–30.
Guedes TG, Moura ERF, Almeida PC. Particularities of family planning in women with mental disorders. Rev Lat Am Enfermagem. 2009;17(5):639–44.
Seeman MV, Ross R. Prescribing contraceptives for women with schizophrenia. J Psychiatr Pract. 2011;17:258–69.
McCullough LB, Coverdale J, Bayer T, Chernenak FA. Ethically justified guidelines for family planning interventions to prevent pregnancy in female patients with chronic mental illness. Am J Obstet Gynecol. 1992;167:19–25.
Coverdale JH, Bayer TL, McCullough LB, Chervenak FA. Respecting the autonomy of chronic mentally ill women in decisions about contraception. Hosp Community Psychiatry. 1993;44(7):671–4.
Magalhaes PVS, Kapczinkski F, Kauer-Sant’Anna M. Use of contraceptive methods among women treated for bipolar disorder. Arch Womens Ment Health. 2009;12:183–5.
Lang DL, Sales JM, Salazar LR, DiClemente RJ, Crosby RA, Brown LK, et al. Determinants of multimethod contraceptive use in a sample of adolescent women diagnosed with psychological disorders. Infect Dis Obstet Gynecol. 2000;2011:1–8.
Berenson AB, Asem H, Tan A, Wilkinson GS. Continuation rates and complications of intrauterine contraception in women diagnosed with bipolar disorder. Obstet Gynecol. 2011;118(6):1331–6.
Whitmore EA, Mikulich SK, Ehlers KM, Crowley TJ. One-year outcome of adolescent females referred for conduct disorder and substance abuse/dependence. Drug Alcohol Depend. 2000;59(2):131–41.
Smith MD. HIV risk in adolescents with severe mental illness: literature review. J Adolesc Health. 2001;29(5):320–9.
Auslander WF, McMillen JC, Elze D, Thompson R, Jonson-Reid M, Stiffman A. Mental health problems and sexual abuse among adolescents in foster care: relationship to HIV risk behaviors and intentions. AIDS Behav. 2002;6(4):351–9.
Tubman JG, Gil AG, Wagner EF, Artigues H. Patterns of sexual risk behaviors and psychiatric disorders in a community sample of young adults. J Behav Med. 2003;26(5):473–500.
DiClemente RJ, Ponton LE. HIV-related risk behaviors among psychiatrically hospitalized adolescents and school- based adolescents. Am J Psychiatry. 1993;150(2):324–5.
Haboubi NH, Lincoln N. Views of health professionals on discussing sexual issues with patients. Disabil Rehabil. 2003;25:291–6.
Wright ER, Wright DE, Perry BL, Foote-Ardah CE. Stigma and the sexual isolation of people with serious mental illness. Soc Prob. 2007;54:78–98.
Abel K, Rees S. Reproductive and sexual health of women service users: what’s the fuss? Adv Psychiatr Treat. 2010;16:279–80.
Cropsey KL, Matthews C, Campbel S, Ivey S, Adawadkar S. Long-term, reversible contraception use among high-risk women treated in a university-based gynecology clinic: comparison between IUD and depo-provera. J Womens Health (Larchmt). 2010;19:349–53.
Verhaeghe J. Hormonal contraception in women with the metabolic syndrome: a narrative review. Eur J Contracept Reprod Health Care. 2010;15:305–13.
Crawford P. Interactions between antiepileptic drugs and hormonal contraception. CNS Drugs. 2002;16:263–72.
Dutton C, Foldvary-Schaefer N. Contraception in women with epilepsy: pharmacokinetic interactions, contraceptive options, and management. Int Rev Neurobiol. 2008;83:113–34.
Seeman MV. Antipsychotic-induced amenorrhea. J Ment Health. 2011;20(5):484–91.
Richer-Rossler A, Schmid C, Bleuer S, Birkhauser M. Antipsychotics and hyperprolactinaemia: pathophysiology, clinical relevance, diagnosis and therapy. Neuropsychiatr. 2009;23(2):71–83.
Riecher-Rössler A. Oestrogen effects in schizophrenia and their potential therapeutic implications—review. Arch Womens Ment Health. 2002;5(3):111–8.
Kulkarni J, de Castella A, Fitzgerald PB, Gurvich CT, Bailey M, Bartholomeusz C, et al. Estrogen in severe mental illness: a potential new treatment approach. Arch Gen Psychiatry. 2008;65:955–60.
Riecher-Rössler A, de Geyter C. The forthcoming role of treatment with oestrogens in mental health. Swiss Med Wkly. 2007;137:565–72.
Currier GW, Simpson GM. Psychopharmacology: antipsychotic medications and fertility. Psychiatr Serv. 1998;49:175–6.
Gaffield ME, Culwell KR, Lee CR. The use of hormonal contraception among women taking anticonvulsant therapy. Contraception. 2011;83:16–29.
Spina E, Pisani F, Perucca E. Clinically significant pharmacokinetic drug interactions with carbamazepine. An update. Clin Pharmacokinet. 1996;31:198–214.
Herzog AG, Blum AS, Farina EL, Maestri XE, Newman J, Garcia E, et al. Valproate and lamotrigine level variation with menstrual cycle phase and oral contraceptive use. Neurology. 2009;72:911–4.
Wegner I, Edelbroek PM, Bulk S, Lindhout D. Lamotrigine kinetics within the menstrual cycle, after menopause, and with oral contraceptives. Neurology. 2009;73:1388–93.
Bialer M, Doose DR, Murthy B, Curtin C, Wang SS, Twyman RE, et al. Pharmacokinetic interactions of topiramate. Clin Pharmacokinet. 2004;43:763–80.
Johannessen Landmark C, Patsalos PN. Drug interactions involving the new second- and third-generation antiepileptic drugs. Expert Rev Neurother. 2010;10:119–40.
Reddy DS. Clinical pharmacokinetic interactions between antiepileptic drugs and hormonal contraceptives. Expert Rev Clin Pharmacol. 2010;3:183–92.
Gabbay V, O’Dowd MA, Mamamtavrishvili M, Asnis GM. Clozapine and oral contraceptives: a possible drug interaction. J Clin Psychopharmacol. 2002;22:621–2.
Brown D, Goosen TC, Chetty M, Hamman JH. Effect of oral contraceptives on the transport of chlorpromazine across the CACO-2 intestinal epithelial cell line. Eur J Pharm Biopharm. 2003;56:159–65.
Chetty M, Miller R. Oral contraceptives increase the plasma concentrations of chlorpromazine. Ther Drug Monit. 2001;23:556–8.
World Health Organization. Mental Health Aspects of Women’s Reproductive Health: A global review of the literature. Geneva, Switzerland:WHO; 2009.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Hall, K.S., Steinberg, J.R., Marcus, S.M. (2014). Contraception for Women with Mental Health Conditions. In: Allen, R., Cwiak, C. (eds) Contraception for the Medically Challenging Patient. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-1233-9_5
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1233-9_5
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-1232-2
Online ISBN: 978-1-4939-1233-9
eBook Packages: MedicineMedicine (R0)