Abstract
Addiction to tobacco smoking is a deadly disease that consumes millions of lives each year. However, the neurobiology underlying the disease remains an enigma. One reason for this is the relative complexity of nicotine’s effects on the brain, with a multitude of targets throughout many different brain regions, each subserving individual components of the disease. Still, a handful of brain circuits mediate particularly significant roles in the disease. The epithalamic habenulo-interpeduncular (Hb-IPN) pathway participates in the aversive aspects of nicotine dependence, including the aversive experience of nicotine withdrawal. Many hypotheses regarding the exact mechanisms for these behavioral roles exist, but the convergent feature of those hypotheses is that nicotine acts at populations of nicotinic acetylcholine receptors (nAChRs) across the brain, including the Hb-IPN pathway. Of note, the Hb-IPN pathway is one of the brain regions with the highest density of nAChRs, including both heteromeric (e.g., α3β4 and α4β2) and homomeric (i.e., α7) receptors. As nAChR subtypes that subserve multiple aspects of affective and reinforcement behaviors are expressed along this pathway, it is of no surprise that the Hb-IPN pathway participates in similar affective behaviors. This chapter will discuss the roles of nAChRs along the Hb-IPN in aversive nicotine-associated behaviors, as well as touch upon the innate roles of those populations of nAChRs over biology and behavior in healthy animals.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Nicotinic acetylcholine receptor
- α5 subunit
- β4 subunit
- Medial habenula
- Interpeduncular nucleus
- Nicotine
- Aversion
- Negative reinforcement
- Nicotine withdrawal
1 Introduction
Tobacco smoking is the leading cause of preventable death in the world, with estimates of four to five million annual deaths worldwide [1–3]. Containing over 60 identified carcinogenic compounds [4], tobacco smoke is highly carcinogenic, as roughly one third of all cancer-related mortalities in developed countries can be attributed to tobacco use [1]. The fact that rates of tobacco use in developing countries remain high, despite costly antitobacco campaigns, speaks to the global pervasiveness of this health threat [5, 6]. As a consequence, there is strong need to develop therapies to aid smoking cessation by addressing dependence to nicotine, the primary addictive component of tobacco smoke [3, 7–9].
The first and arguably greatest barrier to successful smoking cessation is the collection of withdrawal symptoms that emerges soon after an attempt to quit [10–14]. Comprising both physical and affective symptoms, nicotine withdrawal can be a considerably unpleasant experience, with an onset as early as a few hours following the suspension of nicotine consumption. Successful strategies to develop new treatments for nicotine dependence should incorporate the existing knowledge of nicotine’s effects over the neuronal pathways and molecular mechanisms that underlie this disease.
Fortunately, inroads toward understanding the neurobiology of nicotine dependence have been made on many fronts [9, 15, 16]. A significant body of knowledge has already been obtained regarding the biophysical, pharmacological, and cellular properties of nicotinic acetylcholine receptors (nAChRs), which constitute the primary molecular targets of nicotine in the body [7–9, 17]. Progress is also being made toward the definition of the brain circuits that underlie various aspects of nicotine dependence, from reward to withdrawal symptoms [9, 18].
nAChRs are pentameric acetylcholine (ACh)-gated ion channels that exist as homomeric (all α subunits) or heteromeric (α and β subunits) structures [7, 17, 19, 20]. Genes encoding nAChR subunits are found in both vertebrates and invertebrates [7, 21], and sequences among mammals are fairly conserved [22, 23]. Within mammalian genomes, separate genes encode eight distinct α nAChR subunits and three distinct β subunits [7]. Expression in heterologous systems has allowed the study of the contribution of individual subunits to receptor function [24–30]. nAChRs are expressed in almost all brain regions, including the circuits that underlie nicotine’s influence over reinforcement, aversion, attention, and learning and memory [7, 9, 18, 31, 32].
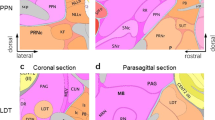
In this chapter, we discuss molecular, cellular, circuit, and behavioral facets of nicotine withdrawal and related negative aspects of nicotine dependence. In so doing, we focus primarily on the nAChRs along the habenulo-interpeduncular (Hb-IPN) pathway, a circuit with emerging roles in negative reinforcement and aversion (Fig. 18.1) [33–35]. As we enumerate the physiological and behavioral roles of this circuit, we discuss the relevant functional roles of the nAChRs expressed along this pathway. Ultimately, we integrate these topics into a basic framework for the understanding of the function of habenulo-interpeduncular nAChRs in overall dependence to nicotine.
The Hb-IPN pathway bridges forebrain nuclei to those within the mid- and hindbrain. Diagram of a sagittal view of the mouse brain illustrating the anatomical connectivity of the Hb-IPN pathway in mice. The Hb-IPN pathway, principally composed of the medial (green) and lateral (pink) habenulae, the fasciculus retroflexus, and the interpeduncular nucleus (sky blue), bridges various nuclei within the forebrain to mid- and hindbrain nuclei. Afferent projections to and efferent projections from the medial (red arrows) and lateral (purple arrows) habenulae are displayed
2 Nicotine’s Influences on nAChRs and Cell Function
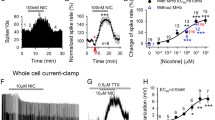
To understand the effects of nicotine on brain circuits and ultimately behavior, it is necessary to first consider its effects at a molecular level. The binding of nicotine to nAChRs occurs at specific sites on the interface between two adjacent subunits [7, 36, 37]. In homomeric nAChRs, such as in α7 nAChRs, binding occurs between any two of the subunits and results in a total of five binding sites. In heteromeric nAChRs, such as α4β2 nAChRs, nicotine binding occurs at the interface between specific α and β subunits, resulting in a total of two binding sites. Nicotine binding activates the nAChR, resulting in the flux of mono- and divalent cations such as Na+, K+, and Ca2+ across the plasma membrane [7, 38]. The influx of cations (primarily Na+, but also Ca2+) leads to a membrane depolarization that consequently triggers a variety of intracellular events. In addition, intracellular Ca2+ signaling is important in many cellular processes [39–42]. Influenced by the specific subunit composition, many nAChR subtypes have sizable Ca2+ permeabilities. For example, α7 nAChRs have Ca2+ permeabilities that are comparable to those of NMDA glutamate receptors [43, 44]. Inclusion of the α5 subunit in receptors with other α and β subunits also confers increased Ca2+ permeability, especially in receptors that contain β2 [45]. Furthermore, the activation of nAChRs can also lead to intracellular Ca2+ elevations via indirect means, either through depolarization-induced activation of voltage-gated calcium channels or through Ca2+-activated Ca2+ release from intracellular stores [46]. In addition to the classical role of high Ca2+-permeable nAChRs in facilitating neurotransmitter release at presynaptic sites [47, 48], intracellular Ca2+ elevations generated by nAChR activation are involved in a number of cellular processes, such as modulation of cellular excitability and transcriptional regulation [49–52]. Ultimately, the functional cellular outcome of nAChR activation will also depend on the brain region- and cell-specific subcellular localization of the channels, which may include pre- and postsynaptic expression, as well as somatic or axonal locations [7].
Complementary to the activation of nAChRs, receptor desensitization is another important property of nAChRs that determines their overall function and must be considered when examining the acute or chronic effects of nicotine [7, 53–56]. In addition to open and closed conformations, nAChRs can exist in desensitized conformations following exposure to elevated concentrations of ligand. In a desensitized conformation, nAChRs are unable to evoke the response that occurs during open states, despite the presence of bound ligands on receptors. The kinetics of desensitization are characterized by multiple exponential functions and are influenced by receptor composition. α7 nAChRs desensitize quickly, while α4β2 nAChRs desensitize with slower kinetics [57–60]. However, due to their high affinity for nicotine, α4β2 nAChRs desensitize at lower concentrations of nicotine (<0.1 μM), while α7 nAChRs do not efficiently desensitize below a concentration of 1 μM. At concentrations of nicotine typically found in smokers, α4β2 nAChRs in the human brain are nearly fully occupied by nicotine [61]. Given that desensitization occurs at these concentrations or lower, it is likely that most of the brain’s α4β2 nAChRs are maintained in a desensitized state during habitual cigarette smoking. nAChR desensitization is regulated by many factors, including intracellular Ca2+. In both heterologous expression systems and neurons isolated from the medial habenula, the level of intracellular Ca2+ is inversely proportional to the recovery of nAChRs from desensitization to nicotine [62–64]. It is suggested that the presence of Ca2+ stabilizes a desensitized conformation. Since nAChR desensitization is functionally analogous to blockade of those receptors, to some degree, this phenomenon can have significant consequences across many levels of brain function, from molecular and cellular to systems and behavioral.
Finally, one should consider that as a tertiary amine, nicotine exists in both charged and uncharged states. In the nonpolar uncharged form, nicotine becomes membrane permeable and can freely enter the cytosolic space where it interferes with various cellular mechanisms, including actions at the endoplasmic reticulum and/or proteasome complex [65, 66]. Given that nAChR subunits are degraded by the proteasome and proteasome inhibition enhances nAChR assembly within the endoplasmic reticulum [67], nicotine-mediated inhibition of the proteasome complex causes enhanced nAChR plasma membrane expression as well [68, 69].
3 Neuroadaptations During Chronic Nicotine Exposure
The chronic use of nicotine causes multiple neuroadaptations in the brain, demonstrated by many in vitro studies in heterologous expression systems, as well as in vivo studies in rodents [25, 70–74]. The most commonly observed molecular phenomena are alterations in membrane expression of nAChRs that occur in a subtype-, brain region-, and time-dependent fashion [75]. The α4β2 nAChR subtype, in particular, has been shown in vitro to exhibit functional upregulation in response to chronic nicotine treatment, in the form of acetylcholine-induced current increases, in both heterologous expression systems and cultured neurons [72, 76–78]. Furthermore, in vivo nicotine exposure increases these measures for neurons in mouse brain slices [79]. It is suggested that these functional upregulations are due to dual mechanisms [80]. A short-lived switch in the conformation of surface nAChRs from a low-affinity to a higher-affinity state constitutes a rapid response following nicotine exposure. Secondarily, an effect with slower kinetics ensues, increasing surface α4β2 nAChRs via reduced proteasomal degradation of subunits and increased maturation of the receptors [65, 66].
4 Nicotine Withdrawal Syndrome: nAChRs Along the MHb-IPN Pathway Are Critical for the Physical Symptoms of Nicotine Withdrawal
Several physical and affective symptoms emerge during the period of acute nicotine withdrawal that may last for as long as a month following the start of abstinence [9, 14, 81]. These symptoms include a collection of unpleasant and aversive experiences such as intense cravings for nicotine, irritability, anger, anxiety, difficulty concentrating, insomnia, and increased appetite with consequent weight gain [11, 82–84]. Other physical manifestations accompany these behavioral symptoms of nicotine withdrawal, including restlessness, decreased heart rates, fluctuations of hormonal levels, drowsiness, headaches, gastrointestinal disturbances, and reduction in the electroencephalography (EEG) theta band [11, 85–87]. The emergence of these negative and/or aversive symptoms is the result of brain circuits, accustomed to the chronic presence of nicotine, readapting to a new steady state in its absence [9].
Behaviorally, symptoms of nicotine withdrawal can be classified as physical or affective [88, 89]. Physical symptoms of nicotine withdrawal have been successfully simulated in the laboratory to study the neurobiology underlying these behavioral disruptions [90–93]. Normal naïve mice display a number of typical behaviors when idle, including grooming, scratching, and chewing. However, when mice are subjected to withdrawal from nicotine following chronic treatment, the instances of these behaviors increase substantially and are accompanied by the emergence of other behaviors indicative of physical discomfort, including shaking, cage scratching, head nodding, and jumping. Using this behavioral paradigm in combination with mutant mice, the nAChR subunits important for the emergence of these physical symptoms of withdrawal were determined. In wild-type mice chronically treated with nicotine, systemic injection of the broad nAChR antagonist mecamylamine elicited an elevation of the physical signs of nicotine withdrawal over that of control mice chronically treated with a vehicle solution. However, in mice null for the β4 nAChR subunit, this elevation was completely abolished [92]. Along with previously established roles of this subunit in the modulation of anxiety and the anxiolytic properties of nicotine [94], this finding began to build a framework for the function of β4-containing (β4*) nAChRs in aversive and negatively reinforcing behaviors. In vivo, the most common assembly partner of the β4 subunit in neuronal nAChRs is the α3 subunit [9, 14, 27, 95].
Further experiments with additional nAChR subunit mutant mice revealed that physical withdrawal from nicotine also depends on α5, α2, and partially on α7 nAChR subunits [93, 96, 97]. Human genetic studies also identified multiple single-nucleotide polymorphisms in the gene cluster encoding the α5, α3, and β4 nAChR subunits that associate with various aspects of nicotine dependence and tobacco-related diseases [98–106]. The MHb-IPN pathway is among the brain areas with the highest co-expression of α5, α3, α2, and β4 [98, 107–111]. The habenular complex is composed of the medial (MHb) and lateral (LHb) habenular nuclei, with projections traveling along the fasciculus retroflexus, the white matter tract that bridges the habenular nuclei and their projection sites. The interpeduncular nucleus (IPN) is the main projection site for the MHb, while the LHb extends behaviorally important projections to the rostromedial tegmental nucleus (RMTg) in the midbrain. These brain areas are now understood to mediate negative reinforcement, negative prediction errors, negative motivation, and aversion [34, 112–117]. The emerging roles of the LHb were motivation for the investigation of the nAChRs along the MHb-IPN pathway in the nicotine withdrawal syndrome, and behavioral pharmacological experiments indicated that these receptors are indeed important for this behavioral manifestation [93]. In mice chronically treated with nicotine, the nAChR antagonist, mecamylamine, was sufficient to produce nicotine withdrawal behaviors only when microinjected into the Hb or the IPN, but not when microinjected into other brain areas such as the hippocampus or cerebral cortex. Interestingly, experiments using mice bearing an α2 null mutation suggest that the roles of MHb-IPN pathway nAChRs in physical withdrawal are context specific [93, 97]. While this mutation produced decreased physical signs in animals assayed in their home environments, those assayed in novel environments exhibited potentiated physical signs [97]. Altogether, this series of experiments demonstrates the importance of the MHb-IPN pathway to the nicotine withdrawal syndrome.
5 The Affective Symptoms of Nicotine Withdrawal
Affective symptoms accompany the physical symptoms of nicotine withdrawal and have a major role in relapse [89]. These withdrawal symptoms can manifest in animals as anhedonia, conditioned place aversion, anxiety-related behaviors, and conditioned fear [9]. Anhedonia, the inability to experience pleasure from activities that are normally pleasurable, has been modeled in electrical self-stimulation assays [118]. In animals that are trained to press a lever to electrically stimulate reward nuclei, the threshold for continued brain stimulation is viewed as a measure of the rewarding effect of electrical stimulation. Anhedonic animals will exhibit an increase in this threshold, suggesting a decrease in the reward value of the stimulation. Increases in self-stimulation thresholds are observed during both spontaneous withdrawal [119, 120] and withdrawal precipitated by a systemic injection of the nAChR antagonist, mecamylamine [121].
Humans learn negative associations with specific environments, and this is modeled in rodents in the conditioned place aversion (CPA) paradigm, wherein animals try to avoid an environment that was previously paired with a negative stimulus [89]. Successful CPA in chronic nicotine-treated mice was induced by pairing an environment with injections of nAChR or opioid receptor antagonists, such as mecamylamine, dihydro-β-erythroidine, and naloxone [89, 122]. The aversion generated by the induced withdrawal was sufficient to cause animals to associate the aversive experience with a specific environment.
Smokers undergoing nicotine withdrawal may experience extreme anxiety resembling levels experienced by depressed individuals or those with anxiety disorders [123, 124]. Anxiety is routinely analyzed in rodents using the elevated plus maze (EPM) assay [125]. This assay is essentially a four-armed maze elevated above the ground, with two open arms and two closed arms. Mice generally prefer to remain in the closed arms, and the amount of time spent in the closed vs. open arms is considered a measure of the animal’s state of anxiety. Multiple investigations have demonstrated that both mice and rats experiencing nicotine withdrawal exhibit increased anxiety-like behavior in this assay [126, 127], mimicking symptoms of withdrawal observed in humans. It is possible that the MHb-IPN pathway also participates in this facet of the nicotine withdrawal syndrome. Mice null for the β4 nAChR subunit, which is densely expressed along the MHb-IPN pathway [111], exhibit modified anxiety-related behavior from wild-type mice [94]. β4 null mice display anxiolytic behavior in the elevated plus and staircase mazes but also display increased anxiety in the social isolation test, suggesting that nAChRs along the MHb-IPN pathway regulate anxiety-related behavior in a nuanced manner, with the output behavior dependent on specific environmental conditions.
A type of learning influenced by nicotine withdrawal is fear conditioning, a hippocampus-dependent form of Pavlovian learning where a conditioned stimulus is associated with an aversive unconditioned stimulus [128]. The conditioned fear assay measures the degree to which an animal is able to display this type of learning. Acutely administered nicotine enhances conditioned fear responses, regardless of whether the context is a foreground or background stimulus [129]. Furthermore, nicotine withdrawal impairs novel contextual fear conditioning but does not affect previously learned conditioned responses [130]. The impaired contextual fear conditioning occurs with or without pairing to an auditory stimulus (i.e., background vs. foreground) [131]. Evidence indicates that withdrawal-mediated deficits in contextual fear conditioning are mediated through β2* nAChRs [130, 132].
6 Other Medial Habenula-Dependent Behaviors Relevant to Nicotine Dependence
More recent studies have complemented the work in nicotine withdrawal to highlight roles for the MHb, in particular, with respect to its functional ties to nAChRs [34, 116, 117, 133]. Contributing further to the involvement of this brain area in aversion-related behaviors, those studies showed that α5* nAChRs along the MHb-IPN pathway mediate the aversive properties of nicotine at high doses, thereby regulating nicotine intake [34]. Using a self-administration paradigm, in which mice chose to intravenously self-administer nicotine over placebo, the authors demonstrated that mice lacking the α5 nAChR subunit will self-administer nicotine at substantially elevated levels compared to wild-type mice. That is, α5 null mice will continue to self-administer nicotine despite reaching a threshold at which wild-type mice would find nicotine to be aversive. They further demonstrated, through focal pharmacological microinjection and lentiviral RNAi knockdown or re-expression of the α5 subunit in the MHb or IPN, that α5* nAChRs in those nuclei are directly involved in the regulation of nicotine intake.
Other investigators used genomic and lentiviral overexpression of the β4 and α5 nAChR subunits, respectively, to further corroborate the role of α5β4* nAChRs in aversion to nicotine and described the functional interplay between these subunits [116]. They demonstrated that the β4 subunit enhances nAChR-mediated currents when overexpressed. Conversely, the α5 subunit competes with β4 to temper its effect, particularly when α5 is a variant (398N α5) that is linked to increased genetic risk of nicotine dependence in humans [99–106]. With β4 overexpression, mice experience reduced nicotine intake and nicotine-associated conditioned place aversion. Furthermore, lentiviral expression of the D398N α5 variant in the MHb alongside β4 overexpression reverted the nicotine intake phenotype to wild-type levels.
Utilizing immunotoxin-mediated ablation of two separate afferents to the MHb, another study dissected their contribution to MHb-dependent behavior [117]. Ablating the inputs from the nucleus triangularis (NT) in the septal area decreased anxiety-related behaviors in the open field, elevated plus maze, and marble burying task, while the analogous lesion of the bed nucleus of the anterior commissure (BAC) spared the performance in these tasks. Conversely, only ablation of the BAC inputs to the MHb caused deficits in the fear conditioning and passive avoidance tasks, indicating that these inputs are vital for proper fear expression.
Lastly, through a genetic approach, another group elaborated the influence of the MHb and IPN in behaviors involving motivational and emotive processes [133]. Neurons in the MHb were genetically ablated in mice using Cre-recombinase-mediated expression of diphtheria toxin A (DTA) in transgenic mice with strong Cre expression in the MHb and very sparse expression in few other brain areas. The expression of DTA induces apoptotic cell death [134] and, in these experiments, resulted in the dramatic loss of Nissl-stained neurons in the MHb. Furthermore, the IPN suffered reductions in acetylcholine concentration and overall volume. Thus, mice bearing the genetic ablation of the MHb (MHb:DTA) showed significant damage to the Hb-IPN pathway, with habenular damage predominantly restricted to the MHb.
As a consequence of the genetic ablation, many behaviors in MHb:DTA mice were severely impaired [133]. Where wild-type mice exhibited habituation to novel environments, habituation was absent in MHb:DTA mice. In the 5-choice serial reaction time task (5-CSRTT), which assesses impulsiveness, compulsiveness, and attention [135, 136], MHb:DTA mice were found to have increased premature responses, which is indicative of impulsive behavior. Compulsive behavior is displayed through perseverative nose-pokes following correct trials, even if reward is delivered only once for the initial correct choice. Also, sensorimotor gating is disrupted, as MHb:DTA mice have impaired acoustic pre-pulse inhibition, while baseline startle responses were unaffected.
To further investigate the MHb’s influence over impulsiveness and compulsiveness, delay- and effort-based decision-making tasks were used [133]. MHb:DTA mice are more likely to choose a low-reward choice if a high-reward choice is associated with a delay longer than 10 s or they encounter an obstacle barrier (effort). These results indicate that, as delay and effort increase, mice lacking the MHb will discount reward value more readily than wild-type mice and will select the option that provides the quickest reward.
In the open field arena (OFA) and elevated plus maze (EPM), which assess anxiety, MHb:DTA mice exhibited minor deficits in both tasks. MHb:DTA mice made slightly fewer entries to the center in the OFA and to the open arms of the EPM, together indicating a modest increase in anxiety. This appears in slight contrast to the previous study [117], which found decreased anxiety following ablation of afferent innervation from the NT, excitatory (glutamatergic and ATPergic) inputs into the MHb [137]. Our group demonstrated that mice null for the α5 and β4 nAChR subunits display reduced anxiety-like behavior in the EPM, suggesting a direct role for the nicotinic cholinergic system in these behaviors [94, 138].
To test whether the nAChRs along the MHb-IPN pathway modulate impulsivity and compulsivity, performance in the 5-CSRTT was measured following systemic nicotine administration [133]. In wild-type animals, nicotine administration induced delayed nose-pokes and increased errors due to omission. However, neither of these measures was affected in MHb:DTA mice. Furthermore, while habituation to a novel environment was accelerated by nicotine within and across sessions, neither of these measures was affected by nicotine in MHb:DTA mice. Altogether, this genetic ablation study strengthens the role of MHb-IPN pathway nAChRs in the modulation of these motivational and emotive behaviors.
7 The Potential Role of the MHb-IPN Pathway in Aversion and Negative Reinforcement: Inferences from LHb Studies
The role of the MHb-IPN pathway in basal- and nicotine-related behaviors is consistent with the established influences of the LHb on behavior [117, 139, 140]. Early work hinted at the role of the LHb in the representation of negative motivational value, negative reinforcement, and aversion [140–148]. Physiological studies reported the ability of the LHb (most likely due to its projections caudally, toward the RMTg) to modulate the reward-related centers [149, 150]. In rats, electrical stimulation of the LHb inhibited the firing of DA neurons in the SNc and VTA [151], as well as that of serotonergic neurons in the dorsal and median raphe nuclei [149].
A series of studies in macaques from Hikosaka and colleagues focusing on the behavioral roles of the LHb led to the maturation of our understanding of this modulatory circuit [112, 114, 115, 152, 153]. Since their seminal study, in which they demonstrated that LHb neurons fire in response to negative outcomes, as well as inhibit the firing of SNc DA neurons [112], they have expanded their studies to further clarify the behavioral roles of this nucleus. In cleverly designed experiments that varied the severity of negative outcomes in a task, so as to include punishments and lack of rewards as possible outcomes, LHb neurons fired most robustly in response to the worse-case scenario between the options of the particular task [114]. They further demonstrated that LHb neurons signal reward values derived from both the animal’s experience and inference [152]. Additional studies have also implicated the LHb in the representation of memory for reward, signaling of reward prediction errors, and learning of behaviors to avoid unpleasant outcomes [115, 152, 153]. The involvement of the Hb in error signaling during the prediction of rewards was subsequently demonstrated in humans using functional magnetic resonance imaging (fMRI) [35].
8 Dopaminergic Adaptations During Withdrawal
Given the global reach of nicotine within the brain, multiple mechanisms in different brain areas are likely responsible for the behavioral experiences during nicotine withdrawal. For example, the dopaminergic mesolimbic pathway participates in the mechanisms underlying nicotine abstinence manifestations. Principally consisting of dopaminergic projections from the VTA and SNc to the striatum, the mesolimbic pathway is known to influence behaviors associated with reward and motivation [154, 155]. Upon cessation of nicotine intake, the extracellular levels of DA decrease in the nucleus accumbens [156–160]. Consistent with withdrawal as a qualitatively aversive and generally unpleasant experience, this decrease in extracellular accumbal DA is also observed in withdrawal from many other drugs of abuse, such as that from ethanol, morphine, cocaine, and amphetamine [161, 162]. Therefore, common mechanisms and circuits operate to produce similar behavioral states during withdrawal to nicotine and other drugs of abuse. Because the mesolimbic pathway functionally interacts with the habenular circuitry, which is associated with negative reinforcement and aversion, a potential shift in the balance between these two systems could be responsible for the hypodopaminergic state during withdrawal from nicotine. As already mentioned, the LHb sends excitatory projections to the RMTg [140, 163, 164], which, in turn, projects GABAergic efferents to DA neurons in the VTA and SNc [112, 163]. This inhibitory control of RMTg projections onto DA neurons is a substantial modulator of their firing behavior [164].
Notably, α3β4* nAChRs within the MHb modulate the accumbal DA release in response to acute nicotine [165]. As projections from the MHb to LHb are documented [166], modulation of DA release by the MHb might occur via its anatomical connections with the LHb. However, as discussed above, there is robust evidence that the MHb-IPN pathway mediates aspects of nicotine aversion and withdrawal. Data suggest that MHb can affect the activity of the dopaminergic neurons in the ventral tegmental area (VTA) via the IPN [167], but the anatomical underpinning of this phenomenon remains unclear. One possibility through which the MHb-IPN pathway might regulate the activity of VTA DA neuron firing is via connections of the IPN to the laterodorsal tegmentum (LDTg) [168]. The LDTg is a cholinergic nucleus that sends inputs to the VTA that are required for proper bursting activity of DA neurons [169, 170]. Whether and how this circuit participates in the mechanisms of nicotine withdrawal remains to be established.
It should be noted that the hypodopaminergic state during nicotine withdrawal itself likely reflects a combination of many neuroadaptive processes triggered by withdrawal from nicotine. A reduction of striatal DA release certainly contributes and is accompanied by increased protein levels of vesicular monoamine transporter 2 (VMAT2) in the striatum [171]. An important player in DA reuptake, this elevation of VMAT2 is proposed to be a compensatory mechanism to counteract the deficiencies in DA release. Indeed, increased DA uptake into striatal synaptosomes was observed during nicotine withdrawal, as well as an increase in mRNA expression of another key participant in DA reuptake, the DA transporter (DAT), in the SNc and VTA [172]. Furthermore, an increase in DA clearance during nicotine withdrawal has been observed in vivo using microdialysis, corroborating the model of enhanced DA reuptake during withdrawal [158]. Regardless, these alterations in DA reuptake are transient, as the changes during withdrawal return to basal levels by 48 h of abstinence from nicotine [172]. Due to the synchronicity with nicotine withdrawal behavior, these alterations in DA release and reuptake might be a key mechanism underlying nicotine withdrawal symptoms [9].
Interestingly, DA transmission does not uniformly decrease throughout the brain during nicotine withdrawal. In contrast to striatal effects, DA release in the prefrontal cortex (PFC) is heightened during withdrawal to nicotine [159]. The role of this mesocortical innervation is related to the roles of some DA neurons in motivational salience, as those DA neurons signal the beginning of stimuli via phasic bursts, regardless of valence [115]. Since the experience during nicotine withdrawal can be significantly aversive and PFC DA release increases during aversive and stressful situations, the increased PFC DA release during nicotine withdrawal might coordinate the necessary mechanisms for the proper aversive behavioral response [173–177].
9 Conclusion
Addiction to nicotine, similar to other drugs of abuse, likely results from multiple mechanisms that involve interactions among various brain circuits. nAChRs, which are distributed on almost all brain circuits, stimulate responses to nicotine intake that ultimately produce an addicted state under prolonged use of the drug. Here, we discussed a specific brain circuit, the MHb-IPN pathway, that is involved in the nicotine withdrawal syndrome and other aversive aspects of nicotine use. Recent genome-based studies have identified genes encoding the α5, α3, and β4 subunits as important genetic determinants for the risk of nicotine dependence. All three of these subunits are highly expressed along the MHb-IPN pathway, highlighting its importance to overall addiction to nicotine. Resulting from a series of studies, the prevailing functional model of the Hb and its projection pathways is that it regulates dopaminergic and serotonergic function in the midbrain and, consequently, aversion and negative reinforcement. Given that withdrawal is arguably the most aversive and unpleasant experience associated with nicotine dependence, this model is consistent with the circuit’s roles in withdrawal behavior. Targeting the nAChRs along the MHb-IPN pathway should be a goal in future approaches at pharmacological treatment of nicotine dependence.
References
Vineis P, Alavanja M, Buffler P, et al. Tobacco and cancer: recent epidemiological evidence. J Natl Cancer Inst. 2004;96(2):99–106.
Kenfield SA, Stampfer MJ, Rosner BA, Colditz GA. Smoking and smoking cessation in relation to mortality in women. JAMA. 2008;299(17):2037–47.
Benowitz NL. Pharmacology of nicotine: addiction, smoking-induced disease, and therapeutics. Annu Rev Pharmacol Toxicol. 2009;49:57–71.
Tonini G, D’Onofrio L, Dell’Aquila E, Pezzuto A. New molecular insights in tobacco-induced lung cancer. Future Oncol. 2013;9(5):649–55.
Giovino GA, Mirza SA, Samet JM, et al. Tobacco use in 3 billion individuals from 16 countries: an analysis of nationally representative cross-sectional household surveys. Lancet. 2012;380(9842):668–79.
Kabir MA, Goh KL, Khan MH. A cross-country comparison of tobacco consumption among youths from selected South-Asian countries. BMC Public Health. 2013;13(1):379.
Dani JA, Bertrand D. Nicotinic acetylcholine receptors and nicotinic cholinergic mechanisms of the central nervous system. Annu Rev Pharmacol Toxicol. 2007;47:699–729.
Mansvelder HD, McGehee DS. Cellular and synaptic mechanisms of nicotine addiction. J Neurobiol. 2002;53(4):606–17.
De Biasi M, Dani JA. Reward, addiction, withdrawal to nicotine. Annu Rev Neurosci. 2011;34:105–30.
Piasecki TM, Jorenby DE, Smith SS, Fiore MC, Baker TB. Smoking withdrawal dynamics: I. Abstinence distress in lapsers and abstainers. J Abnorm Psychol. 2003;112(1):3–13.
Hughes JR. Effects of abstinence from tobacco: valid symptoms and time course. Nicotine Tob Res. 2007;9(3):315–27.
al’Absi M, Amunrud T, Wittmers LE. Psychophysiological effects of nicotine abstinence and behavioral challenges in habitual smokers. Pharmacol Biochem Behav. 2002;72(3):707–16.
Swan GE, Ward MM, Jack LM. Abstinence effects as predictors of 28-day relapse in smokers. Addict Behav. 1996;21(4):481–90.
De Biasi M, Salas R. Influence of neuronal nicotinic receptors over nicotine addiction and withdrawal. Exp Biol Med (Maywood). 2008;233(8):917–29.
Drenan RM, Lester HA. Insights into the neurobiology of the nicotinic cholinergic system and nicotine addiction from mice expressing nicotinic receptors harboring gain-of-function mutations. Pharmacol Rev. 2012;64(4):869–79.
Jasinska AJ, Zorick T, Brody AL, Stein EA. Dual role of nicotine in addiction and cognition: a review of neuroimaging studies in humans. Neuropharmacology. 2014;84C:111–22.
Role LW, Berg DK. Nicotinic receptors in the development and modulation of CNS synapses. Neuron. 1996;16(6):1077–85.
Picciotto MR, Mineur YS. Molecules and circuits involved in nicotine addiction: the many faces of smoking. Neuropharmacology. 2014;76:543–53.
McGehee DS, Role LW. Physiological diversity of nicotinic acetylcholine receptors expressed by vertebrate neurons. Annu Rev Physiol. 1995;57:521–46.
Alkondon M, Pereira EF, Barbosa CT, Albuquerque EX. Neuronal nicotinic acetylcholine receptor activation modulates gamma-aminobutyric acid release from CA1 neurons of rat hippocampal slices. J Pharmacol Exp Ther. 1997;283(3):1396–411.
Tomizawa M, Casida JE. Structure and diversity of insect nicotinic acetylcholine receptors. Pest Manag Sci. 2001;57(10):914–22.
Kent WJ, Sugnet CW, Furey TS, et al. The human genome browser at UCSC. Genome Res. 2002;12(6):996–1006.
Meyer LR, Zweig AS, Hinrichs AS, et al. The UCSC Genome Browser database: extensions and updates 2013. Nucleic Acids Res. 2013;41(Database issue):D64–9.
Nelson ME, Lindstrom J. Single channel properties of human alpha3 AChRs: impact of beta2, beta4 and alpha5 subunits. J Physiol. 1999;516(Pt 3):657–78.
Peng X, Gerzanich V, Anand R, Wang F, Lindstrom J. Chronic nicotine treatment up-regulates alpha3 and alpha7 acetylcholine receptor subtypes expressed by the human neuroblastoma cell line SH-SY5Y. Mol Pharmacol. 1997;51(5):776–84.
Tapia L, Kuryatov A, Lindstrom J. Ca2+ permeability of the (alpha4)3(beta2)2 stoichiometry greatly exceeds that of (alpha4)2(beta2)3 human acetylcholine receptors. Mol Pharmacol. 2007;71(3):769–76.
Wang F, Gerzanich V, Wells GB, et al. Assembly of human neuronal nicotinic receptor alpha5 subunits with alpha3, beta2, and beta4 subunits. J Biol Chem. 1996;271(30):17656–65.
Gerzanich V, Wang F, Kuryatov A, Lindstrom J. alpha 5 Subunit alters desensitization, pharmacology, Ca++ permeability and Ca++ modulation of human neuronal alpha 3 nicotinic receptors. J Pharmacol Exp Ther. 1998;286(1):311–20.
Kuryatov A, Berrettini W, Lindstrom J. Acetylcholine receptor (AChR) alpha5 subunit variant associated with risk for nicotine dependence and lung cancer reduces (alpha4beta2)(2)alpha5 AChR function. Mol Pharmacol. 2011;79(1):119–25.
Albuquerque EX, Pereira EF, Alkondon M, Rogers SW. Mammalian nicotinic acetylcholine receptors: from structure to function. Physiol Rev. 2009;89(1):73–120.
Woolf NJ. Cholinergic systems in mammalian brain and spinal cord. Prog Neurobiol. 1991;37(6):475–524.
Miwa JM, Freedman R, Lester HA. Neural systems governed by nicotinic acetylcholine receptors: emerging hypotheses. Neuron. 2011;70(1):20–33.
Sutherland RJ. The dorsal diencephalic conduction system: a review of the anatomy and functions of the habenular complex. Neurosci Biobehav Rev. 1982;6(1):1–13.
Fowler CD, Lu Q, Johnson PM, Marks MJ, Kenny PJ. Habenular alpha5 nicotinic receptor subunit signalling controls nicotine intake. Nature. 2011;471(7340):597–601.
Salas R, Baldwin P, de Biasi M, Montague PR. BOLD responses to negative reward prediction errors in human habenula. Front Hum Neurosci. 2010;4:36.
Karlin A. Emerging structure of the nicotinic acetylcholine receptors. Nat Rev Neurosci. 2002;3(2):102–14.
Sine SM. The nicotinic receptor ligand binding domain. J Neurobiol. 2002;53(4):431–46.
Galzi JL, Devillers-Thiery A, Hussy N, Bertrand S, Changeux JP, Bertrand D. Mutations in the channel domain of a neuronal nicotinic receptor convert ion selectivity from cationic to anionic. Nature. 1992;359(6395):500–5.
Berridge MJ, Lipp P, Bootman MD. The versatility and universality of calcium signalling. Nat Rev Mol Cell Biol. 2000;1(1):11–21.
Bootman MD, Berridge MJ, Roderick HL. Calcium signalling: more messengers, more channels, more complexity. Curr Biol. 2002;12(16):R563–5.
Sudhof TC. Calcium control of neurotransmitter release. Cold Spring Harb Perspect Biol. 2012;4(1):a011353.
Ross WN. Understanding calcium waves and sparks in central neurons. Nat Rev Neurosci. 2012;13(3):157–68.
Seguela P, Wadiche J, Dineley-Miller K, Dani JA, Patrick JW. Molecular cloning, functional properties, and distribution of rat brain alpha 7: a nicotinic cation channel highly permeable to calcium. J Neurosci. 1993;13(2):596–604.
Bertrand D, Galzi JL, Devillers-Thiery A, Bertrand S, Changeux JP. Mutations at two distinct sites within the channel domain M2 alter calcium permeability of neuronal alpha 7 nicotinic receptor. Proc Natl Acad Sci U S A. 1993;90(15):6971–5.
Kuryatov A, Gerzanich V, Nelson M, Olale F, Lindstrom J. Mutation causing autosomal dominant nocturnal frontal lobe epilepsy alters Ca2+ permeability, conductance, and gating of human alpha4beta2 nicotinic acetylcholine receptors. J Neurosci. 1997;17(23):9035–47.
Shen JX, Yakel JL. Nicotinic acetylcholine receptor-mediated calcium signaling in the nervous system. Acta Pharmacol Sin. 2009;30(6):673–80.
McGehee DS, Heath MJ, Gelber S, Devay P, Role LW. Nicotine enhancement of fast excitatory synaptic transmission in CNS by presynaptic receptors. Science. 1995;269(5231):1692–6.
Garduno J, Galindo-Charles L, Jimenez-Rodriguez J, et al. Presynaptic alpha4beta2 nicotinic acetylcholine receptors increase glutamate release and serotonin neuron excitability in the dorsal raphe nucleus. J Neurosci. 2012;32(43):15148–57.
Griguoli M, Scuri R, Ragozzino D, Cherubini E. Activation of nicotinic acetylcholine receptors enhances a slow calcium-dependent potassium conductance and reduces the firing of stratum oriens interneurons. Eur J Neurosci. 2009;30(6):1011–22.
Ji D, Dani JA. Inhibition and disinhibition of pyramidal neurons by activation of nicotinic receptors on hippocampal interneurons. J Neurophysiol. 2000;83(5):2682–90.
Hu M, Liu QS, Chang KT, Berg DK. Nicotinic regulation of CREB activation in hippocampal neurons by glutamatergic and nonglutamatergic pathways. Mol Cell Neurosci. 2002;21(4):616–25.
McKay BE, Placzek AN, Dani JA. Regulation of synaptic transmission and plasticity by neuronal nicotinic acetylcholine receptors. Biochem Pharmacol. 2007;74(8):1120–33.
Dani JA, Radcliffe KA, Pidoplichko VI. Variations in desensitization of nicotinic acetylcholine receptors from hippocampus and midbrain dopamine areas. Eur J Pharmacol. 2000;393(1–3):31–8.
Quick MW, Lester RA. Desensitization of neuronal nicotinic receptors. J Neurobiol. 2002;53(4):457–78.
Wooltorton JR, Pidoplichko VI, Broide RS, Dani JA. Differential desensitization and distribution of nicotinic acetylcholine receptor subtypes in midbrain dopamine areas. J Neurosci. 2003;23(8):3176–85.
Giniatullin R, Nistri A, Yakel JL. Desensitization of nicotinic ACh receptors: shaping cholinergic signaling. Trends Neurosci. 2005;28(7):371–8.
Briggs CA, McKenna DG. Activation and inhibition of the human alpha7 nicotinic acetylcholine receptor by agonists. Neuropharmacology. 1998;37(9):1095–102.
Papke RL, Porter Papke JK. Comparative pharmacology of rat and human alpha7 nAChR conducted with net charge analysis. Br J Pharmacol. 2002;137(1):49–61.
Fenster CP, Rains MF, Noerager B, Quick MW, Lester RA. Influence of subunit composition on desensitization of neuronal acetylcholine receptors at low concentrations of nicotine. J Neurosci. 1997;17(15):5747–59.
Paradiso KG, Steinbach JH. Nicotine is highly effective at producing desensitization of rat alpha4beta2 neuronal nicotinic receptors. J Physiol. 2003;553(Pt 3):857–71.
Brody AL, Mandelkern MA, London ED, et al. Cigarette smoking saturates brain alpha 4 beta 2 nicotinic acetylcholine receptors. Arch Gen Psychiatry. 2006;63(8):907–15.
Khiroug L, Giniatullin R, Sokolova E, Talantova M, Nistri A. Imaging of intracellular calcium during desensitization of nicotinic acetylcholine receptors of rat chromaffin cells. Br J Pharmacol. 1997;122(7):1323–32.
Khiroug L, Sokolova E, Giniatullin R, Afzalov R, Nistri A. Recovery from desensitization of neuronal nicotinic acetylcholine receptors of rat chromaffin cells is modulated by intracellular calcium through distinct second messengers. J Neurosci. 1998;18(7):2458–66.
Guo X, Lester RA. Regulation of nicotinic acetylcholine receptor desensitization by Ca2+. J Neurophysiol. 2007;97(1):93–101.
Rezvani K, Teng Y, Shim D, De Biasi M. Nicotine regulates multiple synaptic proteins by inhibiting proteasomal activity. J Neurosci. 2007;27(39):10508–19.
Lester HA, Xiao C, Srinivasan R, et al. Nicotine is a selective pharmacological chaperone of acetylcholine receptor number and stoichiometry. Implications for drug discovery. AAPS J. 2009;11(1):167–77.
Christianson JC, Green WN. Regulation of nicotinic receptor expression by the ubiquitin-proteasome system. EMBO J. 2004;23(21):4156–65.
Rezvani K, Teng Y, Pan Y, et al. UBXD4, a UBX-containing protein, regulates the cell surface number and stability of alpha3-containing nicotinic acetylcholine receptors. J Neurosci. 2009;29(21):6883–96.
Rezvani K, Teng Y, De Biasi M. The ubiquitin-proteasome system regulates the stability of neuronal nicotinic acetylcholine receptors. J Mol Neurosci. 2010;40(1–2):177–84.
Marks MJ, Pauly JR, Gross SD, et al. Nicotine binding and nicotinic receptor subunit RNA after chronic nicotine treatment. J Neurosci. 1992;12(7):2765–84.
Pauly JR, Marks MJ, Robinson SF, van de Kamp JL, Collins AC. Chronic nicotine and mecamylamine treatment increase brain nicotinic receptor binding without changing alpha 4 or beta 2 mRNA levels. J Pharmacol Exp Ther. 1996;278(1):361–9.
Vallejo YF, Buisson B, Bertrand D, Green WN. Chronic nicotine exposure upregulates nicotinic receptors by a novel mechanism. J Neurosci. 2005;25(23):5563–72.
Huang YY, Kandel ER, Levine A. Chronic nicotine exposure induces a long-lasting and pathway-specific facilitation of LTP in the amygdala. Learn Mem. 2008;15(8):603–10.
Aydin C, Oztan O, Isgor C. Nicotine-induced anxiety-like behavior in a rat model of the novelty-seeking phenotype is associated with long-lasting neuropeptidergic and neuroplastic adaptations in the amygdala: effects of the cannabinoid receptor 1 antagonist AM251. Neuropharmacology. 2012;63(8):1335–45.
Vezina P, McGehee DS, Green WN. Exposure to nicotine and sensitization of nicotine-induced behaviors. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31(8):1625–38.
Buisson B, Vallejo YF, Green WN, Bertrand D. The unusual nature of epibatidine responses at the alpha4beta2 nicotinic acetylcholine receptor. Neuropharmacology. 2000;39(13):2561–9.
Buisson B, Bertrand D. Chronic exposure to nicotine upregulates the human (alpha)4(beta)2 nicotinic acetylcholine receptor function. J Neurosci. 2001;21(6):1819–29.
Nashmi R, Dickinson ME, McKinney S, et al. Assembly of alpha4beta2 nicotinic acetylcholine receptors assessed with functional fluorescently labeled subunits: effects of localization, trafficking, and nicotine-induced upregulation in clonal mammalian cells and in cultured midbrain neurons. J Neurosci. 2003;23(37):11554–67.
Alkondon M, Albuquerque EX. Nicotinic receptor subtypes in rat hippocampal slices are differentially sensitive to desensitization and early in vivo functional up-regulation by nicotine and to block by bupropion. J Pharmacol Exp Ther. 2005;313(2):740–50.
Govind AP, Walsh H, Green WN. Nicotine-induced upregulation of native neuronal nicotinic receptors is caused by multiple mechanisms. J Neurosci. 2012;32(6):2227–38.
Benowitz NL. Nicotine addiction. N Engl J Med. 2010;362(24):2295–303.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association; 2000. Text Revision.
Volkow ND, Fowler JS, Wang GJ, Goldstein RZ. Role of dopamine, the frontal cortex and memory circuits in drug addiction: insight from imaging studies. Neurobiol Learn Mem. 2002;78(3):610–24.
Hogle JM, Kaye JT, Curtin JJ. Nicotine withdrawal increases threat-induced anxiety but not fear: neuroadaptation in human addiction. Biol Psychiatry. 2010;68(8):719–25.
Buchhalter AR, Fant RV, Henningfield JE. Novel pharmacological approaches for treating tobacco dependence and withdrawal: current status. Drugs. 2008;68(8):1067–88.
Yamamoto KI, Domino EF. Cholinergic agonist-antagonist interactions on neocortical and limbic EEG activation. Int J Neuropharmacol. 1967;6(5):357–73.
Kadoya C, Domino EF, Matsuoka S. Relationship of electroencephalographic and cardiovascular changes to plasma nicotine levels in tobacco smokers. Clin Pharmacol Ther. 1994;55(4):370–7.
Hughes JR, Gust SW, Skoog K, Keenan RM, Fenwick JW. Symptoms of tobacco withdrawal. A replication and extension. Arch Gen Psychiatry. 1991;48(1):52–9.
Kenny PJ, Markou A. Neurobiology of the nicotine withdrawal syndrome. Pharmacol Biochem Behav. 2001;70(4):531–49.
Malin DH, Lake JR, Newlin-Maultsby P, et al. Rodent model of nicotine abstinence syndrome. Pharmacol Biochem Behav. 1992;43(3):779–84.
Malin DH, Lake JR, Carter VA, et al. The nicotinic antagonist mecamylamine precipitates nicotine abstinence syndrome in the rat. Psychopharmacology (Berl). 1994;115(1–2):180–4.
Salas R, Pieri F, De Biasi M. Decreased signs of nicotine withdrawal in mice null for the beta4 nicotinic acetylcholine receptor subunit. J Neurosci. 2004;24(45):10035–9.
Salas R, Sturm R, Boulter J, De Biasi M. Nicotinic receptors in the habenulo-interpeduncular system are necessary for nicotine withdrawal in mice. J Neurosci. 2009;29(10):3014–8.
Salas R, Orr-Urtreger A, Broide RS, Beaudet A, Paylor R, De Biasi M. The nicotinic acetylcholine receptor subunit alpha 5 mediates short-term effects of nicotine in vivo. Mol Pharmacol. 2003;63(5):1059–66.
Flores CM, DeCamp RM, Kilo S, Rogers SW, Hargreaves KM. Neuronal nicotinic receptor expression in sensory neurons of the rat trigeminal ganglion: demonstration of alpha3beta4, a novel subtype in the mammalian nervous system. J Neurosci. 1996;16(24):7892–901.
Salas R, Main A, Gangitano D, De Biasi M. Decreased withdrawal symptoms but normal tolerance to nicotine in mice null for the alpha7 nicotinic acetylcholine receptor subunit. Neuropharmacology. 2007;53(7):863–9.
Lotfipour S, Byun JS, Leach P, et al. Targeted deletion of the mouse alpha2 nicotinic acetylcholine receptor subunit gene (Chrna2) potentiates nicotine-modulated behaviors. J Neurosci. 2013;33(18):7728–41.
Boulter J, O’Shea-Greenfield A, Duvoisin RM, et al. Alpha 3, alpha 5, and beta 4: three members of the rat neuronal nicotinic acetylcholine receptor-related gene family form a gene cluster. J Biol Chem. 1990;265(8):4472–82.
Saccone SF, Hinrichs AL, Saccone NL, et al. Cholinergic nicotinic receptor genes implicated in a nicotine dependence association study targeting 348 candidate genes with 3713 SNPs. Hum Mol Genet. 2007;16(1):36–49.
Thorgeirsson TE, Geller F, Sulem P, et al. A variant associated with nicotine dependence, lung cancer and peripheral arterial disease. Nature. 2008;452(7187):638–42.
Amos CI, Wu X, Broderick P, et al. Genome-wide association scan of tag SNPs identifies a susceptibility locus for lung cancer at 15q25.1. Nat Genet. 2008;40(5):616–22.
Bierut LJ, Stitzel JA, Wang JC, et al. Variants in nicotinic receptors and risk for nicotine dependence. Am J Psychiatry. 2008;165(9):1163–71.
Stevens VL, Bierut LJ, Talbot JT, et al. Nicotinic receptor gene variants influence susceptibility to heavy smoking. Cancer Epidemiol Biomarkers Prev. 2008;17(12):3517–25.
Berrettini W, Yuan X, Tozzi F, et al. Alpha-5/alpha-3 nicotinic receptor subunit alleles increase risk for heavy smoking. Mol Psychiatry. 2008;13(4):368–73.
Berrettini WH, Doyle GA. The CHRNA5-A3-B4 gene cluster in nicotine addiction. Mol Psychiatry. 2012;17(9):856–66.
Weiss RB, Baker TB, Cannon DS, et al. A candidate gene approach identifies the CHRNA5-A3-B4 region as a risk factor for age-dependent nicotine addiction. PLoS Genet. 2008;4(7):e1000125.
Boulter J, Evans K, Goldman D, et al. Isolation of a cDNA clone coding for a possible neural nicotinic acetylcholine receptor alpha-subunit. Nature. 1986;319(6052):368–74.
Duvoisin RM, Deneris ES, Patrick J, Heinemann S. The functional diversity of the neuronal nicotinic acetylcholine receptors is increased by a novel subunit: beta 4. Neuron. 1989;3(4):487–96.
Wada E, McKinnon D, Heinemann S, Patrick J, Swanson LW. The distribution of mRNA encoded by a new member of the neuronal nicotinic acetylcholine receptor gene family (alpha 5) in the rat central nervous system. Brain Res. 1990;526(1):45–53.
Sheffield EB, Quick MW, Lester RA. Nicotinic acetylcholine receptor subunit mRNA expression and channel function in medial habenula neurons. Neuropharmacology. 2000;39(13):2591–603.
Gahring LC, Persiyanov K, Rogers SW. Neuronal and astrocyte expression of nicotinic receptor subunit beta4 in the adult mouse brain. J Comp Neurol. 2004;468(3):322–33.
Matsumoto M, Hikosaka O. Lateral habenula as a source of negative reward signals in dopamine neurons. Nature. 2007;447(7148):1111–5.
Matsumoto M, Hikosaka O. Negative motivational control of saccadic eye movement by the lateral habenula. Prog Brain Res. 2008;171:399–402.
Matsumoto M, Hikosaka O. Representation of negative motivational value in the primate lateral habenula. Nat Neurosci. 2009;12(1):77–84.
Bromberg-Martin ES, Hikosaka O. Lateral habenula neurons signal errors in the prediction of reward information. Nat Neurosci. 2011;14(9):1209–16.
Frahm S, Slimak MA, Ferrarese L, et al. Aversion to nicotine is regulated by the balanced activity of beta4 and alpha5 nicotinic receptor subunits in the medial habenula. Neuron. 2011;70(3):522–35.
Yamaguchi T, Danjo T, Pastan I, Hikida T, Nakanishi S. Distinct roles of segregated transmission of the septo-habenular pathway in anxiety and fear. Neuron. 2013;78(3):537–44.
Paterson NE, Markou A. Animal models and treatments for addiction and depression co-morbidity. Neurotox Res. 2007;11(1):1–32.
Epping-Jordan MP, Watkins SS, Koob GF, Markou A. Dramatic decreases in brain reward function during nicotine withdrawal. Nature. 1998;393(6680):76–9.
Harrison AA, Liem YT, Markou A. Fluoxetine combined with a serotonin-1A receptor antagonist reversed reward deficits observed during nicotine and amphetamine withdrawal in rats. Neuropsychopharmacology. 2001;25(1):55–71.
Watkins SS, Stinus L, Koob GF, Markou A. Reward and somatic changes during precipitated nicotine withdrawal in rats: centrally and peripherally mediated effects. J Pharmacol Exp Ther. 2000;292(3):1053–64.
Suzuki T, Ise Y, Tsuda M, Maeda J, Misawa M. Mecamylamine-precipitated nicotine-withdrawal aversion in rats. Eur J Pharmacol. 1996;314(3):281–4.
Dani JA, Harris RA. Nicotine addiction and comorbidity with alcohol abuse and mental illness. Nat Neurosci. 2005;8(11):1465–70.
Pomerleau OF, Pomerleau CS, Mehringer AM, Snedecor SM, Ninowski R, Sen A. Nicotine dependence, depression, and gender: characterizing phenotypes based on withdrawal discomfort, response to smoking, and ability to abstain. Nicotine Tob Res. 2005;7(1):91–102.
Pellow S, Chopin P, File SE, Briley M. Validation of open:closed arm entries in an elevated plus-maze as a measure of anxiety in the rat. J Neurosci Methods. 1985;14(3):149–67.
Damaj MI, Kao W, Martin BR. Characterization of spontaneous and precipitated nicotine withdrawal in the mouse. J Pharmacol Exp Ther. 2003;307(2):526–34.
Irvine EE, Cheeta S, File SE. Tolerance to nicotine’s effects in the elevated plus-maze and increased anxiety during withdrawal. Pharmacol Biochem Behav. 2001;68(2):319–25.
Maren S, Phan KL, Liberzon I. The contextual brain: implications for fear conditioning, extinction and psychopathology. Nat Rev Neurosci. 2013;14(6):417–28.
Coe JW, Brooks PR, Vetelino MG, et al. Varenicline: an alpha4beta2 nicotinic receptor partial agonist for smoking cessation. J Med Chem. 2005;48(10):3474–7.
Portugal GS, Gould TJ. Genetic variability in nicotinic acetylcholine receptors and nicotine addiction: converging evidence from human and animal research. Behav Brain Res. 2008;193(1):1–16.
Andre JM, Gulick D, Portugal GS, Gould TJ. Nicotine withdrawal disrupts both foreground and background contextual fear conditioning but not pre-pulse inhibition of the acoustic startle response in C57BL/6 mice. Behav Brain Res. 2008;190(2):174–81.
Raybuck JD, Gould TJ. Nicotine withdrawal-induced deficits in trace fear conditioning in C57BL/6 mice – a role for high-affinity beta2 subunit-containing nicotinic acetylcholine receptors. Eur J Neurosci. 2009;29(2):377–87.
Kobayashi Y, Sano Y, Vannoni E, et al. Genetic dissection of medial habenula-interpeduncular nucleus pathway function in mice. Front Behav Neurosci. 2013;7:17.
Kobayakawa K, Kobayakawa R, Matsumoto H, et al. Innate versus learned odour processing in the mouse olfactory bulb. Nature. 2007;450(7169):503–8.
Robbins TW. The 5-choice serial reaction time task: behavioural pharmacology and functional neurochemistry. Psychopharmacology (Berl). 2002;163(3–4):362–80.
Patel S, Stolerman IP, Asherson P, Sluyter F. Attentional performance of C57BL/6 and DBA/2 mice in the 5-choice serial reaction time task. Behav Brain Res. 2006;170(2):197–203.
Qin C, Luo M. Neurochemical phenotypes of the afferent and efferent projections of the mouse medial habenula. Neuroscience. 2009;161(3):827–37.
Gangitano D, Salas R, Teng Y, Perez E, De Biasi M. Progesterone modulation of alpha5 nAChR subunits influences anxiety-related behavior during estrus cycle. Genes Brain Behav. 2009;8(4):398–406.
Hikosaka O, Sesack SR, Lecourtier L, Shepard PD. Habenula: crossroad between the basal ganglia and the limbic system. J Neurosci. 2008;28(46):11825–9.
Hikosaka O. The habenula: from stress evasion to value-based decision-making. Nat Rev Neurosci. 2010;11(7):503–13.
Brady JV, Nauta WJ. Subcortical mechanisms in emotional behavior: the duration of affective changes following septal and habenular lesions in the albino rat. J Comp Physiol Psychol. 1955;48(5):412–20.
Nielson HC, McIver AH. Cold stress and habenular lesion effects on rat behaviors. J Appl Physiol. 1966;21(2):655–60.
Dafny N, Qiao JT. Habenular neuron responses to noxious input are modified by dorsal raphe stimulation. Neurol Res. 1990;12(2):117–21.
Cohen SR, Melzack R. The habenula and pain: repeated electrical stimulation produces prolonged analgesia but lesions have no effect on formalin pain or morphine analgesia. Behav Brain Res. 1993;54(2):171–8.
Matsumoto N, Yahata F, Kawarada K, Kamata K, Suzuki TA. Tooth pulp stimulation induces c-fos expression in the lateral habenular nucleus of the cat. Neuroreport. 1994;5(17):2397–400.
Mahieux G, Benabid AL. Naloxone-reversible analgesia induced by electrical stimulation of the habenula in the rat. Brain Res. 1987;406(1–2):118–29.
Lee EH, Huang SL. Role of lateral habenula in the regulation of exploratory behavior and its relationship to stress in rats. Behav Brain Res. 1988;30(3):265–71.
Thornton EW, Bradbury GE, Davies C. Increased immobility in an automated forced swimming test following lesion of the habenula in rats: absence of evidence for a contribution from motor impairment. Behav Neurosci. 1990;104(1):37–43.
Wang RY, Aghajanian GK. Physiological evidence for habenula as major link between forebrain and midbrain raphe. Science. 1977;197(4298):89–91.
Herkenham M, Nauta WJ. Efferent connections of the habenular nuclei in the rat. J Comp Neurol. 1979;187(1):19–47.
Christoph GR, Leonzio RJ, Wilcox KS. Stimulation of the lateral habenula inhibits dopamine-containing neurons in the substantia nigra and ventral tegmental area of the rat. J Neurosci. 1986;6(3):613–9.
Bromberg-Martin ES, Matsumoto M, Hikosaka O. Dopamine in motivational control: rewarding, aversive, and alerting. Neuron. 2010;68(5):815–34.
Matsumoto M, Hikosaka O. Electrical stimulation of the primate lateral habenula suppresses saccadic eye movement through a learning mechanism. PLoS One. 2011;6(10):e26701.
Wise RA. Roles for nigrostriatal – not just mesocorticolimbic – dopamine in reward and addiction. Trends Neurosci. 2009;32(10):517–24.
Dani JA, De Biasi M. Mesolimbic dopamine and habenulo-interpeduncular pathways in nicotine withdrawal. Cold Spring Harb Perspect Med. 2013;3(6):a012138.
Hildebrand BE, Nomikos GG, Hertel P, Schilstrom B, Svensson TH. Reduced dopamine output in the nucleus accumbens but not in the medial prefrontal cortex in rats displaying a mecamylamine-precipitated nicotine withdrawal syndrome. Brain Res. 1998;779(1–2):214–25.
Rada P, Jensen K, Hoebel BG. Effects of nicotine and mecamylamine-induced withdrawal on extracellular dopamine and acetylcholine in the rat nucleus accumbens. Psychopharmacology (Berl). 2001;157(1):105–10.
Rahman S, Zhang J, Engleman EA, Corrigall WA. Neuroadaptive changes in the mesoaccumbens dopamine system after chronic nicotine self-administration: a microdialysis study. Neuroscience. 2004;129(2):415–24.
Carboni E, Bortone L, Giua C, Di Chiara G. Dissociation of physical abstinence signs from changes in extracellular dopamine in the nucleus accumbens and in the prefrontal cortex of nicotine dependent rats. Drug Alcohol Depend. 2000;58(1–2):93–102.
Gaddnas H, Piepponen TP, Ahtee L. Mecamylamine decreases accumbal dopamine output in mice treated chronically with nicotine. Neurosci Lett. 2002;330(3):219–22.
Weiss F, Markou A, Lorang MT, Koob GF. Basal extracellular dopamine levels in the nucleus accumbens are decreased during cocaine withdrawal after unlimited-access self-administration. Brain Res. 1992;593(2):314–8.
Rossetti ZL, Hmaidan Y, Gessa GL. Marked inhibition of mesolimbic dopamine release: a common feature of ethanol, morphine, cocaine and amphetamine abstinence in rats. Eur J Pharmacol. 1992;221(2–3):227–34.
Jhou TC, Geisler S, Marinelli M, Degarmo BA, Zahm DS. The mesopontine rostromedial tegmental nucleus: a structure targeted by the lateral habenula that projects to the ventral tegmental area of Tsai and substantia nigra compacta. J Comp Neurol. 2009;513(6):566–96.
Jhou TC, Fields HL, Baxter MG, Saper CB, Holland PC. The rostromedial tegmental nucleus (RMTg), a GABAergic afferent to midbrain dopamine neurons, encodes aversive stimuli and inhibits motor responses. Neuron. 2009;61(5):786–800.
McCallum SE, Cowe MA, Lewis SW, Glick SD. alpha3beta4 nicotinic acetylcholine receptors in the medial habenula modulate the mesolimbic dopaminergic response to acute nicotine in vivo. Neuropharmacology. 2012;63(3):434–40.
Kim U, Chang SY. Dendritic morphology, local circuitry, and intrinsic electrophysiology of neurons in the rat medial and lateral habenular nuclei of the epithalamus. J Comp Neurol. 2005;483(2):236–50.
Nishikawa T, Fage D, Scatton B. Evidence for, and nature of, the tonic inhibitory influence of habenulo-interpeduncular pathways upon cerebral dopaminergic transmission in the rat. Brain Res. 1986;373(1–2):324–36.
Groenewegen HJ, Ahlenius S, Haber SN, Kowall NW, Nauta WJ. Cytoarchitecture, fiber connections, and some histochemical aspects of the interpeduncular nucleus in the rat. J Comp Neurol. 1986;249(1):65–102.
Lodge DJ, Grace AA. The laterodorsal tegmentum is essential for burst firing of ventral tegmental area dopamine neurons. Proc Natl Acad Sci U S A. 2006;103(13):5167–72.
Grace AA, Floresco SB, Goto Y, Lodge DJ. Regulation of firing of dopaminergic neurons and control of goal-directed behaviors. Trends Neurosci. 2007;30(5):220–7.
Duchemin AM, Zhang H, Neff NH, Hadjiconstantinou M. Increased expression of VMAT2 in dopaminergic neurons during nicotine withdrawal. Neurosci Lett. 2009;467(2):182–6.
Hadjiconstantinou M, Neff NH. Nicotine and endogenous opioids: neurochemical and pharmacological evidence. Neuropharmacology. 2011;60(7–8):1209–20.
Thierry AM, Tassin JP, Blanc G, Glowinski J. Selective activation of mesocortical DA system by stress. Nature. 1976;263(5574):242–4.
Inglis FM, Moghaddam B. Dopaminergic innervation of the amygdala is highly responsive to stress. J Neurochem. 1999;72(3):1088–94.
Bradberry CW, Lory JD, Roth RH. The anxiogenic beta-carboline FG 7142 selectively increases dopamine release in rat prefrontal cortex as measured by microdialysis. J Neurochem. 1991;56(3):748–52.
Broersen LM, Abbate F, Feenstra MG, de Bruin JP, Heinsbroek RP, Olivier B. Prefrontal dopamine is directly involved in the anxiogenic interoceptive cue of pentylenetetrazol but not in the interoceptive cue of chlordiazepoxide in the rat. Psychopharmacology (Berl). 2000;149(4):366–76.
Kawasaki H, Kaufman O, Damasio H, et al. Single-neuron responses to emotional visual stimuli recorded in human ventral prefrontal cortex. Nat Neurosci. 2001;4(1):15–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Dao, D.Q., Salas, R., De Biasi, M. (2014). Nicotinic Acetylcholine Receptors Along the Habenulo-Interpeduncular Pathway: Roles in Nicotine Withdrawal and Other Aversive Aspects. In: Lester, R. (eds) Nicotinic Receptors. The Receptors, vol 26. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-1167-7_18
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1167-7_18
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-1166-0
Online ISBN: 978-1-4939-1167-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)